
Best Nursing Research Topics for Students
What is a nursing research paper.
- What They Include
- Choosing a Topic
- Best Nursing Research Topics
- Research Paper Writing Tips

Writing a research paper is a massive task that involves careful organization, critical analysis, and a lot of time. Some nursing students are natural writers, while others struggle to select a nursing research topic, let alone write about it.
If you're a nursing student who dreads writing research papers, this article may help ease your anxiety. We'll cover everything you need to know about writing nursing school research papers and the top topics for nursing research.
Continue reading to make your paper-writing jitters a thing of the past.
A nursing research paper is a work of academic writing composed by a nurse or nursing student. The paper may present information on a specific topic or answer a question.
During LPN/LVN and RN programs, most papers you write focus on learning to use research databases, evaluate appropriate resources, and format your writing with APA style. You'll then synthesize your research information to answer a question or analyze a topic.
BSN , MSN , Ph.D., and DNP programs also write nursing research papers. Students in these programs may also participate in conducting original research studies.
Writing papers during your academic program improves and develops many skills, including the ability to:
- Select nursing topics for research
- Conduct effective research
- Analyze published academic literature
- Format and cite sources
- Synthesize data
- Organize and articulate findings
About Nursing Research Papers
When do nursing students write research papers.
You may need to write a research paper for any of the nursing courses you take. Research papers help develop critical thinking and communication skills. They allow you to learn how to conduct research and critically review publications.
That said, not every class will require in-depth, 10-20-page papers. The more advanced your degree path, the more you can expect to write and conduct research. If you're in an associate or bachelor's program, you'll probably write a few papers each semester or term.
Do Nursing Students Conduct Original Research?
Most of the time, you won't be designing, conducting, and evaluating new research. Instead, your projects will focus on learning the research process and the scientific method. You'll achieve these objectives by evaluating existing nursing literature and sources and defending a thesis.
However, many nursing faculty members do conduct original research. So, you may get opportunities to participate in, and publish, research articles.
Example Research Project Scenario:
In your maternal child nursing class, the professor assigns the class a research paper regarding developmentally appropriate nursing interventions for the pediatric population. While that may sound specific, you have almost endless opportunities to narrow down the focus of your writing.
You could choose pain intervention measures in toddlers. Conversely, you can research the effects of prolonged hospitalization on adolescents' social-emotional development.
What Does a Nursing Research Paper Include?
Your professor should provide a thorough guideline of the scope of the paper. In general, an undergraduate nursing research paper will consist of:
Introduction : A brief overview of the research question/thesis statement your paper will discuss. You can include why the topic is relevant.
Body : This section presents your research findings and allows you to synthesize the information and data you collected. You'll have a chance to articulate your evaluation and answer your research question. The length of this section depends on your assignment.
Conclusion : A brief review of the information and analysis you presented throughout the body of the paper. This section is a recap of your paper and another chance to reassert your thesis.
The best advice is to follow your instructor's rubric and guidelines. Remember to ask for help whenever needed, and avoid overcomplicating the assignment!
How to Choose a Nursing Research Topic
The sheer volume of prospective nursing research topics can become overwhelming for students. Additionally, you may get the misconception that all the 'good' research ideas are exhausted. However, a personal approach may help you narrow down a research topic and find a unique angle.
Writing your research paper about a topic you value or connect with makes the task easier. Additionally, you should consider the material's breadth. Topics with plenty of existing literature will make developing a research question and thesis smoother.
Finally, feel free to shift gears if necessary, especially if you're still early in the research process. If you start down one path and have trouble finding published information, ask your professor if you can choose another topic.
The Best Research Topics for Nursing Students
You have endless subject choices for nursing research papers. This non-exhaustive list just scratches the surface of some of the best nursing research topics.
1. Clinical Nursing Research Topics
- Analyze the use of telehealth/virtual nursing to reduce inpatient nurse duties.
- Discuss the impact of evidence-based respiratory interventions on patient outcomes in critical care settings.
- Explore the effectiveness of pain management protocols in pediatric patients.
2. Community Health Nursing Research Topics
- Assess the impact of nurse-led diabetes education in Type II Diabetics.
- Analyze the relationship between socioeconomic status and access to healthcare services.
3. Nurse Education Research Topics
- Review the effectiveness of simulation-based learning to improve nursing students' clinical skills.
- Identify methods that best prepare pre-licensure students for clinical practice.
- Investigate factors that influence nurses to pursue advanced degrees.
- Evaluate education methods that enhance cultural competence among nurses.
- Describe the role of mindfulness interventions in reducing stress and burnout among nurses.
4. Mental Health Nursing Research Topics
- Explore patient outcomes related to nurse staffing levels in acute behavioral health settings.
- Assess the effectiveness of mental health education among emergency room nurses .
- Explore de-escalation techniques that result in improved patient outcomes.
- Review the effectiveness of therapeutic communication in improving patient outcomes.
5. Pediatric Nursing Research Topics
- Assess the impact of parental involvement in pediatric asthma treatment adherence.
- Explore challenges related to chronic illness management in pediatric patients.
- Review the role of play therapy and other therapeutic interventions that alleviate anxiety among hospitalized children.
6. The Nursing Profession Research Topics
- Analyze the effects of short staffing on nurse burnout .
- Evaluate factors that facilitate resiliency among nursing professionals.
- Examine predictors of nurse dissatisfaction and burnout.
- Posit how nursing theories influence modern nursing practice.
Tips for Writing a Nursing Research Paper
The best nursing research advice we can provide is to follow your professor's rubric and instructions. However, here are a few study tips for nursing students to make paper writing less painful:
Avoid procrastination: Everyone says it, but few follow this advice. You can significantly lower your stress levels if you avoid procrastinating and start working on your project immediately.
Plan Ahead: Break down the writing process into smaller sections, especially if it seems overwhelming. Give yourself time for each step in the process.
Research: Use your resources and ask for help from the librarian or instructor. The rest should come together quickly once you find high-quality studies to analyze.
Outline: Create an outline to help you organize your thoughts. Then, you can plug in information throughout the research process.
Clear Language: Use plain language as much as possible to get your point across. Jargon is inevitable when writing academic nursing papers, but keep it to a minimum.
Cite Properly: Accurately cite all sources using the appropriate citation style. Nursing research papers will almost always implement APA style. Check out the resources below for some excellent reference management options.
Revise and Edit: Once you finish your first draft, put it away for one to two hours or, preferably, a whole day. Once you've placed some space between you and your paper, read through and edit for clarity, coherence, and grammatical errors. Reading your essay out loud is an excellent way to check for the 'flow' of the paper.
Helpful Nursing Research Writing Resources:
Purdue OWL (Online writing lab) has a robust APA guide covering everything you need about APA style and rules.
Grammarly helps you edit grammar, spelling, and punctuation. Upgrading to a paid plan will get you plagiarism detection, formatting, and engagement suggestions. This tool is excellent to help you simplify complicated sentences.
Mendeley is a free reference management software. It stores, organizes, and cites references. It has a Microsoft plug-in that inserts and correctly formats APA citations.
Don't let nursing research papers scare you away from starting nursing school or furthering your education. Their purpose is to develop skills you'll need to be an effective nurse: critical thinking, communication, and the ability to review published information critically.
Choose a great topic and follow your teacher's instructions; you'll finish that paper in no time.

Joleen Sams is a certified Family Nurse Practitioner based in the Kansas City metro area. During her 10-year RN career, Joleen worked in NICU, inpatient pediatrics, and regulatory compliance. Since graduating with her MSN-FNP in 2019, she has worked in urgent care and nursing administration. Connect with Joleen on LinkedIn or see more of her writing on her website.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. We will not sell or distribute your email address to any third party, and you may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.
List of 350 Brilliant Nursing Research Topics to Investigate in 2024

Nursing education is challenging. Writing hundreds of tedious nursing research pieces is the most frustrating part. But we know how to help you! Discover 350 exciting nursing research topics and learn how to choose the best one.
- Primary Care Topics
- Public Health Topics
- Emergency Nursing Topics
- Midwifery Topics
- Neonatal Nursing Topics
- Pediatric Research Topics
- Nutrition Topics
- Mental Health Topics
- Healthcare Management Topics
- Medical Ethics Topics
- Nursing Leadership Topics
- Qualitative and Quantitative Research
- How to Choose a Nursing Topic
Process of Nursing Research
350 interesting nursing research topics.
Nursing research topics for college students can cover various areas of this field. Below you will find a list of 350 exciting ideas, which we have divided into different areas of activity. No matter what nursing research is in your sphere of interest. We’ve got you covered! You can also check research essay samples on the same topic for more inspiration.
Primary Care Research Topics
Primary care is the leading clinical service that sustains the health of an entire nation. The study of this topic is mandatory for the stable development of the healthcare system. Here are primary nursing research titles examples:
- What healthcare problems can be in primary care?
- The role of private health care providers in primary care.
- Peculiarities of vaccination in rural areas.
- Basic methods for assessing the quality of primary care .
- The role of modern technology in primary care .
- Basic techniques of evaluating the patient’s health .
- Private sector activities in primary care .
- The necessity to provide childcare services.
- Primary care and chronic pain problem .
- Vaccination programs : pros and cons.
- The role of social workers in primary care.
- Responsibility of the pharmacist for public health.
- Effective methods of asthma prevention.
- Advantages and disadvantages of home nursing care.
- How can primary care system help fight depression?
- Vaccination of the elderly: challenges and potential benefits.
- Principles of preventive medicine: primary care for the elderly.
- Migraine diagnosis and treatment methods.
- Innovative methods in cardiology .
- Major causes of anxiety disorders in adults.
- The problem of obesity treatment in primary care .
- Effective ways of taking anamnesis.
- Methods for diagnosing stroke in the elderly.
- Basic precautions for Parkinson’s disease .
- Basic requirements for intensive care .
- Connection of primary care and information technology training .
- Sleep disorders in women.
- Standard protocol for the treatment of headache in adults.
- Basic guidelines for primary care for disaster victims.
- The role of government agencies in primary care.
Based on previous papers, you can try to come up with your nursing research topics, for example, on infection control.
Research Topics in Public Health
The public health area has a strong connection with government issues. However, it is doctors who study the basis of all problems. So, let’s check out these special nursing research paper topics!
- The role of governmental organizations in the public health system .
- Effectiveness of government programs to prevent drug addiction .
- What role do parents play in promoting children’s health?
- Features of the school nurses’ work.
- The importance of proper nutrition and exercise .
- Telemedicine : advantages and disadvantages.
- The role of government in providing nursing education .
- The importance of long-term care facilities to the healthcare system .
- Discovering public health’s primary functions .
- Promoting healthy lifestyle in old age.
- Sedentary change programs for adolescents.
- Educational strategies for healthcare organizations in social media.
- Ways to educate young people about a positive body image .
- Formation of public behavior in the problem of cancer prevention.
- Occupational health and safety for workers in hazardous professions.
- Connection of modern technologies and public health system .
- Government AIDS awareness programs.
- State programs to increase awareness of heart disease .
- Government programs aimed at maintaining a healthy work environment .
- Health promotion methods.
- Companies against alcohol: examples from history.
- Public health policies: sugary drink tax .
- Raising awareness of the importance of vaccines .
- How is lung cancer related to air condition?
- Promotion of activity among children with disabilities .
- Disease eradication as a leading public health policy target .
- Government mental health awareness programs.
- Improving individual health as a way to counter epidemics .
- Ways of transmission of infectious diseases .
- Educating children about the importance of sports .
Public health is an excellent topic choice for a nursing dissertation. Try it!
Emergency Nursing Research Topics
New studies are essential for new practical approaches for nurses in emergencies. Try to discover new methods with these critical care nursing research topics!
- What role can stress play in emergency nursing?
- How to deal with anaphylactic shock?
- Effective methods of providing emergency care .
- Features of decision-making by a nurse in critical situations.
- Analysis of the effectiveness of emergency assistance in case of accidents.
- Analysis of the extreme degrees of pain in a patient.
- Diagnosing problems in ER.
- Emergency training methods.
- How to increase chances to save a drowning person?
- Models for reducing violence in emergency departments .
- The problem of rural residents’ access to ambulance services.
- Can family stay close to the patient during resuscitation?
- What effect do tasers have on the development of heart disease ?
- Diagnosing sepsis in emergencies.
- Effective methods of dealing with the effects of using pepper sprays.
- Screening for alcohol and drug addiction in adolescents.
- The role of ambulance crews in the fight against human trafficking .
- Identification and assistance to victims of violence.
- How to deal with unwanted patient behavior?
- Pediatric trauma and shock.
- Psychiatric screening in first aid cars.
- Ways to develop tolerance in first-aid workers.
- Effective ER worker behavior models.
- The role of private clinics in providing emergency services.
- The role of nurses in the ambulance crew.
- Common causes of death in ER patients.
- Correct gender policy towards ER staff.
- How to organize a working emergency care system?
- How to help relatives survive the death of a patient?
- Techniques for teaching nurses to diagnose and respond to life threats quickly.
These nursing research topics for critical care would be an excellent choice for your papers!
Midwifery Research Topics
Midwifery is one of the more challenging medical areas. We picked 30 of the best nursing research topics on pregnancy and prenatal care to help you improve your knowledge! Take a look:
- How can midwifery recognize domestic violence?
- Excess weight problems during pregnancy .
- How to analyze the effectiveness of childbirth ?
- Disease prevention during pregnancy.
- Effective methods of newborn resuscitation.
- Features of adolescent education in gynecology.
- Prenatal nursing care.
- Precautions for preterm labor.
- Rules of conduct for staff in the delivery room.
- Basic rules for saving mother and child.
- Preparing staff and the patient for a caesarean section.
- Preventing depression during pregnancy .
- Features and importance of family planning .
- Childbirth in water: advantages and disadvantages.
- Features of caring for pregnant women with breast cancer .
- The influence of the autonomic nervous system on the course of pregnancy.
- Methods for predicting preeclampsia.
- Diseases of the cervix associated with human papillomavirus .
- Frequency and possible complications of pregnancy and cervical disease.
- Treatment tactics of pregnancy complications in women with disorders of the upper urinary tract.
- Identifying asymptomatic pregnancy complications.
- The use of modern technologies in the treatment of fetal diseases.
- Features of the reproductive system after termination of pregnancy.
- Reasons for using iodine supplementation during pregnancy.
- Prevention of complications after operations on the pelvic organs .
- Impact of epilepsy on reproductive health .
- Features of reproductive behavior in students and ways to correct it.
- The effect of oral contraceptives on the contents of immune complexes in the blood.
- Operative delivery and influence on the child.
- Psychological assistance to patients with infertility .
Remember some of these nursing research topics on midwifery. Profs love them!
Neonatal Nursing Research Topics
Neonatal studies are one of the most innovative medical spheres. Check out this brilliant list of research topics for nursing students in the neonatal area. They will help you better understand the neonatal care importance.
- The importance of hand hygiene in neonatal units .
- Features of neonatal practice in rural areas.
- The leading causes of child mortality .
- How neonatal care has evolved in recent decades.
- Hygiene of newborns and skincare for babies.
- Postpartum infant care basics.
- Principles of breastfeeding infants.
- Predicting feeding problems and treatments.
- The leading causes of seizures in newborns and methods of treatment.
- Eating disorder in infants.
- Methods for predicting diseases in newborn children.
- Effective medical practices for babies.
- Nursing ethics for newborn care.
- Features of modern neonatal practices.
- Features of the development of the pulmonary tract of newborns.
- Studies of the lungs of a newborn: functions and structural features.
- Influence of inflammatory processes on the infant’s brain.
- The role of biomarkers in the diagnosis of traumatic brain injury in infants.
- The importance of neonatal health services.
- Basic strategies for modeling neonatal education.
- Monitoring the quality of neonatal services.
- Influence of neonatal care on the further treatment of a newborn.
- Impact of maternal obesity on infant development.
- Causes of abnormal neurological development in children.
- Use of hormones to regulate fetal lung development.
- Diagnosis of diaphragmatic hernia in infants.
- Potential lung disease in premature babies.
- Using nitric oxide to treat premature babies.
- Parental drug use and effects on fetal neurological development.
- Use of biomarkers for neonatal sepsis.
A nursing dissertation on neonatal issues is always a wise choice!
Pediatric Nursing Research Topics
Studies in pediatrics are aimed to help students discover children’s health issues to solve. Innovative approaches are mandatory to fight modern challenges. Check out these research topics for nursing students; they’ll help you become more informed:
- The importance of self-care nursing in pediatrics.
- Features of the treatment of children with autism .
- Childhood obesity problem.
- Features of vaccination of minors.
- Therapy for speech disorders .
- Causes of diabetes in young people.
- Music therapy and phlebotomy.
- Suboptimal diabetes: causes and methods of intervention.
- Causes of increased fatigue in adolescents.
- HIV prevention in adolescence.
- Preventing unwanted teenage pregnancies .
- Features of the use of painkillers in children.
- Methods for analyzing adolescent behavior.
- Features of the work of the pediatric department in schools.
- The importance of health promotion in pediatrics .
- Ways to connect with your child.
- Pediatric care basics.
- How can a healthcare professional deal with adolescent aggression ?
- Reducing the risk in children receiving oxygen therapy .
- The role of molecular markers in the diagnosis of childhood leukemia .
- Psychological help for children with cancer .
- Assessment of language models in children with autism .
- The use of stem cells in the treatment of childhood diseases.
- How do environmental problems affect the development of a child’s body?
- Implications of passive smoker syndrome for children.
- Possible complications of measles in children .
- Methods for diagnosing asthma in children .
- Common causes of Tourette’s syndrome in children.
- How does anorexia affect cognitive function in children?
- Diagnosis of ear infections in childhood.
We guess this ultimate list of research topics in pediatric nursing will be helpful for you!
Nutrition Research Topics for College Students
The eating habits of modern people can be harmful to the body. Therefore, doctors are seriously studying the current problems in this area. Here you can find tons of excellent nursing research topics on nutrition and its possible issues.
- What are referral reasons for the dietary assessment?
- Nutrition assistance for the elderly.
- Effects of stress on childhood metabolism .
- Prevention of obesity in adolescents.
- Linking diet to behavioral changes.
- How social media influences teen food choices .
- Patient nutrition problem in healthcare policy .
- Predicting and assessing diabetes .
- The problem of dietary intervention in the elderly.
- Promoting healthy eating as a way to fight obesity.
- Nursing promotion of healthy homemade food.
- Effects of good nutrition on fetal development .
- How does nutrition affect a child’s development ?
- Root causes of weight gain : a clinical study.
- Common diseases caused by poor nutrition .
- Nutrition screening for the elderly.
- The nutritional problem of children with autism .
- The importance of proper nutrition during pregnancy .
- Baby food: preventing eating disorders.
- Diet as a cause of dementia development in adults.
- Osteoporosis : the role of diet in disease prevention.
- The role of diet in healthy aging.
- What is the relationship between cancer and diet ?
- Nursing role in the safety of nutrition.
- The main benefits of a healthy diet : advice to patients.
- The role of parents in maintaining healthy eating habits in children.
- The relationship between healthy eating and cognitive development .
- Modern trends in youth nutrition.
- The nurse’s role in maintaining quality nutrition for pregnant women .
- Innovative nursing nutritional care.
Now let’s move to the next section – research topics in mental health!
Mental Health Nursing Research Topics
Mental health problems are more relevant now than ever. According to the National Alliance on Mental Illness , nearly 20% of the US adult population suffers from mental health problems. That’s why psychiatry research topics capture the interest of college students.
- The importance of nursing in mental health safety .
- Features of mental disorder in alcohol dependence .
- How does police work affect mental health?
- The connection between video games and the development of teenage aggression.
- How is schizophrenia diagnosed?
- Main theories in mental health studies .
- Features of bipolar mental disorder .
- Causes and prevention of drug addiction .
- Mental health problems of athletes after physical injuries .
- Conditions for the use of psychotherapy .
- Reasons and methods for tackling health imbalances.
- The influence of phone usage on mental health .
- Brain stimulation techniques.
- Diversity of sexual orientation psychology features.
- Methods for dealing with physical violence.
- The effectiveness of traditional methods of treating mental illness .
- Features of mental support for the patient’s relatives.
- The role of nurses in the management of geriatric patients with mental disorders.
- Combating burnout in the practice of healthcare professionals.
- The problem of war veterans’ mental health .
- The phenomenon of occupational deformation as a type of mental disorder.
- Chest pain as a symptom of mental health problems in adults.
- The relationship between increased risk of cancer and depression.
- Basic treatments for dementia .
- Nursing refugee mental health help .
- The practice of mirror therapy in rehabilitation.
- Methods to help victims of violence.
- Helping patients after a stroke .
- The use of antipsychotics : benefits and harms.
- How belly massage helps fight residual stomach volume.
We believe you’re going to find one of the best psychiatric nursing research topics!
Healthcare Management Research Topics
The effective functioning of the health care system is impossible without competent leadership. Therefore, nursing research study topics on healthcare management are as important as the others!
- The importance of financial management for the healthcare industry .
- Assessment of the economic component of primary health care .
- How does bias affect healthcare funding?
- How to properly organize health care at home?
- The Importance of a Unified Nursing Code.
- How risk management affects healthcare projects?
- Gender policy in health management .
- Features of the initial stages of private medical practice.
- The importance of the apology law.
- Features of selling medical marijuana .
- Features of healthcare contracts.
- The problem of human resources in the healthcare industry .
- The problem of the shortage of men in healthcare.
- Medicare : how to get benefits.
- How to improve the minimum level of nursing training ?
- Modern trends in the healthcare management area .
- Staff uniform rules.
- Legal risks of medical personnel .
- Gender bias in nursing.
- Features of the organization of the first aid service in private sector.
- Risk management in healthcare.
- The connection of healthcare and conflict management .
- Ways to solve staffing problems in healthcare.
- Ensuring the personnel safety from infectious diseases .
- Strategies to improve the emotional health of employees.
- What is the danger of not having enough nursing staff for patients?
- Personnel policy in public medical institutions.
- International nursing training.
- Basic principles of management in healthcare facilities.
- Possible ways to get a nursing promotion.
These nursing research titles on healthcare management will impress your professors!
Medical Ethics Research Paper Topics
Controversial issues in the field of medical ethics are felt more and more acutely every year. That is why they need to be solved, and research topics related to nursing ethics present a good opportunity for highlighting them:
- The role of ethical values in the nursing decision-making process .
- Particular ethics of data collection in primary care.
- The ethical dilemma of abortion.
- Moral choice in opioid addiction .
- Features of ethics in helping the homeless .
- Ethics of care for patients with mental disorders .
- Phantom pain phenomenon.
- Features of cultural perception in the work of nurses.
- How can religious beliefs affect medical ethics?
- The role of relatives in the treatment of geriatric patients .
- Ethics of the need to increase sales in medicine.
- The problem of sexualizing the image of a nurse.
- The importance of solving moral dilemmas in nursing .
- Assisting female patients by male nurses .
- What are the main medical ethics principles?
- Ethics of care for geriatric patients.
- The problem of compulsory vaccination : solutions.
- The dilemma of artificial feeding of patients.
- Ethics of nursing in preventive medicine.
- The importance of a hospital work ethic.
- The U.S. standard of ethics for nursing .
- The dilemma of medical ethics .
- The difference in medical ethics in Asian countries and European countries.
- How can medical ethics conflict with religious beliefs?
- Assisting suicide as a dilemma in medical ethics.
- The ethical problem of marijuana usage for medical purposes .
- The impact of cultural patterns on medical ethics .
- Child maltreatment : a medical ethics dilemma.
- Implementation of international medical ethics standards for healthcare development.
- Methods for monitoring compliance with medical ethics.
Nursing ethics research questions have a tendency to be the most interesting ones!
Nursing Leadership Paper Topics
The principle of developing leadership among nurses is vital for improving the performance of any clinic. This list consists of 30 nursing research topics about leadership in healthcare field:
- What role does leadership play in nursing?
- Which skills are necessary for effective nursing leadership performance?
- The nurse’s role in providing quality health care .
- Why is it important for nurses to attend medical conferences?
- Features of the classification of nurses.
- What is a retention strategy for experienced nurses?
- How does nursing leadership development affect patient outcomes?
- The problem of obtaining a diploma for a nurse.
- Nursing leadership : key challenges and opportunities.
- Ethical issues in nursing leadership .
- Protecting staff interests in nursing management .
- Analyzing college students’ nursing leadership experience .
- Effective nursing leadership styles .
- Ways to develop nursing leadership in private healthcare facilities.
- Nursing manual: Betty Newman theory.
- The importance of intuitiveness in the workplace.
- The importance of conflict resolution in the nursing leadership sphere .
- Patient advocacy opportunities for the lead nurse.
- Nursing manual: theory of intellectual capital.
- Effective models of professional practice in nursing.
- Professional opportunities for nursing graduates in nursing leadership .
- What are modern approaches in nursing leadership?
- Transformational leadership model for nursing.
- Fundamental theories for effective nursing leadership .
- Methods for applying leadership theories to nursing .
- What is the need for effective nursing leadership ?
- Methods for monitoring the effectiveness of nursing leadership .
- Principles of delegation of authority in nursing leadership practice.
- The importance of nursing leadership in strategic hospital planning.
- Nursing leadership as a method to retain experienced staff.
Evidence-based nursing topics on leadership can become a great start to your career!
Easy Topics for Nursing Qualitative and Quantitative Research
The division into qualitative and quantitative research can be confusing. But don’t worry, we’ll help you figure it out! Each type of nursing research topic and other materials may depend on dry numbers or subjective opinions. Keep reading for more detailed information and examples of quantitative and qualitative research topics in nursing!
Qualitative vs. Quantitative Nursing Research
Empirical research methods can be divided into two broad categories: quantitative and qualitative. As their name suggests, each view relies on specific types of data. Therefore, your nursing paper topics can also reveal either qualitative or quantitative aspects of the problem. Let’s take a quick look at the main differences between these two methods.
The quantitative method relies entirely on numbers and statistics. Your task is to find patterns and come to a conclusion by analyzing a large amount of data. This type of nursing research is as structured and objective as possible. These are the quantitative method characteristics:
- Sources of information are polls, reviews, records, documents.
- The deductive methodology involved.
- As objective as possible.
- The main content is numbers and data.
- Validity depends on the selected analysis tools.
The qualitative method , on the contrary, is a reflection of the author’s thoughts and conclusions. It depends entirely on the depth of understanding of the problem and the existing materials on the nursing thesis topics. The task of the researcher is to analyze previous works and create their theory through reflection. Check the qualitative method characteristics:
- Sources of information: focus groups, document reviews, interviews.
- The inductive process is involved.
- The subjective opinion of the author is allowed.
- The main content is text and reflections.
- Validity depends on the skill of the author.
You can check lists of topics for nursing research ideas in these spheres below!
Qualitative Nursing Research Topics
Qualitative analysis is a complex but critical aspect of medical practice. Nursing qualitative research topics are designed for students to develop skills of analyzing challenging issues and make proper conclusions:
- The role of technology in improving the quality of nursing care .
- Empowering nurses to prescribe: advantages and disadvantages.
- The problem of equality between doctors and nurses .
- Nursing stereotypes.
- Issues of accreditation of medical schools.
- The problem of systemic racism in the healthcare system.
- How nursing has changed in the 20th and 21st centuries.
- The importance of nursing staff in primary care .
- Priority of cancer in adults.
- Advantages and disadvantages of qualitative research in nursing .
These qualitative nursing research topics can help you improve your analytical skills significantly!
Quantitative Nursing Research Topics
Quantitative type of scientific work is all about statistics, percentages, and numbers. Prepare yourself to analyze tons of information with these nursing quantitative research topics:
- Evaluation of the effectiveness of primary patient care.
- The leading causes of heart disease .
- Analysis of the efficacy of telemedicine .
- The problem of an overabundance of information noise in the modern world.
- Evaluation of methods of assistance in suicide attempts.
- Statistical analysis of the benefits of diets .
- Causes of mental illness in women.
- Using unconventional methods to treat diabetes .
- Benefits of probiotics for treating diarrhea .
- Methods for assessing pain in critically ill patients.
For a successful paper, it’s importnt to pick a good research topics for nursing students based on quantitative evidence.
How to choose a Nursing Research Topic?
Choosing a quality nursing research topic idea can be a daunting task. This is mainly because the variety of possible options is simply too large. But don’t worry, here are some simple tips to help you choose the theme that’s right for you!
📜 Remove large-scale topics . You should not waste your energy on massive topics. Instead, choose narrow evidence-based ideas that allow you to focus on one issue. 📜 Use personal experience . One cannot be informed in all aspects of medicine. So when you write about a topic you have no experience with, you risk getting bogged down in hours of tedious research. Try to remember what problems you faced yourself. This way, you will already have a basic knowledge of the topic. 📜 Review literature . A large amount of ready-made research a topic will be an excellent help in writing about it. Try to do a systematic nursing topics review to find more examples. This does not mean that you should copy the work of another medic. On the contrary, it will be a good opportunity for you to highlight additional information. Therefore, before choosing from easy nursing research topics, look at how much information is already in the public domain.
What is the process of nursing research? Oh, that’s a tricky question. Let’s look at the main stages you need to go through!
✨ Define the research problem . To solve a problem, you first need to find it. That is why the first thing you should do is choose a nursing research question. If you have any experience with the topic, that will be a big plus! ✨ Develop hypothesis . Now, you need to think and create your theory. It can be of any form. The main thing is to make a connection between the data pieces and find a pattern. Of course, the hypothesis must be consistent with the current nursing research topics. ✨ Literature review . Before you start writing, it’s important to tighten your knowledge of the central thesis of the topic you’ve selected. Try reading other people’s research, finding the statistics you want, and just surfing the internet. ✨ Prepare an outline . It is essential to formulate a plan for your work before you start working on it. The more detailed you describe each paragraph of your article, the less time you will need to write it. Quality work begins with a quality plan! ✨ Conduct research . Now you start the longest and most important part of the whole nursing project. You should delve deeper into the problem and find the information you need. Everything that you write should help you prove your hypothesis in one way or another. ✨ Make a conclusion and develop further recommendations . After you have processed all the material, it is time to write a conclusion. Here, you must indicate whether you have succeeded in proving the hypothesis and recommend the application for your scientific work.
Congratulations, you did it! Writing a good paper is not that difficult. It all depends on a well-chosen research topic in the nursing field; luckily, you have a list of 350 topics to look through in this article! You can find more nursing research ideas on our website!
❓ What Is Translational Research in Nursing?
Translational research is a kind of scientific work, and its task is to transform theory into new practical approaches. In other words, discoveries made in laboratories become the basis for creating a new actionable framework in nursing.
❓ What Is an Example of a Clinical Question?
The clinical question is an integral part of your scientific work. It can relate to categories such as the cause of the problem, the manifestation of the disease in the patient, possible solutions, and potential results. A well-formulated clinical question helps you write a quality article.
❓ How to Determine Level of Evidence in Nursing Research?
Several criteria determine the level of evidence in nursing research. These include quality of design, validity, and applicability of results to patient care. Therefore, you should constantly monitor the reliability of your sources and the correctness of your conclusions.
❓ What Are Some Controversial Issues in Nursing?
In modern nursing, there are some controversial issues, mainly of an ethical nature. Such problems include the issue of vaccination of people who are against it, artificial nutrition, opioid addiction, and others. There is a lively discussion about how to act correctly in some instances and what factors the decision may depend on.
📎 References:
- Evidence-Based Practice: PICO. Duke University .
- Asking the clinical question. Penn State University
- Evidence-Based Practice Toolkit. Darrell W. Krueger Library
- Top 5 Ethical Issues in Nursing. American Mobile
- Differences Between Qualitative and Quantitative Research Methods.
- Qualitative vs. Quantitative Research – What Is the difference? Imotions
- The Seven Steps of the Research Process. Teacherph
- Research Paper Writing Guide. Grammarly
- Choosing a research topic. Florida Gulf Coast University
- Nursing Process. NCBI
- Sample Research Topics. CFAES
- Selecting a Research Topic: Overview. MIT Libraries
- Three Important Nursing Subjects Students Should Know. Distant learning systems
- Evidence-Based Practice Tutorial: Asking Clinical Questions. University of Maryland
- Top 5 Ethical Issues in Nursing. Avant Healthcare
- Ethical Issues in Nursing: Explanations & Solutions. Duquesne University
- Clinical & Translational Research. UNC
- Writing a Thesis for Nursing School | Nursejournal.org
- A practical approach to the process of writing a dissertation. Nursing Times
- Share to Facebook
- Share to Twitter X
- Share to LinkedIn
You might also like
Memorable human trafficking essay: topics & outline [2024], credible sources 101: how to evaluate them + 60 reliable websites for students, 265 powerful research proposal topics to consider [+ writing tips].

14 Research Topics for Nursing Students
.png?width=50&height=50&name=stencil.amz%20(3).png)
What are you struggling with in nursing school?
NURSING.com is the BEST place to learn nursing. With over 2,000+ clear, concise, and visual lessons, there is something for you!
As a nursing student, you will be expected to conduct research as part of your coursework. Choosing a research topic can be challenging, but it's essential to find a topic that is both interesting and relevant to your field. In this post, we'll explore some good research topics for nursing students and provide links to resources where you can learn more.
The effects of shift work on nurses' health and well-being Shift work is a common practice in nursing, but it can have negative effects on nurses' health and well-being. This research topic could explore the impact of shift work on sleep patterns, stress levels, and overall health.
Improving patient outcomes through evidence-based practice Nurses play a crucial role in delivering evidence-based care. This research topic could explore the use of evidence-based practice to improve patient outcomes in a particular area, such as wound care or medication management.
Examining the role of the nurse in end-of-life care End-of-life care is an important aspect of nursing practice. This research topic could explore the nurse's role in providing end-of-life care, including ethical considerations and communication with patients and families.
Reducing healthcare-associated infections in hospitals Healthcare-associated infections (HAIs) are a significant problem in hospitals. This research topic could explore strategies for reducing HAIs, such as hand hygiene and infection control measures.
Exploring the impact of cultural diversity on healthcare outcomes Cultural diversity is an essential aspect of nursing practice. This research topic could explore the impact of cultural diversity on healthcare outcomes, including patient satisfaction, adherence to treatment, and health disparities.
Investigating the use of technology in nursing practice Technology is increasingly being used in nursing practice. This research topic could explore the use of technology in areas such as telehealth, electronic health records, and medication administration.
Addressing healthcare disparities among underserved populations Healthcare disparities are a significant problem in the United States. This research topic could explore the factors contributing to healthcare disparities among underserved populations and strategies for addressing these disparities.
Improving pain management in hospitalized patients Pain management is an essential aspect of nursing practice. This research topic could explore strategies for improving pain management in hospitalized patients, including the use of non-pharmacological interventions.
Examining the effectiveness of nursing interventions in preventing falls in hospitalized patients Falls are a significant problem in hospitals, particularly among older adults. This research topic could explore the effectiveness of nursing interventions in preventing falls in hospitalized patients.
Investigating the use of complementary and alternative therapies in nursing practice Complementary and alternative therapies are becoming increasingly popular among patients. This research topic could explore the use of these therapies in nursing practice, including their efficacy and safety.
The impact of social determinants of health on healthcare outcomes Social determinants of health, such as income and education level, can have a significant impact on healthcare outcomes. This research topic could explore the relationship between social determinants of health and healthcare outcomes.
Investigating the relationship between nurse staffing and patient outcomes Nurse staffing levels can have a significant impact on patient outcomes. This research topic could explore the relationship between nurse staffing levels and patient outcomes, including mortality rates and length of stay.
Examining the use of simulation in nursing education Simulation is becoming an increasingly popular teaching tool in nursing education. This research topic could explore the use of simulation in nursing education, including its effectiveness and best practices.
Improving nursing leadership and management in healthcare organizations Nursing leadership and management are essential components of healthcare organizations. This research topic could explore strategies for improving nursing leadership and
Setting Yourself Up for Success: What Are SMART Goals for Nursing Students?
I failed the nclex 6 times . . . how i finally passed, similar blog posts.

Why Passing the NCLEX® in 75 Questions Doesn't Matter | NURSING.com

Burn Injuries NCLEX Review for Nursing Students + Free Download
Breaking down Lymphoma for your NCLEX review + Free download
Nursing Education Research Paper Topics

Nursing education research paper topics are crucial for the development of the nursing profession. The field of nursing education is vast and encompasses a wide range of topics, from teaching and learning strategies to curriculum development and technology integration. Research in this area is essential for the continuous improvement of nursing education practices, which ultimately leads to better-prepared nurses and improved patient outcomes. This article will provide a comprehensive list of research paper topics in nursing education, as well as an in-depth article discussing the significance of nursing education and various aspects of it. Additionally, the article will present iResearchNet’s writing services, offering students the opportunity to order a custom nursing education research paper on any topic.
100 Nursing Education Research Paper Topics
The significance of nursing education cannot be overstated. It is a critical component in the preparation of nursing professionals who are competent, compassionate, and prepared to meet the diverse health needs of populations worldwide. Nursing education encompasses a wide range of topics, from theories and concepts to curriculum development, teaching and learning strategies, assessment and measurement, simulation, technology integration, continuing education, leadership and management, legal and ethical issues, and innovations and future trends. Research in these areas is vital for the continuous improvement and evolution of nursing education, ultimately leading to better-prepared nurses and improved patient outcomes. This section provides a comprehensive list of nursing education research paper topics, divided into ten categories.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code.
Theories and Concepts in Nursing Education
- The role of self-efficacy in nursing education.
- Applying adult learning theories in nursing education.
- The impact of constructivism on nursing education.
- The relevance of social learning theory in nursing education.
- The influence of transformative learning in nursing education.
- Critical thinking development in nursing education.
- The role of reflective practice in nursing education.
- The importance of emotional intelligence in nursing education.
- The impact of experiential learning in nursing education.
- The role of cognitive load theory in nursing education curriculum.
Curriculum Development and Evaluation
- The impact of competency-based education on nursing curriculum.
- Strategies for integrating cultural competence in the nursing curriculum.
- The role of evidence-based practice in nursing curriculum development.
- The impact of interprofessional education on nursing curriculum.
- Strategies for integrating mental health into the nursing curriculum.
- The role of simulation in nursing curriculum development.
- Strategies for integrating community health nursing into the curriculum.
- The impact of global health education on nursing curriculum.
- Strategies for developing a culturally inclusive nursing curriculum.
- The role of accreditation standards in nursing curriculum development.
Teaching and Learning Strategies
- The effectiveness of case-based learning in nursing education.
- The impact of problem-based learning on nursing students’ critical thinking skills.
- The role of team-based learning in nursing education.
- The effectiveness of flipped classroom in nursing education.
- The impact of online learning on nursing education.
- Strategies for promoting active learning in nursing education.
- The role of clinical reasoning in nursing education.
- The effectiveness of peer teaching in nursing education.
- The impact of concept mapping on nursing students’ learning outcomes.
- Strategies for promoting self-directed learning in nursing education.
Assessment and Measurement in Nursing Education
- The effectiveness of formative assessment in nursing education.
- The impact of summative assessment on nursing students’ learning outcomes.
- The role of self-assessment in nursing education.
- The effectiveness of peer assessment in nursing education.
- The impact of objective structured clinical examination (OSCE) in nursing education.
- Strategies for promoting authentic assessment in nursing education.
- The role of portfolio assessment in nursing education.
- The effectiveness of simulation-based assessment in nursing education.
- The impact of written examinations on nursing students’ learning outcomes.
- Strategies for promoting continuous assessment in nursing education.
Simulation in Nursing Education
- The effectiveness of high-fidelity simulation in nursing education.
- The impact of simulation on nursing students’ clinical reasoning skills.
- The role of simulation in developing nursing students’ communication skills.
- The effectiveness of simulation in teaching nursing procedures.
- The impact of simulation on nursing students’ self-confidence.
- Strategies for promoting realism in simulation-based nursing education.
- The role of debriefing in simulation-based nursing education.
- The effectiveness of simulation in interprofessional education.
- The impact of simulation on nursing students’ decision-making skills.
- Strategies for integrating simulation into the nursing curriculum.
Technology Integration in Nursing Education
- The effectiveness of virtual reality in nursing education.
- The impact of mobile applications on nursing education.
- The role of e-learning in nursing education.
- The effectiveness of online discussions in nursing education.
- The impact of electronic health records on nursing education.
- Strategies for promoting digital literacy in nursing education.
- The role of social media in nursing education.
- The effectiveness of computer-based simulations in nursing education.
- The impact of telehealth on nursing education.
- Strategies for integrating technology into the nursing curriculum.
Continuing Education and Lifelong Learning
- The effectiveness of continuing education programs for nurses.
- The impact of lifelong learning on nurses’ professional development.
- The role of continuing education in maintaining nursing competency.
- The effectiveness of online continuing education for nurses.
- The impact of continuing education on nurses’ job satisfaction.
- Strategies for promoting a culture of lifelong learning among nurses.
- The role of professional associations in continuing education for nurses.
- The effectiveness of certification programs in nursing.
- The impact of continuing education on nurses’ clinical practice.
- Strategies for integrating continuing education into nurses’ professional development plans.
Leadership and Management in Nursing Education
- The effectiveness of leadership development programs for nursing students.
- The impact of leadership styles on nursing students’ learning outcomes.
- The role of mentorship in developing nursing leaders.
- The effectiveness of management training for nurse educators.
- The impact of leadership and management education on nurses’ job satisfaction.
- Strategies for promoting a culture of leadership among nursing students.
- The role of leadership in promoting a positive learning environment.
- The effectiveness of leadership in promoting interprofessional collaboration.
- The impact of leadership on nursing students’ clinical practice.
- Strategies for integrating leadership and management education into the nursing curriculum.
Legal and Ethical Issues in Nursing Education
- The effectiveness of ethics education in nursing.
- The impact of legal education on nursing students’ clinical practice.
- The role of ethics and legal education in developing nursing students’ decision-making skills.
- The effectiveness of ethics and legal case studies in nursing education.
- The impact of ethics and legal education on nurses’ professional development.
- Strategies for promoting a culture of ethical practice among nursing students.
- The role of professional codes of ethics in nursing education.
- The effectiveness of ethics and legal education in preventing malpractice.
- The impact of ethics and legal education on nurses’ job satisfaction.
- Strategies for integrating ethics and legal education into the nursing curriculum.
Innovations and Future Trends in Nursing Education
- The effectiveness of innovative teaching strategies in nursing education.
- The impact of emerging technologies on nursing education.
- The role of innovation in promoting a positive learning environment.
- The effectiveness of innovative assessment strategies in nursing education.
- The impact of innovation on nursing students’ learning outcomes.
- Strategies for promoting a culture of innovation among nursing students.
- The role of innovation in promoting interprofessional collaboration.
- The effectiveness of innovation in promoting self-directed learning.
- The impact of innovation on nurses’ professional development.
- Strategies for integrating innovation into the nursing curriculum.
Research in nursing education is essential for the continuous improvement and evolution of nursing education practices. The diverse range of nursing education research paper topics listed above provides a solid foundation for exploring various aspects of nursing education, from theories and concepts to curriculum development, teaching and learning strategies, assessment and measurement, simulation, technology integration, continuing education, leadership and management, legal and ethical issues, and innovations and future trends. It is encouraged that students and researchers explore these topics in-depth to contribute to the body of knowledge in nursing education and ultimately lead to better-prepared nurses and improved patient outcomes.
Rhe Range of Nursing Education Research Paper Topics
Nursing education holds immense significance in the healthcare sector. It serves as the foundation for preparing competent and compassionate nursing professionals who play a pivotal role in ensuring the health and well-being of individuals and communities worldwide. Nursing education involves a comprehensive approach that encompasses various aspects such as curriculum development, teaching and learning strategies, technology integration, assessment and measurement, simulation, continuing education, leadership and management, legal and ethical issues, and innovations and future trends. This article aims to discuss the significance of nursing education and examine various aspects of it, highlighting a range of nursing education research paper topics.
Significance of Nursing Education
Nursing education is the cornerstone of preparing nursing professionals who are equipped with the knowledge, skills, and attitudes necessary to provide high-quality care to patients. It involves not only the transmission of knowledge but also the development of critical thinking, decision-making, communication, and clinical skills. Nursing education prepares nurses to work in various healthcare settings, from hospitals and clinics to community health centers and home care. It also instills a commitment to lifelong learning, professional development, and ethical practice. Moreover, nursing education plays a crucial role in addressing the current and future challenges faced by the healthcare system, such as the increasing prevalence of chronic diseases, aging population, healthcare disparities, and the need for interprofessional collaboration.
Curriculum Development
Curriculum development in nursing education involves the design and organization of educational experiences to achieve the desired learning outcomes. It encompasses the identification of competencies, development of learning objectives, selection of content, organization of learning experiences, and evaluation of learning outcomes. Curriculum development is a dynamic process that requires continuous evaluation and revision to ensure its relevance, effectiveness, and alignment with the needs of the students, healthcare system, and society. Some of the nursing education research paper topics related to curriculum development include:
Teaching and learning strategies in nursing education involve the selection and implementation of methods and activities that facilitate the achievement of learning objectives. These strategies can vary from traditional lectures and discussions to more interactive and innovative approaches such as case-based learning, problem-based learning, team-based learning, flipped classroom, online learning, simulation, and peer teaching. The selection of teaching and learning strategies should consider the characteristics of the learners, the nature of the content, and the context in which the learning occurs. Some of the nursing education research paper topics related to teaching and learning strategies include:
Technology Integration
Technology integration in nursing education involves the use of technology to enhance the teaching and learning process. It encompasses a wide range of tools and applications, from computers and mobile devices to virtual reality, simulation, electronic health records, and telehealth. Technology integration can facilitate access to information, promote interactive and self-directed learning, enhance clinical reasoning and decision-making skills, and prepare nursing students for the technology-rich healthcare environment. However, it also poses challenges related to digital literacy, privacy and security, and equitable access to technology. Some of the nursing education research paper topics related to technology integration include:
In conclusion, nursing education is of paramount importance in preparing competent and compassionate nursing professionals who can address the current and future challenges faced by the healthcare system. It involves various aspects such as curriculum development, teaching and learning strategies, and technology integration, each of which offers a range of nursing education research paper topics for exploration. Conducting research in these areas can contribute to the continuous improvement and evolution of nursing education practices, ultimately leading to better-prepared nurses and improved patient outcomes.
iResearchNet’s Custom Writing Services
In the world of academia, writing research papers is a fundamental and unavoidable task. This is particularly true for nursing students, who must not only master the complex body of knowledge associated with their field but also actively contribute to it through original research. Unfortunately, many students find themselves overwhelmed by the demands of their nursing programs, and struggle to find the time, resources, or expertise needed to complete their research papers to a high standard. That’s where iResearchNet comes in. Our company is dedicated to providing customized writing services to students in need, and we specialize in helping nursing students tackle the vast array of nursing education research paper topics.
- Expert Degree-Holding Writers : Our team is comprised of professional writers, all of whom hold advanced degrees in their fields. This ensures that they have the knowledge and expertise necessary to provide high-quality content on a wide range of nursing education research paper topics.
- Custom Written Works : Each paper we produce is crafted from scratch, according to the specific requirements and guidelines provided by the client. This ensures that the final product is not only of high quality but also entirely original and tailored to the client’s needs.
- In-Depth Research : Our writers are trained to conduct thorough and meticulous research using reliable and up-to-date sources. This ensures that the papers we produce are well-informed and grounded in the latest scientific knowledge and research.
- Custom Formatting : We understand that different institutions and professors have different requirements when it comes to formatting. That’s why we offer custom formatting services to ensure that your paper adheres to the specific formatting guidelines of your institution, whether it be APA, MLA, Chicago/Turabian, or Harvard style.
- Top Quality : We take pride in the quality of the work we produce. Our writers are not only knowledgeable and experienced but also dedicated to producing the highest quality work possible. This means well-researched, well-written, and well-formatted papers that meet or exceed the client’s expectations.
- Customized Solutions : We understand that each client and each research paper is unique. That’s why we offer customized solutions to meet the individual needs of each client. Whether you need help with selecting a topic, conducting research, writing, editing, or formatting, we can provide the support you need.
- Flexible Pricing : We offer flexible pricing options to accommodate the budgetary constraints of our clients. Our pricing is based on the complexity of the project, the level of expertise required, and the deadline for completion.
- Short Deadlines : We understand that sometimes deadlines can creep up on you, and you may find yourself in need of urgent help. That’s why we offer the option to complete orders with a deadline as short as three hours.
- Timely Delivery : We understand the importance of meeting deadlines, and we make it a priority to deliver all orders on time. This ensures that you have ample time to review the work and request any necessary revisions.
- 24/7 Support : Our customer support team is available 24/7 to address any questions, concerns, or issues you may have. Whether you need help with placing an order, have a question about our services, or need assistance with an ongoing project, we are here to help.
- Absolute Privacy : We take your privacy very seriously. All personal and payment information provided by our clients is kept strictly confidential and is never shared with third parties.
- Easy Order Tracking : Our user-friendly online platform allows you to easily track the progress of your order, communicate with your writer, and access all the necessary documents and files.
- Money-Back Guarantee : We are confident in the quality of the work we produce, but we also understand the importance of providing a safety net for our clients. That’s why we offer a money-back guarantee. If you are not satisfied with the final product, and we are unable to rectify the situation, we will provide a full refund.
In conclusion, iResearchNet is your one-stop-shop for all your research paper needs. With our team of expert degree-holding writers, custom written works, in-depth research, and a host of other features, we are equipped to provide top-quality customized solutions for a wide range of nursing education research paper topics. Whether you are struggling to find a topic, conduct research, write, edit, or format your paper, we can provide the support you need. Our flexible pricing, timely delivery, 24/7 support, absolute privacy, easy order tracking, and money-back guarantee ensure that you can place your order with confidence. Don’t hesitate to reach out to us for help with your nursing education research paper. We are here to support you every step of the way.
Unlock Success with iResearchNet
Are you struggling with your nursing education research paper? Overwhelmed by the vast array of topics, the intricacies of research, or the rigors of formatting? Don’t let the stress get to you! iResearchNet is here to help. Our comprehensive writing services are designed to provide support at every stage of the research paper writing process. From selecting a topic to conducting research, from writing to editing, from formatting to final review, our team of expert degree-holding writers is equipped to provide customized solutions to meet your specific needs. With our flexible pricing, timely delivery, 24/7 support, and money-back guarantee, you can place your order with confidence. Don’t miss out on the opportunity to submit a high-quality research paper that will impress your professors and set you on the path to success.
Success is not just about talent or luck; it is about making smart choices and taking control of your destiny. One smart choice you can make is to seek help when you need it. If you are struggling with your nursing education research paper, don’t hesitate to reach out for help. iResearchNet is here to provide the support you need to overcome the challenges you face and achieve your goals. Our comprehensive writing services are designed to provide customized solutions for a wide range of nursing education research paper topics. Whether you need help with selecting a topic, conducting research, writing, editing, or formatting, we have the expertise and resources to help you succeed. Take control of your success by ordering a custom nursing education research paper from iResearchNet today!
ORDER HIGH QUALITY CUSTOM PAPER


The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity (2021)
Chapter: 11 the future of nursing: recommendations and research priorities, 11 the future of nursing: recommendations and research priorities.
The next 10 years will test the nation’s nearly 4 million nurses in new and complex ways. Nurses live and work at the intersection of health, education, and communities. In the decade since the prior The Future of Nursing report was published ( IOM, 2011 ), the world has come to understand the critical importance of health to all aspects of life, particularly the relationship among social determinants of health (SDOH), health equity, and health outcomes. Consistent with this broader understanding, the National Advisory Council on Nurse Education and Practice (NACNEP) (2020) advanced an important set of recommendations that the committee endorses. The NACNEP report Integration of Social Determinants of Health in Nursing Education, Practice, and Research conveys the importance of investing in SDOH and research to strengthen the nursing workforce and help nurses provide more effective care, as well as design, implement, and assess new care models.
In a year that was designated to honor and uplift nursing (the International Year of the Nurse and the Midwife 2020 1 ), nurses have been placed in unimaginable circumstances by the COVID-19 pandemic. The decade ahead will demand a stronger, more diversified workforce that is prepared to provide care; promote health and well-being among nurses, individuals, and communities; and address the systemic inequities that have fueled wide and persistent health disparities.
The COVID-19 pandemic has revealed in the starkest terms that illness and access to quality health care are unequally distributed across groups and commu-
___________________
1 See https://www.who.int/campaigns/annual-theme/year-of-the-nurse-and-the-midwife-2020 (accessed April 12, 2021).
nities, and has spotlighted the reality that much of what affects health happens outside of medical care. The pandemic and continued calls for racial justice have illuminated the extent to which structural racism—from decades of neglect and disinvestment in neighborhoods, schools, communities, and health care to discrimination and bias—has placed communities of color at much higher risk for poor health and well-being.
The committee’s recommendations call for change at both the individual and system levels, constituting a call for action to the nation’s largest health care workforce, including nurses in all settings and at all levels, to listen, engage, deeply examine practices, collect evidence, and act to move the country toward greater health equity for all. The committee’s recommendations also are targeted to the actions required of policy makers, educators, health care system leaders, and payers to enable these crucial changes, supported by the research agenda with which this chapter concludes. With implementation of this report’s recommendations, the committee envisions 10 outcomes that position the nursing profession to contribute meaningfully to achieving health equity (see Box 11-1 ).
In this chapter, the committee provides its recommendations for charting a 10-year path forward to enable and support today’s and the next generation of nurses to create fair and just opportunities for health and well-being for
everyone. These recommendations are aimed at all nurses, including those working in hospitals, schools, and health departments; policy makers; educators; health care system leaders; and payers. The chapter concludes with a research agenda to fill current and critical gaps that would support this future-oriented path.
CREATING A SHARED AGENDA
In order for nurses to engage fully in efforts to achieve health equity, it will be necessary for nursing organizations to work together to identify priorities for education, practice, and policy, and to develop mechanisms for leveraging existing nursing expertise and resources. Creating a shared agenda will focus efforts and ensure that all nurses—no matter where they are educated or where they practice—are prepared, supported, and empowered to address SDOH and eliminate inequities in health and health care.
Recommendation 1: In 2021, all national nursing organizations should initiate work to develop a shared agenda for addressing social determinants of health and achieving health equity. This agenda should include explicit priorities across nursing practice, education, leadership, and health policy
engagement. The Tri-Council for Nursing 2 and the Council of Public Health Nursing Organizations, 3 with their associated member organizations, should work collaboratively and leverage their respective expertise in leading this agenda-setting process. Relevant expertise should be identified and shared across national nursing organizations, including the Federal Nursing Service Council 4 and the National Coalition of Ethnic Minority Nurse Associations. With support from the government, payers, health and health care organizations, and foundations, the implementation of this agenda should include associated timelines and metrics for measuring impact.
Specific actions should include the following:
- Assess diversity, equity, and inclusion, and eliminate policies, regulations, and systems that perpetuate structural racism, cultural racism, and discrimination with respect to identity (e.g., sexual orientation, gender), place (e.g., rural, inner city), and circumstances (e.g., disabilities, depression).
- Develop mechanisms for leveraging the expertise of public health nursing (e.g., in population health, SDOH, community-level assessment) as a resource for the broader nursing community, health plans, and health systems, as well as public policy makers.
- Develop mechanisms for leveraging the expertise of relevant nursing organizations in care coordination and care management. Care coordination and care management principles, approaches, and evidence should be used to create new cross-sector models for meeting social needs and addressing SDOH.
- Develop mechanisms for prioritizing and sharing continuing education and skill-training resources focused on nurses’ health, well-being, resilience, and self-care to ensure a healthy nursing workforce.
2 The Tri-Council for Nursing includes the following organizations as members: the American Association of Colleges of Nursing, the American Nurses Association, the American Organization for Nursing Leadership, the National Council of State Boards of Nursing, and the National League for Nursing.
3 The Council of Public Health Nursing Organizations includes the following organizations as members: the Alliance of Nurses for Healthy Environments, the American Nurses Association, the American Public Health Association—Public Health Nursing Section, the Association of Community Health Nursing Educators, the Association of Public Health Nurses, and the Rural Nurse Organization.
4 The Federal Nursing Service Council is a united federal nursing leadership team representing the U.S. Army, Air Force, Navy, National Guard and Reserves, Public Health Service Commissioned Corps, American Red Cross, U.S. Department of Veteran Affairs, and the Uniformed Services University of the Health Sciences Graduate School of Nursing.
- These resources should be used by nurses and others in leadership positions.
- Develop and use communication strategies, including social media, to amplify for the public, policy makers, and the media nursing research and expertise on health equity–related issues.
- Increase the number and diversity of nurses, especially those with expertise in health equity, population health, and SDOH, on boards and in other leadership positions within and outside of health care (e.g., community boards, housing authorities, school boards, technology-related positions).
- Establish a joint annual award or series of awards recognizing the measurable and scalable contributions of nurses and their partners to achieving health equity through policy, education, research, and practice. Priority should be given to interprofessional and multisector collaboration.
SUPPORTING NURSES TO ADVANCE HEALTH EQUITY
Promoting health and well-being for all should be a national priority, and a collective and sustained commitment is needed to achieve this priority. To chart this path, nurses should be fully supported with robust education, resources, and autonomy. Key stakeholders should commit to investing fully in strengthening and diversifying the nursing workforce so that it is sufficiently prepared to promote health and appropriately reflects the people and communities it serves. Nursing schools, health care institutions, and public health and community health organizations can do significantly more to empower nurses to raise their voices and use their considerable expertise to improve people’s lives, health, and well-being.
Recommendation 2: By 2023, state and federal government agencies, health care and public health organizations, payers, and foundations should initiate substantive actions to enable the nursing workforce to address social determinants of health and health equity more comprehensively, regardless of practice setting.
This can be accomplished through the following actions:
- Rapidly increase both the number of nurses with expertise in health equity and the number of nurses in specialties with significant shortages, including public and community health, behavioral health, primary care, long-term care, geriatrics, school health, and maternal health. The Health Resources and Services Administration (HRSA), the Substance
- Abuse and Mental Health Services Administration, the Centers for Disease Control and Prevention (CDC), and state governments should support this effort through workforce planning and funding.
- Provide major investments for nursing education and traineeships in public health, including through state-level workforce programs; foundations; and the U.S. Department of Health and Human Services’ (HHS’s) HRSA (including nursing workforce programs and Maternal and Child Health Bureau programs), CDC (including the National Center for Environmental Health), and the Office of Minority Health.
- State governments, foundations, employers, and HRSA should direct funds to nurses and nursing schools to sustain and increase the gender, geographic, and racial diversity of the licensed practical nurse (LPN), registered nurse (RN), and advanced practice registered nurse (APRN) workforce.
- HRSA and the Indian Health Service (IHS) should make substantial investments in nurse loan and scholarship programs to address nurse shortages, including in public health, in health professional shortage areas for HRSA, and in IHS designated sites; and invest in technical assistance that focuses on nurse retention.
- In all relevant Title 8 programs, HRSA should prioritize longitudinal community-based learning opportunities that address social needs, population health, SDOH, and health equity. These experiences should be established through academic–community-based partnerships.
- Foundations, state government workforce programs, and the federal government should support the academic progression of socioeconomically disadvantaged students by encouraging partnerships among baccalaureate and higher-degree nursing programs and community colleges; tribal colleges; historically Black colleges and universities; Hispanic-serving colleges and universities; and nursing programs that serve a high percentage of Asian, Native Hawaiian, and Pacific Islander students.
- Report on and propose actions to fill critical gaps in the current nursing workforce and prepare the future workforce to address health equity.
- Use findings, including those from workforce centers, on the ° diversity, capacity, supply, and distribution of nurses; associated competencies; and organizational support for the nursing workforce in addressing social needs, SDOH, and health equity. Recommend actions to ensure nurses’ continued engagement in these areas.
- Further develop recommendations for nursing education and prac- ° tice with respect to addressing social needs, SDOH, and health equity, and assess the implications of these changes for nurse credentialing and regulatory actions.
- Identify and address gaps in evidence-based nursing and interpro- ° fessional and multisectoral approaches for addressing social needs, SDOH, and health equity.
- Provide information to the secretary of HHS regarding activities of ° federal agencies that relate to the nursing workforce and its impact on health equity.
- Public health and health care systems should quantify nursing expenditures related to health equity and SDOH. This includes providing support for nurses in activities that explicitly target social needs, SDOH, and health equity through health care organization policies, governance and related advisory structures, and collective bargaining agreements.
- Representatives of social sectors, consumer organizations, and government entities should include nursing expertise when health-related multisector policy reform is being advanced.
- State and federal governments should provide sustainable funding to prepare sufficient numbers of baccalaureate, APRN, and PhD-level nurses to address SDOH, advance health equity, and increase access to primary care.
- Employers should support nurses at all levels in all settings with the financial, technical, educational, and staffing resources to help them play a leading role in achieving health equity.
PROMOTING NURSES’ HEALTH AND WELL-BEING
During the course of their work, nurses encounter physical, mental, emotional, and ethical challenges, and burnout is an increasingly prevalent problem. The COVID-19 pandemic has only exacerbated these issues. In order for nurses to help others be healthy and well, they must be healthy and well themselves; a lack of nurse well-being has consequences for nurses, patients, employers, and communities. As nurses are asked to take a more prominent role in advancing health equity, it will become even more imperative that all stakeholders—including educators, employers, leaders, and nurses themselves—take steps to ensure nurse well-being.
Recommendation 3: By 2021, nursing education programs, employers, nursing leaders, licensing boards, and nursing organizations should initiate the implementation of structures, systems, and evidence-based interventions to promote nurses’ health and well-being, especially as they take on new roles to advance health equity.
This can be accomplished by taking the following steps:
- Integrate content on nurses’ health and well-being into their programs to raise nursing students’ awareness of the importance of these concerns and provide them with associated skill training and support that can be used as they transition to practice.
- Create mechanisms, including organizational policy and regulations, to protect students most at risk for behavioral health challenges, including those students who may be experiencing economic hardships or feel that they are unsafe; isolated; or targets of bias, discrimination, and injustice.
- Provide sufficient human and material resources (including personal protective equipment) to enable nurses to provide high-quality person-, family-, and community-centered care effectively and safely. This effort should include redesigning processes and increasing staff capacity to improve workflow, promote transdisciplinary collaboration, reduce modifiable burden, and distribute responsibilities to reflect nurses’ expertise and scope of practice.
- Establish a culture of physical and psychological safety and ethical practice in the workplace, including dismantling structural racism; addressing bullying and incivility; using evidence-informed approaches; investing in organizational infrastructure, such as resilience engineering; 5 and creating accountability for nurses’ health and well-being outcomes.
- Create mechanisms, including organizational policy and regulations, to protect nurses from retaliation when advocating on behalf of themselves and their patients and when reporting unsafe working conditions, biases, discrimination, and injustice.
- Support diversity, equity, and inclusion across the nursing workforce, and identify and eliminate policies and systems that perpetuate structural racism, cultural racism, and discrimination in the nursing profession, recognizing that nurses are accountable for
5 Resilience engineering is focused on “understanding the nature of adaptations, learning from success and increasing adaptive capacity” ( Anderson et al., 2016 , p. 1).
- building an antiracist culture, and employers are responsible for establishing an antiracist, inclusive work environment.
- Prioritize and invest in evidence-based mental, physical, behavioral, social, and moral health interventions, including reward programs meaningful to nurses in diverse roles and specialties, to promote nurses’ health, well-being, and resilience within work teams and organizations.
- Establish and standardize institutional processes that strengthen nurses’ contributions to improving the design and delivery of care and decision making, including the setting of institutional policies and benchmarks in health care organizations and in educational, public health, and other settings.
- Evaluate and strengthen policies, programs, and structures within employing organizations and licensing boards to reduce stigma associated with mental and behavioral health treatment for nurses.
- Collect systematic data at the employer, state (including state workforce centers and state nursing associations), and national levels to better understand the health and well-being of the nursing workforce. This enhanced understanding should be used to inform the development of evidence-based interventions for mitigating burnout; fatigue; turnover; and the development of physical, behavioral, and mental health problems.
CAPITALIZING ON NURSES’ POTENTIAL
Nurses often have untapped potential to help people live their healthiest lives because their education and experience are grounded in caring for the whole person and whole family in a community context. However, this potential is too often underutilized. Nurses, particularly RNs, need environments that facilitate their ability to fully leverage their skills and expertise across all practice settings—in hospitals, primary care settings, rural and underserved areas, homes, community organizations, long-term care facilities, and schools. To engage fully in advancing health equity, all nurses need the autonomy to practice to the full extent of their education and training, even as they work collaboratively with other health professionals. They are, however, frequently hindered in this regard by restrictive laws and institutional policies. Policy makers and health care systems need to lift permanently all barriers that stand in the way of nurses in their efforts to address the root causes of poor health, expand access to care, and create more equitable communities.
Recommendation 4: All organizations, including state and federal entities and employing organizations, should enable nurses to practice to the full extent of their education and training by removing barriers that prevent them from more fully addressing social needs and social determinants of
health and improving health care access, quality, and value. These barriers include regulatory and public and private payment limitations; restrictive policies and practices; and other legal, professional, and commercial 6 impediments.
To this end, the following specific actions should be prioritized:
- By 2022, all changes to institutional policies and state and federal laws adopted in response to the COVID-19 pandemic that expand scope of practice, telehealth eligibility, insurance coverage, and payment parity for services provided by APRNs and RNs should be made permanent.
- Federal authority (e.g., Veterans Health Administration regulations, Centers for Medicare & Medicaid Services [CMS]) should be used where available to supersede restrictive state laws, including those addressing scope of practice, telehealth, and insurance coverage and payment, that decrease access to care and burden nursing practice, and to encourage nationwide adoption of the Nurse Licensure Compact. 7
- The Health Care Regulator Collaborative should work to advance interstate compacts and the adoption of model legislation to improve access, standardize care quality, and build interprofessional collaboration and interstate cooperation.
PAYING FOR NURSING CARE
Nurses are bridge builders, engaging and connecting with individuals, communities, public health and health care, and social services organizations to improve health for all. Without strong financial and institutional support, however, their reach and impact are limited. How care is paid for can determine one’s access to and the quality of care. Thus, it is important to improve and strengthen the design of public and private payment models so nurses are supported, encouraged, and incentivized to bridge health and social needs for people, families, and communities. Nurses also can play a key role in helping to design those models. Also important is for local, state, and federal governments to place more value
6 The term “commercial” refers to contractual agreements and customary practices that make antiquated or unjustifiable assumptions about nursing.
7 Under the Nurse Licensure Compact (NLC), “nurses can practice in other NLC states without having to obtain additional licenses. The current NLC allows for RNs and LPNs/licensed vocational nurses (LVNs) to have one multistate license in any one of the 35 member states” (see https://www.ncsbn.org/nlcmemberstates.pdf ). According to the National Council of State Boards of Nursing (NCSBN), “An APRN must hold an individual state license in each state of APRN practice” (see https://www.ncsbn.org/2018_eNLC_FAQs.pdf ). There is a movement, organized by the National Council of State Boards of Nursing, to have an APRN Compact (see https://aprncompact.com/about.htm ) (all accessed April 12, 2021).
on the vital role of school and public health nurses in advancing health equity by adequately funding and deploying these nurses where they are needed to promote health in communities.
Recommendation 5: Federal, tribal, state, local, and private payers and public health agencies should establish sustainable and flexible payment mechanisms to support nurses in both health care and public health, including school nurses, in addressing social needs, social determinants of health, and health equity.
Specific payment reforms should include the following:
- ensuring that the Current Procedure Terminology (CPT) code set includes appropriate codes to describe and reimburse for such nurse-led services as case management, care coordination, and team-based care to address behavioral health, addiction, SDOH, and health equity, and that the relative value units attached to the CPT codes result in adequate and direct reimbursement for this work;
- reimbursing for school nursing; and
- enabling nurses to bill for telehealth services.
- using clinical performance measures stratified by such risk factors as race, ethnicity, and socioeconomic status;
- supporting nursing interventions through clinical performance measures that incentivize reductions in health disparities between more and less advantaged populations, improvements in measures for at-risk populations, and attainment of absolute target levels of high-quality performance for at-risk populations; and
- incorporating disparities-sensitive measures that support and incentivize nursing interventions that advance health equity (e.g., process measures such as care management and team-based care for chronic conditions; outcomes such as prevention of hospitalizations for ambulatory care–sensitive conditions).
- providing flexible funding (capitated payments, global budgets, shared savings, per member per month payments, accountable health communities models) for nursing and infrastructure that address SDOH; and
- incorporating value-based payment metrics that enable nurses to address SDOH and advance health equity.
- Create a National Nurse Identifier to facilitate recognition and measurement of the value of services provided by RNs.
- implementing state policies that allow school nurses to bill Medicaid and supporting schools, particularly rural schools, in meeting documentation requirements;
- reimbursing school nursing services that include collaboration with clinical and community health care providers;
- promoting new ways of financing public health to address SDOH in the community (e.g., having federal, state, and local leaders, along with public health departments and organizations, partner with payers, health systems, and accountable health communities, and blend or braid multiple funding sources);
- creating funding mechanisms and joint accountability metrics for the efforts of the health, public health, and social sectors to address SDOH and advance health equity that align incentives and behavior across the various stakeholders, including school health;
- leveraging nonprofit hospital community benefit requirements to create partnerships with and among school and public health nursing, primary care organizations, and other social sectors; and
- using pay scales for public health nurses that are competitive with those for nursing positions in other health care organizations and sectors, and that provide equal pay when the services provided (e.g., immunizations) are the same.
USING TECHNOLOGY TO INTEGRATE DATA ON SOCIAL DETERMINANTS OF HEALTH INTO NURSING PRACTICE
The advent and adoption of new technologies have dramatically changed nursing practice over the past several decades, and will continue to do so into the future. Given the rapid acceleration of technical advances, nurses practicing in the coming decade will need to be adept at and comfortable with using emerging technology and have the skills to support others in doing the same. Nurses are well positioned to design, adopt, and adapt new technologies in practice and leverage data on SDOH to identify and address the needs of populations, individualize care, and reduce health disparities. With care expanding beyond the walls of traditional health care settings, including hospitals and clinics, the deployment of such advanced technologies as artificial intelligence and telehealth can assist nurses in connecting to health care networks, reaching individuals in their homes and other settings, and promoting health and well-being within communities. As key stakeholders in the design, adoption, and evaluation of new care tools, nurses also need to understand how to use new technologies to reduce rather than exacerbate inequities.
Recommendation 6: All public and private health care systems should incorporate nursing expertise in designing, generating, analyzing, and applying
data to support initiatives focused on social determinants of health and health equity using diverse digital platforms, artificial intelligence, and other innovative technologies.
- With leadership from CMS and The Office of the National Coordinator for Health Information Technology, accelerate interoperability projects that integrate data on SDOH from public health, social services organizations, and other community partners into electronic health records, and build a nationwide infrastructure to capture and share community-held knowledge, facilitate referrals for care (including by decreasing the “digital divide”), and facilitate coordination and connectivity among health care settings and the public and nonprofit sectors.
- Ensure that existing public/private health equity data collaboratives (e.g., the Gravity Project 8 ) encompass nursing-specific care processes that improve visualization of data on SDOH and associated decision making by nurses.
- Employ nurses with requisite expertise in informatics to improve individual and population health through large-scale integration of data on SDOH into nursing practice, as well as expertise in the use of telehealth and advanced digital technologies.
- To personalize care based on person- and family-centered preferences and individual needs, give nurses in clinical settings responsibility and associated resources to innovate and use technology, including in the use of data on SDOH as context for planning and evaluating care; in the design of personal and mobile health tools; in coordination of community and public health portals across care settings; in methods for effective communication using technology; in evaluation of datasets and artificial intelligence algorithms (e.g., for racial bias); and in partnerships with corporate settings outside of health care delivery (e.g., large technology organizations, private insurers) that are addressing health equity in the nonclinical setting.
- expanding the national strategy for a broadband/5G infrastructure to enable comprehensive community access to these services; and
- increasing the availability of the necessary hardware, including smartphones, computers, and webcams, for high-risk populations.
8 See https://sirenetwork.ucsf.edu/TheGravityProject (accessed April 12, 2021).
STRENGTHENING NURSING EDUCATION
Regardless of the setting in which they work or their level of education, nurses of the future will be expected to have a sophisticated understanding of social needs, SDOH, and health equity and to be capable of applying this knowledge in their practice. The World Health Organization has emphasized the importance of monitoring equitable service coverage across wealth and education gradients as part of achieving universal health coverage. Similarly, leading public health researchers have advocated for using markers of health equity to monitor health and health care as a first step in confronting inequities. Recognizing and meeting social needs could both lower health care spending and improve health outcomes.
Nursing schools need to prepare nurses to understand and identify the social, economic, and environmental factors that influence health by embedding content on SDOH throughout their curricula. Schools need to ensure that nurses have substantive, enduring, relevant community-based experiences and that they value diverse perspectives and cultures in order to help all people and families thrive. Nurses should have this content updated and reinforced throughout their careers through continuing education.
Recommendation 7: Nursing education programs, including continuing education, and accreditors and the National Council of State Boards of Nursing should ensure that nurses are prepared to address social determinants of health and achieve health equity.
To implement this recommendation, deans, administrative faculty leaders, faculty, course directors, and staff of nursing education programs should take the following steps:
- Integrate social needs, SDOH, population health, environmental health, trauma-informed care, and health equity as core concepts and competencies throughout coursework and clinical and experiential learning. These core concepts and competencies should be commensurate and seamless with academic level and included in continuing education.
- By the 2022–2023 school year, initiate an assessment of individual student access to technology, and ensure that all students can engage in virtual learning, including such opportunities as multisector simulation. Access to nursing education for geographically and socioeconomically disadvantaged students should be ensured through the development and expansion of the use of remote and virtual instructional capabilities. For rural areas, emphasis should be on baccalaureate preparation given the lower proportion of nurses educated at this level.
- To promote equity, inclusivity, and diversity grounded in social justice, identify and eliminate policies, procedures, curricular content, and clin
- ical experiences that perpetuate structural racism, cultural racism, and discrimination among faculty, staff, and students.
- Increase academic progression for geographically and socioeconomically disadvantaged students through academic partnerships that include community and tribal colleges located in rural and urban underserved areas.
- Recruit diverse faculty with expertise in SDOH, population health (including environmental health), and health equity and associated policy expertise, and, through evidence-based and other training, develop the skills of current faculty with the objective of ensuring that students have access across the curriculum to expertise in these areas. Faculty should also have the technical competencies for online teaching.
- Ensure that students have learning opportunities with care coordination experiences that include working with health care teams to address individual and family social needs, as well as learning opportunities with multisector stakeholders that include a focus on health in all policies and SDOH. Learning experiences should include working with underserved populations in such settings as federally qualified health centers, rural health clinics, and IHS designated sites.
- Incorporate in all nurse doctoral education content related to SDOH, population health, environmental health, trauma-informed care, health equity, and social justice. All graduates of doctoral programs should have competencies in the use of data on SDOH as context for planning, implementing, and evaluating care and for improving population health through the large-scale application of these data.
- Ensure that PhD nursing graduates are competent to design and implement research that addresses issues of social justice and equity in education and/or health and health care and informs relevant policies. Increase the capacity of these graduates to apply research and scale interventions to address and improve social needs, SDOH, population health, environmental health, trauma-informed care, health equity, the well-being of nurses, and disaster preparedness and to inform relevant policies.
- Prepare all nursing students to advocate for health equity through civic engagement, including engagement in health and health-related public policy and communication through traditional and nontraditional methods, including social media and multisector coalitions.
Accreditors should take the following actions:
- Incorporate standards and competencies for curriculum that reflect the application of knowledge and skills to improve social needs, SDOH, population health, environmental health, trauma-informed care, and health equity.
- Incorporate standards for increasing student and faculty diversity.
- Require nursing education programs to initiate curricular assessments in 2022–2023 and phase in curricular changes that integrate social needs, SDOH, population health, environmental health, trauma-informed care, and health equity throughout the curriculum and are assessed in subsequent midterm and accreditation reporting. These curricular changes and their impact should be subject to continuous accreditation review processes.
- Include standards for nurses’ well-being and ethical practice in accreditation guidelines, and include such content on nurse licensing and certification exams.
The National Council of State Boards of Nursing and specialty certification organizations should take the following action:
- Incorporate test questions on meeting social needs through care coordination and on meeting population health needs, including addressing SDOH, through multisector coordination.
Continuing education providers should take the following action:
- Evaluate each offering for the inclusion of social needs, SDOH, population health, environmental health, trauma-informed care, and health equity and strategies for associated public- and private-sector policy engagement.
PREPARING NURSES TO RESPOND TO DISASTERS AND PUBLIC HEALTH EMERGENCIES
The COVID-19 pandemic has magnified the vital role of nurses on the front lines of crises—whether in the hospital intensive care unit, a community testing site, or an emergency shelter—in keeping communities safe and healthy and helping people and families cope. They are reliable, trusted, experienced, and proven responders during both public health emergencies and natural disasters, such as hurricanes and wildfires. But fundamental reforms and a stronger disaster preparedness infrastructure are needed to improve nursing education, practice, and policy so nurses are fully protected during such events and can better protect and care for recovering populations.
Recommendation 8: To enable nurses to address inequities within communities, federal agencies and other key stakeholders within and outside the nursing profession should strengthen and protect the nursing workforce during the response to such public health emergencies as the COVID-19 pandemic and natural disasters, including those related to climate change.
To this end, the following steps should be taken:
- CDC should fund a National Center for Disaster Nursing and Public Health Emergency Response, along with additional strategically placed regional centers, to serve as the “hub” for providing leadership in education, training, and career development that will ensure a national nursing workforce prepared to respond to such events.
- CDC, in collaboration with the proposed National Center for Disaster Nursing and Public Health Emergency Response, should rapidly articulate a national action plan for addressing gaps in nursing education, support, and protection that have contributed to the lack of nurse preparedness and disparities during such events.
- The Office of the Assistant Secretary for Preparedness and Response, CDC, HRSA, the Agency for Healthcare Research and Quality, CMS, the National Institute of Nursing Research (NINR), and other funders should develop and support the emergency preparedness and response knowledge base of the nursing workforce through regulations, programs, research, and sustainable funding targeted specifically to disaster and public health emergency nursing.
- The American Association of Colleges of Nursing, the National League for Nursing, and the Organization for Associate Degree Nursing should lead transformational change in nursing education to address workforce development in disaster nursing and public health preparedness. NCSBN should expand content in licensing examinations to cover actual responsibilities of nurses in disaster and public health emergency response.
- Employers should incorporate the expertise of nurses to proactively develop and implement an emergency response plan for natural disasters and public health emergencies in coordination with local, state, national, and federal partners. They should also provide additional services throughout a disaster or public health emergency, such as support for families and behavioral health, to support and protect nurses’ health and well-being.
BUILDING THE EVIDENCE BASE
Strengthening and diversifying the nursing workforce of the future, fostering nurse well-being, and developing strong and impactful nurse leaders so that nurses can fully address the wide and persistent health disparities in the United States will require a robust and rigorous evidence base. Below, the committee prioritizes the research needs and identifies gaps in the knowledge base that, if filled, would substantially move the nursing profession forward in the future.
Recommendation 9: The National Institutes of Health, the Centers for Medicare & Medicaid Services, the Centers for Disease Control and Prevention, the Health Resources and Services Administration, the Agency for Healthcare Research and Quality, the Administration for Children and Families, the Administration for Community Living, and private associations and foundations should convene representatives from nursing, public health, and health care to develop and support a research agenda and evidence base describing the impact of nursing interventions, including multisector collaboration, on social determinants of health, environmental health, health equity, and nurses’ health and well-being.
These efforts should be focused on the following actions:
- Develop mechanisms for proposing, evaluating, and scaling evidence-based practice models that leverage collaboration among public health, social sectors, and health systems to advance health equity, including codesigning innovations with individuals and community representatives and responding to community health needs assessments. This effort should emphasize rapidly translating evidence-based interventions into real-world clinical practice and community-based settings to improve health equity and population health outcomes, and applying implementation science strategies in the process of scaling these interventions and strategies.
- Identify effective multisector team approaches to improving health equity and addressing social needs and SDOH, including clearly defining roles and assessing the value of nurses in these models. Specifically, performance and outcome measures should be delineated, and evaluation strategies for community-based models and multisector team functioning should be developed and implemented.
- Review and adapt evidence-based approaches to increasing the number and diversity of students and faculty from disadvantaged and traditionally underrepresented groups to promote a diverse, inclusive learning environment and prepare a culturally competent workforce.
- Determine evidence-based education strategies for preparing nurses at all levels, including through continuing education, to eliminate structural racism and implicit bias and strengthen the delivery of culturally competent care.
- Augment the use of advanced information technology infrastructure, including virtual services and artificial intelligence, to identify and integrate health and social data, including data on SDOH, so as to improve
- nurses’ capacity to support individuals, families, and communities, including through care coordination.
Across all of these efforts, nurses should partner with key community stakeholders in research design; identification of the characteristics of new health models; and the development of related institutional and public policies at the health system, public health, and community levels. To expand the cohort of nurse researchers engaged in this research agenda, NINR should offer continuous summer intensive seminars to build expertise in population health, SDOH, and health equity. Table 11-1 summarizes gaps in the current research base that have been identified throughout this report.
TABLE 11-1 Research Topics for the Future of Nursing, 2020–2030
FINAL THOUGHTS
The nursing profession is vital to the nation’s creation of a culture of health, reduction of health disparities, and improvement in the health and well-being of the population. The committee’s nine recommendations provide a comprehensive path forward for policy makers, practicing nurses, educators, health care system leaders, researchers, and payers to enable and support the nurses of today and the future in creating fair and just opportunities for health and well-being for everyone. The social, political, and health care trends discussed in this report, while replete with myriad challenges, also offer nurses new opportunities for practice and collaboration. Nurses will need to continue to adapt and respond to new and developing health problems at both the individual and community levels, and to deepen their understanding of how social, economic, and environmental issues
and systemic barriers affect the health and well-being of the people and communities they serve. The rapidly deployed changes in community-based and clinical care, nursing education, nursing leadership, and nursing–community partnerships resulting from the COVID-19 pandemic have amplified those challenges. The deployment of all levels of nurses across the care continuum, including in collaborative practice models, will be necessary to address the challenges of building a more equitable and accessible health care system.
The United States is at an inflection point with respect to addressing disparities in health and well-being that have adversely impacted too many people for too long. The nation’s health care system is also at an inflection point in terms of meeting consumers’ health needs in ways and in places commensurate with their preferences. It is imperative that the nursing profession focus on the training and competency development needed to prepare nurses, including advanced practice nurses, to work competently in home and community-based as well as acute care settings and to lead efforts to build a culture of health and health equity. There is no time to waste. Over the next 10 years, nurses will assume even greater responsibility for helping to build an accessible, equitable, high-quality public health and health care system that works for everyone. The recommendations in this report are aimed at ensuring that nurses are inspired, supported, valued, and empowered in pursuing that goal so that by 2030, all individuals and communities will have the opportunities they need to live healthy lives.
Anderson, J. E., A. J. Ross, J. Back, M. Duncan, P. Snell, K. Walsh, and P. Jaye. 2016. Implementing resilience engineering for healthcare quality improvement using the CARE model: A feasibility study protocol. Pilot and Feasibility Studies 2(61). doi: 10.1186/s40814-016-0103-x.
NACNEP (National Advisory Council on Nurse Education and Practice). 2020. Integration of social determinants of health in nursing education, practice, and research . 16th Report to the Secretary of the U.S. Department of Health and Human Services and the U.S. Congress. Washington, DC: Health Resources and Services Administration.
The decade ahead will test the nation's nearly 4 million nurses in new and complex ways. Nurses live and work at the intersection of health, education, and communities. Nurses work in a wide array of settings and practice at a range of professional levels. They are often the first and most frequent line of contact with people of all backgrounds and experiences seeking care and they represent the largest of the health care professions.
A nation cannot fully thrive until everyone - no matter who they are, where they live, or how much money they make - can live their healthiest possible life, and helping people live their healthiest life is and has always been the essential role of nurses. Nurses have a critical role to play in achieving the goal of health equity, but they need robust education, supportive work environments, and autonomy. Accordingly, at the request of the Robert Wood Johnson Foundation, on behalf of the National Academy of Medicine, an ad hoc committee under the auspices of the National Academies of Sciences, Engineering, and Medicine conducted a study aimed at envisioning and charting a path forward for the nursing profession to help reduce inequities in people's ability to achieve their full health potential. The ultimate goal is the achievement of health equity in the United States built on strengthened nursing capacity and expertise. By leveraging these attributes, nursing will help to create and contribute comprehensively to equitable public health and health care systems that are designed to work for everyone.
The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity explores how nurses can work to reduce health disparities and promote equity, while keeping costs at bay, utilizing technology, and maintaining patient and family-focused care into 2030. This work builds on the foundation set out by The Future of Nursing: Leading Change, Advancing Health (2011) report.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
Research Topics & Ideas: Nursing
50+ Nursing Research Topic Ideas To Fast-Track Your Project
Finding and choosing a strong research topic is the critical first step when it comes to crafting a high-quality dissertation, thesis or research project. If you’ve landed on this post, chances are you’re looking for a nursing-related research topic , but aren’t sure where to start. Here, we’ll explore a variety of nursing-related research ideas and topic thought-starters, including general nursing, medical-surgical nursing, pediatric nursing, obstetrics and gynaecological nursing, ICU and mental health nursing.
NB – This is just the start…
The topic ideation and evaluation process has multiple steps . In this post, we’ll kickstart the process by sharing some research topic ideas within the nursing domain. This is the starting point, but to develop a well-defined research topic, you’ll need to identify a clear and convincing research gap , along with a well-justified plan of action to fill that gap.
If you’re new to the oftentimes perplexing world of research, or if this is your first time undertaking a formal academic research project, be sure to check out our free dissertation mini-course. In it, we cover the process of writing a dissertation or thesis from start to end. Be sure to also sign up for our free webinar that explores how to find a high-quality research topic.
Overview: Nursing Research Topics
- General nursing-related topics
- Medical-surgical nursing
- Pediatric nursing
- Obstetrics and gynaecological nursing
- ICU nursing
- Mental health nursing
General Nursing Research Topics & Ideas
- The impact of cultural competence on patient care in the UK
- The importance of evidence-based practice in nursing for patients with HIV/AIDS
- The effects of workplace stress on nurse well-being and performance
- The role of nurse-patient communication for patients transitioning from adolescent to adult care
- The impact of technology on nursing practice and patient outcomes
- The importance of interdisciplinary collaboration in healthcare for the rehabilitation of patients post-surgery
- The effects of fatigue on nurse performance in the emergency room
- The impact of nurse staffing levels on patient outcomes in rural areas
- The effectiveness of nurse-led interventions in managing chronic conditions: a case study of diabetes
- The impact of patient-centred care on health outcomes for the elderly
- The importance of patient safety in nursing: bedside nurse vigilance
- The effects of empathy and compassion in critical care nursing
- The role of nursing in disaster preparedness and response: a case study of the Haiti earthquake of 2021
- The impact of the level of nursing education on patient outcomes
- The importance of ethical considerations in frail care nursing practice
Topics & Ideas: Medical-Surgical Nursing
- The impact of bedside care on patient outcomes in medical-surgical units
- The role of the nurse in managing post-operative patient pain
- The effects of nurse-patient ratios on patient outcomes in medical-surgical units
- A systematic review of different approaches to patient education in medical-surgical units
- The relationship between nurse-patient communication and patient satisfaction in medical-surgical units: perspectives and recommendations to improving patient satisfaction
Topics & Ideas: Pediatrics Nursing
- The impact of family-centered care on pediatric patient outcomes with sickle cell anemia
- The role of nursing interventions in promoting developmental and behavioral health in pediatric patients
- The effects of play therapy on anxiety and pain in pediatric patients during hospitilisation
- A systematic review of different approaches to pain management in pediatric cancer patients
- The relationship between parent involvement and post-operative patient outcomes in pediatric units
Ideas: Obstetrics and Gynecological Nursing
- The impact of nurse-led prenatal care on maternal and fetal outcomes in African American communities
- The role of the nurse in promoting sexual and reproductive health for women in the UK
- The effects of midwifery care on maternal satisfaction of primiparous women and birth outcomes
- A comparative study of different approaches to childbirth education for expectant mothers and partners: perceptions of control
- The relationship between lactation support and breastfeeding success of primiparous women
Topics & Ideas: ICU Nursing
- The impact of nursing interventions on patient outcomes in intensive care units in a developing country
- The role of the nurse in managing palliative and end-of-life care in the ICU
- The effects of family presence on patient outcomes and satisfaction in the ICU: A systematic review of the literature
- A comparative study of different approaches to pain management for trauma patients in the ICU
- The relationship between nurse-patient communication and geriatric patient outcomes in ICU
Topics & Ideas: Mental Health Nursing
- The impact of nurse-led therapy on adolescent patient outcomes in mental health settings
- The role of the nurse in promoting recovery and resiliency in mental health patients through group interventions
- The effects of mindfulness-based interventions on stress and anxiety in mental health patients: A systematic literature review
- A comparative study of the role of nurses in applying different approaches to patient education in mental health settings
- The association between nurse-patient therapeutic alliance and patient outcomes in mental health settings
Nursing Dissertation & Theses
While the ideas we’ve presented above are a decent starting point for finding a nursing-related research topic, they are fairly generic and non-specific. So, it helps to look at actual dissertations and theses to see how this all comes together.
Below, we’ve included a selection of research projects from various nursing-related degree programs to help refine your thinking. These are actual dissertations and theses, written as part of Master’s and PhD-level programs, so they can provide some useful insight as to what a research topic looks like in practice.
- Nursing Workload and Interventions of Licensed Nurses in Nursing Homes: An Observational Time and Motion Study (Kang, 2021)
- Missed Nursing Care: Accounting for Education, Experience, and Job Satisfaction in Registered Nurses (Bechard, 2021)
- Examining Predictors of Attitudes and Knowledge of Registered Nurses and Nursing Students in Tennessee toward Pregnant and Perinatal Women with a Substance Use Disorder (Patrylo, 2021)
- A Program Evaluation of the Organizational Readiness for Pathway to Excellence at Two Community Hospitals (Behling, 2021)
- The Impact of Covid-19 Pandemic Policy Decisions on the Wellbeing of Nursing Home Residents in Missouri (White, 2022)
- Battling A Parallel Pandemic: An Evaluation of Sustainable System-Level Nursing Support in Response To COVID-19 (Gifford, 2022)
- Holistic Nursing Process Maps: a Tool for Student Nurses to Operationalize the Nursing Process to Increase Clinical Reasoning (Reyes, 2022)
- Satisfaction and Work-Life Balance in Undergraduate Nursing Faculty: A Mixed-Methods Study (Crawford, 2021)
- The Effect of Mindfulness Meditation on the Stress, Anxiety, Mindfulness, and Self-Compassion Levels of Nursing Students (Heinrich, 2022)
- Effectiveness of Simulation-Based Case Studies in Undergraduate Nursing Students (Becnel, 2022)
- A Telehealth Simulation Experiment: Exploring Prebriefing (Owen, 2022)
- Perceptions of Lateral Violence Among Vocational Nursing Students, Associate Degree Nursing Students, and Bachelor’s Degree Nursing Students (Martha, 2022)
- Nurse Educators’ Description of Ethics from a Disciplinary Perspective: A Qualitative Descriptive Research Study (Cuchetti, 2022)
- A Literature Review of the Relationship Between Oral Health and Pneumonia Risk in the Geriatric Nursing Home Population (Swift, 2021)
Looking at these titles, you can probably pick up that the research topics here are quite specific and narrowly-focused , compared to the generic ones presented earlier. This is an important thing to keep in mind as you develop your own research topic. That is to say, to create a top-notch research topic, you must be precise and target a specific context with specific variables of interest . In other words, you need to identify a clear, well-justified research gap.
Get 1-On-1 Help
If you’re still feeling a bit unsure about how to find a research topic for your nursing dissertation, thesis or research project, check out our private coaching services below.

You Might Also Like:

To learn from the GRAD Coach is a lofty goal for me. I am unable to express my gratitude for your teaching style. I need assistance with my thesis as a master’s in nursing candidate. Please assist me.
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
251+ Nursing Research Topics To Explore In 2024

Nursing research is an essential aspect of healthcare education, and it involves exploring various topics to improve patient care and outcomes. However, choosing the right nursing research topic can be challenging, especially for students who are new to the field. To help nursing students and professionals, we have compiled a list of 26 categories and 260 research ideas related to nursing research topics.
These categories include a large number of nursing research topics, including nursing ethics, paediatric nursing, mental health nursing, nursing education, nursing informatics, community health nursing, evidence-based nursing, nursing leadership, nursing management, nursing theory, holistic nursing, palliative care nursing, critical care nursing, maternal-child nursing, public health nursing, and more. By exploring these categories and research ideas, nursing students and professionals can gain valuable insights and inspiration for their research projects.
7 Tips For Nursing Students To Stay Fit And Healthy
Table of Contents
Before jumping on to the nursing research topics let us have a look at some of the tips for nursing students to stay fit and healthy:
- Stay Active: Take breaks during study sessions to stretch or walk. Find activities you enjoy, like dancing or cycling.
- Balanced Diet: Treat your body with a balanced diet and have good and healthy food. Include fruits, vegetables, proteins, and whole grains.
- Stay Hydrated: To stay fit, your water intake should be good to keep your body hydrated and drink water regularly.
- Tackle Stress: Practise relaxation techniques like deep breathing or meditation. Take breaks to recharge.
- Sleeping Schedule: Take regular sleep of around 7 to 9 hours. Quality sleep boosts energy and supports learning.
- Socialise: Connect with friends, join study groups, or engage in hobbies. Social support is key for mental health.
- Self-Care Routine: Take time for yourself. Whether it’s a warm bath, reading, or listening to music, prioritise self-care to recharge.
251+ Nursing Research Topics
Here we have made different categories and listed top 10 research topics for all of them. Let us start.
Nursing Research Topics On Patient Care Management
- Impact of Telehealth Services on Patient Care Outcomes
- Comparative Analysis of Nurse-Patient Ratios on Care Quality
- Role of Interdisciplinary Teams in Enhancing Patient Care
- Effectiveness of Patient Education Programs on Self-Management
- Integration of Technology in Patient Care: Efficacy and Challenges
- Assessing the Influence of Cultural Competency Training on Care Delivery
- Patient-Centred Care Models: Evaluation and Implementation
- Evaluating the Long-Term Effects of Care Continuity on Patient Health
- Utilisation of Evidence-Based Practice in Patient Care Decision-Making
- Patient Satisfaction and its Correlation with Care Management Practices
Nursing Education Techniques
- Efficacy of Simulation-Based Learning in Nursing Education
- Integrating Virtual Reality in Nursing Curriculum
- Impact of Peer-to-Peer Teaching Methods in Nursing Programs
- Assessing the Effectiveness of Online Education for Nursing Students
- Use of Gamification in Enhancing Nursing Education
- Comparative Analysis of Clinical vs. Classroom Learning in Nursing
- Cultural Competence Training in Nursing Education: Outcomes and Implementation
- Evaluation of Mentorship Programs for Nursing Students
- Incorporating Interprofessional Education in Nursing Curricula
- Adaptive Learning Techniques for Diverse Nursing Learners
Pain Management In Nursing
- Efficacy of Non-Pharmacological Interventions in Pain Management
- Comparative Analysis of Different Pharmacological Approaches for Pain Relief
- Impact of Holistic Care Practices on Pain Management Outcomes
- Nurse-Led Pain Management Interventions: Effectiveness and Patient Satisfaction
- Addressing Barriers to Effective Pain Assessment in Clinical Settings
- Integrating Complementary and Alternative Medicine in Pain Management Protocols
- Exploring the Role of Nursing Staff Training in Improved Pain Control
- Pain Management Strategies for Special Populations (Pediatrics, Geriatrics, etc.)
- The Influence of Patient Education on Pain Perception and Coping Mechanisms
- Pain Management in Palliative Care: Challenges and Best Practices
Quality Improvement In Healthcare
- Implementation of Lean Management Principles in Healthcare Settings
- Analysing the Impact of Electronic Health Records (EHR) on Quality Improvement
- Patient Safety Initiatives and their Effectiveness in Healthcare Quality
- Role of Interdisciplinary Teams in Enhancing Healthcare Quality
- Planning for Reducing Medical Errors and Adverse Events
- Continuous Quality Improvement Models in Healthcare Institutions
- Evaluating the Effectiveness of Benchmarking in Healthcare Quality
- Impact of Patient-Centred Care Models on Healthcare Quality
- Addressing Disparities in Healthcare Quality: Strategies and Interventions
- The Influence of Quality Improvement Initiatives on Cost-Efficiency in Healthcare
Mental Health Nursing Interventions
- Effectiveness of Mindfulness-Based Interventions in Mental Health Nursing
- Evaluating the Impact of Psychoeducation in Mental Health Nursing Practices
- Role of Therapeutic Communication in Psychiatric Nursing Care
- Integrating Art Therapy in Mental Health Nursing Interventions
- Comparative Analysis of Pharmacological vs. Non-Pharmacological Interventions
- Analysing the Efficacy of Cognitive Behavioral Therapy (CBT) in Mental Health Nursing
- Trauma-Informed Care in Mental Health Nursing: Implementation and Outcomes
- Evaluation of Family-Based Interventions in Psychiatric Nursing
- Integrating Technology-Assisted Interventions in Mental Health Nursing Care
- Addressing Stigma Reduction Interventions in Mental Health Nursing
Pediatric Nursing Practices
- Pain Management Strategies in Pediatric Nursing Care
- Impact of Family-Centred Care in Pediatric Nursing
- Effectiveness of Play Therapy in Pediatric Nursing Interventions
- Pediatric Immunization Practices: Efficacy and Adherence
- Psychosocial Support for Children with Chronic Illnesses
- Nurse-Led Education Programs for Pediatric Health Promotion
- Comparative Analysis of Pediatric Care in Different Healthcare Settings
- Integrating Technology in Pediatric Nursing: Benefits and Challenges
- Mental Health Screening and Support in Pediatric Nursing
- Palliative Care in Pediatrics: Enhancing Quality of Life
Geriatric Nursing Studies
- Fall Prevention Strategies in Geriatric Nursing Care
- Comparative Analysis of Pharmacological vs. Non-Pharmacological Approaches in Geriatric Care
- Assessing the Effectiveness of Dementia Care Models in Geriatric Nursing
- Role of Nutrition and Diet in Geriatric Health and Nursing Interventions
- Polypharmacy and Medication Management in Geriatric Nursing
- Geriatric Mental Health Interventions: Efficacy and Challenges
- Geriatric Palliative Care and End-of-Life Nursing Practices
- Evaluating Gerontechnology Integration in Geriatric Nursing Care
- Handling Social Isolation and Loneliness in Geriatric Nursing
- Nurse-Led Health Promotion Programs for Elderly Populations
Holistic Nursing Approaches
- Integrative Medicine and Holistic Nursing Practices
- Impact of Mind-Body Interventions in Holistic Nursing Care
- Comparative Analysis of Holistics vs. Traditional Nursing Interventions
- Spirituality and its Role in Holistic Nursing Care
- Wellness Promotion through Holistic Nursing Models
- Exploring the Efficacy of Alternative Therapies in Holistic Nursing
- Holistic Pain Management Strategies in Nursing Care
- Environmental and Occupational Health in Holistic Nursing Practices
- Holistic Health Assessments in Nursing Practice
- Cultural Competence and Diversity in Holistic Nursing Care
Nursing Ethics And Professionalism
- Ethical Dilemmas in End-of-Life Care: Nursing Perspectives
- Professional Boundaries in Nurse-Patient Relationships
- Ethical Implications of Artificial Intelligence in Nursing Practice
- Cultural Competence and Ethical Decision-Making in Nursing
- Professionalism and Social Media Use among Nurses
- Ethical Issues in Resource Allocation and Healthcare Equity
- Patient Advocacy and Ethical Nursing Practices
- Ethical Considerations in Nursing Research and Publication
- Legal and Ethical Challenges in Nursing Informatics
- Integrity and Ethical Decision-Making in Nursing Leadership
Nursing Research Topics On Nursing Informatics
- Impact of Electronic Health Records (EHR) on Nursing Workflow
- Integration of Artificial Intelligence in Nursing Informatics
- Usability and User Experience of Nursing Informatics Systems
- Data Security and Privacy in Nursing Informatics
- Telehealth and Remote Patient Monitoring in Nursing Informatics
- Standardisation and Interoperability in Nursing Informatics
- Big Data Analytics in Nursing for Improved Patient Outcomes
- Nursing Informatics and Clinical Decision Support Systems
- Mobile Health (mHealth) Applications in Nursing Practice
- Evaluating the Role of Informatics in Evidence-Based Nursing Practice
Community Health Nursing
- Effectiveness of Health Promotion Programs in Underserved Communities
- Effect of Community Health Nurses in Disease Prevention and Control
- Addressing Health Disparities in Urban vs. Rural Communities
- Effect of Community-Based Interventions on Public Health Outcomes
- Mental Health Support in Community Health Nursing
- Evaluating the Efficacy of School-Based Health Programs
- Community Health Nursing in Disaster Response and Preparedness
- Community Health Assessment and Planning Strategies
- Collaborative Partnerships in Community Health Nursing
- Assessing the Role of Technology in Enhancing Community Health Services
Palliative Care Research
- Level of Life Assessment in Palliative Care Settings
- Family Caregiver Support in Palliative Care
- Implementation of Palliative Care in Chronic Disease Management
- Spiritual and Existential Concerns in Palliative Care
- Palliative Care in Non-Oncological Conditions
- Palliative Care and End-of-Life Decision-Making
- Advance Care Planning and Preferences in Palliative Care
- Palliative Care for Paediatric Populations
- Healthcare Provider Training in Palliative Care Practices
- Cultural Competence in Palliative Care Settings
Nursing Leadership And Management
- Transformational Leadership in Nursing
- Diversity and Inclusion in Nursing Leadership
- Effective Strategies for Nurse Retention and Satisfaction
- Nurse Manager’s Role in Staff Well-being and Burnout Prevention
- Change Management in Nursing Practice
- Leadership Styles and its Effect on Patient Outcomes
- Collaborative Leadership in Interprofessional Healthcare Teams
- Mentorship and Succession Planning in Nursing Leadership
- Ethical Leadership in Nursing Management
- Financial Management in Nursing Practice
Nursing And Technology Integration
- Adoption and Implementation of Wearable Health Devices in Nursing
- Impact of Telemedicine on Nursing Practice and Patient Care
- Cybersecurity Challenges in Nursing Technology Integration
- Role of Artificial Intelligence in Nursing Decision Support Systems
- Robotics and Automation in Nursing Care
- Nursing Workflow Efficiency through Electronic Health Records (EHR)
- Assessing the effect of Virtual Reality in Nursing Education and Practice
- Patient Engagement and Empowerment through Health Apps
- Augmented Reality Applications in Nursing Training
- Blockchain Technology in Healthcare and Nursing Documentation
Evidence-Based Practice In Nursing
- Implementation Strategies for Evidence-Based Practice in Clinical Settings
- Assessing Barriers to the Adoption of Evidence-Based Nursing Interventions
- Long-Term Outcomes of Evidence-Based Practice in Nursing
- Impact of Evidence-Based Protocols on Patient Safety
- Evaluating the Role of Nursing Research in Shaping Evidence-Based Practice
- Patient Outcomes and Adherence to Evidence-Based Guidelines
- Incorporating Patient Preferences in Evidence-Based Nursing Care
- Sustainability of Evidence-Based Practice Initiatives in Nursing
- Nurse Education and Training in Evidence-Based Practice
- Comparative Effectiveness of Evidence-Based vs. Traditional Nursing Interventions
Cultural Competence In Nursing
- Cultural Competence Training Impact on Nursing Care
- Assessing Communication Challenges in Cross-Cultural Nursing
- Culturally Sensitive Care in End-of-Life Nursing Practices
- Effectiveness of Cultural Competence Assessments for Nursing Staff
- Cultural Competence and Health Disparities in Nursing Care
- Integrating Cultural Competence into Nursing Curriculum
- Cultural Competence in Mental Health Nursing Interventions
- Role of Cultural Competence in Patient Satisfaction and Outcomes
- Cultural Competence and Decision-Making in Nursing Practice
- Addressing Ethical Dilemmas in Culturally Diverse Nursing Settings
Women’s Health Nursing
- Maternal Health and Pregnancy Outcomes
- Addressing Disparities in Women’s Access to Healthcare
- Menopause Management and Quality of Life
- Breast Health and Screening Practices
- Women’s Mental Health and Nursing Interventions
- Reproductive Health and Family Planning Services
- Gender-Based Violence and Nursing Support
- Chronic Disease Management in Women’s Health
- Cultural Influences on Women’s Health Decision-Making
- Innovations in Women’s Health Nursing Care
Nursing Research Topics On Nursing Workforce Issues
- Nursing Shortages: Causes and Solutions
- Consequences of Nurse Staffing Levels on Patient Outcomes
- Nurse Burnout and Mental Health in the Workforce
- Diversity and Inclusion in the Nursing Profession
- Job Satisfaction and Retention Strategies for Nurses
- Transitioning to Remote Work in Nursing
- Effect of Shift Length and Schedule on Nursing Performance
- Generational Differences in the Nursing Workforce
- Global Mobility and Migration of Nurses
- Impact of Technology on the Future Nursing Workforce
Nursing And Chronic Disease Management
- Nurse-Led Chronic Disease Management Programs
- Impact of Education Programs on Chronic Disease Self-Management
- Integrative Medicine in Chronic Disease Nursing Care
- Nurse Practitioner Role in Chronic Disease Management
- Home-Based Chronic Disease Care by Nursing Teams
- Palliative Care Integration in Chronic Disease Management
- Telemedicine and Remote Monitoring in Chronic Disease Nursing
- Cultural Competence in Chronic Disease Nursing Care
- Addressing Health Disparities in Chronic Disease Management
- Long-Term Outcomes of Nursing Interventions in Chronic Disease
Critical Care Nursing Research
- Early Mobilisation in Critical Care Patients
- Nurse Staffing Ratios and Patient Outcomes in Critical Care Units
- Sedation Practices and Patient Outcomes in Intensive Care
- Family-Centred Care in Critical Care Settings
- Infection Control Measures in Critical Care Nursing
- Impact of Nurse Education on Critical Care Patient Outcomes
- Ethical Dilemmas in Critical Care Nursing Practice
- End-of-Life Care in Critical Care Settings
- Technology Integration in Critical Care Nursing
- Burnout and Resilience among Critical Care Nurses
Healthcare Policy And Nursing
- Impact of Health Policy Changes on Nursing Practice
- Advocacy Role of Nurses in Health Policy Development
- Nursing Workforce Policies and Healthcare Delivery
- Access to Healthcare Services and Nursing Advocacy
- Health Equity Policies and Nursing Interventions
- Regulatory Policies and Nursing Practice Standards
- Nursing Leadership Influence on Health Policy
- Global Health Policy and Nursing Contributions
- Telehealth Policy Implementation in Nursing Practice
- Healthcare Financing Policies and Nursing Implications
Nursing In Disaster Management
- Communication Strategies in Disaster Nursing
- Psychological First Aid in Disaster Situations
- Triage Protocols during Natural Disasters
- Role of Nurses in Mass Casualty Incidents
- Resilience and Coping Mechanisms in Disaster Nursing
- Community Preparedness and Nursing Response
- Mobile Health Units in Disaster Relief
- Ethics and Decision Making in Crisis Nursing
- Nursing Leadership in Disaster Response
- Training and Education for Nurses in Disaster Management
Health Promotion And Diseases Prevention
- Effectiveness of Community-Based Health Promotion Programs
- Role of Technology in Disease Prevention Initiatives
- Impact of Lifestyle Modifications on Disease Prevention
- Cultural Adaptation in Health Promotion Strategies
- Workplace Wellness Programs and Disease Prevention
- Public Policy and Disease Prevention Interventions
- Health Literacy and Disease Prevention Outcomes
- Integrative Medicine in Health Promotion
- Behavioral Economics and Health Behavior Change
- Environmental Factors in Disease Prevention
Nursing Research Topics On Ethical Issues In Nursing
- End-of-Life Decision Making and Nursing Ethics
- Informed Consent in Nursing Practice
- Ethical Challenges in Nurse-Patient Relationships
- Confidentiality and Privacy in Nursing Care
- Cultural Competence and Ethical Care Delivery
- Allocation of Scarce Resources in Nursing
- Ethical Implications of Advanced Technology in Nursing
- Moral Distress Among Nurses
- Ethical Dilemmas in Mental Health Nursing
- Professional Boundaries and Ethical Practice in Nursing
Infectious Disease Control
- Effectiveness of Vaccination Campaigns in Disease Control
- Antibiotic Resistance and Infection Control
- Nosocomial Infections and Hospital Protocols
- Contact Tracing Strategies in Controlling Outbreaks
- Behavioral Interventions for Infectious Disease Prevention
- Pandemic Preparedness and Response Plans
- Role of Public Health Policies in Disease Control
- Environmental Factors in Infectious Disease Transmission
- Community Engagement in Disease Control Efforts
- Surveillance Systems for Infectious Disease Monitoring
Wound Care And Healing
- Advanced Wound Dressings and Healing Outcomes
- Biofilm Management in Chronic Wounds
- Role of Nutrition in Wound Healing
- Pressure Ulcer Prevention and Treatment Strategies
- Regenerative Medicine in Wound Care
- Innovations in Wound Closure Techniques
- Pain Management in Wound Care
- Psychological Impact of Chronic Wounds on Patients
- Factors Influencing Scar Formation and Management
- Telemedicine Applications in Wound Assessment
As we wrap up this exploration of nursing research topics, remember, the world of nursing is vast, diverse, and always evolving. These 26 categories we’ve covered offer an introduction into the huge possibilities for research within this field. With 260 research ideas to spark your curiosity, there’s something here for every aspiring nurse researcher.
But this is just the beginning. The beauty of nursing research lies in its ability to make a real impact, from improving patient care to shaping healthcare policies. Your journey doesn’t end here; it’s the first step towards contributing to a healthier, more informed world.
So, take these categories and ideas as inspiration. Dive deeper, ask questions, and let your passion for nursing guide your research works. Each idea is a curiosity waiting to bloom into a significant contribution to the nursing profession. Increase your curiosity, enjoy the challenges, and most importantly, feel the journey of discovery in nursing research. The future of healthcare eagerly awaits your perception and innovations!
Related Posts

Step by Step Guide on The Best Way to Finance Car

The Best Way on How to Get Fund For Business to Grow it Efficiently
Top Nursing Research Topics for Students and Professionals
This article was written in collaboration with Christine T. and ChatGPT, our little helper developed by OpenAI.
Nursing research is an essential component of the nursing profession. Its primary purpose is to enhance patient outcomes, elevate the quality of care, and advance nursing as a whole. For nursing students and practitioners, selecting an appropriate research topic is crucial for academic and professional success. This article highlights some current and interesting topics in nursing research that students and professionals can explore.
Nursing Workforce
One of the major topics in nursing research is the challenges that nurses face in their workplace, and how to address them. This is particularly relevant in light of the current shortage of nurses and the healthcare industry’s growing demands.
List of Nursing Research Topics: Nursing Workforce
- The impact of nurse staffing levels on patient outcomes in acute care settings
- The effectiveness of nurse retention strategies on improving nurse job satisfaction
- The role of nursing leadership in creating a positive work environment
- The relationship between nurse staffing ratios and nurse burnout
- The impact of nurse-to-patient ratios on nursing care quality in long-term care settings
- The effectiveness of nurse residency programs in improving new nurse retention rates
- The impact of nursing unit culture on nurse job satisfaction and retention
- The impact of nurse-patient ratios on patient outcomes
- Strategies for retaining experienced nurses in the workforce
- Analyzing the role of advanced practice nurses in healthcare teams
- The challenges and benefits of international nursing recruitment
- Addressing generational differences in the nursing workforce
- The relationship between nurse work schedules and nurse burnout
- The impact of nurse staffing levels on medication errors in hospital settings
- The role of interprofessional collaboration in reducing nursing workload and improving patient outcomes
- The impact of nursing education level on nursing practice and patient outcomes
- The relationship between nurse staffing levels and patient falls in acute care settings
- The impact of nurse workload on patient satisfaction with nursing care
- The role of nursing leadership in promoting staff well-being and reducing burnout
- The relationship between nurse staffing levels and patient mortality rates in critical care settings
- The effectiveness of nurse-led care models in improving patient outcomes and reducing healthcare costs
- The impact of nurse staffing levels on patient readmission rates in acute care settings
- The role of nursing autonomy in improving nursing practice and patient outcomes
- The relationship between nurse job satisfaction and patient outcomes in long-term care settings
- The impact of nursing staff turnover on patient safety and quality of care
- Healthcare management: career paths and requirements
- The role of technology in improving nursing efficiency and reducing workload
- The relationship between nurse staffing levels and patient satisfaction with nursing care
- The impact of nurse staffing levels on nurse job stress and burnout in pediatric settings
- The effectiveness of nurse-led interventions in improving patient outcomes for chronic conditions
- The role of nursing leadership in promoting a culture of safety and reducing patient harm
- The relationship between nurse staffing levels and patient outcomes in psychiatric settings
- The impact of nurse staffing levels on nurse job satisfaction and burnout in emergency departments
- The effectiveness of nursing education programs in improving nurse practice and patient outcomes
- The role of nurse practitioners in improving access to healthcare in underserved communities
- The relationship between nurse staffing levels and patient outcomes in rehabilitation settings
- The impact of nurse staffing levels on nurse retention rates in rural healthcare facilities
- The effectiveness of nurse-led discharge planning in reducing hospital readmissions
- The role of nursing leadership in promoting interprofessional collaboration and teamwork
- The relationship between nurse staffing levels and patient outcomes in outpatient care settings
- The impact of nursing workloads on patient safety in intensive care units
- The role of nursing research in improving nursing practice and patient outcomes
- The relationship between nurse staffing levels and nurse job satisfaction in surgical settings
- The impact of nurse staffing levels on patient satisfaction with pain management in acute care settings
- The effectiveness of nursing education programs in improving nursing knowledge and skills
- The role of nursing advocacy in promoting patient-centered care and improving healthcare outcomes
Medical Studies Overwhelming?
Delegate Your Nursing Papers to the Pros!
Get 15% Discount
+ Plagiarism Report for FREE
Patient Safety
Another crucial area of nursing research is patient safety. Studying ways to enhance patient safety, reduce adverse events, and improve the quality of care in hospitals and other healthcare settings can help prevent patient harm and improve patient outcomes.
List of Nursing Research Topics: Patient Safety
- Exploring the impact of workplace stress on nurses’ job satisfaction and performance
- Investigating the factors that influence nurse turnover and retention rates
- Assessing the role of nurse staffing levels in patient outcomes and quality of care
- Examining the relationship between nurse burnout and patient safety incidents
- Investigating the effectiveness of nursing leadership in creating a positive work environment
- The influence of nursing handovers on patient safety
- Strategies to reduce medication errors in hospital settings
- The role of electronic health records in enhancing patient safety
- Impact of nurse-to-patient ratios on patient safety outcomes
- Evaluating the effectiveness of patient safety training programs for nurses
- Exploring the experiences of nurses from diverse backgrounds in the workplace
- Assessing the impact of shift work on nurses’ physical and mental health
- Investigating the relationship between nurse-patient ratios and patient outcomes
- Examining the role of interprofessional collaboration in improving the nursing work environment
- Exploring the use of technology to improve nursing workflow and productivity
- Mitigating the economic and social costs of heart diseases among the aging population in the US
- Investigating the effectiveness of nursing mentorship programs in retaining new nurses
- Assessing the role of organizational culture in promoting nurse well-being and job satisfaction
- Examining the impact of nursing education on nursing workforce preparedness
- Exploring the factors that contribute to job satisfaction among nurses
- Combating health care-associated infections: a community-based approach
- Investigating the impact of nurse-led care on patient outcomes and satisfaction
- Assessing the effectiveness of nursing support programs for nurses with mental health issues
- Examining the role of nursing unions in advocating for the nursing workforce
- Exploring the experiences of male nurses in the nursing workforce
- Investigating the effectiveness of nurse-led clinics in reducing emergency department visits
- Assessing the impact of nursing teamwork on patient outcomes and quality of care
- Examining the role of nursing informatics in improving nursing workflow and patient care
- Exploring the impact of nursing shortages on patient outcomes and quality of care
- Investigating the effectiveness of nurse-led interventions for reducing hospital readmissions
- Assessing the impact of nursing certification on nursing workforce competence and confidence
- Examining the role of nursing education in promoting cultural competence in the nursing workforce
- Exploring the experiences of nurses working in rural healthcare settings
- Investigating the effectiveness of nursing delegation in improving patient outcomes and quality of care
- Assessing the impact of nursing shortages on nurse job satisfaction and burnout
- Examining the role of nursing research in informing nursing workforce policies and practices
- Exploring the impact of nurse-led quality improvement initiatives on patient outcomes and satisfaction
- Investigating the role of nursing leaders in promoting nursing workforce diversity and inclusion
- Assessing the impact of nursing autonomy on nurse job satisfaction and performance
- Examining the effectiveness of nursing residency programs in preparing new nurses for the workforce
- Exploring the experiences of nurses working in correctional healthcare settings
- Investigating the impact of nurse staffing levels on patient falls and injuries
- Assessing the role of nursing education in promoting evidence-based practice in the nursing workforce
- Examining the effectiveness of nursing preceptorship programs in improving nurse job satisfaction and retention
- Exploring the role of nursing education in preparing nurses for leadership roles in the nursing workforce
- Investigating the effectiveness of nursing empowerment interventions in improving nursing job satisfaction and performance
- Assessing the impact of nursing shortages on the quality of nursing care provided to older adults in long-term care facilities.
Chronic Illness Management
Managing chronic diseases, such as diabetes, cancer, and heart disease, is a significant challenge for healthcare providers. Exploring different strategies for chronic disease management can help improve patient outcomes and enhance the quality of care.
List of Nursing Research Topics: Chronic Illness Management
- The Role of Nurses in Managing Chronic Heart Disease
- Impact of Nurse-led Interventions in Managing Chronic Obstructive Pulmonary Disease (COPD)
- The Effectiveness of Self-management Education in Patients with Type 2 Diabetes
- Nursing Strategies for Chronic Pain Management
- Chronic Kidney Disease Management: A Nursing Perspective
- Palliative Care in Chronic Illness Management
- Community Nursing and Chronic Illness: A Study on Patient Outcomes
- The Role of Nurses in Managing Chronic Pediatric Asthma
- Telehealth and Chronic Disease Management: The Future of Nursing Practice?
- Evaluating the role of nursing in diabetes self-management
- Strategies for improving patient adherence to chronic illness treatment plans
- The impact of nurse-led interventions on chronic obstructive pulmonary disease (COPD) management
- Exploring the role of telehealth in chronic illness follow-up and monitoring
- The effectiveness of nurse-led educational programs for patients with cardiovascular diseases
- The Importance of Nurse-led Clinics in Chronic Illness Management
- The Role of Nursing in Depression Management among Chronically Ill Patients
- Empowering the vulnerable: enhancing health and social care for individuals with specific needs
- Advanced Practice Nurses and Chronic Illness Management: A Systematic Review
- The Impact of Holistic Nursing Care on Chronic Disease Management
- The Effect of Nurse-led Health Education on Compliance in Chronic Disease Patients
- The Role of Family Nurses in the Management of Chronic Illness in Home Settings
- Nursing and the Management of Chronic Illness in Geriatric Populations
- The Influence of Nursing Interventions on Quality of Life in Patients with Chronic Illness
- Challenges Faced by Nurses in Managing Chronic Illness in Low-resource Settings
- Cancer Pain: Assessment, Management, and Patient Empowerment
- Evaluating the Role of School Nurses in Managing Chronic Illnesses in Children
- Developing a Chronic Disease Management Model: The Crucial Role of Nursing
- Nursing Intervention in Lifestyle Modification for Chronic Illness Patients
- The Impact of Patient-Nurse Communication in Chronic Illness Management
- The Role of Nursing in Medication Management for Chronic Illness Patients
- The Effects of Nursing Care Coordination on Chronic Illness Outcomes
- Mental Health and Chronic Illness: The Importance of Psychiatric Nursing
- The Role of Nursing in the Self-Management of Chronic Illness: A Meta-Analysis
- Nursing Interventions for Chronic Illness Management in Rural Areas
- Nurses’ Role in Reducing Hospital Readmissions for Chronic Illness Patients
- Digital healthcare and organizational learning: enhancing patient care through technology and knowledge management
- The Impact of Nursing on Patient Empowerment in Chronic Illness Management
- Cultural Competence in Nursing and Its Effect on Chronic Disease Management
- The Role of Nursing Informatics in Chronic Illness Management
- Evaluating the Role of Community Health Nurses in Chronic Illness Prevention
- The Impact of Home Nursing on Chronic Illness Management in Aging Populations
- The ongoing risk of HIV/AIDS among men who have sex with men
- The Role of Oncology Nurses in the Management of Chronic Cancer Pain
- The Effects of Nursing-led Cognitive Behavioral Therapy in Chronic Illness Management
- The Impact of Advanced Nursing Practice on Health Outcomes in Chronic Disease Management
- The Use of Digital Health Technologies in Chronic Disease Management: A Nursing Perspective
Mental Health
Promoting mental health and well-being in vulnerable patient populations is another important area of nursing research. Nurses can investigate various interventions and programs that can help prevent mental health problems and improve patients’ overall well-being.
List of Nursing Research Topics: Mental Health
- The impact of COVID-19 on mental health in healthcare workers
- The effectiveness of telehealth for delivering mental health services
- The role of social support in promoting mental health and wellbeing
- Investigating the effectiveness of mindfulness-based interventions for mental health
- Examining the use of virtual reality in treating mental health disorders
- The impact of sleep on mental health outcomes
- The role of exercise in promoting mental health and wellbeing
- The effectiveness of psychotherapy in treating depression
- Exploring the relationship between mental health and chronic pain
- Investigating the impact of workplace stress on mental health in nurses
- The effectiveness of nurse-led interventions for patients with depression
- Exploring the impact of nurse-patient relationships on mental health outcomes
- Strategies for improving mental health literacy among nursing professionals
- Evaluating the role of nurses in suicide prevention and intervention
- The challenges and strategies in nursing care for patients with dual diagnoses (co-existing mental health and substance use disorders)
- Examining the use of music therapy for mental health promotion
- The effectiveness of cognitive-behavioral therapy for anxiety disorders
- The relationship between mental health and nutrition
- The impact of trauma on mental health outcomes
- Investigating the use of art therapy in promoting mental health and wellbeing
- The role of spirituality in mental health and coping
- The effectiveness of group therapy for mental health disorders
- The impact of stigma on mental health outcomes
- Examining the effectiveness of psychopharmacology in treating mental health disorders
- The role of family support in promoting mental health and wellbeing
- Investigating the relationship between mental health and substance abuse
- The effectiveness of animal-assisted therapy in promoting mental health and wellbeing
- The impact of social media on mental health outcomes
- Examining the use of humor in promoting mental health and wellbeing
- The effectiveness of cognitive training for improving mental health outcomes
- Investigating the impact of gender and cultural factors on mental health outcomes
- The role of occupational therapy in promoting mental health and wellbeing
- Examining the effectiveness of acceptance and commitment therapy for mental health disorders
- The relationship between mental health and physical activity
- Investigating the use of peer support for mental health promotion
- The effectiveness of mindfulness-based stress reduction for mental health
- The impact of technology on mental health outcomes
- The role of nutrition in treating mental health disorders
- Examining the use of hypnotherapy in promoting mental health and wellbeing
- The effectiveness of psychotherapy for PTSD
- Investigating the relationship between mental health and social determinants of health
- The impact of social isolation on mental health outcomes
- Examining the use of dance therapy in promoting mental health and wellbeing
- The effectiveness of cognitive processing therapy for mental health disorders
- The role of self-care in promoting mental health and wellbeing in nurses
Health Promotion
Research into health promotion strategies using technology, social media, and other digital tools is a rapidly growing area of nursing research. Such research can help identify innovative and effective ways to promote health and well-being in communities and patient populations.
List of Nursing Research Topics: Health Promotion
- The effectiveness of community-based interventions in promoting physical activity and healthy eating habits
- Investigating the impact of social media on health behavior and lifestyle changes
- The role of nursing in promoting healthy behaviors and preventing chronic diseases
- Identifying effective strategies for improving health literacy among underserved populations
- Exploring the use of wearable technology in promoting physical activity and healthy lifestyles
- Evaluating the effectiveness of nurse-led health promotion campaigns on community health outcomes
- The role of nurses in promoting vaccinations in various populations
- Strategies for nurses to address health literacy and its impact on patient outcomes
- The influence of cultural competence in health promotion and disease prevention
- Assessing the role of nurses in promoting physical activity and healthy lifestyles in at-risk populations
- Investigating the role of family support in promoting healthy behaviors among children and adolescents
- Examining the effectiveness of peer-led interventions in promoting healthy lifestyles
- Investigating the impact of workplace wellness programs on employee health and productivity
- The impact of milk consumption on children’s growth
- The role of nursing in promoting smoking cessation and reducing tobacco use
- Exploring the use of motivational interviewing in promoting behavior change and improving health outcomes
- Investigating the effectiveness of mindfulness-based interventions in promoting mental and physical health
- The role of social support in promoting healthy behaviors and preventing chronic diseases
- Examining the effectiveness of school-based interventions in promoting healthy behaviors among children and adolescents
- Exploring the use of technology in promoting health education and behavior change
- Investigating the role of culture and ethnicity in promoting healthy behaviors and preventing chronic diseases
- Nursing: a beautiful blend of art and science
- Examining the effectiveness of community health worker programs in promoting healthy lifestyles
- The role of nursing in promoting healthy aging and preventing age-related diseases
- Investigating the impact of environmental factors on health behavior and lifestyle changes
- Exploring the use of incentives in promoting behavior change and improving health outcomes
- Investigating the effectiveness of group-based interventions in promoting healthy lifestyles
- Examining the impact of policy interventions on health behavior and lifestyle changes
- The effects of sleep deprivation on students’ cognitive functions and emotional state
- The role of nursing in promoting healthy sleep habits and reducing sleep disorders
- Investigating the effectiveness of mobile health interventions in promoting behavior change and improving health outcomes
- Exploring the use of positive psychology interventions in promoting mental and physical health
- Investigating the role of healthcare providers in promoting healthy behaviors and preventing chronic diseases
- Examining the effectiveness of workplace policies in promoting healthy lifestyles
- The role of nursing in promoting healthy sexual behaviors and preventing sexually transmitted infections
- Investigating the impact of stress on health behavior and lifestyle changes
- Exploring the use of community-based participatory research in promoting healthy behaviors and preventing chronic diseases
- The delicate dance: balancing art and science in the nursing profession
- Investigating the role of nutrition in promoting healthy behaviors and preventing chronic diseases
- Examining the effectiveness of self-management interventions in promoting healthy lifestyles
- The role of nursing in promoting healthy pregnancy and preventing maternal and child health problems
- Investigating the impact of socioeconomic status on health behavior and lifestyle changes
- Exploring the use of health coaching in promoting behavior change and improving health outcomes
- Investigating the role of spirituality in promoting mental and physical health
- Examining the effectiveness of school-based policies in promoting healthy lifestyles
- The role of nursing in promoting healthy relationships and preventing intimate partner violence
- Investigating the impact of social determinants of health on health behavior and lifestyle changes
- Exploring the use of mobile applications in promoting healthy behaviors and preventing chronic diseases
- Investigating the role of health literacy in promoting healthy behaviors and preventing chronic diseases
Palliative Care
Improving the quality of life of seriously ill patients and their families during end-of-life care is another critical area of nursing research. Nurses can explore different interventions and support programs that can enhance the palliative care experience.
List of Nursing Research Topics: Palliative Care
- The effectiveness of palliative care on improving quality of life for cancer patients
- Understanding the needs and experiences of family caregivers in palliative care
- Palliative care and end-of-life decision-making: exploring patient and family preferences
- Optimizing the clarifying diagnosis of stomach cancer
- Improving access to palliative care for patients in rural areas
- The role of spirituality in palliative care for terminally ill patients
- Investigating the impact of music therapy on patients receiving palliative care
- Developing effective communication strategies for discussing end-of-life care with patients and families
- Exploring the experiences and needs of patients with non-cancer diagnoses in palliative care
- The impact of nurse-led interventions in improving the quality of life for patients in palliative care
- Evaluating the training needs of nurses in delivering end-of-life care
- The role of nursing in managing symptoms and side effects in palliative care patients
- Strategies for improving communication between nurses and families during end-of-life care
- Assessing the ethical considerations and challenges faced by nurses in palliative care settings
- Evaluating the effectiveness of home-based palliative care programs
- Palliative care for pediatric patients: understanding unique challenges and opportunities
- The impact of cultural and ethnic differences on palliative care provision
- Investigating the role of social support in palliative care for older adults
- The effectiveness of advance care planning in improving end-of-life care
- Understanding the experiences and needs of patients with neurological diseases in palliative care
- Exploring the impact of palliative care on reducing healthcare costs
- Investigating the role of complementary therapies in palliative care
- Improving symptom management in palliative care through medication optimization
- Palliative care and spiritual care: exploring the intersection of these two domains
- The impact of palliative care on reducing hospital readmissions
- Investigating the role of occupational therapy in palliative care
- Developing effective pain management strategies for patients receiving palliative care
- Understanding the experiences and needs of patients with heart failure in palliative care
- The role of pet therapy in improving quality of life for patients in palliative care
- Investigating the impact of palliative care on reducing caregiver burden
- Understanding the experiences and needs of patients with lung disease in palliative care
- Exploring the impact of palliative care on reducing healthcare utilization
- Investigating the role of nutrition in palliative care for patients with cancer
- Understanding the experiences and needs of patients with kidney disease in palliative care
- Improving palliative care for patients with dementia: exploring unique challenges and opportunities
- The role of art therapy in improving quality of life for patients in palliative care
- Investigating the impact of palliative care on reducing emergency department visits
- Developing effective communication strategies for discussing end-of-life care with patients with cognitive impairment
- Understanding the experiences and needs of patients with liver disease in palliative care
- Palliative care for patients with substance use disorders: unique challenges and opportunities
- Investigating the role of physiotherapy in palliative care
- The effectiveness of psychotherapy in improving mental health outcomes for patients in palliative care
- Understanding the experiences and needs of patients with multiple chronic conditions in palliative care
- Improving symptom management in palliative care through non-pharmacological interventions
- Investigating the impact of palliative care on reducing healthcare disparities
- Palliative care and medical aid in dying: exploring ethical and legal considerations
Healthcare Disparities
Studying the factors that contribute to healthcare disparities between different populations and identifying strategies to address these disparities is an important area of nursing research. Nurses can examine the role of social determinants of health in healthcare disparities and propose solutions to improve access and equity in healthcare.
List of Nursing Research Topics: Healthcare Disparities
- Examining the relationship between socioeconomic status and healthcare disparities
- Investigating the impact of implicit bias on healthcare disparities
- Analyzing the impact of racial and ethnic disparities on health outcomes
- Identifying disparities in access to preventative care among different populations
- Exploring the impact of language barriers on healthcare disparities
- Investigating the impact of discrimination on healthcare outcomes
- Identifying disparities in health insurance coverage and access to healthcare services
- Exploring the importance of national health insurance for socioeconomic growth
- Analyzing the impact of geographic location on healthcare disparities
- Evaluating the role of nursing in addressing healthcare disparities in underserved communities
- The impact of socioeconomic factors on patient outcomes and nursing interventions
- Strategies for nurses to promote health equity in diverse patient populations
- Assessing the influence of cultural competence on reducing healthcare disparities
- The role of nursing advocacy in shaping policies to reduce health inequities
- Examining disparities in mental health care access and utilization
- Investigating disparities in maternal and child health outcomes
- Exploring the relationship between healthcare disparities and chronic disease outcomes
- Identifying disparities in end-of-life care and hospice utilization
- Analyzing the impact of cultural differences on healthcare outcomes
- Investigating disparities in healthcare provider communication and patient engagement
- Examining the impact of healthcare policy on healthcare disparities
- Global health learning in nursing and health care disparities
- Identifying disparities in healthcare access and utilization among the LGBTQ+ community
- Exploring the impact of environmental factors on healthcare disparities
- Analyzing the impact of social determinants of health on healthcare disparities
- Investigating disparities in healthcare access and utilization among rural populations
- Examining disparities in healthcare access and utilization among urban populations
- Identifying disparities in healthcare access and utilization among immigrants and refugees
- Analyzing the impact of education level on healthcare disparities
- Investigating disparities in healthcare access and utilization among older adults
- Examining disparities in dental health access and utilization
- Identifying disparities in mental health treatment and access to services
- Analyzing the impact of stigma on healthcare outcomes for marginalized populations
- Investigating disparities in healthcare access and utilization among incarcerated populations
- Exploring disparities in healthcare access and utilization among individuals with disabilities
- Analyzing the impact of institutional racism on healthcare disparities
- Investigating disparities in healthcare access and utilization among low-income populations
- Examining disparities in cancer screening and early detection
- Identifying disparities in access to clinical trials and experimental treatments
- Analyzing the impact of the digital divide on healthcare disparities
- Investigating disparities in healthcare access and utilization among veterans
- Exploring the impact of healthcare worker bias on healthcare disparities
- Examining the relationship between healthcare disparities and infant mortality rates
- Identifying disparities in healthcare access and utilization among people with limited English proficiency
- Analyzing the impact of gender on healthcare disparities
- Investigating disparities in healthcare access and utilization among individuals experiencing homelessness
- Exploring the impact of COVID-19 on healthcare disparities among different populations
Patient-Centered Care
Enhancing patient-centered care, including patient feedback, patient-centered communication, and patient education, is another vital area of nursing research. Nurses can investigate the impact of patient-centered care on patient outcomes and identify ways to incorporate patient preferences and values in the care process.
List of Nursing Research Topics: Patient-Centered Care
- The importance of patient-centered care in improving health outcomes
- Exploring the effectiveness of patient-centered communication in clinical practice
- Assessing patient satisfaction with patient-centered care
- The impact of nursing staffing on patient-centered care
- The role of family and caregiver involvement in patient-centered care
- The use of technology to enhance patient-centered care
- Patient education and empowerment in promoting patient-centered care
- The role of nurses in facilitating shared decision-making in patient care
- Evaluating the impact of personalized care plans on patient outcomes and satisfaction
- Strategies for nurses to engage patients in their care across diverse cultural backgrounds
- The influence of effective communication strategies on the delivery of patient-centered care
- Assessing the barriers and facilitators to implementing patient-centered care in various healthcare settings
- The impact of culture on patient-centered care
- Measuring the quality of patient-centered care in healthcare settings
- The benefits of interdisciplinary collaboration in patient-centered care
- Understanding home dialysis: benefits, barriers, and impacts on elderly patients and the healthcare system
- Addressing language barriers in patient-centered care
- Exploring the challenges of implementing patient-centered care in healthcare organizations
- The role of patient-centered care in reducing healthcare costs
- The impact of patient-centered care on patient safety
- The importance of patient-centered care for vulnerable populations
- The role of leadership in promoting patient-centered care
- Evaluating the impact of patient-centered care on healthcare outcomes
- Examining the effectiveness of patient-centered care in chronic disease management
- The impact of patient-centered care on patient adherence to treatment
- The importance of patient-centered care in pediatric healthcare settings
- The use of patient feedback to improve patient-centered care
- Pediatric oncology: working towards better treatment through evidence-based research
- The role of patient-centered care in addressing health disparities
- Patient-centered care in end-of-life and palliative care settings
- The role of healthcare professionals in promoting patient-centered care
- The impact of patient-centered care on healthcare provider job satisfaction
- The importance of patient-centered care in emergency and critical care settings
- The use of simulation-based training to enhance patient-centered care
- The impact of patient-centered care on patient experience and engagement
- The role of healthcare policy in promoting patient-centered care
- Addressing the needs of patients with complex medical needs in patient-centered care
- The role of the nursing profession in promoting patient-centered care
- Patient-centered care in mental health and psychiatric settings
- The impact of patient-centered care on healthcare provider burnout
- The role of patient-centered care in promoting shared decision-making
- Examining the effectiveness of patient-centered care in rural healthcare settings
- The impact of patient-centered care on patient quality of life
- The use of patient-centered care in managing acute and chronic pain
- Addressing the needs of elderly patients in patient-centered care
- The impact of patient-centered care on healthcare system performance
- Promoting patient-centered care through the use of standardized patient education materials
Nursing Education
Exploring innovative approaches to nursing education and training, such as simulation-based learning and online learning, is a growing area of nursing research. Such research can help identify effective ways to prepare nursing students for their future roles in the healthcare system.
List of Nursing Research Topics: Nursing Education
- The impact of simulation-based training on nursing education outcomes
- The effectiveness of online learning in nursing education
- Innovative approaches to clinical teaching in nursing education
- The role of technology in nursing education
- Student perceptions of nursing education and their impact on learning outcomes
- The impact of cultural competence training on nursing students’ attitudes and behaviors
- The effectiveness of peer-led teaching in nursing education
- Best practices for incorporating interprofessional education into nursing curricula
- The role of reflective practice in nursing education
- The effectiveness of flipped classroom models in nursing education
- The impact of virtual reality and augmented reality tools in nursing education
- Evaluating the effectiveness of online vs. traditional classroom nursing education
- Strategies for enhancing interprofessional education in nursing curricula
- The role of continuous professional development in enhancing nursing competencies
- Assessing the influence of mentorship programs on nursing student success and retention
- Transforming advanced nursing practice: embracing IOM recommendations and higher education
- The impact of mentorship on nursing students’ learning and professional development
- The use of team-based learning in nursing education
- The effectiveness of hands-on skills training in nursing education
- Student perceptions of clinical experiences in nursing education
- The impact of service learning on nursing students’ attitudes and behaviors
- The role of cultural humility in nursing education
- The effectiveness of blended learning in nursing education
- Best practices for incorporating patient-centered care into nursing curricula
- The impact of standardized patient encounters on nursing education outcomes
- Importance and application of patient education technology in healthcare
- The use of case-based learning in nursing education
- The role of faculty development in improving nursing education outcomes
- The effectiveness of clinical reasoning strategies in nursing education
- The impact of nursing education on patient outcomes
- The role of simulation in teaching critical thinking in nursing education
- Best practices for incorporating evidence-based practice into nursing curricula
- The use of gamification in nursing education
- The effectiveness of problem-based learning in nursing education
- The impact of nursing education on student stress and burnout
- The role of intercultural competence in nursing education
- The effectiveness of collaborative learning in nursing education
- The impact of teaching communication skills in nursing education
- Best practices for incorporating patient safety into nursing curricula
- The role of interprofessional collaboration in nursing education
- The effectiveness of clinical coaching in nursing education
- The impact of teaching teamwork skills in nursing education
- The use of high-fidelity simulation in nursing education
- The role of experiential learning in nursing education
- Best practices for incorporating leadership development into nursing curricula
- The impact of nursing education on student retention and graduation rates
- The effectiveness of self-directed learning in nursing education
Healthcare Policy
Studying the impact of healthcare policy on the nursing profession and patient outcomes, including the role of nursing in healthcare reform efforts, is a crucial area of nursing research. Nurses can examine the policy’s effect on healthcare access, quality, and affordability and propose solutions to address policy gaps and challenges.
List of Nursing Research Topics: Healthcare Policy
- The impact of the affordable care act on the nursing profession
- Exploring healthcare informatics: evolution, challenges, and solutions
- The role of nursing in healthcare reform efforts
- The impact of medicare and Medicaid on nursing practice
- The impact of private insurance on nursing practice
- The impact of healthcare policies on nursing workforce development
- Combating workplace violence in nursing: the impact of policies, legislation, and organizational culture
- The role of nursing in healthcare policy decision-making
- The impact of healthcare policies on patient outcomes
- The role of nurses in implementing healthcare policies
- The implications of universal healthcare policies on nursing roles and responsibilities
- Evaluating the impact of health insurance reforms on nursing care delivery
- Strategies for nurses to influence healthcare policy decisions at the national and state levels
- The role of nursing in shaping policies related to patient rights and autonomy
- Assessing the influence of healthcare policy on nursing education and licensure requirements
- Evaluating the impact of nurse advocacy on shaping health policies at local and national levels
- Strategies for nurses to stay updated on changing healthcare policies and their implications
- The role of nursing in shaping policies related to electronic health records and patient privacy
- Assessing the implications of global health policies on nursing practices and education
- The influence of healthcare policies on the scope of practice for advanced practice nurses
- The impact of healthcare policies on nursing education and training
- The impact of healthcare policies on nurse staffing ratios
- The impact of healthcare policies on patient satisfaction
- Understanding the impact of the American Healthcare System Regulatory Acts
- The impact of healthcare policies on healthcare costs
- The impact of healthcare policies on healthcare disparities
- The role of nursing in advocating for healthcare policy changes
- The impact of healthcare policies on patient safety
- The impact of healthcare policies on nursing job satisfaction
- Understanding the US. Health Care Reform: necessity, challenges, and implementation
- The impact of healthcare policies on nursing burnout
- The impact of healthcare policies on nursing retention rates
- The impact of healthcare policies on nursing leadership
- The role of nursing in shaping healthcare policies
- The impact of healthcare policies on healthcare quality
- Workplace violence in healthcare: causes, regulations, and prevention strategies
- The impact of healthcare policies on nursing productivity
- The impact of healthcare policies on healthcare access
- The impact of healthcare policies on nursing workload
- The impact of healthcare policies on nursing autonomy
- The impact of healthcare policies on nursing scope of practice
- The impact of healthcare policies on nursing professional development
- The impact of healthcare policies on nursing research
- The role of nursing in developing healthcare policies
- Massachusetts Health Reform Act: striving for universal coverage and controlled costs
- The impact of healthcare policies on nursing career advancement
- The impact of healthcare policies on nursing licensure and certification
- The impact of healthcare policies on nursing accreditation
- The impact of healthcare policies on nursing ethics
- The impact of healthcare policies on nursing professionalism
- The role of nursing in healthcare policy implementation and evaluation
- The impact of healthcare policies on nursing informatics
- The impact of healthcare policies on nursing diversity and inclusion
- The impact of healthcare policies on nursing practice in rural areas
- The impact of healthcare policies on nursing practice in underserved communities
- The impact of healthcare policies on international nursing practice
The Importance of Research in Nursing
Research is the bedrock of nursing practice. It provides evidence-based knowledge that informs clinical decision-making, enhances patient outcomes, and advances the nursing profession. For nursing students, engaging in research activities offers several benefits:
- Enhanced Clinical Practice
Evidence-based research provides nurses with the latest knowledge and techniques to deliver optimal patient care. It bridges the gap between theoretical learning and practical application, ensuring that patients receive the most current and effective treatments.
- Professional Development
Engaging in research sharpens critical thinking and analytical skills. It fosters a culture of continuous learning, allowing nurses to stay updated with the ever-evolving medical field.
- Contribution to the Field
By conducting research, nurses contribute to the larger body of knowledge in healthcare. Their findings can lead to improvements in patient care, the development of new interventions, or changes in healthcare policies.
- Enhanced Patient Outcomes
Research equips nurses with the knowledge to educate patients, advocate for their needs, and make informed decisions. This ensures better health outcomes and improved patient satisfaction.
- Career Advancement
For those looking to advance in their careers, research can open doors to academic positions, leadership roles, or specialized fields within nursing.
Tips for Selecting a Suitable Research Topic
- Align with Interests
Choose a topic that genuinely interests you. This will keep you motivated throughout the research process.
- Relevance to Current Trends
Consider current trends and challenges in healthcare. Addressing contemporary issues can make your research more impactful.
- Feasibility
Ensure that you have access to the necessary resources and tools to conduct your research. This includes access to participants, equipment, and relevant literature.
It’s essential to choose a topic that’s neither too broad nor too narrow. A well-defined research question will guide your study and ensure it’s manageable.
- Seek Guidance
Don’t hesitate to seek advice from mentors, professors, or professionals in the field. Their insights can help refine your topic and provide valuable direction.
In conclusion, research is a vital component of the nursing profession, driving innovation and ensuring the best patient outcomes. For nursing students and professionals, engaging in research is not only a pathway to academic and career success but also a means to contribute meaningfully to the betterment of patient care.
📎 Related Articles
1. Key EBP Nursing Topics: Enhancing Patient Results through Evidence-Based Practice 2. Nursing Debate Topics: The Importance of Discussing and Debating Nursing Issues 3. Mental Health Nursing Research Topics: Inspiring Ideas for Students 4. Top Nursing Argumentative Essay Topics: Engage in Thought-Provoking Debates 5. Top Nursing Topics for Discussion: Engaging Conversations for Healthcare Professionals 6. Interesting Nursing Research Topics To Choose 7. Examples of Research Questions 8. Exploring Controversial Issues in Nursing: Key Topics and Examples 9. Pediatric Nursing Research Topics for Students: A Comprehensive Guide
Table of content
Crafted with Care:
Nursing Essays!
Precision, Passion, & Professionalism in Every Page.
- Practice Test
- Fundamentals of Nursing
- Anatomy and Physiology
- Medical and Surgical Nursing
- Perioperative Nursing
- Psychiatric Mental Health Nursing
- Maternal & Child Nursing
- Community Health Nursing
- Pathophysiology
- Nursing Research
- Study Guide and Strategies
- Nursing Videos
- Work for Us!
- Privacy Policy

- Nursing Notes
200+ Great Ideas of Nursing Research Topics to Get Started

Running out of topic ideas for your nursing research paper?
Stay on this page to find really cool and helpful lists of interesting research topics for your nursing dissertation or thesis.

What are Some Cool topics to Research?
Whenever students are asked to work on a research paper or present their thesis, the very first concern for them is choosing a unique, interesting, and research-worthy topic that makes their research significant and has enough future scope.
When it comes to finding a unique topic without working on something that’s already been done, most of the nursing and healthcare students struggle. A good research topic should be unique, relevant to current times, and have future scope as well. And you’ll find all three qualities in the topics mentioned below:
1. Primary Healthcare Nursing Research Topics
Primary healthcare refers to essential or basic health care service based on socially acceptable and scientifically sound methods and technology. Since it includes physical, social, emotional, and mental well-being, there are many topics for nursing scholars to explore:
- Strengthening primary healthcare system as the first line of referral system
- Introduction of home health nursing in the community set up
- Primary health care delivery system clinical pathways
- From home visits to home health care: strengthening primary health care delivery system
- Expanding the roles of community health nurses
- Millennial models of health care system
- Strengthening disease surveillance program in the community health set-up
- Home health care of debilitated patients
- Acceptance of evidence-based practice in the primary health care
- Strengthening continuity of care in the community / home health care post hospitalization
- Physical rehabilitation and occupational therapy in the community health care setting
2. Good Research Topics in Healthcare Management
Healthcare management is the management, administration, or oversight of healthcare systems, hospitals, public health systems, and other medical facilities. Since it comprises the overall management of all the work of the hospitals, it opens avenues for a lot of research work. Take, for example, the following:
- Evaluating who is responsible for failure in surgeries?
- Healthcare Contracts Limitations
- Medical Home Service
- Analysing nursing channels that nurses can use for becoming physicians?
- Gender Bias in Nursing Profession
- Starting Private Practice as a Nurse
- Medicare: Pros and Cons
- What are the most appropriate methods for increasing staff retention in a health care setting?
- Nursing Uniform Code Rules
- Role of nurses in enhancing a hospital quality improvement
- Legal Risks with Non-English Patients
- Medical Marijuana: Risk, Benefits, and Management Rules
- Shortage of Men in Healthcare
- Health tracking apps for continuity of care post discharge to home
- Telehealth: the impact of virtual care to urban and rural areas
- Strategic referral system to prevent tertiary hospital congestion
- Clinical pathways for referral system
- Drive-thru pharmacy
- Strenghtening the roles of social works and social workers in the health care team
- Case management approach in the healthcare delivery system
- Defining and application of Expected Length of Stay in patient management
- Impact of case managers in Expected Length of Stay and patient outcomes
- Redefining hospital cultures on bed rest versus mobilization
- Redefining hospital cultures on diet and food services
- Redefining hospital cultures on the assumption of the sick roles
- Strict implementation of Expected Length of Stay to prevent hospital congestion
- Roles of Case manager in the Clinical pathways
- Case Manager as a new nursing role an specialization
- Nurse navigator as a new form of nurse entrepreneurship
- Case management clinical pathway for smooth admission, patient flow and continuity of care after discharge
- Increase nursing specialization
- Internet savvy for healthcare providers
3. Nursing Research Topics about Pain Management
Pain management, in nursing, includes study of all the interventions nurses can make during their hospital hours – mainly to relieve a patient’s pain or ailments through medicinal interventions. Pain is complex, with many treatment options such as therapies, medicines, and also mind-body techniques. Nursing research scholars can research about the following topics:
- Pain management in children suffering from life-limiting illnesses: learning about the best practices
- Headache Treatment Protocol
- A closer look at hemophilia patient’s pain management
- Myofascial Pain Rehabilitation
- Labor and delivery: best practices for pain management
- Using Opioid for Rheumatoid Arthritis
- Fetal pain perception: analysis by medical experts
- Innovative Injection Use
- Therapeutic Injections: Cons & Pros
- Cognitive hypnotherapy application: how effective are they in pain management?
- Evaluating the effectiveness of Benson’s relaxation therapy as a pain management practice.
- Post-discharge pain-management strategies: evaluating their effectiveness in a health care setting?
- Phantom Pains Phenomenon
- Pain management in cancer patients: best practices according to expert nurses
- Spinal cord nerve injury related to chronic constipation
- Mobile pain unit
4. Pediatric Nursing Research Topics
In Pediatric nursing, the nursing staff is responsible for medical care of the children and neonates, and adolescents – mainly in a day-clinic or the in-patient setting. Though the main role of child health nursing is administering procedures and medicines to all children as per their prescribed nursing care plans, the research scholars can write papers on the following topics:
- Speech Disorders Therapy
- ADHD Causes & treatment
- Prevalence of misdiagnosis in child health or paediatric ward
- Vaccination & Autism
- Systematic review of range of child health nursing services in UK
- Antibiotic Resistance in Preschool Children
- Mental and Emotional health of children under 10
- Eating Disorders in Children
- Social Media Impact on Teenagers
- Seizures Causes in Infants
- Teething issues in children under 10
- Psychological Aspects of Infant Care
- Use of social media platforms in preparation and prevention of hospital phobia among pediatric groups
- Family engagement in the pediatric care by using hospital information system
- Safety and efficacy of telehealth for pediatric patients
What are the Current issues in Nursing?
Nursing is a high-pressure job. It demands patience, determination, and perseverance. As a high-pressure job, it gets quite challenging and leads to issues from time to time. Some of the examples being staff shortages, long working hours, workplace hazards, personal health, and workplace violence. All of these can be addressed in nursing research papers:
- Analysis of the registered nurse workforce and the relationship to work environments
- Transforming loss: A developing concept for nursing
- Nursing Staff Shortages
- Nursing Practitioners
- Meeting Patient Expectations: A challenge for nurses
- Biggest obstacles nurses face in their education and maintaining career alongside
- Workplace Violence and Hazards Nurses face
- Diversity in Healthcare
- Importance of Community Nursing
- Future of Nursing in the Digital Age
- What measure can a nurse take for helping a person with their eating disorder?
- Clinical Nurse Roles
- How can nurses help in treating patients who already know they don’t have a survival rate?
- Ethics and Homeless People Treatment
- Critical Care Nursing Management
- A nurse’s role in helping and assisting patients with chronic diseases?
- Nursing Theorists Works
- Remote Intensive Care Unit
- Stress Management Practice for Nurses Working in Night Shifts
- Between Career & Professional Service
- Preceptorship and training after distant education program and online learning
- Centralized infectious disease surveillance
- Centralized reporting of chronic diseases
- Patient become more educated: the pros and cons of social media
- Fake news and misinformation on health related issue with the rise of social media platforms
- BPO and call centers for medical procedures booking and admission to decongest emergency room
- Application of BPO in the quality assurance monitoring in documentation
What are Some of the Research Topic Ideas in Surgical Nursing?
- Moral distress among nurses in Surgical units
- Patient’s satisfaction and experience about care provided by nurses in the surgical units
- Organizational effects on patient satisfaction in surgical units
- Medical-Surgical nurses and their perceived leadership abilities as responders in patient deterioration events
- Role of Nurses in Surgical Wards
- Medical-surgical nursing: Critical thinking in client care
- Pain assessment and management in surgical nursing
- Understanding technology in contemporary surgical nursing
- Understanding Medical surgical nursing as an integrated approach
- Standardising fast-track surgical nursing care
- Mobilization team for the fast recovery of post-operative patients
- Use of telehealth for pre-operative preparations and elective surgical admissions to lessen hospital length of stay among surgical patients
- Continuity of care post surgery in the community health care
What have been some of the more important nursing research questions discussed in nursing class?
If you are here to find more important topics for your nursing dissertations, then scroll through this section for topics that are often discussed in nursing classes. Nursing research articles and topics change over time. However, we find these relevant to current times and challenges in healthcare:
1. Research topic ideas for Midwifery Nursing
Nurse-midwife, as a licensed healthcare professional, specialises in child birth and also women’s reproductive health. Apart from attending pregnant women during childbirth, they are responsible for several roles during emergencies, and pre and postnatal care. Hence, opening avenues for research topics such as:
- Role of nurses in improving patient safety during childbirth: Evidence from obstetric trauma
- Evaluate the impact of delayed umbilical cord clamping after child birth
- Maternal & Neonatal Practices in Rural Areas
- Emerging trends in obstetrical and midwifery nursing
- First Antenatal Appointment Analysis
- Limiting interventions during a low-risk labour
- Mental Illness & Post-natal Period
- Analysing the role of prenatal care in pregnant women
- Shift Study Midwives & Length
- Evaluating impact of AIDS and Hepatitis B in the pregnant women
- Self-Instruction Kits & Natal Safety
- Studying advanced trends in obstetrics and gynaecology
- Midwifery Continued Care
- Evaluating pros and cons of labouring in water
- Gestational Weight Gain Challenges
- Vitamin D’s role as a supplement during pregnancy
- Studying clinical reasoning integration into midwifery practice
- Obese Pregnant Women Safety Rules
- A decade after BEmONC and CEmONC
2. Health Promotion Research Topics
Health promotion mainly comes from behavioral social science which draws from the environmental, biological, psychological, medical, and physical sciences for promoting health and preventing diseases. For health promotion, the research topics include the following:
- Healthcare Dangers of Digital Age
- Benefits and Shortages of Telemedicine
- Healthy living and Preventive medicine for Senior Citizens
- Role of School Nurses
- Obstacles for Smoking cessation
- Healthy Eating & Sports
- Causes of Youth Inactivity
- Roles of Parents for Healthy Lifestyle of Children
- Obesity and Mental Stability
- Pharmacist Responsibility
- Social Media and Educational Strategies
- HealthBank as new form of medical insurance inside the hospital organization
- Collaboration of private health insurance company with public and private hospitals
3. Adult Research Topics for Nursing Students
As a nursing scholar, you can also write research papers on adult healthcare, disease prevention, and management. Take, for example, reasons behind anxiety disorders in adults. Find more topics in the list below:
- Nurses’ experiences with urinary catheter insertion: A qualitative focus group study
- Clinical Cardiology Innovations
- CV Imaging Process
- Migraine Case Example
- Bipolar Disorder Non-Chemical Practices
- Mental Health & Psychiatric Care in Adults
- Online nursing education program
- Self care in Nursing
- Home health care for longterm vented patients
- Clinical Instructor, Preceptorship, Educator and Professor as specialized field requiring licensure
- Specialization program in nursing education
4. Geriatric Care Nursing Journal Topics
Nurses working in Geriatric care and management are responsible for coordinating and planning care of the elderly people dealing with mental or physical disabilities. Some of the research work topic ideas for geriatric care include the following:
- Cerebrovascular Disease and Stroke in Elderly people
- Pain in elderly people: Assessment and Management
- Joint Disorders Study in Elderly Population
- Rapid Nutritional assessment in Elderly
- Alzheimer’s Disease
- Bladder Cancer Therapy
- Atrial Fibrillation Study
- Critical Care Requirements
- Cardiovascular Risk Reduction
- Geriatrics Ethics
- Restless Legs Syndrome
- Parkinson’s Disease Precautions
- Geriatric care clinical pathways of care: holistic approach
What are the recent nursing research paper topics?
If you’re facing the challenge of choosing a recent nursing research topic, we’ve got your back. Many nurses, including experienced and freshers, are faced with this challenge at some point. But there’s no need to panic. So, without further ado, let’s jump-start the list of most recent research topics for nursing students:
1. Women’s Health Nursing Research Topics
Research topics related to women’s health are always trending, relevant, and have future scope as well. Hence, these topics are still worth exploring and researching:
- Culture affects women’s health
- Substance Abuse and Addiction in Women
- Menopause Challenges
- Infertility Ethical Rules
- Ovarian Cancer and Ovarian Disorder Analysis
- Modern Neonatal Practices
- Pregnancy Prevention Measures
- Sepsis after labour
- Cosmetic Dermatology
- Cystic Fibroids
- Sleep Disorders in Women
- Reproductive Endocrinology
- Women’s Sexual Health Disorders
- HPV and Cervical Cancer
- Vaginal Atrophy Causes
- Sleep disturbances in Women
2. Mental Health Nursing Research Articles Topics
Research papers focusing on mental health are still one of the most read and referred papers. And there’s still more scope for research on topics such as:
- Evaluating the concept of Integrated Mental and Physical Health Care
- Psychiatric Nursing and Mental Health
- Possible skills required for Nurses in Mental health care setting
- Assessing the mental health of nurses
- Depression Causes
- Schizophrenia Diagnostics
- Alcohol Addiction Disorders
- Bipolar Disorder
- Studying the impact of PTSD in the Army Veterans
- Impact of Video Games on Teenage Aggression
- Stress Among Police Officers
- Psychiatric Patient Ethics
- Forbidden Substances: Prevention and Use
- Bioterrorism Medicine
- Physical Traumas & Recovery Methods
- Application of Nursing Case Management in Psychiatry
Nursing leaders have called for research focusing on which of the following topics?
If you’d like to take an expert’s opinion before choosing a topic for your nursing dissertation, this section will be helpful. Our list of best nursing research topics doesn’t end here. We’ve got here more interesting topics that are recommended by nursing leaders and experts. Take a look at some more relevant topics:
- Preterm Labor Dangers
- Labor and Delivery Management Practices
- Saving Mother & Child Challenges
- Abortion Care Ethical Side
- Adolescent Gynecology Education
- Antenatal Care Recommendations
- Hypertensive Disorders Causes
- Newborn Resuscitation Rules
- Caesarean Section Preparation
- Delivery Room Behavior Checklist
- Nurses play vital roles in healthcare. Why are they invisible in the media?
- Increasing nursing research capacity: The roles of nurse scientists within healthcare systems
- Microeconomics and macroeconomics for sources of hospital funds
- Diverting patients and funds to economical services
- Culture vs evidence based practice
- Social media influencer in health education dissemination
- Acceptance of evidence based practice in the hospital
- Impact of socio-cultural nursing to evidence-based practice
- Hindrances in the implementation of evidence-based practice
- Nursing faculty shortage and brain-drain
- Online continuing professional education and development
Academic Writing Service: Work Directly With the Experts
The are list of best nursing research paper topics ends here. However, we still have something helpful for you. Writing a dissertation or a nursing paper is time consuming – needless to mention the mental exertion. That explains why the majority of students prefer seeking research writing help.
Take, for example, apessay.com , a place where you can get in touch with registered experts who have successfully passed their competency examinations to provide academic writing service at an affordable rate. The three USPs include plagiarism free content, complete privacy and security standards to protect your personal info, and money-back guarantee.

What makes apessay.com academic writing service unique is you can work in direct cooperation with your preferred writer and consult them for everything – from choosing a relevant topic to revisions for final submission.
Feel free to get professional help from nursing research paper writing service which will take care of your nursing papers online.
Final Thoughts
Nursing research topics for a dissertation or thesis should not be difficult to find through the ideas suggestion above. Just make sure that you provide a twist (segment or expand the topic, perhaps) and come up with a unique topic for your paper.
During the initial stages of finalising a nursing research topic, you can struggle with a lot of choices or overwhelming information. However, when you start to consider a research topic’s limitations and scope, and outline your topic into a question, you’ll be able to get a better understanding of the topic you can manage in terms of workload.
We hope these nursing research topics mentioned above help you find that unique thesis statement or idea you’re looking for. In case you’re still having a tough time making a choice, leave us a comment or drop a mail, and we will direct you to better resources.
- https://www.journals.elsevier.com/applied-nursing-research/recent-articles
- https://www.syberscribe.com.au/blog/10-emerging-trends-healthcare-technology-2019-beyond/
- https://www.purdueglobal.edu/blog/nursing/top-10-nursing-trends/
- http://ojin.nursingworld.org/
RELATED ARTICLES MORE FROM AUTHOR
Evidence-based practice in nursing: beyond the scientific proof of care, nursing research definition: the importance and nurses roles.
It’s was very helpful for me
Disparities in enumeration of staff nurses in developing countries are not researched on.
LEAVE A REPLY Cancel reply
Save my name, email, and website in this browser for the next time I comment.

Best Evidence-Based Practice (EBP) Nursing Research Topics and Ideas

We have already explored as much as there is regarding evidence-based nursing in our comprehensive EBP paper-writing guide . A time comes in your nursing school journey, either at basic (ADN, LPN, or BSN) or advanced levels (MSN, DNP, or PhD), when you are required to select a suitable evidence-based practice nursing research topic, research, and write an evidence-based nursing paper, report, or white paper. The process for selecting the topic is more or less the same as when selecting a nursing dissertation topic or topic for a nursing capstone .
You have to go through the instructions, consider an area of nursing specialization that interests you, do some thorough research, reading, and analysis, come up with a few topics, and eliminate and remain with the most suitable topic for your EBP nursing paper. You can locate good EBP project ideas from course materials (readings, handouts, PPTs, and class notes), online blogs and websites (like NurseMyGrade), nursing textbooks, nursing journals and articles, and other online resources.
General, Current, and Latest Evidence-Based Nursing Topics
- Effects of evidence-based practice on the quality and safety of patients
- Attitudes and readiness for Evidence-Based Nursing Practice among newly hired nurses
- Engaging advanced practice nurses in evidence-based practice through an e-monitoring program
- Effectiveness of EBP practice guidelines in preventing adverse events in clinical settings
- The attitudes of nurses toward adhering to clinical guidelines regarding the management of various conditions
- Prevention of deep vein thrombosis (DVT) among surgical patients
- Effectiveness of warming interventions for women undergoing Cesarean Section
- Strategies for managing second-stage labor
- Effects of gum chewing and early mobilization on intestinal mobility after cesarean birth
- Therapeutic use of music in maternity wards post-cesarean section
- Strategies for preparing women for unplanned Cesarean birth
- Effectiveness of hydrotherapy during labor
- Strategies to implement skin-to-skin contact in the OR following Cesarean birth
- Benefits of the EBP Organizational culture and readiness scale
- Transferability, reach, and impact of the EBP Questionnaire
- Barriers and facilitators influencing the implementation of EBP in clinical settings
- Challenges to implementing EBP in healthcare systems
- The beliefs and competencies of medical-surgery nurses on EBP
- Effects of EBP courses on MSN and DNP students' attitudes and beliefs on EBP
- The impacts of gamification on EBP training among nursing students
- Strategies to promote evidence-based nursing practice among nursing students
- The link between knowledge of EBP and nurse job satisfaction
- Impacts of nursing ethics on evidence-based practice
- Strategies to address the implementation gap between practice, research, and knowledge in nursing
- Using social media to promote the dissemination of evidence-based practice
- Strategies for implementing and translating evidence-based practice
- Benefits of frequently training nursing staff on evidence-based practice
- Role of evidence-based practice in modeling professional nursing practice
- Strategies for enhancing utility and understanding of evidence-based practice during undergraduate nursing education
- Knowledge, attitude, beliefs, and use of evidence-based practice among registered pediatric nurses
- Improving the readiness of evidence-based practice in critical care units
- Strategies for improving evidence-based practice among registered nurses (RNs)
- Best strategies for assessing compliance to EBP guidelines for VAP prevention among ICU nurses
- Impacts of EBP guidelines on clinical decision-making
- Challenges in communicating research evidence and translating it to practice
- Effectiveness of SBAR Tool Implementation to advanced communication and collaboration in clinical settings
- Knowledge of EBP and the confidence of newly recruited nurses
- Role of evidence-based practice guidelines in maintaining competence among mental health nurses
- Impacts of teaching advanced evidence-based practice research in doctoral nursing programs
Evidence-Based Topics for Anesthesia
- Primary concerns in the process of extubation in the anesthesia settings
- Perceptions and attitudes of anesthesia professionals on digital anesthesia information management system
- Benefits of nurse anesthetist perioperative dialog
- Causes of high attrition rates and turnover among nurse anesthetists
- Perceptions and attitudes of nurses on automatic dispensing cabinets
- Strategies for translating evidence-based research into anesthesia practice
- Addressing challenges associated with anesthesia in clinical settings
- Causes and solutions to anesthesia-associated mortality and morbidity
- An evidence-based approach to airway management via anesthesia administration
- Attitudes, knowledge, skills, and use of anesthesia teams toward EBP practice in clinical settings
- Why anesthetists are hesitant to implement ERAS guidelines
Related read: How to complete Shadow Health Assessments .
Cardiovascular and Respiratory Evidence-Based Topics
- Improving the quality of cardiovascular care through evidence-based practice
- Addressing social determinants of health as a means of addressing cardiovascular diseases
- Effects of listening to music during cardiac rehabilitation on clinical outcomes
- Effectiveness of physical activity on cardiovascular health
- Role of physical therapists in the management of venous thromboembolism
- Effectiveness of aerobic exercise training in improving aerobic capacity after heart transplant
- Impacts of guarding on the outcomes of the 6-minute walk test
- Role of Mitsungumin 53 in cardiovascular diseases (CVD)
- Effects of autophagy on the cardiovascular system
- The ethics of using embryonic stem cells in cardiovascular research
- Use of telehealth in early detection of anxiety and depression in post-coronary patients
- Effectiveness of indoor allergen reduction in the management of asthma
- Non-invasive technologies for diagnosing coronary artery disease in women
- Impacts of smoking on the lungs of a fetus
- Strategies to address obstructive sleep apnea and cardiovascular disease
- The link between consuming fatty animal meat and cardiovascular health
- Benefits of prone positioning for patients with ARDS
- Response of COPD to prophylactic antibiotics
- Evidence-based nursing strategies for the prevention of contrast-induced acute kidney injury
- Impacts of home monitoring on COPD patients
Complementary and Alternative Medicine Evidence-Based Topics
- The link between probiotics use and diarrhea
- The effectiveness of vitamin C in the prevention of complex regional pain syndrome following wrist fractures
- The link between using essential oils and hypertension
- Effectiveness of cranberry products for the treatment of UTIs
- Effectiveness of botulism toxin in the treatment of restless legs syndrome
- Using therapeutic honey in tropical wound management
- Impacts of scalp cooling on alopecia among cancer patients
- Effects of spiritual beliefs on type 2 diabetes mellitus patients
- Effects of aromatherapy in the management of depression and anxiety
- Non-pharmacologic interventions for treatment-resistant depression among adolescents
Nursing Ethics Evidence-Based Topics
- Effects of abandonment on nursing staff shortage
- Effects of negligence on patient outcomes
- AI ethics awareness, attitudes, and beliefs, and the behavioral intentions of nursing students
- Attitudes and perspectives of nursing faculty on noncompliance with ethics in nursing academic environments
- Application of Nightingale's professionalism among student nurses
- Influence of nursing ethics on clinical decision-making
- Perceptions and awareness of student nurses on social justice in the healthcare system
- Benefits of increased ethical competency of nurses in clinical settings
- Ethical problems of clinical nursing practice
- Factors influencing professionalism in nursing among Registered Nurses
- Information literacy and ethical decision-making among nurses
- The link between clinical dishonesty and perceived clinical stress among nursing students
- Strategies to help nurses handle compassion fatigue
- Ethical perspectives of evidence-based practice
- Influence of laws and Legislation on evidence-based practice
- Moral distress among Registered Nurses
- Barriers and facilitators of addressing nursing research ethics
- Role of nursing ethics in the implementation of evidence-based practice
Family Practice Evidence-Based Topics
- The significance of genetic counseling in diabetes prevention
- Challenges for contraception for women with diabetes
- Management of autism in children
- Diagnosis, treatment, and management of psoriasis
- Using a gluten-free diet to improve outcomes in patients with psoriasis
- The link between psoriasis and cardiovascular diseases
- Impacts of nutritional counseling on the BMI of patients
- Using Metformin over Sulfonylurea for initial treatment of gestational diabetes
- Best ways to diagnose menopause in perimenopausal women
- Dinoprostone vs. vaginal misoprostol in labor induction: which is better?
- Effectiveness of using narcotics to treat patients with chronic daily headaches
- Vitamins and cognitive decline in Alzheimer's disease
- The link between regular family dinners and obesity in adolescent patients
- Is the Mediterranean diet better for bone health?
- Benefits of self-managed diabetes programs
- Is acupuncture effective in the treatment of allergic rhinitis?
- The link between antibiotic use and acute sinusitis
- Effectiveness of Flu vaccine on prevention of community-acquired pneumonia
- The link between male obesity and infertility
- Lower back pains and NSAIDS
- Seasonal Nasal Irrigation and Seasonal Allergic Reactions: Best management strategies
- Effectiveness of abortive treatment for acute migraine
- Effectiveness of combination treatment for hepatitis C
- Benefits of tailored education for melanoma management
- Genetic testing and obesity
- Treatment and management of atopic dermatitis
Nursing Forensics Evidence-Based Topics
- Strategies to document injuries from domestic violence abuse by forensic nurses
- Perceptions of forensic nurses on victim counseling before post-domestic violence cases
- Stress management and coping strategies in prison settings
- Mental health as a risk factor for sexual assault
- Barriers and challenges to implementing remote sexual assault nurse examiner programs
- Limit setting and de-escalation in forensic mental health units
- The risk factors for domestic minor sex trafficking in the USA
- Benefits of sexual assault nurse examiners practicing trauma-informed care
- Ethical issues involved during forensic nursing investigations
- Strategies for preparing victims of sexual assault to be witnesses in courts of law
- Role of forensic nurses in combating human and sexual trafficking
- The link between sexual assault and suicide
- Strategies to handle compassion fatigue among forensic nurses
- Strategies for emergency contraception administration among the SANE and non-SANE medical providers
- Strategies forensic nurses use to resolve difficulties in supporting offenders with mental health disorders
- Role of forensic nurses in addressing challenges for children in foster care
- Forensic nursing interventions for patients with personality disorders
- Application of telehealth among sexual assault forensic examiners
- Strategies for handling children facing maltreatment from parents
- Interprofessional collaboration to optimize trauma-informed care
- Role of pediatric forensics in clinical settings
- Role of forensic nurses in abortion investigations
- Steps and evidence-based methods for screening children for neglect or abuse
- Strategies for solving burnout among forensic nurses
- Role of forensic nurses in death investigations
- Attitudes of Sexual Assault Nurse Examiners (SANE) toward sexual assault victims
- Methods for promoting resilience, competence, and quality of life of Sexual Assault Nurse Examiners
- Role of correctional nurses in advocating for pregnant women's rights in prison
- An evidence-based approach to suicide risk assessment following sexual assault
Gastroenterology Evidence-Based Topics
- The use of probiotics to treat and manage irritable bowel syndrome (IBS)
- Using behavioral therapy adjunct to drug therapy in the management of urinary incontinence
- Pharmacological strategies for the management of Crohn's disease
- Complementary alternative medicine approaches to the management of Gastroesophageal Reflux Disease (GERD)
- Intermittent fasting among obese women and the management of pylori
- Homemade solutions for constipation among pregnant women
Geriatrics or Long-Term Care Evidence-Based Topics
- The effectiveness of the North Dakota Association of director of Nursing Administration (NADONA) /Long-Term Care standards of Practice in managing long-term care facilities
- Strategies to encourage elderly people to age in place
- Methods to improve drug adherence among elderly patients with Alzheimer's disease
- Methods for managing polypharmacy among elderly adults
- Design strategies to address falls for patients aging in place
- Use of technology to address the challenges of elderly adults who choose to age in place
- Benefits of music therapy for patients with Multiple Sclerosis
- Strategies for addressing pressure ulcers among the elderly
- Benefits of teaching self-care practices to elderly patients with long-term in-dwelling catheter
- Using stories to entertain and give hope to elderly patients in long-term care facilities
- Multifactorial approach towards management of falls in long-term care facilities
Hospital-Acquired Infections Evidence-Based Topics
- Effectiveness of hand hygiene in reducing hospital-acquired infections
- Strategies to prevent blood contamination and infection during transfusion
- The value of Central Line-Associated Bloodstream Infection Bundle Compliance in preventing CLABSI
- Impacts of implementing central nervous catheter bundle in reducing central line-associated bloodstream infections (CLABSI)
- The knowledge and attitudes of nurses on evidence-based guidelines for the prevention of surgical site infections
- Benefits of governments supporting nursing homes in infection management
- How effective are leadership rounds in reducing healthcare-associated infections?
- Knowledge, beliefs, and attitude of newly graduated nurses on infection prevention and control
- Evidence-based strategies to prevent ventilator-associated pneumonia
- Perceptions of NICU nurses regarding measures to prevent HAIs
- The role of chlorhexidine gluconate bathing in preventing HAIs
- Importance of communication networks in the management of infections in ICUs
- Strategies to reduce catheter-associated urinary tract infections (CAUTIs)
- The perspectives and experiences of patients on HAIs
- Nurse-led quality improvement interventions to reduce hospital-acquired infections in the NICU
- Using a multimodal approach to institute hand hygiene
- The correlation between hospital length of stay and acquiring infections
- Evidence-based strategies to prevent nosocomial infections in clinical settings
- Value of e-learning for preventing healthcare-associated infections
- Impacts of nurse burnout and shortage on HAIs
- Core components of an infection prevention and control program for a nursing home
- Leadership skills of the APRNs and prevention of HAIs
- The motivations of healthcare workers to reduce HAIs
- Hand hygiene knowledge and beliefs among newly recruited nurses
- Impacts of hospital design on HAIs
- Overcrowding in the ER and hospital-acquired infections
- Effects of training on nurses' knowledge and skills in indwelling urinary catheters in preventing CAUTIs
- Low rates of Influenza vaccination among nurses and HAIs
- Role of environmental cleaning in the control of HAIs
- Green cleaning and HAIs
- Compliance with Chlorhexidine wipes to prevent Hospital-acquired infections
- The knowledge of nurses of the WHO Five Moments of Hand hygiene and HAIs in the Operating rooms
Nursing Education Evidence-Based Topics
- Effectiveness of situated e-learning on medical and nursing education
- Benefits of cultural competence training among nurses on the patient satisfaction
- Experiences and attitudes of student nurses on formal preceptor programs
- The effectiveness of using virtual and augmented reality in nursing education
- Strategies to attract, train, and retain student nurses until retirement
- The application of gamification in nursing training
- Should nurses be taught basic coding concepts?
- Inclusion of LGBTQ student nurses in clinical settings
- The use of social media to facilitate learning among nursing students
- Benefits of introducing students to reflective nursing practice
- Benefits of e-learning for nursing education
- Online nursing programs as a means to prepare nurses for leadership roles
- The nurse training pipeline is an essential aspect of addressing nurse shortages
- Discrimination among nurse student acceptance of some programs/nursing schools
- Factors affecting the progress of nursing students in the USA
- Should the nursing career be ubiquitous globally?
- Student nurses should join professional organizations that advocate for their rights
- Steps to improve collaboration and teamwork among nurse students
Pain Management Evidence-Based Topics
- Effectiveness of ERAS in postoperative pain management
- Non-pharmacological methods and perceived barriers in pain management by nurses
- Psychological and behavioral pain management strategies in pediatric oncology departments
- Mindfulness mediation as a strategy for chronic pain management
- Impacts of relaxation techniques for pain management during labor
- The efficacy of cannabis-based medicines for pain management
- Use of music therapy during labor
- Impacts of massage therapy on cancer pain management
- The effectiveness of craniosacral therapy for chronic pain management
- Effectiveness of manual therapy vs. exercise therapy in the management of adult neck-pain
- Non-pharmacological pain management approaches for cancer patients
- Music-induced analgesia in chronic pain management
- The effectiveness of transcutaneous electric nerve stimulation for cancer pain
- The efficacy of acupuncture in the management of postoperative pain
- The application of cannabinoids in pain management
- Acupressure for pain management during labor
Pediatrics Evidence-Based Topics
- Practical strategies for preventing failure to rescue obstetric patients
- Effectiveness of neonatal pain management via oral sucrose
- Benefits of nutritional assessment and intervention in a pediatric oncology unit
- Strategies to manage inguinal hernias in children
- Impacts of clinical settings appearance on the anxiety of kids in cancer care facilities
- Evidence-based strategies for the management of the acute phase of Kawasaki disease
- Strategies to address diabetes ketoacidosis among pediatric patients
- The use of virtual reality in managing anxiety among pediatric patients
- The use of probiotics in the prevention of diarrhea among children
- The efficiency of using gastronomy tubes among pediatric patients
- Best strategies to treat and manage infant colic
- Management of ventilator-associated pneumonia (VAP) among neonates and children
- Strategies parents can use to cope during acute pediatric hospitalizations
- Strategies to address childhood constipation
- Strategies to prevent SIDS during breastfeeding
- The safety of corticosteroids in young children with acute respiratory conditions
- Management of hospital-acquired venous thromboembolism in pediatric patients
- Efficacy of insertion and maintenance bundles in preventing central-line associated bloodstream infections in critically ill pediatric patients
- Prevalent and management strategies for burnout among pediatric nurses
- The efficacy of magnesium supplementation in addressing postoperative arrhythmias after cardiopulmonary bypass among pediatric patients
As we come to the End of this Article '
You can select a topic among the ones we have listed above or get inspired to select a topic whose research direction interests you. If you need unique topics, kindly place a one-page order and get 3-4 topics researched, suggested, and listed by an expert based on your preferences.
Nobody understands evidence-based nursing practice more than our online nursing writers. Through the years, we have helped students at the ADN, BSN, MSN, DNP, and Ph.D. nursing levels access unique and exciting evidence-based topics. What's more, if you need help writing an evidence-based practice paper (report, term paper, change project, thesis, research paper, or dissertation), our astute writers can help you. You will get a 100% original, well-formatted (in APA or Harvard format), and edited paper that meets your rubric requirements.
Struggling with
Related Articles
Nursing Student's Ultimate Guide to Writing a Nursing Care Plan

How to Fight Nursing Student Dismissal and Win
Nursing Diagnosis - An Ultimate Guide for Nursing Students
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
- NLN Certification
- Assessment Services
- CNEA Accreditation
- NLN Foundation
- Mission & Core Values
- History & Archives
- Board of Governors
- Senior Management
- NLN Nominations
- Career Center

Research Priorities in Nursing Education

The NLN Research Priorities in Nursing Education 2024-2027 continue to support nurse researchers who undertake research that contributes to the science of nursing education. The 2024-2027 priorities create a roadmap that connects the science of nursing education with the science of learning to develop an evidentiary base to guide educators in the preparation of nurses whose practice promotes and maintains wellness and care throughout the lifespan.
The 2024-2027 research priorities include:
- Build the science of nursing education through the generation and translation of innovative teaching and learning strategies
- Build a diverse nurse faculty capacity and enhance teaching practice
- Create teaching and learning environments that enhance the diversity, equity, and inclusivity for student learning and progression across all academic programs
The ultimate goal of these research endeavors is to develop the science of nursing education that will be used to prepare practitioners who deliver excellent health care. To accomplish this goal, robust research methodologies are needed that focus on the generation and translation of evidence in the areas of innovative teaching and learning strategies, faculty workforce capacity and teaching practice, and student academic progression and success.
NLN Research Priorities in Nursing Education 2024 - 2027
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on the Future of Nursing 2020–2030; Flaubert JL, Le Menestrel S, Williams DR, et al., editors. The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. Washington (DC): National Academies Press (US); 2021 May 11.

The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity.
- Hardcopy Version at National Academies Press
7 Educating Nurses for the Future
You cannot transmit wisdom and insight to another person. The seed is already there. A good teacher touches the seed, allowing it to wake up, to sprout, and to grow. —Thich Nhat Hanh, global spiritual leader and peace activist
By 2030, the nursing profession will look vastly different and will be caring for a changing America. Nursing school curricula need to be strengthened so that nurses are prepared to help promote health equity, reduce health disparities, and improve the health and well-being of everyone. Nursing schools will need to ensure that nurses are prepared to understand and identify the social determinants of health, have expanded learning experiences in the community so they can work with different people with varied life experiences and cultural values, have the competencies to care for an aging and more diverse population, can engage in new professional roles, are nimble enough to adapt continually to new technologies, and can lead and collaborate with other professions and sectors. And nursing students—and faculty—not only need to reflect the diversity of the population, but also need to help break down barriers of structural racism prevalent in today’s nursing education.
Throughout the coming decade, it will be essential for nursing education to evolve rapidly in order to prepare nurses who can meet the challenges articulated in this report with respect to addressing social determinants of health (SDOH), improving population health, and promoting health equity. Nurses will need to be educated to care for a population that is both aging, with declining mental and physical health, and becoming increasingly diverse; to engage in new professional roles; to adapt to new technologies; to function in a changing policy environment; and to lead and collaborate with professionals from other sectors and professions. As part of their education, aspiring nurses will need new competencies and different types of learning experiences to be prepared for these new and expanded roles. Also essential will be recruiting and supporting diverse students and faculty to create a workforce that more closely resembles the population it serves. Given the growing focus on SDOH, population health, and health equity within the public health and health care systems, the need to make these changes to nursing education is clear. Nurses’ close connection with patients and communities, their role as advocates for well-being, and their placement across multiple types of settings make them well positioned to address SDOH and health equity. For future nurses to capitalize on this potential, however, SDOH and equity must be integrated throughout their educational experience to build the competencies and skills they will need.
The committee’s charge included examining whether nursing education provides the competencies and skills nurses will need—the capacity to acquire new competencies, to work outside of acute care settings, and to lead efforts to build a culture of health and health equity—as they enter the workforce and throughout their careers. A thorough review of the current status and future needs of nursing education in the United States was beyond the scope of this study, but in this chapter, the committee identifies priorities for the content and nature of the education nurses will need to meet the challenge of addressing SDOH, advancing health equity, and improving population health. Nursing education is a lifelong pursuit; nurses gain knowledge and skills in the classroom, at work, through continuing professional development, and through other formal and informal mechanisms ( IOM, 2016b ). While the scope of this study precluded a thorough discussion of learning outside of nursing education programs, readers can find further discussion of lifelong learning in A Framework for Educating Health Professionals to Address the Social Determinants of Health ( IOM, 2016b ), Redesigning Continuing Education in the Health Professions ( IOM, 2010 ), and Exploring a Business Case for High-Value Continuing Professional Development: Proceedings of a Workshop ( NASEM, 2018a ).
To change nursing education meaningfully so as to produce nurses who are prepared to meet the above challenges in the decade ahead will require changes in four areas: what is taught, how it is taught, who the students are, and who teaches them. This chapter opens with a description of the nursing education system and the need for integrating equity into education, and then examines each of these four areas in turn:
- domains and competencies for equity,
- expanded learning opportunities,
- recruitment of and support for diverse prospective nurses, and
- strengthening and diversification of the nursing faculty.
In addition to changes in these specific areas, there is a need for a fundamental shift in the idea of what constitutes a “quality” nursing education. Currently, National Council Licensure Examination (NCLEX) pass rates are used as the primary indicator of quality, along with graduation and employment rates ( NCSBN, 2020a ; O’Lynn, 2017 ). This narrow focus on pass rates has been criticized for diverting time and attention away from other goals, such as developing student competencies, investing in faculty, and implementing innovative curricula ( Giddens, 2009 ; O’Lynn, 2017 ; Taylor et al., 2014 ). In addition, the NCLEX is heavily focused on acute care rather than on such areas of nursing as primary care, disease prevention, SDOH, and health equity ( NCSBN, 2019 ). In response to such concerns about the NCLEX, the National Council of State Boards of Nursing (NCSBN) conducted a study to identify additional quality indicators for nursing education programs; indicators were identified in the areas of administration, program director, faculty, students, curriculum and clinical experiences, and teaching and learning resources ( Spector et al., 2020 ). To realize the committee’s vision for nursing education, it will be necessary for nursing schools, accreditors, employers, and students to look beyond NCLEX pass rates and include these types of indicators in the assessment of a quality nursing education.
- OVERVIEW OF NURSING EDUCATION
Nurses are educated at universities, colleges, hospitals, and community colleges and can follow a number of educational pathways. Table 7-1 identifies the various degrees that nurses can hold, and describes the programs that lead to each degree and the usual amount of time required to complete them. In 2019, there were more than 200,000 graduates from baccalaureate, master’s, and doctoral nursing programs in the United States and its territories, including 144,659 who received a baccalaureate degree ( AACN, 2020a ) (see Table 7-2 ).
Pathways in Nursing Education.
Number of Graduates from Nursing Programs in the United States and Territories, 2019.
Nursing programs are nationally accredited by the Accreditation Commission for Education in Nursing (ACEN); the Commission on Collegiate Nursing Education (CCNE); the Commission for Nursing Education and Accreditation (CNEA); and other bodies focused on specialty areas of nursing, such as midwifery. Graduating registered nurses (RNs) seek licensure as nurses through state boards, and take examinations administered by the NCSBN as graduates with their first professional degree and then as specialists with certification exams offered through specialty organizations. These bodies set minimum standards for nursing programs and establish criteria for certification and licensing, faculty qualifications, course offerings, and other features of nursing programs ( Gaines, n.d. ).
The Need for Nursing Education on Social Determinants of Health and Health Equity
A report of the Institute of Medicine (IOM) from nearly two decades ago asserts that all health professionals, including nurses, need to “understand determinants of health, the link between medical care and healthy populations, and professional responsibilities” ( IOM, 2003 , p. 209). The literature is replete with calls for all nurses to understand concepts associated with health equity, such as disparities, culturally competent care, equity, and social justice. For example, Morton and colleagues (2019) identify essential content to prepare nurses for community-based practice, including SDOH, health disparities/health equity, cultural competency, epidemiology, community leadership, and the development of enhanced skills in community-based settings. O’Connor and colleagues (2019) call for an inclusive educational environment that prepares nurses to care for diverse patient populations, including the study of racism’s impacts on health from the genetic to the societal level, systems of marginalization and oppression, critical self-reflection, and preparation for lifelong learning in these areas. And Thornton and Persaud (2018) state that the content of nursing education should include instruction in cultural sensitivity and culturally competent care, trauma-informed care and motivational interviewing, screening for social needs, and referring for services. These calls align with the Health Resources and Services Administration’s (HRSA’s) most recent strategic plan, which prioritizes the development of a health care workforce that is able to address current and emerging needs for improving equity and access ( HRSA, 2019 ). Additionally, recommendations of the National Advisory Council on Nurse Education and Practice (NACNEP) (2016) include that population health concepts be incorporated into nursing curriculum and that undergraduate programs create partnerships with HRSA, the U.S. Department of Veterans Affairs (VA), and the Indian Health Service (IHS), agencies that serve rural and frontier areas, to increase students’ exposure to different competencies, experiences, and environments.
In concert with these perspectives and recommendations, nursing organizations have developed guidelines for how nursing education should prepare nurses to work on health equity issues and address SDOH. In 2019, the National League for Nursing (NLN) issued a Vision for Integration of the Social Determinants of Health into Nursing Education Curricula , which describes the importance of SDOH to the mission of nursing and makes recommendations for how SDOH should be integrated into nursing education (see Box 7-1 ).
National League for Nursing’s (NLN’s) Vision for Integration of the Social Determinants of Health into Nursing Education Curricula.
As described in Chapter 9 , the American Association of Colleges of Nursing’s (AACN’s) Essentials 1 provides an outline for the necessary curriculum content and expected competencies for graduates of baccalaureate, master’s, and doctor of nursing practice (DNP) programs. Essentials identifies “Clinical Prevention and Population Health” as one of the nine essential areas of baccalaureate nursing education. Among other areas of focus, Essentials calls for baccalaureate programs to prepare nurses to
- collaborate with other health care professionals and patients to provide spiritually and culturally appropriate health promotion and disease and injury prevention interventions;
- assess the health, health care, and emergency preparedness needs of a defined population;
- collaborate with others to develop an intervention plan that takes into account determinants of health, available resources, and the range of activities that contribute to health and the prevention of illness, injury, disability, and premature death;
- participate in clinical prevention and population-focused interventions with attention to effectiveness, efficiency, cost-effectiveness, and equity; and
- advocate for social justice, including a commitment to the health of vulnerable populations and the elimination of health disparities.
Curriculum content and expected competencies laid out in Essentials for master’s- and DNP-level nursing education also address SDOH, disparities, equity, and social justice ( AACN, 2006 , 2011 ). While Essentials only guides baccalaureate, master’s, and DNP programs, the document’s emphasis on health equity and SDOH demonstrates the importance of these topics to the nursing profession as a whole.
As of 2020, AACN has been shifting toward a competency-based curriculum. As part of this effort, AACN published a draft update to Essentials that identifies 10 domains for nursing education: knowledge for nursing practice; person-centered care; population health; scholarship for nursing discipline; quality and safety; interprofessional partnerships; systems-based practice; informatics and health care technologies; professionalism; and personal, professional, and leadership development. Within these 10 domains are specific competencies that AACN believes are essential for nursing practice ( AACN, 2020b ), including
- engage in effective partnerships,
- advance equitable population health policy,
- demonstrate advocacy strategies,
- use information and communication technologies and informatics processes to deliver safe nursing care to diverse populations in a variety of settings, and
- use knowledge of nursing and other professions to address the health care needs of patients and populations.
Nurses themselves have also indicated the need for more education and training on these topics. The 2018 National Sample Survey of Registered Nurses (NSSRN) asked the question, “As of December 31, 2017, what training topics would have helped you do your job better?” Figure 7-1 shows the percentage of six different training topics that RNs said would help them do their job better. Overall, RNs working in schools, public health, community health, and emergency and urgent care were more likely than RNs working in all other employment settings listed in Figure 7-1 to indicate that they could have done their job better if they had received training in SDOH, population health, working in underserved communities, caring for individuals with complex health and social needs, and especially mental health. These results could reflect RNs encountering increasingly complex individuals and populations, rising numbers of visits and caseloads, the fact that the RNs working in these settings frequently provide care for people facing multiple social risk factors that harm their health and well-being, or inadequacy of the training in these areas that RNs had received. RNs—particularly those working in informatics, health care management and administration, and education—also indicated that training in value-based care would have been helpful. Additionally, RNs who had graduated after 2010 were more likely than those who had graduated before then to indicate that they could have done their job better with training across all of these topics.
Training topics that would have helped registered nurses do their jobs better, by type of work performed and graduation from their nursing program, 2018. SOURCE: Calculations based on the 2018 National Sample Survey of Registered Nurses (HRSA, 2020). (more...)
Nurse practitioners (NPs) have also indicated the need for more training in SDOH. In response to the 2018 NSSRN question described above, NPs working in public health and community health, emergency and urgent care, education, and long-term care reported that they could have done their job better if they had received training in SDOH, mental health, working in underserved communities, and providing care for medically complex/special needs. Across all types of practice settings, one-third felt that training in mental health issues would have helped them do their job better, while very few NPs indicated that training in value-based care would have been helpful. Additionally, NPs who had graduated since 2010 were more likely than those who had graduated before then to indicate that they would have benefited from training in these topics. Figure 7-2 shows the percentage of six different training topics that NPs mentioned would have helped them do their job better.
Training topics that would have helped nurse practitioners do their jobs better, by type of work performed and graduation from their nursing education program, 2018. SOURCE: Calculations based on the 2018 National Sample Survey of Registered Nurses (HRSA, (more...)
The Need for Integration of Social Determinants of Health and Health Equity into Nursing Education
Despite guidelines from both the American Association of Colleges of Nursing (AACN) and the National League for Nursing (NLN) and numerous calls for including equity, population health, and SDOH in nursing education, SDOH and related concepts are not currently well integrated into undergraduate and graduate nursing education. Nor has the degree to which nurses are prepared and educated in these areas been studied systematically ( NACNEP, 2019 ; Tilden et al., 2018 ). The committee was unable to locate a central repository of information about the coursework and other educational experiences available to nursing students across types of programs and institutions, or any other source of systematic analysis of nursing curricula. This lack of information about nursing preparation programs limits the conclusions that can be drawn about them. Thus, the discussion in this chapter is based on the assumption that some nursing programs are likely already pursuing many of the goals identified herein, but that this critically important content is not yet standard practice throughout nursing education.
One way to explore whether and how health equity and related concepts are currently integrated into nursing education is to look at accreditation standards. While the standards do not detail every specific topic to be covered in nursing curricula, they do set expectations, convey priorities, and identify important areas of study. For example, the accreditation standards of the CCNE state that advanced practice registered nurse (APRN) programs must include study of advanced physiology, advanced health assessment, and advanced pharmacology ( CCNE, 2018 ). Accreditation standards could be used to prioritize the inclusion of health equity and SDOH in nursing curriculum; however, this is not currently the case. The CCNE standards state that accredited programs must incorporate the AACN Essentials into their curricula, and while these standards do not specifically mention equity, SDOH, or other relevant concepts ( CCNE, 2018 ), that is expected to change to correspond with the updates to the Essentials described previously (see Box 7-1 ). CNEA’s accreditation standards likewise include no mention of population health, SDOH, or health equity ( NLN, 2016 ), although a more recent document from NLN makes a strong case for the integration of SDOH into nursing education curricula ( NLN, 2019 ). ACEN’s associate’s and baccalaureate standards call for inclusion of “cultural, ethnic, and socially diverse concepts” in the curriculum; the master’s and doctoral standards require that curriculum be “designed so that graduates of the program are able to practice in a culturally and ethnically diverse global society,” but do not address health equity, population health, or SDOH.
Another approach for examining the inclusion of these concepts in nursing education is to look at exemplar programs. As part of the Future of Nursing: Campaign for Action, the Robert Wood Johnson Foundation commissioned a study of best practices in nursing education to support population health ( Campaign for Action, 2019b ). That report notes that although many nursing programs reported including population health content in their curriculum, few incorporated the topic substantially. However, the report also identifies exemplars of programs with promising population health models. These exemplars include Oregon Health & Science University, which incorporates population health throughout the curriculum as a key competency; Rush University, which incorporates cultural competence throughout the curriculum; and Thomas Jefferson University, which offers courses in health promotion, population health, health disparities, and SDOH. NACNEP has also examined exemplars of nursing programs that incorporate health equity and SDOH into their curricula ( NACNEP, 2019 ). The programs highlighted include the University of Pennsylvania School of Nursing, which has a course called Case Study—Addressing the Social Determinants of Health: Community Engagement Immersion ( Schroeder et al., 2019 ). This course offers experiential learning opportunities that focus on SDOH in vulnerable and underserved populations and helps students design health promotion programs for these communities. The school also offers faculty education in SDOH.
As far as the committee was able to determine, most programs include content on SDOH in community or public health nursing courses. However, this material does not appear to be integrated thoroughly into the curriculum in the majority of programs, nor could the committee identify well-established designs for curricula that address this content outside of community health rotations ( Campaign for Action, 2019b ; Storfjell et al., 2017 ; Thornton and Persaud, 2018 ). In the committee’s view, a single course in community and/or public health nursing is insufficient preparation for creating a foundational understanding of health equity and for preparing nurses to work in the wide variety of settings and roles envisioned in this report. Ideally, education in these concepts would be integrated throughout the curriculum to give nurses a comprehensive understanding of the social determinants that contribute to health inequities ( NACNEP, 2019 ; NLN, 2019 ; Siegel et al., 2018 ). Moreover, academic content alone is insufficient to provide students with the knowledge, skills, and abilities they need to advance health equity; rather, expanded opportunities for experiential and community learning are critical for building the necessary competencies ( Buhler-Wilkerson, 1993 ; Fee and Bu, 2010 ; NACNEP, 2016 ; Sharma et al., 2018 ). All those involved in nursing education—administrators, faculty, accreditors, and students—need to understand that health equity is a core component of nursing, no less important than alleviating pain or caring for individuals with acute illness. Graduating students need to understand and apply knowledge of the impact of such issues as classism, racism, sexism, ageism, and discrimination and to be empowered to advocate on these issues for people who they care for and communities.
As currently constituted, then, nursing education programs fall short of conveying this information sufficiently in the curriculum or through experiential learning opportunities. Yet, the existing evidence on what nursing education programs offer is scant. Research is therefore needed to assess whether and how many nursing programs are offering sufficient coursework and learning opportunities related to SDOH and health equity and to examine the extent to which graduating nurses have the competencies necessary to address these issues in practice.
The Need for BSN-Prepared Nurses
The 2011 The Future of Nursing report includes the recommendation that the percentage of nurses who hold a baccalaureate degree or higher be increased to 80 percent by 2020. The report gives several reasons for this goal, including that baccalaureate-prepared nurses are exposed to competencies including health policy, leadership, and systems thinking; they have skills in research, teamwork, and collaboration; and they are better equipped to meet the increasingly complex demands of care both inside and outside the hospital ( IOM, 2011 , p. 170). In 2011, 50 percent of employed nurses held a baccalaureate degree or higher; as of 2019, that proportion had increased to 59 percent ( Campaign for Action, 2020 ). Both the number of baccalaureate programs and program enrollment have increased substantially since 2011 2 ( AACN, 2019a ), and the number of RNs who went on to receive BSNs in RN-to-BSN programs increased 236 percent between 2009 and 2019 ( Campaign for Action, n.d. ). However, the goal of 80 percent of nurses holding a BSN was still not achieved by 2020, for a number of reasons. Although the proportion of new graduates with a BSN is higher than the proportion of existing nurses with a BSN, the percentage of new graduates joining the nursing workforce each year is small. Given this ratio, it would have been “extraordinarily difficult” to achieve the goal of 80 percent by 2020 ( IOM, 2016a ; McMenamin, 2015 ). Nurses already in the workforce face barriers to pursuing a BSN, including time, money, work–life balance, and a perception that additional postlicense education is not worth the effort ( Duffy et al., 2014 ; Spetz, 2018 ). Moreover, schools and programs have limited capacity for first-time nursing students and ADN, LPN nurses, or RNs without BSN degrees ( Spetz, 2018 ).
Nonetheless, the goal of achieving a nursing workforce in which 80 percent of nurses hold a baccalaureate degree or higher remains relevant, and continuing efforts to increase the number of nurses with a BSN are needed. Across the globe, the proportion of BSN-educated nurses is correlated with better health outcomes ( Aiken et al., 2017 ; Baker et al., 2020 ), and there are clear differences as well as similarities between associate’s degree in nursing (ADN) programs and BSN programs. In particular, BSN programs are more likely to cover topics relevant to liberal education, organizational and systems leadership, evidence-based practice, health care policy, finance and regulatory environments, interprofessional collaboration, and population health ( Kumm et al., 2014 ). Accelerated, nontraditional, and other pathways to the BSN degree are discussed later in this chapter.
The Need for PhD-Prepared Nurses
There are two types of doctoral degrees in nursing: the PhD and the DNP. The former is designed to prepare nurse scientists to conduct research, whereas the latter is a clinically focused doctoral degree designed to prepare graduates with advanced competencies in leadership and management, quality improvement, evidence-based practice, and a variety of specialties. PhD-prepared nurses are essential to the development of the research base required to support evidence-based practice and add to the body of nursing knowledge, and DNP-educated nurses play a key role in translating evidence into practice and in educating nursing students in practice fundamentals ( Tyczkowski and Reilly, 2017 ) (see Chapter 3 for further discussion of the role of DNPs).
The number of nurses with doctoral degrees has grown rapidly since the 2011 The Future of Nursing report was published ( IOM, 2011 ). As a proportion of doctorally educated nurses, however, the number of PhD graduates has remained nearly flat. In 2010, there were 1,282 graduates from DNP programs and 532 graduates receiving a PhD in nursing. By 2019, the number of DNP graduates had grown more than 500 percent to 7,944, while the number of PhD graduates had grown about 50 percent to 804 ( AACN, 2011 , 2020a ).
The slow growth in PhD-prepared nurses is a major concern for the profession and for the nation, because it is these nurses who serve as faculty at many universities and who systematically study issues related to health and health care, including the impact of SDOH on health outcomes, health disparities, and health equity. PhD-prepared nurses conduct research on a wide variety of issues relating to SDOH, including the effect of class on children’s health; linguistic, cultural, and educational barriers to care; models of care for older adults aging in place; and gun violence (Richmond and Foman, 2018; RWJF, 2020 ; Szanton et al., 2014 ). Nurse-led research provided evidence-based solutions in the early days of the COVID-19 pandemic for such challenges as the shift to telehealth care, expanding demand for health care workers, and increased moral distress ( Lake, 2020 ). However, Castro-Sánchez and colleagues (2021) note a dearth of nurse-led research specifically related to COVID-19; they posit that this gap can be attributed to workforce shortages, a lack of investment in clinical academic leadership, and the redeployment of nurses into clinical roles. More PhD-prepared nurses are needed to conduct research aimed at improving clinical and community health, as well as to serve as faculty to educate the next generation of nurses ( Broome and Fairman, 2018 ; Fairman et al., 2020 ; Greene et al., 2017 ).
Nursing practice is dependent on a robust pipeline of research to advance evidence-based care, inform policy, and address the health needs of people and communities ( Bednash et al., 2014 ). The creation of the BSN-to-PhD direct entry option has helped produce more research-oriented nurse faculty ( Greene et al., 2017 ), but time, adequate faculty mentorship, mental health issues, and financial hardships, including the cost of tuition, are barriers for nurses pursuing these advanced degrees ( Broome and Fairman, 2018 ; Fairman et al., 2020 ; Squires et al., 2013 ). One approach for increasing the number of PhD-prepared nurses is the Future of Nursing Scholars program, which successfully graduated approximately 200 PhD students through an innovative accelerated 3-year program ( RWJF, 2021 ). Similar programs have been funded by such foundations as the Hillman Foundation and Jonas Philanthropies to help stimulate the pipeline, build capacity (especially in health policy) among graduates, and model innovative curricular approaches ( Broome and Fairman, 2018 ; Fairman et al., 2020 ).
- DOMAINS AND COMPETENCIES FOR EQUITY
As noted earlier, a number of existing recommendations specify what nurses need to know to address SDOH and health inequity in a meaningful way. In addition, the Future of Nursing: Campaign for Action surveyed and interviewed faculty and leaders in nursing and public health, asking about core content and competencies for all nurses ( Campaign for Action, 2019b ). Respondents specifically recommended that nursing education cover seven areas:
- policy and its impact on health outcomes;
- epidemiology and biostatistics;
- a basic understanding of SDOH and illness across populations and how to assess and intervene to improve health and well-being;
- health equity as an overall goal of health care;
- interprofessional team building as a key mechanism for improving population health;
- the economics of health care, including an understanding of basic payment models and their impact on services delivered and outcomes achieved; and
- systems thinking, including the ability to understand complex demands, develop solutions, and manage change at the micro and macro system levels.
Drawing on all of these recommendations, guidelines, and perspectives, as well as looking at the anticipated roles and responsibilities outlined in other chapters of this report, the committee identified the core concepts pertaining to SDOH, health equity, and population health that need to be covered in nursing school and the core knowledge and skills that nurses need to have upon graduation. For consistency with the language used by the AACN, these are referred to, respectively, as “domains” (see Box 7-2 ) and “competencies” (see Box 7-3 ). The domains in Box 7-2 are fundamental content that the committee believes can no longer be covered in public health courses alone, but need to be incorporated and applied by nursing students throughout nursing curricula. All nurses, regardless of setting or type of nursing, need to understand and be prepared to address the underlying barriers to better health in their practice.
Domains for Nursing Education.
Competencies for Nursing Education, Depending on Preparation Level.
The committee believes that incorporation of these domains and competencies can guide expeditious and meaningful changes in nursing education. The committee acknowledges that making room for these concepts will inevitably require eliminating some existing material in nursing education. The committee does not believe that it is the appropriate entity to identify what specific curriculum changes should be made; a nationwide evaluation will be needed to ensure that nursing curricula are preparing the future workforce with the skills and competencies they will need. The committee also acknowledges that nursing programs differ in length, and that an ADN program cannot cover SDOH equity to the same extent as a BSN program. The specific knowledge and skills a nurse will need will vary depending on her or his level of nursing education. For example, a nurse with a BSN may need to understand and be able to use the technologies that are relevant to his or her area of work (e.g., telehealth applications, electronic health records [EHRs], home monitors), while an APRN may need a deeper understanding of how to analyze health records in order to provide care and monitor health status for populations outside clinical settings.
Nonetheless, nursing education at all levels—from licensed practical nurse (LPN) to ADN to BSN and beyond—needs to incorporate and integrate the domains and competencies in Boxes 7-2 and 7-3 to the extent possible so as to develop knowledge and skills that will be relevant and useful to nurses and essential to achieving equity in health and health care. Given the relationship among SDOH, social needs, and health outcomes and the increasing focus of health care systems on addressing these community and individual needs, the domains and competencies identified here are essential to ensure that all nurses understand and can apply concepts related to these issues; work effectively with people, families, and communities across the spectrum of SDOH; promote physical, mental, and social health; and assume leadership and entrepreneurial roles to create solutions, such as by fostering partnerships in the health and social sectors, scaling successful interventions, and engaging in policy development. While none of the domains listed in Box 7-2 are new to nursing, the health inequities that have become increasingly visible—especially as a result of the COVID-19 pandemic—demand that these domains now be substantively integrated into the fabric of nursing education and practice.
Many sources highlight both the challenges faced by front-line graduates when confronted with these issues, and the reality that many nursing schools lack faculty members with the knowledge and competencies to educate nurses effectively on these issues ( Befus et al., 2019 ; Effland et al., 2020 ; Hermer et al., 2020 ; Levine et al., 2020 ; Porter et al., 2020 ; Rosa et al., 2019 ; Valderama-Wallace and Apesoa-Varano, 2019 ). To remedy the latter gap, educators need to have a clear understanding of these issues and their links to both educational and patient outcomes (see the section below on strengthening and diversifying the nursing faculty). It is important to note as well that some of these topics, including the connections among implicit biases, structural racism, and health equity, may be difficult for educators and students to discuss (see Box 7-4 ).
Discussing Difficult Topics.
Given the limited scope of this report, the committee has chosen to highlight three of the competencies from Box 7-3 in this section. 3 The first is delivering person-centered care to diverse populations. As the United States becomes increasingly diverse, nurses will need to be aware of their own implicit biases and be able to interact with diverse patients, families, and communities with empathy and humility. The second is learning to collaborate across professions, disciplines, and sectors. As discussed previously in this report, addressing SDOH is necessarily a multisectoral endeavor given that these determinants go beyond health to include such issues as housing, education, justice, and the environment. The third is continually adapting to new technologies. Advances in technology are reshaping both health care and education, and making it possible for both to be delivered in nontraditional settings and nontraditional ways. In the present context, technology can expand access to underserved populations of patients and students—for example, telehealth and online platforms can be used to connect with those living in rural areas—but it can also exacerbate existing disparities and inequities. Nurses need to understand both the promises and perils of technology, and be able to adapt their practice and learning accordingly.
Delivering Person-Centered Care and Education to Diverse Populations
As discussed in Chapter 2 , people’s family and cultural background, community, and other experiences may have profound impacts on their health. Given the increasing diversity of the U.S. population, it is critical that nurses understand the impact of these factors on health, can communicate and connect with people of different backgrounds, and can be self-reflective about how their own beliefs and biases may affect the care they provide. To this end, the committee believes it is essential that nursing education include the concepts of cultural humility and implicit bias as a thread throughout the curriculum.
An integral part of learning about these concepts is an opportunity to reflect on what one is learning and to draw connections with past learning and experiences. Researchers have established that instruction that guides students in reflection helps reinforce skills and competencies (see, e.g., NASEM, 2018c ). This idea has been explored in the context of education in health professions and has been identified as a valuable way to foster understanding of health equity and SDOH ( IOM, 2016b ; Mann et al., 2007). While the strategies, goals, and structure of such reflection may vary, the process in general helps learners in health care settings examine their own values, assumptions, and beliefs ( El-Sayed and El-Sayed, 2014 ; Scheel et al., 2017 ). In the course of structured reflection, for example, students might consider how such issues as racism, implicit bias, trauma, and policy affect the care people receive and create conditions for poor health, or how their own experiences and identities influence the care they provide.
Cultural Humility
In recent years, the focus in discussions of patient care has shifted from cultural competency to cultural humility ( Barton et al., 2020 ; Brennan et al., 2012 ; Kamau-Small et al., 2015 ; Periyakoil, 2019 ; Purnell et al., 2018 ; Walker et al., 2016 ). The concept of cultural competency has been interpreted by some as limited for a number of reasons. First, it implies that “culture” is a technical skill in which clinicians can develop expertise, and it can become a series of static dos and don’ts ( Kleinman and Benson, 2006 ). Second, the concept of cultural competency tends to promote a colorblind mentality that ignores the role of power, privilege, and racism in health care (Waite and Nardi, 2017). Third, cultural competency is not actively antiracist but instead leaves institutionalized structures of White privilege and racism intact ( Schroeder and DiAngelo, 2010 ).
In contrast, cultural humility is defined by flexibility, a lifelong approach to learning about diversity, and a recognition of the role of individual bias and systemic power in health care interactions ( Agner, 2020 ). Cultural humility is considered a self-evaluating process that recognizes the self within the context of culture ( Campinha-Bacote, 2018 ). The concept of cultural humility can be woven into most aspects of nursing and interprofessional education. For example, case studies in which students learn about the experience of a particular disease or strategies for disease prevention can be designed to model culturally humble approaches in the provision of nursing care and the avoidance of stereotypical thinking ( Foronda et al., 2016 ; Mosher et al., 2017 ). One effective approach to cultivating cultural humility is to accompany experiential learning opportunities or case studies with reflection that expands learning beyond skills and knowledge. This includes questioning current practices and proposing changes to improve the efficiency and quality of care, equality, and social justice ( Barton et al., 2020 ; Foronda et al., 2013 ). Programs designed to develop nurses’ cultural sensitivity and humility, as well as cultural immersion programs, have been developed, and research suggests that such programs can effectively develop skills that strengthen nurses’ confidence in treating diverse populations, improve patient and provider relationships, and increase nurses’ compassion ( Allen, 2010 ; Gallagher and Polanin, 2015 ; Sanner et al., 2010 ).
Implicit Bias
Implicit bias is an unconscious or automatic mental association made between members of a group and an attribute or evaluation ( FitzGerald and Hurst, 2017 ). For example, a clinician may unconsciously view White patients as more medically compliant than Black patients ( Sabin et al., 2008 ). These types of biases not only can have consequences for individual health outcomes ( Aaberg, 2012 ; Linden and Redpath, 2011 ) but also may play a role in maintaining or exacerbating health disparities ( Blair et al., 2011 ). There are many resources available for implicit bias awareness and training; for example, Harvard University offers a number of Implicit Association Tests (IATs), the Institute for Healthcare Improvement offers free online resources to address implicit bias, and the AACN offers implicit bias workshops for nurses ( AACN, n.d. ; Foronda et al., 2018 ).
Evidence on the use of implicit bias training is limited. One review of the use of an IAT in health professions education found that the test had contrasting uses, with some curricula using it as a measure of implicit bias and others using it to initiate discussions and reflection. The review found a dearth of research on the use of IATs; the authors note that the nature of implicit bias is highly complex and cannot necessarily be reduced to the “time-limited” use of an IAT ( Sukhera et al., 2019 ). A systematic review of interventions designed to reduce implicit bias found that many such interventions are ineffective, and some may even increase implicit biases. The authors note that while there is no clear path for reducing biases, the lack of evidence does not weaken the case for “implementing widespread structural and institutional changes that are likely to reduce implicit biases” (FitzGerald et al., 2019). One promising model is an intervention that helps participants break the “prejudice habit” ( Devine et al., 2012 ). This multifaceted intervention, which includes situational awareness of bias, education about the consequences of bias, strategies for reducing bias, and self-reflection, has been shown to reduce implicit racial bias for at least 2 months ( Devine et al., 2012 ). Clearly, more research is needed in this area.
Learning to Collaborate Across Professions, Disciplines, and Sectors
As discussed in Chapter 9 , eliminating health disparities will require the active engagement and advocacy of a broad range of stakeholders working in partnership to address the drivers of structural inequities in health and health care ( NASEM, 2017 ). In these efforts, nurses may lead or work with people from a variety of professions, disciplines, and sectors, including, for example, physicians, social workers, educators, policy makers, lawyers, faith leaders, government employees, community advocates, and community members. Working across sectors, especially as they relate to SDOH (food insecurity, transportation barriers, housing, etc.), is a critical competence. Collaboration among these types of stakeholders has multiple benefits, including broader expertise and perspective, the capacity to address wide-ranging social needs, the ability to reach underserved populations, and sustainability and alignment of efforts (see Chapter 9 for further discussion). A traditional nursing education, which focuses on what is taught rather than on building competencies, is unlikely to give students the understanding of broader social, political, and environmental contexts that is necessary for working in these types of strategic partnerships ( IOM, 2016b ). If nursing students are to be prepared to practice interprofessionally after graduation, they must be given opportunities to collaborate with others before graduation ( IOM, 2013 ) and to build the competencies they will need for collaborative practice. The Interprofessional Education Collaborative (IPEC) identified four core competencies for interprofessional collaborative practice ( IPEC, 2016 ). While these competencies were developed specifically to prepare students for interprofessional practice within health care, they are also applicable to broader collaborations among other professions, disciplines, and sectors both within and outside of health care:
- Work with individuals of other professions to maintain a climate of mutual respect and shared values.
- Use the knowledge of one’s own role and those of other professionals to appropriately assess and address the health care needs of patients and to promote and advance the health of populations.
- Communicate with patients, families, communities, and professionals in health and other fields in a responsive and responsible manner that supports a team approach to the promotion and maintenance of health and the prevention and treatment of disease.
- Apply relationship-building values and the principles of team dynamics to perform effectively in different team roles in planning, delivering, and evaluating patient/population-centered care and population health programs and policies that are safe, timely, efficient, effective, and equitable.
There are opportunities for nursing students to gain interprofessional and multisector collaborative competencies through both experiential learning in the community (discussed in detail below) and classroom work. Increasingly, nursing schools are working with other institutions to offer students classes in which they learn with or from students and professionals in other disciplines. For example, the University of Michigan Center for Interprofessional Education offers courses in such topics as health care delivery in low- and middle-income countries, social justice, trauma-informed practice, interprofessional communication, and teamwork. Courses are open to students from the schools of social work, pharmacy, medicine, nursing, dentistry, physical therapy, public health, and business. 4
Despite the benefits of interprofessional education, however, there are barriers that affect the implementation of such programs in health professions education, including different schedules, lack of meeting space, incongruent curricula plans, faculty not trained to teach interprofessionally, faculty overload, and the challenge of providing adequate opportunities for all levels of students ( NLN, 2015a ). The use of simulation has been proposed as a vehicle for overcoming such barriers to impart interprofessional collaborative competencies ( NLN, 2013 ); a systematic review of the evidence found that this approach can be effective ( Marion-Martins and Pinho, 2020 ). Nurses can also gain interprofessional experience by pursuing dual degrees. For example, the University of Pennsylvania offers dual degrees that combine nursing with health care management, bioethics, public health, law, or business administration.
Continually Adapting to New Technologies
Nurses can use a wide variety of existing and emerging technologies and tools to address SDOH and provide high-quality care to all patients (see Box 7-5 ). Broadly speaking, these technologies and tools fall into three categories: patient-facing, clinician-facing, and data analytics. Patient- and clinician-facing tools collect data and help providers and patients connect and make decisions about care. Data analytics uses data, collected from patients or other sources, to analyze trends, identify disparities, and guide policy decisions. Beginning as students, all nurses need to be familiar with these technologies, be able to engage with patients or other professionals around their appropriate use, and understand how their use has the potential to exacerbate inequalities.
Highlights from the Seattle Townhall on Technology and Health Equity and Implications for Nursing Education.
Patient-facing technologies include apps and software, such as mobile and wearable health devices, as well as telehealth and virtual visit technologies ( FDA, 2020 ). These tools allow nurses and other health care providers to expand their reach to those who might otherwise not have access because of geography, transportation, social support, or other challenges. For example, telehealth and mobile apps allow providers to see people in their homes, mitigating such barriers to care as transportation while also helping providers understand people in the context of their everyday lives. Essential skills for nurses using these new tools will include the ability to project a caring relationship through technology (Massachusetts Department of Higher Nursing Education Initiative, 2016 ) and to use technology to personalize care based on patient preferences, technology access, and individual needs ( NLN, 2015b ). The role of telehealth and the importance of training nurses in this technology have been recognized for several years ( NONPF, 2018 ; Rutledge et al., 2017 ), but the urgent need for telehealth services during the COVID-19 pandemic has made it “imperative” to include telehealth training in nursing curricula ( Love and Carrington, 2020 ). Moreover, it is anticipated that the shift to telehealth for some types of care will become a permanent feature of the health care system in the future ( Bestsennyy et al., 2020 ).
Clinician-facing technologies include EHRs, clinical decision support tools, mobile apps, and screening and referral tools ( Bresnick, 2017 ; CDC, 2018 ; Heath, 2019 ). A number of available digital technologies can facilitate the collection and integration of data on social needs and SDOH and help clinicians hold compassionate and empathetic conversations about those needs ( AHA, 2019 ; Giovenco and Spillane, 2019 ). In 2019, for example, Kaiser Permanente launched its Thrive Local network (Kaiser Permanente, 2019 ), which can be used to screen for social needs and connect people with community resources that can meet these needs. The system is integrated with the EHR, and it is capable of tracking referrals and outcomes to measure whether needs are being met; these data can then be used to continuously improve the network.
Nurses will need to understand how and when to use these types of tools, and can leverage their unique understanding of patient and community needs to improve and expand them. As described in Chapter 10 , such technologies as EHRs and clinical alarms can burden nurses and contribute to workplace stress. However, nurses have largely been left out of conversations about how to design and use these systems. For example, although nurses are one of the primary users of EHR systems, little research has been conducted to understand their experiences with and perceptions of these systems, which may be different from those of other health care professionals ( Cho et al., 2016 ; Higgins et al., 2017 ). Out of 346 usability studies on health care technologies conducted between 2003 and 2009, only 2 examined use by nurses ( Yen and Bakken, 2012 ). Educating nurses to understand and assess the benefits and drawbacks of health care technologies and have the capacity to help shape and revamp them can ultimately improve patient care and the well-being of health professionals.
Tools for data analytics are increasingly important for improving patient care and the health of populations ( Ibrahim et al., 2020 ; NEJM Catalyst, 2018 ). Analysis of large amounts of data from such sources as EHRs, wearable monitors, and surveys can help in detecting and tracking disease trends, identifying disparities, and finding patterns of correlation ( Breen et al., 2019 ; NASEM, 2016a ; Shiffrin, 2016 ). The North Carolina Institute for Public Health, for example, collaborated with a local health system in analyzing data to inform a community health improvement plan ( Wallace et al., 2019 ). Data on 12 SDOH indicators were sourced from the American Community Survey and mapped by census tract. The mapping provided a visualization of the disparities in the community and allowed the health system to focus its efforts strategically to improve community health. The North Carolina Department of Health and Human Services later replicated this strategy across the entire state ( NCDHHS, 2020 ).
There are opportunities for nurses to specialize in this type of work. For example, nursing informatics is a specialized area of practice in which nurses with expertise in such disciplines as information science, management, and analytical sciences use their skills to assess patient care and organizational procedures and identify ways to improve the quality and efficiency of care. In the context of SDOH, nursing informaticists will be needed to leverage artificial intelligence and advanced visualization methods to summarize and contextualize SDOH data in a way that provides actionable insights while also eliminating bias and not overwhelming nurses with extraneous information. Big data are increasingly prevalent in health care, and nurses need the skills and competencies to capitalize on its potential ( Topaz and Pruinelli, 2017 ). Even nurses who do not specialize in informatics will need to understand how the analysis of massive datasets can impact health ( Forman et al., 2020 ; NLN, 2015b ). Investments in expanding program offerings, certifications, and student enrollment will be needed to meet the demand for nurses with such skills.
As noted, however, despite its promise for improving patient care and community health, technology can also exacerbate existing disparities ( Ibrahim et al., 2020 ). For example, people who lack access to broadband Internet and/or devices are unable to take advantage of such technologies as remote monitoring and telehealth appointments ( Wise, 2012 ). Older adults, people with limited formal education, those living in rural and remote areas, and the poor are less likely to have access to the Internet. As health care becomes more reliant on technology, these groups are likely to fall behind ( Arcaya and Figueroa, 2017 ). In addition, such technologies as artificial intelligence and algorithmic decision-making tools may exacerbate inequities by reflecting existing biases ( Ibrahim et al., 2020 ). Nursing education needs to prepare nurses to understand these potential downsides of technology in order to prevent and mitigate them. This has become a particularly critical issue during the COVID-19 pandemic, with the rapid shift to telehealth potentially having consequences for those with low digital literacy, limited English proficiency, and a lack of access to the Internet ( Velasquez and Mehrotra, 2020 ).
Not all nurses will need to acquire all of the key technological competencies; curricula can be developed according to the likely needs of nurses working at different levels. For example, most nurses will need the knowledge and skills to use telehealth, digital health tools, and data-driven clinical decision-making skills in practice, whereas nurse informaticians and some doctoral-level nurses will need to be versed in device design, bias assessment in algorithms, and big data analysis.
- EXPANDING LEARNING OPPORTUNITIES
As stated previously, the domains and competencies enumerated above cannot be conveyed to nursing students through traditional lectures alone. Building the competencies to address population health, SDOH, and health inequities will require substantive experiential learning, collaborative learning, an integrated curriculum, and continuing professional development throughout nurses’ careers ( IOM, 2016b ). The 2019 Campaign for Action survey of nursing educators and leaders found that a majority of respondents identified “innovative community clinical experiences” and “interprofessional education experiences” as the top methods for teaching population health ( Campaign for Action, 2019b ). A recurrent theme in interviews with respondents was the importance of active and experiential learning, with opportunities for partnering with nontraditional agencies ( Campaign for Action, 2019b ). These types of community-based educational opportunities, particularly when they involve partnerships with others, are critical for nursing education for multiple reasons.
First, experience in the community is essential to understanding SDOH and gaining the competencies necessary to advance health equity ( IOM, 2016b ). In fact, restricting education in SDOH to the classroom may even be harmful, given the finding of a 2016 study that medical students who learned about SDOH in the classroom rather than through experiential learning demonstrated an increase in negative attitudes toward medically underserved populations ( Schmidt et al., 2016 ).
Second, community-based education offers opportunities for students to engage with community partners from other sectors, such as government offices of housing and transportation or community organizations, preparing them for the essential work of participating in and leading partnerships to address SDOH. An example is a pilot interdisciplinary partnership between a school of nursing and a city fire department in the Pacific Northwest that allows students to practice such skills as motivational interviewing to identify the range of problems (e.g., transportation issues, difficulty accessing insurance or providers, lack of caregiving support) faced by people calling emergency services ( Yoder and Pesch, 2020 ).
Third, nursing is increasingly practiced in community settings, such as schools and workplaces, as well as through home health care ( WHO, 2015 ). Nursing students are prepared to practice in hospitals, but do not necessarily receive the same training and preparation for these other environments ( Bjørk et al., 2014 ). Education in the community allows nursing students to learn about the broad range of care environments and to work collaboratively with other professionals who work in these environments. For example, students may work in a team with community health workers, social workers, and those from other sectors (e.g., housing and transportation), work that both enriches the experience of student nurses and creates bridges between nursing and other fields ( Zandee et al., 2010) . Nurses who have these experiences during school may then be more prepared to lead and participate in multisector efforts to address SDOH—the importance of which is emphasized throughout this report—once they enter practice. Evidence suggests that graduating students are more likely to seek work in areas that are familiar to them from their education, clinical experience, and theoretical training ( Jamshidi et al., 2016 ); thus, these nontraditional educational experiences may increase the number of nurses interested in working in the community. Moreover, while training in acute care settings has often been regarded as more valuable than that provided in community settings, evidence indicates that the two offer comparable opportunities for learning clinical skills ( Morton et al., 2019 ). In fact, clinical care in community-based settings can present greater complexity relative to that in the hospital, and some technical skills (e.g., epidemiologic disease tracking, tuberculosis assessment and management, immunizations) are more available in community than in acute care settings ( Morton et al., 2019 ).
Some nursing programs have incorporated community-based experiential learning into their programs. At community colleges and universities, schools have implemented nurse-managed clinics that serve the local population and their own students while also giving students technical skills and experience in interacting with the community. Lewis and Clark Community College, for example, operates a mobile health unit that brings health and dental care to six counties in southern Illinois ( Lewis and Clark, n.d. ), while nursing students at Alleghany College of Maryland can gain experience in the Nurse Managed Wellness Clinic, which offers such services as immunizations, screenings, and physicals ( Alleghany College, 2020 ). At the baccalaureate and master’s level, a number of schools offer longitudinal, integrated experiences in settings as varied as federally qualified health centers (FQHCs), public health departments, homeless shelters, public housing sites, public libraries, and residential addiction programs ( AACN, 2020c ). Students and faculty at the University of Washington School of Nursing, for example, support community-oriented projects in partnership with three underserved communities in the Seattle area. Graduate students work for 1 year on grassroots projects (e.g., food banks, school health) and then reinforce this experience with 1 year of work at the policy level ( AACN, 2020c ). At the doctoral level, Washburn University transformed its DNP curriculum to incorporate SDOH and reinforce that instruction through experiential learning in the community (see Box 7-6 ). In addition to clinical education, nursing students can participate in nontraditional clinical community engagement and service learning opportunities, such as volunteering at a homeless shelter or working in a service internship for a community organization. These opportunities get students into the community, help them build relationships with people from health care and other sectors, and promote understanding of and engagement with SDOH ( Bandy, 2011 ).
Pine Ridge Family Health Center.
Simulation-Based Education
Simulation-based education is another useful tool for teaching nursing concepts and developing competencies and skills ( Kononowicz et al., 2019 ; Poore et al., 2014 ; Shin et al., 2015 ). It can range from very low-tech (e.g., using oranges to practice injections) to very high-tech (e.g., a virtual reality emergency room “game”), but all simulations share the ability to bridge the gap between education and practice by imparting skills in a low-risk environment ( SSIH, n.d. ).
Simulations give students an opportunity to make real-time decisions and interact with virtual patients without having to face many of the challenges of traditional clinical education ( Hayden et al., 2014 ). They can be used to enhance many types of skills, including communication ( NASEM, 2018b ), cultural sensitivity ( Lau et al., 2016 ), and screening for SDOH ( Thornton and Persaud, 2018 ). Several simulation-based tools are available for learning about the realities of poverty, such as the Community Action Poverty Simulation (see Box 7-7 ) and the Cost of Poverty Experience ( ThinkTank, n.d. ). Such tools can help nurses identify ways in which their practice could directly mitigate the effects of poverty on individuals, families, and communities. Evaluations of poverty simulations have found that they can positively impact attitudes toward poverty and empathy among nurses and nursing students ( Phillips et al., 2020 ; Turk and Colbert, 2018 ), although one study noted that the simulations should be accompanied by the inclusion of social justice concepts throughout the curriculum to achieve lasting change ( Menzel et al., 2014 ).
The Community Action Poverty Simulation.
Individual schools may or may not have the resources or faculty to support some types of simulation activities. For those that do not, simulation centers shared by schools of multiple professions and hospitals can provide access ( Marken et al., 2010 ). For example, the New York Simulation (NYSIM) Center was created through a public–private partnership to manage interprofessional, simulation-based education for students and hospital employees across multiple sites ( NYSIM, 2017 ). The opportunity to take part in simulation experiences with students from other health professions can also improve collaboration and teamwork and prepare nurses for practicing interprofessionally in the workplace (von Wendt and Niemi-Murola, 2018 ).
Limitations on in-person clinical training during the COVID-19 pandemic conditions have demonstrated the promise of simulation-based education as a way to supplement traditional nursing education, allowing students to complete their education and sustaining the nursing workforce pipeline ( Horn, 2020 ; Jiménez-Rodríguez et al., 2020 ; Yale, 2020 ). Before the pandemic, the NCSBN conducted a longitudinal, randomized controlled trial of the use of simulation and concluded that substituting simulation-based education for up to half of a nursing student’s clinical hours produces comparable educational outcomes and students who are ready to practice ( Hayden et al., 2014 ). The COVID-19 pandemic has necessitated and accelerated the use of simulation to replace direct care experience in nursing schools, and state boards of nursing have loosened previous restrictions on its use ( NCSBN, 2020b ). Evaluation of this expanded use of simulation and other virtual experiences during the pandemic is needed, both in preparation for future emergencies and for use in nursing education generally.
- RECRUITING AND SUPPORTING DIVERSE PROSPECTIVE NURSES
The composition of the population of prospective nurses and the ways they are supported throughout their education are important factors in how prepared the future nursing workforce will be to address SDOH and health equity. As discussed in prior chapters, developing a more diverse nursing workforce will be key to achieving the goals of reducing health disparities, providing culturally relevant care for all populations, and fostering health equity (Center for Health Affairs, 2018 ; IOM, 2011 , 2016 ; Williams et al., 2014 ). A diverse workforce is one that reflects the variations in the nation’s population in such characteristics as socioeconomic status, religion, sexual orientation, gender, race, ethnicity, and geographic origin.
The nursing workforce has historically been overwhelmingly White and female, although it is steadily becoming more diverse (see Chapter 3 ). The 2016 IOM report assessing progress on the 2011 The Future of Nursing report notes that shifting the demographics of the overall workforce is inevitably a slow process since only a small percentage of the workforce leaves and enters each year ( IOM, 2016a ). The pipeline of students entering the field, on the other hand, can respond much more rapidly to efforts to increase diversity ( IOM, 2016a ). Since the 2011 report was published, significant gains have been realized in the diversity of nursing students. The number of graduates from historically underrepresented ethnic and racial groups more than doubled for BSN programs, more than tripled for entry-level master’s programs, and more than doubled for PhD programs ( AACN, 2020a ). The number of underrepresented students graduating from DNP programs grew by more than 1,000 percent, although this gain was due in large part to rapid growth in these programs generally. Yet, despite these gains, nursing students remain largely female and White: in 2019, 85–90 percent of students were female, and around 60 percent were White. The percentages of ADN, BSN, entry-level master’s, PhD, and DNP graduates in 2019 by race/ethnicity and gender are shown in Tables 7-3 and 7-4 , respectively. For example, the proportion of Hispanic or Latino nurses is highest among ADN graduates (12.8 percent) and lowest among PhD (5.5 percent) and DNP (6 percent) graduates, while the proportion of Asian nurses is highest among MSN graduates (11.2 percent) and lower among graduates with all other degrees. The proportion of PhD graduates who are male (9.9 percent) is significantly lower than the proportion of graduates with other degrees who are male.
Nursing Program Graduates by Degree Type and by Race/Ethnicity, 2019.
Nursing Program Graduates by Degree Type and Gender, 2019.
Diversifying and strengthening the nursing student body—and eventually, the nursing workforce—requires cultivating an inclusive environment, recruiting and admitting a diverse group of students, and providing students with support and addressing barriers to their success throughout their academic career and into practice. In addition, it is essential to make available information that will enable prospective students to make informed decisions about their education and give them multiple pathways for completing their education (e.g., distance learning, accelerated programs). Accrediting bodies can play a role in advancing diversity and inclusion in nursing schools by requiring certain policies, practices, or systems. For example, the accreditation standards for medical schools of the Liaison Committee on Medical Education (LCME) include the following expectation ( LCME, 2018 ):
A medical school has effective policies and practices in place, and engages in ongoing, systematic, and focused recruitment and retention activities, to achieve mission appropriate diversity outcomes among its students, faculty, senior administrative staff, and other relevant members of its academic community. These activities include the use of programs and/or partnerships aimed at achieving diversity among qualified applicants for medical school admission and the evaluation of program and partnership outcomes.
Currently, none of the major nursing accreditors (ACEN, CCNE, CNEA) includes similar language in its accreditation standards. As shown in Table 7-5 , of six possible areas for standards on diversity and inclusion, ACEN and CCEN have standards only for student training, while CNEA has standards for student training and faculty diversity. No nursing accreditors have standards for student diversity; in comparison, accrediting bodies for pharmacy, physician assistant, medical, and dental schools all have such standards.
Diversity and Inclusion in Accreditation Standards.
Cultivating an Inclusive Environment
Efforts to recruit and educate prospective nurses to serve a diverse population and advance health equity will be fruitless unless accompanied by efforts to acknowledge and dismantle racism within nursing education and nursing practice ( Burnett et al., 2020 ; Schroeder and DiAngelo, 2010 ; Villaruel and Broome, 2020 ; Waite and Nardi, 2019 ). The structural, individual, and ideological racism that exists in nursing is rarely called out, and this silence further entrenches the idea of Whiteness as the norm within nursing while marginalizing and silencing other groups and their perspectives ( Burnett et al., 2020 ; Iheduru-Anderson, 2020 ; Schroeder and DiAngelo, 2010 ). Non-White students report a wide variety of negative experiences in nursing school, including unsupportive faculty, discrimination and microaggressions 5 on the part of faculty and peers, bias in grading, loneliness and social isolation, feeling unwelcome and excluded, being viewed as a homogeneous population despite being from varying racial/ethnic groups, lack of support for career choices, and a lack of mentors ( Ackerman-Barger et al., 2020 ; Graham et al., 2016 ; Johansson et al., 2011 ; Loftin et al., 2012 ; Metzger et al., 2020 ). These experiences are associated with adverse outcomes that include disengagement from education, loss of “self,” negative perceptions of inclusivity and diversity at the institution, and institutions’ inability to recruit and retain a diversity of students ( Metzger et al., 2020 ). By contrast, when students characterize the learning environment as inclusive, they are more satisfied and confident in their learning and rate themselves higher on clinical self-efficacy and clinical belongingness ( Metzger and Taggart, 2020 ).
Notably, however, underrepresented and majority students describe inclusive environments differently. In a study of fourth-year baccalaureate nursing students, both groups described an inclusive classroom as one where they felt comfortable and respected and had a sense of belonging, but underrepresented minority students also noted the importance of feeling safe, feeling free from hostility, and being seen as themselves and not a representative of their group ( Metzger and Taggart, 2020 ). Both groups agreed that inclusivity requires a top-down approach, and that faculty are particularly influential in creating an inclusive environment, yet underrepresented students shared many experiences in which faculty either disrupted the sense of belonging or did not intervene when someone else did ( Metzger and Taggart, 2020 ).
While increased attention has recently been focused on increasing diversity in nursing education, the pervasiveness of racism requires more open acknowledgment and discussion and a systematic and intentional approach that may, as discussed earlier, be uncomfortable for some ( Ackerman-Barger et al., 2020 ; Villaruel and Broome, 2020 ). Cultivating an inclusive environment requires acknowledging and challenging racism in all aspects of the educational experience, including curricula, institutional policies and structures, pedagogical strategies, and the formal and informal distribution of resources and power ( Iheduru-Anderson, 2020 ; Koschmann et al., 2020 ; Metzger and Taggart, 2020 ; Schroeder and DiAngelo, 2010 ; Villaruel and Broome, 2020 ; Waite and Nardi, 2019 ). Nursing school curricula have historically focused on the contributions of White and female nurses ( Waite and Nardi, 2019 ). The weight given to this curricular content sends a message to students—both White students and students of color—about what faculty consider important ( Villaruel and Broome, 2020 ). Moving forward, curricula need to include a critical examination of the history of racism within nursing and an acknowledgment and celebration of the contribution of nurses of color ( Waite and Nardi, 2019 ). Such efforts need to be led by a broad group of individuals from all levels within an institution; racism in institutional practices can be so ingrained that it is difficult for those with power to recognize ( Villaruel and Broome, 2020 ). Faculty often understand the importance of an inclusive learning environment, but struggle with moving from intention to action (Beard, 2013, 2014 ; Metzger et al., 2020 ).
While institutional efforts to change organizational culture are thoroughly described in the literature, they remain too rare to address the problems described above effectively ( Breslin et al., 2018 ). In the early 2000s, the University of Washington School of Nursing implemented a project designed to change the “climate of whiteness” at the school ( Schroeder and DiAngelo, 2010 ). The project involved many facets, including year-long antiracist workshops; a comprehensive and institutionalized diversity statement; and action plans for addressing admission barriers, encouraging ongoing education for faculty, and disseminating antiracist information to the entire campus. The authors of an evaluation of the project note that while initial feedback was positive, changing the sociopolitical climate of a school is a long-term process that requires institutional commitment, innovative leadership, long- and short-term strategies, and patience ( Schroeder and DiAngelo, 2010 ). Unfortunately, many administrators and leaders may hesitate to initiate dialogues about these issues or may lack knowledge of how to address the challenges, and in many institutions, faculty and administrators from underserved groups have been expected to carry this burden, which can allow their colleagues to remain passive ( Lim et al., 2015 ). The committee stresses that addressing racism and discrimination within the nursing profession requires more than mere programs or statements; it requires developing action-oriented strategies, holding difficult conversations about privilege, dismantling long-standing structures and traditions, conducting curricular reviews to detect biases and correct as necessary, and exploring how interpersonal and structural racism shapes the student experience both consciously and unconsciously ( Burnett et al., 2020 ; Iheduru-Anderson, 2020 ; Waite and Nardi, 2019 ).
Recruitment and Admissions
Many social and structural barriers impede the entry of underrepresented students into the nursing profession ( NACNEP, 2019 ). Several approaches can be taken to improve access for prospective underrepresented students and, by extension, increase the diversity of the nursing workforce. Recruitment of underrepresented students can start years before nursing school through such approaches as improved K–12 science education ( AAPCHO, 2009 ) and outreach to junior high and high school students, such as through summer pipeline programs ( Katz et al., 2016 ) or health career clubs ( Murray et al., 2016 ). K–12 education is particularly important for sparking students’ interest in the health professions, as well as for giving them the foundational knowledge necessary for success ( NASEM, 2016b ). One innovative approach to preparing young people for a career in nursing is the Rhode Island Nurses Institute Middle College Charter High School (RINIMC). RINIMC offers a free, 4-year, nursing-focused, high school education open to any student in Rhode Island; students graduate with experience in health care as well as up to 20 college credits. Nearly half of the program’s students are Latinx, and more than one-third are Black ( RINIMC, n.d. ). Establishing a pathway to nursing education for diverse students well before undergraduate school is important, particularly for first-generation students ( Katz et al., 2016 ; McCue, 2017 ). Some states offer dual enrollment programs. An example is Ohio’s College Credit Plus program, in which students in grades 7 to 12 have the opportunity to earn college and high school credits simultaneously, thus preparing them for postsecondary success. 6
Once students have applied to nursing school, a system of holistic admissions can improve the diversity of the incoming class ( Glazer et al., 2016 , 2020 ). A holistic admissions system involves evaluating an applicant based not only on academic achievement but also on experiences, attributes, potential contributions, and the fit between the applicant and the institutional mission ( DeWitty, 2018 ; NACNEP, 2019 ). Schools that have implemented such a system have seen an increase in the diversity of their student body ( Glazer et al., 2016 , 2018 ). Academic measures (e.g., graduation and exam pass rates) have remained unchanged or improved, and schools have reported increases in such measures as student engagement, cooperation and teamwork, and openness to different perspectives ( Artinian et al., 2017 ; Glazer et al., 2016 , 2020 ). In a recent paper published by AACN (2020d) , the following promising practices in holistic admissions were identified: (1) review institutional mission, vision, and values statements to ensure that they value diversity and inclusion; (2) create an “experience, attributes, and metrics (E-A-M) model” (p. 16) that connects back to the institution’s mission statement; (3) identify recruitment practices that align with the E-A-M model; (4) design rubrics to be used by admissions committees that are reflective of the E-A-M model; (5) engage faculty and staff in the holistic admissions review process; (6) use technology resources such as a centralized application system to maintain efficiencies; (7) develop tailored support services for underrepresented students; and (8) engage in a review and assessment of the entire process.
Addressing Barriers to Success
Part of cultivating an inclusive educational environment is acknowledging and addressing barriers that may prevent students from achieving their potential. As noted previously, some students—particularly those from underrepresented groups—may need support in a number of areas, including economic, social and emotional, and academic and career progression. Attention to the barriers faced by students is essential at each step along the pathway from high school preparation; to recruitment, admission, retention, and academic success in nursing school; to graduation and placement in a job; to retention and advancement within a nursing career ( IOM, 2016b ).
Providing Economic Supports
Cost is a key factor in decisions about nursing education for most students, and is particularly salient for those from underrepresented groups, who come disproportionately from families with comparatively low incomes and levels of wealth ( Diefenbeck et al., 2016 ; Graham et al., 2016 ; Sullivan, 2004 ). Sabio and Petges (2020) interviewed associate’s degree nursing students in a Midwestern state and found that the total cost of a baccalaureate degree and student debt was the greatest barrier to pursuing a degree, followed by family and personal, such as head-of-household, responsibilities. This challenge is pervasive in higher education, and there are indications that the problem is growing (Advisory Committee on Student Financial Assistance, 2013 ). Students need to have the financial resources not only for tuition but also for an array of education-related expenses, including housing, food, work attire, books, and supplies.
Providing clear information about the costs of nursing education and available financial supports early in the recruitment and admission process is key to identifying those who need help and encouraging them to enroll ( Pritchard et al., 2016 ). Recruitment and admission practices need to take into account student finances and how future salaries affect choices, particularly for certain groups of students. Most health care systems provide some level of tuition reimbursement for baccalaureate and higher education, and this support may lead students toward certain settings (e.g., acute care) and away from others (e.g., public health, primary care) ( Larsen, 2012 ). Other financial support options are available, including the Public Service Loan Forgiveness program, which offers full forgiveness after 10 years for employees of nonprofit or government organizations ( U.S. Department of Education, n.d.b ), and programs through HRSA that award loan repayment to RNs and advanced practice nurses who work in health professions shortage areas for at least 2 years ( HRSA, 2021 ).
State policy reform can help remove some of the structural barriers to education. For example, New York State has implemented a program that allows New York households earning less than $125,000 annually to qualify for free instate tuition at state public universities ( New York State, n.d. ). New nurses who complete an associate’s degree in New York are required to complete a bachelor’s degree within 10 years of graduation; free in-state tuition could make a considerable difference for these nurses in pursuing their next degree. While it is too early to assess the effects on the composition of the nursing workforce, this approach bears further evaluation. Certainly it is critical for state policies to facilitate the financing of nursing education using models other than additional student loans. There are demonstrated disparities in the burden of student debt between Black and White students (Brookings Institution, 2016 ), and the risk of assuming large amounts of debt for students from disadvantaged backgrounds may be one they cannot afford to take. Therefore, innovative financing models are necessary to ensure that all nurses can pursue educational opportunities.
It is also important to note that as they progress in their education, students of many backgrounds may experience food insecurity, struggles with housing, or issues with transportation that affect their ability to perform ( AAC&U, 2019 ; Laterman, 2019 ; Strauss, 2020 ). Institutions need to ensure that students’ basic needs are met during their studies through sustained, multiyear funding and resources to support students facing financial emergencies.
Social and Academic Supports
Once students have been admitted, some nursing schools offer programs, such as summer programs that bridge high school and college, designed to prepare them academically and socially for the rigors of nursing education. Some of these programs are designed specifically for underrepresented and/or first-generation college students ( Pritchard et al., 2016 ), who may lack adequate family, emotional, and moral support; mentorship opportunities; professional socialization; and academic support ( Banister et al., 2014 ; Loftin et al., 2012 ). A study at the University of Cincinnati College of Nursing found that the impact of its summer bridge program lasted throughout the first year of school, and that grade point averages and retention were similar between underrepresented and majority students ( Pritchard et al., 2016 ). The Recruitment & Retention of American Indians into Nursing (RAIN) program at the University of North Dakota conducts a “No Excuses Orientation” workshop to give incoming American Indian students an opportunity to create connections and become acquainted with people and resources at the university ( UND, 2020 ). Tribal leaders are included in the orientation, along with discussions of cultural and family values and issues.
Another approach for supporting students is through mentoring programs. As discussed in Chapter 9 , these programs create supportive environments by providing peer and faculty role modeling, academic guidance, and support ( Wilson et al., 2010 ). Evidence indicates that mentoring programs for students from underrepresented groups are more effective when they include nurses and faculty from those groups, who have firsthand understanding of the unique challenges these students and nurses regularly confront ( Banister et al., 2014 ). This observation underscores the need for diverse faculty, mentors, and preceptors with the availability and willingness to guide these students and teach them leadership. For example, the RAIN program provides mentoring to American Indian students; staff and leaders are heavily involved in the local American Indian communities, and many are tribal members themselves (Minority Nurse, 2013 ).
Students who represent the first generation in their families to enter a postsecondary institution may face challenges other students do not, and are more likely to graduate if they receive support ( Costello et al., 2018 ). Parents and significant others can be a crucial source of support ( Pritchard et al., 2020 ); socializing and educating family members about the rigors of nursing programs may facilitate their support for students. A variety of programs around the country have succeeded in increasing graduation rates among first-generation students, including pipeline programs that have successfully increased the diversity of candidates entering nursing. These programs include HRSA pipeline programs; HOSA-Future Health Professionals; and university-based programs such as the Niganawenimaanaanig program at Bemidji State University in Minnesota, created to support American Indian nursing students ( HOSA, 2012 ; HRSA, 2017 ; Wilkie, 2020 ). Federal funding is available for these types of programs from sources that include HRSA’s Health Careers Opportunity Program and Nursing Workforce Diversity Grant program. However, the need for such programs exceeds the available funding. Box 7-8 lists some of the ways in which nursing programs can support their students’ success.
Examples of Supports for Nursing Students.
Data on Quality
One important tool for recruiting a more diverse student population is providing relevant data to prospective students so they can make informed decisions about where to study. These data could include NCLEX pass rates; however, these rates alone are insufficient to determine whether a school is likely to have the resources to support a student through to graduation. Data on student retention, graduation by demographic, full cost to attend, tuition, and other quality indicators can signal to both consumers and funders whether a nursing education program has the necessary infrastructure and support to retain students from diverse backgrounds. Pass rates can be reported by race, ethnicity, socioeconomic status, first-time college/university attendees, adult learners with children living at home, and status as an English as a second language (ESL) learner to help students choose a program that best suits their needs. It is also important for schools to provide on their websites demographic information about their current enrollees. As discussed above, NCSBN identified additional quality indicators for nursing education; as these indicators begin to be measured and reported, the data can help prospective students make more informed choices.
Educational Pathways and Options
As nursing education programs adapt their curricula and other learning experiences to better address SDOH and health equity, it will be important to consider the educational pathways students may follow, both in their initial preparation and as they progress in their careers. A key way of strengthening the nursing workforce will be to encourage nurses to pursue the next level of education and certification available to them and to improve access to these educational opportunities, especially for those from underrepresented communities ( Jones et al., 2018 ; Phillips and Malone, 2014 ).
One way to improve access and encourage nurses to take the next step in their education is by offering expedited programs that allow them to complete their degree in less time. For example, there are articulation agreements, either among educational institutions or at the state or regional level, that align the content and requirements of programs. These types of agreements accelerate the RN-to-BSN and RN-to-MSN pathways and allow students to easily transfer credits between community colleges and universities ( AACN, 2019b ). There are also bridge programs available for LPNs who wish to pursue the ADN or BSN degree. Investments in articulation programs have been responsible in part for an increase in the number of employed nurses with a baccalaureate degree, from 49 percent in 2010 to 59 percent in 2019 ( Campaign for Action, n.d. ). Further progress in this area is needed, however, particularly for partnerships between baccalaureate nursing programs and academic institutions that serve underrepresented populations (e.g., tribal colleges, historically Black colleges and universities). A model of this type of partnership can be found in the New Mexico Nursing Education Consortium, 7 which coordinates prelicensure nursing curricula in 16 locations at state, tribal, and community colleges.
Nursing education can also be expedited through the use of a competency-based curriculum that allows students to progress by demonstrating the required competencies rather than meeting specific hour requirements ( U.S. Department of Education, n.d.a ). With this approach, which is currently used, for example, by Western Governors University, students can self-pace their education and potentially save time and money by learning the material quickly or tapping previous knowledge ( WGU, 2020 ). This type of educational approach may be particularly useful for nontraditional students who are entering nursing with other experiences and education. For example, a person with a background as a nursing or medical assistant may find that he or she can quickly master some of the required material for a nursing degree, particularly at the beginning. Workers from other sectors may also be able to pivot to nursing. During the COVID-19 pandemic, a study identified health care jobs, such as nursing assistant, that out-of-work hospitality workers could quickly transition to pursue ( Miller and Haley, 2020 ). While the study did not include jobs that required further education or certification, the shared skill sets that the authors identified include many skills that are central to nursing.
Another approach for increasing access to nursing education is to expand the use of distance learning opportunities. Distance learning gives students flexibility, and may be particularly beneficial for those from rural areas or other areas without a nursing school in the vicinity ( NCSBN, 2020b ). Rural areas face multiple challenges: rural populations have high rates of chronic disease and have difficulty accessing care because of provider shortages in these areas (see Chapter 2 ). Relative to their urban counterparts, rural nurses are less likely to hold a BSN ( Merrell et al., 2020 ). Distance learning has been used for many years to reach rural populations, but there are challenges with respect to regulation and ensuring the quality of education ( NCSBN, 2020a ). Efforts have been made to assess and improve the quality of distance learning; Quality Matters, for example, is an organization that provides peer-reviewed evaluation of distance or hybrid programs using a set of quality standards. 8 While many nursing programs are adhering to these standards ( Quality Matters, 2020 ), many are not, and the quality of distance learning remains uneven. The rapid rollout of distance learning during the COVID-19 pandemic has provided a unique opportunity to evaluate the effectiveness of different strategies for distance learning and to leverage this experience to expand and improve distance learning opportunities in the future.
- STRENGTHENING AND DIVERSIFYING THE NURSING FACULTY
A system of nursing education that can prepare students from diverse backgrounds to address SDOH and health equity requires a diverse faculty ( NACNEP, 2019 ; Thornton and Persaud, 2018 ). Unfortunately, the faculty currently teaching in nursing programs is overwhelmingly White and female: as of 2018, full-time faculty in nursing schools were about 93 percent female, and only 17.3 percent were from underrepresented groups, up from 11.5 percent in 2009 ( AACN, 2020c ).
In addition to this lack of diversity, the number of faculty may be inadequate to prepare the next generation of nurses: not only were there 1,637 faculty vacancies in 2019 across 892 nursing schools, but the schools surveyed hoped to create 134 new faculty positions in that year ( AACN, 2020c ). These shortages contributed to decisions to turn away more than 80,000 qualified applicants, although other insufficiencies also played a part. The AACN report cites several key reasons for faculty shortages: increasing average age of faculty members and associated increasing retirement rates, high compensation in other settings that attracts current and potential nurse educators, and an insufficient pool of graduates from master’s and doctoral programs ( AACN, 2020c ; Fang and Bednash, 2017 ). A 2020 NACNEP report calls the faculty shortage a “long-standing crisis threatening the supply, education, and training of registered nurses” and recommends federal efforts as well as a coordinated private–public response to address the shortage ( NACNEP, 2020 ).
Finally, faculty must have the knowledge, skills, and competencies to prepare their students for the challenges of advancing health equity and fully understanding the implications of SDOH for their daily practice ( NACNEP, 2019 ). If health equity and SDOH are to be integrated throughout the curriculum (as discussed earlier in this chapter), all faculty, including tenure-track faculty, clinical instructors, mentors, and preceptors, must have these competencies ( Thornton and Persaud, 2018 ). To develop these competencies, nursing schools must commit resources and support to faculty development ( Thornton and Persaud, 2018 ).
Diversifying the Faculty
As noted, diverse faculty are needed to broaden the perspectives and experiences to which nursing students are exposed and to serve as mentors and role models for diverse students ( Phillips and Malone, 2014 ). Unfortunately, minority faculty members often face barriers similar to those faced by students, including an unwelcoming environment; feeling marginalized, underappreciated, and invisible; a lack of support; feelings of tokenism; and the inability to integrate into existing faculty structures ( Beard and Julion, 2016 ; Hamilton and Haozous, 2017 ; Iheduru-Anderson, 2020 ; Kolade, 2016 ; Salvucci and Lawless, 2016 ; Whitfield-Harris and Lockhart, 2016 ). Faculty from underrepresented groups report feeling isolated, lacking in mentorship and collegial support, and burdened by having to represent the entire underrepresented community ( Kolade, 2016 ; Whitfield-Harris et al., 2017 ). In addition, as discussed in Chapter 9 , faculty from underrepresented racial and ethnic groups face a “diversity tax,” in which they are asked to be part of efforts to improve diversity and inclusion to serve on committees; mentor underrepresented students; and participate in other activities that are uncompensated, unacknowledged, and unrewarded ( Gewin, 2020 ). These demands on underrepresented faculty can lead to frustration, burnout, and a feeling that they have been given responsibility for institutional diversity ( Gewin, 2020 ).
These experiences of minority faculty can result in high attrition and low satisfaction ( Whitfield-Harris et al., 2017 ), and further research is needed on specific ways in which institutions can recruit and support a diverse faculty ( Whitfield-Harris et al., 2017 ). Proposed approaches include cultivating an inclusive educational environment ( Hamilton and Haozous, 2017 ), taking intentional action and holding open discourse to strengthen the institutional commitment to diversity ( Beard and Julion, 2016 ), improving financial assistance and mentorship opportunities for faculty ( Salvucci and Lawless, 2016 ), and conducting climate surveys to better understand the feelings and experiences of underrepresented faculty and using these data to improve the institutional culture ( DeWitty and Murray, 2020 ). The challenges these faculty face and the opportunities to address these challenges highlight the importance of efforts by schools of nursing to recruit, support, and retain diverse faculty.
Faculty Development
Collectively, nursing school faculty need to be prepared to teach their students about the complex linkages among population health, SDOH, and health outcomes ( NLN, 2019 ; Thornton and Persaud, 2018 ). To do so, as discussed above, nurse educators need to move beyond teaching abstract principles to integrating the core concepts and competencies related to these linkages into the entire learning experience across nursing education programs. They also need to create a truly inclusive and safe educational environment and prepare nurses to care for a diverse population, which, as discussed above, requires that they understand issues of racism and systems of marginalization and engage in critical self-reflection ( O’Connor et al., 2019 , Peek et al., 2020 ). Yet, many faculty in nursing schools lack the knowledge and experience needed to develop curricula and strategies for incorporating SDOH into all areas of nursing education ( NACNEP, 2019 ; Valderama-Wallace and Apesoa-Varano, 2019 ).
Several approaches are available for preparing nursing school faculty to teach content related to SDOH and health equity. One approach, discussed above, is to actively recruit more diverse faculty who reflect the nation’s population and provide different perspectives and role models for students ( The Macy Foundation, 2020 ). Another approach is to encourage the development and dissemination of evidence-based methods for teaching nursing students how they can incorporate these core concepts into nursing practice. For example, educators involved in developing innovative models of classroom and experiential learning could focus on disseminating these models with the assistance of nursing associations and organizations, including through publication, continuing education programs, or faculty-to-faculty education and mentoring. Finally, institutions can provide in-depth and sustained learning opportunities for faculty, staff, and preceptors focused on how they can support their students in learning about SDOH and health equity both within and outside of the classroom ( IOM, 2016b ). While some funding sources are available for these types of efforts, including support from private foundations and HRSA grants for faculty development, the critical importance of this content to health outcomes argues for providing more such resources.
- IMPLICATIONS OF COVID-19 FOR NURSING EDUCATION
It has been 100 years since a global event has had an impact on nursing education in the United States and around the world equal to that of the COVID-19 pandemic. Both World War I and the influenza pandemic of 1918 to 1920 led to transformations in nursing education, including standardization of training and professionalization of the field. The COVID-19 pandemic has already led to innovations that are likely to shape the future of nursing education. Faculty have adopted new teaching strategies, demonstrating creativity and adaptability, within a span of days or weeks, while such technologies as simulation-based education have quickly been adapted to replace in-person clinical hours ( Jiménez-Rodríguez et al., 2020 ). In one example of a rapid pivot, educators at the University of Pennsylvania School of Nursing transitioned a community immersion course from in-person to virtual form when all in-person classes were canceled. While they faced challenges, the educators found that students were able to remain dedicated to their community partnerships and to think creatively about how to meet their learning objectives ( Flores et al., 2020 ). These and similar innovations may ultimately guide the way to expanding and improving nursing education.
At the same time, however, the pandemic has highlighted challenges and inequities in nursing education. Simulated clinical experiences are practical only if a school and its students have access to computers with enough power to run the software, for example. While online learning has been in use for more than a decade, not all schools or faculty are prepared to deliver content in this way, nor are all students capable of accessing the necessary technology. Moreover, as practice settings have been emptied of non-COVID patients, programs have been facing multiple challenges in providing students with sufficient hours of instruction, training, and clinical practice. These challenges have underscored the limitations of traditional ways of educating nurses even as they have presented unique opportunities for innovation. To translate these short-term challenges into long-term improvements in nursing education will require
- evaluation of such practices as distance learning and virtual experiential learning to identify and disseminate best practices;
- a sense of urgency in the development of substantial changes, such as modifications of curriculum and the adoption of new technologies; and
- partnership with public- and private-sector organizations, associations, and researchers that can bring both resources and expertise to the tasks of strengthening nursing education.
- CONCLUSIONS
Currently, most nursing schools tend to cover the topics of SDOH, health equity, and population health in isolated, stand-alone courses. This approach is insufficient for creating a foundational understanding of these critical issues and for preparing nurses to work in a wide variety of settings. This content needs to be integrated and sustained throughout nursing school curricula and paired with community-based experiential opportunities whereby students can apply their knowledge, build their skills, and reflect on their experiences.
Conclusion 7-1: A curriculum embedded in coursework and experiential learning that effectively prepares students to promote health equity, reduce health disparities, and improve the health and well-being of the population will build the capacity of the nursing workforce.
Preparing nursing students to address SDOH and improve health equity will require more than didactic learning and traditional clinical experiences. It will require that students engage actively in experiences that will expand and diversify their understanding of nursing practice, prepare them to care for diverse populations with empathy, and allow them to build the necessary skills and competencies for the nursing practice of tomorrow.
Conclusion 7-2: Increasing the number of nurses with PhD degrees who focus on the connections among social determinants of health, health disparities, health equity, and overall health and well-being will build the evidence base in this area. Building capacity in schools of nursing will require financial resources, including scholarship/loan repayment opportunities; adequate numbers of expert faculty available to mentor; and curriculum revisions to focus more attention on social determinants of health and health equity.
Having more nurses prepared at the PhD level will help build the knowledge base in the nursing profession for other nurses to translate (DNPs) and use in practice settings (LPNs, RNs, APRNs).
Conclusion 7-3: Learning experiences that develop nursing students’ understanding of health equity, social determinants of health, and population health and prepare them to incorporate that understanding into their professional practice include opportunities to learn cultural humility and recognize one’s own implicit biases; gain experience with interprofessional collaboration and multisector partnerships to enable them to address social needs comprehensively and drive structural improvements; develop such technical competencies as use of telehealth, digital health tools, and data analytics; and gain substantive experience with delivering care in diverse community settings, such as public health departments, schools, libraries, workplaces, and neighborhood clinics.
Building a diverse nursing workforce is a critical component of the effort to prepare nurses to address SDOH and health equity. While the nursing workforce has steadily grown more diverse, nursing schools need to continue and expand their efforts to recruit, support, and mentor diverse students.
Conclusion 7-4: Successfully diversifying the nursing workforce will depend on holistic efforts to support and mentor/sponsor students and faculty from a wide range of backgrounds, including cultivating an inclusive environment; providing economic, social, professional, and academic supports; ensuring access to information on school quality; and minimizing inequities.
- Aaberg VA. A path to greater inclusivity through understanding implicit attitudes toward disability. Journal of Nursing Education. 2012; 51 (9):505–510. [ PubMed : 22766074 ]
- AAC&U (Association of American Colleges & Universities). Majority of college students experience food insecurity, housing insecurity, or homelessness. 2019. [March 29, 2021]. https://www .aacu.org /aacu-news/newsletter /majority-college-students-experience-food-insecurity-housing-insecurity-or .
- AACN (American Association of Colleges of Nursing). The essentials of doctoral education for advanced nursing practice. Washington, DC: American Association of Colleges of Nursing; 2006.
- AACN. The essentials of master’s education in nursing. 2011. [July 6, 2021]. https://www .aacnnursing .org/portals/42/publications /mastersessentials11.pdf .
- AACN. 2018–2019 enrollment and graduations in baccalaureate and graduate programs in nursing. Washington, DC: American Association of Colleges of Nursing; 2019a.
- AACN. Articulation agreements among nursing education programs. 2019b. [January 25, 2021]. https://www .aacnnursing .org/News-Information /Fact-Sheets/Articulation-Agreements .
- AACN. 2020a. [January 8, 2021]. 2019–2020 enrollment and graduations in baccalaureate and graduate programs in nursing. https://www .aacnnursing .org/Store/product-info /productcd/IDSR_20ENROLLBACC .
- AACN. Essentials task force. 2020b. [May 18, 2020]. https://www .aacnnursing .org/About-AACN/AACNGovernance /Committees-and-Task-Forces/Essentials .
- AACN. Nursing faculty. 2020c. [March 9, 2021]. https://www .aacnnursing .org/news-information /fact-sheets/nursing-faculty-shortage .
- AACN. Curriculum improvement. 2020c. [January 25, 2021]. https://www .aacnnursing .org/Population-Health-Nursing /Curriculum-Improvement .
- AACN. Promising practices in holistic admissions review: Implementation in academic nursing. 2020d. [January 25, 2021]. https://www .aacnnursing .org/Portals/42/News /White-Papers/AACN-White-Paper-PromisingPractices-in-Holistic-Admissions-Review-December-2020.pdf .
- AACN. Diversity & inclusion offerings. [April 23, 2020]. n.d. https://www .aacnnursing .org/Diversity-Inclusion /HolisticAdmissions /Diversity-and-Inclusion-Offerings .
- AAPCHO (Association of Asian Pacific Community Health Organizations). Pipeline programs to improve racial and ethnic diversity in the health professions. 2009. [June 2, 2021]. https://www .aapcho.org /wp/wp-content/uploads /2012/11/PipelineToImproveDiversityInHealthProfessions .pdf .
- AARP. Preparation and roles of nursing care providers in America. 2010. [October 28, 2020]. http: //championnursing .org/resources/preparation-and-roles-nursing-care-providers-america .
- Ackerman-Barger K, Boatright D, Gonzalez-Colaso R, Orozco R, Latimore D. Seeking inclusion excellence: Understanding racial microaggressions as experienced by underrepresented medical and nursing students. Academic Medicine. 2020; 95 (5):758–763. [ PMC free article : PMC7185051 ] [ PubMed : 31725462 ]
- Advisory Committee on Student Financial Assistance. Federal Register. 2013; 78 (152) [June 2, 2021]; https://fsapartners .ed .gov/sites/default /files/attachments/fregisters /FR080713AdvisoryCommitteeonStudentFinancialAssistance.pdf .
- Agner J. Moving from cultural competence to cultural humility in occupational therapy: A paradigm shift. American Journal of Occupational Therapy. 2020; 74 (4):7404347010. [ PubMed : 32602456 ]
- AHA (American Hospital Association). Screening for social needs: Guiding care teams to engage patients. 2019. [November 11, 2020]. https://www .aha.org/system /files/media/file /2019/09/screening-for-social-needstool-value-initiative-rev-9-26-2019.pdf .
- Aiken LH, Sloane D, Griffiths P, Rafferty AM, Bruyneel L, McHugh M, Maier CB, Moreno-Casbas T, Ball JE, Ausserhofer D, Sermeus W. Nursing skill mix in European hospitals: Cross-sectional study of the association with mortality, patient ratings, and quality of care. BMJ Quality & Safety. 2017; 26 (7):559–568. [ PMC free article : PMC5477662 ] [ PubMed : 28626086 ]
- Alleghany College of Maryland. Nurse managed wellness clinic. 2020. [June 2, 2021]. https://www .allegany .edu/health-clinics/nurse-managed-wellness-clinic .
- Allen J. Improving cross-cultural care and antiracism in nursing education: A literature review. Nurse Education Today. 2010; 30 (4):314–320. [ PubMed : 19758731 ]
- Arcaya MC, Figueroa JF. Emerging trends could exacerbate health inequities in the United States. Health Affairs (Millwood). 2017; 36 (6):992–998. [ PubMed : 28583956 ]
- Artinian NT, Drees BM, Glazer G, Harris K, Kaufman LS, Lopez N, Danek JC, Michaels J. Holistic admissions in the health professions: Strategies for leaders. College & University. 2017; 92 (2):65–68. [ PMC free article : PMC5708588 ] [ PubMed : 29200468 ]
- Baker C, Cary AH, da Conceicao Bento M. Global standards for professional nursing education: The time is now. Journal of Professional Nursing. 2020; 37 (1):86–92. doi: 10.1016/j.profnurs.2020.10.001. [ PMC free article : PMC7571445 ] [ PubMed : 33674114 ]
- Bandy J. Vanderbilt University Center for Teaching. 2011. [March 29, 2021]. What is service learning or community engagement? https://cft .vanderbilt .edu/guides-sub-pages /teaching-through-community-engagement .
- Banister G, Bowen-Brady HM, Winfrey ME. Using career nurse mentors to support minority nursing students and facilitate their transition to practice. Journal of Professional Nursing. 2014; 30 (4):317–325. [ PubMed : 25150417 ]
- Barton AJ, Murray TA, Spurlock DR Jr. An open letter to members of the nursing education community. Journal of Nursing Education. 2020; 59 (4):183. [ PubMed : 32243547 ]
- Batra S, Orban J. Oral presentation at the National Center for Interprofessional Education and Practice NEXUS Summit 2020, October 15, 2020, Virtual. 2020. Social mission and accreditation standards.
- Beard KV. How much diversity in nursing is enough? American Journal of Nursing. 2014; 114 (9):11. [ PubMed : 25166226 ]
- Beard KV, Julion WA. Does race still matter in nursing? The narratives of African-American nursing faculty members. Nursing Outlook. 2016; 64 :583–596. https://doi .org/10.1016/j .outlook.2016.06.005 . PMID:27432213. [ PubMed : 27432213 ]
- Bednash G, Breslin ET, Kirschling JM, Rosseter RJ. PhD or DNP: Planning for doctoral nursing education. Nursing Science Quarterly. 2014; 27 (4):296–301. [ PubMed : 25248773 ]
- Befus DR, Kumodzi T, Schminkey D, Ivany AS. Advancing health equity and social justice in forensic nursing research, education, practice, and policy: Introducing structural violence and trauma-and violence-informed care. Journal of Forensic Nursing. 2019; 15 (4):199–205. [ PubMed : 31764523 ]
- Bestsennyy O, Gilbert G, Harris A, Rost J. Telehealth: A quarter-trillion-dollar post-COVID-19 reality? 2020. [February 24, 2021]. https://www .mckinsey .com/industries/healthcare-systems-and-services /our-insights /telehealth-a-quarter-trillion-dollar-post-covid-19-reality .
- Bjørk IT, Berntsen K, Brynildsen G, Hestetun M. Nursing students’ perceptions of their clinical learning environment in placements outside traditional hospital settings. Journal of Clinical Nursing. 2014; 23 (19–20):2958–2967. [ PMC free article : PMC4263152 ] [ PubMed : 24460862 ]
- Blair IV, Steiner JF, Havranek EP. Unconscious (implicit) bias and health disparities: Where do we go from here? The Permanente Journal. 2011; 15 (2):71–78. PMID: 21841929. [ PMC free article : PMC3140753 ] [ PubMed : 21841929 ]
- Breen N, Jackson JS, Wood F, Wong D, Zhang X. Translational health disparities research in a data-rich world. American Journal of Public Health. 2019; 109 (S1):S41–S42. [ PMC free article : PMC6356140 ] [ PubMed : 30699034 ]
- Brennan AMW, Barnsteiner J, Siantz ML, Cotter VT, Everett J. Lesbian, gay, bisexual, transgendered, or intersexed content for nursing curricula. Journal of Professional Nursing. 2012; 28 (2):96–104. [ PubMed : 22459139 ]
- Breslin ET, Nuri-Robins K, Ash J, Kirschling JM. The changing face of academic nursing: Nurturing diversity, inclusivity, and equity. Journal of Professional Nursing. 2018; 34 (2):103–109. [ PubMed : 29703311 ]
- Bresnick J. Health IT Analytics. 2017. [November 11, 2020]. Understanding the basics of clinical decision support systems. https: //healthitanalytics .com/features/understanding-the-basics-of-clinical-decision-support-systems .
- Brookings Institution. Black-White disparity in student loan debt more than triples after graduation. 2016. [November 11, 2020]. https://www .brookings .edu/research/black-white-disparity-in-student-loan-debt-more-than-triples-after-graduation .
- Broome ME, Fairman J. Changing the conversation about doctoral education in nursing. Nursing Outlook. 2018; 66 (2018):217–218. [ PubMed : 29887188 ]
- Buhler-Wilkerson K. Bringing care to the people: Lillian Wald’s legacy to public health nursing. American Journal of Public Health. 1993; 83 (12):1778–1786. [ PMC free article : PMC1694935 ] [ PubMed : 7695663 ]
- Burnett A, Moorley C, Grant J, Kahin M, Sagoo R, Rivers E, Deravin L, Darbyshire P. Dismantling racism in education: In 2020, the year of the nurse & midwife, “it’s time” Nurse Education Today. 2020; 93 :104532. https://doi .org/10.1016/j .nedt.2020.104532 . [ PMC free article : PMC7354251 ] [ PubMed : 32683224 ]
- Campaign for Action. New RN graduates by degree type, by gender. 2019a. [May 13, 2020]. https: //campaignforaction .org/resource/new-rn-graduates-degree-type-gender .
- Campaign for Action. Nursing education and the path to population health improvement. 2019b. [March 13, 2020]. https: //campaignforaction .org/wp-content /uploads/2019/03/NursingEducationPathtoHealthImprovement.pdf .
- Campaign for Action. Campaign for Action dashboard. 2020. [May 14, 2020]. https: //campaignforaction .org/wpcontent/uploads /2019/07/r2_CCNA-0029 _2019-Dashboard-Indicator-Updates_1-29-20.pdf .
- Campaign for Action. Transforming nursing education. [May 14, 2020]. n.d. https: //campaignforaction .org/issue/transforming-nursing-education .
- Campinha-Bacote J. Cultural competemility: A paradigm shift in the cultural competence versus cultural humility debate—part I. The Online Journal of Issues in Nursing. 2018; 24 (1)
- Castro-Sánchez E, Russell AM, Dolman L, Wells M. International Nursing Review. 2021. What place does nurse-led research have in the COVID-19 pandemic? pp. 1–5. [ PMC free article : PMC8013712 ] [ PubMed : 33565619 ]
- CCNE (Commission on Collegiate Nursing Education). Standards for accreditation of baccalaureate and graduate nursing programs. 2018. [September 29, 2020]. https://www .aacnnursing .org/Portals/42/CCNE /PDF/Standards-Final-2018.pdf .
- CDC (Centers for Disease Control and Prevention). Health care provider/clinician apps. 2018. [November 11, 2020]. https://www .cdc.gov/mobile /healthcareproviderapps.html .
- Center for Health Affairs. LPNs crucial to nursing workforce diversity. 2018. [May 14, 2020]. https: //neohospitals .org/TheCenterForHealthAffairs /MediaCenter /NewsReleases/2018 /August/Nursing-WorkforceDiversity .
- Cho I, Kim E, Choi WH, Staggers N. Comparing usability testing outcomes and functions of six electronic nursing record systems. International Journal of Medical Informatics. 2016; 88 :78–85. [ PubMed : 26878766 ]
- Costello M, Ballin A, Diamond R, Gao ML. First generation college students and non-first generation college students: Perceptions of belonging. Journal of Nursing Education and Practice. 2018; 8 (12):59–65.
- Devine PG, Forscher PS, Austin AJ, Cox WT. Long-term reduction in implicit race bias: A prejudice habit-breaking intervention. Journal of Experimental Social Psychology. 2012; 48 (6):1267–1278. https://doi .org/10.1016/j .jesp.2012.06.003 . [ PMC free article : PMC3603687 ] [ PubMed : 23524616 ]
- DeWitty VP. What is holistic admissions review, and why does it matter? Journal of Nursing Education. 2018; 57 (4):195–196. [ PubMed : 29614186 ]
- DeWitty VP, Murray TA. Influence of climate and culture on minority faculty retention. Journal of Nursing Education. 2020; 59 (9):483–484. [ PubMed : 32865579 ]
- DiAngelo R. White fragility. International Journal of Critical Pedagogy. 2011; 3 (3):54–71.
- DiAngelo RJ. White fragility: Why it’s so hard for White people to talk about racism. Boston, MA: Beacon Press; 2018.
- Diefenbeck C, Michalec B, Alexander R. Lived experiences of racially and ethnically underrepresented minority BSN students: A case study specifically exploring issues related to recruitment and retention. Nursing Education Perspectives. 2016; 37 (1):41–44. [ PubMed : 27164777 ]
- Duffy MT, Friesen MA, Speroni KG, Swengros D, Shanks LA, Waiter PA, Sheridan MJ. BSN completion barriers, challenges, incentives, and strategies. The Journal of Nursing Administration. 2014; 44 (4):232–236. [ PubMed : 24662693 ]
- Effland KJ, Hays K, Ortiz FM, Blanco BA. Incorporating an equity agenda into health professions education and training to build a more representative workforce. Journal of Midwifery & Women’s Health. 2020; 65 (1):149–159. [ PubMed : 31957220 ]
- El-Sayed M, El-Sayed J. Achieving lifelong learning outcomes in professional degree programs. International Journal of Process Education. 2014; 6 (1):37–42.
- Fairman JA, Giordano NA, McCauley K, Villaruel A. Invitational summit: Re-envisioning research focused PHD programs of the future. Journal of Professional Nursing. 2020; 37 doi: 10.1016/j.profnurs.2020.09.004. [ PubMed : 33674099 ]
- Fang D, Bednash GD. Identifying barriers and facilitators to future nurse faculty careers for DNP students. Journal of Professional Nursing. 2017; 33 (1):56–67. doi: 10.1016/j.profnurs.2016.05.008. [ PubMed : 28131149 ]
- FDA (U.S. Food and Drug Administration). Digital health. 2020. [May 14, 2020]. https://www .fda.gov/medicaldevices /digital-health .
- Fee E, Bu L. The origins of public health nursing: The Henry Street Visiting Nurse Service. American Journal of Public Health. 2010; 100 (7):1206–1207. [ PMC free article : PMC2882394 ] [ PubMed : 20466947 ]
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: A systematic review. BMC Medical Ethics. 2017; 18 (1):19. [ PMC free article : PMC5333436 ] [ PubMed : 28249596 ]
- Flores DD, Bocage C, Devlin S, Miller M, Savarino A, Lipman TH. Pedagogy in Health Promotion. Epub October 16, 2020. 2020. [November 11, 2020]. When community immersion becomes distance learning: Lessons learned from a disrupted semester. https://journals .sagepub .com/doi/pdf/10.1177 /2373379920963596 .
- Forman TM, Armor DA, Miller AS. A review of clinical informatics competencies in nursing to inform best practices in education and nurse faculty development. Nursing Education Perspectives. 2020; 41 (1):E3–E7. [ PubMed : 31860501 ]
- Foronda C, Liu S, Bauman EB. Evaluation of simulation in undergraduate nurse education: An integrative review. Clinical Simulation in Nursing. 2013; 9 (10):E409–E416.
- Foronda C, Baptiste DL, Reinholdt MM, Ousman K. Cultural humility: A concept analysis. Journal of Transcultural Nursing. 2016; 27 (3):210–217. [ PubMed : 26122618 ]
- Foronda CL, Baptiste DL, Pfaff T, Velez R, Reinholdt M, Sanchez M, Hudson KW. Cultural competency and cultural humility in simulation-based education: An integrative review. Clinical Simulation in Nursing. 2018; 15 :42–60.
- Gaines K. Why nursing school accreditation matters. [April 30, 2020]. n.d. https://nurse .org/education /nursing-school-accreditation .
- Gallagher RW, Polanin JR. A meta-analysis of educational interventions designed to enhance cultural competence in professional nurses and nursing students. Nurse Education Today. 2015; 35 (2):333–340. [ PubMed : 25466790 ]
- Gewin V. The time tax put on scientists of colour. Nature. 2020; 583 :479–481. [ PubMed : 32647354 ]
- Giddens JF. Changing paradigms and challenging assumptions: Redefining quality and NCLEX-RN pass rates. Journal of Nursing Education. 2009; 48 (3):123–124. [ PubMed : 19297961 ]
- Giovenco DP, Spillane TE. Improving efficiency in mobile data collection for place-based public health research. American Journal of Public Health. 2019; 109 (S2):S123–S125. [ PMC free article : PMC6383969 ] [ PubMed : 30785801 ]
- Glazer G, Clark A, Bankston K. Holistic admissions in nursing: We can do this. Journal of Professional Nursing. 2016; 32 (4) [ PMC free article : PMC4955639 ] [ PubMed : 27424931 ]
- Glazer G, Tobias B, Mentzel T. Increasing healthcare workforce diversity: Urban universities as catalysts for change. Journal of Professional Nursing. 2018; 34 (4):306–313. [ PMC free article : PMC6069531 ] [ PubMed : 30055674 ]
- Graham CL, Phillips SM, Newman SD, Atz TW. Baccalaureate minority nursing students perceived barriers and facilitators to clinical education practices: An integrative review. Nursing Education Perspectives. 2016; 37 (3):130–137. [ PubMed : 27405193 ]
- Greene MZ, FitzPatrick MK, Romano J, Aiken LH, Richmond TS. Clinical fellowship for an innovative, integrated BSN-PhD program: An academic and practice partnership. Journal of Professional Nursing. 2017; 33 (4):282–286. [ PMC free article : PMC5523847 ] [ PubMed : 28734488 ]
- Hamilton N, Haozous EA. Retention of faculty of color in academic nursing. Nursing Outlook. 2017; 65 (2):212–221. https://doi .org/10.1016/j .outlook.2016.11.003 . PMID: 28087139. [ PubMed : 28087139 ]
- Hayden J, Smiley R, Alexander M, Kardong-Edgren S, Jeffries P. The NCSBN national simulation study: A longitudinal, randomized, controlled study replacing clinical hours with simulation in prelicensure nursing education. Journal of Nursing Regulation. 2014; 5 (2S):S1–S64.
- Heath S. Health IT Analytics. 2019. [April 21, 2021]. Top considerations for SDOH screening, referral technologies. https: //patientengagementhit .com/news/top-considerations-for-sdoh-screening-referral-technologies .
- Hermer J, Hirsch A, Bekemeier B, Nyirati C, Wojnar D, Wild L, Oneal G. Integrating population health into nursing education: The process of gaining commitment from Washington’s nursing deans and directors. Journal of Professional Nursing. 2020; 36 (2):6–12. [ PubMed : 32204862 ]
- Higgins LW, Shovel JA, Bilderback AL, Lorenz HL, Martin SC, Rogers DJ, Minnier TE. Hospital nurses’ work activity in a technology-rich environment: A triangulated quality improvement assessment. Journal of Nursing Care Quality. 2017; 32 (3):208–217. [ PubMed : 28541263 ]
- Horn C. University of South Carolina. 2020. [April 28, 2021]. COVID-19 response: Virtual simulation keeps nursing students on track for graduation. https://www .sc.edu/uofsc /posts/2020/04/covid _resilience_virtual _simulation_nursing.php#.X5S1e0JKjfY .
- HOSA (Future Health Professionals/Health Occupations Students of America). About HOSA. 2012. [March 30, 2020]. http://www .hosa.org/about .
- HRSA (Health Resources and Services Administration). Health careers pipeline and diversity programs. 2017. [April 30, 2020]. https://bhw .hrsa.gov /sites/default/files /bhw/health-workforce-analysis /programhighlights /diversity-and-pipeline-training-programs-2017.pdf .
- HRSA. Strategic plan FY 2019–2022. 2019. [April 30, 2020]. https://www .hrsa.gov /about/strategic-plan/index.html .
- HRSA. 2018 national sample survey of registered nurses. 2020. [April 30, 2020]. https://data .hrsa.gov /DataDownload/NSSRN /GeneralPUF18/2018_NSSRN _Summary_Report-508.pdf .
- HRSA. HRSA National Health Service Corps. 2021. [March 29, 2021]. NHSC loan repayment program. https://nhsc .hrsa.gov /loan-repayment/nhsc-loan-repayment-program.html .
- Ibrahim SA, Charlson ME, Neill DB. Health Equity I. 1. 2020. Big data analytics and the struggle for equity in health care: The promise and perils; pp. 99–101. [ PMC free article : PMC7133425 ] [ PubMed : 32258961 ]
- Iheduru-Anderson KC. Journal of Professional Nursing. 2020. The White/Black hierarchy institutionalizes White supremacy in nursing and nursing leadership in the United States. Advance online publication. https://doi .org/10.1016/j .profnurs.2020.05.005 . [ PubMed : 33867099 ]
- Iheduru-Anderson KC, Wahi MM. Prevention of lateral violence in nursing through education: The bullying awareness seminar. The Journal of Nursing Education. 2017; 56 (12):762–763. [ PubMed : 29206270 ]
- IOM (Institute of Medicine). Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press; 2003. [ PubMed : 25032386 ]
- IOM. Redesigning continuing education in the health professions. Washington, DC: The National Academies Press; 2010. [ PubMed : 25032352 ]
- IOM. The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press; 2011. [ PubMed : 24983041 ]
- IOM. Interprofessional education for collaboration: Learning how to improve health from interprofessional models across the continuum of education to practice: Workshop summary. Washington, DC: The National Academies Press; 2013. [ PubMed : 24901189 ]
- IOM. Assessing progress on the Institute of Medicine report The Future of Nursing. Washington, DC: The National Academies Press; 2016a. [ PubMed : 27010049 ]
- IOM. A framework for educating health professionals to address the social determinants of health. Washington, DC: The National Academies Press; 2016b. [ PubMed : 27854400 ]
- IPEC (Interprofessional Education Collaborative). Core competencies for interprofessional collaborative practice: 2016 update. Washington, DC: Interprofessional Education Collaborative; 2016. [June 2, 2021]. https://ipec .memberclicks .net/assets/2016-Update.pdf .
- Jamshidi N, Molazem Z, Sharif F, Torabizadeh C, Najafi Kalyani M. The challenges of nursing students in the clinical learning environment: A qualitative study. Scientific World Journal. 2016; 2016 :1846178. [ PMC free article : PMC4913003 ] [ PubMed : 27366787 ]
- Jiménez-Rodríguez D, Torres Navarro MDM, Plaza Del Pino FJ, Arrogante O. Simulated nursing video consultations: An innovative proposal during COVID-19 confinement. Clinical Simulation of Nursing. 2020; 48 :29–37. doi: 10.1016/j.ecns.2020.08.004. [ PMC free article : PMC7425773 ] [ PubMed : 32837633 ]
- Johansson P, Jones DE, Watkins CC, Haisfield-Wolfe ME, Gaston-Johansson F. Physicians’ and nurses’ experiences of the influence of race and ethnicity on the quality of healthcare provided to minority patients, and on their own professional careers. Journal of National Black Nurses Association. 2011; 22 (1):43–56. [ PubMed : 21888150 ]
- Jones CB, Toles M, Knafl GJ, Beeber AS. An untapped resource in the nursing workforce: Licensed practical nurses who transition to become registered nurses. Nursing Outlook. 2018; 66 (1):46–55. [ PubMed : 29306576 ]
- Permanente Kaiser. Kaiser Permanente launches social health network to address needs on a broad scale. 2019. [November 11, 2020]. https://permanente .org /kaiser-permanente-launches-social-health-network-to-address-needs-on-a-broad-scale .
- Kamau-Small S, Joyce B, Bermingham N, Roberts J, Robbins C. The impact of the care equity project with community/public health nursing students. Public Health Nursing. 2015; 32 (2):169–176. [ PubMed : 24850360 ]
- Katz JR, Barbosa-Leiker C, Benavides-Vaello S. Measuring the success of a pipeline program to increase nursing workforce diversity. Journal of Professional Nursing. 2016; 32 (1):6–14. [ PMC free article : PMC4724384 ] [ PubMed : 26802586 ]
- Kleinman A, Benson P. Anthropology in the clinic: The problem of cultural competency and how to fix it. PLoS Medicine. 2006; 3 (10) [ PMC free article : PMC1621088 ] [ PubMed : 17076546 ]
- Kolade FM. The lived experience of minority nursing faculty: A phenomenological study. Journal of Professional Nursing. 2016; 32 (2):107–114. https://doi .org/10.1016/j .profnurs.2015.09.002 . [ PubMed : 27000195 ]
- Kononowicz AA, Woodham LA, Edelbring S, Stathakarou N, Davies D, Saxena N, Tudor Car L, Carlstedt-Duke J, Car J, Zary N. Virtual patient simulations in health professions education: Systematic review and meta-analysis by the digital health education collaboration. Journal of Medical Internet Research. 2019; 21 (7):e14676. https://doi .org/10.2196/14676 . [ PMC free article : PMC6632099 ] [ PubMed : 31267981 ]
- Koschmann KS, Jeffers NK, Heidari O. “I can’t breathe”: A call for antiracist nursing practice. Nursing Outlook. 2020; 68 (5):539–541. doi: 10.1016/j.outlook.2020.07.004. [ PMC free article : PMC7428668 ] [ PubMed : 32811661 ]
- Kumm S, Godfrey N, Martin D, Tucci M, Muenks M, Spaeth T. Baccalaureate outcomes met by associate degree nursing programs 2014. Nurse Education. 2014; 39 (5):216–220. PMID: 24978014. doi: 10.1097/NNE.0000000000000060. [ PubMed : 24978014 ]
- Lake ET. How effective response to COVID-19 relies on nursing research. Research in Nursing and Health. 2020; 43 (3):213–214. [ PMC free article : PMC7264727 ] [ PubMed : 32306403 ]
- Larsen R, Reif L, Frauendienst R. Baccalaureate nursing students’ intention to choose a public health career. Public Health Nursing. 2012; 29 :424–432. https://doi .org/10.1111/j .1525-1446.2012.01031.x . [ PubMed : 22924565 ]
- Laternman The New York Times. May 2, 2019. [March 29, 2021]. Tuition or dinner? Nearly half of college students surveyed in a new report are going hungry. https://www .nytimes.com /2019/05/02/nyregion /hunger-college-food-insecurity.html .
- LCME (Liaison Committee on Medical Education). Functions and structure of a medical school: Standards for accreditation of medical education programs leading to the MD degree. 2018. [November 16, 2020]. http://lcme .org/wp-content /uploads/filebase /standards/2019-20 _Functions-and-Structure_2018-09-26 .docx .
- Levine S, Varcoe C, Browne AJ. “We went as a team closer to the truth”: Impacts of interprofessional education on trauma-and violence-informed care for staff in primary care settings. Journal of Interprofessional Care. 2020; 35 (1):46–54. [ PubMed : 31928247 ]
- Lewis and Clark Community College. Lewis and Clark mobile health unit. [February 21, 2021]. n.d. https://www .lc.edu/Mobile_Clinics .
- Lim F, Johnson M, Eliason M. A national survey of faculty knowledge, experience, and readiness for teaching lesbian, gay, bisexual, and transgender health in baccalaureate nursing programs. Nursing Education Perspectives. 2015; 36 :144–152.
- Linden MA, Redpath SJ. A comparative study of nursing attitudes towards young male survivors of brain injury: A questionnaire survey. International Journal of Nursing Studies. 2011; 48 (1):62–69. [ PubMed : 20965077 ]
- Loftin C, Newman SD, Dumas BP, Gilden G, Bond ML. Perceived barriers to success for minority nursing students: An integrative review. International Scholarly Research Network Nursing. 2012; 2012 :806543. [ PMC free article : PMC3369480 ] [ PubMed : 22701183 ]
- Love R, Carrington JM. Journal of the American Association of Nurse Practitioners. 2020. Introducing telehealth skills into the doctor of nursing practice curriculum. Epub ahead of print. doi: 10.1097/JXX.0000000000000505. [ PubMed : 33038114 ]
- Mann K, Gordon J, MacLeod A. Reflection and reflective practice in health professions education: A systematic review. Advances in Health Sciences Education Theory and Practice. 2009; 14 (4):595–621. [ PubMed : 18034364 ]
- Marion-Martins AD, Pinho DLM. Interprofessional simulation effects for healthcare students: A systematic review and meta-analysis. Nurse Education Today. 2020; 94 :104568. [ PubMed : 32932058 ]
- Marken PA, Zimmerman C, Kennedy C, Schremmer R, Smith K. Human simulators and standardized patients to teach difficult conversations to interprofessional health care teams. American Journal of Pharmaceutical Education. 2010; 74 (7):120. [ PMC free article : PMC2972514 ] [ PubMed : 21088725 ]
- Massachusetts Department of Higher Education Nursing Initiative. Massachusetts nursing of the future nursing core competencies. 2016. [January 12, 2021]. https://www .mass.edu /nahi/documents/NOFRNCompetencies _updated_March2016.pdf .
- McCue PL. Open Access Dissertations. 2017. The pre-collegiate pipeline to diversify the nursing workforce. Paper 575.
- McMenamin P. ANA Community blog. 2015. [June 2, 2021]. Diversity among registered nurses: Slow but steady progress. https://community .ana .org/blogs/peter-mcmenamin /2015/08/21/rn-diversity-note?ssopc=1 .
- Menzel N, Willson LH, Doolen J. International Journal of Nursing Education Scholarship. 11. 2014. Effectiveness of a poverty simulation in Second Life®: Changing nursing student attitudes toward poor people; p. 11. doi: 10.1515/ijnes-2013-0076. [ PubMed : 24615491 ]
- Merrell M, Probst J, Crouch E, Abshire D, McKinney S, Haynes E. A national survey of RN-to-BSN programs: Are they reaching rural students? Journal of Nursing Education. 2020; 59 (10):557–565. [ PMC free article : PMC8641547 ] [ PubMed : 33002161 ]
- Metzger M, Taggart J. A longitudinal mixed methods study describing 4th year baccalaureate nursing students’ perceptions of inclusive pedagogical strategies. Journal of Professional Nursing. 2020; 36 (4):229–235. [ PubMed : 32819549 ]
- Metzger M, Dowling T, Guinn J, Wilson DT. Inclusivity in baccalaureate nursing education: A scoping study. Journal of Professional Nursing. 2020; 36 (1):5–14. [ PubMed : 32044053 ]
- Miller S, Haley P. Federal Reserve Bank of Atlanta. 2020. [February 24, 2021]. Transitioning from hospitality to health care occupations. https://www .frbatlanta .org/cweo/workforce-currents /2020/08/28 /transitioning-from-hospitality-to-health-care-occupations .
- Minority Nurse. Mentors to the max. 2013. [November 11, 2020]. https: //minoritynurse .com/mentors-to-the-max .
- Morton JL, Weierbach FM, Sutter R, Livsey K, Goehner E, Liesveld J, Goldschmidt MK. New education models for preparing pre-licensure students for community-based practice. Journal of Professional Nursing. 2019; 35 (6):491–498. [ PubMed : 31857060 ]
- Mosher DK, Hook JN, Captari LE, Davis DE, DeBlaere C, Owen J. Cultural humility: A therapeutic framework for engaging diverse clients. Practice Innovations. 2017; 2 (4):221.
- Murray TA, Pole DC, Ciarlo EM, Holmes S. A nursing workforce diversity project: Strategies for recruitment, retention, graduation, and NCLEX-RN success. Nursing Education Perspectives. 2016; 37 (3):138–143. PMID: 27405194. [ PubMed : 27405194 ]
- NACNEP (National Advisory Council on Nurse Education and Practice). Preparing nurses for new roles in population health management. 2016. [May 15, 2020]. https://www .hrsa.gov /sites/default/files /hrsa/advisory-committees /nursing/reports /2016-fourteenthreport.pdf .
- NACNEP. Integration of social determinants of health in nursing education, practice, and research. 2019. [March 29, 2021]. https://www .hrsa.gov /sites/default/files /hrsa/advisory-committees /nursing/reports /nacnep-2019-sixteenthreport.pdf .
- NACNEP. Preparing nurse faculty, and addressing the shortage of nurse faculty and clinical preceptors. 2020. [March 29, 2021]. https://www .hrsa.gov /sites/default/files /hrsa/advisory-committees /nursing/reports /nacnep-17report-2021.pdf .
- NASEM (National Academies of Sciences, Engineering, and Medicine). Big data and analytics for infectious disease research, operations, and policy: Proceedings of a workshop. Washington, DC: The National Academies Press; 2016a. [ PubMed : 27977088 ]
- NASEM. Developing a national STEM workforce strategy: A workshop summary. Washington, DC: The National Academies Press; 2016b.
- NASEM. Communities in action: Pathways to health equity. Washington, DC: The National Academies Press; 2017. [ PubMed : 28418632 ]
- NASEM. Proceedings of a workshop. Washington, DC: The National Academies Press; 2018a. Exploring a business case for high-value continuing professional development: [ PubMed : 29757596 ]
- NASEM. How people learn II: Learners, contexts, and cultures. Washington, DC: The National Academies Press; 2018b.
- NASEM. Improving health professional education and practice through technology: Proceedings of a workshop. Washington, DC: The National Academies Press; 2018c. [ PubMed : 30407779 ]
- NASEM. Integrating social care into the delivery of health care: Moving upstream to improve the nation’s health. Washington, DC: The National Academies Press; 2019. [ PubMed : 31940159 ]
- NCDHHS (North Carolina Department of Health and Human Services). North Carolina health atlas. 2020. [November 11, 2020]. https://schs .dph.ncdhhs.gov/data/hsa .
- NCSBN (National Council of State Boards of Nursing). NCLEX-RN examination. 2019. [May 1, 2020]. https://www .ncsbn.org /2019_RN_TestPlan-English.pdf .
- NCSBN. Number of candidates taking NCLEX examination and percent passing, by type of candidate. 2020a. [May 1, 2020]. https://www .ncsbn.org /Table_of_Pass_Rates_2019_Q4.pdf .
- NCSBN. Distance education. 2020b. [November 11, 2020]. https://www .ncsbn.org/6662.htm .
- NEJM (New England Journal of Medicine) Catalyst. Healthcare big data and the promise of value-based care. 2018. [November 11, 2020]. https://catalyst .nejm .org/doi/full/10.1056/CAT.18.0290 .
- New York State. Leading the way to college affordability. [May 15, 2020]. n.d. https://www .ny.gov/programs /tuition-free-degree-program-excelsior-scholarship .
- NLN (National League for Nursing). Interprofessional education and healthcare simulation symposium. 2013. [February 24, 2021]. http://www .nln.org/docs /default-source/professional-development-programs /white-papersymposium-ipe-in-healthcare-simulation-2013-(pdf) .pdf?sfvrsn=0 .
- NLN. A diving Document from the National League for Nursing NLN Board of Governors. 2015a. [January 25, 2021]. A vision for the changing faculty role: Preparing students for the technological world of health care. http://www .nln.org/docs /default-source/about /nln-vision-series- %28position-statements%29 /nlnvision_8.pdf?sfvrsn=4 . [ PubMed : 29194143 ]
- NLN. Interprofessional collaboration in education and practice. 2015b. [January 25, 2021]. http://www .nln.org/docs /default-source/default-document-library/ipe-ipp-vision .pdf?sfvrsn=14 .
- NLN. Accreditation standards for nursing education programs. 2016. [January 10, 2020]. http://www .nln.org/docs /default-source/accreditation-services /cnea-standards-final-february-201613f2bf5c78366c709642ff00005f0421 .pdf?sfvrsn=12 .
- NLN. A vision for integration of the social determinants of health into nursing education curricula. 2019. [January 10, 2020]. http://www .nln.org/docs /default-source/default-document-library /social-determinantsof-health .pdf?sfvrsn=2 . [ PubMed : 31644458 ]
- NONPF (National Organization of Nurse Practitioner Faculties). NONPF supports telehealth in nurse practitioner education 2018. 2018. [January 18, 2020]. https://cdn .ymaws.com/www .nonpf.org/resource /resmgr/2018_Slate /Telehealth_Paper_2018.pdf .
- NYSIM (City University of New York Grossman School of Medicine). NYSIM Center. 2017. [May 18, 2020]. http://nysimcenter .org .
- O’Connor MR, Barrington WE, Buchanan DT, Bustillos D, Eagen-Torkko M, Kalkbrenner A, de Castro AB. Short-term outcomes of a diversity, equity, and inclusion institute for nursing faculty. Journal of Nursing Education. 2019; 58 (11):633–640. [ PubMed : 31665527 ]
- O’Lynn C. Rethinking indicators of academic quality in nursing programs. Journal of Nursing Education. 2017; 56 (4):195–196. [ PubMed : 28383741 ]
- Peek ME, Vela MB, Chin MH. Practical lessons for teaching about race and racism: Successfully leading free, frank, and fearless discussions. Academic Medicine. 2020; 95 (12S):S139–S144. [ PubMed : 32889939 ]
- Periyakoil VS. Building a culturally competent workforce to care for diverse older adults: Scope of the problem and potential solutions. Journal of the American Geriatrics Society. 2019; 67 (2):S423–S432. [ PubMed : 31074850 ]
- Phillips JM, Malone B. Increasing racial/ethnic diversity in nursing to reduce health disparities and achieve Health Equity. Public Health Reports. 2014; 129 (Suppl 2):45–50. [ PMC free article : PMC3863700 ] [ PubMed : 24385664 ]
- Phillips KE, Roberto A, Salmon S, Smalley V. Nursing student interprofessional simulation increases empathy and improves attitudes on poverty. Journal of Community Health Nursing. 2020; 37 (1):19–25. [ PubMed : 31905301 ]
- Poore JA, Cullen DL, Schaar GL. Simulation-based interprofessional education guided by Kolb’s experiential learning theory. Clinical Simulation in Nursing. 2014; 10 (5):e241–e247.
- Porter K, Jackson G, Clark R, Waller M, Stanfill AG. Applying social determinants of health to nursing education using a concept-based approach. Journal of Nursing Education. 2020; 59 (5):293–296. [ PubMed : 32352547 ]
- Pritchard TJ, Perazzo JD, Holt JA, Fishback BP, McLaughlin M, Bankston KD, Glazer G. Evaluation of a summer bridge: Critical component of the Leadership 2.0 Program. Journal of Nursing Education. 2016; 55 (4):196–202. [ PubMed : 27023888 ]
- Pritchard TJ, Glazer G, Bankston KD, McGinnis K. Leadership 2.0: Nursing’s next generation: Lessons learned on increasing nursing student diversity. The Online Journal of Issues in Nursing. 2020; 25 (2)
- Purnell TS, Marshall JK, Olorundare I, Stewart RW, Sisson S, Gibbs B, Cooper LA. Provider perceptions of the organization’s cultural competence climate and their skills and behaviors targeting patient-centered care for socially at-risk populations. Journal of Health Care for the Poor and Underserved. 2018; 29 (1):481–496. [ PubMed : 29503313 ]
- Quality Matters. QM-Certified Programs. 2020. [November 11, 2020]. https://www .qualitymatters .org/qm-membership /faqs/qm-certified-programs .
- Richmond TS, Foman M. Firearm violence: A global priority for nursing science. Journal of Nursing Scholarship. 2019; 51 :229–240. https://doi .org/10.1111/jnu.12421 . [ PMC free article : PMC6417970 ] [ PubMed : 30215887 ]
- RINIMC (Rhode Island Nurses Institute Middle College Charter High School). RINIMC Charter High School. [March 29, 2021]. n.d. https://rinimc .org/rinimc-charter-high-school .
- Rosa WE, Ojemeni MT, Karanja V, Cadet G, Charles A, McMahon C, Davis S. Education equity in nursing: A cornerstone of sustainable development goal attainment. Public Health Nursing. 2019; 36 (4):447–448. [ PubMed : 31309621 ]
- Rutledge CM, Kott K, Schweickert PA, Poston R, Fowler C, Haney TS. Telehealth and eHealth in nurse practitioner training: Current perspectives. Advances in Medical Education and Practice. 2017; 8 :399–409. https://doi .org/10.2147/AMEP.S116071 . [ PMC free article : PMC5498674 ] [ PubMed : 28721113 ]
- RWJF (Robert Wood Johnson Foundation). Future of nursing scholars: PhD nurse profiles. 2020. [November 11, 2020]. http: //futureofnursingscholars .org/phd-nurse-profiles .
- RWJF. Future of nursing scholars. 2021. [June 2, 2021]. http: //futureofnursingscholars.org .
- Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Medical Care. 2008; 46 (7):678–685. [ PubMed : 18580386 ]
- Sabio C, Petges N. Understanding the barriers to BSN education among ADN students: A qualitative study. Teaching and Learning in Nursing. 2020; 15 (1):45–52.
- Salvucci C, Lawless CA. Nursing faculty diversity: Barriers and perceptions on recruitment, hiring, and retention. Journal of Cultural Diversity. 2016; 23 (2):65–75. PMID: 27439233. [ PubMed : 27439233 ]
- Sanner S, Baldwin DEE, Cannella KA, Charles J. The impact of cultural diversity forum on students’ openness to diversity. Journal of Cultural Diversity. 2010; 17 (2) [ PubMed : 20586367 ]
- Scheel LS, Peters MD, Møbjerg ACM. Reflection in the training of nurses in clinical practice settings: A scoping review protocol. JBI Database of Systematic Reviews and Implementation Reports. 2017; 15 (12):2871–2880. [ PubMed : 29219871 ]
- Schmidt S, George M, Bussey-Jones J. Welcome to the neighborhood: Service-learning to understand social determinants of health and promote local advocacy. Diversity Equality Health Care. 2016; 13 (6):389–390.
- Schroeder C, DiAngelo R. Addressing whiteness in nursing education: The sociopolitical climate project at the University of Washington School of Nursing. Advances in Nursing Science. 2010; 33 (3):244–255. PMID: 20693833. doi: 10.1097/ANS.0b013e3181eb41cf. [ PubMed : 20693833 ]
- Schroeder K, Garcia B, Phillips RS, Lipman TH. Addressing social determinants of health through community engagement: An undergraduate nursing course. Journal of Nursing Education. 2019; 58 (7):423–426. [ PubMed : 31242312 ]
- Sharma M, Pinto AD, Kumagai AK. Teaching the social determinants of health: A path to equity or a road to nowhere? Academic Medicine. 2018; 93 (1):25–30. [ PubMed : 28445214 ]
- Shiffrin RM. Drawing causal inference from big data. Proceedings of the National Academy of Sciences. 2016; 113 (27):7308–7309. [ PMC free article : PMC4941473 ] [ PubMed : 27382143 ]
- Shin S, Park JH, Kim JH. Effectiveness of patient simulation in nursing education: Meta-analysis. Nurse Education Today. 2015; 35 (1):176–182. doi: 10.1016/j.nedt.2014.09.009. [ PubMed : 25459172 ]
- Siegel J, Coleman DL, James T. Integrating social determinants of health into graduate medical education: A call for action. Academic Medicine. 2018; 93 (2):159–162. [ PubMed : 29140918 ]
- Spector N, Silvestre J, Alexander M, Martin B, Hooper J, Squires A, Ojemeni M. NCSBN regulatory guidelines and evidence-based quality indicators for nursing education programs. Journal of Nursing Regulation. 2020; 11 (2S):S1–S64.
- Spetz J. Projections of progress toward the 80% bachelor of science in nursing recommendation and strategies to accelerate change. Nursing Outlook. 2018; 66 (4):394–400. [ PubMed : 29903501 ]
- Squires A, Kovner C, Faridaben F, Chyun D. Assessing nursing student intent for PhD study. Nurse Education Today. 2013; 34 (11):1405–1410. [ PubMed : 24080267 ]
- SSIH (Society for Simulation in Healthcare). About simulation. [January 12, 2021]. n.d. https://www .ssih.org /About-SSH/About-Simulation .
- Storfjell J, Winslow B, Saunders J. Catalysts for change: Harnessing the power of nurses to build population health in the 21st century. Princeton, NJ: Robert Wood Johnson Foundation; 2017.
- Strauss V. Housing and food insecurity affecting many college students, new data says. 2020. [January 12, 2021]. https://www .washingtonpost .com/education /2020/02/20/housing-food-insecurity-affecting-many-college-students-new-data-says .
- Sukhera J, Wodzinski M, Rehman M, Gonzalez CM. The implicit association test in health professions education: A meta-narrative review. Perspectives in Medical Education. 2019; 8 (5):267–275. [ PMC free article : PMC6820611 ] [ PubMed : 31535290 ]
- Sullivan LW. A report of the Sullivan Commission on Diversity in the Healthcare Workforce. The Sullivan Commission. 2004. [March 29, 2021]. Missing persons: Minorities in the health professions. https: //campaignforaction .org/wp-content /uploads/2016/04/SullivanReport-Diversity-inhref="https: //campaignforaction .org/wp-content /uploads/2016 /04/SullivanReport-Diversity-inHealthcare-Workforce1 .pdfHealthcare-Workforce1.pdf .
- Szanton SL, Wolff JW, Leff B, Thorpe RJ, Tanner EK, Boyd C, Xue Q, Guralnik J, Bishai D, Gitlin LN. CAPABLE trial: A randomized controlled trial of nurse, occupational therapist and handyman to reduce disability among older adults: Rationale and design. Contemporary Clinical Trials. 2014; 38 (1):102–112. https://doi .org/10.1016/j .cct.2014.03.005 . [ PMC free article : PMC4074085 ] [ PubMed : 24685996 ]
- Taylor H, Loftin C, Reyes H. First-time NCLEX-RN pass rate: Measure of program quality or something else? Journal of Nursing Education. 2014; 53 (6):336–341. [ PubMed : 24855991 ]
- The Macy Foundation. Conference recommendations February 24–27, 2020. Atlanta, GA: Josiah Macy Jr. Foundation; 2020. Addressing harmful bias and eliminating discrimination in health professions learning environments. [ PubMed : 32889942 ]
- The Poverty Simulation. The Poverty Simulation. [May 14, 2020]. n.d. http://www .povertysimulation.net/about .
- ThinkTank. The cost of poverty experience. [November 11, 2020]. n.d. https: //thinktank-inc.org/cope .
- Thornton M, Persaud S. Preparing today’s nurses: Social determinants of health and nursing education. The Online Journal of Issues in Nursing. 2018; 23 (3)
- Tilden VP, Cox KS, Moore JE, Naylor MD. Strategic partnerships to address adverse social determinants of health: Redefining health care. Nursing Outlook. 2018; 66 (3):233–236. [ PubMed : 29685323 ]
- Topaz M, Pruinelli L. Big data and nursing: Implications for the future. Studies in Health Technology and Informatics. 2017; 232 :165–171. [ PubMed : 28106594 ]
- Turk MT, Colbert AM. Using simulation to help beginning nursing students learn about the experience of poverty: A descriptive study. Nurse Education Today. 2018; 71 :174–179. Epub September 29, 2018. PMID: 30292059. doi: 10.1016/j.nedt.2018.09.035. [ PubMed : 30292059 ]
- Tyczkowski BL, Reilly J. DNP-prepared nurse leaders: Part of the solution to the growing faculty shortage. The Journal of Nursing Administration. 2017; 47 (7–8):359–360. [ PubMed : 28678051 ]
- UND (University of North Dakota). RAIN: No excuses orientation. 2020. [November 11, 2020]. https://cnpd .und.edu/rain/no-excuses .html .
- U.S. Department of Education. Competency-based learning or personalized learning. [November 11, 2020]. n.d.a. https://www .ed.gov/oii-news /competency-based-learning-or-personalized-learning .
- U.S. Department of Education. Public service loan forgiveness. [September 2, 2020]. n.d.b. https://studentaid .gov /manageloans/forgiveness-cancellation /public-service .
- Valderama-Wallace CP, Apesoa-Varano EC. “Social justice is a dream”: Tensions and contradictions in nursing education. Public Health Nursing. 2019; 36 (5):735–743. [ PubMed : 31168869 ]
- Velasquez D, Mehrotra A. Health Affairs Blog. 2020. Ensuring the growth of telehealth during COVID-19 does not exacerbate disparities in care. doi: 10.1377/hblog20200505.591306.
- Villarruel AM, Broome ME. Beyond the naming: Institutional racism in nursing. Nursing Outlook. 2020; 68 (4):375–376. [ PMC free article : PMC7473708 ] [ PubMed : 32896302 ]
- von Wendt CEA, Niemi-Murola L. Simulation in interprofessional clinical education. Simulation in Healthcare. 2018; 13 (2):131–138. [ PubMed : 29117089 ]
- Waite R, Nardi D. Nursing colonialism in America: Implications for nursing leadership. Journal of Professional Nursing. 2019; 35 (1):18–25. doi: 10.1016/j.profnurs.2017.12. [ PubMed : 30709460 ]
- Walker K, Arbour M, Waryold J. Educational strategies to help students provide respectful sexual and reproductive health care for lesbian, gay, bisexual, and transgender persons. Journal of Midwifery and Women’s Health. 2016; 61 (6):737–743. [ PubMed : 27783889 ]
- Wallace J, Decosimo K, Simon M. Applying data analytics to address social determinants of health in practice. North Carolina Medical Journal. 2019; 80 :244–248. [ PubMed : 31278189 ]
- WGU (Western Governors University). Competency-based education. 2020. [November 11, 2020]. https://www .wgu.edu/about /competency-based-education.html .
- Whitfield-Harris L, Lockhart JS. The workplace environment for African American faculty employed in predominantly White institutions. The Association of Black Nursing Faculty Journal. 2016; 27 (2):28–38. PMID: 27263232. [ PubMed : 27263232 ]
- Whitfield-Harris L, Lockhart JS, Zoucha R, Alexander R. The lived experience of Black nurse faculty in predominantly White schools of nursing. Journal of Transcultural Nursing. 2017; 28 (6):608–615. [ PubMed : 28826318 ]
- WHO (World Health Organization). Regional Office for the Eastern Mediterranean. The growing need for home health care for the elderly: Home health care for the elderly as an integral part of primary health care services. 2015. [March 29, 2021]. https://apps .who.int /iris/handle/10665/326801 .
- Wilkie ML. Empowered by cultural identity and catalyzed by resilience: A path to support American Indian nursing student success. Creative Nursing. 2020; 26 (1):43–47. [ PubMed : 32024738 ]
- Williams SD, Hansen K, Smithey M, Burnley J, Koplitz M, Koyama K, Bakos A. Using social determinants of health to link health workforce diversity, care quality and access, and health disparities to achieve health equity in nursing. Public Health Reports. 2014; 129 (1):32–36. [ PMC free article : PMC3863698 ] [ PubMed : 24385662 ]
- Wilson AH, Sanner S, McAllister LE. An evaluation study of a mentoring program to increase the diversity of the nursing workforce. Journal of Cultural Diversity. 2010; 17 (4) [ PubMed : 22303649 ]
- Wise PH. The Future of Children. 2012. Emerging technologies and their impact on disability; pp. 169–191. [ PubMed : 22550690 ]
- Yale School of Nursing. Simulation technology redirects nursing curriculum during COVID-19. 2020. [January 12, 2021]. https://nursing .yale .edu/news/simulation-technology-redirects-nursing-curriculum-during-covid-19 .
- Yen PY, Bakken S. Review of health information technology usability study methodologies. Journal of the American Medical Informatics Association. 2012; 19 (3):413–422. [ PMC free article : PMC3341772 ] [ PubMed : 21828224 ]
- Yoder CM, Pesch MS. An academic–fire department partnership to address social determinants of health. Journal of Nursing Education. 2020; 59 (1):34–37. [ PubMed : 31945173 ]
- Zandee G, Bossenbroek D, Friesen M, Blech K, Engbers R. Effectiveness of community health worker/nursing student teams as a strategy for public health nursing education. Public Health Nursing. 2010; 27 (3):277–284. [ PubMed : 20525101 ]
See https://www .aacnnursing .org/Education-Resources /AACN-Essentials (accessed April 13, 2021).
See Chapter 3 for demographic information on employed nurses in the United States.
For further discussion of domains and competencies, see AACN, 2020b ; Campaign for Action, 2019b ; IOM, 2016b ; NACNEP, 2019 ; NLN, 2019 ; Thornton and Persaud, 2018 .
Not all courses are open to students from all schools.
Brief and commonplace daily indignities (see Chapter 10 ).
See https://www .ohiohighered .org/collegecreditplus (accessed April 13, 2021).
See https://www .nmnec.org (accessed April 13, 2021).
See https://www .qualitymatters.org (accessed April 13, 2021).
- Cite this Page National Academies of Sciences, Engineering, and Medicine; National Academy of Medicine; Committee on the Future of Nursing 2020–2030; Flaubert JL, Le Menestrel S, Williams DR, et al., editors. The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity. Washington (DC): National Academies Press (US); 2021 May 11. 7, Educating Nurses for the Future.
- PDF version of this title (5.6M)
In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Educating Nurses for the Future - The Future of Nursing 2020-2030 Educating Nurses for the Future - The Future of Nursing 2020-2030
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
7 Key Challenges Faced by Nurse Educators Today

NurseJournal.org is committed to delivering content that is objective and actionable. To that end, we have built a network of industry professionals across higher education to review our content and ensure we are providing the most helpful information to our readers.
Drawing on their firsthand industry expertise, our Integrity Network members serve as an additional step in our editing process, helping us confirm our content is accurate and up to date. These contributors:
- Suggest changes to inaccurate or misleading information.
- Provide specific, corrective feedback.
- Identify critical information that writers may have missed.
Integrity Network members typically work full time in their industry profession and review content for NurseJournal.org as a side project. All Integrity Network members are paid members of the Red Ventures Education Integrity Network.
Explore our full list of Integrity Network members.

America is in the middle of a severe and long-standing nursing shortage. It is threatening the supply of registered nurses. The shortage has also affected the number of clinical preceptors and nursing faculty who prepare nursing students.
Nursing school enrollment cannot grow fast enough to meet the projected need. The shortage of nursing school faculty members has also limited enrollment numbers.
Nurse educators often are active clinicians, which is important to maintain quality nurse teaching . However, this also places a strain on educators with higher workloads, forcing them to work short-staffed in practice and education.
These stressors have led to a crisis in the profession. More nurses and nurse educators are seeking positions outside of nursing and feel less committed to their profession than in the past.
We interviewed several influential nurse educators who shared the challenges they face. We also explore the changes needed to improve the system and how nurses can advocate for those changes.
Nurse Educators Face Challenges Due to Nursing Shortage
The nursing shortage is expected to worsen as the baby boomer generation ages and more nurses retire. According to the American Association of Colleges of Nursing (AACN), faculty staff shortages limit student capacity at a time when growth is necessary.
There is a critical need to increase the number of nurse educators to meet the demand, but nurse educators are also under a lot of stress. To retain experienced educators and preceptors, it’s important to support their efforts.
Many challenges affect educators today. Nurse educators identified the following challenges that affect their ability to nurture and educate the future generation of nurses.
1. Lack of Resources
Nurse educators are well aware of a faculty shortage in programs around the country.
- Schools were forced to turn away 80,407 qualified students from undergraduate and graduate programs in 2019. This is an increase from the 68,000 turned away in 2014.
- In one survey of 892 nursing schools, 1,637 vacancies were identified. There is also a need to create an additional 134 positions to accommodate the rising demand.
Erica Jastrow has been a nurse educator for over 17 years and sees firsthand the lack of human resources in nursing facilities.
“In some schools,” she says, “faculty members manage all aspects for the nursing program from admissions, to advising, to instruction.”
This lack of human resources places additional stress on stretched-thin faculty members with limited time and resources. In addition to the faculty who have reached retirement age, other nurse educators are leaving the profession, furthering the issue.
Anne Dabrow Woods has witnessed and experienced the challenges facing faculty. She teaches in the graduate program at Drexel University and says it is imperative we address the issues faced by educators today.
Woods says we must:
- Increase nurse educator salaries and pay them what they are worth
- Provide learning opportunities for adjunct faculty
- Use academic and practice partnerships to develop and fund adjunct faculty programs.
2. Curriculum Challenges
Sherri Wilson, DNP, is the director of health career programs at Stride, a provider of tech-enabled education programs. She identifies several curriculum challenges that impact new nursing students and teaching faculty.
Students must overcome several barriers just to enroll in nursing programs. Once accepted, they face additional challenges to succeed in the program. Some students don’t have the tools they need, and others may not understand what the career involves.
Wilson suggests starting early by offering ways high school students can prepare for a nursing career . Students may learn more through classwork, clubs, mentorship, or dual enrollment.
“The sooner we can introduce students to the prerequisites, requirements, and opportunities in nursing and nurse education, the better,” she says.
Nurse educators also face curriculum challenges. Most programs are seeking faculty with doctorates. According to the Special Survey on Vacant Faculty Positions in 2019 reported by the AACN, 89.7% of faculty openings required or preferred a doctoral degree.
Wilson notes that doctorates are either research focused or clinical focused. Yet most programs do not include substantial academic coursework to prepare graduates for a teaching or faculty role, she says. It is necessary to reevaluate the curriculum used to teach future teachers.
3. Representation in Faculty and Training
Wilson also seeks representation of different cultural backgrounds in faculty and preceptors. A recent AACN study found that 93% of full-time faculty were female, and only 17% were from underrepresented groups.
“A more diverse nursing faculty can help to broaden the perspectives of nursing students and can provide sources of mentorship for minority nurses,” Wilson says.
The recent Future of Nursing Report 2020-2030 explored how the profession could develop different curricula. The goal would prepare nurses to reduce health disparities and inequities, like how nurses can address disparities in infant mortalit y, by using cost-effective strategies. These include technology and maintaining patient- and family-focus care.
To address these issues, there needs to be better representation in nursing and cultural competence in nursing . With a diverse workforce, nurses can serve communities better by understanding and identifying the social determinants of health.
“Finding ways to connect more nursing students to learning opportunities in the communities they serve will empower them to work with people of different backgrounds and from various life experiences,” Wilson says.
4. Fostering and Maintaining Student Relationships
Student-teacher relationships are important from elementary school through graduate school. They lead to:
- Academic achievement
- Increased motivation to learn
- Professional student development
Yet, stressed and overworked faculty often have little time to build constructive and authentic relationships with their students.
The lack of student-teacher relationships may have an unfortunate trickle-down effect on some students’ future career development. It could discourage students from furthering their education and choosing a career as a nurse educator.
Strong student-teacher relationships can help bridge the gap and support students’ efforts. Some students are working in healthcare while completing their education. Mandated hours or extra shifts are obstacles to completing assignments, maintaining grades, and attending class.
“Showing a student that you care about them and are there to support them may make the difference between a student who drops out or fails in the program and one that is successful,” Jastrow says.
5. Pay Inequality
Pay inequality in nurse educator roles is a significant obstacle to attracting new faculty. According to the U.S. Bureau of Labor Statistics , the median salary for a nurse educator is $75,470.
Nurses with comparable education levels make far more than nurse educators, with nurse practitioners making $114,510 annually , on average. This pay deficit causes master’s- and doctoral-level nurses to not pursue nurse teaching.
It is crucial that the compensation for nurse educators match their experience and education. This will help to attract quality faculty to nursing programs.
H. Eva Hvingelby is a faculty member at Walden University and clinical advisor at Optum. She sees the challenges with pay inequality and the need for immediate change.
She says that higher educator pay and smaller teacher-to-student ratios will make training new nurses more attractive to clinicians. But these adjustments will not come easily.
“While it is difficult to implement these changes when there is already an acute shortage,” she says, “not doing so risks further loss of capable personnel, worsened patient outcomes, and higher healthcare costs.”
6. Lack of Preceptors
Nurse educators and nursing students are impacted by the lack of preceptors available to nursing students. The nursing shortage has meant that many nursing units work short-staffed with higher than normal staff-to-patient ratios.
Nursing preceptors are a guiding hand and a steady voice for nursing students. When there is not enough available or low staffing, it can impact the quality of a nursing student’s education or new nursing graduate.
Tony Anno is a core faculty member at Walden University. He says online and traditional classroom learning face challenges from the restrictions and lack of access to clinical sites and preceptors.
However, nursing programs have a role in addressing the shortage in innovative ways.
For instance, Anno notes that Walden University has identified areas where students could complete some or all of their clinical hours using telehealth nursing services .
7. Lack of Opportunity to Update Knowledge and Skills
The nursing shortage in academia and clinically has stretched nurse educators’ resources thin. Nurse educators do not have the time to update their knowledge and skills.
This lack of opportunity was the most frequently described frustration for clinical nurse educators in one study. Additionally, this can contribute to the rising levels of nursing burnout as it contributes to nurse educators’ acute and chronic stress levels.
One study confirmed what most nurse educators know: Nurses value professional development and believe it is integral to improving patient care standards.
Access to continuing education for nurses to update knowledge and skill levels helps maintain high standards of care. This is essential when educating and training the next generation of nurses.
“Universities, as well as hospital systems and other healthcare providers, should look for ways to continually upskill their existing workforce and faculty on the latest practices and technologies,” Wilson says.
Wilson stresses the need for continued education and skill development in the face of rapidly changing technology. Nurse educators are expected to possess these skills to advance quality and address emerging needs.
What Needs to Change and How Nurses Can Get Involved
Despite challenges during the pandemic, turning away thousands of qualified candidates, and a shortage of nurse educators, enrollment in nursing programs across the country was up by 5.6% in 956 programs surveyed. However, significant changes must be made to raise enrollment and fill open nursing positions.
The pandemic has highlighted long-standing issues in healthcare that have contributed to the nursing shortage. Wilson says nurses are currently “uniquely positioned to become involved in the policy process to advocate for resources to address this complex issue.”
Woods believes the answer lies in innovation, perseverance, and resilience.
“Given this landscape, investing in learning technologies is no longer a ‘nice to have’ for nursing education but truly essential,” she says.
With the increased adoption of educational technology, we will also see a shift in funding to address previous hurdles that nurse educators faced in accessing these technologies, Wilson says.
What Needs to Change to Increase the Nurse Educator Retention Rates
- Bridge the wage gap between clinical roles and educators, so salaries align with other nurses holding graduate and doctoral degrees.
- Reduce teacher-to-student ratios to improve education and make the nurse educator role more attractive to clinicians.
- Better prepare nurse educators in their master’s or doctoral programs with academic coursework to prepare them for a teaching role.
- Increase human resource support for admission and advising so faculty can focus on teaching.
- Value the time and effort necessary to foster better student-faculty relationships, which improves a student’s education and faculty job satisfaction.
- Provide recognition for faculty members within the nursing program.
- Offer nursing scholarships that encourage students to pursue positions as nurse educators.
- Improve clinical working conditions, staff ratios, and work-life balance for nurses and nurse educators.
- Give faculty the opportunity and time to update their knowledge and skills.
- Partner academic centers with healthcare systems to develop adjunct faculty training programs.
- Invest in better mental health resources for nurses and nurse educators.
- Invest in innovation technologies.
Nurse educators can advocate for change and promote ways for nurses to effect change in their profession. They can provide information and perspective from professionals working in the field through taking advantage of professional nursing associations and advocacy groups.
Often involvement does not require hours of time and energy but rather phone calls and emails to state legislators to support or defend policy change.
Nurse educators may also consider working with the administration in their program to use creative strategies to meet the needs of the students and faculty.
It can be challenging to push for change. Yet, many colleges and universities are now recognizing the need for innovation to reduce the nursing shortage and attract qualified nurses as teachers and faculty.
Meet Our Contributors

Sherri Wilson, DNP
Sherri Wilson oversees the development and implementation of curriculum and partnerships in the healthcare field as director of health career programs at Stride, Inc. – a provider of tech-enabled education programs. Prior to joining Stride, Wilson served as a public health administrator with Fairfax County.
Wilson earned her doctor of nursing practice from Johns Hopkins University, a master’s in public administration from Seton Hall University, and a bachelor of science in nursing from Hampton University. In 2021, Wilson was named president-elect of the Virginia Nurses Association.

Erica L. Jastrow, Ed.D., MSN, RN, CNE
Erica Jastrow has been a registered nurse for over 20 years and a nurse educator in higher education for over 17. She has led several prelicensure nursing programs and currently serves as an assistant professor and RN-to-BSN program director at William Peace University . She has a BSN from Lenoir Rhyne University, an MSN in nursing education from UNC-Greensboro, and a doctorate in education from Grand Canyon University.

Tony Anno, DNP, ACNPC-AG, AGACNP-BC, CCDS, CEPS, RDCS, FHRS
Tony Anno is a core faculty member in Walden University’s master of science in nursing program. Anno currently practices in cardiology/electrophysiology at the Kansas City VA Medical Center and volunteers as the sole provider for Health Partnership Clinic. The clinic provides healthcare to patients regardless of income or insurance status.
Anno is certified by the International Board of Heart Rhythm Examiners as a certified cardiac device specialist and certified electrophysiology specialist. He is also a registered cardiac diagnostic sonographer.

H. Eva Hvingelby, Ph.D., ACNP
H. Eva Hvingelby is a faculty member in Walden University’s master of science in nursing program and a clinical advisor for Optum. She has 21 years of experience as a healthcare clinician. In addition, she spent seven years with the federal government researching and supporting outreach to marginalized populations. Hvingelby consults on strategies to improve clinical communication and collaboration across disciplines.

Anne Dabrow Woods, DNP, RN, CRNP, ANP-BC, AGACNP-BC, FAAN
Anne Dabrow Woods is the chief nurse at Wolters Kluwer, Health, Learning, Research and Practice . She drives the strategic development of evidence-based solutions for nurses and nursing institutions. A nurse for over 37 years and a nurse practitioner since 1998, Dabrow Woods currently practices as an acute care/critical care nurse practitioner at Penn Medicine, Chester County Hospital. She also teaches in the graduate nursing program at Drexel University as clinical adjunct faculty.
Dabrow Woods earned a bachelor’s from West Chester University, a master’s from LaSalle University, a postmaster’s certificate from Drexel University, and a doctor of nursing practice from Texas Christian University. She is also a fellow in the American Academy of Nursing.
Page last reviewed December 16, 2021

An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Research Initiatives
- Meet Our Researchers
- Meet Our Program Officers
- RESEARCH LENSES
- Health Equity
- Social Determinants of Health
- Population and Community Health
- Prevention and Health Promotion
- Systems and Models of Care
- Funding Opportunities
- Small Business Funding
- Grant Applicant Resources
- Training Grants
- Featured Research
- Strategic Plan
- Budget and Legislation
- Connect With Us
- Jobs at NINR

Advancing health equity into the future.
NINR's mission is to lead nursing research to solve pressing health challenges and inform practice and policy – optimizing health and advancing health equity into the future.

Funding Opportunities Newsletter
Subscribe to receive the latest funding opportunities and updates from NINR.

Funding opportunities that improve health outcomes
NINR believes that nursing research is the key to unlocking the power and potential of nursing. NINR offers grants to individuals at all points in their career, from early investigators to established scientists. NINR grants also support small businesses and research centers.
Research Funding

Small Business

Training Funding
Homepage events stories, addressing public health challenges through research.
NINR-supported researchers explore and address some of the most important challenges affecting the health of the American people. Learn about accomplishments from the community of NINR-supported scientists across the United States.

Advancing social determinants of health research at NIH
Over 20 NIH Institutes, Centers, and Offices are working collaboratively to accelerate NIH-wide SDOH research across diseases and conditions, populations, stages of the life course, and SDOH domains.

Trending Topics in Nursing Education: Mentoring Clinical Faculty and Finding a Healthy Work-Life Balance

Related Reading
- Where’s the Fire? Why Nurse Educators Must Fight for Joy in Order to Transform Nursing Education
- “Who Are You?” Why Identifying Your Motivating Drive as a Nurse/Educator Matters
- Are You Running Out of Gas? Here’s How to Get Filled Up!
Keith Rischer – Ph.D., RN, CCRN, CEN
As a nurse with over 35 years of experience who remained in practice as an educator, I’ve witnessed the gap between how nursing is taught and how it is practiced, and I decided to do something about it! Read more…
The Ultimate Solution to Develop Clinical Judgment Skills
KeithRN’s Think Like a Nurse Membership
Access exclusive active learning resources for faculty and students, including KeithRN Case Studies, making it your go-to resource.
Sign up to receive a free KeithRN NextGen Case Study!
Develop clinical judgment skills with this innovative new case study on asthma to prepare your students for nextgen nclex and practice.
" * " indicates required fields
Keith Rischer
Introduction to using the science of learning to develop clinical judgment, recommended for you.
Have Any Questions !
[email protected]
Whatsapp chats only
+ 1 (315) 636 5076
- Personal Statement
- College Essay
- Nursing Report Writing Service
- Course Work
- Nursing Homework Help
- Assignments
- Entrance Essays
- Essay Writing
- Presentations
- Term Papers
- Dissertation
- Case Studies
- Shadow Health Assessment Help
- Annotated Bibliography
- Research Papers
- Grant Proposals
- Open access
- Published: 03 April 2024
The environmental awareness of nurses as environmentally sustainable health care leaders: a mixed method analysis
- Olga María Luque-Alcaraz ORCID: orcid.org/0000-0003-1598-1422 1 , 2 , 3 , 5 ,
- Pilar Aparicio-Martínez ORCID: orcid.org/0000-0002-2940-8697 3 , 4 ,
- Antonio Gomera ORCID: orcid.org/0000-0003-0603-3017 2 &
- Manuel Vaquero-Abellán ORCID: orcid.org/0000-0002-0602-317X 2 , 3 , 4
BMC Nursing volume 23 , Article number: 229 ( 2024 ) Cite this article
338 Accesses
6 Altmetric
Metrics details
People worldwide are concerned with the possibility of climate change, microplastics, air pollution, and extreme weather affecting human health. Countries are implementing measures to reduce environmental impacts. Nurses play a vital role, primarily through Green Teams, in the process of promoting sustainable practices and minimizing the environmental footprint of health care facilities. Despite existing knowledge on this topic, assessing nurses’ environmental awareness and behavior, including the barriers they face, is crucial with regard to improving sustainable health care practices.
To analyze the environmental awareness and behavior of nurses, especially nurse leaders, as members of the Green Team and to identify areas for improvement with regard to the creation of a sustainable environment.
A sequential mixed-method study was conducted to investigate Spanish nurses. The study utilized an online survey and interviews, including participant observation. An online survey was administered to collect quantitative data regarding environmental awareness and behavior. Qualitative interviews were conducted with environmental nurses in specific regions, with a focus on Andalusia, Spain.
Most of the surveyed nurses ( N = 314) exhibited moderate environmental awareness (70.4%), but their environmental behavior and activities in the workplace were limited (52.23% of participants rarely performed relevant actions, and 35.03% indicated that doing so was difficult). Nurses who exhibited higher levels of environmental awareness were more likely to engage in sustainable behaviors such as waste reduction, energy conservation, and environmentally conscious purchasing decisions ( p < 0.05). Additionally, the adjusted model indicated that nurses’ environmental behavior and activities in the workplace depend on the frequency of their environmental behaviors outside work as well as their sustainable knowledge ( p < 0.01). The results of the qualitative study ( N = 10) highlighted certain limitations in their daily practices related to environmental sustainability, including a lack of time, a lack of bins and the pandemic. Additionally, sustainable environmental behavior on the part of nursing leadership and the Green Team must be improved.
Conclusions
This study revealed that most nurses have adequate knowledge, attitudes, and behaviors related to environmental sustainability both inside and outside the workplace. Limitations were associated with their knowledge and behaviors outside of work. This study also highlighted the barriers and difficulties that nurses face in their attempts to engage in adequate environmental behaviors in the workplace. Based on these findings, interventions led by nurses and the Green Team should be developed to promote sustainable behaviors among nurses and address the barriers and limitations identified in this research.
Graphical Abstract
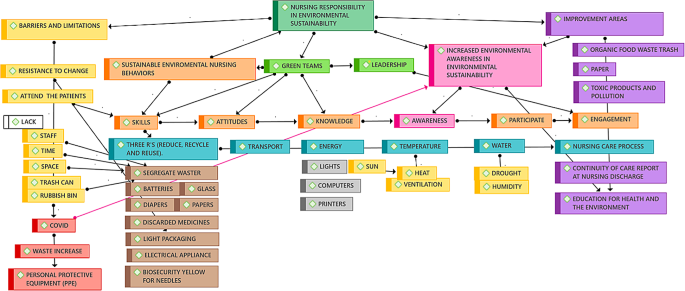
Peer Review reports
Introduction
The impact of climate change on human society is a global concern, especially with regard to microplastics, resource shortages, air pollution, droughts, and extreme weather. Such consequences affect human health both directly and indirectly, resulting in an increase in pathologies and a deterioration in medical attention [ 1 , 2 ]. In this context, diverse measures aimed at reducing the environmental impact of daily activities and minimizing the ecological footprint thereof [ 3 ] have been implemented by multiple countries [ 4 , 5 , 6 , 7 ]; these activities have been framed as environmental regulations in line with the Sustainable Development Goals (SDGs) [ 8 ].
The SDGs are being integrated into governments and a variety of other contexts, including the health care system. Spain is dedicated to such a goal, i.e., that of promoting a greener and more democratic health care transition. To achieve this goal, strategic plans have been developed to mitigate the effects of climate change [ 9 , 10 ]. One specific such program is the Strategic Health and Environment Plan (PESMA) [ 11 ], whose aim is to enhance the synergy between health and the environment innovatively by assessing the impact of the population in terms of 14 environmental indicators [ 12 ].
One such indicator focuses on the resources and support needed for sustainable practices, especially for nurses, due to the impact of the environment on their work [ 13 , 14 ]. The PESMA highlights the fact that health care providers should be included in strategies to reduce carbon footprints, build resilience to address the challenges associated with climate change and embrace a leadership role in the task of promoting sustainable health care practices [ 13 , 14 , 15 , 16 ]. Another critical aspect of PESMA focuses on education, training, and incentives that can promote sustainable behavior among health care workers, especially nurses [ 17 , 18 ]. As frontline health care workers, nurses have a unique opportunity to advocate for sustainable practices and reduce the environmental impact of the health care system. Nurses’ knowledge and behavior are limited despite the fact that nurses have positive attitudes toward environmental sustainability [ 19 ].
This situation stands in contrast to the role of nurses in the creation of more sustainable hospitals via the “Green Team” [ 20 ]. The Green Team, which originated in the United States of America a decade ago, is a committee that is responsible for finding and implementing sustainability projects to decrease the environmental impacts of daily operations. Members of various departments collaborate with sustainability staff to detect opportunities, spread awareness, and promote staff involvement in line with the Committee’s mission [ 21 ]. The team, which typically consists of and is led by nurses, aims to increase awareness of the health care industry’s effect on the environment and to develop tactics to mitigate the adverse environmental effects of hospitals.
In Spain, Green Teams, which span multiple disciplines and usually led by nursing professionals, are committed to sustainable change in health care [ 22 ]. Environmental nursing leaders on Green Teams control environmental sustainability in health care settings and provide education, resources, and support to other professionals with regard to the implementation of sustainable practices [ 23 ]. Accordingly, all nurses can contribute to the tasks of mitigating the impact of climate change on public health outcomes and promoting sustainable health for all [ 24 ]. These actions improve nurses’ knowledge, attitudes, and behavior in terms of sustainability and promote sustainable practices in health care settings, thus leading to a better understanding of the barriers faced by nurses in this context [ 24 , 25 , 26 ].
However, measuring and identifying nurses’ environmental awareness is essential for the promotion of sustainable hospitals [ 27 , 28 ]. Multidimensional indicators have been proposed for this purpose [ 16 ], the responsibility for which lies with nurse leaders on Green Teams. Nurses are responsible for promoting sustainability in health care organizations, as discussed by Kallio et al. (2018) [ 29 ], as well as for promoting nursing competencies related to environmental sustainability [ 30 ]. Several studies, including Harris et al. (2009) and Phiri et al. (2022), have examined nurses’ roles in environmental health and the effects of their leadership on the promotion of sustainability, especially during the COVID-19 pandemic, thereby emphasizing the importance of leadership [ 31 , 32 ].
As Ojemeni et al. (2019) discussed, leadership effectiveness in Green Teams, nursing teams and health care organizations must prioritize quality control and health care improvement to ensure sustainable development [ 33 ].
The topic of environmental management in health care organizations has been studied extensively, and an environmental or ecological model of care for promoting sustainability has been proposed [ 34 ]. As environmental creators and leaders on Green Teams, nurses are vital for minimizing hazardous waste in health care settings and improving awareness [ 35 ].
Although nurses have some degree of existing knowledge and awareness of sustainability, it is crucial to assess their proficiency in environmental matters and to gauge their environmental awareness. Such an evaluation can help identify areas for improvement within clinical management units [ 20 , 33 , 36 ]. Education and training programs can effectively promote sustainable behavior among nurses, but interventions should also address the barriers they face in their attempts to implement sustainable practices [ 37 ]. Therefore, it is imperative to examine the factors that foster sustainable behavior among nurses and to identify effective interventions that can promote sustainable health care practices and minimize the environmental footprint of health care facilities. Accordingly, this study aimed to analyze the environmental awareness and behavior of nurses, especially nurse leaders, as members of the Green Team and to identify areas for improvement with regard to creating a sustainable environment.
Study design
A sequential mixed-method study was conducted based on an online survey and interviews with a representative sample of Spanish nurses, including participant observation.
The study was divided into two phases. In the first phase, a cross-sectional, descriptive exploratory analysis was performed; this analysis relied on the results revealed using the Nurse’s Environmental Awareness Tool in Spanish (NEAT-es) [ 38 ], which was divided into three subscales: nursing awareness scale (NAS), environmental behaviors outside the workplace (PEB) and sustainable behaviors in the workplace (NPEB). In the second phase, qualitative interviews with environmental nurses (see Supplementary file 1 ) were conducted in regions featuring specific environmental units that were available in person (Andalusia).
Participants
The participants were recruited from public and private institutions associated with the National Health System, particularly from the nursing staff. The scope of the study focused on Spain, and the sample included all the nursing staff who completed the questionnaire and met the inclusion criteria.
The sampling process focused on the population of nurses in Spain in 2020, which was estimated to consist of 388,153 nurses. Therefore, a random sample of 314 participating individuals was sufficient to estimate the population with 95% confidence and an accuracy of +/- 2% units, which was expected to account for approximately 90% of the overall population. The inclusion and exclusion criteria used for the sample focused on nursing staff, nursing care auxiliary technicians, and students with relevant degrees, as this members of this group have the most significant presence in the health system and engage in direct and daily contact with environmental management in health centers (hospitals, primary care centers, sociosanitary centers and others). The remaining health and nonhealth personnel were excluded.
Additionally, the person from each unit who served as the environmental coordinator and other nurses from the ward who were members of the Green Team were asked to participate in the interviews and observations. The environmental coordinators, most of who were nursing supervisors, were determined based on the number of members of the Green Team and the sampling calculation used for the observational study. The interviews took place after various sessions, talks, or courses pertaining to environmental sustainability at the clinical management units.
Data collection
An intentional sampling process was implemented, and the data collection period spanned from November 2019 to March 2021. The observational data were collected in Spain via messages and posts on social media with the goal of quantifying nurses’ environmental awareness.
The initial sample of qualitative study included five environmental nursing leaders (NLs), 14 registered nurses (RNs), and ten nursing undergraduates. The final sample was reduced when the interviews reached data saturation ( N = 10, five NLs, and five RNs). Before the interviews, a focal group composed of one nurse, one physician, two engineers and a psychologist was tested using the questions included in this research as part of a pilot study ( Supplementary file 1 ). These interviews were conducted at the beginning of the participant’s shift, usually in the morning, and they featured a median time of 30 min, a minimum of 20 min and a maximum of one hour per participant.
One researcher (O.A.L.) also observed nurses during their daily work after the interview from a position within the ward as an added team member or staff member. Nevertheless, the observer did not highlight mistakes or sustainability issues during the observation process. No other researcher was involved in this step of the ethnographic analysis to avoid bias with regard to observing a variety of tasks ranging from preparing medication to implementing treatments.
The data collected through the interviews were recorded on a Samsung Galaxy 31 A, and observations were collected in a field notebook based on the Google Keep and Evernote mobile applications from November 2019 to mid-March 2021. This study was conducted at a regional level 1 hospital in southern Spain, particularly in various clinical management units (neurosurgery, internal medicine, cardiology, traumatology, and COVID-19 units, among others), and it focused on nursing supervisors, who are the leaders who bear responsibility for environmental awareness (NLs), and registered nurses (RNs) who were members of the Green Team.
Data analysis
The quantitative data were analyzed by reference to descriptive statistics, including the mean, standard deviation (SD), and 95% confidence interval (CI); the relative frequencies of the variables were also analyzed. Normalization tests, Kolmogorov‒Smirnov tests with Lilliefors correction, and Q‒Q tests were used to compare the goodness-of-fit to an average data distribution with regard to continuous or discrete quantitative variables. The comparison of two or three independent means was performed using Student’s t test and analyses of variance for each variable. The Χ 2 test with Yates’ correction was used to compare percentages and Pearson’s correlation (r) coefficients across the quantitative variables. Finally, associations among the NPEB and the other variables were studied through multiple linear regression. Participant observation was used to support the qualitative study of the reflective ethnographic type [ 39 , 40 ], and this process ended when the data reached saturation. Two researchers developed transcripts for the interviews based on the recorded interviews and added descriptions based on the notes from the field notebook. The identification of themes and patrons was based on a process of triangulation among the researchers and by cross-checking the results. The interviews with nurses were analyzed to summarize the content analysis and identify keywords and concurrency among the terms. The themes thus identified included Green Teams, sustainable environmental behaviors, environment awareness, leadership barriers and limitations and areas for improvement.
EPIDAT (version 4.2) and SPSS (version 25) software were used to support the quantitative analysis. The computer program ATLAS.ti (version 22) and the Office Package with Microsoft Word Excel (version 2019) were used for the interviews and the visualization of the keywords based on the themes identified based on the records, observations and field notebooks.
Nurses’ awareness, knowledge, attitudes and skills.
The ages of the Spanish staff, mainly nurses, included in this study ( N = 314) ranged from 19 to 68, with a mean age of 37.02 ± 12.7, CI = 95%, 35.6–38.4 years); in addition, 76.4% of these participants were women with more than 20 years of working experience (35.1%), and the majority were registered nurses (70.4%). Moreover, 113 (36%) participants worked at a local or regional hospital (30%) and were employees of a public institution (85.3%). Half of the nurses (157) worked only a morning shift (Table 1 ) in Andalusia, Madrid, or Catalonia (62.4%). The diverse autonomous regions on which this research focused were homogenously distributed and structured in line with the population. The analysis of these areas was also based on the specific inclusion of environmental units led by nurses (Andalusia, Madrid, and Catalonia), in contrast with regions featuring undetermined units or leaders related to this topic (such as Valencia) (37.5%).
Regarding nursing awareness, nurses scored higher on the PEB (31.83 ± 8.02 CI 95% 30.94–32.72 with regard to frequency vs. 32.36 ± 7.15 CI 95% 31.57–33.15 with respect to difficulty) than on the NAS (26.13 ± 9.91 CI 95% 25.03–27.23 with regard to knowledge vs. 47.39 ± 5.97 CI 95% 46.73–48.05 with respect to impact) and the NPEB (23.82 ± 6.45 CI 95% 23.10-24.53 with regard to frequency vs. 25.71 ± 6.31 CI 95% 25.01–26.41 with respect to difficulty). These results indicated that environmental knowledge among the Spanish population was limited (55.7%), although the nurses included in this research were aware of their potential impact on the environment (70.4%). The PEB subscale focused mostly on following environmental guidelines in their homes (57.3%) because these sustainable domestic tasks are easier for them (63.1%) than tasks in the professional field. The second subscale, NPEB, indicated that sustainable activities such as recycling were easy for the participants (57.6%), but sometimes they engaged in such activities less frequently than they would like (52.2%) (Fig. 1 and Fig. 2 ).
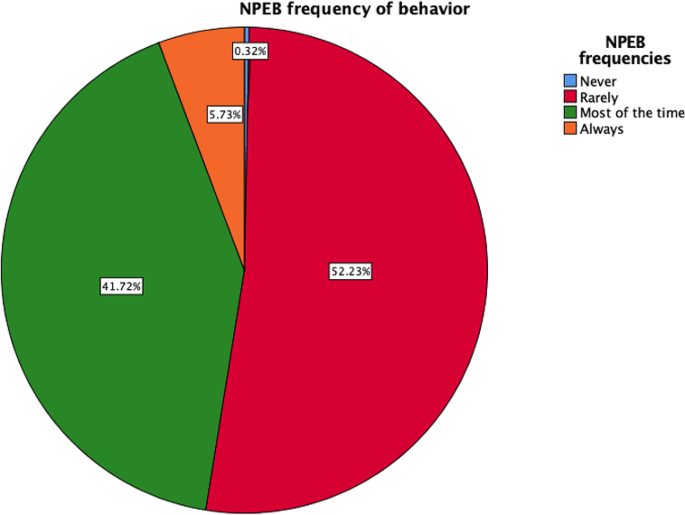
Representation of the frequency of nursing environmental behavior
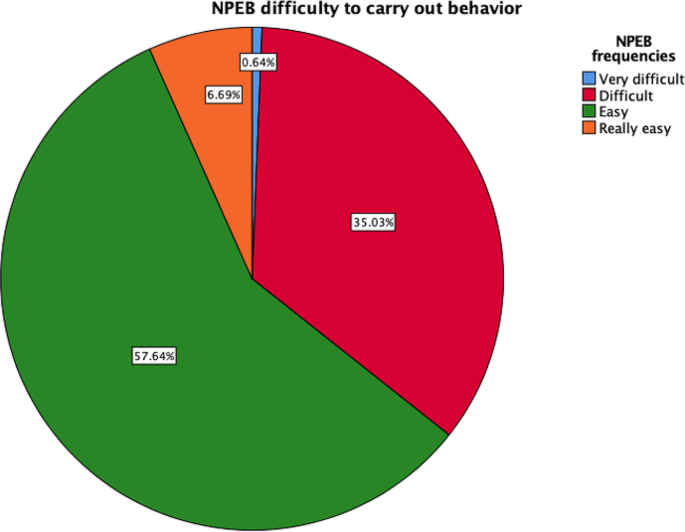
Difficulty of engaging in adequate environmental behaviors
The sociodemographic variables indicated differences among the NEAT subscales (Table 2 ). Gender, working experience (with a median value of 10 years), and the position held in the institution and region were relevant with regard to environmental knowledge ( p < 0.01), environmental behavior outside the workplace ( p < 0.01), and environmental behavior in the workplace ( p < 0.01).
The NPEB was associated with the worst scores, thereby reflecting the nurses’ environmental behavior and activities in the workplace (52.23% rarely performed relevant activities, and 35.03% indicated that doing so was difficult) (Fig. 1 and Fig. 2 ). The NPEB values pertaining to environmental behavior were positively linked to age ( r = 0.412; p < 0.001), NAS knowledge ( r = 0.526; p < 0.001), PEB frequency ( r = 0. 57; p < 0.001), PEB difficulty ( r = 0.329; p < 0.001), and finally, difficulty performing adequate environmental behaviors ( r = 0.499; p < 0.001). Additionally, the value of the NPEB with regard to the difficulty of performing adequate environmental behaviors was positively associated with age ( r = 0.149; p = 0.008), NAS knowledge ( r = 0.249; p < 0.001), PEB frequency ( r = 0. 244; p < 0.001) and PEB difficulty ( r = 0.442; p < 0.001).
Based on the relevance of certain sociodemographic variables, the nurses’ environmental awareness (NAS) and their behavior outside the workplace (PEB), linear multiple regression was performed to investigate nursing behavior in the workplace (NPEB). The initial model (square sum = 488.655; p < 0.0001) indicated that age, the impact of nursing awareness (NAS), and the frequency of sustainable behaviors outside the workplace (PEB) were not relevant to nursing behavior in the workplace (NPEB) in terms of the frequency of performing adequate behavior or the difficulties experienced ( p > 0.05). Based on these results, the adjusted model was calculated (Table 3 ), indicating that NPEB depends on PEB frequency and NAS knowledge ( p < 0.01).
Nursing environmental behavior in the context of Green Teams: Barriers and areas for improvement.
The participants in the qualitative study ( N = 10) included nine women and one man; their median age was 49 years; they exhibited an interval quartile range of 35–60; they had levels of working experience ranging between 20 and 30 years, and they worked only in the mornings (7/10). Furthermore, the group including nurses and nursing supervisors (5/10) exhibited higher levels of education (see Supplementary file 2 ). The themes identified via repetition and associations during the interviews and observations indicated links among nurses’ responsibilities on the Green Team since they conformed to the nature of such teams (i). This team and nursing leaders identified sustainable environmental behavior (ii) that could improve environmental awareness (iii), knowledge, aptitude, and skills. The nurses who are responsible for sustainable changes should be the leaders (iv), and the relevant barriers and limitations (v) and areas for improvement (vi) in diverse areas should be identified simultaneously.
Green teams were linked to nursing responsibilities in the context of environmental sustainability.
In the interviews, the Green Teams, led by environmental leader nurses and comprising various staff members, were identified as crucial committees dedicated to enhancing environmental awareness and knowledge among hospital staff. Participants indicated that these teams facilitated regular meetings to discuss sustainable practices and played a pivotal role in testing behaviors and knowledge related to environmental sustainability. The Green Teams were highlighted as platforms for fostering collaboration and discussion surrounding sustainable practices. Participants noted that these teams facilitated the main purpose of the team and its members to improve the hospital staff’s knowledge and attitudes via meetings (RN 2,3 and NL 1,3). Subsequently, the NL also indicated a key role of the team in the testing of behaviors and knowledge. The behavior of registered nurses should be tested using questions according to the NLs. Also, the NLs are included in disponibility of of proper disposal methods for medical waste:
“So, where is the rubbish bin for medicines, that white one that you showed in the session that is used for the remains of medicines that we do not give to patients?” [(NL5)]
By such comments, it can be inferred that the Green Team not only disseminates information, manages the training and measures knowledge but also ensures that staff members understand and adhere to best practices in waste management. These tasks of the NLs and other RNs in the Green Team contribute to the overall efficiency and effectiveness of environmental sustainability efforts within the hospital.
Sustainable environmental behaviors were emerged by Green Teams.
The results of the analysis indicated some degree of resistance among the nurses working at the clinical management units with regard to their lack of competencies, especially those pertaining to knowledge, skills and attitudes. The comments from the interviews highlighted potential factors contributing to this resistance, including age-related differences, varying levels of awareness, and challenges in applying the principles of reduce, reuse, and recycle (the three Rs). For instance, one repetitive comment expressed a sentiment of uncertainty, stating “It is what is, but we don’t know it or what to do with it” (RN 3,4,5, and NL 2,3).
“We know what the light packing is, and they (maintenance people) installed it to reduce the lights and reduce the expense and cost, but we don’t know what to do with the rubbish bins” [(NL 4)]
This comment highlights a disconnect between awareness of specific sustainable initiatives and the practical knowledge to implement them effectively. All comments reflect the importance of addressing knowledge gaps and providing practical guidance to support nurses in adopting sustainable environmental behaviours. By acknowledging and addressing these challenges, healthcare facilities can enhance their environmental stewardship efforts and promote a culture of sustainability among staff members.
Environmental awareness were drawn from the nursing responsibilities that led to the creation of the Green Team.
The comments indicated that environmental awareness among nurses was influenced by training sessions and courses on environmental sustainability. After receiving training featuring lectures and courses on environmental sustainability, the leaders also reflected on the ways in which nurses put the recommendations made during the environmental sustainability courses into practice. Moreover, the leaders indicated that education should be beyond formal training sessions. The environmental leaders were interested in supplementing these courses with environmental education practices for the general population, as noted, for example, in reports of discharge from patient care or cycling on the ward. These activities indicated the ideal of including a holistic approach to sustainability within the healthcare setting.
Relevant statements included, “We have to separate residues according to the material… light plastic goes to… it is important for the unit and all of us” (NL 2,5). One key point that the referees and registered nurses highlighted pertained to the climate, particularly the lack of water (NL 1–5 and RN 1,2).
“The drought is getting worse; I don’t know how we are going to keep up… we hope it rains soon” [(RN1)]
Overall, the interviews shed light on the efforts to foster environmental awareness among nurses through formal training and practical integration into everyday practices. These observations emphasize the importance of ongoing education and action in addressing environmental concerns within healthcare settings.
Leadership, which was linked by comments to the Green Teams.
The interviews revealed that leadership, particularly within the context of Green Teams, is crucial in promoting environmental awareness and fostering a culture of sustainability among nursing staff. All the participants ( n = 10) indicated that the presence of adequate knowledge, meetings and awareness among nursing staff were the most important factors. These factors were identified as key drivers in promoting sustainable practices within the healthcare environment. NLs indicated the importance of creating a supportive working environment where nurses feel comfortable asking questions and seeking clarification without fear of negative feedback. Relevant statements included, “It is key to receive feedback from the nurses and provide a good working environment so that they can ask questions and reflect without negative comments” (NL 1,2,4, and RN 1,2). This working environment allowed the registered nurses to ask for help regarding the three Rs:
“Could you remind me (referring to the environmental coordinator) how the sustainable guidelines were included in the discharge report for the continuity of care; I remember some things from the course you gave us, but I want to convey it completely to my patient” [(RN2)]
Barriers and limitations, were drawn from nurses’ responsibilities.
Several nurses indicated that the difficulties they encountered with regard to performing environmental behaviors pertained to the lack of time, adequate bins, and space as well as the limited number of nurses per patient in the wards. Despite these challenges, participants noted a positive outcome in the form of increased awareness of sustainability issues among nurses, indicating a growing recognition of the importance of environmental stewardship within the healthcare setting. One factor that increased the barriers to environmental adequacy was the pandemic, which increased waste and rubbish. Despite these challenges, participants noted a positive outcome in the form of increased awareness of sustainability issues among nurses, indicating a growing recognition of the importance of environmental stewardship within the healthcare setting. Relevant statements included “There are not enough green rubbish bins for COVID waste” (EL 1,4,5 and RN1,2) and “How are we going to recycle if we don’t even have time to care for patients?” (RN 1,2 and NL 3).
All these comments indicated the barriers the nurses faced, but they also suggested possibilities for improvement. The pandemic, despite overloading nurses, also improved their awareness.
Areas subject to improvement emerged from nursing responsibilities, limitations and leadership.
Nurses indicated that despite their general levels of environmental awareness and the courses they had received, participants performed better regarding their recycling behaviors at home than at the hospital. Participants acknowledged performing better in recycling practices within their personal spaces, suggesting a potential gap in translating theoretical knowledge into practical action within the healthcare environment. Relevant statements included “It’s just that I recycle almost everything in my house, especially glass…, but here, there is no time…” (RN 1,4,5).
Moreover, time constraints emerged as a significant barrier impeding nurses’ ability to engage fully in environmental sustainability efforts. Participants cited the demanding nature of their work, particularly in the context of patient care responsibilities, as limiting their capacity to prioritize sustainability initiatives. This highlights the need for strategies to streamline environmental practices and integrate them seamlessly into nurses’ daily routines without adding undue burden.
Some statements also highlighted nurses’ willingness to improve paperwork and records. Nurses recognized the importance of incorporating environmental considerations into patient discharge reports and other documentation processes but sought further guidance on how to effectively implement these practices. Relevant statements included “Can you tell me how the patient’s continuity care report upon discharge was included in the recommendations for environmental sustainability… I want to do the report well with what you gave us in the clinical session the other day…” [(NL4)]
These comments indicated the opportunities for improvement in fostering a culture of environmental sustainability within the hospital setting. By addressing the identified challenges and providing targeted support and guidance, especially the lack of time, nurses can contribute to environmental stewardship efforts more effectively.
The current research highlights the relevance of nurses as promoters of environmentally sustainable behaviors in their roles as members of Green Teams and important leaders. The findings suggest that nurses exhibit acceptable knowledge, attitudes, and behaviors with regard to environmental sustainability both inside and outside the workplace. These results are complemented by a qualitative analysis indicating that such behaviors originate from nursing responsibility, Green Teams, leadership identification of barriers and areas of improvement. Both analyses highlight the fact that environmental nursing behavior in the workplace depends on sustainable behaviors outside the workplace. The qualitative analysis also identifies diverse barriers to the task of promoting sustainable behavior within the workplace, such as the COVID-19 pandemic and the need for more time to be allocated to this process. One key point identified by both analyses is that nurses have acceptable levels of knowledge; however, their attitudes, although as yet imperfect, are improving.
Several studies of nurses’ awareness of environmental sustainability have revealed that nurses exhibit moderate levels of awareness and a considerable degree of concern regarding the health impacts of climate change [ 37 , 42 , 43 ], as reflected in the NEAT-es results.
Interestingly, the participants exhibited a tendency to perform environmentally sustainable behaviors more consistently in their personal lives than in professional settings. These results are consistent with previous research on registered nurse and nursing students [ 36 , 41 , 42 ]. According to Swedish research, nurses generally recognize environmental issues but may lack awareness of the environmental impact of health care [ 43 ]. Polivka Barbara J. et al. (2012) highlighted the gap between nurses’ knowledge of sustainability and workplace behaviors, thereby emphasizing the need for education and training programs to promote sustainable practices [ 44 ]. These issues were also observed in a study conducted in Taiwan, which revealed that while nursing students exhibit positive attitudes toward sustainability, their knowledge and behaviors are inadequate [ 45 ].
By conducting qualitative analysis, this research also identified multiple barriers to the adoption of sustainable practices among nurses, including time constraints, disruptions caused by the COVID-19 pandemic, a lack of bins, and a lack of health care personnel. These findings are in line with those reported in other research, but certain barriers (in terms of resources, time, and support) to the implementation of sustainable practices in the workplace remain [ 29 ]. This study suggests that interventions should be designed to address these barriers and promote sustainable behavior among nurses, a suggestion which is consistent with the current research. These findings highlight the importance of comprehending nurses’ perspectives on environmental sustainability in health care contexts as well as the necessity for targeted interventions and support mechanisms [ 46 ]. The tasks assigned to nursing leaders and the Green Team involved addressing these barriers and promoting sustainable practices among nurses in the context of their professional roles. Environmental nursing leaders seem to be crucial with regard to establishing a more environmentally conscious health care environment, which is in line with recommendations to create a greener health care system [ 21 , 31 ]. Despite the results of the interviews, some global qualitative studies of nurses’ views on environmental issues have exhibited variations across countries [ 47 , 48 ]. In Sweden, nurses already exhibit pro-sustainability attitudes before the introduction of the 2030 SDGs [ 16 ]. However, the integration of environmental sustainability education into nursing programs can prepare future nurses more effectively to address the challenges associated with climate change and promote sustainable health outcomes [ 49 ].
Limitations
Although this investigation provides valuable insights, it is important to acknowledge its limitations. First, the study was conducted during the COVID-19 pandemic in Spain, which may have influenced the results due to the unique circumstances and stressors faced by health care workers during this period. Additionally, the assessment of nurses’ environmental awareness was performed on a larger scale, i.e., across multiple regions, and therefore may not accurately reflect individual attitudes and behaviors since the qualitative investigations focused on a specific region. However, this approach was adopted to minimize the risk of the ecological fallacy. Future studies could explore individual perspectives and experiences by reference to more diverse and representative samples.
Despite these limitations, this research is highly relevant because it sheds light on the role of nurses in the task of promoting environmental sustainability in health care settings. The research also emphasized the role of nursing leadership in the tasks of promoting environmental sustainability and providing nurses with the necessary resources and support to implement sustainable practices.
In conclusion, while nurses generally exhibit acceptable levels of knowledge, attitudes, and behaviors regarding environmental sustainability, a notable gap persists in terms of the frequency of sustainable actions within the professional settings in which they operate. This finding highlights the importance of closely aligning nurses’ personal and professional sustainability practices.
The qualitative analysis conducted as part of this study identified several barriers to the adoption of sustainable practices among nurses, including time constraints, disruptions resulting from the COVID-19 pandemic, issues with waste disposal, and challenges related to health care personnel. Despite the fact that these findings are in line with those reported in previous research, persistent barriers such as limited resources, time, and support hinder the implementation of sustainable practices in the workplace. Therefore, interventions aimed at addressing these barriers and promoting sustainable behavior among nurses are essential, as highlighted by both current research and the corresponding qualitative insights. Therefore, nursing leaders and Green Teams are pivotal with regard to overcoming these barriers and fostering sustainable practices within health care environments. Environmental nursing leaders in particular are instrumental to the cultivation of a more environmentally conscious health care system, thereby aligning with recommendations for greener health care practices.
Data availability
The datasets used and/or analyzed as part of the current study are available from the corresponding author upon reasonable request.
Romanello M, Di Napoli C, Drummond P, Green C, Kennard H, Lampard P, et al. The 2022 report of the Lancet countdown on health and climate change: health at the mercy of fossil fuels. Lancet. 2022;400(10363):1619–54. https://doi.org/10.1016/S0140-6736(22)01540-9
Article PubMed Google Scholar
Watts N, Amann M, Ayeb-Karlsson S, Belesova K, Bouley T, Boykoff M, et al. The Lancet countdown on health and climate change: from 25 years of inaction to a global transformation for public health. Lancet. 2018;391(10120):581–630. https://doi.org/10.1016/S0140-6736(17)32464-9
Fadhullah W, Imran NIN, Ismail SNS, Jaafar MH, Abdullah H. Household solid waste management practices and perceptions among residents in the East Coast of Malaysia. BMC Public Health. 2022;22(1):1. https://doi.org/10.1186/s12889-021-12274-7
Article PubMed PubMed Central Google Scholar
Castañeda-Hidalgo H, Visovsky C, Hernández DE, González-Quirarte NH, Compeán-Ortiz L, Campiño SM. Nursing’s contributions to Sustainable Development Goals in Latin America through education, leadership, and partnerships. Int J Nurs Studi. 2021;121:104004. https://doi.org/10.1016/j.ijnurstu.2021.104004
Article Google Scholar
Dossey BM, Rosa WE, Beck DM. Nursing and the Sustainable Development Goals: from Nightingale to now. Am J Nurs. 2019;119(5):44–9. https://doi.org/10.1097/01.NAJ.0000557912.35398.8f
Rosa WE, Dossey BM, Koithan M, Kreitzer MJ, Manjrekar P, Meleis AI, et al. Nursing theory in the Quest for the Sustainable Development Goals. Nurs Sci Q. 2020;33(2):178–82. https://doi.org/10.1177/0894318420903495
United Nations Department of Economic and Social Affairs. Sustainable Development Knowledge Platform. In: Open Working Group proposal for Sustainable Development Goals. 2023. https://sustainabledevelopment.un.org/content/documents/1579SDGs Proposal.pdf.Accessed 17 Apr 2023.
Sanahuja JA. El Pacto Verde, NextGenerationEU y la nueva Europa geopolítica. In: Fundación Carolina.2022. https://www.fundacioncarolina.es/dt_fc_63/ . Accessed 17 Apr 2023.
Boto-Álvarez A, García-Fernández R. Implementation of the 2030 Agenda Sustainable Development Goals in Spain. Sustainability. 2020;12(6):2546. https://doi.org/10.3390/su12062546
Gomera Martínez A,Villamandos, de la Torre F, Vaquero Abellán. M,. Measurement and categorization of environmental awareness in university students: the contribution of the University to strengthen it. Ambientalización curricular y sostenibilidad. Nuevos retos de profesionalización docente. 2012;16(2):215– 28.
Ministerio de Sanidad. Plan Estratégico de Salud y Medioambiente 2022–2026. In: Ministerio para la Transición Ecológica y el Reto Demográfico.2021. https://www.sanidad.gob.es/ciudadanos/pesma/docs/241121_PESMA.pdf . Accessed 25 Apr 2023.
Ministerio de Sanidad. Plan Estratégico de Salud y Medioambiente. In: 1 a Programa de Actuación. Ministerio para la Transición Ecológica y el Reto Demográfico;2022. https://www.sanidad.gob.es/ciudadanos/pesma/docs/1er_PA_PESMA.pdf . Accessed 25 Apr 2023.
Hart J. Health Care without Harm: taking Environmental Action to improve lives and the planet. Integr Complement Ther. 2022;28(5):251–4. https://doi.org/10.1089/ict.2022.29036.pro
Health Care Without Harm. Hospitales que curan el planeta. In: Informe sobre el trabajo de los miembros de la Red Global de Hospitales Verdes y Saludables en América Latina. Red Global de Hospitales Verdes y Saludables en America Latina. 2022. https://saludsindanio.org/sites/default/files/documents-files/7287/Hospitales que curan el planeta 2022-FINAL_web_0 %281%29_0.pdf . Accessed 25 Apr 2023.
McDermott-Levy R. The nurse’s role on green teams: an environmental health opportunity. Pa Nurse. 2011;66(1):17–21.
PubMed Google Scholar
Schenk E, Johnson S. Nurse-sensitive environmental indicators: a qualitative study. J Nurs Manag. 2022;30(8):4378–86. https://doi.org/10.1111/jonm.13861 . Epub 2022 Oct 20.
Eckelman MJ, Sherman JD, MacNeill AJ. Life cycle environmental emissions and health damages from the Canadian healthcare system: an economic-environmental-epidemiological analysis. PLoS Med. 2018;15(7):e1002623. https://doi.org/10.1371/journal.pmed.1002623
Article CAS PubMed PubMed Central Google Scholar
Mateen A, Nisar QA, Nasir N. Fostering pro-environmental behaviors in the healthcare organizations: an empirical analysis of psychological and strategic factors. Asia Pac Manage Rev. 2023;28(1):13–23. https://doi.org/10.1016/j.apmrv.2022.01.004
Michie S, West R. Sustained behavior change is key to preventing and tackling future pandemics. Nat Med. 2021;27(5):749–52. https://doi.org/10.1038/s41591-021-01345-2
Article CAS PubMed Google Scholar
Mejia EA, Sattler B. Starting a Health Care System Green Team. AORN J. 2009;90(1):33–40. https://doi.org/10.1016/j.aorn.2009.03.001
Practice Green Health. Comparison chart of hospital green teams and their structure. 2019. https://practicegreenhealth.org/sites/default/files/2019-02/Comparison chart of hospitals green team structure_2017.pdf . Accessed 1st Frebuary 2024.
Dickman E, Backler C, Berg CD, Komandt M, Schiller J. Climate change and oncology nursing: a call to action. Clin J Oncol Nurs. 2022;26(1):109–13. https://doi.org/10.1188/22.CJON.109-113
de la Gámez J, Padilla Fortes A. Análisis De La producción científica visible en internet de Los técnicos de salud ambiental del Servicio Andaluz De Salud. Rev GeI Inf Doc. 2010;20:409–25.
Google Scholar
Filho W. Non-conventional learning on sustainable development: achieving the SDGs. Environ Sci Eur. 2021. https://doi.org/10.1186/s12302-021-00525-8 . 33;97.
Filho W, Tripathi S, Andrade Guerra JB, Gine R, Orlovic Lovren V, Willats J. Using the sustainable development goals towards a better understanding of sustainability challenges. Int J Sustainable Dev World Ecol. 2018;26:1–12. https://doi.org/10.1080/13504509.2018.1505674
Portela Dos Santos O, Melly P, Joost S, Verloo H. Climate Change, Environmental Health, and challenges for nursing Discipline. Int J Environ Res Public Health. 2023;20(9):5682. https://doi.org/10.3390/ijerph20095682
Sattler B, Randall KS, Choiniere D. Reducing Hazardous Chemical exposures in the neonatal intensive care unit: a New Role for nurses. Crit Care Nurs Q. 2012;35(1):102–11. https://doi.org/10.1097/CNQ.0b013e31823b2084
Trent L, Law J, Grimaldi D. Create intensive care green teams, there is no time to waste. Intensive Care Med. 2023;49(4):440–3. https://doi.org/10.1007/s00134-023-07015-w
Kallio H, Pietilä AM, Johnson M, Kangasniemi M. Environmental responsibility in hospital care: findings from a qualitative study. J Hosp Adm. 2018;7(5):56. https://doi.org/10.5430/jha.v7n5p56
Rosa WE, Catton H, Davidson PM, Hannaway CJ, Iro E, Klopper HC, et al. Nurses and midwives as Global Partners to achieve the Sustainable Development Goals in the Anthropocene. J Nurs Scholarsh. 2021;53(5):552–60. https://doi.org/10.1111/jnu.12672
Harris N, Pisa L, Talioaga S, Vezeau T. Hospitals going green: a holistic view of the issue and the critical role of the nurse leader. Holist Nurs Pract. 2009;23(2):101–11. https://doi.org/10.1097/HNP.0b013e3181a110fe
Phiri MM, MacPherson EE, Panulo M, Chidziwisano K, Kalua K, Chawanangwa M, Chirambo, et al. Preparedness for and impact of COVID-19 on primary health care delivery in urban and rural Malawi: a mixed methods study. BMJ Open. 2022;12(6):e051125. https://doi.org/10.1136/bmjopen-2021-051125
Ojemeni MT, Karanja V, Cadet G, Charles A, Dushimimana E, McMahon C, et al. Fostering nursing leadership: an important key to achieving sustainable development goals and universal health care. Int J Nurs Stud. 2019;100:103421. https://doi.org/10.1016/j.ijnurstu.2019.103421
German E. The environmental or ecological model of care. Nriagu JO. Encyclopedia of Environmental Health. Netherlands:Elsevier Science; 2019. pp. 447–50.
Vasset F, Fagerstrøm L, Frilund M. Sustainable Nursing Leadership in Nordic Health Care Organizations. Scand J Caring Sci. 2021;14(2):2–1527.
Kallio H, Pietilä AM, Kangasniemi M. Environmental responsibility in nursing in hospitals: a modified Delphi study of nurses’ views. J Clin Nurs. 2020;29(21–22):4045–56. https://doi.org/10.1111/jocn.15429
Richardson J, Grose J, Bradbury M, Kelsey J. Developing awareness of sustainability in nursing and midwifery using a scenario-based approach: evidence from a pre and post educational intervention study. Nurse Educ Today. 2017;54:51–5. https://doi.org/10.1016/j.nedt.2017.04.022
Luque-Alcaraz OM, Gomera A, Ruíz Á, Aparicio-Martinez P, Vaquero-Abellan M. Validation of the Spanish Version of the questionnaire on environmental awareness in nursing (NEAT). Healthcare. 2022;10(8):1420. https://doi.org/10.3390/healthcare10081420
Amezcua M. El Trabajo De Campo Etnográfico En Salud. Index Enferm (Gran). 2000;30:30–5.
Jamali HR. Does research using qualitative methods (grounded theory, ethnography, and phenomenology) have more impact? Libr Inform Sci Res. 2018;40(3):201–7. https://doi.org/10.1016/j.lisr.2018.09.002
Cowie J, Nicoll A, Dimova ED, Campbell P, Duncan EA. The barriers and facilitators influencing the sustainability of hospital-based interventions: a systematic review. BMC Health Serv Res. 2020;20(1):588. https://doi.org/10.1186/s12913-020-05434-9
Kircher M, Doheny BM, Raab K, Onello E, Gingerich S, Potter T. Understanding the knowledge, attitudes, and practices of Healthcare professionals toward Climate Change and Health in Minnesota. Challenges. 2022;13(2):57. https://doi.org/10.3390/challe13020057
Boström M, Andersson E, Berg M, Gustafsson K, Gustavsson E, Hysing E, et al. Conditions for transformative learning for Sustainable Development: A Theoretical Review and Approach. Sustainability. 2018;10(12):4479. https://doi.org/10.3390/su10124479
Polivka BJ, Chaudry RV, Crawford JM. Public Health nurses’ knowledge and attitudes regarding Climate Change. Environ Health Perspecti. 2012;120(3):321–5. https://doi.org/10.1289/ehp.1104025
Hsieh PL, Chen SH, Chang LC. School nurses’ perceptions, knowledge, and related factors Associated with evidence-based practice in Taiwan. Int J Environ Res Public Health. 2018;15(9):1845. https://doi.org/10.3390/ijerph15091845
Rojas-Perez HL, Díaz-Vásquez MA, Díaz-Manchay RJ, Zeña-Ñañez S, Failoc-Rojas VE, Smith D. Nurses’ environmental practices in Northern Peruvian hospitals. Workplace Health Saf. 2024;72(2):68–74. https://doi.org/10.1177/21650799231163130
Anåker A, Nilsson M, Holmner Å, Elf M. Nurses’ perceptions of climate and environmental issues: a qualitative study. J Adv Nurs. 2015;71(8):1883–91. https://doi.org/10.1111/jan.12655
Kallio H, Pietilä AM, Johnson M, Kangasniemi M. Systematic methodological review: developing a framework for a qualitative semi-structured interview guide. J Adv Nurs. 2016;72(12):2954–65. https://doi.org/10.1111/jan.13031
International Council of Nurses. International Nurses Day 2023 report. Value, protect, respect and invest in our nurses for a sustainable future for nursing and health care.2023. https://www.icn.ch/news/icn-marks-international-nurses-day-launch-its-our-nurses-our-future-campaign . Accessed 25 Apr 2023.
Download references
Acknowledgements
The authors would like to thank the Excellent Official Nursing School and all the professionals who participated in this research for their support.
This research received no external funding; however, the project did receive an award from the Excellent Official Nursing School in Cordoba, Spain, in 2020.
Author information
Authors and affiliations.
Neurosurgery Department, Hospital Universitario Reina Sofía, Andalusian Health Care System, 14071, Cordoba, Spain
Olga María Luque-Alcaraz
Environmental Protection Office (SEPA), University of Córdoba, Campus Rabanales, 14014, Córdoba, Spain
Olga María Luque-Alcaraz, Antonio Gomera & Manuel Vaquero-Abellán
GE 10 Research Groups of Clinical-Epidemiological Research in Primary Care, University Biomedical Program for Occupational Medicine, Occupational Epidemiology and Sustainability, Maimonides Institute of Biomedicine of Cordoba (IMIBIC), 14071, Cordoba, Spain
Olga María Luque-Alcaraz, Pilar Aparicio-Martínez & Manuel Vaquero-Abellán
Nursing, Pharmacology and Physiotherapy Department, Faculty of Medicine and Nursing, University of Cordoba, 14071, Cordoba, Spain
Pilar Aparicio-Martínez & Manuel Vaquero-Abellán
GA16 Lifestyles, Innovation and Health, Maimonides Institute of Biomedicine of Cordoba (IMIBIC), 14071, Cordoba, Spain
You can also search for this author in PubMed Google Scholar
Contributions
A.G. and M. V-A. conceived and designed the study, and O.M. L. and P.A-M. acquired the data, analyzed and interpreted the data, and drafted the article. The publication and supervision of the article were the responsibility of A.G. and M. V-A. All authors contributed equally to the writing and preparation of the final manuscript.
Corresponding author
Correspondence to Pilar Aparicio-Martínez .
Ethics declarations
Ethical approval and consent to participate.
Ethical approval was obtained from the Ethics Committee of Reina Sofia Hospital of Cordoba, which is part of the Andalusian Health Care System in Spain (Act No. 267, ref.3605). This research was in line with the Organic Law 3/2018 of December 5 on the Protection of Personal Data and Guarantee of Digital Rights as well as the Nursing Ethics Code and the 1964 Declaration of Helsinki. The participants were informed of the study’s purpose before participation; their informed consent was obtained, and they were informed that they were able to withdraw from the study at any stage. All the data were obtained after informed consent was collected; in addition, the data were anonymized and saved securely in a database, thereby maintaining all stipulations of the Personal Data Law.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Luque-Alcaraz, O.M., Aparicio-Martínez, P., Gomera, A. et al. The environmental awareness of nurses as environmentally sustainable health care leaders: a mixed method analysis. BMC Nurs 23 , 229 (2024). https://doi.org/10.1186/s12912-024-01895-z
Download citation
Received : 26 June 2023
Accepted : 26 March 2024
Published : 03 April 2024
DOI : https://doi.org/10.1186/s12912-024-01895-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Environmental health
- Attitude of health personnel
- Sustainable development
- Health Knowledge, attitudes, and practices
- Organizational Culture
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
1. Clinical Nursing Research Topics. Analyze the use of telehealth/virtual nursing to reduce inpatient nurse duties. Discuss the impact of evidence-based respiratory interventions on patient outcomes in critical care settings. Explore the effectiveness of pain management protocols in pediatric patients. 2.
That is why they need to be solved, and research topics related to nursing ethics present a good opportunity for highlighting them: The role of ethical values in the nursing decision-making process. Particular ethics of data collection in primary care. The ethical dilemma of abortion. Moral choice in opioid addiction.
This research topic could explore strategies for improving nursing leadership and. Discover the best research topics for nursing students with our comprehensive list of 14 relevant and interesting ideas. Explore topics like patient outcomes, healthcare-associated infections, end-of-life care, cultural diversity, and more.
The diverse range of nursing education research paper topics listed above provides a solid foundation for exploring various aspects of nursing education, from theories and concepts to curriculum development, teaching and learning strategies, assessment and measurement, simulation, technology integration, continuing education, leadership and ...
TABLE 11-1 Research Topics for the Future of Nursing, 2020-2030. Topic ... Integration of social determinants of health in nursing education, practice, and research. 16th Report to the Secretary of the U.S. Department of Health and Human Services and the U.S. Congress. Washington, DC: Health Resources and Services Administration.
Here, we'll explore a variety of nursing-related research ideas and topic thought-starters, including general nursing, medical-surgical nursing, pediatric nursing, obstetrics and gynaecological nursing, ICU and mental health nursing. NB - This is just the start…. The topic ideation and evaluation process has multiple steps.
Nursing Education Perspectives is the official research journal of the National League for Nursing. Lean more about the journal and subscribe today! ... Nursing Education Perspectives. 44(6):380-381, November/December 2023. Abstract. Favorite; PDF. Permissions Buy ...
Nurse Educator provides practical information and research related to nursing education, with topics ranging from curriculum, teaching and technology in nursing. ... Concept-based learning activities can effectively support specialty nursing education in primary and ambulatory care settings. ... Agency for Healthcare Research and Quality ...
A New Era. Oermann, Marilyn H. PhD, RN, ANEF, FAAN. Author Affiliation: Editor-in-Chief, Nurse Educator, and Thelma M. Ingles Professor of Nursing, Duke University School of Nursing, Durham, North Carolina. The author declares no conflicts of interest. Correspondence: Dr Oermann, Duke University School of Nursing, DUMC 3322, 307 Trent Drive ...
Nurse Education Today is the leading international journal providing a forum for the publication of high quality original research, review and debate in the discussion of nursing, midwifery and interprofessional health care education, publishing papers which contribute to the advancement of educational theory and pedagogy that support the evidence-based practice for educationalists worldwide.
To help nursing students and professionals, we have compiled a list of 26 categories and 260 research ideas related to nursing research topics. These categories include a large number of nursing research topics, including nursing ethics, paediatric nursing, mental health nursing, nursing education, nursing informatics, community health nursing ...
Exploring innovative approaches to nursing education and training, such as simulation-based learning and online learning, is a growing area of nursing research. Such research can help identify effective ways to prepare nursing students for their future roles in the healthcare system. List of Nursing Research Topics: Nursing Education
The Essentials documents published by the American Association of Colleges of Nursing (AACN) have guided curricular development across baccalaureate and higher degree programs since the mid-1980s (AACN, 2019a).In response to shifts within healthcare delivery, AACN began revisions to the Essentials documents in 2018. Since that time, collaboration between academe and practice has resulted in a ...
2. Mental Health Nursing Research Articles Topics. Research papers focusing on mental health are still one of the most read and referred papers. And there's still more scope for research on topics such as: Evaluating the concept of Integrated Mental and Physical Health Care. Psychiatric Nursing and Mental Health.
Impacts of nursing ethics on evidence-based practice. Strategies to address the implementation gap between practice, research, and knowledge in nursing. Using social media to promote the dissemination of evidence-based practice. Strategies for implementing and translating evidence-based practice. Benefits of frequently training nursing staff on ...
The 2024-2027 research priorities include: Build the science of nursing education through the generation and translation of innovative teaching and learning strategies. Build a diverse nurse faculty capacity and enhance teaching practice. Create teaching and learning environments that enhance the diversity, equity, and inclusivity for student ...
Throughout the coming decade, it will be essential for nursing education to evolve rapidly in order to prepare nurses who can meet the challenges articulated in this report with respect to addressing social determinants of health (SDOH), improving population health, and promoting health equity. Nurses will need to be educated to care for a population that is both aging, with declining mental ...
Anne Dabrow Woods is the chief nurse at Wolters Kluwer, Health, Learning, Research and Practice.She drives the strategic development of evidence-based solutions for nurses and nursing institutions. A nurse for over 37 years and a nurse practitioner since 1998, Dabrow Woods currently practices as an acute care/critical care nurse practitioner at Penn Medicine, Chester County Hospital.
The mission of the National Institute of Nursing Research (NINR) is to promote and improve the health of individuals, families, and communities. To achieve this mission, NINR supports and conducts clinical and basic research and research training on health and illness, research that spans and integrates the behavioral and biological sciences, and that develops the scientific basis for clinical ...
The Future of Nursing Education: Reimagined is a special issue of the journal Nursing Education Perspectives that explores how nursing education can adapt to the changing needs and challenges of the health care system. The issue features articles on topics such as curriculum transformation, diversity and inclusion, interprofessional education, simulation, technology, and innovation. The issue ...
Results. This article summarizes the nursing higher education literature reviewed and provides processes and content related to four topic areas in nursing higher education. The descriptions assist researchers in learning more about the complexity of both the action research process and the varied outcomes.
Keith Rischer shares his insights and resources on various topics related to nursing education, such as mentoring clinical faculty, finding a healthy work-life balance, and active learning. He also answers a question from a drained nurse educator and offers some tips to cope with burnout and stress.
As a nursing student, you must be prepared to write unending research papers in college and university. Some students find it challenging to develop nursing education research topics to write about due to the wide nature of the field. When selecting the most intriguing one, it is simple to become confused. This article lists 150 amazing nursing education research topics you can use in your paper.
Background People worldwide are concerned with the possibility of climate change, microplastics, air pollution, and extreme weather affecting human health. Countries are implementing measures to reduce environmental impacts. Nurses play a vital role, primarily through Green Teams, in the process of promoting sustainable practices and minimizing the environmental footprint of health care ...
The Journal of Nursing Research (JNR) is comprised of original articles that come from a variety of national and international institutions and reflect trends and issues of contemporary nursing practice in Taiwan. ... Topics cover not only the field of nursing but also related fields such as psychology, education, management and statistics ...