Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- Systematic Review | Definition, Example, & Guide

Systematic Review | Definition, Example & Guide
Published on June 15, 2022 by Shaun Turney . Revised on November 20, 2023.
A systematic review is a type of review that uses repeatable methods to find, select, and synthesize all available evidence. It answers a clearly formulated research question and explicitly states the methods used to arrive at the answer.
They answered the question “What is the effectiveness of probiotics in reducing eczema symptoms and improving quality of life in patients with eczema?”
In this context, a probiotic is a health product that contains live microorganisms and is taken by mouth. Eczema is a common skin condition that causes red, itchy skin.
Table of contents
What is a systematic review, systematic review vs. meta-analysis, systematic review vs. literature review, systematic review vs. scoping review, when to conduct a systematic review, pros and cons of systematic reviews, step-by-step example of a systematic review, other interesting articles, frequently asked questions about systematic reviews.
A review is an overview of the research that’s already been completed on a topic.
What makes a systematic review different from other types of reviews is that the research methods are designed to reduce bias . The methods are repeatable, and the approach is formal and systematic:
- Formulate a research question
- Develop a protocol
- Search for all relevant studies
- Apply the selection criteria
- Extract the data
- Synthesize the data
- Write and publish a report
Although multiple sets of guidelines exist, the Cochrane Handbook for Systematic Reviews is among the most widely used. It provides detailed guidelines on how to complete each step of the systematic review process.
Systematic reviews are most commonly used in medical and public health research, but they can also be found in other disciplines.
Systematic reviews typically answer their research question by synthesizing all available evidence and evaluating the quality of the evidence. Synthesizing means bringing together different information to tell a single, cohesive story. The synthesis can be narrative ( qualitative ), quantitative , or both.
Prevent plagiarism. Run a free check.
Systematic reviews often quantitatively synthesize the evidence using a meta-analysis . A meta-analysis is a statistical analysis, not a type of review.
A meta-analysis is a technique to synthesize results from multiple studies. It’s a statistical analysis that combines the results of two or more studies, usually to estimate an effect size .
A literature review is a type of review that uses a less systematic and formal approach than a systematic review. Typically, an expert in a topic will qualitatively summarize and evaluate previous work, without using a formal, explicit method.
Although literature reviews are often less time-consuming and can be insightful or helpful, they have a higher risk of bias and are less transparent than systematic reviews.
Similar to a systematic review, a scoping review is a type of review that tries to minimize bias by using transparent and repeatable methods.
However, a scoping review isn’t a type of systematic review. The most important difference is the goal: rather than answering a specific question, a scoping review explores a topic. The researcher tries to identify the main concepts, theories, and evidence, as well as gaps in the current research.
Sometimes scoping reviews are an exploratory preparation step for a systematic review, and sometimes they are a standalone project.
Receive feedback on language, structure, and formatting
Professional editors proofread and edit your paper by focusing on:
- Academic style
- Vague sentences
- Style consistency
See an example

A systematic review is a good choice of review if you want to answer a question about the effectiveness of an intervention , such as a medical treatment.
To conduct a systematic review, you’ll need the following:
- A precise question , usually about the effectiveness of an intervention. The question needs to be about a topic that’s previously been studied by multiple researchers. If there’s no previous research, there’s nothing to review.
- If you’re doing a systematic review on your own (e.g., for a research paper or thesis ), you should take appropriate measures to ensure the validity and reliability of your research.
- Access to databases and journal archives. Often, your educational institution provides you with access.
- Time. A professional systematic review is a time-consuming process: it will take the lead author about six months of full-time work. If you’re a student, you should narrow the scope of your systematic review and stick to a tight schedule.
- Bibliographic, word-processing, spreadsheet, and statistical software . For example, you could use EndNote, Microsoft Word, Excel, and SPSS.
A systematic review has many pros .
- They minimize research bias by considering all available evidence and evaluating each study for bias.
- Their methods are transparent , so they can be scrutinized by others.
- They’re thorough : they summarize all available evidence.
- They can be replicated and updated by others.
Systematic reviews also have a few cons .
- They’re time-consuming .
- They’re narrow in scope : they only answer the precise research question.
The 7 steps for conducting a systematic review are explained with an example.
Step 1: Formulate a research question
Formulating the research question is probably the most important step of a systematic review. A clear research question will:
- Allow you to more effectively communicate your research to other researchers and practitioners
- Guide your decisions as you plan and conduct your systematic review
A good research question for a systematic review has four components, which you can remember with the acronym PICO :
- Population(s) or problem(s)
- Intervention(s)
- Comparison(s)
You can rearrange these four components to write your research question:
- What is the effectiveness of I versus C for O in P ?
Sometimes, you may want to include a fifth component, the type of study design . In this case, the acronym is PICOT .
- Type of study design(s)
- The population of patients with eczema
- The intervention of probiotics
- In comparison to no treatment, placebo , or non-probiotic treatment
- The outcome of changes in participant-, parent-, and doctor-rated symptoms of eczema and quality of life
- Randomized control trials, a type of study design
Their research question was:
- What is the effectiveness of probiotics versus no treatment, a placebo, or a non-probiotic treatment for reducing eczema symptoms and improving quality of life in patients with eczema?
Step 2: Develop a protocol
A protocol is a document that contains your research plan for the systematic review. This is an important step because having a plan allows you to work more efficiently and reduces bias.
Your protocol should include the following components:
- Background information : Provide the context of the research question, including why it’s important.
- Research objective (s) : Rephrase your research question as an objective.
- Selection criteria: State how you’ll decide which studies to include or exclude from your review.
- Search strategy: Discuss your plan for finding studies.
- Analysis: Explain what information you’ll collect from the studies and how you’ll synthesize the data.
If you’re a professional seeking to publish your review, it’s a good idea to bring together an advisory committee . This is a group of about six people who have experience in the topic you’re researching. They can help you make decisions about your protocol.
It’s highly recommended to register your protocol. Registering your protocol means submitting it to a database such as PROSPERO or ClinicalTrials.gov .
Step 3: Search for all relevant studies
Searching for relevant studies is the most time-consuming step of a systematic review.
To reduce bias, it’s important to search for relevant studies very thoroughly. Your strategy will depend on your field and your research question, but sources generally fall into these four categories:
- Databases: Search multiple databases of peer-reviewed literature, such as PubMed or Scopus . Think carefully about how to phrase your search terms and include multiple synonyms of each word. Use Boolean operators if relevant.
- Handsearching: In addition to searching the primary sources using databases, you’ll also need to search manually. One strategy is to scan relevant journals or conference proceedings. Another strategy is to scan the reference lists of relevant studies.
- Gray literature: Gray literature includes documents produced by governments, universities, and other institutions that aren’t published by traditional publishers. Graduate student theses are an important type of gray literature, which you can search using the Networked Digital Library of Theses and Dissertations (NDLTD) . In medicine, clinical trial registries are another important type of gray literature.
- Experts: Contact experts in the field to ask if they have unpublished studies that should be included in your review.
At this stage of your review, you won’t read the articles yet. Simply save any potentially relevant citations using bibliographic software, such as Scribbr’s APA or MLA Generator .
- Databases: EMBASE, PsycINFO, AMED, LILACS, and ISI Web of Science
- Handsearch: Conference proceedings and reference lists of articles
- Gray literature: The Cochrane Library, the metaRegister of Controlled Trials, and the Ongoing Skin Trials Register
- Experts: Authors of unpublished registered trials, pharmaceutical companies, and manufacturers of probiotics
Step 4: Apply the selection criteria
Applying the selection criteria is a three-person job. Two of you will independently read the studies and decide which to include in your review based on the selection criteria you established in your protocol . The third person’s job is to break any ties.
To increase inter-rater reliability , ensure that everyone thoroughly understands the selection criteria before you begin.
If you’re writing a systematic review as a student for an assignment, you might not have a team. In this case, you’ll have to apply the selection criteria on your own; you can mention this as a limitation in your paper’s discussion.
You should apply the selection criteria in two phases:
- Based on the titles and abstracts : Decide whether each article potentially meets the selection criteria based on the information provided in the abstracts.
- Based on the full texts: Download the articles that weren’t excluded during the first phase. If an article isn’t available online or through your library, you may need to contact the authors to ask for a copy. Read the articles and decide which articles meet the selection criteria.
It’s very important to keep a meticulous record of why you included or excluded each article. When the selection process is complete, you can summarize what you did using a PRISMA flow diagram .
Next, Boyle and colleagues found the full texts for each of the remaining studies. Boyle and Tang read through the articles to decide if any more studies needed to be excluded based on the selection criteria.
When Boyle and Tang disagreed about whether a study should be excluded, they discussed it with Varigos until the three researchers came to an agreement.
Step 5: Extract the data
Extracting the data means collecting information from the selected studies in a systematic way. There are two types of information you need to collect from each study:
- Information about the study’s methods and results . The exact information will depend on your research question, but it might include the year, study design , sample size, context, research findings , and conclusions. If any data are missing, you’ll need to contact the study’s authors.
- Your judgment of the quality of the evidence, including risk of bias .
You should collect this information using forms. You can find sample forms in The Registry of Methods and Tools for Evidence-Informed Decision Making and the Grading of Recommendations, Assessment, Development and Evaluations Working Group .
Extracting the data is also a three-person job. Two people should do this step independently, and the third person will resolve any disagreements.
They also collected data about possible sources of bias, such as how the study participants were randomized into the control and treatment groups.
Step 6: Synthesize the data
Synthesizing the data means bringing together the information you collected into a single, cohesive story. There are two main approaches to synthesizing the data:
- Narrative ( qualitative ): Summarize the information in words. You’ll need to discuss the studies and assess their overall quality.
- Quantitative : Use statistical methods to summarize and compare data from different studies. The most common quantitative approach is a meta-analysis , which allows you to combine results from multiple studies into a summary result.
Generally, you should use both approaches together whenever possible. If you don’t have enough data, or the data from different studies aren’t comparable, then you can take just a narrative approach. However, you should justify why a quantitative approach wasn’t possible.
Boyle and colleagues also divided the studies into subgroups, such as studies about babies, children, and adults, and analyzed the effect sizes within each group.
Step 7: Write and publish a report
The purpose of writing a systematic review article is to share the answer to your research question and explain how you arrived at this answer.
Your article should include the following sections:
- Abstract : A summary of the review
- Introduction : Including the rationale and objectives
- Methods : Including the selection criteria, search method, data extraction method, and synthesis method
- Results : Including results of the search and selection process, study characteristics, risk of bias in the studies, and synthesis results
- Discussion : Including interpretation of the results and limitations of the review
- Conclusion : The answer to your research question and implications for practice, policy, or research
To verify that your report includes everything it needs, you can use the PRISMA checklist .
Once your report is written, you can publish it in a systematic review database, such as the Cochrane Database of Systematic Reviews , and/or in a peer-reviewed journal.
In their report, Boyle and colleagues concluded that probiotics cannot be recommended for reducing eczema symptoms or improving quality of life in patients with eczema. Note Generative AI tools like ChatGPT can be useful at various stages of the writing and research process and can help you to write your systematic review. However, we strongly advise against trying to pass AI-generated text off as your own work.
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Student’s t -distribution
- Normal distribution
- Null and Alternative Hypotheses
- Chi square tests
- Confidence interval
- Quartiles & Quantiles
- Cluster sampling
- Stratified sampling
- Data cleansing
- Reproducibility vs Replicability
- Peer review
- Prospective cohort study
Research bias
- Implicit bias
- Cognitive bias
- Placebo effect
- Hawthorne effect
- Hindsight bias
- Affect heuristic
- Social desirability bias
A literature review is a survey of scholarly sources (such as books, journal articles, and theses) related to a specific topic or research question .
It is often written as part of a thesis, dissertation , or research paper , in order to situate your work in relation to existing knowledge.
A literature review is a survey of credible sources on a topic, often used in dissertations , theses, and research papers . Literature reviews give an overview of knowledge on a subject, helping you identify relevant theories and methods, as well as gaps in existing research. Literature reviews are set up similarly to other academic texts , with an introduction , a main body, and a conclusion .
An annotated bibliography is a list of source references that has a short description (called an annotation ) for each of the sources. It is often assigned as part of the research process for a paper .
A systematic review is secondary research because it uses existing research. You don’t collect new data yourself.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Turney, S. (2023, November 20). Systematic Review | Definition, Example & Guide. Scribbr. Retrieved April 8, 2024, from https://www.scribbr.com/methodology/systematic-review/
Is this article helpful?

Shaun Turney
Other students also liked, how to write a literature review | guide, examples, & templates, how to write a research proposal | examples & templates, what is critical thinking | definition & examples, what is your plagiarism score.

Handbook of Research Methods in Health Social Sciences pp 805–826 Cite as
Conducting a Systematic Review: A Practical Guide
- Freya MacMillan 2 ,
- Kate A. McBride 3 ,
- Emma S. George 4 &
- Genevieve Z. Steiner 5
- Reference work entry
- First Online: 13 January 2019
2247 Accesses
2 Citations
It can be challenging to conduct a systematic review with limited experience and skills in undertaking such a task. This chapter provides a practical guide to undertaking a systematic review, providing step-by-step instructions to guide the individual through the process from start to finish. The chapter begins with defining what a systematic review is, reviewing its various components, turning a research question into a search strategy, developing a systematic review protocol, followed by searching for relevant literature and managing citations. Next, the chapter focuses on documenting the characteristics of included studies and summarizing findings, extracting data, methods for assessing risk of bias and considering heterogeneity, and undertaking meta-analyses. Last, the chapter explores creating a narrative and interpreting findings. Practical tips and examples from existing literature are utilized throughout the chapter to assist readers in their learning. By the end of this chapter, the reader will have the knowledge to conduct their own systematic review.
- Systematic review
- Search strategy
- Risk of bias
- Heterogeneity
- Meta-analysis
- Forest plot
- Funnel plot
- Meta-synthesis
This is a preview of subscription content, log in via an institution .
Buying options
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Barbour RS. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog? BMJ. 2001;322(7294):1115–7.
Article Google Scholar
Butler A, Hall H, Copnell B. A guide to writing a qualitative systematic review protocol to enhance evidence-based practice in nursing and health care. Worldviews Evid-Based Nurs. 2016;13(3):241–9.
Cook DJ, Mulrow CD, Haynes RB. Systematic reviews: synthesis of best evidence for clinical decisions. Ann Intern Med. 1997;126(5):376–80.
Dixon-Woods M, Bonas S, Booth A, Jones DR, Miller T, Sutton AJ, … Young B. How can systematic reviews incorporate qualitative research? A critical perspective. Qual Res. 2006;6(1):27–44. https://doi.org/10.1177/1468794106058867 .
Greenhalgh T. How to read a paper: the basics of evidence-based medicine. 4th ed. Chichester/Hoboken: Wiley-Blackwell; 2010.
Google Scholar
Hannes K, Lockwood C, Pearson A. A comparative analysis of three online appraisal instruments’ ability to assess validity in qualitative research. Qual Health Res. 2010;20(12):1736–43. https://doi.org/10.1177/1049732310378656 .
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions (Version 5.1.0 [updated March 2011]). The Cochrane Collaboration; 2011. http://handbook-5-1.cochrane.org/
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, … Sterne JAC. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343. https://doi.org/10.1136/bmj.d5928 .
Hillier S, Grimmer-Somers K, Merlin T, Middleton P, Salisbury J, Tooher R, Weston A. FORM: an Australian method for formulating and grading recommendations in evidence-based clinical guidelines. BMC Med Res Methodol. 2011;11:23. https://doi.org/10.1186/1471-2288-11-23 .
Humphreys DK, Panter J, Ogilvie D. Questioning the application of risk of bias tools in appraising evidence from natural experimental studies: critical reflections on Benton et al., IJBNPA 2016. Int J Behav Nutr Phys Act. 2017; 14 (1):49. https://doi.org/10.1186/s12966-017-0500-4 .
King R, Hooper B, Wood W. Using bibliographic software to appraise and code data in educational systematic review research. Med Teach. 2011;33(9):719–23. https://doi.org/10.3109/0142159x.2011.558138 .
Koelemay MJ, Vermeulen H. Quick guide to systematic reviews and meta-analysis. Eur J Vasc Endovasc Surg. 2016;51(2):309. https://doi.org/10.1016/j.ejvs.2015.11.010 .
Lucas PJ, Baird J, Arai L, Law C, Roberts HM. Worked examples of alternative methods for the synthesis of qualitative and quantitative research in systematic reviews. BMC Med Res Methodol. 2007;7:4–4. https://doi.org/10.1186/1471-2288-7-4 .
MacMillan F, Kirk A, Mutrie N, Matthews L, Robertson K, Saunders DH. A systematic review of physical activity and sedentary behavior intervention studies in youth with type 1 diabetes: study characteristics, intervention design, and efficacy. Pediatr Diabetes. 2014;15(3):175–89. https://doi.org/10.1111/pedi.12060 .
MacMillan F, Karamacoska D, El Masri A, McBride KA, Steiner GZ, Cook A, … George ES. A systematic review of health promotion intervention studies in the police force: study characteristics, intervention design and impacts on health. Occup Environ Med. 2017. https://doi.org/10.1136/oemed-2017-104430 .
Matthews L, Kirk A, MacMillan F, Mutrie N. Can physical activity interventions for adults with type 2 diabetes be translated into practice settings? A systematic review using the RE-AIM framework. Transl Behav Med. 2014;4(1):60–78. https://doi.org/10.1007/s13142-013-0235-y .
Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel group randomized trials. BMC Med Res Methodol. 2001;1:2. https://doi.org/10.1186/1471-2288-1-2 .
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097 .
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. https://doi.org/10.1186/2046-4053-4-1 .
Mulrow CD, Cook DJ, Davidoff F. Systematic reviews: critical links in the great chain of evidence. Ann Intern Med. 1997;126(5):389–91.
Peters MDJ. Managing and coding references for systematic reviews and scoping reviews in EndNote. Med Ref Serv Q. 2017;36(1):19–31. https://doi.org/10.1080/02763869.2017.1259891 .
Steiner GZ, Mathersul DC, MacMillan F, Camfield DA, Klupp NL, Seto SW, … Chang DH. A systematic review of intervention studies examining nutritional and herbal therapies for mild cognitive impairment and dementia using neuroimaging methods: study characteristics and intervention efficacy. Evid Based Complement Alternat Med. 2017;2017:21. https://doi.org/10.1155/2017/6083629 .
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, … Higgins JP. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355. https://doi.org/10.1136/bmj.i4919 .
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57. https://doi.org/10.1093/intqhc/mzm042 .
Tong A, Palmer S, Craig JC, Strippoli GFM. A guide to reading and using systematic reviews of qualitative research. Nephrol Dial Transplant. 2016;31(6):897–903. https://doi.org/10.1093/ndt/gfu354 .
Uman LS. Systematic reviews and meta-analyses. J Can Acad Child Adolesc Psychiatry. 2011;20(1):57–9.
Download references
Author information
Authors and affiliations.
School of Science and Health and Translational Health Research Institute (THRI), Western Sydney University, Penrith, NSW, Australia
Freya MacMillan
School of Medicine and Translational Health Research Institute, Western Sydney University, Sydney, NSW, Australia
Kate A. McBride
School of Science and Health, Western Sydney University, Sydney, NSW, Australia
Emma S. George
NICM and Translational Health Research Institute (THRI), Western Sydney University, Penrith, NSW, Australia
Genevieve Z. Steiner
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Freya MacMillan .
Editor information
Editors and affiliations.
School of Science and Health, Western Sydney University, Penrith, NSW, Australia
Pranee Liamputtong
Rights and permissions
Reprints and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this entry
Cite this entry.
MacMillan, F., McBride, K.A., George, E.S., Steiner, G.Z. (2019). Conducting a Systematic Review: A Practical Guide. In: Liamputtong, P. (eds) Handbook of Research Methods in Health Social Sciences. Springer, Singapore. https://doi.org/10.1007/978-981-10-5251-4_113
Download citation
DOI : https://doi.org/10.1007/978-981-10-5251-4_113
Published : 13 January 2019
Publisher Name : Springer, Singapore
Print ISBN : 978-981-10-5250-7
Online ISBN : 978-981-10-5251-4
eBook Packages : Social Sciences Reference Module Humanities and Social Sciences Reference Module Business, Economics and Social Sciences
Share this entry
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Reference management. Clean and simple.
How to write a systematic literature review [9 steps]
What is a systematic literature review?
Where are systematic literature reviews used, what types of systematic literature reviews are there, how to write a systematic literature review, 1. decide on your team, 2. formulate your question, 3. plan your research protocol, 4. search for the literature, 5. screen the literature, 6. assess the quality of the studies, 7. extract the data, 8. analyze the results, 9. interpret and present the results, registering your systematic literature review, frequently asked questions about writing a systematic literature review, related articles.
A systematic literature review is a summary, analysis, and evaluation of all the existing research on a well-formulated and specific question.
Put simply, a systematic review is a study of studies that is popular in medical and healthcare research. In this guide, we will cover:
- the definition of a systematic literature review
- the purpose of a systematic literature review
- the different types of systematic reviews
- how to write a systematic literature review
➡️ Visit our guide to the best research databases for medicine and health to find resources for your systematic review.
Systematic literature reviews can be utilized in various contexts, but they’re often relied on in clinical or healthcare settings.
Medical professionals read systematic literature reviews to stay up-to-date in their field, and granting agencies sometimes need them to make sure there’s justification for further research in an area. They can even be used as the starting point for developing clinical practice guidelines.
A classic systematic literature review can take different approaches:
- Effectiveness reviews assess the extent to which a medical intervention or therapy achieves its intended effect. They’re the most common type of systematic literature review.
- Diagnostic test accuracy reviews produce a summary of diagnostic test performance so that their accuracy can be determined before use by healthcare professionals.
- Experiential (qualitative) reviews analyze human experiences in a cultural or social context. They can be used to assess the effectiveness of an intervention from a person-centric perspective.
- Costs/economics evaluation reviews look at the cost implications of an intervention or procedure, to assess the resources needed to implement it.
- Etiology/risk reviews usually try to determine to what degree a relationship exists between an exposure and a health outcome. This can be used to better inform healthcare planning and resource allocation.
- Psychometric reviews assess the quality of health measurement tools so that the best instrument can be selected for use.
- Prevalence/incidence reviews measure both the proportion of a population who have a disease, and how often the disease occurs.
- Prognostic reviews examine the course of a disease and its potential outcomes.
- Expert opinion/policy reviews are based around expert narrative or policy. They’re often used to complement, or in the absence of, quantitative data.
- Methodology systematic reviews can be carried out to analyze any methodological issues in the design, conduct, or review of research studies.
Writing a systematic literature review can feel like an overwhelming undertaking. After all, they can often take 6 to 18 months to complete. Below we’ve prepared a step-by-step guide on how to write a systematic literature review.
- Decide on your team.
- Formulate your question.
- Plan your research protocol.
- Search for the literature.
- Screen the literature.
- Assess the quality of the studies.
- Extract the data.
- Analyze the results.
- Interpret and present the results.
When carrying out a systematic literature review, you should employ multiple reviewers in order to minimize bias and strengthen analysis. A minimum of two is a good rule of thumb, with a third to serve as a tiebreaker if needed.
You may also need to team up with a librarian to help with the search, literature screeners, a statistician to analyze the data, and the relevant subject experts.
Define your answerable question. Then ask yourself, “has someone written a systematic literature review on my question already?” If so, yours may not be needed. A librarian can help you answer this.
You should formulate a “well-built clinical question.” This is the process of generating a good search question. To do this, run through PICO:
- Patient or Population or Problem/Disease : who or what is the question about? Are there factors about them (e.g. age, race) that could be relevant to the question you’re trying to answer?
- Intervention : which main intervention or treatment are you considering for assessment?
- Comparison(s) or Control : is there an alternative intervention or treatment you’re considering? Your systematic literature review doesn’t have to contain a comparison, but you’ll want to stipulate at this stage, either way.
- Outcome(s) : what are you trying to measure or achieve? What’s the wider goal for the work you’ll be doing?
Now you need a detailed strategy for how you’re going to search for and evaluate the studies relating to your question.
The protocol for your systematic literature review should include:
- the objectives of your project
- the specific methods and processes that you’ll use
- the eligibility criteria of the individual studies
- how you plan to extract data from individual studies
- which analyses you’re going to carry out
For a full guide on how to systematically develop your protocol, take a look at the PRISMA checklist . PRISMA has been designed primarily to improve the reporting of systematic literature reviews and meta-analyses.
When writing a systematic literature review, your goal is to find all of the relevant studies relating to your question, so you need to search thoroughly .
This is where your librarian will come in handy again. They should be able to help you formulate a detailed search strategy, and point you to all of the best databases for your topic.
➡️ Read more on on how to efficiently search research databases .
The places to consider in your search are electronic scientific databases (the most popular are PubMed , MEDLINE , and Embase ), controlled clinical trial registers, non-English literature, raw data from published trials, references listed in primary sources, and unpublished sources known to experts in the field.
➡️ Take a look at our list of the top academic research databases .
Tip: Don’t miss out on “gray literature.” You’ll improve the reliability of your findings by including it.
Don’t miss out on “gray literature” sources: those sources outside of the usual academic publishing environment. They include:
- non-peer-reviewed journals
- pharmaceutical industry files
- conference proceedings
- pharmaceutical company websites
- internal reports
Gray literature sources are more likely to contain negative conclusions, so you’ll improve the reliability of your findings by including it. You should document details such as:
- The databases you search and which years they cover
- The dates you first run the searches, and when they’re updated
- Which strategies you use, including search terms
- The numbers of results obtained
➡️ Read more about gray literature .
This should be performed by your two reviewers, using the criteria documented in your research protocol. The screening is done in two phases:
- Pre-screening of all titles and abstracts, and selecting those appropriate
- Screening of the full-text articles of the selected studies
Make sure reviewers keep a log of which studies they exclude, with reasons why.
➡️ Visit our guide on what is an abstract?
Your reviewers should evaluate the methodological quality of your chosen full-text articles. Make an assessment checklist that closely aligns with your research protocol, including a consistent scoring system, calculations of the quality of each study, and sensitivity analysis.
The kinds of questions you'll come up with are:
- Were the participants really randomly allocated to their groups?
- Were the groups similar in terms of prognostic factors?
- Could the conclusions of the study have been influenced by bias?
Every step of the data extraction must be documented for transparency and replicability. Create a data extraction form and set your reviewers to work extracting data from the qualified studies.
Here’s a free detailed template for recording data extraction, from Dalhousie University. It should be adapted to your specific question.
Establish a standard measure of outcome which can be applied to each study on the basis of its effect size.
Measures of outcome for studies with:
- Binary outcomes (e.g. cured/not cured) are odds ratio and risk ratio
- Continuous outcomes (e.g. blood pressure) are means, difference in means, and standardized difference in means
- Survival or time-to-event data are hazard ratios
Design a table and populate it with your data results. Draw this out into a forest plot , which provides a simple visual representation of variation between the studies.
Then analyze the data for issues. These can include heterogeneity, which is when studies’ lines within the forest plot don’t overlap with any other studies. Again, record any excluded studies here for reference.
Consider different factors when interpreting your results. These include limitations, strength of evidence, biases, applicability, economic effects, and implications for future practice or research.
Apply appropriate grading of your evidence and consider the strength of your recommendations.
It’s best to formulate a detailed plan for how you’ll present your systematic review results. Take a look at these guidelines for interpreting results from the Cochrane Institute.
Before writing your systematic literature review, you can register it with OSF for additional guidance along the way. You could also register your completed work with PROSPERO .
Systematic literature reviews are often found in clinical or healthcare settings. Medical professionals read systematic literature reviews to stay up-to-date in their field and granting agencies sometimes need them to make sure there’s justification for further research in an area.
The first stage in carrying out a systematic literature review is to put together your team. You should employ multiple reviewers in order to minimize bias and strengthen analysis. A minimum of two is a good rule of thumb, with a third to serve as a tiebreaker if needed.
Your systematic review should include the following details:
A literature review simply provides a summary of the literature available on a topic. A systematic review, on the other hand, is more than just a summary. It also includes an analysis and evaluation of existing research. Put simply, it's a study of studies.
The final stage of conducting a systematic literature review is interpreting and presenting the results. It’s best to formulate a detailed plan for how you’ll present your systematic review results, guidelines can be found for example from the Cochrane institute .
University Libraries University of Nevada, Reno
- Skill Guides
- Subject Guides
Systematic, Scoping, and Other Literature Reviews: Overview
- Project Planning
What Is a Systematic Review?
Regular literature reviews are simply summaries of the literature on a particular topic. A systematic review, however, is a comprehensive literature review conducted to answer a specific research question. Authors of a systematic review aim to find, code, appraise, and synthesize all of the previous research on their question in an unbiased and well-documented manner. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) outline the minimum amount of information that needs to be reported at the conclusion of a systematic review project.
Other types of what are known as "evidence syntheses," such as scoping, rapid, and integrative reviews, have varying methodologies. While systematic reviews originated with and continue to be a popular publication type in medicine and other health sciences fields, more and more researchers in other disciplines are choosing to conduct evidence syntheses.
This guide will walk you through the major steps of a systematic review and point you to key resources including Covidence, a systematic review project management tool. For help with systematic reviews and other major literature review projects, please send us an email at [email protected] .
Getting Help with Reviews
Organization such as the Institute of Medicine recommend that you consult a librarian when conducting a systematic review. Librarians at the University of Nevada, Reno can help you:
- Understand best practices for conducting systematic reviews and other evidence syntheses in your discipline
- Choose and formulate a research question
- Decide which review type (e.g., systematic, scoping, rapid, etc.) is the best fit for your project
- Determine what to include and where to register a systematic review protocol
- Select search terms and develop a search strategy
- Identify databases and platforms to search
- Find the full text of articles and other sources
- Become familiar with free citation management (e.g., EndNote, Zotero)
- Get access to you and help using Covidence, a systematic review project management tool
Doing a Systematic Review
- Plan - This is the project planning stage. You and your team will need to develop a good research question, determine the type of review you will conduct (systematic, scoping, rapid, etc.), and establish the inclusion and exclusion criteria (e.g., you're only going to look at studies that use a certain methodology). All of this information needs to be included in your protocol. You'll also need to ensure that the project is viable - has someone already done a systematic review on this topic? Do some searches and check the various protocol registries to find out.
- Identify - Next, a comprehensive search of the literature is undertaken to ensure all studies that meet the predetermined criteria are identified. Each research question is different, so the number and types of databases you'll search - as well as other online publication venues - will vary. Some standards and guidelines specify that certain databases (e.g., MEDLINE, EMBASE) should be searched regardless. Your subject librarian can help you select appropriate databases to search and develop search strings for each of those databases.
- Evaluate - In this step, retrieved articles are screened and sorted using the predetermined inclusion and exclusion criteria. The risk of bias for each included study is also assessed around this time. It's best if you import search results into a citation management tool (see below) to clean up the citations and remove any duplicates. You can then use a tool like Rayyan (see below) to screen the results. You should begin by screening titles and abstracts only, and then you'll examine the full text of any remaining articles. Each study should be reviewed by a minimum of two people on the project team.
- Collect - Each included study is coded and the quantitative or qualitative data contained in these studies is then synthesized. You'll have to either find or develop a coding strategy or form that meets your needs.
- Explain - The synthesized results are articulated and contextualized. What do the results mean? How have they answered your research question?
- Summarize - The final report provides a complete description of the methods and results in a clear, transparent fashion.
Adapted from
Types of reviews, systematic review.
These types of studies employ a systematic method to analyze and synthesize the results of numerous studies. "Systematic" in this case means following a strict set of steps - as outlined by entities like PRISMA and the Institute of Medicine - so as to make the review more reproducible and less biased. Consistent, thorough documentation is also key. Reviews of this type are not meant to be conducted by an individual but rather a (small) team of researchers. Systematic reviews are widely used in the health sciences, often to find a generalized conclusion from multiple evidence-based studies.
Meta-Analysis
A systematic method that uses statistics to analyze the data from numerous studies. The researchers combine the data from studies with similar data types and analyze them as a single, expanded dataset. Meta-analyses are a type of systematic review.
Scoping Review
A scoping review employs the systematic review methodology to explore a broader topic or question rather than a specific and answerable one, as is generally the case with a systematic review. Authors of these types of reviews seek to collect and categorize the existing literature so as to identify any gaps.
Rapid Review
Rapid reviews are systematic reviews conducted under a time constraint. Researchers make use of workarounds to complete the review quickly (e.g., only looking at English-language publications), which can lead to a less thorough and more biased review.
Narrative Review
A traditional literature review that summarizes and synthesizes the findings of numerous original research articles. The purpose and scope of narrative literature reviews vary widely and do not follow a set protocol. Most literature reviews are narrative reviews.
Umbrella Review
Umbrella reviews are, essentially, systematic reviews of systematic reviews. These compile evidence from multiple review studies into one usable document.
Grant, Maria J., and Andrew Booth. “A Typology of Reviews: An Analysis of 14 Review Types and Associated Methodologies.” Health Information & Libraries Journal , vol. 26, no. 2, 2009, pp. 91-108. doi: 10.1111/j.1471-1842.2009.00848.x .
- Next: Project Planning >>
How to Write a Systematic Review of the Literature
Affiliations.
- 1 1 Texas Tech University, Lubbock, TX, USA.
- 2 2 University of Florida, Gainesville, FL, USA.
- PMID: 29283007
- DOI: 10.1177/1937586717747384
This article provides a step-by-step approach to conducting and reporting systematic literature reviews (SLRs) in the domain of healthcare design and discusses some of the key quality issues associated with SLRs. SLR, as the name implies, is a systematic way of collecting, critically evaluating, integrating, and presenting findings from across multiple research studies on a research question or topic of interest. SLR provides a way to assess the quality level and magnitude of existing evidence on a question or topic of interest. It offers a broader and more accurate level of understanding than a traditional literature review. A systematic review adheres to standardized methodologies/guidelines in systematic searching, filtering, reviewing, critiquing, interpreting, synthesizing, and reporting of findings from multiple publications on a topic/domain of interest. The Cochrane Collaboration is the most well-known and widely respected global organization producing SLRs within the healthcare field and a standard to follow for any researcher seeking to write a transparent and methodologically sound SLR. Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA), like the Cochrane Collaboration, was created by an international network of health-based collaborators and provides the framework for SLR to ensure methodological rigor and quality. The PRISMA statement is an evidence-based guide consisting of a checklist and flowchart intended to be used as tools for authors seeking to write SLR and meta-analyses.
Keywords: evidence based design; healthcare design; systematic literature review.
- Evidence-Based Medicine* / organization & administration
- Research Design*
- Systematic Reviews as Topic*
Literature Review vs Systematic Review
- Literature Review vs. Systematic Review
- Primary vs. Secondary Sources
- Databases and Articles
- Specific Journal or Article
Subject Guide

Definitions
It’s common to confuse systematic and literature reviews because both are used to provide a summary of the existent literature or research on a specific topic. Regardless of this commonality, both types of review vary significantly. The following table provides a detailed explanation as well as the differences between systematic and literature reviews.
Kysh, Lynn (2013): Difference between a systematic review and a literature review. [figshare]. Available at: http://dx.doi.org/10.6084/m9.figshare.766364
- << Previous: Home
- Next: Primary vs. Secondary Sources >>
- Last Updated: Dec 15, 2023 10:19 AM
- URL: https://libguides.sjsu.edu/LitRevVSSysRev
- Locations and Hours
- UCLA Library
- Research Guides
- Biomedical Library Guides
Systematic Reviews
- Types of Literature Reviews
What Makes a Systematic Review Different from Other Types of Reviews?
- Planning Your Systematic Review
- Database Searching
- Creating the Search
- Search Filters & Hedges
- Grey Literature
- Managing & Appraising Results
- Further Resources
Reproduced from Grant, M. J. and Booth, A. (2009), A typology of reviews: an analysis of 14 review types and associated methodologies. Health Information & Libraries Journal, 26: 91–108. doi:10.1111/j.1471-1842.2009.00848.x
- << Previous: Home
- Next: Planning Your Systematic Review >>
- Last Updated: Mar 1, 2024 10:55 AM
- URL: https://guides.library.ucla.edu/systematicreviews

- Research Process
Systematic Literature Review or Literature Review?
- 3 minute read
- 41.5K views
Table of Contents
As a researcher, you may be required to conduct a literature review. But what kind of review do you need to complete? Is it a systematic literature review or a standard literature review? In this article, we’ll outline the purpose of a systematic literature review, the difference between literature review and systematic review, and other important aspects of systematic literature reviews.
What is a Systematic Literature Review?
The purpose of systematic literature reviews is simple. Essentially, it is to provide a high-level of a particular research question. This question, in and of itself, is highly focused to match the review of the literature related to the topic at hand. For example, a focused question related to medical or clinical outcomes.
The components of a systematic literature review are quite different from the standard literature review research theses that most of us are used to (more on this below). And because of the specificity of the research question, typically a systematic literature review involves more than one primary author. There’s more work related to a systematic literature review, so it makes sense to divide the work among two or three (or even more) researchers.
Your systematic literature review will follow very clear and defined protocols that are decided on prior to any review. This involves extensive planning, and a deliberately designed search strategy that is in tune with the specific research question. Every aspect of a systematic literature review, including the research protocols, which databases are used, and dates of each search, must be transparent so that other researchers can be assured that the systematic literature review is comprehensive and focused.
Most systematic literature reviews originated in the world of medicine science. Now, they also include any evidence-based research questions. In addition to the focus and transparency of these types of reviews, additional aspects of a quality systematic literature review includes:
- Clear and concise review and summary
- Comprehensive coverage of the topic
- Accessibility and equality of the research reviewed
Systematic Review vs Literature Review
The difference between literature review and systematic review comes back to the initial research question. Whereas the systematic review is very specific and focused, the standard literature review is much more general. The components of a literature review, for example, are similar to any other research paper. That is, it includes an introduction, description of the methods used, a discussion and conclusion, as well as a reference list or bibliography.
A systematic review, however, includes entirely different components that reflect the specificity of its research question, and the requirement for transparency and inclusion. For instance, the systematic review will include:
- Eligibility criteria for included research
- A description of the systematic research search strategy
- An assessment of the validity of reviewed research
- Interpretations of the results of research included in the review
As you can see, contrary to the general overview or summary of a topic, the systematic literature review includes much more detail and work to compile than a standard literature review. Indeed, it can take years to conduct and write a systematic literature review. But the information that practitioners and other researchers can glean from a systematic literature review is, by its very nature, exceptionally valuable.
This is not to diminish the value of the standard literature review. The importance of literature reviews in research writing is discussed in this article . It’s just that the two types of research reviews answer different questions, and, therefore, have different purposes and roles in the world of research and evidence-based writing.
Systematic Literature Review vs Meta Analysis
It would be understandable to think that a systematic literature review is similar to a meta analysis. But, whereas a systematic review can include several research studies to answer a specific question, typically a meta analysis includes a comparison of different studies to suss out any inconsistencies or discrepancies. For more about this topic, check out Systematic Review VS Meta-Analysis article.
Language Editing Plus
With Elsevier’s Language Editing Plus services , you can relax with our complete language review of your systematic literature review or literature review, or any other type of manuscript or scientific presentation. Our editors are PhD or PhD candidates, who are native-English speakers. Language Editing Plus includes checking the logic and flow of your manuscript, reference checks, formatting in accordance to your chosen journal and even a custom cover letter. Our most comprehensive editing package, Language Editing Plus also includes any English-editing needs for up to 180 days.

- Publication Recognition
How to Make a PowerPoint Presentation of Your Research Paper

- Manuscript Preparation
What is and How to Write a Good Hypothesis in Research?
You may also like.

Descriptive Research Design and Its Myriad Uses

Five Common Mistakes to Avoid When Writing a Biomedical Research Paper

Making Technical Writing in Environmental Engineering Accessible

To Err is Not Human: The Dangers of AI-assisted Academic Writing

When Data Speak, Listen: Importance of Data Collection and Analysis Methods

Choosing the Right Research Methodology: A Guide for Researchers

Why is data validation important in research?

Writing a good review article
Input your search keywords and press Enter.
- Library Guides
- Literature Reviews
- Choosing a Type of Review
Literature Reviews: Choosing a Type of Review
Selecting a review type.

You'll want to think about the kind of review you are doing. Is it a selective or comprehensive review? Is the review part of a larger work or a stand-alone work ?
For example, if you're writing the Literature Review section of a journal article, that's a selective review which is part of a larger work. Alternatively, if you're writing a review article, that's a comprehensive review which is a stand-alone work. Thinking about this will help you develop the scope of the review.
Defining the Scope of Your Review
This exercise will help define the scope of your Literature Review, setting the boundaries for which literature to include and which to exclude.
A FEW GENERAL CONSIDERATIONS WHEN DEFINING SCOPE
- Which populations to investigate — this can include gender, age, socio-economic status, race, geographic location, etc., if the research area includes humans.
- What years to include — if researching the legalization of medicinal cannabis, you might only look at the previous 20 years; but if researching dolphin mating practices, you might extend many more decades.
- Which subject areas — if researching artificial intelligence, subject areas could be computer science, robotics, or health sciences
- How many sources — a selective review for a class assignment might only need ten, while a comprehensive review for a dissertation might include hundreds. There is no one right answer.
- There will be many other considerations that are more specific to your topic.
Most databases will allow you to limit years and subject areas, so look for those tools while searching. See the Searching Tips tab for information on how use these tools.
Four Common Types of Reviews
Literature review.
- Often used as a generic term to describe any type of review
- More precise definition: Published materials that provide an examination of published literature . Can cover wide range of subjects at various levels of comprehensiveness.
- Identifies gaps in research, explains importance of topic, hypothesizes future work, etc.
- Usually written as part of a larger work like a journal article or dissertation
SCOPING REVIEW
- Conducted to address broad research questions with the goal of understanding the extent of research that has been conducted.
- Provides a preliminary assessment of the potential size and scope of available research literature. It aims to identify the nature and extent of research evidence (usually including ongoing research)
- Doesn't assess the quality of the literature gathered (i.e. presence of literature on a topic shouldn’t be conflated w/ the quality of that literature)
SYSTEMATIC REVIEW
- Common in the health sciences
- Goal: collect all literature that meets specific criteria (methodology, population, treatment, etc.) and then appraise its quality and synthesize it
- Follows strict protocol for literature collection, appraisal and synthesis
- Typically performed by research teams
- Takes 12-18 months to complete
- Often written as a stand alone work
META-ANALYSIS
- Goes one step further than a systematic review by statistically combining the results of quantitative studies to provide a more precise effect of the results.
- Evidence Synthesis Guide Learn more about Systematic Reviews, Scoping Reviews, Rapid Reviews, Umbrella Reviews, Meta-Analyses
Attribution
Thanks to Librarian Jamie Niehof at the University of Michigan for providing permission to reuse and remix this Literature Reviews guide.
Evidence Synthesis Guide
- Evidence Synthesis Guide Learn more about Systematic Reviews, Scoping Reviews, Rapid Reviews, Umbrella Reviews, and Meta-Analyses
Which Review is Right for You?

The Right Review tool has questions about your lit review process and plans. It offers a qualitative and quantitative option. At completion, you are given a lit review type recommendation.
More Review Types

This article by Sutton & Booth (2019) explores 48 distinct types of Literature Reviews:
- Last Updated: Apr 4, 2024 4:51 PM
- URL: https://info.library.okstate.edu/literaturereviews
- Open access
- Published: 01 April 2024
The impact of housing prices on residents’ health: a systematic review
- Ashmita Grewal 1 ,
- Kirk J. Hepburn 1 ,
- Scott A. Lear 1 ,
- Marina Adshade 2 &
- Kiffer G. Card 1
BMC Public Health volume 24 , Article number: 931 ( 2024 ) Cite this article
360 Accesses
19 Altmetric
Metrics details
Rising housing prices are becoming a top public health priority and are an emerging concern for policy makers and community leaders. This report reviews and synthesizes evidence examining the association between changes in housing price and health outcomes.
We conducted a systematic literature review by searching the SCOPUS and PubMed databases for keywords related to housing price and health. Articles were screened by two reviewers for eligibility, which restricted inclusion to original research articles measuring changes in housing prices and health outcomes, published prior to June 31st, 2022.
Among 23 eligible studies, we found that changes in housing prices were heterogeneously associated with physical and mental health outcomes, with multiple mechanisms contributing to both positive and negative health outcomes. Income-level and home-ownership status were identified as key moderators, with lower-income individuals and renters experience negative health consequences from rising housing prices. This may have resulted from increased stress and financial strain among these groups. Meanwhile, the economic benefits of rising housing prices were seen to support health for higher-income individuals and homeowners – potentially due to increased wealth or perception of wealth.
Conclusions
Based on the associations identified in this review, it appears that potential gains to health associated with rising housing prices are inequitably distributed. Housing policies should consider the health inequities born by renters and low-income individuals. Further research should explore mechanisms and interventions to reduce uneven economic impacts on health.
Peer Review reports
Introduction
In contemporary society, the structures we live in, as well as our legal relationships to these structures, are intertwined with our fundamental senses of self and belonging [ 1 , 2 , 3 ]. For decades, homeownership has been recognized as a core measure of success [ 4 , 5 ]. Recognizing the importance of housing, studies have variously examined the effects of wide-ranging housing-related factors on health, including housing quality, overcrowding, neighbourhood deprivation, social cohesion, housing density, housing suitability or sufficiency, and neighbourhood socioeconomic status [ 6 , 7 ]. While these effects continue to be explored, it is generally agreed that housing is a fundamental determinant of health [ 7 ], which broadly exerts impacts on health through a variety of mechanisms.
Indeed, housing-related health effects arise from specific housing conditions, as well as the legal conditions that define our relationships to these spaces, and our emotional attachments to these various factors. For example, living and owning a home can create access to opportunities that can further bolster health [ 8 ]. Similarly, housing related factors—such as indebtedness, mortgage stress, and credit problems—can cause severe mental health problems, depression, and suicide ideation [ 9 , 10 ]. With these factors in mind, people in most countries face numerous barriers to securing their right to a home [ 5 , 11 ], and a wide array of policies have been proposed and implemented to address these barriers [ 12 , 13 , 14 ]. In addition to these factors, the location of a home, the quality of a building, or the neighbourhood context in which a home exists are also hugely influential to health [ 7 , 15 , 16 ].
In conceptualizing these varied mechanisms, it is important to consider both direct and indirect mechanisms through which the relationship between housing and health manifests. Direct effects predominantly emerge from psycho-physiological stress responses. Elevated housing costs can induce chronic stress, leading to mental health conditions, like anxiety and depression, and other health problems [ 17 ]. Indirectly, escalating housing prices exert economic pressures that limit individuals' capacity to allocate resources towards health-promoting activities and necessities. This economic strain can result in compromised nutrition, reduced access to healthcare services, and diminished ability to manage chronic conditions, therefore, exacerbating health disparities. Moreover, the financial burden can lead to other lifestyle changes that further impair physical and mental well-being, such as increased substance use or reduced physical activity.
Despite these effects being documented in previous studies, there are no systematic reviews on the impact of rising housing prices on health. The present review aims to examine the effect of housing price on health by considering whether changes in housing market price impact the health of residents living in an area. To accomplish this aim, we conduct a systematic review. This review is especially timely since housing prices have risen in the past five years at an alarming rate.
Article search
The first step in our multi-stage systematic literature review was to manually identify relevant articles through a rudimentary search on SCOPUS and PubMed ( Appendix B ). We then created a list of keywords to use for our search. Keywords aimed to identify articles that measured changes in housing prices and health impacts, Appendix A outlines how we identified keywords and provides a complete list of selected keywords. After conducting the keyword search in PubMed and SCOPUS, duplicates were removed and the remaining articles were then uploaded to Rayyan, an online software that aids in systematic reviews [ 18 ]. To assess whether our search is comprehensive, AG confirmed that the articles identified in the rudimentary initial search, mentioned earlier, were also included in this search. For the purposes of this literature review, we define health using the language provided by the World Health Organization (1948): “health is a complete state of mental, physical, and social well-being, and not merely the absence of disease.” As such, no additional inclusion or exclusion criteria were used to exclude or include specific health conditions. We felt this was appropriate given that this is the first literature review on this topic and because after a review of included articles, it was apparent that a wide variety of health outcomes have been considered. Furthermore, the biopsychosocial models of health that we engage to inform our view that housing prices have direct and indirect effects on health underscore that diverse and nuanced pathways across various mental and physical domains of health are likely important to consider. Using Rayyan, AG and LW reviewed the titles of each manuscript to remove articles that were clearly not relevant to this review [ 18 ]. The application of inclusion and exclusion criteria resulted in 21 articles that were directly relevant to this review. AG and LW also searched the reference lists for these 21 articles to identify any additional articles. These missed articles were added to our final inclusion list, creating a total of 23 included articles.
Data extraction
Data were extracted by AG and LW from each of the identified and included articles and AG re-reviewed the data extraction to verify accuracy. Extracted variables included: first author name, year of publication, years of data collection, sample size, location(s) of study, study design (e.g., case control, cohort, cross-sectional, serial cross-sectional study), analysis type (e.g., regression), outcome, explanatory factor, confounders/mediators/moderators, and a summary of primary findings (including effect size measures). This data extraction is provided as Table 1 .
Risk of bias assessment
During the data extraction process, we conducted an assessment based on the Joanna Briggs Institute Critical Appraisal Tools [ 42 ]. Each study was classified according to its study design and rated using the appropriate tool designed for each study. However, despite varying methodological quality, no studies were excluded based on risk of bias assessment, as there were no clear sources of systematic bias with sufficient likelihood of challenging the conclusions of the source studies.
Narrative synthesis
During the data extraction and risk of bias assessment phases, AG and LW recorded general notes on each of the studies. These notes, along with the extracted information, were used to construct a narrative synthesis of the evidence. This process was guided by Popay et al.’s [ 43 ] Guidance for Narrative Synthesis in Systematic Reviews. A narrative approach was selected to allow for an examination of the potential complexity inherent in the synthesis of findings across contexts, time periods, and populations to provide a nuanced discussion of what roles housing and rental markets might play in shaping health, with attention to both outcomes and potential mechanisms. Findings within study classes were reviewed to determine potential mediation and moderation. These explorations informed the development of a list of key points used to organize the presentation of our results. We then integrated and contextualized these findings with those from other relevant (though excluded) studies identified through our review process and from the texts of the included articles.
Included studies
Our keyword search returned 6,180 articles. Of these, 5,590 were removed based on review of the abstract and title as they were not directly related to our review topic (i.e., they did not measure changes in housing price and/or health outcomes). The remaining articles were reviewed based on their full-texts and a final list of 26 articles were considered for inclusion. However, five articles were not able to be retrieved (even after emailing the original authors), leaving us with 21 articles. The reference lists and bibliographies for these 21 included articles were then screened and two additional articles were thus included in our review resulting in a final sample of 23 articles. Figure 1 shows the flow diagram for included studies and these studies are listed in Appendix B .
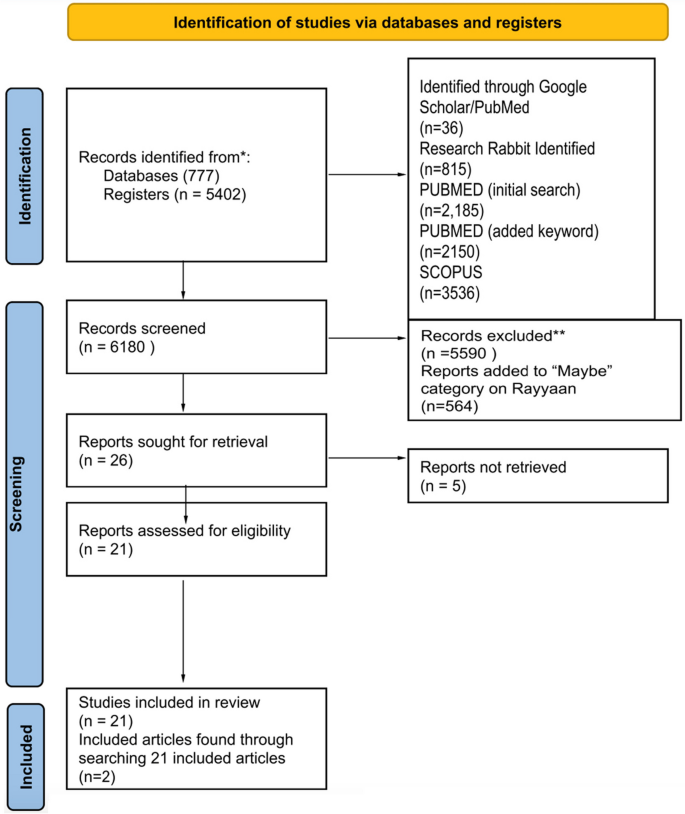
PRISMA systematic review flow diagram
Dates and locations of studies
A full description of studies is included in Table 1 . Studies were published from 2013–2022. Ten studies were from East Asia, eight from the United States, three in Europe, one from Australia, and one included nine countries (France, Japan, Netherlands, Spain, Switzerland, Sweden, United Kingdom, USA).
Study design
Of the included studies, ten had a longitudinal study design, and thirteen studies were serial cross-sectional studies. Studies examined the effect of housing prices on health over time by repeatedly surveying a specific geographical area or population. One study included both qualitative and quantitative data collection.
Outcome variable measurement
Most studies compared multiple outcomes. Seven studies focused on mental health as the outcome variable—utilizing various measures, including self-rated mental health, standardized scales for depression or anxiety, and receipt of pharmaceutical prescriptions [ 22 , 32 , 33 , 35 , 40 , 41 ]. Nine studies analyzed the impact of housing prices on physical health—utilizing various measures of physical health, including objective assessments of physical health (e.g., body mass), self-rated physical health assessments, reports of specific health conditions (e.g., COVID-19), reported health behaviours (e.g., alcohol use, smoking), and mortality ( [ 24 , 28 , 29 , 37 , 44 , 30 , 36 , 38 , 39 ]). Seven studies included both physical and mental health measures as their outcome variable [ 19 , 20 , 23 , 26 , 27 , 34 , 45 ].
Explanatory variable measurement
Housing prices were measured using many different types of data, including house price index, self-reported housing price (extracted from surveys), and average market price. Many studies used house price index as a measure of housing prices [ 19 , 21 , 22 , 30 , 38 , 39 , 41 ]. Zhang & Zhang [ 33 ] included self-reported housing price. Alternatively, many studies examined housing market prices using existing survey data [ 20 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 31 , 32 , 34 , 35 , 36 , 37 , 40 ].
Key findings
Studies included in our review highlighted a plurality of results when testing the relationships between housing prices and health. As shown in Tables 2 (physical health) and Table 3 (mental health), the included articles reported mixed findings across the outcomes explored. Given the heterogeneity of findings regarding the associations between housing prices and health outcomes, several authors examined potential moderators and mediators in attempt to understand the mechanisms at play. These included studies examine the role of wealth effects (by comparing effects on homeowners and renters), socioeconomic status (e.g., income level), and broader economic forces (e.g., area-level improvements). While keeping these pathways in mind, there are likely other alternative explanations beyond those explored. However, these appear to be the most dominant frameworks used to understand the effects in our included studies.
Wealth effects
The first major pathway has been described as a “wealth effect” – which produces different effects for homeowners and renters [ 19 , 20 , 23 , 25 , 27 , 33 , 35 , 37 , 45 ]. For example, Hamoudi & Dowd [ 37 ] report that homeowners living in areas with steep price increases, perceive this as an increase in their overall wealth, resulting in positive health outcomes (not observed for renters). Similarly, Zhang & Zhang [ 33 ] show that increases in house prices has a positive effect on homeowner’s subjective well-being. De & Segura [ 30 ] specifically notes that price depreciation causes homeowners to experience feelings of a loss of wealth, leading to increases in alcohol consumption. Among studies that fail to show a wealth effect, Daysal et al. [ 29 ] shows that rising prices in Denmark do not impact households due to the buffering effects of government supports. Conversely, when examining the effects among renters, Wang & Liang [ 31 ] argue that rising housing prices have detrimental "strain" effect, which is also observed in several studies included in our review [ 25 , 27 , 38 , 39 , 45 ].
Income level
In addition to the wealth and strain effects illustrated through studies among homeowners and renters, many studies also examined the mediating effects of income [ 19 , 20 , 22 , 28 , 29 , 30 , 32 , 33 , 35 , 38 , 39 , 40 ]. Several of these studies show that housing unaffordability constrains spending and that low-income individuals are particularly impacted [ 22 , 24 , 33 , 38 ]. For example, Wong et al. [ 39 ] show that housing prices lead to reduced fruit consumption. However, results also show positive impacts for low-income homeowners – as exemplified by work showing that low-income homeowners are more sensitive to housing price gains [ 38 , 40 ].
Broader economic forces
In considering both mechanisms described above, authors of included studies have also considered whether housing prices are merely an indicator of broader economic trends merits consideration. The most common strategy for accounting for this has been to include other indicators that might capture area level improvements. Indeed, most studies controlled for both individual characteristics or variables, such as age, gender, marital status, years of education, race/ethnicity, and employment status [ 20 , 23 , 24 , 25 , 26 , 27 , 29 , 30 , 32 , 34 , 35 , 37 , 39 , 40 , 41 , 45 ], and a variety of economic factors, including individual income, country-level median income, and local area characteristics [ 19 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 30 , 32 , 36 , 37 , 38 , 39 , 40 , 44 , 45 ]. These factors are important to control for because rising housing prices can indicate a growing economy in which there are substantial improvements to neighbourhoods and communities [ 27 , 29 , 33 , 38 , 40 ]. As such, the observed improvements in health could simply arise from broader economic benefits (rather than being specifically attributable to housing prices) [ 31 , 33 ]. However, generally speaking studies showed that there were independent effects of housing price or value, even after controlling for local area level improvements, and wider economic conditions [ 19 , 27 , 38 ].
Strength of effects
Given heterogeneity in the direction of effects, the lack of standardization in the reporting of effect sizes from study to study, differences in the measurement of exposure and outcome variables, and variation in the inclusion of mediators, moderators, and confounders, we did not conduct a meta-analysis to describe the effect size of housing price on health. However, housing prices appear to exert influence on health and wellbeing with statistically significant effects across various health-related outcomes (See Table 1 for range of effect measures). The effects generally appear to be smaller when considering specific health conditions and greater when considering more subjective and more broad definitions of health (e.g., self-rated health). Of course, at a population-level, even relatively small effect sizes may pose a considerable challenge. For example, Xu & Wang [ 36 ] report that a 10% increase in housing prices is associated with a 6.5% increase in probability of reporting a chronic disease – a relatively small increase on a person-level, but when scaled could easily pose a considerable burden to the health system. In summary, further careful measurement and methodological refinement is needed to quantify the effects of housing prices on various health conditions. For any given health condition, this will require multiple well-designed studies across place and time. Such replication is particularly important given the observed sensitivity of findings to the inclusion of confounders, moderators, and mediators.
Primary findings
While examining whether changes in housing prices are associated with changes in health, we recognized it is difficult to establish a directional and causal relationship between housing price and health. This is particularly true given that health may increase opportunities for home ownership and economic success [ 3 , 46 , 47 , 48 , 49 ]. Nevertheless, given the wealth of literature highlighting housing affordability as a key determinant of health [ 7 , 9 , 10 ], it is reasonably anticipated that rising housing prices would be associated with worse health outcomes among individuals who do not own housing. However, based on analyses of the studies included in this review, the relationship between housing price and health is complex and nuanced, with a significant degree of heterogeneity across outcomes and populations.
First, this review illuminates that changing housing prices impacted different people differently, depending on for example, income level, gender and/or homeownership status [ 19 , 22 , 25 ]. The negative impact of housing price on health for renters and low-income individuals could be due to the existential angst from being excluded from home ownership, which is often considered an important indicator of social class and success [ 8 ]. However, this could also be due to the cost effect that is created from the rising house prices, subsequently raising low-income owners and renters’ cost of living [ 31 ]. Additionally, renting may be associated with lower neighbourhood tenure, especially when individuals are priced out of a neighbourhood [ 8 ]. As a result, they may experience deleterious health effects associated with loneliness, social isolation, lack of neighbourhood cohesion, and community disconnectedness [ 8 ]. Likewise, the positive effect observed among homeowners and high-income individuals may be explained by increases in psychological safety leading to changes in health behaviors, for example, knowing they have invested in a home that will support them or their heirs financially, people may be better able to focus on their well-being. As well, homeowners may be able to directly leverage the value of their home to gain access to additional capital and investment opportunities – which could support increased financial wellbeing [ 8 ].
The effects of housing on health can be conceptualized as arising from two sources. It appears that rising “cost effects” (the increased costs of houses and the costs passed on to tenants) are inversely correlated with health while “wealth effects” (the contributions of housing price to person wealth) contribute positively to health (for example, for homeowners and investors whose wealth increases due to the rising cost of housing). The balance of these effects differs depending on their unique impact on individuals – with lower income people and renters more strongly impacted by cost effects, and higher income people and homeowners more strongly impacted by wealth effects.
In considering these effects, we note that there is likely considerable geographic, temporal, and contextual variation in the health effects of rising housing prices. For example, rising housing prices may occur alongside neighbourhood improvements (or degradation) and economic booms (or recessions) [ 45 ], which themselves are associated with improvements (or deterioration) to health [ 8 ]. As such, the presence of these factors may obscure or interact with the gains to health. Similarly, variations across cultures and countries may change how individuals internalize the rising housing prices [ 50 ], causing them to experience greater or lesser distress in reaction to rising prices.
Limitations of included studies and directions for future research
Given these two primary factors, research highlights several opportunities for improving this literature. First, future studies should give more careful attention to how moderators and mediators are conceptualized. For example, “home-owners” are hardly a homogenous class of individuals: some own their homes outright and others are paying mortgages that offer varying levels of security (e.g., fixed vs. variable mortgages, 5-year vs. 30-year mortgages) [ 8 ]. Second, a broader range of effect moderators should be explored. For example, few studies specifically examined the health effects of rising home prices on vulnerable populations, including young adults and first time home buyers who may be especially disadvantaged by rapidly growing housing prices [ 50 ]. Similarly, isolating effects as arising from economic, legal, environmental, and social pathways can help identify strategies for mitigating health harms. For example, it may be important to understand whether changes to neighbourhood environments drive health harms as opposed to changes in personal financial status. Third, more within-person studies are needed to understand the potential mechanisms and situational factors that promote or mitigate the health effects of rising housing prices. Along with use of appropriate, theoretically informed moderators, isolating the within-person effects can help us better quantify the effects of interest to inform policies and prevention strategies. Fourth, longer follow-up times may allow for better understanding regarding the time-horizons of the effects explored. Indeed, it is possible that rising housing prices could have differential effects on the health of a population in the short versus long term. This is particularly important given the interaction between housing prices (which may act as a price signal for investments) and other economic factors with strong potential to increase health [ 8 ]. Fifth, the studies used a variety of measures for housing price and health outcomes – which varied in quality. For example, health outcomes were primarily measured using self-reported measures [ 19 , 20 , 23 , 25 , 26 , 27 , 30 , 31 , 33 , 34 , 35 , 37 , 38 , 39 , 40 , 41 ] – which may be highly sensitive to bias due to the likelihood that individuals might report worse health when they are unhappy with economic factors. Improving measurement of outcomes can be done by leveraging administrative and other data sources. Sixth, it can be difficult to link area-level and individual-level factors, particularly in the context of limited cross-sectional studies or in longitudinal studies with only a few follow-up points. Likewise, many cohort-based studies have limited geographic coverage or insufficient temporal scope. As such, longer, larger, and wider studies are needed to fully ascertain the relationships under consideration.
Implications of findings
Although further research is required to overcome the limitations mentioned, existing evidence indicates that increases in housing prices may significantly influence health outcomes. Future studies should aim to exclude alternative explanations, examine the effects over longer periods, and establish consistent measurement methods to predict the impact of housing prices more accurately on health. The findings of those students will aid policymakers in creating strategies that address the health implications of rising housing prices. Policy makers should develop frameworks that respond to the impacts of rising housing prices on health. Such approaches could be facilitated through frameworks such as the WHO’s Health in All Policies (HiAP) policy, which advocates for the inclusion of health and social impacts among other criteria used throughout decision making processes [ 51 ]. Many studies in this review support this view and describe their work as having important implications for housing and health policy [ 19 , 20 , 21 , 24 , 26 , 27 , 28 , 29 , 31 , 34 , 35 , 37 , 38 , 39 ]. For example, Yuan et al. [ 26 ] notes the importance of directing government support and housing subsidies towards vulnerable groups – though these should be packaged with other policies [ 26 ]. Such supports can apparently buffer against the negative effects of rising housing prices by creating a saftey net that reduces the psychosocial and cognitive effects associated with economic changes in one's personal circumnstance. Arcaya et al. [ 21 ] also recommends governments investigate establishing more mental health facilities in areas where housing price fluctuations impact people's mental health but warns economic development that allows for greater investment in health infrastructure can also lead to increases in housing prices.
Of course, other types of interventions may also be warranted, including broader financial interventions (e.g., direct loans; [ 52 ], those which promote community, neighborhood, and social cohesion among residents [ 53 ], or those that aim to change how people value home ownership [ 26 ]. With respect to this final option, communities should consider whether renting may in fact be a desirable outcome for some individuals and therefore promote a culture in which individuals realize the variety of investment opportunities available to them rather than being overly-focused on a traditional model of investment [ 26 , 32 ]. For example, Zhang & Zhang [ 33 ] writes that homeowners should be provided financial and economic knowledge to better manage wealth gains, however, this could be taken one step further and include the importance of educating people on the dangers on the commodification of housing, to prevent an over reliance on the importance of housing wealth gains.
Limitations of our review
In addition to the limitations specific to studies included in our review, our review itself also has several limitations. First, while we trained two reviewers to conduct article screening, assessed inter-rater reliability as greater than 80%, and adjudicated conflicts with the help of a third reviewer, it is possible some articles that could have been included were excluded due to the many different forms of outcome and explanatory variable measurement. Second, while we have searched multiple databases, used comprehensive key words for our search, and conducted manual searches of the reference lists, it is possible there were studies that we missed and failed to include in this study. That said, it is unlikely the exclusion of these articles would change our conclusion that the literature is currently mixed and that there is a need to flesh out the mechanisms and moderators that link housing prices to health. Third, we were not able to conduct a meta-analysis, and our numeric reports of the number of studies with each characteristic should not be treated as a meta-analysis. Rather, these findings and analyses of these studies should be interpreted as a descriptive analysis that highlights significant heterogeneity of findings and critical inconsistencies in the mechanisms, mediators, and moderators that give rise to these associations. Fourth, we did not exclude any studies based on article quality because we did not find there to be sufficient heterogeneity in the quality of the observational studies to merit exclusion according to variable inclusion, study design, or sampling method. In other words, we sought to avoid introducing bias by arbitrarily excluding articles – particularly given that the number of articles captured here was already relatively low (at least given the diversity of methods, measures, and populations captured). However, future reviews might consider more narrowed inclusion and exclusion criteria when a sufficient body of literature is available for a given outcome. For example, limiting analyses to only well-designed cohort studies might support a more careful selection of articles. Finally, we note that we included studies across a wide variety of health outcomes. While this was done to maximize inclusion (given the wide heterogeneity of measures used), we acknowledge that future research might be strengthened by studying specific pathways linking housing prices to specific health and social outcomes. Such detailed research is greatly needed so as to not only highlight the relevance of housing prices to health but identify strategies for mitigating potential harms of rising housing prices.
Our review shows that there are complex relationships between housing prices and health – with studies arriving to mixed conclusions across a wide-variety of health outcomes and populations. Yet, there is insufficient evidence for a causal relationship, but it appears that if such a relationship exists it likely differs according to homeownership status, income-level, and as a factor of the broader economic and structural forces in play, including the level of economic supports provided by governments for low income individuals. Future research should explore these pathways, moderators, and confounders using long-term, geographically diverse, cohort studies that account for a broad diversity of causal or alternative mechanisms. Such future research will allow for a more nuanced understanding of health and health inequities related to rising housing prices.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Saunders P. The meaning of ‘home’ in contemporary english culture. Hous Stud. 1989;4:177–92.
Article Google Scholar
Shields M. Community belonging and self-perceived health. Health Rep. 2008;19:51–60.
PubMed Google Scholar
Smith A. Exploring the interrelationship between the meanings of homeownership and identity management in a liquid society: a case study approach. [Doctoral dissertation, Keele University] Keele Business School. 2017.
Després C. The meaning of home: literature review and directions for future research and theoretical development. Locke Sci Publ Co Inc. 1991;8:96–115.
Goodman LS, Mayer C. Homeownership and the American Dream. J Econ Perspect. 2018;32:31–58.
Kawachi I. Social Capital and Community Effects on Population and Individual Health. Ann N Y Acad Sci. 1999;896:120–30.
Article CAS PubMed Google Scholar
Rolfe S, Garnham L, Godwin J, Anderson I, Seaman P, Donaldson C. Housing as a social determinant of health and wellbeing: developing an empirically-informed realist theoretical framework. BMC Public Health. 2020;20:1138.
Article PubMed PubMed Central Google Scholar
Rohe WM, Van Zandt S, McCarthy G. Home Ownership and Access to Opportunity. Hous Stud. 2002;17:51–61.
Turunen E, Hiilamo H. Health effects of indebtedness: a systematic review. BMC Public Health. 2014;14:489.
Waldron R, Redmond D. “We’re just existing, not living!” Mortgage stress and the concealed costs of coping with crisis. Hous Stud. 2017;32:584–612.
Lemphers B. Barriers & Opportunities; A Meta-Analysis of Affordable Rental Housing In Canada. Dalhousie University; 2017. https://cdn.dal.ca/content/dam/dalhousie/pdf/faculty/architecture-planning/school-of-planning/pdfs/studentwork/MPlanIndependentStudy/Lemphers-Barriers%20and%20Opportunity-A%20Meta-Analysis%20of%20Affordable%20Rental%20Housing%20in%20Canada-2017.pdf .
Canadian Mortgage and Housing Association. Demand or Supply Side Housing Assistance?. 2019. https://www.cmhc-schl.gc.ca/professionals/housing-markets-data-and-research/housing-research/research-reports/accelerate-supply/research-insight-updating-debate-between-demand-supply-side-housing-assistance .
Glaeser EL. Rethinking the Federal Bias Toward Homeownership. SSRN Electron J. 2011. https://doi.org/10.2139/ssrn.1914468 .
Pomeroy S. Optimizing Demand and Supply Side Housing Assistance Programs. 2016. Carleton University Centre for Urban Research and Education (CURE). https://www.focus-consult.com/wp-content/uploads/Policy-Brief_Optimizing-Supply-and-Demand-Measures-2016.pdf .
Ige-Elegbede J, Pilkington P, Orme J, Williams B, Prestwood E, Black D, et al. Designing healthier neighbourhoods: a systematic review of the impact of the neighbourhood design on health and wellbeing. Cities Health. 2022;6:1004–19.
Article PubMed Google Scholar
Pérez E, Braën C, Boyer G, Mercille G, Rehany É, Deslauriers V, et al. Neighbourhood community life and health: A systematic review of reviews. Health Place. 2020;61: 102238.
Çalıyurt O. The Mental Health Consequences of the Global Housing Crisis. Alpha Psychiatry. 2022;23:264–5.
Rayyan. 2022. https://www.rayyan.ai
Yue D, Ponce NA. Booms and Busts in Housing Market and Health Outcomes for Older Americans. Innov Aging. 2021;5:igab012.
Chen N, Shen Y, Liang H, Guo R. Housing and Adult Health: Evidence from Chinese General Social Survey (CGSS). Int J Environ Res Public Health. 2021;18:916.
Article CAS PubMed PubMed Central Google Scholar
Arcaya MC, Nidam Y, Binet A, Gibson R, Gavin V. Rising home values and Covid-19 case rates in Massachusetts. Soc Sci Med. 2020;265: 113290.
Lee CY, Chen PH, Lin YK. An Exploratory Study of the Association between Housing Price Trends and Antidepressant Use in Taiwan: A 10-Year Population-Based Study. Int J Environ Res Public Health. 2021;18:4839.
Fichera E, Gathergood J. Do Wealth Shocks Affect Health? New Evidence from the Housing Boom. Health Econ. 2016;25:57–69.
Kim I. Spatial distribution of neighborhood-level housing prices and its association with all-cause mortality in Seoul, Korea (2013–2018): A spatial panel data analysis. SSM - Popul Health. 2021;16: 100963.
Hamoudi A, Dowd JB. Housing Wealth, Psychological Well-being, and Cognitive Functioning of Older Americans. J Gerontol Ser B. 2014;69:253–62.
Yuan W, Gong S, Han Y. How does rising housing price affect the health of middle-aged and elderly people? The complementary mediators of social status seeking and competitive saving motive. PLoS ONE. 2020;15: e0243982.
Atalay K, Edwards R, Liu BYJ. Effects of house prices on health: New evidence from Australia. Soc Sci Med. 2017;192:36–48.
Bao W, Tao R, Afzal A, Dördüncü H. Real Estate Prices, Inflation, and Health Outcomes: Evidence From Developed Economies. Front Public Health. 2022;10: 851388.
Daysal NM, Lovenheim M, Siersbæk N, Wasser DN. Home prices, fertility, and early-life health outcomes. J Public Econ. 2021;198:104366.
De PK, Segura-Escano R. Drinking during downturn: New evidence from the housing market fluctuations in the United States during the Great Recession. Econ Hum Biol. 2021;43: 101070.
Wang H-Q, Liang L-Q. How Do Housing Prices Affect Residents’ Health? New Evidence From China. Front Public Health. 2022;9: 816372.
Wei G, Zhu H, Han S, Chen J, Shi L. Impact of house price growth on mental health: Evidence from China. SSM - Popul Health. 2021;13: 100696.
Zhang C, Zhang F. Effects of housing wealth on subjective well-being in urban China. J Hous Built Environ. 2019;34:965–85.
Feng Y, Nie C. The effect of housing price on health: new evidence from China. Appl Econ Lett. 2022;29:1439–46.
Chun H. Do housing price changes affect mental health in South Korea? Ethiop J Health Dev. 2020;34:48–59.
Google Scholar
Xu Y, Wang F. The health consequence of rising housing prices in China. J Econ Behav Organ. 2022;200:114–37.
Hamoudi A, Dowd JB. Physical health effects of the housing boom: quasi-experimental evidence from the health and retirement study. Am J Public Health. 2013;103:1039–45.
Sung J, Qiu Q. The Impact of Housing Prices on Health in the United States Before, During, and After the Great Recession. South Econ J. 2020;86:910–40.
Wong ES, Oddo VM, Jones-Smith JC. Are Housing Prices Associated with Food Consumption? Int J Environ Res Public Health. 2020;17:3882.
Ratcliffe A. Wealth Effects, Local Area Attributes, and Economic Prospects: On the Relationship between House Prices and Mental Wellbeing. Rev Income Wealth. 2015;61:75–92.
Joshi NK. Local house prices and mental health. Int J Health Econ Manag. 2016;16:89–102.
Joanna Briggs Institute. Critical Appraisal Tools. 2022. https://jbi.global/critical-appraisal-tools
Popay J, Roberts H, Sowden AJ, Petticrew M, Arai L, Rodgers ME., Britton, N. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. 2006. https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf .
Arcaya MC, Nidam Y, Binet A, Gibson R, Gavin V. Rising home values and Covid-19 case rates in Massachusetts. Soc Sci Med. 1982;2020(265): 113290.
Wang H-Q, Liang L-Q. How Do Housing Prices Affect Residents’ Health? New Evidence From China. Front Public Health. 2022;9:1–11.
Shlay AB. Low-income Homeownership: American Dream or Delusion? Urban Stud. 2006;43:511–31.
Boehm TP, Schlottmann AM. The dynamics of race, income, and homeownership. J Urban Econ. 2004;55:113–30.
Fazel S, Khosla V, Doll H, Geddes J. The Prevalence of Mental Disorders among the Homeless in Western Countries: Systematic Review and Meta-Regression Analysis. PLOS Med. 2008;5: e225.
McConnell ED. Who has Housing Affordability Problems? Disparities in Housing Cost Burden by Race, Nativity, and Legal Status in Los Angeles. Race Soc Probl. 2013;5:173–90.
Ding Y, Chin L, Lu M, Deng P. Do high housing prices crowd out young professionals?—Micro-evidence from China. Econ Res-Ekon Istraživanja. 2022;36(2):1–19.
CAS Google Scholar
World Health Organization. 2023. https://www.who.int/about/accountability/governance/constitution .
Fernald LC, Hamad R, Karlan D, Ozer EJ, Zinman J. Small individual loans and mental health: a randomized controlled trial among South African adults. BMC Public Health. 2008;8:409.
Silverstein M, Cong Z, Li S. Intergenerational Transfers and Living Arrangements of Older People in Rural China: Consequences for Psychological Well-Being. J Gerontol Ser B. 2006;61:S256–66.
Download references
Acknowledgements
We would like to acknowledge the support of Logan White for his support in conducting the literature review.
KGC is supported by a Michael Smith Health Research BC Scholar Award. This project was funded by grants from The Canadian Institutes for Health Research and the GenWell Project.
Author information
Authors and affiliations.
Faculty of Health Sciences, Simon Fraser University, Blusson Hall, 8888 University Dr. , Burnaby, BC, V5A 1S6, Canada
Ashmita Grewal, Kirk J. Hepburn, Scott A. Lear & Kiffer G. Card
Vancouver School of Economics, University of British Columbia, Vancouver, BC, Canada
Marina Adshade
You can also search for this author in PubMed Google Scholar
Contributions
KGC & AG conceptualized the study design. KGC, LW, and AG conducted the literature review, search, and data extraction. KGC & AG drafted the initial manuscript. All authors provided substantive intellectual and editorial revisions and approved the final manuscript.
Corresponding author
Correspondence to Ashmita Grewal .
Ethics declarations
Ethics approval and consent to participate.
This study does not require ethics approval as it is a literature review.
Consent for publication
There are no figures or materials presented in this manuscript that require consent.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Grewal, A., Hepburn, K.J., Lear, S.A. et al. The impact of housing prices on residents’ health: a systematic review. BMC Public Health 24 , 931 (2024). https://doi.org/10.1186/s12889-024-18360-w
Download citation
Received : 04 August 2023
Accepted : 14 March 2024
Published : 01 April 2024
DOI : https://doi.org/10.1186/s12889-024-18360-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Housing price
- Economic stress
- Social determinants of health

BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 23 August 2022
Prognostic risk factors for moderate-to-severe exacerbations in patients with chronic obstructive pulmonary disease: a systematic literature review
- John R. Hurst 1 ,
- MeiLan K. Han 2 ,
- Barinder Singh 3 ,
- Sakshi Sharma 4 ,
- Gagandeep Kaur 3 ,
- Enrico de Nigris 5 ,
- Ulf Holmgren 6 &
- Mohd Kashif Siddiqui 3
Respiratory Research volume 23 , Article number: 213 ( 2022 ) Cite this article
6315 Accesses
20 Citations
33 Altmetric
Metrics details
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality worldwide. COPD exacerbations are associated with a worsening of lung function, increased disease burden, and mortality, and, therefore, preventing their occurrence is an important goal of COPD management. This review was conducted to identify the evidence base regarding risk factors and predictors of moderate-to-severe exacerbations in patients with COPD.
A literature review was performed in Embase, MEDLINE, MEDLINE In-Process, and the Cochrane Central Register of Controlled Trials (CENTRAL). Searches were conducted from January 2015 to July 2019. Eligible publications were peer-reviewed journal articles, published in English, that reported risk factors or predictors for the occurrence of moderate-to-severe exacerbations in adults age ≥ 40 years with a diagnosis of COPD.
The literature review identified 5112 references, of which 113 publications (reporting results for 76 studies) met the eligibility criteria and were included in the review. Among the 76 studies included, 61 were observational and 15 were randomized controlled clinical trials. Exacerbation history was the strongest predictor of future exacerbations, with 34 studies reporting a significant association between history of exacerbations and risk of future moderate or severe exacerbations. Other significant risk factors identified in multiple studies included disease severity or bronchodilator reversibility (39 studies), comorbidities (34 studies), higher symptom burden (17 studies), and higher blood eosinophil count (16 studies).
Conclusions
This systematic literature review identified several demographic and clinical characteristics that predict the future risk of COPD exacerbations. Prior exacerbation history was confirmed as the most important predictor of future exacerbations. These prognostic factors may help clinicians identify patients at high risk of exacerbations, which are a major driver of the global burden of COPD, including morbidity and mortality.
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide [ 1 ]. Based upon disability-adjusted life-years, COPD ranked sixth out of 369 causes of global disease burden in 2019 [ 2 ]. COPD exacerbations are associated with a worsening of lung function, and increased disease burden and mortality (of those patients hospitalized for the first time with an exacerbation, > 20% die within 1 year of being discharged) [ 3 ]. Furthermore, patients with COPD consider exacerbations or hospitalization due to exacerbations to be the most important disease outcome, having a large impact on their lives [ 4 ]. Therefore, reducing the future risk of COPD exacerbations is a key goal of COPD management [ 5 ].
Being able to predict the level of risk for each patient allows clinicians to adapt treatment and patients to adjust their lifestyle (e.g., through a smoking cessation program) to prevent exacerbations [ 3 ]. As such, identifying high-risk patients using measurable risk factors and predictors that correlate with exacerbations is critical to reduce the burden of disease and prevent a cycle of decline encompassing irreversible lung damage, worsening quality of life (QoL), increasing disease burden, high healthcare costs, and early death.
Prior history of exacerbations is generally thought to be the best predictor of future exacerbations; however, there is a growing body of evidence suggesting other demographic and clinical characteristics, including symptom burden, airflow obstruction, comorbidities, and inflammatory biomarkers, also influence risk [ 6 , 7 , 8 , 9 ]. For example, in the prospective ECLIPSE observational study, the likelihood of patients experiencing an exacerbation within 1 year of follow-up increased significantly depending upon several factors, including prior exacerbation history, forced expiratory volume in 1 s (FEV 1 ), St. George’s Respiratory Questionnaire (SGRQ) score, gastroesophageal reflux, and white blood cell count [ 9 ].
Many studies have assessed predictors of COPD exacerbations across a variety of countries and patient populations. This systematic literature review (SLR) was conducted to identify and compile the evidence base regarding risk factors and predictors of moderate-to-severe exacerbations in patients with COPD.
- Systematic literature review
A comprehensive search strategy was designed to identify English-language studies published in peer-reviewed journals providing data on risk factors or predictors of moderate or severe exacerbations in adults aged ≥ 40 years with a diagnosis of COPD (sample size ≥ 100). The protocol is summarized in Table 1 and the search strategy is listed in Additional file 1 : Table S1. Key biomedical electronic literature databases were searched from January 2015 until July 2019. Other sources were identified via bibliographic searching of relevant systematic reviews.
Study selection process
Implementation and reporting followed the recommendations and standards of the Preferred Reporting Items for Systematic reviews and Meta-analyses (PRISMA) statement [ 10 ]. An independent reviewer conducted the first screening based on titles and abstracts, and a second reviewer performed a quality check of the excluded evidence. A single independent reviewer also conducted the second screening based on full-text articles, with a quality check of excluded evidence performed by a second reviewer. Likewise, data tables of the included studies were generated by one reviewer, and another reviewer performed a quality check of extracted data. Where more than one publication was identified describing a single study or trial, data were compiled into a single entry in the data-extraction table to avoid double counting of patients and studies. One publication was designated as the ‘primary publication’ for the purposes of the SLR, based on the following criteria: most recently published evidence and/or the article that presented the majority of data (e.g., journal articles were preferred over conference abstracts; articles that reported results for the full population were preferred over later articles providing results of subpopulations). Other publications reporting results from the same study were designated as ‘linked publications’; any additional data in the linked publications that were not included in the primary publication were captured in the SLR. Conference abstracts were excluded from the SLR unless they were a ‘linked publication.’
Included studies
A total of 5112 references (Fig. 1 ) were identified from the database searches. In total, 76 studies from 113 publications were included in the review. Primary publications and ‘linked publications’ for each study are detailed in Additional file 1 : Table S2, and study characteristics are shown in Additional file 1 : Table S3. The studies included clinical trials, registry studies, cross-sectional studies, cohort studies, database studies, and case–control studies. All 76 included studies were published in peer-reviewed journals. Regarding study design, 61 of the studies were observational (34 retrospective observational studies, 19 prospective observational studies, four cross-sectional studies, two studies with both retrospective and prospective cohort data, one case–control study, and one with cross-sectional and longitudinal data) and 15 were randomized controlled clinical trials.
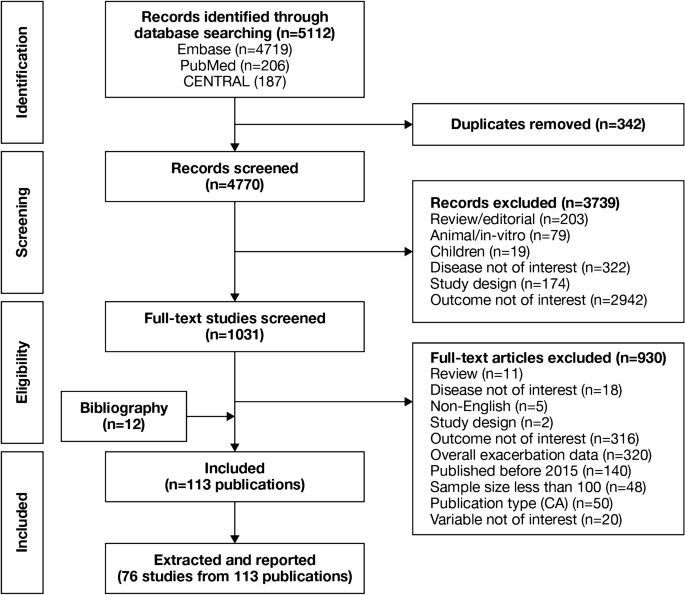
PRISMA flow diagram of studies through the systematic review process. CA conference abstract, CENTRAL Cochrane Central Register of Controlled Trials, PRISMA Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Of the 76 studies, 16 were conducted in North America (13 studies in the USA, two in Canada, and one in Mexico); 26 were conducted in Europe (seven studies in Spain, four in the UK, three in Denmark, two studies each in Bulgaria, the Netherlands, and Switzerland, and one study each in Sweden, Serbia, Portugal, Greece, Germany, and France) and 17 were conducted in Asia (six studies in South Korea, four in China, three in Taiwan, two in Japan, and one study each in Singapore and Israel). One study each was conducted in Turkey and Australia. Fifteen studies were conducted across multiple countries.
The majority of the studies (n = 54) were conducted in a multicenter setting, while 22 studies were conducted in a single-center setting. The sample size among the included studies varied from 118 to 339,389 patients.
Patient characteristics
A total of 75 studies reported patient characteristics (Additional file 1 : Table S4). The mean age was reported in 65 studies and ranged from 58.0 to 75.2 years. The proportion of male patients ranged from 39.7 to 97.6%. The majority of included studies (85.3%) had a higher proportion of males than females.
Exacerbation history (as defined per each study) was reported in 18 of 76 included studies. The proportion of patients with no prior exacerbation was reported in ten studies (range, 0.1–79.5% of patients), one or fewer prior exacerbation in ten studies (range, 46–100%), one or more prior exacerbation in eight studies (range, 18.4–100%), and two or more prior exacerbations in 12 studies (range, 6.1–55.0%).
Prognostic factors of exacerbations
A summary of the risk factors and predictors reported across the included studies is provided in Tables 2 and 3 . The overall findings of the SLR are summarized in Figs. 2 and 3 .
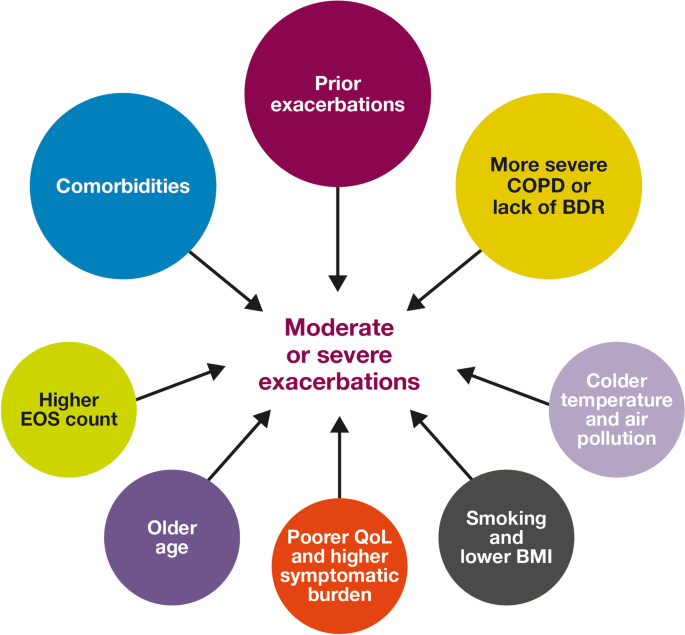
Risk factors for moderate-to-severe exacerbations in patients with COPD. Factors with > 30 supporting studies shown as large circles; factors with ≤ 30 supporting studies shown as small circles and should be interpreted cautiously. BDR bronchodilator reversibility, BMI body mass index, COPD chronic obstructive pulmonary disease, EOS eosinophil, QoL quality of life
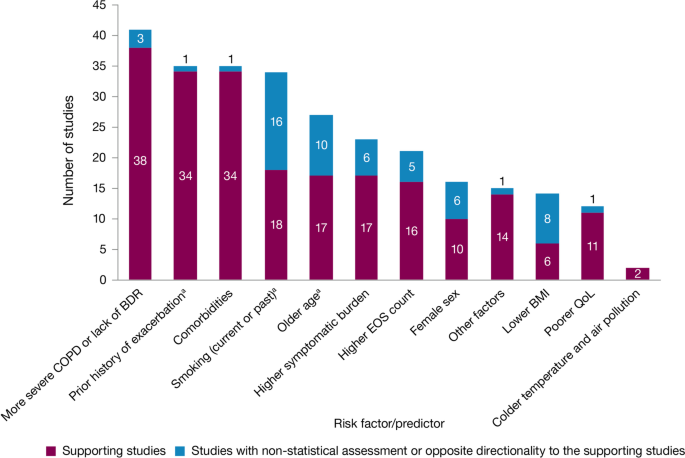
Summary of risk factors for exacerbation events. a Treatment impact studies removed. BDR bronchodilator reversibility, BMI body mass index, COPD chronic obstructive pulmonary disease, EOS eosinophil, QoL quality of life
Exacerbation history within the past 12 months was the strongest predictor of future exacerbations. Across the studies assessing this predictor, 34 out of 35 studies (97.1%) reported a significant association between history of exacerbations and risk of future moderate-to-severe exacerbations (Table 3 ). Specifically, two or more exacerbations in the previous year or at least one hospitalization for COPD in the previous year were identified as reliable predictors of future moderate or severe exacerbations. Even one moderate exacerbation increased the risk of a future exacerbation, with the risk increasing further with each subsequent exacerbation (Fig. 4 ). A severe exacerbation was also found to increase the risk of subsequent exacerbation and hospitalization (Fig. 5 ). Patients experiencing one or more severe exacerbations were more likely to experience further severe exacerbations than moderate exacerbations [ 11 , 12 ]. In contrast, patients with a history of one or more moderate exacerbations were more likely to experience further moderate exacerbations than severe exacerbations [ 11 , 12 ].
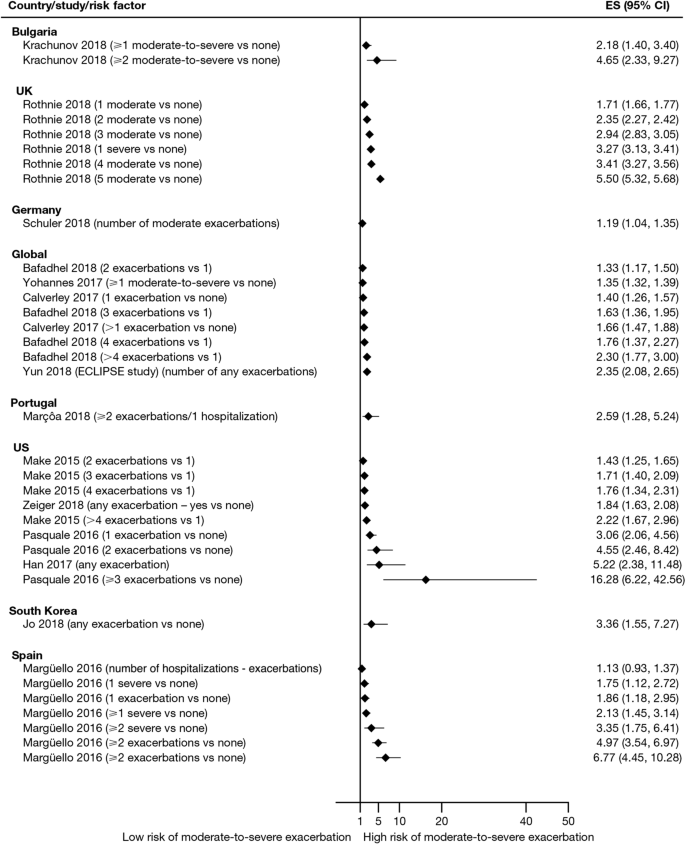
Exacerbation history as a risk factor for moderate-to-severe exacerbations. Yun 2018 included two studies; the study from which data were extracted (COPDGene or ECLIPSE) is listed in parentheses. CI confidence interval, ES effect size
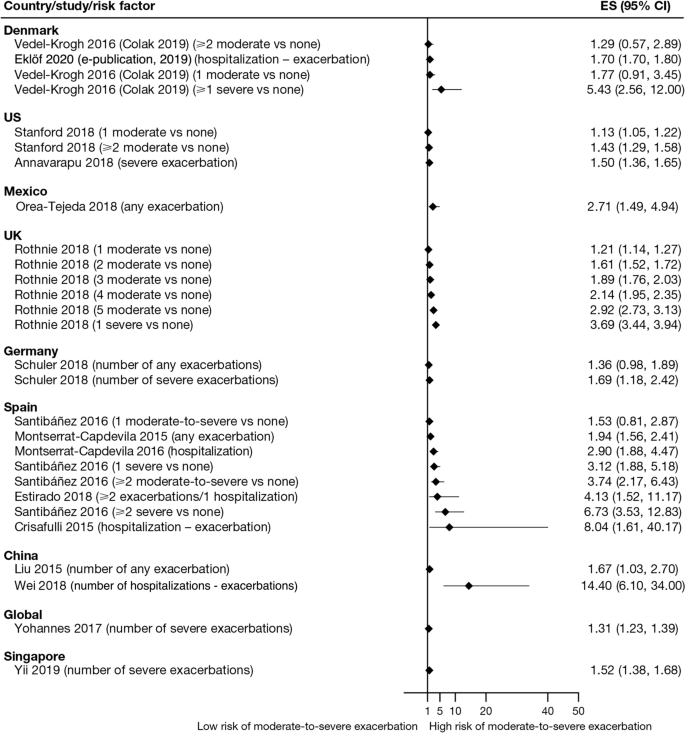
Exacerbation history as a risk factor for severe exacerbations. Where data have been extracted from a linked publication rather than the primary publication, the linked publication is listed in parentheses. CI confidence interval, ES , effect size
Overall, 35 studies assessed the association of comorbidities with the risk of exacerbation. All studies except one (97.1%) reported a positive association between comorbidities and the occurrence of moderate-to-severe exacerbations (Table 3 ). In addition to the presence of any comorbidity, specific comorbidities that were found to significantly increase the risk of moderate-to-severe exacerbations included anxiety and depression, cardiovascular comorbidities, gastroesophageal reflux disease/dyspepsia, and respiratory comorbidities (Fig. 6 ). Comorbidities that were significant risk factors for severe exacerbations included cardiovascular, musculoskeletal, and respiratory comorbidities, diabetes, and malignancy (Fig. 7 ). Overall, the strongest association between comorbidities and COPD readmissions in the emergency department was with cardiovascular disease. The degree of risk for both moderate-to-severe and severe exacerbations also increased with the number of comorbidities. A Dutch cohort study found that 88% of patients with COPD had at least one comorbidity, with hypertension (35%) and coronary heart disease (19%) being the most prevalent. In this cohort, the comorbidities with the greatest risk of frequent exacerbations were pulmonary cancer (odds ratio [OR] 1.85) and heart failure (OR 1.72) [ 7 ].
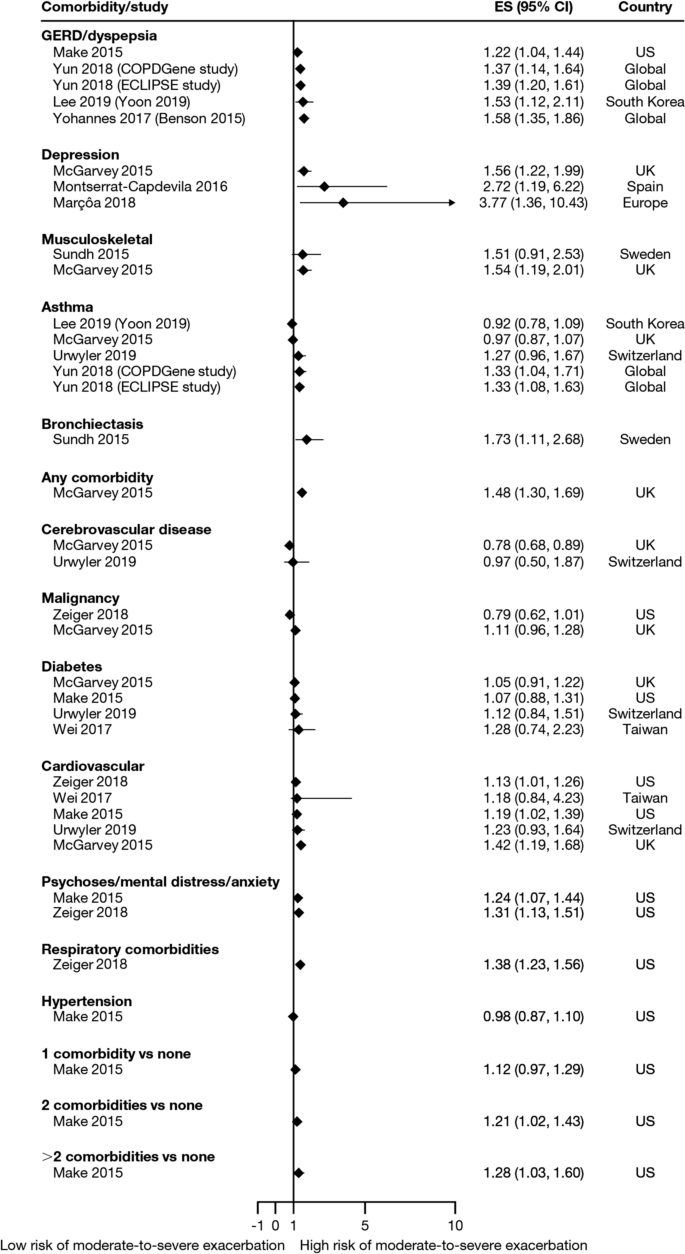
Comorbidities as risk factors for moderate-to-severe exacerbations. Yun 2018 included two studies; the study from which data were extracted (COPDGene or ECLIPSE) is listed in parentheses. Where data have been extracted from a linked publication rather than the primary publication, the linked publication is listed in parentheses. CI confidence interval, ES effect size, GERD gastroesophageal disease
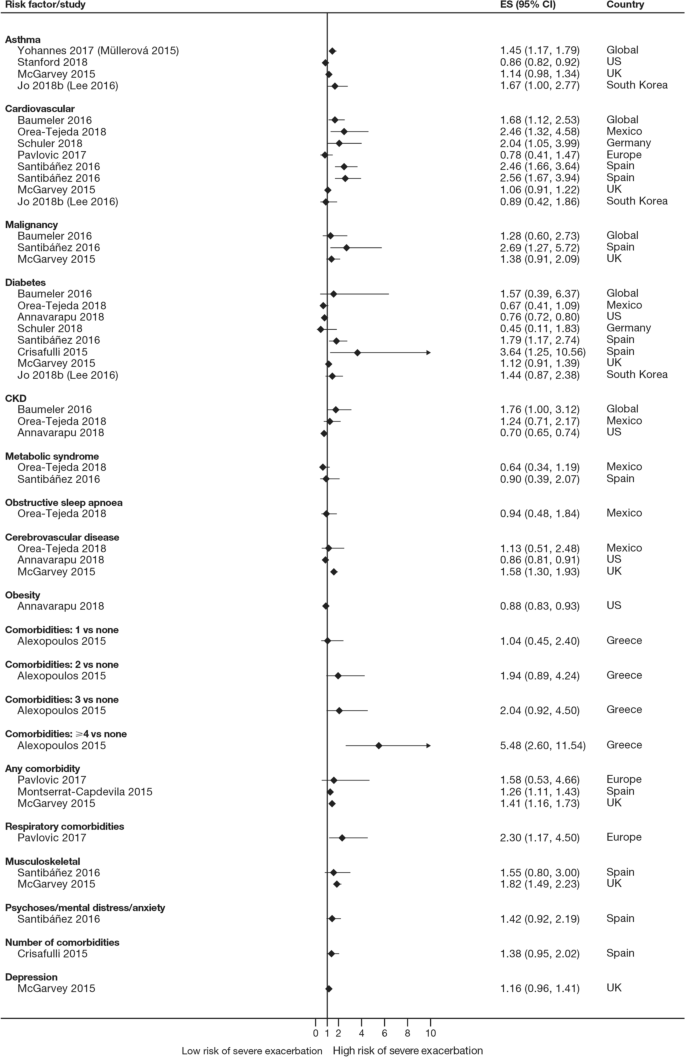
Comorbidities as risk factors for severe exacerbations. Where data have been extracted from a linked publication rather than the primary publication, the linked publication is listed in parentheses. CI confidence interval, CKD , chronic kidney disease, ES effect size
The majority of studies assessing disease severity or bronchodilator reversibility (39/41; 95.1%) indicated a significant positive relation between risk of future exacerbations and greater disease severity, as assessed by greater lung function impairment (in terms of lower FEV 1 , FEV 1 /forced vital capacity ratio, or forced expiratory flow [25–75]/forced vital capacity ratio) or more severe Global Initiative for Chronic Obstructive Lung Disease (GOLD) class A − D, and a positive relationship between risk of future exacerbations and lack of bronchodilator reversibility (Table 3 , Figs. 8 and 9 ).
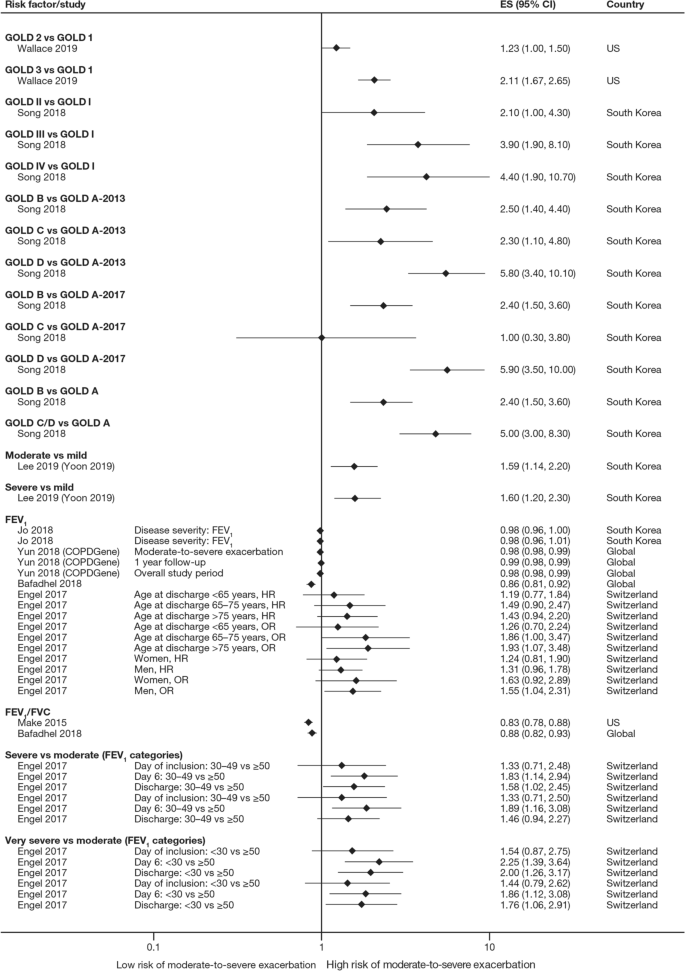
Disease severity as a risk factor for moderate-to-severe exacerbations. Yun 2018 included two studies; the study from which data were extracted (COPDGene or ECLIPSE) is listed in parentheses. Where data have been extracted from a linked publication rather than the primary publication, the linked publication is listed in parentheses. CI confidence interval, ES effect size, FEV 1 f orced expiratory volume in 1 s, FVC , forced vital capacity, GOLD Global Initiative for Obstructive Lung Disease, HR hazard ratio, OR odds ratio
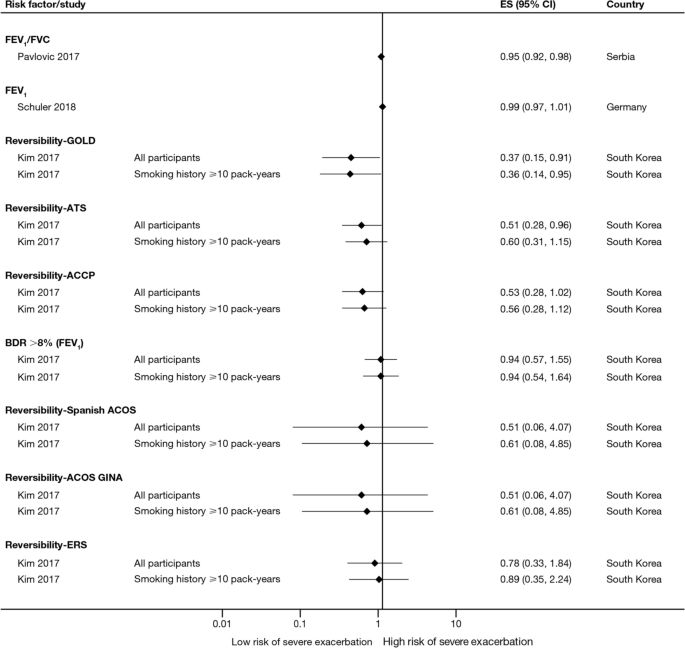
Disease severity and BDR as risk factors for severe exacerbations. ACCP American College of Chest Physicians, ACOS Asthma-COPD overlap syndrome, ATS American Thoracic Society, BDR bronchodilator reversibility, CI confidence interval, ERS European Respiratory Society, ES effect size, FEV 1 forced expiratory volume in 1 s, FVC forced vital capacity, GINA Global Initiative for Asthma, GOLD Global Initiative for Obstructive Lung Disease
Of 21 studies assessing the relationship between blood eosinophil count and exacerbations (Table 3 ), 16 reported estimates for the risk of moderate or severe exacerbations by eosinophil count. A positive association was observed between higher eosinophil count and a higher risk of moderate or severe exacerbations, particularly in patients not treated with an inhaled corticosteroid (ICS); however, five studies reported a significant positive association irrespective of intervention effects. The risk of moderate-to-severe exacerbations was observed to be positively associated with various definitions of higher eosinophil levels (absolute counts: ≥ 200, ≥ 300, ≥ 340, ≥ 400, and ≥ 500 cells/mm 3 ; % of blood eosinophil count: ≥ 2%, ≥ 3%, ≥ 4%, and ≥ 5%). Of note, one study found reduced efficacy of ICS in lowering moderate-to-severe exacerbation rates for current smokers versus former smokers at all eosinophil levels [ 13 ].
Of 12 studies assessing QoL scales, 11 (91.7%) studies reported a significant association between the worsening of QoL scores and the risk of future exacerbations (Table 3 ). Baseline SGRQ [ 14 , 15 ], Center for Epidemiologic Studies Depression Scale (for which increased scores may indicate impaired QoL) [ 16 ], and Clinical COPD Questionnaire [ 17 , 18 ] scores were found to be associated with future risk of moderate and/or severe COPD exacerbations. For symptom scores, six out of eight studies assessing the association between moderate-to-severe or severe exacerbations with COPD Assessment Test (CAT) scores reported a significant and positive relationship. Furthermore, the risk of moderate-to-severe exacerbations was found to be significantly higher in patients with higher CAT scores (≥ 10) [ 15 , 19 , 20 , 21 ], with one study demonstrating that a CAT score of 15 increased predictive ability for exacerbations compared with a score of 10 or more [ 18 ]. Among 15 studies that assessed the association of modified Medical Research Council (mMRC) scores with the risk of moderate-to-severe or severe exacerbation, 11 found that the risk of moderate-to-severe or severe exacerbations was significantly associated with higher mMRC scores (≥ 2) versus lower scores. Furthermore, morning and night symptoms (measured by Clinical COPD Questionnaire) were associated with poor health status and predicted future exacerbations [ 17 ].
Of 36 studies reporting the relationship between smoking status and moderate-to-severe or severe exacerbations, 22 studies (61.1%) reported a significant positive association (Table 3 ). Passive smoking was also significantly associated with an increased risk of severe exacerbations (OR 1.49) [ 20 ]. Of note, three studies reported a significantly lower rate of moderate-to-severe exacerbations in current smokers compared with former smokers [ 22 , 23 , 24 ].
A total of 14 studies assessed the association of body mass index (BMI) with the occurrence of frequent moderate-to-severe exacerbations in patients with COPD. Six out of 14 studies (42.9%) reported a significant negative association between exacerbations and BMI (Table 3 ). The risk of moderate and/or severe COPD exacerbations was highest among underweight patients compared with normal and overweight patients [ 23 , 25 , 26 , 27 , 28 ].
In the 29 studies reporting an association between age and moderate or severe exacerbations, more than half found an association of older age with an increased risk of moderate-to-severe exacerbations (58.6%; Table 3 ). Four of these studies noted a significant increase in the risk of moderate-to-severe or severe exacerbations for every 10-year increase in age [ 25 , 26 , 29 , 30 ]. However, 12 studies reported no significant association between age and moderate-to-severe or severe exacerbation risk.
Sixteen out of 33 studies investigating the impact of sex on exacerbation risk found a significant association (48.5%; Table 3 ). Among these, ten studies reported that female sex was associated with an increased risk of moderate-to-severe exacerbations, while six studies showed a higher exacerbation risk in males compared with females. There was some variation in findings by geographic location and exacerbation severity (Additional file 2 : Figs. S1 and S2). Notably, when assessing the risk of severe exacerbations, more studies found an association with male sex compared with female sex (6/13 studies vs 1/13 studies, respectively).
Both studies evaluating associations between exacerbations and environmental factors reported that colder temperature and exposure to major air pollution (NO 2 , O 3 , CO, and/or particulate matter ≤ 10 μm in diameter) increased hospital admissions due to severe exacerbations and moderate-to-severe exacerbation rates [ 31 , 32 ].
Four studies assessed the association of 6-min walk distance with the occurrence of frequent moderate-to-severe exacerbations (Table 3 ). One study (25.0%) found that shorter 6-min walk distance (representing low physical activity) was significantly associated with a shortened time to severe exacerbation, but the effect size was small (hazard ratio 0.99) [ 33 ].
Five out of six studies assessing the relationship between race or ethnicity and exacerbation risk reported significant associations (Table 3 ). Additionally, one study reported an association between geographic location in the US and exacerbations, with living in the Northeast region being the strongest predictor of severe COPD exacerbations versus living in the Midwest and South regions [ 34 ].
Overall, seven studies assessed the association of biomarkers with risk of future exacerbations (Table 3 ), with the majority identifying significant associations between inflammatory biomarkers and increased exacerbation risk, including higher C-reactive protein levels [ 8 , 35 ], fibrinogen levels [ 8 , 30 ], and white blood cell count [ 8 , 15 , 16 ].
This SLR has identified several demographic and clinical characteristics that predict the future risk of COPD exacerbations. Key factors associated with an increased risk of future moderate-to-severe exacerbations included a history of prior exacerbations, worse disease severity and bronchodilator reversibility, the presence of comorbidities, a higher eosinophil count, and older age (Fig. 2 ). These prognostic factors may help clinicians identify patients at high risk of exacerbations, which are a major driver of the burden of COPD, including morbidity and mortality [ 36 ].
Findings from this review summarize the existing evidence, validating the previously published literature [ 6 , 9 , 23 ] and suggesting that the best predictor of future exacerbations is a history of exacerbations in the prior year [ 8 , 11 , 12 , 13 , 14 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 26 , 29 , 34 , 35 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 ]. In addition, the effect size generally increased with the number of prior exacerbations, with a stronger effect observed with prior severe versus moderate exacerbations. This effect was observed across regions, including in Europe and North America, and in several global studies. This relationship represents a vicious circle, whereby one exacerbation predisposes a patient to experience future exacerbations and leading to an ever-increasing disease burden, and emphasizes the importance of preventing the first exacerbation event through early, proactive exacerbation prevention. The finding that prior exacerbations tended to be associated with future exacerbations of the same severity suggests that the severity of the underlying disease may influence exacerbation severity. However, the validity of the traditional classification of exacerbation severity has recently been challenged [ 61 ], and further work is required to understand relationships with objective assessments of exacerbation severity.
In addition to exacerbation history, disease severity and bronchodilator reversibility were also strong predictors for future exacerbations [ 8 , 14 , 16 , 18 , 19 , 20 , 22 , 23 , 24 , 26 , 28 , 29 , 33 , 37 , 40 , 43 , 44 , 45 , 46 , 48 , 50 , 51 , 52 , 56 , 59 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 ]. The association with disease severity was noted in studies that used GOLD disease stages 1–4 and those that used FEV 1 percent predicted and other lung function assessments as continuous variables. Again, this risk factor is self-perpetuating, as evidence shows that even a single moderate or severe exacerbation may almost double the rate of lung function decline [ 79 ]. Accordingly, disease severity and exacerbation history may be correlated. Margüello et al. concluded that the severity of COPD could be associated with a higher risk of exacerbations, but this effect was partly determined by the exacerbations suffered in the previous year [ 23 ]. It should be noted that FEV 1 is not recommended by GOLD for use as a predictor of exacerbation risk or mortality alone due to insufficient precision when used at the individual patient level [ 5 ].
Another factor that should be considered when assessing individual exacerbation risk is the presence of comorbidities [ 7 , 14 , 16 , 18 , 19 , 20 , 21 , 22 , 24 , 25 , 26 , 27 , 28 , 30 , 33 , 34 , 35 , 40 , 41 , 44 , 45 , 46 , 47 , 48 , 51 , 52 , 53 , 54 , 56 , 58 , 59 , 63 , 64 , 73 , 74 , 76 , 77 , 80 , 81 , 82 , 83 , 84 , 85 ]. Comorbidities are common in COPD, in part due to common risk factors (e.g., age, smoking, lifestyle factors) that also increase the risk of other chronic diseases [ 7 ]. Significant associations were observed between exacerbation risk and comorbidities, such as anxiety and depression, cardiovascular disease, diabetes, and respiratory comorbidities. As with prior exacerbations, the strength of the association increased with the number of comorbidities. Some comorbidities that were found to be associated with COPD exacerbations share a common biological mechanism of systemic inflammation, such as cardiovascular disease, diabetes, and depression [ 86 ]. Furthermore, other respiratory comorbidities, including asthma and bronchiectasis, involve inflammation of the airways [ 87 ]. In these patients, optimal management of comorbidities may reduce the risk of future COPD exacerbations (and improve QoL), although further research is needed to confirm the efficacy of this approach to exacerbation prevention. As cardiovascular conditions, including hypertension and coronary heart disease, are the most common comorbidities in people with COPD [ 7 ], reducing cardiovascular risk may be a key goal in reducing the occurrence of exacerbations. For other comorbidities, the mechanism for the association with exacerbation risk may be related to non-biological factors. For example, in depression, it has been suggested that the mechanism may relate to greater sensitivity to symptom changes or more frequent physician visits [ 88 ].
There is now a growing body of evidence reporting the relationship between blood eosinophil count and exacerbation risk [ 8 , 13 , 14 , 20 , 37 , 48 , 52 , 56 , 59 , 60 , 62 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 ]. Data from many large clinical trials (SUNSET [ 89 ], FLAME [ 96 ], WISDOM [ 98 ], IMPACT [ 13 ], TRISTAN [ 99 ], INSPIRE [ 99 ], KRONOS [ 91 ], TRIBUTE [ 48 ], TRILOGY [ 52 ], TRINITY [ 56 ]) have also shown relationships between treatment, eosinophil count, and exacerbation rates. Evidence shows that eosinophil count, along with other effect modifiers (e.g., exacerbation history), can be used to predict reductions in exacerbations with ICS treatment. Identifying patients most likely to respond to ICS should contribute to personalized medicine approaches to treat COPD. One challenge in drawing a strong conclusion from eosinophil counts is the choice of a cut-off value, with a variety of absolute and percentage values observed to be positively associated with the risk of moderate-to-severe exacerbations. The use of absolute counts may be more practical, as these are not affected by variations in other immune cell numbers; however, there is a lack of consensus on this point [ 100 ].
Across the studies examined, associations between sex and the risk of moderate and/or severe exacerbations were variable [ 14 , 16 , 18 , 20 , 21 , 22 , 23 , 24 , 26 , 27 , 28 , 29 , 37 , 40 , 42 , 44 , 45 , 46 , 47 , 48 , 51 , 52 , 56 , 58 , 59 , 63 , 73 , 74 , 77 , 80 , 83 , 84 , 85 ]. A greater number of studies showed an increased risk of exacerbations in females compared with males. In contrast, some studies failed to detect a relationship, suggesting that country-specific or cultural factors may play a role. A majority of the included studies evaluated more male patients than female patients; to further elucidate the relationship between sex and exacerbations, more studies in female patients are warranted. Over half of the studies that assessed the relationship between age and exacerbation risk found an association between increasing age and increasing risk of moderate-to-severe COPD exacerbations [ 14 , 16 , 18 , 20 , 21 , 22 , 23 , 24 , 26 , 27 , 28 , 29 , 33 , 40 , 42 , 44 , 45 , 47 , 51 , 52 , 54 , 56 , 63 , 73 , 74 , 77 , 80 , 83 , 85 ].
Our findings also suggested that patients with low BMI have greater risk of moderate and/or severe exacerbations. The mechanism underlying this increased risk in underweight patients is poorly understood; however, loss of lean body mass in patients with COPD may be related to ongoing systemic inflammation that impacts skeletal muscle mass [ 101 , 102 , 103 ].
A limitation of this SLR, that may have resulted in some studies with valid results being missed, was the exclusion of non-English-language studies and the limitation by date; however, the search strategy was otherwise broad, resulting in the review of a large number of studies. The majority of studies captured in this SLR were from Europe, North America, and Asia. The findings may therefore be less generalizable to patients in other regions, such as Africa or South America. Given that one study reported an association between geographic location within different regions of the US and exacerbations [ 34 ], it is plausible that risk of exacerbations may be impacted by global location. As no formal meta-analysis was planned, the assessments are based on a qualitative synthesis of studies. A majority of the included studies looked at exposures of certain factors (e.g., history of exacerbations) at baseline; however, some of these factors change over time, calling into question whether a more sophisticated statistical analysis should have been conducted in some cases to consider time-varying covariates. Our results can only inform on associations, not causation, and there are likely bidirectional relationships between many factors and exacerbation risk (e.g., health status). Finally, while our review of the literature captured a large number of prognostic factors, other variables such as genetic factors, lung microbiome composition, and changes in therapy over time have not been widely studied to date, but might also influence exacerbation frequency [ 104 ]. Further research is needed to assess the contribution of these factors to exacerbation risk.
This SLR captured publications up to July 2019. However, further studies have since been published that further support the prognostic factors identified here. For example, recent studies have reported an increased risk of exacerbations in patients with a history of exacerbations [ 105 ], comorbidities [ 106 ], poorer lung function (GOLD stage) [ 105 ], higher symptomatic burden [ 107 ], female sex [ 105 ], and lower BMI [ 106 , 108 ].
In summary, the literature assessing risk factors for moderate-to-severe COPD exacerbations shows that there are associations between several demographic and disease characteristics with COPD exacerbations, potentially allowing clinicians to identify patients most at risk of future exacerbations. Exacerbation history, comorbidities, and disease severity or bronchodilator reversibility were the factors most strongly associated with exacerbation risk, and should be considered in future research efforts to develop prognostic tools to estimate the likelihood of exacerbation occurrence. Importantly, many prognostic factors for exacerbations, such as symptom burden, QoL, and comorbidities, are modifiable with optimal pharmacologic and non-pharmacologic treatments or lifestyle modifications. Overall, the evidence suggests that, taken together, predicting and reducing exacerbation risk is an achievable goal in COPD.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Body mass index
COPD Assessment Test
Chronic obstructive pulmonary disease
Forced expiratory volume in 1 s
Global Initiative for Chronic Obstructive Lung Disease
Inhaled corticosteroid
Modified Medical Research Council
Quality of life
St. George’s Respiratory Questionnaire
World Health Organization. The top 10 causes of death. 2018. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death . Accessed 22 Jul 2020.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020;396:1204–22.
Article Google Scholar
Hurst JR, Skolnik N, Hansen GJ, Anzueto A, Donaldson GC, Dransfield MT, Varghese P. Understanding the impact of chronic obstructive pulmonary disease exacerbations on patient health and quality of life. Eur J Intern Med. 2020;73:1–6.
Article PubMed Google Scholar
Zhang Y, Morgan RL, Alonso-Coello P, Wiercioch W, Bała MM, Jaeschke RR, Styczeń K, Pardo-Hernandez H, Selva A, Ara Begum H, et al. A systematic review of how patients value COPD outcomes. Eur Respir J. 2018;52:1800222.
Global Initiative for Chronic Obstructive Lung Disease. 2022 GOLD Report. Global strategy for the diagnosis, management and prevention of COPD. 2022. https://goldcopd.org/2022-gold-reports-2/ . Accessed 02 Feb 2022.
Müllerová H, Shukla A, Hawkins A, Quint J. Risk factors for acute exacerbations of COPD in a primary care population: a retrospective observational cohort study. BMJ Open. 2014;4: e006171.
Article PubMed PubMed Central Google Scholar
Westerik JAM, Metting EI, van Boven JFM, Tiersma W, Kocks JWH, Schermer TR. Associations between chronic comorbidity and exacerbation risk in primary care patients with COPD. Respir Res. 2017;18:31.
Vedel-Krogh S, Nielsen SF, Lange P, Vestbo J, Nordestgaard BG. Blood eosinophils and exacerbations in chronic obstructive pulmonary disease. The Copenhagen General Population Study. Am J Respir Crit Care Med. 2016;193:965–74.
Hurst JR, Vestbo J, Anzueto A, Locantore N, Müllerová H, Tal-Singer R, Miller B, Lomas DA, Agusti A, Macnee W, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363:1128–38.
Article CAS PubMed Google Scholar
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Çolak Y, Afzal S, Marott JL, Nordestgaard BG, Vestbo J, Ingebrigtsen TS, Lange P. Prognosis of COPD depends on severity of exacerbation history: a population-based analysis. Respir Med. 2019;155:141–7.
Rothnie KJ, Müllerová H, Smeeth L, Quint JK. Natural history of chronic obstructive pulmonary disease exacerbations in a general practice-based population with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198:464–71.
Pascoe S, Barnes N, Brusselle G, Compton C, Criner GJ, Dransfield MT, Halpin DMG, Han MK, Hartley B, Lange P, et al. Blood eosinophils and treatment response with triple and dual combination therapy in chronic obstructive pulmonary disease: analysis of the IMPACT trial. Lancet Respir Med. 2019;7:745–56.
Yun JH, Lamb A, Chase R, Singh D, Parker MM, Saferali A, Vestbo J, Tal-Singer R, Castaldi PJ, Silverman EK, et al. Blood eosinophil count thresholds and exacerbations in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2018;141:2037-2047.e10.
Yoon HY, Park SY, Lee CH, Byun MK, Na JO, Lee JS, Lee WY, Yoo KH, Jung KS, Lee JH. Prediction of first acute exacerbation using COPD subtypes identified by cluster analysis. Int J Chron Obstruct Pulmon Dis. 2019;14:1389–97.
Article CAS PubMed PubMed Central Google Scholar
Yohannes AM, Mulerova H, Lavoie K, Vestbo J, Rennard SI, Wouters E, Hanania NA. The association of depressive symptoms with rates of acute exacerbations in patients with COPD: results from a 3-year longitudinal follow-up of the ECLIPSE cohort. J Am Med Dir Assoc. 2017;18:955-959.e6.
Tsiligianni I, Metting E, van der Molen T, Chavannes N, Kocks J. Morning and night symptoms in primary care COPD patients: a cross-sectional and longitudinal study. An UNLOCK study from the IPCRG. NPJ Prim Care Respir Med. 2016;26:16040.
Jo YS, Yoon HI, Kim DK, Yoo CG, Lee CH. Comparison of COPD Assessment Test and Clinical COPD Questionnaire to predict the risk of exacerbation. Int J Chron Obstruct Pulmon Dis. 2018;13:101–7.
Marçôa R, Rodrigues DM, Dias M, Ladeira I, Vaz AP, Lima R, Guimarães M. Classification of Chronic Obstructive Pulmonary Disease (COPD) according to the new Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2017: comparison with GOLD 2011. COPD. 2018;15:21–6.
Han MK, Quibrera PM, Carretta EE, Barr RG, Bleecker ER, Bowler RP, Cooper CB, Comellas A, Couper DJ, Curtis JL, et al. Frequency of exacerbations in patients with chronic obstructive pulmonary disease: an analysis of the SPIROMICS cohort. Lancet Respir Med. 2017;5:619–26.
Yii ACA, Loh CH, Tiew PY, Xu H, Taha AAM, Koh J, Tan J, Lapperre TS, Anzueto A, Tee AKH. A clinical prediction model for hospitalized COPD exacerbations based on “treatable traits.” Int J Chron Obstruct Pulmon Dis. 2019;14:719–28.
McGarvey L, Lee AJ, Roberts J, Gruffydd-Jones K, McKnight E, Haughney J. Characterisation of the frequent exacerbator phenotype in COPD patients in a large UK primary care population. Respir Med. 2015;109:228–37.
Margüello MS, Garrastazu R, Ruiz-Nuñez M, Helguera JM, Arenal S, Bonnardeux C, León C, Miravitlles M, García-Rivero JL. Independent effect of prior exacerbation frequency and disease severity on the risk of future exacerbations of COPD: a retrospective cohort study. NPJ Prim Care Respir Med. 2016;26:16046.
Engel B, Schindler C, Leuppi JD, Rutishauser J. Predictors of re-exacerbation after an index exacerbation of chronic obstructive pulmonary disease in the REDUCE randomised clinical trial. Swiss Med Wkly. 2017;147: w14439.
PubMed Google Scholar
Benson VS, Müllerová H, Vestbo J, Wedzicha JA, Patel A, Hurst JR. Evaluation of COPD longitudinally to identify predictive surrogate endpoints (ECLIPSE) investigators. Associations between gastro-oesophageal reflux, its management and exacerbations of chronic obstructive pulmonary disease. Respir Med. 2015;109:1147–54.
Santibáñez M, Garrastazu R, Ruiz-Nuñez M, Helguera JM, Arenal S, Bonnardeux C, León C, García-Rivero JL. Predictors of hospitalized exacerbations and mortality in chronic obstructive pulmonary disease. PLoS ONE. 2016;11: e0158727.
Article PubMed PubMed Central CAS Google Scholar
Jo YS, Kim YH, Lee JY, Kim K, Jung KS, Yoo KH, Rhee CK. Impact of BMI on exacerbation and medical care expenses in subjects with mild to moderate airflow obstruction. Int J Chron Obstruct Pulmon Dis. 2018;13:2261–9.
Alexopoulos EC, Malli F, Mitsiki E, Bania EG, Varounis C, Gourgoulianis KI. Frequency and risk factors of COPD exacerbations and hospitalizations: a nationwide study in Greece (Greek Obstructive Lung Disease Epidemiology and health ecoNomics: GOLDEN study). Int J Chron Obstruct Pulmon Dis. 2015;10:2665–74.
PubMed PubMed Central Google Scholar
Liu D, Peng SH, Zhang J, Bai SH, Liu HX, Qu JM. Prediction of short term re-exacerbation in patients with acute exacerbation of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:1265–73.
Müllerová H, Maselli DJ, Locantore N, Vestbo J, Hurst JR, Wedzicha JA, Bakke P, Agusti A, Anzueto A. Hospitalized exacerbations of COPD: risk factors and outcomes in the ECLIPSE cohort. Chest. 2015;147:999–1007.
de Miguel-Díez J, Hernández-Vázquez J, López-de-Andrés A, Álvaro-Meca A, Hernández-Barrera V, Jiménez-García R. Analysis of environmental risk factors for chronic obstructive pulmonary disease exacerbation: a case-crossover study (2004–2013). PLoS ONE. 2019;14: e0217143.
Krachunov II, Kyuchukov NH, Ivanova ZI, Yanev NA, Hristova PA, Borisova ED, Popova TP, Pavlov PS, Nikolova PT, Ivanov YY. Impact of air pollution and outdoor temperature on the rate of chronic obstructive pulmonary disease exacerbations. Folia Med (Plovdiv). 2017;59:423–9.
Article CAS Google Scholar
Baumeler L, Papakonstantinou E, Milenkovic B, Lacoma A, Louis R, Aerts JG, Welte T, Kostikas K, Blasi F, Boersma W, et al. Therapy with proton-pump inhibitors for gastroesophageal reflux disease does not reduce the risk for severe exacerbations in COPD. Respirology. 2016;21:883–90.
Annavarapu S, Goldfarb S, Gelb M, Moretz C, Renda A, Kaila S. Development and validation of a predictive model to identify patients at risk of severe COPD exacerbations using administrative claims data. Int J Chron Obstruct Pulmon Dis. 2018;13:2121–30.
Crisafulli E, Torres A, Huerta A, Méndez R, Guerrero M, Martinez R, Liapikou A, Soler N, Sethi S, Menéndez R. C-reactive protein at discharge, diabetes mellitus and ≥1 hospitalization during previous year predict early readmission in patients with acute exacerbation of chronic obstructive pulmonary disease. COPD. 2015;12:311–20.
Bollmeier SG, Hartmann AP. Management of chronic obstructive pulmonary disease: a review focusing on exacerbations. Am J Health Syst Pharm. 2020;77:259–68.
Bafadhel M, Peterson S, De Blas MA, Calverley PM, Rennard SI, Richter K, Fagerås M. Predictors of exacerbation risk and response to budesonide in patients with chronic obstructive pulmonary disease: a post-hoc analysis of three randomised trials. Lancet Respir Med. 2018;6:117–26.
Calverley PM, Anzueto AR, Dusser D, Mueller A, Metzdorf N, Wise RA. Treatment of exacerbations as a predictor of subsequent outcomes in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:1297–308.
Calverley PM, Tetzlaff K, Dusser D, Wise RA, Mueller A, Metzdorf N, Anzueto A. Determinants of exacerbation risk in patients with COPD in the TIOSPIR study. Int J Chron Obstruct Pulmon Dis. 2017;12:3391–405.
Eklöf J, Sørensen R, Ingebrigtsen TS, Sivapalan P, Achir I, Boel JB, Bangsborg J, Ostergaard C, Dessau RB, Jensen US, et al. Pseudomonas aeruginosa and risk of death and exacerbations in patients with chronic obstructive pulmonary disease: an observational cohort study of 22 053 patients. Clin Microbiol Infect. 2020;26:227–34.
Estirado C, Ceccato A, Guerrero M, Huerta A, Cilloniz C, Vilaró O, Gabarrús A, Gea J, Crisafulli E, Soler N, Torres A. Microorganisms resistant to conventional antimicrobials in acute exacerbations of chronic obstructive pulmonary disease. Respir Res. 2018;19:119.
Fuhrman C, Moutengou E, Roche N, Delmas MC. Prognostic factors after hospitalization for COPD exacerbation. Rev Mal Respir. 2017;34:1–18.
Krachunov I, Kyuchukov N, Ivanova Z, Yanev NA, Hristova PA, Pavlov P, Glogovska P, Popova T, Ivanov YY. Stability of frequent exacerbator phenotype in patients with chronic obstructive pulmonary disease. Folia Med (Plovdiv). 2018;60:536–45.
Make BJ, Eriksson G, Calverley PM, Jenkins CR, Postma DS, Peterson S, Östlund O, Anzueto A. A score to predict short-term risk of COPD exacerbations (SCOPEX). Int J Chron Obstruct Pulmon Dis. 2015;10:201–9.
Montserrat-Capdevila J, Godoy P, Marsal JR, Barbé F. Predictive model of hospital admission for COPD exacerbation. Respir Care. 2015;60:1288–94.
Montserrat-Capdevila J, Godoy P, Marsal JR, Barbé F, Galván L. Risk factors for exacerbation in chronic obstructive pulmonary disease: a prospective study. Int J Tuberc Lung Dis. 2016;20:389–95.
Orea-Tejeda A, Navarrete-Peñaloza AG, Verdeja-Vendrell L, Jiménez-Cepeda A, González-Islas DG, Hernández-Zenteno R, Keirns-Davis C, Sánchez-Santillán R, Velazquez-Montero A, Puentes RG. Right heart failure as a risk factor for severe exacerbation in patients with chronic obstructive pulmonary disease: prospective cohort study. Clin Respir J. 2018;12:2635–41.
Papi A, Vestbo J, Fabbri L, Corradi M, Prunier H, Cohuet G, Guasconi A, Montagna I, Vezzoli S, Petruzzelli S, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391:1076–84.
Lipson DA, Barnhart F, Brealey N, Brooks J, Criner GJ, Day NC, Dransfield MT, Halpin DMG, Han MK, Jones CE, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med. 2018;378:1671–80.
Pasquale MK, Xu Y, Baker CL, Zou KH, Teeter JG, Renda AM, Davis CC, Lee TC, Bobula J. COPD exacerbations associated with the modified Medical Research Council scale and COPD assessment test among Humana Medicare members. Int J Chron Obstruct Pulmon Dis. 2016;11:111–21.
Schuler M, Wittmann M, Faller H, Schultz K. Including changes in dyspnea after inpatient rehabilitation improves prediction models of exacerbations in COPD. Respir Med. 2018;141:87–93.
Singh D, Papi A, Corradi M, Pavlišová I, Montagna I, Francisco C, Cohuet G, Vezzoli S, Scuri M, Vestbo J. Single inhaler triple therapy versus inhaled corticosteroid plus long-acting β 2 -agonist therapy for chronic obstructive pulmonary disease (TRILOGY): a double-blind, parallel group, randomised controlled trial. Lancet. 2016;388:963–73.
Søgaard M, Madsen M, Løkke A, Hilberg O, Sørensen HT, Thomsen RW. Incidence and outcomes of patients hospitalized with COPD exacerbation with and without pneumonia. Int J Chron Obstruct Pulmon Dis. 2016;11:455–65.
Stanford RH, Nag A, Mapel DW, Lee TA, Rosiello R, Schatz M, Vekeman F, Gauthier-Loiselle M, Merrigan JFP, Duh MS. Claims-based risk model for first severe COPD exacerbation. Am J Manag Care. 2018;24:e45–53.
Stanford RH, Lau MS, Li Y, Stemkowski S. External validation of a COPD risk measure in a commercial and medicare population: the COPD treatment ratio. J Manag Care Spec Pharm. 2019;25:58–69.
Vestbo J, Papi A, Corradi M, Blazhko V, Montagna I, Francisco C, Cohuet G, Vezzoli S, Scuri M, Singh D. Single inhaler extrafine triple therapy versus long-acting muscarinic antagonist therapy for chronic obstructive pulmonary disease (TRINITY): a double-blind, parallel group, randomised controlled trial. Lancet. 2017;389:1919–29.
Wei X, Ma Z, Yu N, Ren J, Jin C, Mi J, Shi M, Tian L, Gao Y, Guo Y. Risk factors predict frequent hospitalization in patients with acute exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:121–9.
Whalley D, Svedsater H, Doward L, Crawford R, Leather D, Lay-Flurrie J, Bosanquet N. Follow-up interviews from The Salford Lung Study (COPD) and analyses per treatment and exacerbations. NPJ Prim Care Respir Med. 2019;29:20.
Zeiger RS, Tran TN, Butler RK, Schatz M, Li Q, Khatry DB, Martin U, Kawatkar AA, Chen W. Relationship of blood eosinophil count to exacerbations in chronic obstructive pulmonary disease. J Allergy Clin Immunol Pract. 2018;6:944-954.e945.
Vogelmeier CF, Kostikas K, Fang J, Tian H, Jones B, Morgan CL, Fogel R, Gutzwiller FS, Cao H. Evaluation of exacerbations and blood eosinophils in UK and US COPD populations. Respir Res. 2019;20:178.
Celli BR, Fabbri LM, Aaron SD, Agusti A, Brook R, Criner GJ, Franssen FME, Humbert M, Hurst JR, O’Donnell D, et al. An updated definition and severity classification of COPD exacerbations: the Rome proposal. Am J Respir Crit Care Med. 2021;204:1251–8.
Adir Y, Hakrush O, Shteinberg M, Schneer S, Agusti A. Circulating eosinophil levels do not predict severe exacerbations in COPD: a retrospective study. ERJ Open Research. 2018;4:00022–2018.
Bartels W, Adamson S, Leung L, Sin DD, van Eeden SF. Emergency department management of acute exacerbations of chronic obstructive pulmonary disease: factors predicting readmission. Int J Chron Obstruct Pulmon Dis. 2018;13:1647–54.
Kim V, Zhao H, Regan E, Han MK, Make BJ, Crapo JD, Jones PW, Curtis JL, Silverman EK, Criner GJ, COPDGene Investigators. The St. George’s Respiratory Questionnaire definition of chronic bronchitis may be a better predictor of COPD exacerbations compared with the classic definition. Chest. 2019;156:685–95.
Abston E, Comellas A, Reed RM, Kim V, Wise RA, Brower R, Fortis S, Beichel R, Bhatt S, Zabner J, et al. Higher BMI is associated with higher expiratory airflow normalised for lung volume (FEF25-75/FVC) in COPD. BMJ Open Respir Res. 2017;4: e000231.
Emura I, Usuda H, Satou K. Appearance of large scavenger receptor A-positive cells in peripheral blood: a potential risk factor for severe exacerbation of chronic obstructive pulmonary disease. Pathol Int. 2019;69:187–92.
Erol S, Sen E, Gizem Kilic Y, Yousif A, Akkoca Yildiz O, Acican T, Saryal S. Does the 2017 revision improve the ability of GOLD to predict risk of future moderate and severe exacerbation? Clin Respir J. 2018;12:2354–60.
Han MZ, Hsiue TR, Tsai SH, Huang TH, Liao XM, Chen CZ. Validation of the GOLD 2017 and new 16 subgroups (1A–4D) classifications in predicting exacerbation and mortality in COPD patients. Int J Chron Obstruct Pulmon Dis. 2018;13:3425–33.
Huang TH, Hsiue TR, Lin SH, Liao XM, Su PL, Chen CZ. Comparison of different staging methods for COPD in predicting outcomes. Eur Resp J. 2018;51:1700577.
Jung YH, Lee DY, Kim DW, Park SS, Heo EY, Chung HS, Kim DK. Clinical significance of laryngopharyngeal reflux in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:1343–51.
CAS PubMed PubMed Central Google Scholar
Kim J, Kim WJ, Lee CH, Lee SH, Lee MG, Shin KC, Yoo KH, Lee JH, Lim SY, Na JO, et al. Which bronchodilator reversibility criteria can predict severe acute exacerbation in chronic obstructive pulmonary disease patients? Respir Res. 2017;18:107.
Kobayashi S, Hanagama M, Ishida M, Sato H, Ono M, Yamanda S, Yamada M, Aizawa H, Yanai M. Clinical characteristics and outcomes in Japanese patients with COPD according to the 2017 GOLD classification: the Ishinomaki COPD Network Registry. Int J Chron Obstruct Pulmon Dis. 2018;13:3947–55.
Lee SH, Lee JH, Yoon HI, Park HY, Kim TH, Yoo KH, Oh YM, Jung KS, Lee SD, Lee SW. Change in inhaled corticosteroid treatment and COPD exacerbations: an analysis of real-world data from the KOLD/KOCOSS cohorts. Respir Res. 2019;20:62.
Pavlovic R, Stefanovic S, Lazic Z, Jankovic S. Factors associated with the rate of COPD exacerbations that require hospitalization. Turk J Med Sci. 2017;47:134–41.
Song JH, Lee CH, Um SJ, Park YB, Yoo KH, Jung KS, Lee SD, Oh YM, Lee JH, Kim EK, Kim DK. Clinical impacts of the classification by 2017 GOLD guideline comparing previous ones on outcomes of COPD in real-world cohorts. Int J Chron Obstruct Pulmon Dis. 2018;13:3473–84.
Sundh J, Johansson G, Larsson K, Lindén A, Löfdahl CG, Sandström T, Janson C. The phenotype of concurrent chronic bronchitis and frequent exacerbations in patients with severe COPD attending Swedish secondary care units. Int J Chron Obstruct Pulmon Dis. 2015;10:2327–34.
Urwyler P, Hussein NA, Bridevaux PO, Chhajed PN, Geiser T, Grendelmeier P, Zellweger LJ, Kohler M, Maier S, Miedinger D, et al. Predictive factors for exacerbation and reexacerbation in chronic obstructive pulmonary disease: an extension of the Cox model to analyze data from the Swiss COPD cohort. Multidiscip Respir Med. 2019;14:7.
Wallace AE, Kaila S, Bayer V, Shaikh A, Shinde MU, Willey VJ, Napier MB, Singer JR. Health care resource utilization and exacerbation rates in patients with COPD stratified by disease severity in a commercially insured population. J Manag Care Spec Pharm. 2019;25:205–17.
Halpin DMG, Decramer M, Celli BR, Mueller A, Metzdorf N, Tashkin DP. Effect of a single exacerbation on decline in lung function in COPD. Respir Med. 2017;128:85–91.
Bade BC, DeRycke EC, Ramsey C, Skanderson M, Crothers K, Haskell S, Bean-Mayberry B, Brandt C, Bastian LA, Akgün KM. Sex differences in veterans admitted to the hospital for chronic obstructive pulmonary disease exacerbation. Ann Am Thorac Soc. 2019;16:707–14.
Iyer AS, Bhatt SP, Dransfield M, Kinney G, Holm K, Wamboldt FS, Hanania N, Martinez C, Regan E, Foreman MG, et al. Psychological distress prospectively predicts severe exacerbations in smokers with and without airflow limitation—a longitudinal follow-up study of the COPDGene cohort [abstract]. Am J Respir Crit Care Med. 2017. https://doi.org/10.1164/ajrccm-conference.2017.195.1_MeetingAbstracts.A4709 .
Diamond M, Zhao H, Armstrong HF, Morrison M, Bailey KL, Carretta EE, Criner GJ, Han MK, Bleeker E, Cooper CB, et al. Anxiety and depression, either alone or in combination, are associated with respiratory exacerbations in smokers with and without COPD [abstract]. Am J Respir Crit Care Med. 2017;195:1615–31.
Google Scholar
Lau CS, Siracuse BL, Chamberlain RS. Readmission After COPD Exacerbation Scale: determining 30-day readmission risk for COPD patients. Int J Chron Obstruct Pulmon Dis. 2017;12:1891–902.
Pikoula M, Quint JK, Nissen F, Hemingway H, Smeeth L, Denaxas S. Identifying clinically important COPD sub-types using data-driven approaches in primary care population based electronic health records. BMC Med Inform Decis Mak. 2019;19:86.
Wei YF, Tsai YH, Wang CC, Kuo PH. Impact of overweight and obesity on acute exacerbations of COPD—subgroup analysis of the Taiwan Obstructive Lung Disease cohort. Int J Chron Obstruct Pulmon Dis. 2017;12:2723–9.
Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Resp J. 2009;33:1165–85.
Polverino E, Dimakou K, Hurst J, Martinez-Garcia MA, Miravitlles M, Paggiaro P, Shteinberg M, Aliberti S, Chalmers JD. The overlap between bronchiectasis and chronic airway diseases: state of the art and future directions. Eur Respir J. 2018;52:1800328.
Xu W, Collet JP, Shapiro S, Lin Y, Yang T, Platt RW, Wang C, Bourbeau J. Independent effect of depression and anxiety on chronic obstructive pulmonary disease exacerbations and hospitalizations. Am J Respir Crit Care Med. 2008;178:913–20.
Chapman KR, Hurst JR, Frent SM, Larbig M, Fogel R, Guerin T, Banerji D, Patalano F, Goyal P, Pfister P, et al. Long-term triple therapy de-escalation to indacaterol/glycopyrronium in patients with chronic obstructive pulmonary disease (SUNSET): a randomized, double-blind, triple-dummy clinical trial. Am J Respir Crit Care Med. 2018;198:329–39.
Couillard S, Larivée P, Courteau J, Vanasse A. Eosinophils in COPD exacerbations are associated with increased readmissions. Chest. 2017;151:366–73.
Ferguson GT, Rabe KF, Martinez FJ, Fabbri LM, Wang C, Ichinose M, Bourne E, Ballal S, Darken P, DeAngelis K, et al. Triple therapy with budesonide/glycopyrrolate/formoterol fumarate with co-suspension delivery technology versus dual therapies in chronic obstructive pulmonary disease (KRONOS): a double-blind, parallel-group, multicentre, phase 3 randomised controlled trial. Lancet Respir Med. 2018;6:747–58.
Ko FWS, Chan KP, Ngai J, Ng SS, Yip WH, Ip A, Chan TO, Hui DSC. Blood eosinophil count as a predictor of hospital length of stay in COPD exacerbations. Respirology. 2019;25:259–66.
MacDonald MI, Osadnik CR, Bulfin L, Hamza K, Leong P, Wong A, King PT, Bardin PG. Low and high blood eosinophil counts as biomarkers in hospitalized acute exacerbations of COPD. Chest. 2019;156:92–100.
Müllerová H, Hahn B, Simard EP, Mu G, Hatipoğlu U. Exacerbations and health care resource use among patients with COPD in relation to blood eosinophil counts. Int J Chron Obstruct Pulmon Dis. 2019;14:683–92.
Bafadhel M, Greening NJ, Harvey-Dunstan TC, Williams JEA, Morgan MD, Brightling CE, Hussain SF, Pavord ID, Singh SJ, Steiner MC. Blood eosinophils and outcomes in severe hospitalised exacerbations of COPD. Chest. 2016;150:320–8.
Roche N, Chapman KR, Vogelmeier CF, Herth FJF, Thach C, Fogel R, Olsson P, Patalano F, Banerji D, Wedzicha JA. Blood eosinophils and response to maintenance chronic obstructive pulmonary disease treatment. Data from the FLAME trial. Am J Respir Crit Care Med. 2017;195:1189–97.
Vestbo J, Vogelmeier CF, Small M, Siddall J, Fogel R, Kostikas K. Inhaled corticosteroid use by exacerbations and eosinophils: a real-world COPD population. Int J Chron Obstruct Pulmon Dis. 2019;14:853–61.
Watz H, Tetzlaff K, Wouters EFM, Kirsten A, Magnussen H, Rodriguez-Roisin R, Vogelmeier C, Fabbri LM, Chanez P, Dahl R, et al. Blood eosinophil count and exacerbations in severe chronic obstructive pulmonary disease after withdrawal of inhaled corticosteroids: a post-hoc analysis of the WISDOM trial. Lancet Respir Med. 2016;4:390–8.
Pavord ID, Lettis S, Locantore N, Pascoe S, Jones PW, Wedzicha JA, Barnes NC. Blood eosinophils and inhaled corticosteroid/long-acting beta-2 agonist efficacy in COPD. Thorax. 2016;71:118–25.
Singh D. Predicting corticosteroid response in chronic obstructive pulmonary disease. Blood eosinophils gain momentum. Am J Respir Crit Care Med. 2017;196:1098–100.
Vestbo J, Prescott E, Almdal T, Dahl M, Nordestgaard BG, Andersen T, Sørensen TIA, Lange P. Body mass, fat-free body mass, and prognosis in patients with chronic obstructive pulmonary disease from a random population sample: findings from the Copenhagen City Heart Study. Am J Respir Crit Care Med. 2006;173:79–83.
Agustí AGN, Noguera A, Sauleda J, Sala E, Pons J, Busquets X. Systemic effects of chronic obstructive pulmonary disease. Eur Respir J. 2003;21:347–60.
Agustí AGN, Sauleda J, Miralles C, Gomez C, Togores B, Sala E, Batle S, Busquets X. Skeletal muscle apoptosis and weight loss in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;166:485–9.
Labaki WW, Martinez FJ. Time to understand the infrequency of the frequent exacerbator phenotype in COPD. Chest. 2018;153:1087–8.
Hartley BF, Barnes NC, Lettis S, Compton CH, Papi A, Jones P. Risk factors for exacerbations and pneumonia in patients with chronic obstructive pulmonary disease: a pooled analysis. Respir Res. 2020;21:5.
Kim Y, Kim YJ, Kang YM, Cho WK. Exploring the impact of number and type of comorbidities on the risk of severe COPD exacerbations in Korean Population: a Nationwide Cohort Study. BMC Pulm Med. 2021;21:151.
Mackay AJ, Kostikas K, Roche N, Frent SM, Olsson P, Pfister P, Gupta P, Patalano F, Banerji D, Wedzicha JA. Impact of baseline symptoms and health status on COPD exacerbations in the FLAME study. Respir Res. 2020;21:93.
Smulders L, van der Aalst A, Neuhaus EDET, Polman S, Franssen FME, van Vliet M, de Kruif MD. Decreased risk of COPD exacerbations in obese patients. COPD. 2020;17:485–91.
Battisti WP, Wager E, Baltzer L, Bridges D, Cairns A, Carswell CI, Citrome L, Gurr JA, Mooney LA, Moore BJ, et al. Good publication practice for communicating company-sponsored medical research: GPP3. Ann Intern Med. 2015;163:461–4.
Putcha N, Barr RG, Han M, Woodruff PG, Bleecker ER, Kanner RE, Martinez FJ, Tashkin DP, Rennard SI, Breysse P, et al. Understanding the impact of passive smoke exposure on outcomes in COPD [abstract]. Am J Respir Crit Care Med. 2015;191:411–20.
Wu Z, Yang D, Ge Z, Yan M, Wu N, Liu Y. Body mass index of patients with chronic obstructive pulmonary disease is associated with pulmonary function and exacerbations: a retrospective real world research. J Thorac Dis. 2018;10:5086–99.
Download references
Acknowledgements
Medical writing support, under the direction of the authors, was provided by Julia King, PhD, and Sarah Piggott, MChem, CMC Connect, McCann Health Medical Communications, funded by AstraZeneca in accordance with Good Publication Practice (GPP3) guidelines [ 109 ].
This study was supported by AstraZeneca.
Author information
Authors and affiliations.
UCL Respiratory, University College London, London, WC1E 6BT, UK
John R. Hurst
Division of Pulmonary and Critical Care, University of Michigan, Ann Arbor, MI, USA
MeiLan K. Han
Formerly of Parexel International, Mohali, India
Barinder Singh, Gagandeep Kaur & Mohd Kashif Siddiqui
Parexel International, Mohali, India
Sakshi Sharma
Formerly of AstraZeneca, Cambridge, UK
Enrico de Nigris
AstraZeneca, Gothenburg, Sweden
Ulf Holmgren
You can also search for this author in PubMed Google Scholar
Contributions
The authors have made the following declaration about their contributions. JRH and MKH made substantial contributions to the interpretation of data; BS, SS, GK, and MKS made substantial contributions to the acquisition, analysis, and interpretation of data; EdN and UH made substantial contributions to the conception and design of the work and the interpretation of data. All authors contributed to drafting or critically revising the article, have approved the submitted version, and agree to be personally accountable for their own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. All authors read and approved the final manuscript.
Corresponding author
Correspondence to John R. Hurst .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
JRH reports consulting fees from AstraZeneca; speaker fees from AstraZeneca, Chiesi, Pfizer, and Takeda; and travel support from GlaxoSmithKline and AstraZeneca. MKH reports assistance with conduction of this research and publication from AstraZeneca; personal fees from Aerogen, Altesa Biopharma, AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, DevPro, GlaxoSmithKline, Integrity, Medscape, Merck, Mylan, NACE, Novartis, Polarean, Pulmonx, Regeneron, Sanofi, Teva, Verona, United Therapeutics, and UpToDate; either in kind research support or funds paid to the institution from the American Lung Association, AstraZeneca, Biodesix, Boehringer Ingelheim, the COPD Foundation, Gala Therapeutics, the NIH, Novartis, Nuvaira, Sanofi, and Sunovion; participation in Data Safety Monitoring Boards for Novartis and Medtronic with funds paid to the institution; and stock options from Altesa Biopharma and Meissa Vaccines. BS, GK, and MKS are former employees of Parexel International. SS is an employee of Parexel International, which was funded by AstraZeneca to conduct this analysis. EdN is a former employee of AstraZeneca and previously held stock and/or stock options in the company. UH is an employee of AstraZeneca and holds stock and/or stock options in the company.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file1: table s1..
Search strategies. Table S2. List of included studies with linked publications. Table S3. Study characteristics across the 76 included studies. Table S4. Clinical characteristics of the patients assessed across the included studies.
Additional file 2: Fig. S1.
Sex (male vs female) as a risk factor for moderate-to-severe exacerbations. Fig. S2. Sex (male vs female) as a risk factor for severe exacerbations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hurst, J.R., Han, M.K., Singh, B. et al. Prognostic risk factors for moderate-to-severe exacerbations in patients with chronic obstructive pulmonary disease: a systematic literature review. Respir Res 23 , 213 (2022). https://doi.org/10.1186/s12931-022-02123-5
Download citation
Received : 02 March 2022
Accepted : 20 July 2022
Published : 23 August 2022
DOI : https://doi.org/10.1186/s12931-022-02123-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Exacerbations
- Comorbidities
- Hospitalization
Respiratory Research
ISSN: 1465-993X
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Med Res Methodol

Defining the process to literature searching in systematic reviews: a literature review of guidance and supporting studies
Chris cooper.
1 Institute of Health Research, University of Exeter Medical School, Exeter, UK
Andrew Booth
2 HEDS, School of Health and Related Research (ScHARR), University of Sheffield, Sheffield, UK
Jo Varley-Campbell
Nicky britten.
3 Institute of Health Research, University of Exeter Medical School, Exeter, UK
Ruth Garside
4 European Centre for Environment and Human Health, University of Exeter Medical School, Truro, UK
Associated Data
Systematic literature searching is recognised as a critical component of the systematic review process. It involves a systematic search for studies and aims for a transparent report of study identification, leaving readers clear about what was done to identify studies, and how the findings of the review are situated in the relevant evidence.
Information specialists and review teams appear to work from a shared and tacit model of the literature search process. How this tacit model has developed and evolved is unclear, and it has not been explicitly examined before.
The purpose of this review is to determine if a shared model of the literature searching process can be detected across systematic review guidance documents and, if so, how this process is reported in the guidance and supported by published studies.
A literature review.
Two types of literature were reviewed: guidance and published studies. Nine guidance documents were identified, including: The Cochrane and Campbell Handbooks. Published studies were identified through ‘pearl growing’, citation chasing, a search of PubMed using the systematic review methods filter, and the authors’ topic knowledge.
The relevant sections within each guidance document were then read and re-read, with the aim of determining key methodological stages. Methodological stages were identified and defined. This data was reviewed to identify agreements and areas of unique guidance between guidance documents. Consensus across multiple guidance documents was used to inform selection of ‘key stages’ in the process of literature searching.
Eight key stages were determined relating specifically to literature searching in systematic reviews. They were: who should literature search, aims and purpose of literature searching, preparation, the search strategy, searching databases, supplementary searching, managing references and reporting the search process.
Conclusions
Eight key stages to the process of literature searching in systematic reviews were identified. These key stages are consistently reported in the nine guidance documents, suggesting consensus on the key stages of literature searching, and therefore the process of literature searching as a whole, in systematic reviews. Further research to determine the suitability of using the same process of literature searching for all types of systematic review is indicated.
Electronic supplementary material
The online version of this article (10.1186/s12874-018-0545-3) contains supplementary material, which is available to authorized users.
Systematic literature searching is recognised as a critical component of the systematic review process. It involves a systematic search for studies and aims for a transparent report of study identification, leaving review stakeholders clear about what was done to identify studies, and how the findings of the review are situated in the relevant evidence.
Information specialists and review teams appear to work from a shared and tacit model of the literature search process. How this tacit model has developed and evolved is unclear, and it has not been explicitly examined before. This is in contrast to the information science literature, which has developed information processing models as an explicit basis for dialogue and empirical testing. Without an explicit model, research in the process of systematic literature searching will remain immature and potentially uneven, and the development of shared information models will be assumed but never articulated.
One way of developing such a conceptual model is by formally examining the implicit “programme theory” as embodied in key methodological texts. The aim of this review is therefore to determine if a shared model of the literature searching process in systematic reviews can be detected across guidance documents and, if so, how this process is reported and supported.
Identifying guidance
Key texts (henceforth referred to as “guidance”) were identified based upon their accessibility to, and prominence within, United Kingdom systematic reviewing practice. The United Kingdom occupies a prominent position in the science of health information retrieval, as quantified by such objective measures as the authorship of papers, the number of Cochrane groups based in the UK, membership and leadership of groups such as the Cochrane Information Retrieval Methods Group, the HTA-I Information Specialists’ Group and historic association with such centres as the UK Cochrane Centre, the NHS Centre for Reviews and Dissemination, the Centre for Evidence Based Medicine and the National Institute for Clinical Excellence (NICE). Coupled with the linguistic dominance of English within medical and health science and the science of systematic reviews more generally, this offers a justification for a purposive sample that favours UK, European and Australian guidance documents.
Nine guidance documents were identified. These documents provide guidance for different types of reviews, namely: reviews of interventions, reviews of health technologies, reviews of qualitative research studies, reviews of social science topics, and reviews to inform guidance.
Whilst these guidance documents occasionally offer additional guidance on other types of systematic reviews, we have focused on the core and stated aims of these documents as they relate to literature searching. Table 1 sets out: the guidance document, the version audited, their core stated focus, and a bibliographical pointer to the main guidance relating to literature searching.
Guidance documents audited for this literature review
Once a list of key guidance documents was determined, it was checked by six senior information professionals based in the UK for relevance to current literature searching in systematic reviews.
Identifying supporting studies
In addition to identifying guidance, the authors sought to populate an evidence base of supporting studies (henceforth referred to as “studies”) that contribute to existing search practice. Studies were first identified by the authors from their knowledge on this topic area and, subsequently, through systematic citation chasing key studies (‘pearls’ [ 1 ]) located within each key stage of the search process. These studies are identified in Additional file 1 : Appendix Table 1. Citation chasing was conducted by analysing the bibliography of references for each study (backwards citation chasing) and through Google Scholar (forward citation chasing). A search of PubMed using the systematic review methods filter was undertaken in August 2017 (see Additional file 1 ). The search terms used were: (literature search*[Title/Abstract]) AND sysrev_methods[sb] and 586 results were returned. These results were sifted for relevance to the key stages in Fig. 1 by CC.

The key stages of literature search guidance as identified from nine key texts
Extracting the data
To reveal the implicit process of literature searching within each guidance document, the relevant sections (chapters) on literature searching were read and re-read, with the aim of determining key methodological stages. We defined a key methodological stage as a distinct step in the overall process for which specific guidance is reported, and action is taken, that collectively would result in a completed literature search.
The chapter or section sub-heading for each methodological stage was extracted into a table using the exact language as reported in each guidance document. The lead author (CC) then read and re-read these data, and the paragraphs of the document to which the headings referred, summarising section details. This table was then reviewed, using comparison and contrast to identify agreements and areas of unique guidance. Consensus across multiple guidelines was used to inform selection of ‘key stages’ in the process of literature searching.
Having determined the key stages to literature searching, we then read and re-read the sections relating to literature searching again, extracting specific detail relating to the methodological process of literature searching within each key stage. Again, the guidance was then read and re-read, first on a document-by-document-basis and, secondly, across all the documents above, to identify both commonalities and areas of unique guidance.
Results and discussion
Our findings.
We were able to identify consensus across the guidance on literature searching for systematic reviews suggesting a shared implicit model within the information retrieval community. Whilst the structure of the guidance varies between documents, the same key stages are reported, even where the core focus of each document is different. We were able to identify specific areas of unique guidance, where a document reported guidance not summarised in other documents, together with areas of consensus across guidance.
Unique guidance
Only one document provided guidance on the topic of when to stop searching [ 2 ]. This guidance from 2005 anticipates a topic of increasing importance with the current interest in time-limited (i.e. “rapid”) reviews. Quality assurance (or peer review) of literature searches was only covered in two guidance documents [ 3 , 4 ]. This topic has emerged as increasingly important as indicated by the development of the PRESS instrument [ 5 ]. Text mining was discussed in four guidance documents [ 4 , 6 – 8 ] where the automation of some manual review work may offer efficiencies in literature searching [ 8 ].
Agreement between guidance: Defining the key stages of literature searching
Where there was agreement on the process, we determined that this constituted a key stage in the process of literature searching to inform systematic reviews.
From the guidance, we determined eight key stages that relate specifically to literature searching in systematic reviews. These are summarised at Fig. Fig.1. 1 . The data extraction table to inform Fig. Fig.1 1 is reported in Table 2 . Table Table2 2 reports the areas of common agreement and it demonstrates that the language used to describe key stages and processes varies significantly between guidance documents.
The order of literature search methods as presented in the guidance documents
For each key stage, we set out the specific guidance, followed by discussion on how this guidance is situated within the wider literature.
Key stage one: Deciding who should undertake the literature search
The guidance.
Eight documents provided guidance on who should undertake literature searching in systematic reviews [ 2 , 4 , 6 – 11 ]. The guidance affirms that people with relevant expertise of literature searching should ‘ideally’ be included within the review team [ 6 ]. Information specialists (or information scientists), librarians or trial search co-ordinators (TSCs) are indicated as appropriate researchers in six guidance documents [ 2 , 7 – 11 ].
How the guidance corresponds to the published studies
The guidance is consistent with studies that call for the involvement of information specialists and librarians in systematic reviews [ 12 – 26 ] and which demonstrate how their training as ‘expert searchers’ and ‘analysers and organisers of data’ can be put to good use [ 13 ] in a variety of roles [ 12 , 16 , 20 , 21 , 24 – 26 ]. These arguments make sense in the context of the aims and purposes of literature searching in systematic reviews, explored below. The need for ‘thorough’ and ‘replicable’ literature searches was fundamental to the guidance and recurs in key stage two. Studies have found poor reporting, and a lack of replicable literature searches, to be a weakness in systematic reviews [ 17 , 18 , 27 , 28 ] and they argue that involvement of information specialists/ librarians would be associated with better reporting and better quality literature searching. Indeed, Meert et al. [ 29 ] demonstrated that involving a librarian as a co-author to a systematic review correlated with a higher score in the literature searching component of a systematic review [ 29 ]. As ‘new styles’ of rapid and scoping reviews emerge, where decisions on how to search are more iterative and creative, a clear role is made here too [ 30 ].
Knowing where to search for studies was noted as important in the guidance, with no agreement as to the appropriate number of databases to be searched [ 2 , 6 ]. Database (and resource selection more broadly) is acknowledged as a relevant key skill of information specialists and librarians [ 12 , 15 , 16 , 31 ].
Whilst arguments for including information specialists and librarians in the process of systematic review might be considered self-evident, Koffel and Rethlefsen [ 31 ] have questioned if the necessary involvement is actually happening [ 31 ].
Key stage two: Determining the aim and purpose of a literature search
The aim: Five of the nine guidance documents use adjectives such as ‘thorough’, ‘comprehensive’, ‘transparent’ and ‘reproducible’ to define the aim of literature searching [ 6 – 10 ]. Analogous phrases were present in a further three guidance documents, namely: ‘to identify the best available evidence’ [ 4 ] or ‘the aim of the literature search is not to retrieve everything. It is to retrieve everything of relevance’ [ 2 ] or ‘A systematic literature search aims to identify all publications relevant to the particular research question’ [ 3 ]. The Joanna Briggs Institute reviewers’ manual was the only guidance document where a clear statement on the aim of literature searching could not be identified. The purpose of literature searching was defined in three guidance documents, namely to minimise bias in the resultant review [ 6 , 8 , 10 ]. Accordingly, eight of nine documents clearly asserted that thorough and comprehensive literature searches are required as a potential mechanism for minimising bias.
The need for thorough and comprehensive literature searches appears as uniform within the eight guidance documents that describe approaches to literature searching in systematic reviews of effectiveness. Reviews of effectiveness (of intervention or cost), accuracy and prognosis, require thorough and comprehensive literature searches to transparently produce a reliable estimate of intervention effect. The belief that all relevant studies have been ‘comprehensively’ identified, and that this process has been ‘transparently’ reported, increases confidence in the estimate of effect and the conclusions that can be drawn [ 32 ]. The supporting literature exploring the need for comprehensive literature searches focuses almost exclusively on reviews of intervention effectiveness and meta-analysis. Different ‘styles’ of review may have different standards however; the alternative, offered by purposive sampling, has been suggested in the specific context of qualitative evidence syntheses [ 33 ].
What is a comprehensive literature search?
Whilst the guidance calls for thorough and comprehensive literature searches, it lacks clarity on what constitutes a thorough and comprehensive literature search, beyond the implication that all of the literature search methods in Table Table2 2 should be used to identify studies. Egger et al. [ 34 ], in an empirical study evaluating the importance of comprehensive literature searches for trials in systematic reviews, defined a comprehensive search for trials as:
- a search not restricted to English language;
- where Cochrane CENTRAL or at least two other electronic databases had been searched (such as MEDLINE or EMBASE); and
- at least one of the following search methods has been used to identify unpublished trials: searches for (I) conference abstracts, (ii) theses, (iii) trials registers; and (iv) contacts with experts in the field [ 34 ].
Tricco et al. (2008) used a similar threshold of bibliographic database searching AND a supplementary search method in a review when examining the risk of bias in systematic reviews. Their criteria were: one database (limited using the Cochrane Highly Sensitive Search Strategy (HSSS)) and handsearching [ 35 ].
Together with the guidance, this would suggest that comprehensive literature searching requires the use of BOTH bibliographic database searching AND supplementary search methods.
Comprehensiveness in literature searching, in the sense of how much searching should be undertaken, remains unclear. Egger et al. recommend that ‘investigators should consider the type of literature search and degree of comprehension that is appropriate for the review in question, taking into account budget and time constraints’ [ 34 ]. This view tallies with the Cochrane Handbook, which stipulates clearly, that study identification should be undertaken ‘within resource limits’ [ 9 ]. This would suggest that the limitations to comprehension are recognised but it raises questions on how this is decided and reported [ 36 ].
What is the point of comprehensive literature searching?
The purpose of thorough and comprehensive literature searches is to avoid missing key studies and to minimize bias [ 6 , 8 , 10 , 34 , 37 – 39 ] since a systematic review based only on published (or easily accessible) studies may have an exaggerated effect size [ 35 ]. Felson (1992) sets out potential biases that could affect the estimate of effect in a meta-analysis [ 40 ] and Tricco et al. summarize the evidence concerning bias and confounding in systematic reviews [ 35 ]. Egger et al. point to non-publication of studies, publication bias, language bias and MEDLINE bias, as key biases [ 34 , 35 , 40 – 46 ]. Comprehensive searches are not the sole factor to mitigate these biases but their contribution is thought to be significant [ 2 , 32 , 34 ]. Fehrmann (2011) suggests that ‘the search process being described in detail’ and that, where standard comprehensive search techniques have been applied, increases confidence in the search results [ 32 ].
Does comprehensive literature searching work?
Egger et al., and other study authors, have demonstrated a change in the estimate of intervention effectiveness where relevant studies were excluded from meta-analysis [ 34 , 47 ]. This would suggest that missing studies in literature searching alters the reliability of effectiveness estimates. This is an argument for comprehensive literature searching. Conversely, Egger et al. found that ‘comprehensive’ searches still missed studies and that comprehensive searches could, in fact, introduce bias into a review rather than preventing it, through the identification of low quality studies then being included in the meta-analysis [ 34 ]. Studies query if identifying and including low quality or grey literature studies changes the estimate of effect [ 43 , 48 ] and question if time is better invested updating systematic reviews rather than searching for unpublished studies [ 49 ], or mapping studies for review as opposed to aiming for high sensitivity in literature searching [ 50 ].
Aim and purpose beyond reviews of effectiveness
The need for comprehensive literature searches is less certain in reviews of qualitative studies, and for reviews where a comprehensive identification of studies is difficult to achieve (for example, in Public health) [ 33 , 51 – 55 ]. Literature searching for qualitative studies, and in public health topics, typically generates a greater number of studies to sift than in reviews of effectiveness [ 39 ] and demonstrating the ‘value’ of studies identified or missed is harder [ 56 ], since the study data do not typically support meta-analysis. Nussbaumer-Streit et al. (2016) have registered a review protocol to assess whether abbreviated literature searches (as opposed to comprehensive literature searches) has an impact on conclusions across multiple bodies of evidence, not only on effect estimates [ 57 ] which may develop this understanding. It may be that decision makers and users of systematic reviews are willing to trade the certainty from a comprehensive literature search and systematic review in exchange for different approaches to evidence synthesis [ 58 ], and that comprehensive literature searches are not necessarily a marker of literature search quality, as previously thought [ 36 ]. Different approaches to literature searching [ 37 , 38 , 59 – 62 ] and developing the concept of when to stop searching are important areas for further study [ 36 , 59 ].
The study by Nussbaumer-Streit et al. has been published since the submission of this literature review [ 63 ]. Nussbaumer-Streit et al. (2018) conclude that abbreviated literature searches are viable options for rapid evidence syntheses, if decision-makers are willing to trade the certainty from a comprehensive literature search and systematic review, but that decision-making which demands detailed scrutiny should still be based on comprehensive literature searches [ 63 ].
Key stage three: Preparing for the literature search
Six documents provided guidance on preparing for a literature search [ 2 , 3 , 6 , 7 , 9 , 10 ]. The Cochrane Handbook clearly stated that Cochrane authors (i.e. researchers) should seek advice from a trial search co-ordinator (i.e. a person with specific skills in literature searching) ‘before’ starting a literature search [ 9 ].
Two key tasks were perceptible in preparing for a literature searching [ 2 , 6 , 7 , 10 , 11 ]. First, to determine if there are any existing or on-going reviews, or if a new review is justified [ 6 , 11 ]; and, secondly, to develop an initial literature search strategy to estimate the volume of relevant literature (and quality of a small sample of relevant studies [ 10 ]) and indicate the resources required for literature searching and the review of the studies that follows [ 7 , 10 ].
Three documents summarised guidance on where to search to determine if a new review was justified [ 2 , 6 , 11 ]. These focused on searching databases of systematic reviews (The Cochrane Database of Systematic Reviews (CDSR) and the Database of Abstracts of Reviews of Effects (DARE)), institutional registries (including PROSPERO), and MEDLINE [ 6 , 11 ]. It is worth noting, however, that as of 2015, DARE (and NHS EEDs) are no longer being updated and so the relevance of this (these) resource(s) will diminish over-time [ 64 ]. One guidance document, ‘Systematic reviews in the Social Sciences’, noted, however, that databases are not the only source of information and unpublished reports, conference proceeding and grey literature may also be required, depending on the nature of the review question [ 2 ].
Two documents reported clearly that this preparation (or ‘scoping’) exercise should be undertaken before the actual search strategy is developed [ 7 , 10 ]).
The guidance offers the best available source on preparing the literature search with the published studies not typically reporting how their scoping informed the development of their search strategies nor how their search approaches were developed. Text mining has been proposed as a technique to develop search strategies in the scoping stages of a review although this work is still exploratory [ 65 ]. ‘Clustering documents’ and word frequency analysis have also been tested to identify search terms and studies for review [ 66 , 67 ]. Preparing for literature searches and scoping constitutes an area for future research.
Key stage four: Designing the search strategy
The Population, Intervention, Comparator, Outcome (PICO) structure was the commonly reported structure promoted to design a literature search strategy. Five documents suggested that the eligibility criteria or review question will determine which concepts of PICO will be populated to develop the search strategy [ 1 , 4 , 7 – 9 ]. The NICE handbook promoted multiple structures, namely PICO, SPICE (Setting, Perspective, Intervention, Comparison, Evaluation) and multi-stranded approaches [ 4 ].
With the exclusion of The Joanna Briggs Institute reviewers’ manual, the guidance offered detail on selecting key search terms, synonyms, Boolean language, selecting database indexing terms and combining search terms. The CEE handbook suggested that ‘search terms may be compiled with the help of the commissioning organisation and stakeholders’ [ 10 ].
The use of limits, such as language or date limits, were discussed in all documents [ 2 – 4 , 6 – 11 ].
Search strategy structure
The guidance typically relates to reviews of intervention effectiveness so PICO – with its focus on intervention and comparator - is the dominant model used to structure literature search strategies [ 68 ]. PICOs – where the S denotes study design - is also commonly used in effectiveness reviews [ 6 , 68 ]. As the NICE handbook notes, alternative models to structure literature search strategies have been developed and tested. Booth provides an overview on formulating questions for evidence based practice [ 69 ] and has developed a number of alternatives to the PICO structure, namely: BeHEMoTh (Behaviour of interest; Health context; Exclusions; Models or Theories) for use when systematically identifying theory [ 55 ]; SPICE (Setting, Perspective, Intervention, Comparison, Evaluation) for identification of social science and evaluation studies [ 69 ] and, working with Cooke and colleagues, SPIDER (Sample, Phenomenon of Interest, Design, Evaluation, Research type) [ 70 ]. SPIDER has been compared to PICO and PICOs in a study by Methley et al. [ 68 ].
The NICE handbook also suggests the use of multi-stranded approaches to developing literature search strategies [ 4 ]. Glanville developed this idea in a study by Whitting et al. [ 71 ] and a worked example of this approach is included in the development of a search filter by Cooper et al. [ 72 ].
Writing search strategies: Conceptual and objective approaches
Hausner et al. [ 73 ] provide guidance on writing literature search strategies, delineating between conceptually and objectively derived approaches. The conceptual approach, advocated by and explained in the guidance documents, relies on the expertise of the literature searcher to identify key search terms and then develop key terms to include synonyms and controlled syntax. Hausner and colleagues set out the objective approach [ 73 ] and describe what may be done to validate it [ 74 ].
The use of limits
The guidance documents offer direction on the use of limits within a literature search. Limits can be used to focus literature searching to specific study designs or by other markers (such as by date) which limits the number of studies returned by a literature search. The use of limits should be described and the implications explored [ 34 ] since limiting literature searching can introduce bias (explored above). Craven et al. have suggested the use of a supporting narrative to explain decisions made in the process of developing literature searches and this advice would usefully capture decisions on the use of search limits [ 75 ].
Key stage five: Determining the process of literature searching and deciding where to search (bibliographic database searching)
Table Table2 2 summarises the process of literature searching as reported in each guidance document. Searching bibliographic databases was consistently reported as the ‘first step’ to literature searching in all nine guidance documents.
Three documents reported specific guidance on where to search, in each case specific to the type of review their guidance informed, and as a minimum requirement [ 4 , 9 , 11 ]. Seven of the key guidance documents suggest that the selection of bibliographic databases depends on the topic of review [ 2 – 4 , 6 – 8 , 10 ], with two documents noting the absence of an agreed standard on what constitutes an acceptable number of databases searched [ 2 , 6 ].
The guidance documents summarise ‘how to’ search bibliographic databases in detail and this guidance is further contextualised above in terms of developing the search strategy. The documents provide guidance of selecting bibliographic databases, in some cases stating acceptable minima (i.e. The Cochrane Handbook states Cochrane CENTRAL, MEDLINE and EMBASE), and in other cases simply listing bibliographic database available to search. Studies have explored the value in searching specific bibliographic databases, with Wright et al. (2015) noting the contribution of CINAHL in identifying qualitative studies [ 76 ], Beckles et al. (2013) questioning the contribution of CINAHL to identifying clinical studies for guideline development [ 77 ], and Cooper et al. (2015) exploring the role of UK-focused bibliographic databases to identify UK-relevant studies [ 78 ]. The host of the database (e.g. OVID or ProQuest) has been shown to alter the search returns offered. Younger and Boddy [ 79 ] report differing search returns from the same database (AMED) but where the ‘host’ was different [ 79 ].
The average number of bibliographic database searched in systematic reviews has risen in the period 1994–2014 (from 1 to 4) [ 80 ] but there remains (as attested to by the guidance) no consensus on what constitutes an acceptable number of databases searched [ 48 ]. This is perhaps because thinking about the number of databases searched is the wrong question, researchers should be focused on which databases were searched and why, and which databases were not searched and why. The discussion should re-orientate to the differential value of sources but researchers need to think about how to report this in studies to allow findings to be generalised. Bethel (2017) has proposed ‘search summaries’, completed by the literature searcher, to record where included studies were identified, whether from database (and which databases specifically) or supplementary search methods [ 81 ]. Search summaries document both yield and accuracy of searches, which could prospectively inform resource use and decisions to search or not to search specific databases in topic areas. The prospective use of such data presupposes, however, that past searches are a potential predictor of future search performance (i.e. that each topic is to be considered representative and not unique). In offering a body of practice, this data would be of greater practicable use than current studies which are considered as little more than individual case studies [ 82 – 90 ].
When to database search is another question posed in the literature. Beyer et al. [ 91 ] report that databases can be prioritised for literature searching which, whilst not addressing the question of which databases to search, may at least bring clarity as to which databases to search first [ 91 ]. Paradoxically, this links to studies that suggest PubMed should be searched in addition to MEDLINE (OVID interface) since this improves the currency of systematic reviews [ 92 , 93 ]. Cooper et al. (2017) have tested the idea of database searching not as a primary search method (as suggested in the guidance) but as a supplementary search method in order to manage the volume of studies identified for an environmental effectiveness systematic review. Their case study compared the effectiveness of database searching versus a protocol using supplementary search methods and found that the latter identified more relevant studies for review than searching bibliographic databases [ 94 ].
Key stage six: Determining the process of literature searching and deciding where to search (supplementary search methods)
Table Table2 2 also summaries the process of literature searching which follows bibliographic database searching. As Table Table2 2 sets out, guidance that supplementary literature search methods should be used in systematic reviews recurs across documents, but the order in which these methods are used, and the extent to which they are used, varies. We noted inconsistency in the labelling of supplementary search methods between guidance documents.
Rather than focus on the guidance on how to use the methods (which has been summarised in a recent review [ 95 ]), we focus on the aim or purpose of supplementary search methods.
The Cochrane Handbook reported that ‘efforts’ to identify unpublished studies should be made [ 9 ]. Four guidance documents [ 2 , 3 , 6 , 9 ] acknowledged that searching beyond bibliographic databases was necessary since ‘databases are not the only source of literature’ [ 2 ]. Only one document reported any guidance on determining when to use supplementary methods. The IQWiG handbook reported that the use of handsearching (in their example) could be determined on a ‘case-by-case basis’ which implies that the use of these methods is optional rather than mandatory. This is in contrast to the guidance (above) on bibliographic database searching.
The issue for supplementary search methods is similar in many ways to the issue of searching bibliographic databases: demonstrating value. The purpose and contribution of supplementary search methods in systematic reviews is increasingly acknowledged [ 37 , 61 , 62 , 96 – 101 ] but understanding the value of the search methods to identify studies and data is unclear. In a recently published review, Cooper et al. (2017) reviewed the literature on supplementary search methods looking to determine the advantages, disadvantages and resource implications of using supplementary search methods [ 95 ]. This review also summarises the key guidance and empirical studies and seeks to address the question on when to use these search methods and when not to [ 95 ]. The guidance is limited in this regard and, as Table Table2 2 demonstrates, offers conflicting advice on the order of searching, and the extent to which these search methods should be used in systematic reviews.
Key stage seven: Managing the references
Five of the documents provided guidance on managing references, for example downloading, de-duplicating and managing the output of literature searches [ 2 , 4 , 6 , 8 , 10 ]. This guidance typically itemised available bibliographic management tools rather than offering guidance on how to use them specifically [ 2 , 4 , 6 , 8 ]. The CEE handbook provided guidance on importing data where no direct export option is available (e.g. web-searching) [ 10 ].
The literature on using bibliographic management tools is not large relative to the number of ‘how to’ videos on platforms such as YouTube (see for example [ 102 ]). These YouTube videos confirm the overall lack of ‘how to’ guidance identified in this study and offer useful instruction on managing references. Bramer et al. set out methods for de-duplicating data and reviewing references in Endnote [ 103 , 104 ] and Gall tests the direct search function within Endnote to access databases such as PubMed, finding a number of limitations [ 105 ]. Coar et al. and Ahmed et al. consider the role of the free-source tool, Zotero [ 106 , 107 ]. Managing references is a key administrative function in the process of review particularly for documenting searches in PRISMA guidance.
Key stage eight: Documenting the search
The Cochrane Handbook was the only guidance document to recommend a specific reporting guideline: Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [ 9 ]. Six documents provided guidance on reporting the process of literature searching with specific criteria to report [ 3 , 4 , 6 , 8 – 10 ]. There was consensus on reporting: the databases searched (and the host searched by), the search strategies used, and any use of limits (e.g. date, language, search filters (The CRD handbook called for these limits to be justified [ 6 ])). Three guidance documents reported that the number of studies identified should be recorded [ 3 , 6 , 10 ]. The number of duplicates identified [ 10 ], the screening decisions [ 3 ], a comprehensive list of grey literature sources searched (and full detail for other supplementary search methods) [ 8 ], and an annotation of search terms tested but not used [ 4 ] were identified as unique items in four documents.
The Cochrane Handbook was the only guidance document to note that the full search strategies for each database should be included in the Additional file 1 of the review [ 9 ].
All guidance documents should ultimately deliver completed systematic reviews that fulfil the requirements of the PRISMA reporting guidelines [ 108 ]. The guidance broadly requires the reporting of data that corresponds with the requirements of the PRISMA statement although documents typically ask for diverse and additional items [ 108 ]. In 2008, Sampson et al. observed a lack of consensus on reporting search methods in systematic reviews [ 109 ] and this remains the case as of 2017, as evidenced in the guidance documents, and in spite of the publication of the PRISMA guidelines in 2009 [ 110 ]. It is unclear why the collective guidance does not more explicitly endorse adherence to the PRISMA guidance.
Reporting of literature searching is a key area in systematic reviews since it sets out clearly what was done and how the conclusions of the review can be believed [ 52 , 109 ]. Despite strong endorsement in the guidance documents, specifically supported in PRISMA guidance, and other related reporting standards too (such as ENTREQ for qualitative evidence synthesis, STROBE for reviews of observational studies), authors still highlight the prevalence of poor standards of literature search reporting [ 31 , 110 – 119 ]. To explore issues experienced by authors in reporting literature searches, and look at uptake of PRISMA, Radar et al. [ 120 ] surveyed over 260 review authors to determine common problems and their work summaries the practical aspects of reporting literature searching [ 120 ]. Atkinson et al. [ 121 ] have also analysed reporting standards for literature searching, summarising recommendations and gaps for reporting search strategies [ 121 ].
One area that is less well covered by the guidance, but nevertheless appears in this literature, is the quality appraisal or peer review of literature search strategies. The PRESS checklist is the most prominent and it aims to develop evidence-based guidelines to peer review of electronic search strategies [ 5 , 122 , 123 ]. A corresponding guideline for documentation of supplementary search methods does not yet exist although this idea is currently being explored.
How the reporting of the literature searching process corresponds to critical appraisal tools is an area for further research. In the survey undertaken by Radar et al. (2014), 86% of survey respondents (153/178) identified a need for further guidance on what aspects of the literature search process to report [ 120 ]. The PRISMA statement offers a brief summary of what to report but little practical guidance on how to report it [ 108 ]. Critical appraisal tools for systematic reviews, such as AMSTAR 2 (Shea et al. [ 124 ]) and ROBIS (Whiting et al. [ 125 ]), can usefully be read alongside PRISMA guidance, since they offer greater detail on how the reporting of the literature search will be appraised and, therefore, they offer a proxy on what to report [ 124 , 125 ]. Further research in the form of a study which undertakes a comparison between PRISMA and quality appraisal checklists for systematic reviews would seem to begin addressing the call, identified by Radar et al., for further guidance on what to report [ 120 ].
Limitations
Other handbooks exist.
A potential limitation of this literature review is the focus on guidance produced in Europe (the UK specifically) and Australia. We justify the decision for our selection of the nine guidance documents reviewed in this literature review in section “ Identifying guidance ”. In brief, these nine guidance documents were selected as the most relevant health care guidance that inform UK systematic reviewing practice, given that the UK occupies a prominent position in the science of health information retrieval. We acknowledge the existence of other guidance documents, such as those from North America (e.g. the Agency for Healthcare Research and Quality (AHRQ) [ 126 ], The Institute of Medicine [ 127 ] and the guidance and resources produced by the Canadian Agency for Drugs and Technologies in Health (CADTH) [ 128 ]). We comment further on this directly below.
The handbooks are potentially linked to one another
What is not clear is the extent to which the guidance documents inter-relate or provide guidance uniquely. The Cochrane Handbook, first published in 1994, is notably a key source of reference in guidance and systematic reviews beyond Cochrane reviews. It is not clear to what extent broadening the sample of guidance handbooks to include North American handbooks, and guidance handbooks from other relevant countries too, would alter the findings of this literature review or develop further support for the process model. Since we cannot be clear, we raise this as a potential limitation of this literature review. On our initial review of a sample of North American, and other, guidance documents (before selecting the guidance documents considered in this review), however, we do not consider that the inclusion of these further handbooks would alter significantly the findings of this literature review.
This is a literature review
A further limitation of this review was that the review of published studies is not a systematic review of the evidence for each key stage. It is possible that other relevant studies could help contribute to the exploration and development of the key stages identified in this review.
This literature review would appear to demonstrate the existence of a shared model of the literature searching process in systematic reviews. We call this model ‘the conventional approach’, since it appears to be common convention in nine different guidance documents.
The findings reported above reveal eight key stages in the process of literature searching for systematic reviews. These key stages are consistently reported in the nine guidance documents which suggests consensus on the key stages of literature searching, and therefore the process of literature searching as a whole, in systematic reviews.
In Table Table2, 2 , we demonstrate consensus regarding the application of literature search methods. All guidance documents distinguish between primary and supplementary search methods. Bibliographic database searching is consistently the first method of literature searching referenced in each guidance document. Whilst the guidance uniformly supports the use of supplementary search methods, there is little evidence for a consistent process with diverse guidance across documents. This may reflect differences in the core focus across each document, linked to differences in identifying effectiveness studies or qualitative studies, for instance.
Eight of the nine guidance documents reported on the aims of literature searching. The shared understanding was that literature searching should be thorough and comprehensive in its aim and that this process should be reported transparently so that that it could be reproduced. Whilst only three documents explicitly link this understanding to minimising bias, it is clear that comprehensive literature searching is implicitly linked to ‘not missing relevant studies’ which is approximately the same point.
Defining the key stages in this review helps categorise the scholarship available, and it prioritises areas for development or further study. The supporting studies on preparing for literature searching (key stage three, ‘preparation’) were, for example, comparatively few, and yet this key stage represents a decisive moment in literature searching for systematic reviews. It is where search strategy structure is determined, search terms are chosen or discarded, and the resources to be searched are selected. Information specialists, librarians and researchers, are well placed to develop these and other areas within the key stages we identify.
This review calls for further research to determine the suitability of using the conventional approach. The publication dates of the guidance documents which underpin the conventional approach may raise questions as to whether the process which they each report remains valid for current systematic literature searching. In addition, it may be useful to test whether it is desirable to use the same process model of literature searching for qualitative evidence synthesis as that for reviews of intervention effectiveness, which this literature review demonstrates is presently recommended best practice.
Additional file
Appendix tables and PubMed search strategy. Key studies used for pearl growing per key stage, working data extraction tables and the PubMed search strategy. (DOCX 30 kb)
Acknowledgements
CC acknowledges the supervision offered by Professor Chris Hyde.
This publication forms a part of CC’s PhD. CC’s PhD was funded through the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) Programme (Project Number 16/54/11). The open access fee for this publication was paid for by Exeter Medical School.
RG and NB were partially supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South West Peninsula.
The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Abbreviations
Authors’ contributions.
CC conceived the idea for this study and wrote the first draft of the manuscript. CC discussed this publication in PhD supervision with AB and separately with JVC. CC revised the publication with input and comments from AB, JVC, RG and NB. All authors revised the manuscript prior to submission. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Consent for publication, competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Chris Cooper, Email: [email protected] .
Andrew Booth, Email: [email protected] .
Jo Varley-Campbell, Email: [email protected] .
Nicky Britten, Email: [email protected] .
Ruth Garside, Email: [email protected] .
- Open access
- Published: 06 December 2022
What improves access to primary healthcare services in rural communities? A systematic review
- Zemichael Gizaw 1 ,
- Tigist Astale 2 &
- Getnet Mitike Kassie 2
BMC Primary Care volume 23 , Article number: 313 ( 2022 ) Cite this article
13k Accesses
9 Citations
1 Altmetric
Metrics details
To compile key strategies from the international experiences to improve access to primary healthcare (PHC) services in rural communities. Different innovative approaches have been practiced in different parts of the world to improve access to essential healthcare services in rural communities. Systematically collecting and combining best experiences all over the world is important to suggest effective strategies to improve access to healthcare in developing countries. Accordingly, this systematic review of literature was undertaken to identify key approaches from international experiences to enhance access to PHC services in rural communities.
All published and unpublished qualitative and/or mixed method studies conducted to improvement access to PHC services were searched from MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar. Articles published other than English language, citations with no abstracts and/or full texts, and duplicate studies were excluded. We included all articles available in different electronic databases regardless of their publication years. We assessed the methodological quality of the included studies using mixed methods appraisal tool (MMAT) version 2018 to minimize the risk of bias. Data were extracted using JBI mixed methods data extraction form. Data were qualitatively analyzed using emergent thematic analysis approach to identify key concepts and coded them into related non-mutually exclusive themes.
Our analysis of 110 full-text articles resulted in ten key strategies to improve access to PHC services. Community health programs or community-directed interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telemedicine, working with traditional healers, working with non-profit private sectors and non-governmental organizations including faith-based organizations are the key strategies identified from international experiences.
This review identified key strategies from international experiences to improve access to PHC services in rural communities. These strategies can play roles in achieving universal health coverage and reducing disparities in health outcomes among rural communities and enabling them to get healthcare when and where they want.
Peer Review reports
Introduction
Universal health coverage (UHC) is used to provide expanding services to eliminate access barriers. Universal health coverage is defined by the world health organization (WHO) as access to key promotional, preventive, curative and rehabilitative health services for all at an affordable rate and ensuring equity in access. The term universal has been described as the State's legal obligation to provide healthcare to all its citizens, with particular attention to ensuring that all poor and excluded groups are included [ 1 , 2 , 3 ].
Strengthening primary healthcare (PHC) is the most comprehensive, reliable and productive approach to improving people's physical and mental wellbeing and social well-being, and that PHC is a pillar of a sustainable health system for UHC and health-related sustainable development goals [ 4 , 5 ]. Despite tremendous progress over the last decades, there are still unaddressed health needs of people in all parts of the world [ 6 , 7 ]. Many people, particularly the poor and people living in rural areas and those who are in vulnerable circumstances, face challenges to remain healthy [ 8 ].
Geographical and financial inaccessibility, inadequate funding, inconsistent medication supply and equipment and personnel shortages have left the reach, availability and effect of PHC services in many countries disappointingly limited [ 9 , 10 ]. A recent Astana Declaration recognized those aspects of PHC need to be changed to adapt adequately to current and emerging threats to the healthcare system. This declaration discussed that implementation of a need-based, comprehensive, cost-effective, accessible, efficient and sustainable healthcare system is needed for disadvantaged and rural populations in more local and convenient settings to provide care when and where they want it [ 8 ].
Different innovative approaches have been practiced in different parts of the world to improve access to essential healthcare services in rural communities. Systematically collecting and combining best experiences all over the world is important to suggest effective strategies to improve access to healthcare in developing countries. Accordingly, this systematic review of literature was undertaken to identify key approaches from international experiences to enhance access to PHC services in rural communities. The findings of this systematic literature review can be used by healthcare professionals, researchers and policy makers to improve healthcare service delivery in rural communities.
Methodology
Research question.
What improves access to PHC services in rural communities? We used the PICO (population, issue/intervention, comparison/contrast, and outcome) construct to develop the search question [ 11 ]. The population is rural communities or remote communities in developing countries who have limited access to healthcare services. Moreover, we extended the population to developed countries to capture experiences of both developing and developed countries. The issue/intervention is implementation of different community-based health interventions to access to essential healthcare services. In this systematic review, we focused on PHC health services, mainly essential or basic healthcare services, community or public health services, and health promotion or health education. Primary healthcare is “a health care system that addressed social, economic, and political causes of poor health promotes health though health services at the primary care level enhances health of the community” [ 12 ]. Comparison/contrast is not appropriate for this review. The outcome is improved access to essential healthcare services.
Outcome measures
The outcome of this review is access to PHC services, such as preventive, promotive, curative, rehabilitative, and palliative health services which are affordable, convenient or acceptable, and available to all who need care.
Criteria for considering studies for this review
All published and unpublished qualitative and/or mixed method studies conducted to improve access to PHC services were included. Government and international or national organizations reports were also included. Different organizations whose primary mission is health or promotion of community health were selected. We included articles based on these eligibility criteria: context or scope of studies (access to PHC services), article type (primary studies), and publication language (English). Articles published other than English language, citations with no abstracts and/or full texts, reviews, and duplicate studies were excluded. We included all articles available in different electronic databases regardless of their publication years. We didn’t use time of publication for screening.
Information sources and search strategy
We searched relevant articles from MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar to access all forms of evidence. An initial search of MEDLINE was undertaken followed by analysis of the text words contained in the title and abstract, and of the index terms used to describe articles. We used the aforementioned performance indicators of PHC delivery and the PICO as we described above to choose keywords. A second search using all identified keywords and index terms was undertaken across all included databases. Thirdly, references of all identified articles were searched to get additional studies. The full electronic search strategy for MEDLINE, a major database we used for this review is included as a supplementary file (Additional file 1 : Appendix 1).
Study selection and assessment of methodological quality
Search results from different electronic databases were exported to Endnote reference manager version 7 to remove duplication. Two independent reviewers (ZG and BA) screened out records. An initial screening of titles and abstracts was done based on the PICO criteria and language of publication. Secondary screening of full-text papers was done for studies we included at the initial screening phase. We further investigated and assessed records included in the full-text articles against the inclusion and exclusion criteria. We sat together and discussed the eligibility assessment. The interrater agreement was 90%. We resolved disagreements by consensus for points we had different rating. We used the PRISMA flow diagram to summarize the study selection processes.
Methodological quality of the included studies was assessed using mixed methods appraisal tool (MMAT) version 2018 [ 13 ]. As it is clearly indicated in the user guide of the MMAT tool, it is discouraged to calculate an overall score from the ratings of each criterion. Instead, it is advised to provide a more detailed presentation of the ratings of each criterion to better inform quality of the included studies. The rating of each criterion was, therefore, done as per the detail explanations included in the guideline. Almost all the included full text articles fulfilled the criteria and all the included full text articles were found to be better quality.
Data extraction
We independently extracted data from papers included in the review using JBI mixed methods data extraction form. This form is only used for reviews that follow a convergent integrated approach, i.e. integration of qualitative data and qualitative data [ 14 ]. The data extraction form was piloted on randomly selected papers and modified accordingly. One reviewer extracted the data from the included studies and the second reviewer checked the extracted data. Disagreements were resolved by discussion between the two reviewers. Information was extracted from each included study on: list of authors, year of publication, study area, population of interest, study type, methods, focus of the studies, main findings, authors’ conclusion, and limitations of the study.
Synthesis of findings
The included full-text articles were qualitatively analyzed using emergent thematic analysis approach to identify key concepts and coded them into related non-mutually exclusive themes. Themes are strategies mentioned or discussed in the included records to improve access to PHC services. Themes were identified manually by reading the included records again and again. We then synthesized each theme by comparing the discussion and conclusion of the included articles.
Systematic review registration number
The protocol of this review is registered in PROSPERO (the registration number is: CRD42019132592) to avoid unplanned duplication and to enable comparison of reported review methods with what was planned in the protocol. It is available at https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019132592 .
Schematic of the systematic review and reporting of the search
We used PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) 2009 checklist [ 15 ] for reporting of this systematic review.
Study selection
The search strategy identified 1148 titles and abstracts [914 from PubMed (Table 1 ) and 234 from other sources] as of 10 March 2022. We obtained 900 after we removed duplicated articles. Following assessment by title and abstract, 485 records were excluded because these records did not meet the criteria as mentioned in the method section. Additional 256 records were discarded because the records did not discuss the outcome of interest well and some records were systematic reviews. The full text of the remaining 159 records was examined in more detail. It appeared that 49 studies did not meet the inclusion criteria as described in the method section. One hundred ten records met the inclusion criteria and were included in the systematic review or synthesis (Fig. 1 ).
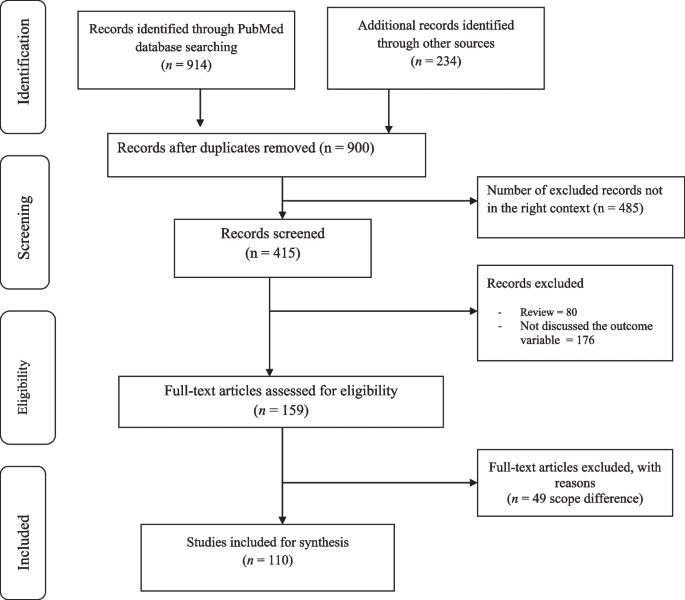
Study selection flow diagram
Of 900 articles resulting from the search term, 110 (12.2%) met the inclusion criteria. The included full-text articles were published between 1993 and 2021. Ninety-two (83.6%) of the included full-text articles were research articles, 5(4.5%) were technical reports, 3 (2.7%) were perspective, 4 (3.6%) was discussion paper, 3(2.7%) were dissertation or thesis, 2 (1.8%) were commentary, and 1 (0.9) was a book. Thirty-six (33%) and 29 (26%) of the included full-text articles were conducted in Africa and North America, respectively (Fig. 2 ).
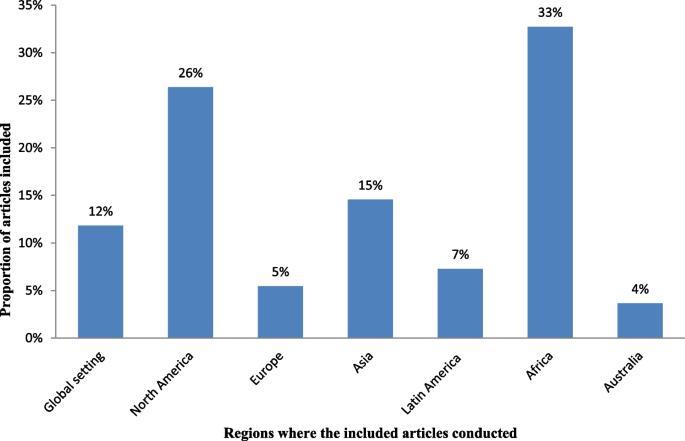
Regions where the included full-test articles conducted
Key strategies identified
The analysis of 110 full-text articles resulted in 10 themes. The themes are key strategies to improve access to PHC services in rural communities. The key strategies identified are community health programs or community-directed healthcare interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telemedicine, promoting the role of traditional medicine, working with non-profit private sectors and non-governmental organizations (NGOs) including faith-based organizations (Table 2 ).
Description of strategies
a. Community health programs or community-directed healthcare interventions
Twenty-four (21.8%) of the full-text articles included in this review discussed that community health programs (CHPs) or community-directed healthcare interventions are best strategies to provide basic health and medical care close to the community to increase access and coverage of essential health services. Community health programs are locally based health promotion, disease prevention, and treatment programs available typically to communities in need and community-directed intervention strategy is an approach in which communities themselves direct the planning and implementation of intervention delivery. Rural communities, especially, in developing countries have no access to healthcare facilities in the near distance and have less chance to receive healthcare from doctors, health officers, nurses or midwives. In response to this critical problems, many countries have been investing heavily in community based primary health care to bring services to rural and remote areas where most of the population lives. Community health programs include construction of health posts or community health centers close to the community and deployment of community health workers (CHWs), such as health extension workers, to reach-out every village, who play a prominent role as the gatekeepers of healthcare in rural communities. Community-directed healthcare intervention is an approach in which communities themselves direct the planning and implementation of healthcare interventions. Community participation remains crucial in the identification of health problems, planning or designing of health interventions and implementation of the interventions, which enhances need-based and demand-driven provision of health services while promoting sustainability and ownership (Additional file 2 : Appendix 2, Table A1).
b. School-based primary healthcare
In this review, 9 of 110 (8.2%) of the included full-text articles pointed out that school-based healthcare services can be effective to improve access to PHC services. School-based health services are health programs that offer health care to children and youth either in a school or on school grounds and usually staffed according to school community needs and resources. School-based health services provide a variety of healthcare services to underserved children, youth and vulnerable populations in a convenient and accessible environment. Access to comprehensive health services via schools leads to improved access to healthcare (Additional file 3 : Appendix 3, Table A2).
c. Student-led healthcare services
In this review, 5 of 110 (4.5%) of the full-text articles discussed that the use of medical and health science students as healthcare service providers can minimize problems related with shortage of health professionals in rural healthcare system and can play appreciable roles to minimize healthcare service access problems in rural communities. Student-led healthcare services are developed through consultation between universities and local health providers and are purposefully designed clinical placements with a focus on clinical educational activities for pre-registration students. Student-led clinics link students, healthcare professionals, community-based organizations, universities, and communities. In this approach, students can gain practical experience in an interdisciplinary setting and through exposure to a community with unique and severe needs (Additional file 4 : Appendix 4, Table A3).
d. Outreach services or mobile clinics
In this systematic literature review, 18 of 110 (16.4%) of the included studies discussed that outreach services or mobile clinics in primary care and rural hospital settings can improve access to PHC services in rural communities. Mobile outreach service is defined as healthcare services provided by a mobile team of trained providers, from a higher-level health facility to a lower-level health facilities or locally available community facilities that are not used for clinical services, such as schools, health posts, or other community structures. Outreach services improve access to specialists and hospital-based services, strengthen connections between specialists and PHC providers, and give the benefits of consultations in primary care settings. Specialist outreach services have the potential to overcome access barriers faced by disadvantaged rural and remote communities. Furthermore, a community-based mobile clinics can be effective in uncovering illness and in directing patients to a healthcare home (Additional file 5 : Appendix 5, Table A4).
e. Family health program
Four (3.6%) of the included full-text articles discussed that family health program (FHP) is highly cost-effective tool for improving access to healthcare services for deprived areas (such as rural communities). Family health program means the program is a program designed to provide primary care as well as the prevention and early treatment of communicable and non-communicable diseases in defined populations by deploying interdisciplinary healthcare teams include physicians, nurses, nurse assistants, and full-time community health agents. It has evolved into a robust approach to providing primary care for defined populations by deploying interdisciplinary healthcare teams. The nucleus of each team includes a physician, a nurse, a nurse assistant, and full-time community health agents. This approach is effective on improving access to healthcare and eliminating health disparities (Additional file 6 : Appendix 6, Table A5).
f. Empanelment
This systematic review of literature identified that empanelment (also known as rostering) is a best strategy to proactively provide coordinated primary healthcare towards achieving universal health coverage. Empanelment is a continuous, iterative set of processes that identify and assign populations to facilities, care teams, or primary care providers who have a responsibility to know their assigned population. It enables health systems to improve health outcomes and to reduce costs. Empanelment establishes a point of care for individuals and simultaneously holds primary healthcare providers and care teams accountable for actively managing care for a specific group of individuals (Additional file 7 : Appendix 7, Table A6).
g. Community health funding schemes
In this systematic review of literature, 11 (10%) of the included articles discussed that community health funding schemes such as community-based health insurance (CBHI) increases access to healthcare services in low-income rural communities. Community-based health insurance schemes are usually voluntary and characterized by community members pooling funds to offset the cost of healthcare. Moreover, this approach is effective to mobilize domestic resources for health at low income levels. For low-income countries, community health financing has modest ability to increase the total amount of funds for healthcare. Properly structured community health financing system can significantly improve efficiency, reduce the cost of healthcare, improve quality and health outcomes, and pool risks. Community-financing schemes could improve preventive services and reduce the incidence of diseases. It could also improve people’s access to healthcare and the quality of services, thus improving their health status. Community health financing could also improve risk pooling and reduce health-induced impoverishment. Community health insurance has potential positive impacts on health and social security (Additional file 8 : Appendix 8, Table A7).
h. Telemedicine
In this review, 13 of 110 (11.8%) articles discussed that telemedicine is one of the solutions for rural subspecialty healthcare delivery. Telemedicine can be defined as the use of technology (computers, video, phone, messaging) by a medical professional to diagnose and treat patients in a remote location. The provision of subspecialty services using telemedicine to a remote and medically underserved population provides improved access to subspecialty care. Telemedicine brings sustainable healthcare to rural populations. Use of information and communication technologies in support of health and health-related fields, including healthcare services, health surveillance, health education, and health research has the potential to greatly improve health service efficiency, expand or scale up treatment delivery to thousands of patients in the rural populations (Additional file 9 : Appendix 9, Table A8).
i. Promoting the role of traditional medicine
Seven (6.4%) of the included articles showed that incorporating traditional healers into public health system addresses healthcare needs of people with limited access to allopathic medicine. Traditional medicine is the sum total of the knowledge, skill, and practices based on the theories, beliefs, and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health as well as in the prevention, diagnosis, improvement or treatment of physical and mental illness. Knowledge about traditional medicine has a catalyzing effect in meeting health sector development objectives. Integrating traditional medicine into national health systems in combination with national policy and regulation for products, practices and providers can enhance access to PHC services in remote populations (Additional file 10 : Appendix 10, Table A9).
j. Working with non-profit private sectors and non-governmental organizations
In this systematic review, 15 of 110 (13.6%) of the included articles revealed that working with non-profit private sectors and NGOs strengthens the healthcare system. Involving the non-profit private sectors, faith-based organizations (FBOs), and NGOs for health system strengthening eventually contributes to create a healthcare system reflecting an increased efficiency, more equity and good governance in health. International and local NGOs have endeavored to fill the gaps in access to healthcare services, research and advocacy. Non-profit private sectors and NGOs have a key role in improving health in low- and middle-income countries. With networks that reach even the most remote communities, many FBOs are well positioned to promote demand and access for healthcare services. Partnership among FBOs is critical in increasing access to healthcare services, and ensuring sustainability by influencing behaviors at the community, family and individual level. Faith-based organizations play an integral role in the healthcare system by increasing health seeking behaviors and delivering supportive services that address common access and cultural barriers (Additional file 11 : Appendix 11, Table A10).
This systematic literature review found that community health programs or community-directed healthcare interventions, school-based healthcare services, student-led healthcare services, outreach services or mobile clinics, family health program, empanelment, community health funding schemes, telehealth, integrative medicine, and working with non-profit private sectors and NGOs are key strategies to improve access to PHC services in rural communities. The identified strategies address the four major pillars of primary healthcare (i.e., community participation, inter-sectoral coordination, appropriate technology, and support mechanism made available) [ 126 ]. Moreover, the identified strategies are effective to improve access to healthcare services to rural communities. Moreover, the identified strategies are effective to solve shortage of manpower and to build knowledge and skill of the local health workforces in rural healthcare system. The ability of a healthcare system to meet health needs of the population depends largely on the knowledge, skills, motivation and deployment of the people responsible for organizing and delivering health services. The results of this review can strengthen the health information system, which are core elements of the healthcare system that ensure community engagement through dissemination and use of timely and reliable health information to rural populations. This review also suggests strategies to narrow down the health disparities among rural populations, which is wide in most Least and Middle Income Countries (LMICs). Healthcare services are usually disproportionately concentrated in major urban areas. As a result, rural communities face growing health disparities, largely attributed to weak policies, inefficiencies, poor leadership, and governance in healthcare system.
This review identified that community health programs or community-directed healthcare interventions address health disparities by ensuring equitable access to health resources in communities where health equity is limited by socioeconomic and geographical factors. Community health programs include identifying and prioritizing public health problems in a specific geographic area; designing and implementing public health interventions (such as establishing community health centers, mobile clinics, and outreach programs); providing services (such as health education, screenings, social support, and counseling), and deploying community health workers to promote healthy behaviors; advocating for improved care for populations at risk; and working with stakeholders to address community healthcare needs [ 16 , 17 , 18 , 127 , 128 , 129 , 130 ]. The community-oriented PHC model which is socially responsive medicine makes a healthcare system more rational, accountable, appropriate, and socially relevant to the public. Consequently, this model serves as a paradigm for reforming healthcare systems. Community-directed interventions can be considered as a realistic means to increase accessibility of interventions at community-level in rural areas [ 32 , 33 , 34 , 35 , 36 , 37 , 38 ]. This approach is best in situations where there are cultural barriers to implement interventions because this strategy is effective to develop ownership in the community. In-service and on-the-job training for community health workers, close supervision and government support, and program evaluation is very important to strengthen the community health program [ 131 , 132 , 133 ].
This review identified that school-based PHC services are effective strategies to improve access to PHC services. School-based health services provide a variety of healthcare services to children, youth and vulnerable populations in a convenient and accessible environment which indirectly improve leadership and governance. Science teachers and home room teachers play important roles to implement this strategy. It impacts on delivering preventive care such as immunizations, managing chronic illnesses and providing reproductive health services for adolescents. Comprehensive health services via schools improve access to healthcare information [ 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ]. Access to school around the world increased drastically in the last century [ 134 ]. This high schooling rate is a good opportunity to provide healthcare services to school learners in accessible places and to disseminate health messages to families. Prior researches suggest that school-based healthcare services increase access to healthcare by increasing utilization of primary care, prevention services, and health maintenance visits [ 135 , 136 ]. Including science teachers, home room teachers, school principals, students, communities, community health workers, and other interested parties in the school-based healthcare system as main actors or promoters must be considered to sustain the impact. Health and education sectors should work in collaboration with the above-mentioned actors to plan, implement and monitor the progress. School-based healthcare services are preferable in situations when there is high schooling rate and limited access to healthcare institutions. This strategy is also an alternative way in areas where the health seeking behavior of the community is low.
The use of medical and health science students in rural healthcare system was identified as a key strategy to minimize health inequalities in rural communities due to shortages in health workforce and distribution of healthcare resources [ 49 , 50 , 51 , 52 , 53 ]. Student-led health intervention is an alternative approach to provide essential healthcare services to the community where there is shortage of healthcare workers [ 137 , 138 ]. Students will have opportunities to learn professional skills and competencies while they are providing healthcare services to the community. Moreover, benefits for student learning include increased communication, collaboration, and leadership skills [ 53 , 139 ]. Student-led health intervention also enables increased access to services, more time for assessments and treatments, increased depth of health teaching, holistic and integrated healthcare, and free health supports [ 140 , 141 , 142 , 143 ]. However, the use of medical and health science students in the rural healthcare system may have ethical and competency issues. Supporting strategies such as close supervision, preparing clear protocols, and including senior experts in the team should be considered.
This systematic review of literature found that outreach services or mobile clinics can improve access to PHC service delivery in rural populations [ 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 ]. In developing countries, the highest proportion of people lives in rural areas where doctor services are not available. Rural communities travel to major cities to get specialist services. This reflects a desire for closer integration between primary and secondary care. Specialist outreach services or mobile clinics have become one of the effective solution to solve health disparities, to improve access to healthcare services, and to build capacity of local healthcare workforces. This strategy is preferable in situations when there are high loads in tertiary or referral level hospitals and when there is high patient leakage in the referral system [ 63 , 64 , 65 , 66 , 67 , 68 , 69 ]. However, the implementation may not be easy. It needs well established healthcare system and budget. Moreover, the efficiency of care may be lower compared with hospital-based cares and the effect on patients’ health outcomes might be small [ 56 , 57 , 61 ] . Irregular specialist visits in rural areas may not have real impacts unless the services are sustainable with a strong commitment at national and local levels. Outreach activities should be included in health policies with strong leadership, healthcare financing, and private initiatives must be encouraged to maintain the activities over time.
This review revealed that FHP is highly effective tool for improving health for rural communities. The FHP has provided a new, more robust model of primary healthcare services designed to provide accessible, first contact, comprehensive, and whole person care that is coordinated with other healthcare services. It has positive results to improved availability, access to, and use of health services, and improved health indicators, such as reduced infant mortality, improved detection of cases of neglected diseases, and reduced health disparities [ 73 , 144 , 145 , 146 ]. The FHP deploys interdisciplinary healthcare teams. The team includes a physician, a nurse, a nurse assistant, and full-time community health agents. Family health teams are organized geographically. The teams are responsible for delivering public health interventions [ 72 , 74 ]. Family health program is an alternative strategy in rural healthcare system in situations when there are inequities in access to care; when there is high hospitalization rate; when there is low health seeking behavior in the community; and when there is poor case detecting and reporting system. Despite these remarkable achievements, the FHP has some challenges include difficulties in the recruitment and retention of doctors trained appropriately to deliver primary healthcare, large variations in quality of local care, patchy integration of primary care services with existing secondary and tertiary care, and slow adoption of FHP in large population [ 147 ].
In this review, empanelment has been identified as a best strategy to deliver coordinated primary healthcare towards achieving universal health coverage [ 76 , 77 , 78 , 79 ]. The goal of empanelment is provide people-centered healthcare services based on their needs to ensure that every established patient receives optimal care, whether he/she regularly visits healthcare centers. Major activities in this approach include assignment of all patients to a healthcare provider panel; update panel assignments on a regular basis; and use panel data to educate, and track patients [ 79 ]. Empanelment enables healthcare systems to improve patient experiences, reduce costs, and improve health outcomes. Empanelment is an effective strategy to deliver four key functions: first-contact accessibility, continuity, comprehensiveness, and coordination [ 148 ]. Effective empanelment requires responsibility for the health of a target population, including providing healthcare services based on their health status, which is an important step in moving towards people-centered integrated healthcare [ 79 ].
This review identified that community health funding schemes such as community-based health insurance (CBHI) increases access to healthcare in low-income rural communities. Moreover, this approach is effective to mobilize domestic resources for health at low income levels [ 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 ]. Community-based health insurance is an emerging strategy to provide financial protection against the cost of illness. It is an effective strategy to improve access to quality health services for low-income rural households [ 149 ]. Existence of social capital in the community is a determinant factor for the effectiveness of CBHI as social capital has a positive effect on the community's demand for insurance [ 150 , 151 ]. Moreover, solidarity and trust between the members are the key principles for the good functioning of a CBHI. Solidarity and trust stir-up members who are susceptible to risk to put together their resources for common use [ 149 , 152 , 153 ]. Affordability of premiums or contributions, technical arrangements made by the scheme management, timing of collecting the contributions, trust in the integrity and competence of the managers of the CBHI, The quality of care offered through the CBHI, accessible across different population groups are some of the determinant factors to be considered to increase people’s decision to join the CBHI schemes [ 154 , 155 ].
In this review, telemedicine has been identified as one of the many possible solutions for rural subspecialty healthcare delivery. Telemedicine is a vital technological tool to increase healthcare access, improve care delivery systems, engage in culturally competent outreach, health workforce development, and health information system [ 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 ]. Telemedicine can be a great alternative to the traditional healthcare system in situations like diagnoses of common medical problems; inquiries about various medical issues for home treatments; post-treatment check-ins or follow-up for chronic care; holidays, weekends, late night or any other situation when regular medical care is not possible; patient inability to leave the house; patients who lack regular access to relevant medical expertise in their geographic area ; and etc. However, technological issues are challenges when dealing with telemedicine, especially in developing countries. General problems of Internet connectivity and access to infrastructure can minimize benefits of this strategy. Costs associated with technology can also be a barrier. Furthermore, health technology requires human capacity to use it. Therefore, strengthening the information communication technologies (ICT) and human capacity building on ICT are important to address the health needs of the rural communities.
This systematic review of literature identified that promoting the role of TM solves problems of access to allopathic medicine. Integration of TM in health system will result in increased coverage and access to healthcare services. The role of complementary and alternative medicine for health is undisputed particularly in light of its role in health promotion and well-being. It also supports local health workforces [ 104 , 105 , 106 , 107 , 108 , 109 ]. Incorporating traditional healers into the public health system addresses healthcare needs [ 156 , 157 ]. However, integrating TM to the public healthcare system is challenging. It is a general belief that TM defies scientific procedures in terms of objectivity, measurement, codification and classification [ 157 ]. If integrated, who provides training to medical doctors on the ontology, epistemology and the efficacies of TM in modern medicine [ 157 ]. Due to these, some scholars suggest that both TM and modern medicine be allowed to operate and develop independent of one another [ 158 , 159 ]. Another fundamental challenge to TM is the widespread reported cases of fake healers and healings [ 157 ]. Generally, this strategy is more of feasible in areas where formal trainings on integrative medicine are available. Even though the integration is challenging, the health sector can use traditional healers as health educators or health promoters by providing training and continuous support. It can be also possible to use traditional healers as facilitators in the community-directed approaches. In general TM can be used in the primary healthcare system where no access to allopathic medicine and when conventional medicine is ineffective in treatment of disease [ 160 ].
Working with non-profit private sectors and NGOs has been identified as effective strategies to strengthen the healthcare system in developing countries [ 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 ]. Since governments in developing countries are challenged to meet the health needs of their populations because of financial constraints, limited human resources, and weak health infrastructure; the private sector (especially the non-profit private sectors) and non-governmental organizations can help expand access to healthcare services through its resources, expertise, and infrastructure. However, the presence of an NGO in the operation, may contribute to unrealistic expectations of health services, affecting perceptions of the latter negatively [ 113 ]. Moreover, reports have it that besides other issues in many instances NGOs allocated funds only to disease specific projects (vertical programming) rather than to broad based investments (horizontal programming) [ 161 ]. There are also concerns that donor expenditures in developing countries are not only unsustainable but may be considered as inadequate considering the enormous healthcare burden [ 161 , 162 , 163 , 164 ]. To avoid unrealistic expectations and dissatisfaction, and to increase and sustain the population’s trust in the organization, NGOs should operate in a manner that is as integrated as possible within the existing structure and should work close to the population it serves, with services anchored in the community. Moreover, faith-based organizations contribute in health such as disease prevention, health education or promotion, and community health development beyond psychological and spiritual care [ 119 , 120 , 121 , 122 , 123 , 124 ]. Religious organizations can reach all segments of rural populations. Therefore, integrating PHC services, especially health education and promotion, diseases prevention and community health development with religious organizations intensifies delivery of healthcare services. Working with FBOs is a best way in situations where cultural and faith-based barriers are common and in areas, where access problems are often related to lack of providers. However, religious organizations need intensive training on health promotion and health system to enable them to respond to local contexts within the framework of national policies. Moreover, there should be strong partnership with government agenesis to sustain the effort [ 165 , 166 , 167 , 168 ].
Contribution of this review
Various studies reported one or more strategies to improve access to primary healthcare services. However, the strategies reported by individual studies are not compiled together and there is lack of pooled evidence on effective strategies to improve access to healthcare system. This systematic literature review was, therefore, conducted to compile effective strategies to improve access to healthcare services in rural communities. The review suggests key strategies to improve access to PHC services in rural communities. These suggested strategies are implementable in countries that suffer from shortage of health workers and healthcare financing because all the strategies used locally available opportunities. The local healthcare system needs, therefore, scan the available opportunities in the locality for implementing the suggested strategies and needs to integrate the strategies in the healthcare system to sustain the impacts. Healthcare providers, researchers and policy makers could use the results of this systematic literature review to increase access to healthcare services in hard-to-reach areas. As the strategies are compiled from experiences of different countries (developed and least developed countries), there might be contextual differences like socio-economic, cultural, institutional, and geographical challenges to adopt the identified strategies. Moreover, some of the experiences only come from one or two countries. Therefore, strategy developers and implementers need to consider these contextual challenges or variation during adopting and implementing different strategies.
Strengths and limitations of the study
As a strength, this systematic review explores international (both developed and developing countries) best experiences on primary healthcare service delivery and identified ten key approaches to improve access to PHC services in rural communities. We also searched relevant published or unpublished articles, dissertations or theses, discussion papers, and perspectives from a wide range of sources, such as MEDLINE, Scopus, Web of Science, WHO Global Health Library, and Google Scholar.
As a limitation, we entirely relied on electronic databases to search relevant articles. We didn’t include locally available printed out records. We also applied limits for language. We excluded articles published other than English language. We believed we could get more relevant articles if we had access to records available in prints and if we include articles published other than English language. Furthermore, since the strategies are compiled from experiences of different countries (developed and least developed countries), there might be contextual differences like socio-economic, cultural, institutional and geographical challenges to adopt the identified strategies. There was also limited evidence for some articles, especially reports to rate their methodological quality. Readers should also note that our review might missed some important work in improving access to PHC services and the identified strategies are not the only strategies to improve access to PHC services. There might be other effective strategies which are not included in this review. In addition generalizability might be affected since some of the experiences only come from one or two countries. Moreover, this review focuses on access not quality of care delivered.
This review identified key strategies from international experiences to improve access to PHC services in rural communities. These strategies are effective to improve access to healthcare services in rural or remote communities. They can also play roles in achieving UHC and reducing disparities in health outcomes and increase access to rural communities to get healthcare when and where they want. Therefore, incorporating these key strategies suggested by this review in to the healthcare system is useful to enhance PHC services and to minimize impacts of health disparity in rural communities. However, the identified strategies may not be easy to implement. Increasing number and capacity of human resource for health; strengthening the healthcare financing system; improving medicine and supplies; working in different partners and communities; establishing monitoring and evaluation system; strong and committed leadership; and encouraging private initiatives must be considered to implement and maintain these strategies over time. Moreover, policy makers, program planners and implementers who want to utilize findings of this review should be aware that these are not the only effective strategies to improve access to primary healthcare services.
Availability of data and materials
All the extracted data are included in the manuscript.
Abbreviations
Community-based health insurance
Faith-based organizations
Family health program
Information communication technologies
Mixed methods appraisal tool
Non-governmental organizations
- Primary healthcare
Primary Health Care Performance Initiative
Population, phenomena of interest and context)
Traditional medicine
Universal health coverage
Hampton MB, Kettle AJ, Winterbourn CC. Inside the neutrophil phagosome: oxidants, myeloperoxidase, and bacterial killing. Blood. 1998;92(9):3007–17.
Article CAS Google Scholar
Kirby M. The right to health fifty years on: Still skeptical? Health Hum Rights. 1999;4(1):6–25.
O’Connell T, Rasanathan K, Chopra M. What does universal health coverage mean? The Lancet. 2014;383(9913):277–9.
White F. Primary health care and public health: foundations of universal health systems. Med Princ Pract. 2015;24(2):103–16.
Article Google Scholar
Sanders D, Nandi S, Labonté R, Vance C, Van Damme W. From primary health care to universal health coverage—one step forward and two steps back. The Lancet. 2019;394(10199):619–21.
Brezzi M, Luongo P. Regional Disparities In Access To Health Care. 2016.
Google Scholar
Hartley D. Rural health disparities, population health, and rural culture. Am J Public Health. 2004;94(10):1675–8.
Walraven G. The 2018 Astana declaration on primary health care, is it useful? J Glob Health. 2019;9(1).
Gillam S. Is the declaration of Alma Ata still relevant to primary health care? BMJ (Clinical research ed). 2008;336(7643):536–8.
Tollman S, Doherty J, Mulligan JA. General Primary Care. In: Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M, Evans DB, Jha P, Mills A, Musgrove P, editors. Disease Control Priorities in Developing Countries. Washington: World Bank The International Bank for Reconstruction and Development/The World Bank Group; 2006. Available at https://www.ncbi.nlm.nih.gov/books/NBK11789/pdf/Bookshelf_NBK11789.pdf .
Stern C, Jordan Z, McArthur A. Developing the review question and inclusion criteria. AJN The Am J Nurs. 2014;114(4):53–6.
World Health Organization. losing the gap in a generation. Commission on Social Determinants of Health FINAL REPORT. 2008. Available at https://www.who.int/social_determinants/final_report/csdh_finalreport_2008.pdf . Accessed on 22 March 2022.
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, GagnonM-P GF, Nicolau B, O’Cathain A. Mixed methods appraisal tool (MMAT), version 2018. Canada: IC Canadian Intellectual Property Office, Industry; 2018. Available at https://mixedmethodsappraisaltoolpublicpbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf .
JBI Manual for Evidence Synthesis. Appendix 8.1 JBI Mixed Methods Data Extraction Form following a Convergent Integrated Approach. Available at https://jbi-global-wiki.refined.site/space/MANUAL/3318284375/Appendix+8.1+JBI+Mixed+Methods+Data+Extraction+Form+following+a+Convergent+Integrated+Approach . Accessed on 12 August 2021.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Assefa Y, Gelaw YA, Hill PS, Taye BW, Van Damme W. Community health extension program of Ethiopia, 2003–2018: successes and challenges toward universal coverage for primary healthcare services. Glob Health. 2019;15(1):1–11.
Admassie A, Abebaw D, Woldemichael AD. Impact evaluation of the Ethiopian health services extension programme. J Dev Eff. 2009;1(4):430–49.
Yitayal M, Berhane Y, Worku A, Kebede Y. The community-based Health extension Program significantly improved contraceptive utilization in West gojjam Zone, ethiopia. J Multidiscip Healthc. 2014;7:201.
Croke K, Mengistu AT, O’Connell SD, Tafere K. The impact of a health facility construction campaign on health service utilisation and outcomes: analysis of spatially linked survey and facility location data in Ethiopia. BMJ Glob Health. 2020;5(8):e002430.
Arwal S. Health Posts in Afghanistan. J Gen Practice. 2015;3(213):2.
Negussie A, Girma G. Is the role of Health Extension Workers in the delivery of maternal and child health care services a significant attribute? The case of Dale district, southern Ethiopia. BMC Health Serv Res. 2017;17(1):1–8.
Than KK, Mohamed Y, Oliver V, Myint T, La T, Beeson JG, Luchters S. Prevention of postpartum haemorrhage by community-based auxiliary midwives in hard-to-reach areas of Myanmar: a qualitative inquiry into acceptability and feasibility of task shifting. BMC Pregnancy Childbirth. 2017;17(1):1–10.
Medhanyie A, Spigt M, Kifle Y, Schaay N, Sanders D, Blanco R, GeertJan D, Berhane Y. The role of health extension workers in improving utilization of maternal health services in rural areas in Ethiopia: a cross sectional study. BMC Health Serv Res. 2012;12(1):1–9.
Sakeah E, McCloskey L, Bernstein J, Yeboah-Antwi K, Mills S, Doctor HV. Can community health officer-midwives effectively integrate skilled birth attendance in the community-based health planning and services program in rural Ghana? Reprod Health. 2014;11(1):1–13.
Sarmento DR. Traditional birth attendance (TBA) in a health system: what are the roles, benefits and challenges: a case study of incorporated TBA in Timor-Leste. Asia Pac Fam Med. 2014;13(1):1–9.
Rahmawati R, Bajorek B. Peer Reviewed: A Community Health Worker-Based Program for Elderly People with Hypertension in Indonesia: A Qualitative Study, 2013. Prev Chronic Dis. 2015;12:E175.
Feltner FJ, Ely GE, Whitler ET, Gross D, Dignan M. Effectiveness of community health workers in providing outreach and education for colorectal cancer screening in Appalachian Kentucky. Soc Work Health Care. 2012;51(5):430–40.
Hughes MM, Yang E, Ramanathan D, Benjamins MR. Community-based diabetes community health worker intervention in an underserved Chicago population. J Community Health. 2016;41(6):1249–56.
Panday S, Bissell P, Van Teijlingen E, Simkhada P. The contribution of female community health volunteers (FCHVs) to maternity care in Nepal: a qualitative study. BMC Health Serv Res. 2017;17(1):1–11.
Datiko DG, Lindtjørn B. Health extension workers improve tuberculosis case detection and treatment success in southern Ethiopia: a community randomized trial. PLoS ONE. 2009;4(5):e5443.
le Roux KW, Almirol E, Rezvan PH, Le Roux IM, Mbewu N, Dippenaar E, Stansert-Katzen L, Baker V, Tomlinson M, Rotheram-Borus M. Community health workers impact on maternal and child health outcomes in rural South Africa–a non-randomized two-group comparison study. BMC Public Health. 2020;20(1):1–14.
Witmer A, Seifer SD, Finocchio L, Leslie J, O’Neil EH. Community health workers: integral members of the health care work force. Am J Public Health. 1995;85(8 Pt 1):1055–8.
Wright RA. Community-oriented primary care. The cornerstone of health care reform. Jama. 1993;269(19):2544–7.
Makaula P, Bloch P, Banda HT, Mbera GB, Mangani C, de Sousa A, Nkhono E, Jemu S, Muula AS. Primary Health Care in rural Malawi - a qualitative assessment exploring the relevance of the community-directed interventions approach. BMC Health Serv Res. 2012;12:328.
Katabarwa MN, Habomugisha P, Richards FO Jr, Hopkins D. Community-directed interventions strategy enhances efficient and effective integration of health care delivery and development activities in rural disadvantaged communities of Uganda. Trop Med Int Health : TM & IH. 2005;10(4):312–21.
Madon S, Malecela MN, Mashoto K, Donohue R, Mubyazi G, Michael E. The role of community participation for sustainable integrated neglected tropical diseases and water, sanitation and hygiene intervention programs: A pilot project in Tanzania. Soc Sci Med. 1982;2018(202):28–37.
Okeibunor JC, Orji BC, Brieger W, Ishola G, Otolorin E, Rawlins B, Ndekhedehe EU, Onyeneho N, Fink G. Preventing malaria in pregnancy through community-directed interventions: evidence from Akwa Ibom State, Nigeria. Malaria J. 2011;10:227.
Brieger WR, Sommerfeld JU, Amazigo UV. The Potential for Community-Directed Interventions: Reaching Underserved Populations in Africa. Int Q Community Health Educ. 2015;35(4):295–316.
Braimah JA, Sano Y, Atuoye KN, Luginaah I. Access to primary health care among women: the role of Ghana’s community-based health planning and services policy. Prim Health Care Res Dev. 2019;20:e82.
Kaplan DW, Brindis CD, Phibbs SL, Melinkovich P, Naylor K, Ahlstrand K. A comparison study of an elementary school–based health center: effects on health care access and use. Arch Pediatr Adolesc Med. 1999;153(3):235–43.
Allison MA, Crane LA, Beaty BL, Davidson AJ, Melinkovich P, Kempe A. School-based health centers: improving access and quality of care for low-income adolescents. Pediatrics. 2007;120(4):e887–94.
Keeton V, Soleimanpour S, Brindis CD. School-based health centers in an era of health care reform: Building on history. Curr Probl Pediatr Adolesc Health Care. 2012;42(6):132–56.
Brindis CD, Klein J, Schlitt J, Santelli J, Juszczak L, Nystrom RJ. School-based health centers: Accessibility and accountability. J Adolesc Health. 2003;32(6):98–107.
Hutchinson P, Carton TW, Broussard M, Brown L, Chrestman S. Improving adolescent health through school-based health centers in post-Katrina New Orleans. Child Youth Serv Rev. 2012;34(2):360–8.
Paschall MJ, Bersamin M. School-based health centers, depression, and suicide risk among adolescents. Am J Prev Med. 2018;54(1):44–50.
Minguez M, Santelli JS, Gibson E, Orr M, Samant S. Reproductive health impact of a school health center. J Adolesc Health. 2015;56(3):338–44.
Gibson EJ, Santelli JS, Minguez M, Lord A, Schuyler AC. Measuring school health center impact on access to and quality of primary care. J Adolesc Health. 2013;53(6):699–705.
Bozigar M. A Cross-Sectional Survey to Evaluate Potential for Partnering With School Nurses to Promote Human Papillomavirus Vaccination. Prev Chronic Dis. 2020;17:E111.
Suen J, Attrill S, Thomas JM, Smale M, Delaney CL, Miller MD. Effect of student-led health interventions on patient outcomes for those with cardiovascular disease or cardiovascular disease risk factors: a systematic review. BMC Cardiovasc Disord. 2020;20(1):1–10.
Atuyambe LM, Baingana RK, Kibira SP, Katahoire A, Okello E, Mafigiri DK, Ayebare F, Oboke H, Acio C, Muggaga K. Undergraduate students’ contributions to health service delivery through communitybased education. BMC Med Educ. 2016;16:123.
Stuhlmiller CM, Tolchard B. Developing a student-led health and wellbeing clinic in an underserved community: collaborative learning, health outcomes and cost savings. BMC Nurs. 2015;14(1):1–8.
Campbell DJ, Gibson K, O’Neill BG, Thurston WE. The role of a student-run clinic in providing primary care for Calgary’s homeless populations: a qualitative study. BMC Health Serv Res. 2013;13(1):1–6.
Simpson SA, Long JA. Medical student-run health clinics: important contributors to patient care and medical education. J Gen Intern Med. 2007;22(3):352–6.
Gruen RL, O’Rourke IC, Bailie RS, d’Abbs PH, O’Brien MM, Verma N. Improving access to specialist care for remote Aboriginal communities: evaluation of a specialist outreach service. Med J Aust. 2001;174(10):507–11.
Gruen RL, Weeramanthri T, Bailie R. Outreach and improved access to specialist services for indigenous people in remote Australia: the requirements for sustainability. J Epidemiol Community Health. 2002;56(7):517–21.
Gruen RL, Bailie RS, Wang Z, Heard S, O’Rourke IC. Specialist outreach to isolated and disadvantaged communities: a population-based study. The Lancet. 2006;368(9530):130–8.
Bond M, Bowling A, Abery A, McClay M, Dickinson E. Evaluation of outreach clinics held by specialists in general practice in England. J Epidemiol Community Health. 2000;54(2):149–56.
Irani M, Dixon M, Dean JD. Care closer to home: past mistakes, future opportunities. J R Soc Med. 2007;100(2):75–7.
Bailey JJ, Black ME, Wilkin D. Specialist outreach clinics in general practice. BMJ (Clinical research ed). 1994;308(6936):1083–6.
De Roodenbeke E, Lucas S, Rouzaut A, Bana F. Outreach services as a strategy to increase access to health workers in remote and rural areas. Geneva: WHO; 2011.
Bowling A, Stramer K, Dickinson E, Windsor J, Bond M. Evaluation of specialists’ outreach clinics in general practice in England: process and acceptability to patients, specialists, and general practitioners. J Epidemiol Community Health. 1997;51(1):52–61.
Spencer N. Consultant paediatric outreach clinics–a practical step in integration. Arch Dis Child. 1993;68(4):496–500.
Aljasir B, Alghamdi MS. Patient satisfaction with mobile clinic services in a remote rural area of Saudi Arabia. East Mediterr Health J. 2010;16(10):1085–90.
Lee EJ, O’Neal S. A mobile clinic experience: nurse practitioners providing care to a rural population. J Pediatr Health Care. 1994;8(1):12–7.
Cone PH, Haley JM. Mobile clinics in Haiti, part 1: Preparing for service-learning. Nurse Educ Pract. 2016;21:1–8.
Diaz-Perez Mde J, Farley T, Cabanis CM. A program to improve access to health care among Mexican immigrants in rural Colorado. J Rural Health. 2004;20(3):258–64.
Hill C, Zurakowski D, Bennet J, Walker-White R, Osman JL, Quarles A, Oriol N. Knowledgeable Neighbors: a mobile clinic model for disease prevention and screening in underserved communities. Am J Public Health. 2012;102(3):406–10.
Edgerley LP, El-Sayed YY, Druzin ML, Kiernan M, Daniels KI. Use of a community mobile health van to increase early access to prenatal care. Matern Child Health J. 2007;11(3):235–9.
Peters G, Doctor H, Afenyadu G, Findley S, Ager A. Mobile clinic services to serve rural populations in Katsina State, Nigeria: perceptions of services and patterns of utilization. Health Policy Plan. 2014;29(5):642–9.
Neke NM, Gadau G, Wasem J. Policy makers’ perspective on the provision of maternal health services via mobile health clinics in Tanzania—Findings from key informant interviews. PLoS ONE. 2018;13(9):e0203588.
Padmadas SS, Johnson FA, Leone T, Dahal GP. Do mobile family planning clinics facilitate vasectomy use in Nepal? Contraception. 2014;89(6):557–63.
Macinko J, Harris MJ. Brazil’s family health strategy—delivering community-based primary care in a universal health system. N Engl J Med. 2015;372(23):2177–81.
Macinko J, Lima Costa MF. Access to, use of and satisfaction with health services among adults enrolled in Brazil’s Family Health Strategy: evidence from the 2008 National Household Survey. Tropical Med Int Health. 2012;17(1):36–42.
Dourado I, Oliveira VB, Aquino R, Bonolo P, Lima-Costa MF, Medina MG, Mota E, Turci MA, Macinko J. Trends in primary health care-sensitive conditions in Brazil: the role of the Family Health Program (Project ICSAP-Brazil). Medical care. 2011;49:577–84.
Aquino R, De Oliveira NF, Barreto ML. Impact of the family health program on infant mortality in Brazilian municipalities. Am J Public Health. 2009;99(1):87–93.
Chong P-N, Tang WE. Transforming primary care—the way forward with the TEAMS2 approach. Fam Pract. 2019;36(3):369–70.
Primary Health Care Performance Initiatives (phcpi). Improvement strategies model: Population health management: Empanelment. Available at https://improvingphc.org/sites/default/files/Empanelment%20-%20v1.2%20-%20last%20updated%2012.13.2019.pdf . Accessed on 18 March 2022.
McGough P, Chaudhari V, El-Attar S, Yung P. A health system’s journey toward better population health through empanelment and panel management. Healthcare. 2018;6(66):1–9.
Bearden T, Ratcliffe HL, Sugarman JR, Bitton A, Anaman LA, Buckle G, Cham M, Quan DCW, Ismail F, Jargalsaikhan B. Empanelment: A foundational component of primary health care. Gates Open Res. 2019;3:1654.
Hsiao WC. Unmet health needs of two billion: is community financing a solution? 2001.
Wang W, Temsah G, Mallick L. The impact of health insurance on maternal health care utilization: evidence from Ghana, Indonesia and Rwanda. Health Policy Plan. 2017;32(3):366–75.
Atnafu DD, Tilahun H, Alemu YM. Community-based health insurance and healthcare service utilisation, North-West, Ethiopia: a comparative, cross-sectional study. BMJ Open. 2018;8(8):e019613.
USAID. Ethiopia’s Community-based Health Insurance: A Step on the Road to Universal Health Coverage. Available at https://www.hfgproject.org/ethiopias-community-based-health-insurance-step-road-universal-health-coverage/ . Accessed on 18 March 2022.
Blanchet NJ, Fink G, Osei-Akoto I. The effect of Ghana’s National Health Insurance Scheme on health care utilisation. Ghana Med J. 2012;46(2):76–84.
CAS Google Scholar
Nshakira-Rukundo E, Mussa EC, Nshakira N, Gerber N, von Braun J. Impact of community-based health insurance on utilisation of preventive health services in rural Uganda: a propensity score matching approach. Int J Health Econ Manag. 2021;21(2):203–27.
Mwaura JW, Pongpanich S. Access to health care: the role of a community based health insurance in Kenya. Pan Afr Med J. 2012;12(1):35.
Jutting JP. The Impact Of Health Insurance On The Access To Health Care And Financial Protection In Rural Developing Countries: The Example of Senegal. HNP discussion paper series;. World Bank, Washington, DC. © World Bank. 2011. https://openknowledge.worldbank.org/handle/10986/13774 . License: CC BY 3.0 IGO.
Balamiento NC. The impact of social health insurance on healthcare utilization outcomes: evidence from the indigent program of the Philippine National Health Insurance. International Institute of Social Studies. 2018. Available at https://thesis.eur.nl/pub/46445/Balamiento,%20Neeanne_MA_2017_18%20_ECD.pdf . Accessed 30 Nov 2022.
Farrell CM, Gottlieb A. The effect of health insurance on health care utilization in the justice-involved population: United States, 2014–2016. Am J Public Health. 2020;110(S1):S78–84.
Thuong NTT. Impact of health insurance on healthcare utilisation patterns in Vietnam: a survey-based analysis with propensity score matching method. BMJ Open. 2020;10(10):e040062.
Custodio R, Gard AM, Graham G. Health information technology: addressing health disparity by improving quality, increasing access, and developing workforce. J Health Care Poor Underserved. 2009;20(2):301–7.
Meier CA, Fitzgerald MC, Smith JM. eHealth: extending, enhancing, and evolving health care. Annu Rev Biomed Eng. 2013;15:359–82.
Anstey Watkins JOT, Goudge J, Gomez-Olive FX, Griffiths F. Mobile phone use among patients and health workers to enhance primary healthcare: A qualitative study in rural South Africa. Soc Sci Med. 1982;2018(198):139–47.
Kuntalp M, Akar O. A simple and low-cost Internet-based teleconsultation system that could effectively solve the health care access problems in underserved areas of developing countries. Comput Methods Programs Biomed. 2004;75(2):117–26.
Price M, Yuen EK, Goetter EM, Herbert JD, Forman EM, Acierno R, Ruggiero KJ. mHealth: a mechanism to deliver more accessible, more effective mental health care. Clin Psychol Psychother. 2014;21(5):427–36.
Bashshur RL, Shannon GW, Krupinski EA, Grigsby J, Kvedar JC, Weinstein RS, Sanders JH, Rheuban KS, Nesbitt TS, Alverson DC, et al. National telemedicine initiatives: essential to healthcare reform. Telemed J E Health. 2009;15(6):600–10.
Norton SA, Burdick AE, Phillips CM, Berman B. Teledermatology and underserved populations. Arch Dermatol. 1997;133(2):197–200.
Raza T, Joshi M, Schapira RM, Agha Z. Pulmonary telemedicine–a model to access the subspecialist services in underserved rural areas. Int J Med Informatics. 2009;78(1):53–9.
Shouneez YH. Smartphone hearing screening in mHealth assisted community-based primary care. UPSpace Institutional Repository, Department of Liberary Service. Dissertation (MCommPath)--University of Pretoria. 2016. Available at http://hdl.handle.net/2263/53477 . Accessed 17 Mar 2022.
Marcin JP, Ellis J, Mawis R, Nagrampa E, Nesbitt TS, Dimand RJ. Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community. Pediatrics. 2004;113(1 Pt 1):1–6.
Olu O, Muneene D, Bataringaya JE, Nahimana M-R, Ba H, Turgeon Y, Karamagi HC, Dovlo D. How can digital health technologies contribute to sustainable attainment of universal health coverage in Africa? A perspective. Front Public Health. 2019;7:341.
Ryan MH, Yoder J, Flores SK, Soh J, Vanderbilt AA. Using health information technology to reach patients in underserved communities: A pilot study to help close the gap with health disparities. Global J Health Sci. 2016;8(6):86.
Buckwalter KC, Davis LL, Wakefield BJ, Kienzle MG, Murray MA. Telehealth for elders and their caregivers in rural communities. Fam Community Health. 2002;25(3):31–40.
WHO Regional Committee for Africa. Promoting the role of traditional medicine in health systems: a strategy for the African Region. World Health Organization. Regional Office for Africa. Available at http://www.who.int/iris/handle/10665/95467. .
Mishra SR, Neupane D, Kallestrup P. Integrating complementary and alternative medicine into conventional health care system in developing countries: an example of Amchi. J Evid-Based Complementary Altern Med. 2015;20(1):76–9.
Mbwambo ZH, Mahunnah RL, Kayombo EJ. Traditional health practitioner and the scientist: bridging the gap in contemporary health research in Tanzania. Tanzan Health Res Bull. 2007;9(2):115–20.
Poudyal AK, Jimba M, Murakami I, Silwal RC, Wakai S, Kuratsuji T. A traditional healers’ training model in rural Nepal: strengthening their roles in community health. Trop Med Int Health : TM & IH. 2003;8(10):956–60.
Payyappallimana U. Role of Traditional Medicine in Primary Health Care: An Overview of Perspectives and Challenges. Yokohama J Social Sciences. 2009;14(6):723–43.
Kange’ethe SM. Traditional healers as caregivers to HIV/AIDS clients and other terminally challenged persons in Kanye community home-based care programme (CHBC), Botswana. SAHARA J. 2009;6(2):83–91.
Habtom GK. Integrating traditional medical practice with primary healthcare system in Eritrea. J Complement Integr Med. 2015;12(1):71–87.
Ejaz I, Shaikh BT, Rizvi N. NGOs and government partnership for health systems strengthening: a qualitative study presenting viewpoints of government, NGOs and donors in Pakistan. BMC Health Serv Res. 2011;11(1):1–7.
Wu FS. International non-governmental actors in HIV/AIDS prevention in China. Cell Res. 2005;15(11):919–22.
Biermann O, Eckhardt M, Carlfjord S, Falk M, Forsberg BC. Collaboration between non-governmental organizations and public services in health–a qualitative case study from rural Ecuador. Glob Health Action. 2016;9(1):32237.
Mercer A, Khan MH, Daulatuzzaman M, Reid J. Effectiveness of an NGO primary health care programme in rural Bangladesh: evidence from the management information system. Health Policy Plan. 2004;19(4):187–98.
Baqui AH, Rosecrans AM, Williams EK, Agrawal PK, Ahmed S, Darmstadt GL, Kumar V, Kiran U, Panwar D, Ahuja RC. NGO facilitation of a government community-based maternal and neonatal health programme in rural India: improvements in equity. Health Policy Plan. 2008;23(4):234–43.
Ricca J, Kureshy N, LeBan K, Prosnitz D, Ryan L. Community-based intervention packages facilitated by NGOs demonstrate plausible evidence for child mortality impact. Health Policy Plan. 2014;29(2):204–16.
Ahmed N, DeRoeck D, Sadr-Azodi N. Private sector engagement and contributions to immunisation service delivery and coverage in Sudan. BMJ Glob Health. 2019;4(2):e001414.
Edimond BJ. The Contribution of Non-Governmental Organizations in Delivery of Basic Health Services in Partnership with Local Government. Doctoral Dissertation, Uganda Martyrs University. 2014.
Chand S, Patterson J: Faith-Based Models for Improving Maternal and Newborn Health. IMA World Health and ActionAid International USA, 2007 Available at https://imaworldhealthorg/wp-content/uploads/2014/06/faith_based_models_for_improving_maternal_and_newborn_health.pdf
Magezi V. Churchdriven primary health care: Models for an integrated church and community primary health care in Africa (a case study of the Salvation Army in East Africa). HTS Teologiese Studies/ Theological Studies. 2018;74(2):4365.
Villatoro AP, Dixon E, Mays VM. Faith-based organizations and the Affordable Care Act: Reducing Latino mental health care disparities. Psychol Serv. 2016;13(1):92–104.
Levin J. Faith-based initiatives in health promotion: history, challenges, and current partnerships. American journal of health promotion : AJHP. 2014;28(3):139–41.
Green A, Shaw J, Dimmock F, Conn C. A shared mission? Changing relationships between government and church health services in Africa. Int J Health Plann Manage. 2002;17(4):333–53.
Bandy G, Crouch A. Building from common foundations : the World Health Organization and faith-based organizations in primary healthcare. World Health Organization; 2008. Available at https://apps.who.int/iris/handle/10665/43884 . Accessed 16 Mar 2022.
Zahnd WE, Jenkins WD, Shackelford J, Lobb R, Sanders J, Bailey A. Rural cancer screening and faith community nursing in the era of the Affordable Care Act. J Health Care Poor Underserved. 2018;29(1):71–80.
Wagle K. Primary Health Care (PHC): History, Principles, Pillars, Elements & Challenges. Global Health, 2020. Available at https://www.publichealthnotes.com/primary-health-care-phc-history-principles-pillars-elements-challenges/ . Accessed 4 June 2022.
Bhatt J, Bathija P. Ensuring access to quality health care in vulnerable communities. Acad Med. 2018;93(9):1271.
Arvey SR, Fernandez ME. Identifying the core elements of effective community health worker programs: a research agenda. Am J Public Health. 2012;102(9):1633–7.
Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D, Wang J. Community health needs assessment: potential for population health improvement. Popul Health Manag. 2016;19(3):178–86.
Chudgar RB, Shirey LA, Sznycer-Taub M, Read R, Pearson RL, Erwin PC. Local health department and academic institution linkages for community health assessment and improvement processes: a national overview and local case study. J Public Health Manag Pract. 2014;20(3):349–55.
Desta FA, Shifa GT, Dagoye DW, Carr C, Van Roosmalen J, Stekelenburg J, Nedi AB, Kols A, Kim YM. Identifying gaps in the practices of rural health extension workers in Ethiopia: a task analysis study. BMC Health Serv Res. 2017;17(1):1–9.
Lehmann U, Sanders D. Community health workers: what do we know about them. The state of the evidence on programmes, activities, costs and impact on health outcomes of using community health workers Geneva: World Health Organization; 2007. Available at https://www.hrhresourcecenter.org/node/1587.html . Accessed 17 Mar 2022.
Chen N, Raghavan M, Albert J, McDaniel A, Otiso L, Kintu R, West M, Jacobstein D. The community health systems reform cycle: strengthening the integration of community health worker programs through an institutional reform perspective. Global Health: Sci Practice. 2021;9(Supplement 1):S32–46.
Roser M, Ortiz-Ospina E: Global rise of education. Our World in Data 2017. Available at https://ourworldindata.org/global-rise-of-education . Accessed on 29 May 2019.
Santelli J, Morreale M, Wigton A, Grason H. School health centers and primary care for adolescents: a review of the literature. J Adolesc Health. 1996;18(5):357–66.
Wade TJ, Mansour ME, Guo JJ, Huentelman T, Line K, Keller KN. Access and utilization patterns of school-based health centers at urban and rural elementary and middle schools. Public Health Reports. 2008;123(6):739–50.
Johnson I, Hunter L, Chestnutt IG. Undergraduate students’ experiences of outreach placements in dental secondary care settings. Eur J Dent Educ. 2012;16(4):213–7.
Ndira S, Ssebadduka D, Niyonzima N, Sewankambo N, Royall J. Tackling malaria, village by village: a report on a concerted information intervention by medical students and the community in Mifumi Eastern Uganda. Afr Health Sci. 2014;14(4):882–8.
Frakes K-a, Brownie S, Davies L, Thomas JB, Miller M-E, Tyack Z. Capricornia Allied Health Partnership (CAHP): a case study of an innovative model of care addressing chronic disease through a regional student-assisted clinic. Aust Health Rev. 2014;38(5):483–6.
Frakes KA, Brownie S, Davies L, Thomas J, Miller ME, Tyack Z. The sociodemographic and health-related characteristics of a regional population with chronic disease at an interprofessional student-assisted clinic in Q ueensland C apricornia A llied H ealth P artnership. Aust J Rural Health. 2013;21(2):97–104.
Frakes K-A, Tyzack Z, Miller M, Davies L, Swanston A, Brownie S. The Capricornia Project: Developing and implementing an interprofessional student-assisted allied health clinic. 2011.
Frakes K-A, Brownie S, Davies L, Thomas J, Miller M-E, Tyack Z. Experiences from an interprofessional student-assisted chronic disease clinic. J Interprof Care. 2014;28(6):573–5.
Schutte T, Tichelaar J, Dekker RS, van Agtmael MA, de Vries TP, Richir MC. Learning in student-run clinics: A systematic review. Med Educ. 2015;49(3):249–63.
Paim J, Travassos C, Almeida C, Bahia L, Macinko J. The Brazilian health system: history, advances, and challenges. The Lancet. 2011;377(9779):1778–97.
Rocha R, Soares RR. Evaluating the impact of community-based health interventions: evidence from Brazil’s Family Health Program. Health Econ. 2010;19(S1):126–58.
Rasella D, Harhay MO, Pamponet ML, Aquino R, Barreto ML. Impact of primary health care on mortality from heart and cerebrovascular diseases in Brazil: a nationwide analysis of longitudinal data. BMJ (Clinical research ed). 2014;349:g4014.
Harris M. Brazil’s Family Health Programme: A cost effective success that higher income countries could learn from. BMJ: Br Med J. 2010;341(7784):1171–2.
Starfield B. Is primary care essential? The lancet. 1994;344(8930):1129–33.
Donfouet HPP, Mahieu P-A. Community-based health insurance and social capital: a review. Heal Econ Rev. 2012;2(1):1–5.
Zhang L, Wang H, Wang L, Hsiao W. Social capital and farmer’s willingness-to-join a newly established community-based health insurance in rural China. Health Policy. 2006;76(2):233–42.
Donfouet HPP. Essombè J-RE, Mahieu P-A, Malin E: Social capital and willingness-to-pay for community-based health insurance in rural Cameroon. Global J Health Sci. 2011;3(1):142.
Grunau J. Exploring people’s motivation to join or not to join the community-based health insurance’Sina Passenang’in Sotouboua, Togo. 2013.
Gitahi JW. Innovative Healthcare Financing and Equity through Community Based Health Insurance Schemes (CBHHIS) In Kenya. United States International University-Africa Digital Repository. Available at http://erepo.usiu.ac.ke/11732/3654 . Accessed 18 May 2022.
Carrin G, Waelkens MP, Criel B. Community-based health insurance in developing countries: a study of its contribution to the performance of health financing systems. Tropical Med Int Health. 2005;10(8):799–811.
Umeh CA, Feeley FG. Inequitable access to health care by the poor in community-based health insurance programs: a review of studies from low-and middle-income countries. Global Health: Science And Practice. 2017;5(2):299–314.
Odebiyi AI. Western trained nurses’ assessment of the different categories of traditional healers in southwestern Nigeria. Int J Nurs Stud. 1990;27(4):333–42.
Abdullahi AA. Trends and challenges of traditional medicine in Africa. Afr J Tradit Complement Altern Med : AJTCAM. 2011;8(5 Suppl):115–23.
Taye OR. Yoruba Traditional Medicine and the Challenge of Integration. The J Pan Afr Studies. 2009;3(3):73–90.
Konadu K. Medicine and Anthropology in Twentieth Century Africa: Akan Medicine and Encounters with (Medical) Anthropology. African Studies Quarterly. 2008;10(2 & 3).
Benzie IF, Wachtel-Galor S: Herbal medicine: biomolecular and clinical aspects. 2nd Ed. 2011. Available at https://www.crcpress.com/Herbal-Medicine-Biomolecular-and-Clinical-Aspects-Second-Edition/Benzie-Wachtel-Galor/p/book/9781439807132 . Accessed 21 May 2022.
Ejughemre U. Donor support and the impacts on health system strengthening in sub-saharan africa: assessing the evidence through a review of the literature. Am J Public Health Res. 2013;1(7):146–51.
Seppey M, Ridde V, Touré L, Coulibaly A. Donor-funded project’s sustainability assessment: a qualitative case study of a results-based financing pilot in Koulikoro region. Mali Globalization and health. 2017;13(1):1–15.
Shaw RP, Wang H, Kress D, Hovig D. Donor and domestic financing of primary health care in low income countries. Health Systems & Reform. 2015;1(1):72–88.
Gotsadze G, Chikovani I, Sulaberidze L, Gotsadze T, Goguadze K, Tavanxhi N. The challenges of transition from donor-funded programs: results from a theory-driven multi-country comparative case study of programs in Eastern Europe and Central Asia supported by the Global Fund. Global Health: Science and Practice. 2019;7(2):258–72.
Ascroft J, Sweeney R, Samei M, Semos I, Morgan C. Strengthening church and government partnerships for primary health care delivery in Papua New Guinea: Lessons from the international experience. Health policy and health finance knowledge hub Working paper series. 2011(16).
Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213–34.
Olivier J, Wodon Q. The role of faith-inspired health care providers in Sub-Saharan Africa and public private partnerships: Strengthening the Evidence for faith-inspired health engagement in Africa, Volume 1. Health, Nutrition and Population (HNP) Discussion Paper Series 76223v1. Available at https://documents1.worldbank.org/curated/en/851911468203673017 . Accessed 20 May 2022.
Schumann C, Stroppa A, Moreira-Almeida A. The contribution of faith-based health organisations to public health. Int Psychiatry. 2011;8(3):62–4.
Download references
Acknowledgements
The author would like to thank IPHC- E for funding this review.
This review was funded by International Institute for Primary Health Care- Ethiopia (IPHC- E).
Author information
Authors and affiliations.
Department of Environmental and Occupational Health and Safety, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Zemichael Gizaw
International Institute for Primary Health Care- Ethiopia, Ethiopian Public Health Institute, Addis Ababa, Ethiopia
Tigist Astale & Getnet Mitike Kassie
You can also search for this author in PubMed Google Scholar
Contributions
ZG prepared the manuscript. TA and GMK critically reviewed the protocol and manuscript. All the authors read and approved the final manuscript.
Corresponding author
Correspondence to Zemichael Gizaw .
Ethics declarations
Ethics approval and consent to participate.
Systematic review does not required ethics approval.
Consent for publication
This manuscript does not contain any individual person’s data.
Competing interests
The authors declared that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: .
Searchstrategy. MEDLINE (PubMed).
Additional file 2: Appendix 2: Table A1.
Description of full-text articles which discussed community health programs or community-directed interventions as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 3:
Appendix 3: Table A2. Description of full-text articles which discussed school-based healthcareservices as a strategy to improve PHCservice delivery in rural communities.
Additional file 4:
Appendix 4: Table A3. Description of full-text articles which discussed student-led healthcareservices as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 5: Appendix 5: Table A4
. Descriptionof full-text articles which discussed outreach services or mobile clinics as astrategy to improve PHC service delivery in ruralcommunities.
Additional file 6:
Appendix 6: Table A5. Description of full-text articles which discussed family health program as astrategy to improve PHC service delivery in rural,communities.
Additional file 7:
Appendix 7: Table A6. Description of full-text articles whichdiscussed empanelment as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 8:
Appendix 9: Table A8. Description of full-text articles which discussed telemedicine or mobile healthas a strategy to improve PHC service delivery in ruralcommunities.
Additional file 9:
Appendix 8: Table A7. Description of full-text articles which discussed community health funding schemes as a strategy to improve PHC service delivery in ruralcommunities.
Additional file 10:
Appendix 10: Table A9. Description of full-text articles which discussed promoting the role of workingwith traditional healers as a strategy toimprove PHC service delivery in rural communities.
Additional file 11:
Appendix 11: Table A10. Description of full-text articles which discussed working with non-profitprivate sectors and non-governmental organizations as a strategy to improve PHC service delivery in rural communities.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gizaw, Z., Astale, T. & Kassie, G.M. What improves access to primary healthcare services in rural communities? A systematic review. BMC Prim. Care 23 , 313 (2022). https://doi.org/10.1186/s12875-022-01919-0
Download citation
Received : 09 August 2022
Accepted : 18 November 2022
Published : 06 December 2022
DOI : https://doi.org/10.1186/s12875-022-01919-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Access to PHC services
- Rural communities
- Key strategies to improve access to PHC services
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Literature reviews establish the foundation of academic inquires. However, in the planning field, we lack rigorous systematic reviews. In this article, through a systematic search on the methodology of literature review, we categorize a typology of literature reviews, discuss steps in conducting a systematic literature review, and provide suggestions on how to enhance rigor in literature ...
The best reviews synthesize studies to draw broad theoretical conclusions about what a literature means, linking theory to evidence and evidence to theory. This guide describes how to plan, conduct, organize, and present a systematic review of quantitative (meta-analysis) or qualitative (narrative review, meta-synthesis) information.
A Systematic Literature Review (SLR) is a research methodology to collect, identify, and critically analyze the available research studies (e.g., articles, conference proceedings, books, dissertations) through a systematic procedure [12]. An SLR updates the reader with current literature about a subject [6].
Systematic review vs. literature review. A literature review is a type of review that uses a less systematic and formal approach than a systematic review. Typically, an expert in a topic will qualitatively summarize and evaluate previous work, without using a formal, explicit method.
A systematic review collects secondary data, and is a synthesis of all available, relevant evidence which brings together all existing primary studies for review (Cochrane 2016). A systematic review differs from other types of literature review in several major ways.
The systematic review is a rigorous method of collating and synthesizing evidence from multiple studies, producing a whole greater than the sum of parts. This textbook is an authoritative and accessible guide to an activity that is often found overwhelming.
Once a clear focus and PICO question have been developed, the next step is to conduct an initial scoping search of the literature. A scoping search is a basic, fairly brief search of the existing literature that will give an idea of the breadth of studies on a chosen topic, and whether a systematic review has already been conducted on the same topic.
Screen the literature. Assess the quality of the studies. Extract the data. Analyze the results. Interpret and present the results. 1. Decide on your team. When carrying out a systematic literature review, you should employ multiple reviewers in order to minimize bias and strengthen analysis.
Introduction and background. A literature review provides an important insight into a particular scholarly topic. It compiles published research on a topic, surveys different sources of research, and critically examines these sources [].A literature review may be argumentative, integrative, historical, methodological, systematic, or theoretical, and these approaches may be adopted depending ...
A preliminary review, which can often result in a full systematic review, to understand the available research literature, is usually time or scope limited. Complies evidence from multiple reviews and does not search for primary studies. 3. Identifying a topic and developing inclusion/exclusion criteria.
A systematic review, however, is a comprehensive literature review conducted to answer a specific research question. Authors of a systematic review aim to find, code, appraise, and synthesize all of the previous research on their question in an unbiased and well-documented manner.
Systematic literature reviews (SRs) are a way of synthesising scientific evidence to answer a particular research question in a way that is transparent and reproducible, while seeking to include all published ... SRs treat the literature review process like a scientific process, and apply concepts of empirical research in order to make the ...
A systematic review is a type of study that synthesises research that has been conducted on a particular topic. Systematic reviews are considered to provide the highest level of evidence on the hierarchy of evidence pyramid. Systematic reviews are conducted following rigorous research methodology. ... (literature review or authoritative review ...
This article provides a step-by-step approach to conducting and reporting systematic literature reviews (SLRs) in the domain of healthcare design and discusses some of the key quality issues associated with SLRs. SLR, as the name implies, is a systematic way of collecting, critically evaluating, integrating, and presenting findings from across ...
Abstract. Performing a literature review is a critical first step in research to understanding the state-of-the-art and identifying gaps and challenges in the field. A systematic literature review is a method which sets out a series of steps to methodically organize the review. In this paper, we present a guide designed for researchers and in ...
Regardless of this commonality, both types of review vary significantly. The following table provides a detailed explanation as well as the differences between systematic and literature reviews. Kysh, Lynn (2013): Difference between a systematic review and a literature review.
Mixed studies review/mixed methods review: Refers to any combination of methods where one significant component is a literature review (usually systematic). Within a review context it refers to a combination of review approaches for example combining quantitative with qualitative research or outcome with process studies
Background. A systematic review, as its name suggests, is a systematic way of collecting, evaluating, integrating, and presenting findings from several studies on a specific question or topic.[] A systematic review is a research that, by identifying and combining evidence, is tailored to and answers the research question, based on an assessment of all relevant studies.[2,3] To identify assess ...
The semi-systematic or narrative review approach is designed for topics that have been conceptualized differently and studied by various groups of researchers within diverse disciplines and that hinder a full systematic review process (Wong et al., 2013). That is, to review every single article that could be relevant to the topic is simply not ...
The difference between literature review and systematic review comes back to the initial research question. Whereas the systematic review is very specific and focused, the standard literature review is much more general. The components of a literature review, for example, are similar to any other research paper.
LITERATURE REVIEW. Often used as a generic term to describe any type of review. More precise definition: Published materials that provide an examination of published literature. Can cover wide range of subjects at various levels of comprehensiveness. Identifies gaps in research, explains importance of topic, hypothesizes future work, etc.
We conducted a systematic literature review by searching the SCOPUS and PubMed databases for keywords related to housing price and health. Articles were screened by two reviewers for eligibility, which restricted inclusion to original research articles measuring changes in housing prices and health outcomes, published prior to June 31st, 2022.
Systematic reviews that summarize the available information on a topic are an important part of evidence-based health care. There are both research and non-research reasons for undertaking a literature review. It is important to systematically review the literature when one would like to justify the need for a study, to update personal ...
Systematic literature review. A comprehensive search strategy was designed to identify English-language studies published in peer-reviewed journals providing data on risk factors or predictors of moderate or severe exacerbations in adults aged ≥ 40 years with a diagnosis of COPD (sample size ≥ 100).
The review can also help in identifying unexplored opportunities for promoting media literacy and investigating misinformation, disinformation, and hate speech. Therefore, a systematic review of Internet memes is conducted following Okoli's (Citation 2015) framework. The findings highlight the research gap in terms of examining their economic ...
Background. Systematic literature searching is recognised as a critical component of the systematic review process. It involves a systematic search for studies and aims for a transparent report of study identification, leaving readers clear about what was done to identify studies, and how the findings of the review are situated in the relevant evidence.
In this systematic literature review, 18 of 110 (16.4%) of the included studies discussed that outreach services or mobile clinics in primary care and rural hospital settings can improve access to PHC services in rural communities. Mobile outreach service is defined as healthcare services provided by a mobile team of trained providers, from a ...