Planning and Conducting Health Education for Community Members
Health education is any combination of learning experiences designed to help individuals and communities improve their environmental health literacy. The goals of health education are to increase awareness of local environmental conditions, potential exposures, and the impacts of exposures on individual and public health. Health education can also prepare community members to receive and better understand the findings of your public health work.
Some health education takes the form of shorter, one-on-one, or small group conversations with community members, state, territorial, local, and tribal (STLT) partners, and stakeholders. In the beginning of your public health work, you may need to constantly educate community members about exposure sources and exposure pathways –that is, how they may encounter harmful substances.
Later in your public health work, you may want to do a full community workshop or participate in existing community events to increase understanding about specific exposures related to the chemical of concern. Be sure to address how the harmful substance may be encountered, levels of exposure, and ways community members can prevent, reduce, or eliminate exposure. There may be other concerns that are not chemical-specific, such as environmental odors and community stress.
Health education is a professional discipline with unique graduate-level training and credentialing. Health educators are critical partners that advise in the development and implementation of health education programs. Public health work benefits from the skills that a health educator can provide. (See resource: What Is a Health Education Specialist? external icon ) If you don’t have this training, see what you can do to build your skills and improve your one-on-one and small group educational conversations. Health educators may also work with other public health professionals such as health communication specialists. Health communication specialists develop communication strategies to inform and influence individual and community decisions that enhance health.
- Assess individual and community needs for health education. (See activity: Developing a Community Profile )
- Ask community members about factors that directly or indirectly increase the degree of exposure to environmental contamination. Factors may include community members accessing a hazardous site or the presence of lead in house paint, soil, or water.
- Develop a health education plan.
- Listen for opportunities to provide health education throughout your community engagement work.
Despite nearby mines being shut down, a tribal nation continued to face risks of exposure to uranium and radon. To help the community better understand how to reduce the risk of exposure, a group of federal and tribal agencies developed a uranium education workshop. The agencies established a vision and a set of strategies to ensure the workshop was technically-sound and culturally appropriate.

The agencies ensured that they
- Offered the workshop in English and tribal languages,
- Developed materials at the average US reading level for broad accessibility,
- Invited all local tribal families to participate, and
- Piloted the workshop with three communities before finalizing the content.
Before the first pilot workshop, the agencies sought feedback on content, tone, and complexity from community health representatives from the tribe’s department of health. The community health representatives provided many suggestions to tailor the presentation for tribal community audiences.
The workshop content was further refined after each pilot presentation. Working with local professionals and offering workshops as pilot sessions enabled the agencies to tailor content to the needs, preferences, and beliefs of local community members.
CDC’s National Center for Environmental Health (NCEH) and ATSDR have many existing materials to help educate community members about specific chemicals. ATSDR’s Toxicological Profiles and Tox FAQs provide a comprehensive summary and interpretation of available toxicological and epidemiological information on a substance. ATSDR’s Choose Safe Places for Early Care and Education Program provides a framework and practices to make sure early care and education sites are located away from chemical hazards. Consider leveraging or adapting these resources, as well as the following chemical-specific websites and interventions, when developing health education activities for your community, such as
- NCEH’s Childhood Lead Poisoning Prevention Program Website
- ATSDR’s soilSHOP Toolkit —A toolkit to help people learn if their soil is contaminated with lead
- ATSDR’s Don’t Mess with Mercury — Mercury spill prevention materials for schools
Per-and Polyfluoroalkyl Substances (PFAS):
- ATSDR’s PFAS Website
As noted above there may be other concerns that are not chemical-specific, such as environmental odors and community stress. Some helpful resources to address these concerns can be found here:
- ATSDR Environmental Odors
- ATSDR Community Stress Resource Center
Develop health education materials that are culturally appropriate, with community input.
Be aware that your health education messages may be received by the community differently than you intend. Consider testing your messages with community counterparts before you use them widely. Be aware of community beliefs about health and the environment, so that you can develop culturally appropriate health education materials. Your awareness will help you design, plan, and implement activities that are protective of health and respectful of community beliefs. (See callout box: Cultural Awareness )
Avoid stigmatizing (devaluing) communities living in “contaminated” areas [ ATSDR 2020 ].
- CDC Learning Connection (CDC). A source for information about public health training.
- Characteristics of an Effective Health Education Curriculum (CDC). A list of characteristics that you can use to develop an effective health education curriculum.
- Community Environmental Health Education Presentations (ATSDR). A collection of presentations designed for health educators to use in face-to-face sessions with community members to increase environmental health literacy.
- Promoting Environmental Health in Communities (ATSDR). A guide that includes talking points, PowerPoint presentations, and covers the basic concepts of the environment, toxicology, and health.
- What is a Health Education Specialist? external icon (Society for Public Health Education – SOPHE): A description of a health education specialist including areas of responsibility and competency.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Search form
Schedule an Appointment Apply Online Current Student Resources

- Master of Business Administration
- Master of Science in Nursing
- Master of Public Health
- Master of Science in Management and Organizational Behavior
- Dual MPH/Master of Science in Management and Organizational Behavior
- Dual MSN/Master of Business Administration
- Dual MBA/Master of Public Health
- Graduate Certificate in Health Education and Promotion
- Graduate Certificate in Health Management and Policy
- Graduate Certificate in Epidemiology
- Graduate Certificate in Data Analytics
- Post Master's Nurse Educator Certificate
- Post Master's Nurse Executive Leader Certificate
- Graduate Certificate in Change Management
- Graduate Certificate in Digital Marketing
- Graduate Certificate in Project Management
- Graduate Certificate in Talent Management
- Undergraduate Programs
- RN to Bachelor of Science in Nursing
- Other Benedictine Programs:
- On Campus Programs
- Hybrid Programs
- Admission Requirements
- Admission Process
- Financial Aid
- Scholarships & Awards
- Military Students
- International Students
- Virtual Open House
- Course Experience
- Support Services
- Student Orientation
- Alumni Community
- Professional Development
- Online Student BENefits
- Why Choose Benedictine University
- Mission & Values
- Accreditation
- Request Info

Impact Lives
Empowering communities with health education.

Public health officials are constantly working to inform, educate and empower communities about health issues to encourage a healthier way of life. Through educational programs, these professionals strive to inspire communities to make better health choices. There are many different strategies for effective health education in communities to promote interaction and raise awareness on the elements of health related issues. Through effective health education strategies, public health officials can make a considerable impact on the overall health and knowledge within communities.
What is Public Health?
Public Health is described as the science of protecting and improving the health of communities through education, promotion of healthy lifestyles and research for disease and injury prevention. Professionals in Public Health study health related concerns that are potentially affecting communities and work to find ways to educate individuals to avoid health risks.
This field deals with health issues impacting communities as whole. Compared to traditional medical professionals who work on an individual basis, public health officials treat communities as their patients, whether it is on a global scale or local neighborhood. Main duties of a public health official involve conducting research and sharing their findings by implementing educational programs to prevent problems from occurring.
Increasing Health Literacy
Nearly nine out of 10 adults have difficulty using everyday health information that is routinely available in health care facilities. Defined as the ability to process and understand basic health information needed to make informed health decisions, health literacy requires skills to break down that information. This involves calculating numbers to determine things such as cholesterol and sugar levels, measuring medication and understanding nutrition labels. Poor literacy skills have been associated with higher health care expenses by affecting a patient’s capability to effectively use available information to implement health behaviors or respond to health warnings.
National Action Plan
In 2010, the U.S. Department of Health and Human Services developed the National Action Plan to Improve Health Literacy with the goal of creating a society that:
- Provides everyone access to accurate, actionable health information
- Delivers person-centered health information and services
- Supports life-long learning and skills to promote good health
The Action Plan is based on the idea that each individual has the right and need to access health information that will assist in making informed decisions as well as the need for health services to be provided in a way that can be easily understood by the average citizen and beneficial in encouraging health, longevity and quality of life. The seven goals in the plan include:
- Develop and disseminate health and safety information that is accurate, accessible and actionable.
- Promote changes in the health care delivery system that improve information, communication, informed decision-making and access to health services.
- Incorporate accurate and standards-based health and developmentally appropriate health and science information and curricula into child care and education through the university level.
- Support and expand local efforts to provide adult education, English-language Instruction, and culturally and linguistically appropriate health information services in the community.
- Build partnerships, develop guidance and change policies.
- Increase basic research and the development, implementation, and evaluation of practices and interventions to improve health literacy.
- Increase the dissemination and use of evidence-based health literacy practices and interventions.
Educational and Community-Based Programs
Health educators attempt to bridge the gap between distributed information and the public by developing effective educational programs for communities to prevent disease and injury, improve health and enhance the quality of life. These programs play a key role in reaching people outside of traditional health care settings such as schools, worksites and hospitals.
For a community to effectively improve its health, changes are often needed in physical, social, organizational and political environments in order to adjust factors that could be contributing to health problems. For example, communities may need to implement new programs or policies to change community norms in order to promote better health.
These programs work to educate communities on issues such as:
- Chronic diseases
- Mental illness/behavioral health
- Unintended pregnancies
- Nutrition and obesity prevention
- Substance abuse
Through successful education programs that use proper cultural communication methods, public health professionals are able to promote policy change and advocacy for better health education in communities. Health educators are constantly working to ensure that individuals have a clear understanding of how life choices affect health status. For those interested in being involved in the education of communities to promote health education, Benedictine University offers an online Master of Public Health ( MPH ) with a 35-year legacy as well as a specialized certificate in Health Education and Promotion .
Related Benedictine Programs
With the proper stress management, a health care career in nursing is one of the most rewarding careers available. Benedictine University offers an online accredited Master of Science in Nursing (MSN) degree for those looking to advance their nursing careers while juggling their busy work and personal schedules. To learn more click here or talk with one of our Program Advisors today.

- Donate to BMCC
- About BMCC Home
- Mission Statement and Goals
- College Structure and Governance
- Our Students
- Faculty and Academics
- Campus and NYC
- College Administration
- Institutional Advancement
- History of BMCC
- Public Affairs
- Institutional Effectiveness and Analytics
- Race, Equity and Inclusion
- Admissions Home
- BMCC and Beyond
- Visit Our Campus
- Request Information
- After You Are Admitted
- First-Time Freshmen
- Transfer Students
- Evening/Weekend Programs
- Students Seeking Readmission
- Non Degree Students
- Military and Veterans
- Adult Learners
- International Students
- Academic Affairs
- Academic Departments
- Academic Programs
- Success Programs
- Course Listings
- Learning Options
- Course Schedule
- Honors and Awards
- Academic Calendar
- Academic Advisement
- Activities & Athletics
- Administration and Planning
- Compliance & Diversity
- Financial Aid
- Human Resources
- Information Resources and Technology
- Panther Station
- Public Safety
- Sponsored Programs
- Student Affairs
- The Heights
- Continuing Ed
- Faculty/Staff Resources
- BMCC Experts
- Faculty Affairs
- Student Email
- Faculty/Staff Outlook
- BMCC Portal
- Brightspace (coming Summer 2024)
- DegreeWorks
- Connect2Success
- Linkedin Learning
- Faculty Pages
Reimagining BMCC
Monitoring and Reporting Positive Cases
- Health Education
Community Health Education (A.S.)
- Mission Statement
Programs Offered
- Community Health Education
- Gerontology
- School Health Education
- Public Health
BMCC Admissions
or learn more .
The Community Health Education program will teach you to positively influence the health behavior of individuals, groups and communities. You will also learn to address lifestyle factors (i.e., nutrition, physical activity, sexual behavior and drug use) and living conditions that influence health. Community Health Education is the study and improvement of health characteristics among specific populations. Community health is focused on promoting, protecting and improving the health of individuals, communities, and organizations.
The program focuses on career preparation and teaching individuals and groups how to better care for themselves. The Community Health Education degree is a general health degree that prepares you to work in hospitals, community-based organizations, wellness centers or the fitness industry. It provides a foundation for careers in health promotion, disease prevention, fitness, health education and healthcare administration. It is also an entry point for those interested in pursuing clinical degrees.
Transfer Options
You will have the option to transfer to CUNY colleges such as York, Hunter, Lehman and Brooklyn College or to private schools such as Long Island University Brooklyn and Hofstra to major in Community Health Education, Health Administration, Public Health, Gerontology, Physical Therapy, Exercise Science, or Nursing. BMCC has articulation agreements with several four year colleges to allow you to seamlessly continue your education studies there.
Explore Careers
BMCC is committed to students’ long-term success and will help you explore professional opportunities. Undecided? No problem. The college offers Career Coach for salary and employment information, job postings and a self-discovery assessment to help students find their academic and career paths. Visit Career Express to make an appointment with a career advisor, search for jobs or sign-up for professional development activities with the Center for Career Development. Students can also visit the Office of Internships and Experiential Learning to gain real world experience in preparation for a four-year degree and beyond. These opportunities are available to help BMCC students build a foundation for future success.
Professor Lisa Grace Program Coordinator [email protected]
Related Communities
This program is offered in-person, online and in a hybrid format.
Requirements
Community health education academic program maps.
- Community Health Education Program 2 Year Plan
- Community Health Education Program 5 Semester Plan
Required Common Core
Flexible core 3, curriculum requirements, program electives (areas of study).
Choose 12 credits from 1 area of study below:
Health Education and Promotion
Food studies, exercise science, health services administration, health communication, health education electives.
Choose 1 course (3-4 credits) from:
Please note, these requirements are effective the 2021-2022 catalog year. Please check your DegreeWorks account for your specific degree requirements as when you began at BMCC will determine your program requirements.
- Consult with an advisor on which courses to take to satisfy these areas.
- These areas can be satisfied by taking a STEM variant.
- No more than two courses in any discipline or interdisciplinary field can be used to satisfy Flexible Core requirements.
Health Education Department
199 Chambers Street, Room N-798 New York, NY 10007 Phone: (212) 220-1453
Office Hours: Monday-Friday 9 a.m.-5 p.m
Borough of Manhattan Community College The City University of New York 199 Chambers Street New York, NY 10007 Directions (212) 220-8000 Directory
Notice of Non-Discrimination
Bookstore News Event Calendar Job Opportunities Human Resources Admissions Library Give to BMCC Accessibility Virtual Tour Academic Policies Privacy Policy
Information for: Students Faculty & Staff Alumni
Social Media Directory
Educational and Community-Based Programs Workgroup
- Centers for Disease Control and Prevention (CDC)
- Health Resources and Services Administration (HRSA)
- Office of Disease Prevention and Health Promotion (ODPHP)
- National Center for Health Statistics (NCHS)
Members of the Educational and Community Based Programs (ECBP) Workgroup have expertise in areas including school-based health centers, K-12 school and workplace health programs and policies, and medical/allied professions training curricula. They developed the objectives related to educational and community-based programs, and they’ll provide data to track progress toward achieving these objectives throughout the decade.
Read more about the Educational and Community-Based Programs Workgroup
Objective Status
Learn more about objective types
Educational and Community-Based Programs Workgroup Objectives (14)
About the workgroup, approach and rationale.
Educational and community-based programs and strategies are designed to reach people outside of traditional health care settings. These settings may include:
- Community-based organizations
Each setting provides opportunities for people to interact with physical and programmatic structures on a regular basis.
The core objective selected by the ECBP Workgroup aims to increase participation in daily school physical education by helping schools create a strong, evidence-based foundation for physical education programs.
The developmental objectives focus on kindergarten to 12th-grade health interventions, medical and allied health preparation programs, community-based organization prevention services, and worksite health promotion programs. As more data become available, these developmental objectives may become core objectives.
Understanding Educational and Community-Based Programs
Health and quality of life rely on interwoven community systems and factors — not simply on a well-functioning health and medical care system. Making changes within existing systems, like improving school health programs and policies, can effectively optimize the health of many people in a community.
Chronic diseases like heart disease, cancer, and diabetes are the leading causes of death and disability in the United States. They’re also leading drivers of the nation’s annual health care costs. 1 Promoting health in workplaces and community-based organizations, establishing healthy habits in school-age children, and including public health education in medical and allied health preparation programs can directly address this burden.
To improve community health, it’s often necessary to change aspects of the physical, social, organizational, and even political environments to eliminate or reduce factors that contribute to health problems — and to introduce new elements that promote better health. These changes may include:
- Instituting new programs, policies, and practices
- Changing aspects of the physical or organizational infrastructure
- Changing community attitudes, beliefs, or social norms 2
Emerging issues in Educational and Community-Based Programs
- Adopting a Whole School, Whole Community, Whole Child (WSCC) approach to reduce dropout rates. The WSCC model is CDC’s framework for addressing health in schools. The WSCC model is student-centered and emphasizes the role of the community in supporting the school, the connections between health and academic achievement, and the importance of evidence-based school policies and practices.
- Establishing an evidence base for community health and education policy interventions to determine their impact and effectiveness.
- Increasing the number of community health and other auxiliary public health workers — and building their skill level — to support healthier communities.
Centers for Disease Control and Prevention. (2019). About Chronic Diseases. Retrieved from https://www.cdc.gov/chronicdisease/about/index.htm
Institute of Medicine. (2003). The Future of the Public’s Health in the 21st Century . Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK221239
The Office of Disease Prevention and Health Promotion (ODPHP) cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by ODPHP or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link.
Community Health Education Strategies: Student Experiences
- June 23, 2021
- Health@Emory , Read
Editor’s Note: This summer, Exploring Health will feature posts from students within the Health 1,2,3,4 program’s Health 497 course — Community Health Education Strategies. This piece is an introduction to student blog posts about their experiences participating in the course.
Health 1,2,3,4 is an academic program housed within the Center for the Study of Human Health at Emory University. The four-course series aims to provide students with strategies and resources to play an active role in their own health, while also equipping them with the skills to promote the health of their peers. Â In addition to growing their knowledge of the science of health and strategies for health promotion, students who complete courses within the Health 1,2,3,4 program walk away with tangible skills that prepare them for a wide range of careers or educational programs after graduation.
Recognizing the need for students to translate the skills and knowledge acquired in the Human Health courses, the Health 1,2,3,4 program introduced a new course for the 2020-2021 academic year: Health 497 — Community Health Education Strategies. Â In this two-part course (Fall and Spring semesters), students apply their understanding of health education principles and strategies to develop and facilitate the delivery of health education with collaborative partners in the Atlanta and Emory communities. Students who participate in the course are provided with the opportunity to develop professional skills, including leadership, discussion facilitation, communication, and more. Â This year, Health 497 offered two paths for the students to pursue: group coaching to support Healthy Emory’s Diabetes Prevention Program (DPP) and health education lessons for Martin Luther King Jr. Middle School .
Healthy Emory’s Diabetes Prevention Program (DPP) Group Coaching Path
Developed by the Centers for Disease Control and Prevention, Healthy Emory’s Diabetes Prevention Program (DPP) enables Emory employees with pre-diabetes to modify their behaviors to prevent the progression of the disease. Partnering with Healthy Emory, Health 497 provided optional, student-led group coaching sessions to support DPP participants in maintaining healthy behaviors and reaching their health goals. Students within the Health 497 DPP path trained to become student health coaches, developing and facilitating group coaching support sessions on four different topics: food logging, physical activity, embracing a problem-solving mindset, and overcoming social obstacles to healthful nutrition. By participating in the group coaching support sessions, DPP participants revisited key components of the DPP curriculum, discussed personal health barriers, and developed specific goals to promote well-being.
Martin Luther King Jr. Middle School Health Education Path
The Health 1,2,3,4 program maintains a collaborative partnership with Martin Luther King Jr. Middle School to provide health education to its 6 th -8 th grade student population. Students who pursued the Health 497 King Middle School path developed and facilitated lesson plans on several health-related topics, including nutrition, positive mental health, and time and energy management. The middle school students who participated in the health lessons expanded their understanding of health and health-promoting behaviors.
It is with great pleasure that we share the personal experiences and reflections of our Health 497 students within their specific paths to highlight the impact this course has had on their academic and professional growth. Stay tuned for the student pieces as they are posted in the Exploring Health blog this summer.
To learn more about the Health 1,2,3,4 program, visit the program webpage. For more information about collaborative partnership opportunities, contact program director Lisa DuPree at [email protected] .
Related Posts
- previous post: Hunting for a Dose
- next post: Becoming a Student Health Coach
Health Education, Advocacy and Community Mobilisation Module: 12. Planning Health Education Programmes: 1
Study session 12 planning health education programmes: 1, introduction.
Careful planning is essential to the success of all health education activities. This study session is the first of two sessions that will help you to learn about ways in which you can plan your health education activities. In this study session, you will learn about the purpose of planning health education interventions, the basic concepts of planning, and what steps to take when you are planning. The study session will focus in particular on needs assessment, which is the first step in planning health education and promotion. You will learn about categories of needs and techniques that you can use when carrying out needs assessment.
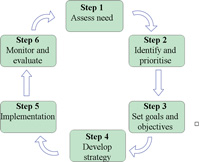
You may have covered some aspects of planning in other modules such as the Health Management, Ethics and Research Module. However, planning in this study session refers specifically to the health education planning process (Figure 12.1).

Learning Outcomes for Study Session 12
When you have studied this session, you should be able to:
12.1 Define and use correctly all of the key words printed in bold . (SAQs 12.1 and 12.2)
12.2 Explaiin the purpose of planning health education activities. (SAQ 12.2)
12.3 List the principles of planning in health education practice. (SAQ 12.2)
12.4 Describe the six steps of planning health education interventions. (SAQ 12.3)
12.5 Describe the main categories of needs assessment. (SAQs 12.4 and 12.5)
12.5 Discuss some of the techniques of needs assessment. (SAQs 12.4 and 12.6)
12.1 Planning health education activities
Before you can begin planning your health education activities, you need to have a clear understanding of what planning means. Planning is the process of making thoughtful and systematic decisions about what needs to be done, how it has to be done, by whom, and with what resources. Planning is central to health education and health promotion activities (Box 12.1). If you do not have a plan, it will not be clear to you how and when you are going to carry out necessary tasks. Everyone makes plans — for looking after their family, for cooking, and so on. You can build on experience you already have in planning, and apply it to health education.
Box 12.1 Key questions to ask when planning
- What will be done?
- When will it be done?
- Where will it be done?
- Who will do it?
- What resources are required?
12.2 The purpose of planning in health education
There are several benefits to planning your activities. Firstly, planning enables you to match your resources to the problem you intend to solve (Figure 12.2). Secondly, planning helps you to use resources more efficiently so you can ensure the best use of scarce resources. Thirdly, it can help avoid duplication of activities. For example, you wouldn’t offer health education to households on the same topic at every visit. Fourthly, planning helps you prioritise needs and activities. This is useful because your community may have a lot of problems, but not the resources or the capacity to solve all these problems at the same time. Finally, planning enables you to think about how to develop the best methods with which to solve a problem.

Haimonot is a Health Extension Practitioner. She is working at a health post near your village. Haimonot is doing health education activities — but not planning them. How would you convince her that planning health education activities would be helpful? What points would you want to talk about? Use the paragraph above to help you plan what you want to say.
To convince Haimonot to plan her own health education activities, you could explain the purpose of planning to her. You could explain that:
- Planning will make it easier for her to identify what she needs to do, and be more efficient in her work.
- Planning would help her to prioritise the health problems in her community that need intervention.
- Planning would help her choose the problems that are most important, and to match resources with the problems she intends to address. This would enable her to use her scarce resources more efficiently, and avoid unnecessary activities.
12.3 Principles of planning in health education
In this section you will learn about the principles you should apply when planning any activity in the community. Planning is not haphazard — that means there is a principle, or a rule, which you should take into account when developing your health education plans. You should always consider the principles shown in Box 12.2 when you plan a piece of work.
Box 12.2 Six principles of planning in health education
- It is important that plans are made with the needs and context of the community in mind. You should try to understand what is currently happening in the community you work in.
- Consider the basic needs and interests of the community. If you do not consider the local needs and interests, your plans will not be effective.
- Plan with the people involved in the implementation of an activity. If you include people they will be more likely to participate, and the plan will be more likely to succeed.
- Identify and use all relevant community resources.
- Planning should be flexible, not rigid. You can modify your plans when necessary. For example, you would have to change your priorities if a new problem, needing an urgent response, arose.
- The planned activity should be achievable, and take into consideration the financial, personnel, and time constraints on the resources you have available. You should not plan unachievable activities.
Meserete is a Health Extension Practitioner. Some time ago she developed a health education programme for her community. At the beginning, she identified some important health problems that were occurring in her community. Local people were recruited to identify their own health problems, and to look for a solution appropriate to their setting. Meserete also identified local resources that would be helpful for her health education activities. Finally, she developed a plan to meet the needs of the community and started to implement it. However, she faced a shortage of resources to carry out all of the items in her plan, so she prioritised the items and modified her plan according to the resources that were available. Look at Box 12.2 above, and work out which principles of planning you think Meserete used.
Meserete has worked well, and used all the principles of planning. She understood local problems [principle 1], and considered the interests of the community [2]. Local people participated in the programme at all stages [3]. She also identified local resources for her health education programme [4], and made sure that her plan was flexible [5]. Meserete also modified her plan, and she thought very carefully about what was achievable [6].
12.4 Steps involved in planning health education activities
Planning is a continuous process. It doesn’t just happen at the start of a project. If you are involved in improving and promoting individual, family and community health, you should make sure that you plan your activities. Planning can be thought of as a cycle that has six steps (Figure 12.3). In this section, you will learn the basic steps to take when planning your health education activities.
12.5 Needs assessment
Conducting a needs assessment is the first, and probably the most important, step in any successful planning process. Sufficient time should be given for each needs assessment. The amount of time required for a needs assessment will depend on the time you have available to address the problem, and the nature and urgency of the problem being assessed.
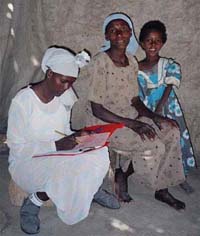
Needs assessment is the process of identifying and understanding the health problems of the community, and their possible causes (Figure 12.4). The problems are then analysed so that priorities can be set for any necessary interventions. The information you collect during a needs assessment will serve as a baseline for monitoring and evaluation at a later stage.

Before you begin a needs assessment, it is important to become familiar with the community you are working in. This involves identifying and talking with the key community members such as the kebele leaders, as well as religious and idir leaders. Ideally, you would involve key community members throughout the planning process, and in the implementation and evaluation of your health education activities.
There are various categories of needs assessment. In order to develop a workable and appropriate plan, several types of needs should be identified, including health needs and resource needs, which are outlined below.
12.5.1 Health needs assessment
In a health needs assessment , you identify health problems prevalent in your community. In other words, you look into any local health conditions which are associated with morbidity, mortality and disability. The local problems may include malaria, TB, HIV/AIDS, diarrhoea, or other conditions arising from the local context, such as goitre caused by lack of iodine in the diet.
Having identified the problems, you need to think about the extent to which local health conditions are a result of insufficient education. For example, are people lacking in knowledge about malaria, or HIV, or diarrhoea? Are they aware that some of their behaviours may be part of the problem?
12.5.2 Resource needs assessment
A resource needs assessment identifies the resources needed to tackle the identified health problems in your community. You should consider whether there is a lack of resources or materials that is preventing the community from practising healthy behaviours. For example, a mother may have good knowledge about malaria and its prevention methods, and want to use Insecticide Treated Bed Nets (ITNs). However, if ITNs are not available, it may not be possible for her to avoid malaria. Therefore, a bed net is a resource which is required to bring about behaviour change. Similarly, a woman may intend to use contraception. However, if contraceptive services are not available in her locality, she remains at risk of unplanned pregnancies. In order to facilitate behaviour change, you should identify ways of addressing this lack of contraceptive resources.
Be aware too that education is in itself one of the great resources you can call on. An education needs assessment should also be part of you plan.
12.5.3 Community resources
First read Case Study 12.1 to help you think about community needs.
Case Study 12.1 Tigist
Ms Tigist is a Health Extension Practitioner. She has been working for three years in a village called Burka. She has conducted a needs assessment in order to develop an appropriate health education plan. During the needs assessment, Ms Tigist identified that malaria, TB, HIV/AIDS and harmful traditional practices, such as female genital mutilation (FGM), were prevalent problems in the village. In addition, she identified that many community members did not know the causes of these problems, or any methods of prevention. For example, many young people did not like to use condoms, and many households did not use bed nets properly due to lack of knowledge. Ms Tigist also identified that many households did not own bed nets.
During a needs assessment, you also need to identify the resources available in the community, such as labour power. This would include finding out about the help that community leaders and volunteers could give, and the local materials and spaces in which to conduct health education sessions. When looking at community resources, you should include local information such as the number of people in each household, their ages and their economic characteristics. You would also include information on community groups and their impact on local health activities and communication networks.
Read Case Study 12.1 again, and then answer the questions below.
- a. Which categories of needs assessment has Ms Tigist conducted?
- b. List the problems Ms Tigist has identified in each of the categories of needs assessment.
a. Ms Tigist has undertaken a health needs assessment (look at Section 12.5.1 if you need to clarify this), and a resource needs assessment (see Section 12.5.2).
b. Problems identified in the health needs assessment showed that malaria, TB, HIV/AIDS and harmful traditional practices were prevalent, and that there is a lack of knowledge about causes and prevention methods for these problems. The main resource need identified was mosquito bed nets in some households.
If you identify malaria as a common health problem in your locality, what additional information would you need in order to plan and implement an appropriate intervention? You will find that looking at Section 12.5.2 again should help here. The important information you need to consider is the effect of current behaviours on the health problem you have chosen.
You should conduct a further assessment for this specific disease to identify the reasons why malaria is a problem in your locality. Knowing it is a problem is only the start. You may identify behavioural factors such as not using bed nets, not seeking timely treatment, or not clearing stagnant water around the dwellings. When all these behavioural factors have been identified, proper health education strategies can be developed to address them, including resources that are needed, and whether you can get them.
12.6 Assessment techniques
Data related to the health needs of the community can be obtained from two main sources — these are called primary and secondary sources . Primary sources are data which you collect during a needs assessment, using techniques such as observation, in-depth interviews, key informant interviews, and focus group discussions. Secondary sources are data that were collected and documented for other purposes, including health centre and health post records, activity reports, and research reports. You may also be able to review data which has already been collected by other people to identify local health problems.
Think about a health education issue you are aware of in your community. Make a list of primary and secondary sources of information you could collect on this issue.
You could collect primary information by conducting some interviews with key people in your community, or holding focus group discussions. Secondary sources of information about the health issue may be available from your local health centre, or health post data.
Various techniques can be used to collect data from the community. These include observation, in-depth interviews, key informant interviews, and focus group discussions — which we describe next.
12.6.1 Observation
To carry out an o bservation , you watch and record events as they are happening. Box 12.3 outlines some situations where observation can be a useful method of collecting relevant data.
Box 12.3 Observation is useful to understand
- Community cultures, norms and values in their social context.
- Human behaviour that may be complex and hidden.
When you are observing households, individuals, or more general practice or behaviour in your community, you may find it useful to use a checklist. For example, you could prepare a checklist to keep a detailed record of household practice and environmental hygiene. Following your checklist might help you to be more systematic about the things you are observing. You cannot observe everything at the same time, so the checklist will help you prioritise what to observe, and how to record what you have seen. A checklist is a very helpful tool for observation, and more generally with planning. There is an example of a checklist in Box 12.4.
Box 12.4 Checklist to organise observations
A Health Extension Practitioner has prepared a checklist to help organise her observations when she visits pregnant mothers in her community to put up new insecticide-treated mosquito nets (ITNs).
The checklist includes the following points:
- Is the net hung above the bed? Yes/No
- Has it been tied at all four angles above the bed? Yes/No
- Is the net tucked under the mattress? Yes/No
- Does the net have a hole anywhere where an insect might get in? Yes/No
You have probably already gathered a lot of information by using observation within your community. If you keep alert to all the things that are happening around you, you will be able to gather a lot of very useful information. Systematically observing and recording what you see is an important technique that you can use to identify health problems and their possible causes (Figure 12.5).
Observation is a real skill, and one you can practise very easily. Make a list of a number of small observations you can make in the next week or so. It doesn’t even have to be work related! Then just try a few out, and make a brief checklist for each.
You could observe how many people greet you over one half-hour period, and make a note of how they do it. You could observe how many bicycles go past in ten minutes and the age of the people riding them. Or choose an observation on health education. The important thing is to really pay attention, and then make some sort of record.
12.6.2 Interviews
The in-depth interview is another important method of data collection. This technique can be used when you want to explore individual beliefs, practices, experiences and attitudes in greater detail. It is usually conducted as a direct personal interview with one person — a single respondent. Using in-depth interviews as a Health Extension Practitioner, you can discover an individual’s motivations, beliefs, attitudes and feelings about health and illness. For example, you may want to explore a mother’s attitudes to — and use of — contraception.
It is a good idea to use open-ended questions to encourage the respondent to talk, rather than closed questions that just require a yes or no answer.
An in-depth interview can take around 30–90 minutes. Box 12.5 lists the steps you should take when conducting an in-depth interview.
Box 12.5 Conducting an in-depth interview
- Identify an individual with whom you are going to conduct an in-depth interview, obtain their consent and arrange a time.
- Prepare your interview guide — this is a list of questions you can use to guide you during the interview. You can generate more questions during the interview if other issues arise that you want to follow up.
- Write down the responses as accurately as you can. You can also use a tape recorder to record the responses. However, you should ask permission from the respondent to use a tape recorder.
- After the interview is completed, review your notes or listen to the tape and prepare a detailed report of what you have learned.

Perhaps you could practise inventing open-ended questions. Try it out on your family and friends until it becomes easy to do. A closed question goes like this: Do you like vegetables? The person can only really say yes or no. An open question goes like this: Tell me something about how vegetables fit into your diet? Then the person can start talking about vegetables much more — and you will get a lot more information.
A good time to do an in-depth interview is when the subject matter is sensitive; for example, gathering data from women regarding their feelings about sexuality and family planning, or if the woman has had an abortion. This is a useful technique when you need to explore an individual’s experiences, beliefs and attitudes in greater detail.
12.6.3 Key informants
Key informants are people who have first-hand knowledge about the community. They include community leaders, cultural leaders, religious leaders, and other people with lots of experience in the community. These community experts, with their particular knowledge and understanding, represent the views of an important sector of the community. They can provide you with detailed information about the community, its health beliefs, cultural practices, and other relevant information that might help you in your work. How do you feel about talking to leaders and people with lots of experience? Do you ask them different sorts of questions from those you ask of other people? Although beliefs and attitudes apply to key informants too, you also have a chance to find out some answers to questions about ‘the bigger picture’ of your community when people are public figures.
12.6.4 Focus group discussions
Focus g roup d iscussion s are group discussions where around 6 to 12 people meet to discuss health problems in detail. The discussion is led by a person known as a ‘facilitator’. Box 12.6 describes the steps to use if you want to conduct a focus group discussion.
Box 12.6 Conducting a focus group discussion
- Select 6–12 participants for your focus group discussion. For the discussion of some sensitive issues, it might be necessary to lead one focus group of men only (Figure 12.7), and another of women only. For other issues, a mixed group could lead to interesting and informative discussions.
- Prepare a focus group discussion guide. This is a set of questions which are used to facilitate the discussion. While the discussion is going, you can also generate more questions to ask the participants.
- There should be one person who facilitates the discussion, and another person who takes notes during the discussion. If possible, it is also useful to record the discussion using a tape recorder, so that you can listen and analyse it later.
You may find it useful to use focus group discussions in the following situations:
- When group interaction might produce better quality data. Interaction between the participants can stimulate richer responses, and allow new and valuable issues to emerge.
- Where resources and time are limited. Focus groups can be done more quickly, and are generally less expensive than a series of in-depth interviews.

In this study session, you have learnt four techniques that will help you to conduct needs assessments. You can either select one technique which best fits the aims of your needs assessment, or use a combination of more than one technique to build a more complete picture of the issues you need more information about.
Spend a few moments thinking about these four techniques. Do you feel more at home with one than another? Do you think it might be best to use more than one method with a particular health education issue?
You do not have to use all of these techniques all the time. Some work better in some situations. But it is worth practising, so that if and when you need a particular technique you have it at your finger tips.
Summary of Study Session 12
In Study Session 12, you have learned that:
- Planning is the process of making thoughtful and systematic decisions about what needs to be done, how it has to be done, by whom, and with what resources.
- Planning health education activities has several advantages. It enables you to prioritise problems, use your resources efficiently, avoid duplication of activities, and develop the most effective methods to solve community health problems.
- Planning should be based on your local situation, and take into account all the interests and needs of the community.
- A needs assessment is the usual starting point for the health planning process. There are a variety of techniques you can use for this, including observation, interviews and focus group discussions.
- No matter what techniques are used to conduct your health and resource needs assessments, the basic concept is to find out more about health problems in your community, and gather information about their underlying causes.
Planning is covered in more depth in Study Session 13.
Self-Assessment Questions (SAQs) for Study Session 12
Now that you have completed this study session, you can assess how well you have achieved its Learning Outcomes by answering the following questions. Write your answers in your Study Diary and discuss them with your Tutor at the next Study Support Meeting. You can check your answers with the Notes on the Self-Assessment Questions at the end of this Module.
SAQ 12.1 (tests Learning Outcome 12.1)
What do you think are the most important elements of:
- a. Health planning?
- b. Health needs assessment?
- a. Planning involves creative thinking. It is the process of making decisions about what needs to be done, when it will be done, where it will be done, who will do it, and with what resources. Planning is central to health education and health promotion activities.
- b. Needs assessment is the process of identifying and understanding the health problems in your community, and their possible causes. This is used to analyse problems and set priorities for intervention.
SAQ 12.2 (tests Learning Outcomes 12.1, 12.2 and 12.3)
Which of the following statements about planning health education activities are false ? In each case, explain what is incorrect.
A Planning should be rigid.
B Planning will create duplication of effort and activities.
C Planning should be based on the local situation.
D It is not important to consider the interests of local people when planning health education activities.
E We should not worry about the availability of resources when we plan our health education activities.
A is false because planning is not rigid. You can adjust or modify your plan at any time.
B is false, planning helps you avoid duplication of activities.
C is true because the local situation is the foundation for all planning. A plan which is not based on local facts cannot be a good plan.
D is false because engagement with the local community in health education activity is one of the core principles of planning. The interest and the needs of the community should be kept at the centre of planning.
E is false because a plan cannot be executed without sufficient resources. Resources are one of the important things that you should consider while planning health education activities.
SAQ 12.3 (tests Learning Outcome 12.4)
Below are the steps you need to go through when planning your health education activities, but they are not in the correct order. Match the steps to the numbers 1 to 6 in the order you should do them.
Needs assessment
Problem identification and prioritisation
Setting goals and objectives
Develop your strategy
Implementation
Monitoring and evaluation
Using the following two lists, match each numbered item with the correct letter.
SAQ 12.4 (tests Learning Outcomes 12.5 and 12.6)
Suppose you are asked to develop a health education plan for the community in which you are working. What are the three categories of needs assessment? What techniques might you use to conduct a health needs assessment?
Categories of needs assessment include health needs assessment, educational needs assessment, and resource needs assessment. In addition, information related to community resources and demographic characteristics should be collected during needs assessment.
Techniques of needs assessment include observation, in-depth interviews, key informant interviews and focus group discussions.
SAQ 12.5 (tests Learning Outcome 12.5)
Derartu has conducted a health needs assessment to develop her health education activity plan. She has assessed the following needs. Which category of need would you put each of these into?
- a. Lack of knowledge about the benefits of latrine use.
- b. Lack of skill in using insecticide-treated bed nets.
- c. Having a negative attitude towards condom use.
- d. Condoms are not available in the village.
- e. Belief that malaria is caused by drinking dirty water.
- a. Educational
- b. Educational
- c. Educational
- d. Resources
- e. Educational.
Read Case Study 12.1 about Ms Tigist again, to see how her needs assessment covered a range of issues.

SAQ 12.6 (tests Learning Outcome 12.6)
Match the correct descriptions with each of the needs assessment techniques.
Uses a checklist
Observation
Used to explore individual beliefs
In-depth interview
Used when the subject is not sensitive
Focus group discussion
Interviews with religious and other community leaders
Key informant
a. Key informant
b. In-depth interview
c. Observation
d. Focus group discussion
Except for third party materials and/or otherwise stated (see terms and conditions ) the content in OpenLearn is released for use under the terms of the Creative Commons Attribution-NonCommercial-Sharealike 2.0 licence . In short this allows you to use the content throughout the world without payment for non-commercial purposes in accordance with the Creative Commons non commercial sharealike licence. Please read this licence in full along with OpenLearn terms and conditions before making use of the content.
When using the content you must attribute us (The Open University) (the OU) and any identified author in accordance with the terms of the Creative Commons Licence.
The Acknowledgements section is used to list, amongst other things, third party (Proprietary), licensed content which is not subject to Creative Commons licensing. Proprietary content must be used (retained) intact and in context to the content at all times. The Acknowledgements section is also used to bring to your attention any other Special Restrictions which may apply to the content. For example there may be times when the Creative Commons Non-Commercial Sharealike licence does not apply to any of the content even if owned by us (the OU). In these stances, unless stated otherwise, the content may be used for personal and non-commercial use. We have also identified as Proprietary other material included in the content which is not subject to Creative Commons Licence. These are: OU logos, trading names and may extend to certain photographic and video images and sound recordings and any other material as may be brought to your attention.
Unauthorised use of any of the content may constitute a breach of the terms and conditions and/or intellectual property laws.
We reserve the right to alter, amend or bring to an end any terms and conditions provided here without notice.
All rights falling outside the terms of the Creative Commons licence are retained or controlled by The Open University.
Head of Intellectual Property, The Open University
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- NAM Perspect
- v.2020; 2020

Health Literacy and Health Education in Schools: Collaboration for Action
M. elaine auld.
Society for Public Health Education
Marin P. Allen
National Institutes of Health (ret.)
Cicily Hampton
University of North Carolina at Charlotte
J. Henry Montes
American Public Health Association
Cherylee Sherry
Minnesota Department of Health
Angela D. Mickalide
American College of Preventive Medicine
Robert A. Logan
U.S. National Library of Medicine and University of Missouri-Columbia
Wilma Alvarado-Little
New York State Department of Health
July 20, 2020
Introduction
This NAM Perspectives paper provides an overview of health education in schools and challenges encountered in enacting evidence-based health education; timely policy-related opportunities for strengthening school health education curricula, including incorporation of essential health literacy concepts and skills; and case studies demonstrating the successful integration of school health education and health literacy in chronic disease management. The authors of this manuscript conclude with a call to action to identify upstream, systems-level changes that will strengthen the integration of both health literacy and school health education to improve the health of future generations. The COVID-19 epidemic [ 10 ] dramatically demonstrates the need for children, as well as adults, to develop new and specific health knowledge and behaviors and calls for increased integration of health education with schools and communities.
Enhancing the education and health of school-age children is a critical issue for the continued well-being of our nation. The 2004 Institute of Medicine (IOM, now the National Academies of Sciences, Engineering, and Medicine [NASEM]) report, Health Literacy: A Prescription to End Confusion [ 27 ] noted the education system as one major pathway for improving health literacy by integrating health knowledge and skills into the existing curricula of kindergarten through 12th grade classes. The NASEM Roundtable on Health Literacy has held multiple workshops and forums to “inform, inspire, and activate a wide variety of stakeholders to support the development, implementation, and sharing of evidence-based health literacy practices and policies” [ 37 ]. This paper strives to present current evidence and examples of how the collaboration between health education and health literacy disciplines can strengthen K–12 education, promote improved health, and foster dialogue among school officials, public health officials, teachers, parents, students, and other stakeholders.
This discussion also expands on a previous NAM Perspectives paper, which identified commonalities and differences in the fields of health education, health literacy, and health communication and called for collaboration across the disciplines to “engage learners in both formal and informal health educational settings across the life span” [ 1 ]. To improve overall health literacy, i.e., “the capacity of individuals to obtain, process, and understand basic health information and services needed to make appropriate health decisions” [ 42 ], it is important to start with youth, when life-long health habits are first being formed.
Another recent NAM Perspectives paper proposed the expansion of the definition of health literacy to include broader contextual factors, including issues that impact K–12 health education efforts like state rather than federal control of education priorities and administration, and subsequent state- or local-level laws that impact specific school policies and practices [ 39 ]. In addition to addressing individual needs and abilities, socio-ecological factors can impact a student’s health. For example, the Centers for Disease Control and Prevention (CDC) uses a four-level social-ecological model to describe “the complex interplay” of (1) individuals (biological and personal history factors), (2) relationships (close peers, family members), (3) community (settings such as neighborhoods, schools, after-school locations), and (4) societal factors (cultural norms, policies related to health and education, or inequalities between groups in societies) that put one at risk or prevent him/her from experiencing negative health outcomes [ 11 ]. Also worth examining are protective factors that help children and adolescents avoid behaviors that place them at risk for adverse health and educational outcomes (e.g., self-efficacy, self-esteem, parental support, adult mentors, and youth programs) [ 21 , 59 ].
Recognizing the influence of this larger social context on learning and health can help catalyze both individual and community-based solutions. For example, students with chronic illnesses such as asthma, which can affect their school attendance, can be educated about the impact of air quality or housing (e.g., mold, mites) in exacerbating their condition. Students in varied locations and at a range of ages continue, often with the guidance of adults, to take health-related social action. Various local, national, and international examples illustrate high schoolers taking social action related to health issues such as tobacco, gun safety, and climate change [ 18 , 21 , 57 ].
By employing a broad approach to K–12 education (i.e., using combined principles of health education and health literacy), the authors of this manuscript foresee a template for the integration of skills and abilities needed by both school health professionals and children and parents to increase health knowledge for a lifetime of improved health [ 1 , 29 , 31 ].
The right measurements to evaluate success and areas that need improvement must be clearly identified because in all matters related to health education and health literacy, it is vital to document the linkages between informed decisions and actions. Often, individuals are presumed to be making informed decisions when actually broader socio-ecological factors are predominant behavioral influences (e.g., an individual who is overweight but has never learned about food label-ling and lives in a community where there are no safe places to be physically active).
Health Education in Schools
Standardized and broadly adopted strategies for how health education is implemented in schools—and by whom and on what schedule—is a continuing challenge. Although the principles of health literacy are inherently important to any instruction in schools and in community settings, the most effective way to incorporate those principles in existing and differing systems becomes a key to successful health education for children and young people.
The concept of incorporating health education into the formal education system dates to the Renaissance. However, it did not emerge in the United States until several centuries later [ 26 ]. In the early 19th century, Horace Mann advocated for school-based health instruction, while William Alcott also underscored the contributions of health services and the school environment to children’s health and well-being [ 17 ]. Public health pioneer Lemuel Shattuck wrote in 1850 that “every child should be taught early in life, that to preserve his own life and his own health and the lives of others, is one of the most important and abiding duties” [ 43 ]. During this same time, Harvard University and other higher education institutions with teacher preparation programs began including hygiene (health) education in their curricula.
Despite such early historical recognition, in the mid-1960s, the School Health Education Study documented serious disarray in the organization and administration of school health education programs [ 45 ]. A renewed call to action, several decades later, introduced the concepts of comprehensive school health programs and school health education [ 26 ].
From 1998 through 2014, the CDC and other organizations began using the term “coordinated school health programs” to encompass eight components affecting children’s health in schools, including nutrition, health services, and health instruction. Unfortunately, the term was not broadly embraced by the educational sector, and in 2014, CDC and ASCD (formerly the Association for Supervision and Curriculum Development) unveiled the Whole School, Whole Community, Whole Child (WSCC) framework [ 36 ]. This framework has ten components, including health education, which aims to ensure that each student is healthy, safe, engaged, supported, and challenged. Among the foundational tenets of the framework is ensuring that every student enters school healthy and, while there, learns about and practices a healthy lifestyle.
At its core, health education is defined as “any combination of planned learning experiences using evidence based practices and/or sound theories that provide the opportunity to acquire knowledge, attitudes, and skills needed to adopt and maintain healthy behaviors” [ 3 ]. Included are a variety of physical, social, emotional, and other components focused on reducing health-risk behaviors and promoting healthy decision making. Health education curricula emphasize a skills-based approach to help students practice and advocate for their health needs, as well as the needs of their families and their communities. These skills help children and adolescents find and evaluate health information needed for making informed health decisions and ultimately provide the foundation of how to advocate for their own well-being throughout their lives.
In the last 40 years, many studies have documented the relationship between student health and academic outcomes [ 29 , 40 , 41 ]. Health-related problems can diminish a student’s motivation and ability to learn [ 4 ]. Complications with vision, hearing, asthma, occurrences of teen pregnancy, aggression and violence, lack of physical activity, and low cognitive and emotional ability can reduce academic success [ 4 ].
To date, there have been no long-term sequential studies of the impact of K–12 health education curricula on health literacy or health outcomes. However, research shows that students who participate in health education curricula in combination with other interventions as part of the coordinated school health model (i.e., physical activity, improved nutrition, and/or family engagement) have reduced rates of obesity and/or improved health-promoting behaviors [ 25 , 30 , 34 ]. In addition, school health education has been shown to prevent tobacco and alcohol use and prevent dating aggression and violence. Teaching social and emotional skills improves academic behaviors of students, increases motivation to do well in school, enhances performance on achievement tests and grades, and improves high school graduation rates.
As with other content areas, it is up to the state and/or local government to determine what should be taught, under the 10th Amendment to the US Constitution [ 48 ]. However, both public and private organizations have produced seminal documents to help guide states and local governments in selecting health education curricula. First published in 1995 and updated in 2004, the National Health Education Standards (NHES) framework comprises eight health education foundations for what students in kindergarten through 12th grade should know and be able to do to promote personal, family, and community health (see Table 1 ) [ 12 ]. The NHES framework serves as a reference for school administrators, teachers, and others addressing health literacy in developing or selecting curricula, allotting instructional resources, and assessing student achievement and progress. The NHES framework contains written expectations for what students should know and be able to do by grades 2, 5, 8, and 12 to promote personal, family, and community health.
SOURCE: Centers for Disease Control and Prevention. 2020. National Health Education Standards. Available at: National Health Education Standards Website. https://www.cdc.gov/healthyschools/sher/standards/index.htm (accessed June 19, 2020).
The Coordinated Approach to Child Health (CATCH) model, which was first developed in the late 1980s with funds by the National Heart, Lung, and Blood Institute, serves to implement the NHES framework and was the largest school-based health promotion study ever conducted in the United States. CATCH has 25 years of continuous research and development of its programs [ 24 ] and aligns with the WSCC framework. Individualized programs like the CATCH model develop programming based on the NHES framework at the local level, so that local control still exists, but the mix and depth of topics can vary based on need and composition of the community.
Based on reviews of effective programs and curricula and experts in the field of health education, CDC recommends that today’s state-of-the-art health education curricula emphasize four core elements: “Teaching functional health information (essential knowledge); shaping personal values and beliefs that support healthy behaviors; shaping group norms that value a healthy lifestyle; and developing the essential health skills necessary to adopt, practice, and maintain health enhancing behavior” [ 13 ]. In addition to the 15 characteristics presented in Box 1 , the CDC website has more detailed explanations and examples of how the statements could be put into practice in the classroom. For example, a curriculum that “builds personal competence, social competence, and self-efficacy by addressing skills” would be expected to guide students through a series of developmental steps that discuss the importance of the skill, its relevance, and relationship to other learned skills; present steps for developing the skill; model the skill; practice and rehearse the skill using real-life scenarios; and provide feedback and reinforcement.
Characteristics of an Effective Health Education Curriculum
- 1. Focuses on clear health goals and related behavioral outcomes.
- 2. Is research-based and theory-driven.
- 3. Addresses individual values, attitudes, and beliefs.
- 4. Addresses individual and group norms that support health-enhancing behaviors.
- 5. Focuses on reinforcing protective factors and increasing perceptions of personal risk and harmfulness of engaging in specific unhealthy practices and behaviors.
- 6. Addresses social pressures and influences.
- 7. Builds personal competence, social competence, and self-efficacy by addressing skills.
- 8. Provides functional health knowledge that is basic, accurate, and directly contributes to health-promoting decisions and behaviors.
- 9. Uses strategies designed to personalize information and engage students.
- 10. Provides age-appropriate and developmentally appropriate information, learning strategies, teaching methods, and materials.
- 11. Incorporates learning strategies, teaching methods, and materials that are culturally inclusive.
- 12. Provides adequate time for instruction and learning.
- 13. Provides opportunities to reinforce skills and positive health behaviors.
- 14. Provides opportunities to make positive connections with influential others.
- 15. Includes teacher information and plans for professional development and training that enhance effectiveness of instruction and student learning.
SOURCE: Centers for Disease Control and Prevention. 2020. Characteristics of an Effective Health Education Curriculum. Available at: https://www.cdc.gov/healthyschools/sher/characteristics/index.htm (accessed June 19, 2020.)
In addition, CDC has developed a Health Education Curriculum Analysis Tool [ 14 ] to help schools conduct an analysis of health education curricula based on the NHES framework and the Characteristics of an Effective Health Education Curriculum.
Despite CDC’s extensive efforts during the past 40 years to help schools implement effective school health education and other components of the broader school health program, the integration of health education into schools has continued to fall short in most US states and cities. According to the CDC’s 2016 School Health Profiles report, the percentage of schools that required any health education instruction for students in any of grades 6 through 12 declined. For example, 8 in 10 US school districts only required teaching about violence prevention in elementary schools and violence prevention plus tobacco use prevention in middle schools, while instruction in only seven health topics was required in most high schools [ 6 ].
Although 8 of every 10 districts required schools to follow either national, state, or district health education standards, just over a third assessed attainment of health standards at the elementary level while only half did so at the middle and high school levels [ 6 ]. No Child Left Behind legislation, enacted in 2002, emphasized testing of core subjects, such as reading, science, and math, which resulted in marginalization of other subjects, including health education [ 22 , 31 ]. Academic subjects that are not considered “core” are at risk of being eliminated as public school principals and administrators struggle to meet adequate yearly progress for core subjects, now required to maintain federal funding.
In addition to the quality and quantity of health education taught in schools, there are numerous problems related to those considered qualified to provide instruction [ 5 , 7 ]. Many school and university administrators lack an understanding of the distinction between health education and physical education (PE) [ 9 , 16 , 19 ] and consider PE teachers to be qualified to teach health education. Yet the two disciplines differ regarding national standards, student learning outcomes, instructional content and methods, and student assessment [ 5 ]. Kolbe notes that making gains in school health education will require more interdisciplinary collaboration in higher education (e.g., those training the public health workforce, the education workforce, school nurses, pediatricians) [ 29 ]. Yet faculty who train various school health professionals usually work within one university college, focus on one school health component, and affiliate with one national professional organization. In addition, Kolbe notes that health education teachers in today’s workforce often lack support and resources for in-service professional development.
Promising Opportunities for Strengthening School Health Education
Comprehensive health education can increase health literacy, which has been estimated to cost the nation $1.6 to $3.6 trillion dollars annually [ 54 ]. The National Action Plan to Improve Health Literacy by the US Department of Health and Human Services (HHS) includes the goal to “Incorporate accurate, standards-based, and developmentally appropriate health and science information and curricula in childcare and education through the university level” [ 49 ].
HHS’s Healthy People Framework presents another significant opportunity for tracking health in education as well as health literacy. The Healthy People initiative launched officially in 1979 with the publication of Healthy People: The Surgeon General’s Report on Health Promotion and Disease Prevention [ 50 ]. This national effort establishes 10-year goals and objectives to improve the health and well-being of people in the United States. Since its inception, Healthy People has undertaken extensive efforts to collect data, assess progress, and engage multi-stakeholder feedback to set objectives for the next ten years. The Healthy People 2020 objectives were self-described as having “input from public health and prevention experts, a wide range of federal, state, and local government officials, a consortium of more than 2,000 organizations, and perhaps most importantly, the public” [ 51 ]. In addition to other childhood and adolescent objectives (e.g., nutrition, physical activity, vaccinations), Healthy People 2020 specified social determinants as a major topic for the first time. A leading health indicator for social determinants was “students graduating from high school within 4 years of starting 9th grade (AH-5.1)” [ 52 ]. The Secretary’s Advisory Committee report on the Healthy People 2030 objectives includes the goal to “eliminate health disparities, achieve health equity, and attain health literacy to improve the health and well-being of all” [ 53 ]. The national objectives are expected to be released in summer 2020 and will help catalyze “leadership, key constituents, and the public across multiple sectors to take action and design policies that improve the health and well-being of all” [ 53 ].
In terms of supports in federal legislation, the Every Student Succeeds Act (ESSA) of 2015 recognized health education as a distinct discipline for the first time and designated it as a “well-rounded” education subject [ 2 , 22 ]. According to Department of Education guidelines, each state must submit a plan that includes four academic indicators that include proficiency in math, English, and English-language proficiency. High schools also must use their graduation rates as their fourth indicator, while elementary and middle schools may use another academic indicator. In addition, states must specify at least one nonacademic indicator to measure school quality or school success, such as health education. Under the law, federal funding also is available for in-service instruction for teachers in well-rounded education subjects such as health education. These two items open additional pathways for both identifying existing or added programs and having the capacity to collect data.
While several states have chosen access to physical education, physical fitness, or school climate as their nonacademic indicators of school success, the majority (36 states and the District of Columbia) have elected to use chronic absenteeism [ 2 ]. Given the underlying causal connection between student health and chronic absenteeism, absenteeism as an indicator represents a significant opportunity to raise awareness of chronic health conditions or other issues (e.g., student social/emotional concerns around bullying, school safety) that contribute to absenteeism. It also represents a significant opportunity for schools to work with stakeholders to prevent and manage such health conditions through school health education and other WSCC strategies to improve school health. Educators are more likely to support comprehensive health education if they are made aware of its immediate benefits related to student learning (e.g., less disruptive behavior, improved attention) and maintaining safe social and emotional school climates [ 31 ].
In an assessment of how states are addressing WSCC, Child Trends reported that health education is either encouraged or required for all grades in all states’ laws, with nutrition (40 states) and personal health (44 states) as the most prominent topics [ 15 ]. However, the depth and breadth of such instruction in schools is not known, nor if health education is being taught by qualified teachers. In 25 states, laws address or otherwise incorporate the NHES as part of the state health education curriculum.
The authors’ review of state 2017–2018 ESSA plans, analyzed by the organization Cairn, showed nine states that have specifically identified health education as one of its required well-rounded subjects (Florida, Georgia, Indiana, Louisiana, Maine, Maryland, Nevada, North Dakota, and Tennessee) [ 8 ]. Cairn recommends that most states include health education and physical education in state accountability systems, school report card indicators, school improvement plans, professional development plans, needs assessment tools, and/or prioritized funding under Title IV, Part A.
In 2019, representatives of the National Committee on the Future of School Health Education, sponsored by the Society for Public Health Education (SOPHE) and the American School Health Association (ASHA), published a dozen recommendations for strengthening school health education [ 5 , 31 , 55 ]. The recommendations addressed issues such as developing and adopting standardized measures of health literacy in children and including them in state accountability systems; changing policies, practices, and systems for quality school health education (e.g., establishing Director of School Health Education positions in all state and territory education agencies tasked with championing health education best practices, and holding schools accountable for improving student health and well-being); and strengthening certification, professional preparation, and ongoing professional development in health education for teachers at both the elementary and secondary levels. Recommendations also call for stronger alignment and coordination between the public health and education sectors. The committee is now moving ahead on prioritizing the recommendations and developing action steps to address them.
Integrating Youth Health Education and Health Literacy: Success Stories
Minnesota statewide model: integrating school health education and health literacy through broad partnership.
The Roundtable on Health Literacy held a workshop on health literacy and public health in 2014, with examples of how state health departments are addressing health literacy in their states [ 28 ]. One recent example of a strong collaboration between K–12 education and public health agencies is the Statewide Health Improvement Partnership (SHIP) within the Minnesota Department of Health’s Office of Statewide Health Initiative [ 35 ].
SHIP was created by a landmark 2008 Minnesota health reform law. The law was intended to improve the health of Minnesotans by reducing the risk factors that lead to chronic disease. The program funds grantees in all of the state’s 87 counties and 10 tribal nations to support the creation of locally driven policies, systems, and environmental changes to increase health equity, improve access to healthy foods, provide opportunities for physical activity, and ensure a tobacco-free environment [ 35 ]. Local public health agencies collaborate with partners including schools, childcare settings, workplaces, multiunit housing facilities, and health care centers through SHIP.
SHIP models the integration of (1) law, (2) policy, (3) goal setting, and (4) resource building and forging some 2,000 collaborative partnerships and measuring outcomes. SHIP sets a helpful example for others attempting to create synergies across the intersections of state government, health education, local communities, and private organizations. The principles of health literacy are within these collaborations.
Grantees throughout the state have received technical assistance and training to improve school nutrition and physical activity strategies (see Figure 1 ). SHIP grantees and their local school partner sites set goals and adopt best practices for physical education and physical activity inside and outside the classroom. They improve access to healthy food environments through locally sourced produce, lunchrooms with healthier food options, and school-based agriculture. In 2017, SHIP grantees partnered with 995 local schools and accounted for 622 policy, systems, and environmental changes.

SOURCE: Minnesota Department of Health, Office of Statewide Health Improvement Initiatives. 2012. Statewide Health Improvement Partnership Evaluation Data, Minnesota Department of Health Legislative Report 2017. Reported by SHIP grantees using the REDCap system. This data represents the activities and reach of partner sites active between September 24, 2016, and August 25, 2017.
Minnesota has also undertaken a broad approach to health literacy by educating stakeholders and decision makers (i.e., administrators, food service and other staff, students, community partners, and parents) about various health-related social and environmental issues to reduce students’ chronic disease risks.
SHIP grantees assist in either convening or organizing an established school health/wellness council that is required by USDA for each local education agency participating in the National School Lunch Program and/or School Breakfast Program [ 46 , 47 ]. A local school wellness policy is required to address the problem of childhood obesity by focusing on nutrition and physical activity. SHIP also requires schools to complete an assessment that aligns with the WSCC model and provides annual updates. Once the assessment is completed by a broad representation of stakeholders, SHIP grantees assist schools in prioritizing and working toward annual goals. The goal setting and assessment and goal-setting cycle is continuous.
The Bigger Picture: A Case Study of Community Integration of Health Education and Health Literacy
Improving the health literacy of young people not only influences their personal health behaviors but also can influence the health actions of their peers, their families, and their communities. According to the SEARCH for Diabetes in Youth study funded by the CDC and the National Institutes of Health’s National Institute of Diabetes, Digestive, and Kidney Diseases, from 2002 to 2012, the national rate of new diagnosed cases of Type 2 diabetes increased 4.8% [ 32 ]. Among youth ages 10–19, the rate of new diagnosed cases of Type 2 diabetes rose most sharply in Native Americans (8.9%) (although not generalizable to all Native American youth because of small sample size), compared to Asian Americans/Pacific Islanders (8.5%), non-Hispanic blacks (6.3%), Hispanics (3.1%), and non-Hispanic whites (0.6%).
Since 2011, Dean Schillinger, Professor of Medicine in Residence at the University of California San Francisco and Chief of the Diabetes Prevention and Control Program for the California Department of Public Health, has led a capacity-building effort to address Type 2 diabetes [ 23 , 28 , 44 ].
This initiative called The Bigger Picture (TBP) has mobilized collaborators to create resources by and for young adults focused on forestalling and, hopefully, reversing the distressing increase in pediatric Type 2 diabetes by exposing the environmental and social conditions that lead to its spread. Type 2 diabetes is increasingly affecting young people of color, and TBP is specifically developed by and directed to them.
TBP seeks to increase the number of well-informed young people who can participate in determining their own lifelong health behaviors and influencing those of their friends, families, communities, and their own children. The project aims to create a movement that changes the conversation about diabetes from blame- and-shame to the social drivers of the epidemic [ 23 ].
TPB is described by the team that created it as a “counter-marketing campaign using youth-created, spoken-word public services announcements to re-frame the epidemic as a socio-environmental phenomenon requiring communal action, civic engagement, and norm change” [ 44 ]. The research team provides a description of questionnaire responses to nine of the public service announcements in the context of campaign messages, film genre and accompanying youth value, participant understanding of film’s public health message, and the participant’s expression of the public health message. The investigators also correlate the responses with dimensions of health literacy such as conceptual foundations, functional health literacy, interactive health literacy, critical skills, and civic orientation.
One of the campaign partners, Youth Speaks, has created a toolkit to equip and empower students and communities to become change agents in their respective environments, raising their voices and joining the conversation about combating the spread of Type 2 diabetes [ 56 ].
In a discussion of qualitative evaluations of TBP and what low-income youth “see,” Schillinger et al. note that “TBP model is unique in how it nurtures and supports the talent, authenticity, and creativity of new health messengers: youth whose lived experience can be expressed in powerful ways” [ 44 ].
COVID-19: Health Crisis Affecting Children and their Families and a Need for Health Education and Health Literacy in K-12
In a recent op-ed, Rebecca Winthrop, co-director of the Center for Universal Education and Senior Fellow of Global and Economic Development of the Brookings Institution asked, “COVID-19 is a health crisis. So why is health education missing from school work?” [ 58 ] She notes that “helping sustain education amid crises in over 20 countries, I’ve learned that one of the first things you do, after finding creative ways to continue educational activities, is to incorporate life-saving health and safety messages.” Her call is impassioned for age-appropriate, immediately available resources on COVID-19 that can be easily incorporated into distance lesson plans for both children and families. Many organizations, such as Child Trends, are curating collections of such resources. Framing these materials using principles of health literacy and incorporating them into health education messages and resources may be an ideal model for incorporating new pathways for public health K–12 learning.
Call to Action for Collaboration
Strategic and dedicated efforts are needed to bridge health education and health literacy. These efforts would foster the expertise to provide students with the information needed to access and assess useful health information, and to develop the necessary skills for an emerging understanding of health.
Starting with students in school settings, learning to be health literate helps overcome the increased incidence of chronic diseases such as Type 2 diabetes, and imbues a sense of self-efficacy and empowerment through health education. It also sets the course for lifelong habits, skills, and decision making, which can also influence community health.
Pursuing institutional changes to reduce disparities and improve the health of future generations will require significant collaboration and quality improvement among leaders within health education and health literacy. Recommendations provided in previous reports such as IOM’s 1997 report, Schools and Health: Our Nation’s Investment [ 26 ]; the 2004 IOM report on Health Literacy [ 27 ]; and the 2010 National Action Plan to Improve Health Literacy [ 49 ] should be revisited. More recently, a November 2019 Health Literacy Roundtable Workshop (1) explored the necessity of developing health literacy skills in youth, (2) examined the research on developmentally appropriate health literacy milestones and transitions and measuring health literacy in youth, (3) described programs and policies that represent best practices for developing health literacy skills in youth, and (4) explored potential collaborations across disciplines for developing health literacy skills in youth [ 38 ]. With its resulting report, the information provided in the workshop should provide additional insights into collaborations needed to reduce institutional barriers to youth health literacy and empowerment.
At the national level, representatives from public sector health and education levels (e.g., HHS’s Office of Disease Prevention and Health Promotion, CDC, Department of Education) can collaborate with school-based nongovernmental organizations (e.g., SOPHE, ASCD, ASHA, National Association of State Boards of Education, School Superintendents Association, Council of Chief State School Officers, Society of State Leaders of Health and Physical Education) to provide data and lead reform efforts. Leaders of higher education (e.g., Association of American Colleges and Universities, Association of Schools and Programs of Public Health) can join with philanthropies and educational scholars to pursue curricular reforms and needed research to further health education and health literacy as an integral component of higher education.
Among the approaches needed are (1) careful incorporation of key principles of leadership within systems; (2) the training and evaluation of professionals; (3) finding and sharing replicable, effective examples of constructive efforts; and (4) including young people in the development of information and materials to ensure their accessibility, appeal, and utility. Uniting the wisdom, passion, commitment, and vision of the leaders in health literacy and health education, we can forge a path to a healthier generation.
Acknowledgments
The authors would like to express our gratitude to Melissa French and Alexis Wojtowicz for their support in the development of this paper.
Funding Statement
The views expressed in this paper are those of the authors and not necessarily of the authors’ organizations, the National Academy of Medicine (NAM), or the National Academies of Sciences, Engineering, and Medicine (the National Academies). The paper is intended to help inform and stimulate discussion. It is not a report of the NAM or the National Academies.
Conflict-of-Interest Disclosures: Wilma Alvarado-Little has no relevant financial or non-financial relationships to disclose. She contributed to this article based on her experience in the field of health literacy and cultural competency and the opinions and conclusions of the article do not represent the official position of the New York State Department of Health. Cherylee Sherry discloses that she works for the Minnesota Department of Health in the Office of Statewide Health Improvement Initiatives which oversees the Statewide Health Improvement Partnership Program funded by the State of Minnesota.
Contributor Information
M. Elaine Auld, Society for Public Health Education.
Marin P. Allen, National Institutes of Health (ret.)
Cicily Hampton, University of North Carolina at Charlotte.
J. Henry Montes, American Public Health Association.
Cherylee Sherry, Minnesota Department of Health.
Angela D. Mickalide, American College of Preventive Medicine.
Robert A. Logan, U.S. National Library of Medicine and University of Missouri-Columbia.
Wilma Alvarado-Little, New York State Department of Health.
Kim Parson, KPCG, LLC.
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Strategies for Effective Community Engagement: Critical Service-Learning Seminar
Come join us in a rich community engagement talk with Dr. Tyler Derreth, an assistant professor in the Department of Health, Behavior and Society and an associate Director of SOURCE. Dr. Derreth will share with BSPH community tools and resources on how public health professionals can engage in community by building authentic relationships, learning through service, redistributing power, and promoting social change during their time here at Hopkins and beyond.
Lunch included.
Part of Public Health Week 2024, hosted by the Anna Baetjer Society for Public Health Practice and sponsored by the Johns Hopkins Bloomberg School of Public Health Student Assembly.
Dr. Tyler Derreth (SOURCE)
Tyler Derreth, PhD is an assistant teaching professor in the Department of Health, Behavior, and Society. He is also the Associate Director of SOURCE, the community engagement and service-learning center at Johns Hopkins. His work concentrates on urban community-university partnerships that work toward social change. He frequently engages in educational practices to advance community goals around various social justice issues. The majority of his work centers on collaboration with Baltimore communities.
Related Content

Filters and Digital Health Program Reduced Participants' Arsenic Levels by Nearly Half in American Indian Households Relying on Well Water

Student Spotlight: Glendedora Dolce

A Seat at Every Table

Study Estimates Nearly 70 Percent of Children Under Six in Chicago May Be Exposed to Lead-Contaminated Tap Water

Wendy Bennett Empowers Women and Families Through Research

The Essential Do’s and Don’ts of Successful Oral Health Programs

In this blog, we’ll explore some essentials of establishing a Community Oral Health Program, some “Do” and “Do not.” Creating a robust community oral health program is more than a goal; it’s a commitment to the well-being of a community. Community Oral Health Program, commonly known as COHP, is a public health initiative aimed at improving oral health of a specific community. It incorporates the principles of health education and promotion and extends beyond oral hygiene education. One of main goal of such programs is focusing on collective well-being and quality of life.
Postgraduate Degree in Community Oral Health
Like what you’re learning? Consider enrolling in the Herman Ostrow School of Dentistry of USC’s online, competency-based certificate or master’s program in Community Oral Health .
Now, why is this topic crucial? The oral health of a community directly impacts its overall health. There are well established research results indication the link between oral health and general health. A well-structured COHP can prevent oral diseases, enhance overall health outcomes, and foster a sense of well-being within the community. Let’s unravel the nuances of this initiative and address the” dos “and “don’ts” that can shape its success.
Understanding the Do’s
Education Initiatives: Implementing informative sessions and workshops can empower community members with knowledge about oral health practices. By also including graphics in flyers or media outlets helps to illustrate the impact of preventive measures, making the information accessible and clear.
Accessible Oral Health Services: Improving access to oral health care by Establishing clinics and organizing mobile dental units in dental deserts to ensure the community has easier access to oral health services to treat untreated tooth decay and other infections. Accessibility is key to the population your program intends to serve.
Involving stakeholders: COHP needs planning, execution, and evaluation. Involving stake holders in all steps are crucial to the success of the program. The program needs to be useful, feasible ethical and evidence- based.
Sustainability: Ensuring the sustainability of the program by securing funding and ensuring a cadre of well-prepared public health workforce will create positive impacts on the current community, as well as the future of that community.
Steering Clear of the Don’ts
Ignoring Cultural Sensitivities: Avoid cultural insensitivity by tailoring educational materials, consents and programs to align with the community’s cultural norms. Respectful representation that fosters a sense of inclusivity.

Figure 3: Elements of Culture
Neglecting Follow-up and Monitoring: Continuous evaluation and monitoring are crucial. Neglecting these aspects can hinder the program’s effectiveness. Present data-driven graphs depicting the positive impact of monitoring efforts. Plan for continuous evaluation, especially in the implementation phase. This helps to identify unexpected barriers and problems to fine-tune and strengthen the COHP.
The journey of establishing a Community Oral Health Program is both dynamic and rewarding. By embracing the do’s: educational initiatives, accessible services, involving stakeholders and creating sustainability and avoiding the don’ts, like cultural insensitivity and neglecting monitoring, we pave the way for healthier, happier communities.
Take-home Messages for Our Community
Empowerment through Education: Education is the cornerstone of a successful program. Empower the community with knowledge to foster long-term oral health practices.
Inclusivity and Continuous Improvement: Prioritize cultural inclusivity and ongoing evaluation. A program that adapts to the community’s needs is a program that thrives.
Earn an Online Postgraduate Degree in Community Oral Health
Like what you’re learning? Consider enrolling in the Herman Ostrow School of Dentistry of USC’s online, competency-based certificate or master’s program in Community Oral Health .
References:
- American Dental Association. Breaking down barriers to oral health for all Americans: the role of workforce. J Calif Dent Assoc. 2011 Jul;39(7):491-502. PMID: 21905545.
- Buischi YA, Axelsson P, Oliveira LB, Mayer MP, Gjermo P. Effect of two preventive programs on oral health knowledge and habits among Brazilian schoolchildren. Community Dent Oral Epidemiol. 1994;22:41–6
- Centers for Disease Control and Prevention. (2017, May 15). Framework for Program Evaluation – CDC. Centers for Disease Control and Prevention. https://www.cdc.gov/evaluation/framework/index.htm
- Cultural Competence Program for Oral Health Professionals! The Office of Minority Health of the Department of Health and Human Service (HHS).
- Kwan SY, Petersen PE, Pine CM, Borutta A. Health-promoting schools: an opportunity for oral health promotion. Bull World Health Organ 2005 Sep;83(9):677-685.
- Redmond CA, Blinkhorn FA, Kay EJ, Davies RM, Worthington HV, Blinkhorn AS. A cluster randomized controlled trial testing the effectiveness of a school-based dental health education program for adolescents. J Public Health Dent. 1999;59:12–7.
- World Health Organization. Global oral health status report: towards universal health coverage for oral health by 2030. Geneva: World Health Organization, 2022.
- World Health Organization. WHO highlights oral health neglect affecting nearly half of the world’s population. Geneva: World Health Organization, 2022.

Dr. Diba is the Dental Director at a community clinic in Los Angeles, bringing over three years of experience in FQHC settings. She holds a DDS degree from UCLA and completed her AEGD residency at UCLA Westwood. Monica's dedication to community oral health led her to pursue a Master's degree in the field. With a passion for global outreach, she has traveled to over 20 countries, collaborating with organizations like Peace World to provide essential care to underserved populations worldwide.
View all posts

Kristine Parungao is an Associate Professor of Clinical Dentistry., graduated from UCSD with a Biology degree, then pursued her Dental Hygiene passion at USC School of Dentistry and earned her Masters in Community Oral Heath. Parungao also completed a Registered Dental Hygienist in Alternative Practice at the University of the Pacific- Treating Medically Complex in Special Needs Patients at USC. Parungao served as a Director for the Children’s Maintenance Program (CHAMP), a first 5 LA grant-funded project, then went on to serve as Director for the Educational Community Health Outreach (ECHO) project until 2021. Associate Professor Parungao currently teaches courses in the Masters in Community Oral Health and on the clinic floor in the Special Patients Clinic.
Pin It on Pinterest
Program to improve health care for marginalized populations puts Black physicians in racialized communities
Marie Claud Felicien, Director of Primary Health Care Services for Women’s Health in Women’s Hands, on Mar 19. WHIWH provides healthcare services for racialized women in Toronto, and surrounding municipalities. Fred Lum/The Globe and Mail
Marie Claud Felicien immigrated to Canada from St. Lucia as a teenager in 2000. As newcomers not yet covered by public health insurance, her family avoided simple visits to the doctor, because they were forced to pay $60 to $70 out-of-pocket for appointments, Ms. Felicien said.
No one suffered a major health crisis during this time, but worry over incurring medical expenses added to her family’s stress. That experience informed how Ms. Felicien treated her patients when she worked as nurse and now shapes the ethos at Women’s Health in Women’s Hands (WHIWH), a community health centre for racialized women in Toronto , where she serves as director of primary health care services.
“Many people don’t realize that newcomers have to pay out-of-pocket for medical services until they are covered by the Ontario Health Insurance Plan,” Ms. Felicien said.
Like her and her family, a majority of the clients that Ms. Felicien serves at WHIWH are Black women from the Caribbean or Africa, seeking medical care as they navigate the immigration process. Despite that, among its current staff – two nurses, six medical doctors and three nurse practitioners – the clinic only has one Black medical clinician, a nurse.
A majority of the clients that Ms. Felicien serves at WHIWH are Black women from the Caribbean or Africa, seeking medical care as they navigate the immigration process. Fred Lum/The Globe and Mail
Ms. Felicien recognizes that health care systems don’t serve all patients equally, and sees the value of having health practitioners and health care workers reflect and understand the experiences of their patients.
“It’s something we have been trying to solve, so that our patients feel more comfortable with doctors and nurses that look like them and might share their experience,” Ms. Felicien said.
Her clinic is one of six community health centres in the Greater Toronto Area that are part of the Community Health Centre Education Program (CHCE), which places first- and second-year Black medical students at community health centres across Ontario. The program is run by the Black Physicians’ Association of Ontario (BPAO).
There are 75 community health centres across Ontario, each incorporated as a non-profit with a primary focus on improving the health and well-being of populations that face barriers accessing health services, according to the province.
The CHCE’s nine-week education program – now in its second year – immerses Black medical students in one of the six publicly funded community health centres near Toronto that are dedicated to providing health care and other vital services to Black and racialized people experiencing homelessness, newcomers, refugees, low-income individuals and others who need help. The program gives them experience in providing care to racialized communities and allows them to learn about a career path at a community health centre (CHC).
A key part of the program is to raise awareness of the need for Black doctors at CHCs, says Chenai Kadungure, executive director at the BPAO, a not-for-profit that strives to combat racialized health disparities.
According to a 2021 literature review published in the Canadian Journal of Science, Mathematics and Technology Education, Black patients report better experiences and increased satisfaction of care when interacting with Black physicians as opposed to white physicians.
“We want Black medical students to know that there are other avenues to providing medical care and making an impact outside of the popular career paths like being a surgeon or working in a hospital,” says Ms. Kadungure.
Toyemi Opeoluwa-Calebs, a third-year medical student at the University of Toronto, had been looking for ways to be more connected to her community in the city.
“When I heard about the CHCE program, I knew it was the perfect opportunity for me to get to know the people working in the CHC space and to also get to know the community,” says Ms. Opeoluwa-Calebs, who came to Canada from Nigeria as an international student in high school.
Ms. Opeoluwa-Calebs was the first to complete the nine-week summer employment program in 2023.
In 2024, the program will be rolled out across all medical schools in Ontario and will offer five Black medical students a chance to work at one of the CHCs in the Greater Toronto Area. For their participation over the summer, Ms. Kadungure says the students will receive $5,000 each.
“It gives the students a chance to work in the medical field over the summer and gain hands-on experience that they won’t be marked on at school,” she says.
At WHIWH, Ms. Felicien said the CHC provides care to women with low incomes, those new to the country, women with HIV and women without health insurance, with a priority for women from African, Caribbean, Latin American and South Asian communities.
“Without knowing where to turn, many of them do not get medical attention, which can make their needs worse,” Ms. Felicien said.
Report an editorial error
Report a technical issue
Editorial code of conduct
Follow related authors and topics
- Daniel Reale-Chin Follow You must be logged in to follow. Log In Create free account
- Greater Toronto Area Follow You must be logged in to follow. Log In Create free account
- Health care Follow You must be logged in to follow. Log In Create free account
- Health insurance Follow You must be logged in to follow. Log In Create free account
- Insurance Follow You must be logged in to follow. Log In Create free account
- Ontario Health Insurance Plan Follow You must be logged in to follow. Log In Create free account
Authors and topics you follow will be added to your personal news feed in Following .
Interact with The Globe
Study Tracks Shifts in Student Mental Health During College
Dartmouth study followed 200 students all four years, including through the pandemic.

Phone App Uses AI to Detect Depression From Facial Cues
A four-year study by Dartmouth researchers captures the most in-depth data yet on how college students’ self-esteem and mental health fluctuates during their four years in academia, identifying key populations and stressors that the researchers say administrators could target to improve student well-being.
The study also provides among the first real-time accounts of how the coronavirus pandemic affected students’ behavior and mental health. The stress and uncertainty of COVID-19 resulted in long-lasting behavioral changes that persisted as a “new normal” even as the pandemic diminished, including students feeling more stressed, less socially engaged, and sleeping more.
The researchers tracked more than 200 Dartmouth undergraduates in the classes of 2021 and 2022 for all four years of college. Students volunteered to let a specially developed app called StudentLife tap into the sensors that are built into smartphones. The app cataloged their daily physical and social activity, how long they slept, their location and travel, the time they spent on their phone, and how often they listened to music or watched videos. Students also filled out weekly behavioral surveys, and selected students gave post-study interviews.
The study—which is the longest mobile-sensing study ever conducted—is published in the Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies .
The researchers will present it at the Association of Computing Machinery’s UbiComp/ISWC 2024 conference in Melbourne, Australia, in October.
These sorts of tools will have a tremendous impact on projecting forward and developing much more data-driven ways to intervene and respond exactly when students need it most.
The team made their anonymized data set publicly available —including self-reports, surveys, and phone-sensing and brain-imaging data—to help advance research into the mental health of students during their college years.
Andrew Campbell , the paper’s senior author and Dartmouth’s Albert Bradley 1915 Third Century Professor of Computer Science, says that the study’s extensive data reinforces the importance of college and university administrators across the country being more attuned to how and when students’ mental well-being changes during the school year.
“For the first time, we’ve produced granular data about the ebb and flow of student mental health. It’s incredibly dynamic—there’s nothing that’s steady state through the term, let alone through the year,” he says. “These sorts of tools will have a tremendous impact on projecting forward and developing much more data-driven ways to intervene and respond exactly when students need it most.”
First-year and female students are especially at risk for high anxiety and low self-esteem, the study finds. Among first-year students, self-esteem dropped to its lowest point in the first weeks of their transition from high school to college but rose steadily every semester until it was about 10% higher by graduation.
“We can see that students came out of high school with a certain level of self-esteem that dropped off to the lowest point of the four years. Some said they started to experience ‘imposter syndrome’ from being around other high-performing students,” Campbell says. “As the years progress, though, we can draw a straight line from low to high as their self-esteem improves. I think we would see a similar trend class over class. To me, that’s a very positive thing.”
Female students—who made up 60% of study participants—experienced on average 5% greater stress levels and 10% lower self-esteem than male students. More significantly, the data show that female students tended to be less active, with male students walking 37% more often.
Sophomores were 40% more socially active compared to their first year, the researchers report. But these students also reported feeling 13% more stressed during their second year than during their first year as their workload increased, they felt pressure to socialize, or as first-year social groups dispersed.
One student in a sorority recalled that having pre-arranged activities “kind of adds stress as I feel like I should be having fun because everyone tells me that it is fun.” Another student noted that after the first year, “students have more access to the whole campus and that is when you start feeling excluded from things.”
In a novel finding, the researchers identify an “anticipatory stress spike” of 17% experienced in the last two weeks of summer break. While still lower than mid-academic year stress, the spike was consistent across different summers.
In post-study interviews, some students pointed to returning to campus early for team sports as a source of stress. Others specified reconnecting with family and high school friends during their first summer home, saying they felt “a sense of leaving behind the comfort and familiarity of these long-standing friendships” as the break ended, the researchers report.
“This is a foundational study,” says Subigya Nepal , first author of the study and a PhD candidate in Campbell’s research group. “It has more real-time granular data than anything we or anyone else has provided before. We don’t know yet how it will translate to campuses nationwide, but it can be a template for getting the conversation going.”
The depth and accuracy of the study data suggest that mobile-sensing software could eventually give universities the ability to create proactive mental-health policies specific to certain student populations and times of year, Campbell says.
For example, a paper Campbell’s research group published in 2022 based on StudentLife data showed that first-generation students experienced lower self-esteem and higher levels of depression than other students throughout their four years of college.
“We will be able to look at campus in much more nuanced ways than waiting for the results of an annual mental health study and then developing policy,” Campbell says. “We know that Dartmouth is a small and very tight-knit campus community. But if we applied these same methods to a college with similar attributes, I believe we would find very similar trends.”
Weathering the pandemic
When students returned home at the start of the coronavirus pandemic, the researchers found that self-esteem actually increased during the pandemic by 5% overall and by another 6% afterward when life returned closer to what it was before. One student suggested in their interview that getting older came with more confidence. Others indicated that being home led to them spending more time with friends talking on the phone, on social media, or streaming movies together.
The data show that phone usage—measured by the duration a phone was unlocked—indeed increased by nearly 33 minutes, or 19%, during the pandemic, while time spent in physical activity dropped by 52 minutes, or 27%. By 2022, phone usage fell from its pandemic peak to just above pre-pandemic levels, while engagement in physical activity had recovered to exceed the pre-pandemic period by three minutes.
Despite reporting higher self-esteem, students’ feelings of stress increased by more than 10% during the pandemic. By the end of the study in June 2022, stress had fallen by less than 2% of its pandemic peak, indicating that the experience had a lasting impact on student well-being, the researchers report.
In early 2021, as students returned to campus, their reunion with friends and community was tempered by an overwhelming concern about the still-rampant coronavirus. “There was the first outbreak in winter 2021 and that was terrifying,” one student recalls. Another student adds: “You could be put into isolation for a long time even if you did not have COVID. Everyone was afraid to contact-trace anyone else in case they got mad at each other.”
Female students were especially concerned about the coronavirus, on average 13% more than male students. “Even though the girls might have been hanging out with each other more, they are more aware of the impact,” one female student reported. “I actually had COVID and exposed some friends of mine. All the girls that I told tested as they were worried. They were continually checking up to make sure that they did not have it and take it home to their family.”
Students still learning remotely had social levels 16% higher than students on campus, who engaged in activity an average of 10% less often than when they were learning from home. However, on-campus students used their phones 47% more often. When interviewed after the study, these students reported spending extended periods of time video-calling or streaming movies with friends and family.
Social activity and engagement had not yet returned to pre-pandemic levels by the end of the study in June 2022, recovering by a little less than 3% after a nearly 10% drop during the pandemic. Similarly, the pandemic correlates with students sticking closer to home, with their distance traveled nearly cut in half during the pandemic and holding at that level since then.
Campbell and several of his fellow researchers are now developing a smartphone app known as MoodCapture that uses artificial intelligence paired with facial-image processing software to reliably detect the onset of depression before the user even knows something is wrong.
Morgan Kelly can be reached at [email protected] .
- Mental Health and Wellness
- Innovation and Impact
- Arts and Sciences
- Class of 2021
- Class of 2022
- Department of Computer Science
- Guarini School of Graduate and Advanced Studies
- Mental Health
A Q&A With Film Critic and Theorist Vinzenz Hediger

After a Year of Turmoil, Harvard’s Applications Drop
Health Topics
Health Topics A-Z
Find diseases and conditions; healthy living; workplace safety; environmental health; injury, violence and safety, global health and more.
Protect yourself from Flu, COVID-19, and RSV.
What is the Health Topics A-Z Index? The Health Topics A-Z Index is a navigational and informational tool that makes the CDC.gov website easier to use. It helps you quickly find and retrieve specific information. Synonyms, acronyms, and cross-references provide multiple ways for you to access the topics and features on CDC.gov. The index includes common and scientific terms to meet the needs of consumers as well as health professionals.
What items are included? The Health Topics A-Z Index lists topics with relevance to a broad cross-section of CDC.gov’s audiences. The items are representative of popular topics, frequent inquiries, or have critical importance to CDC’s public health mission. The index will continue to evolve as additional topics are added.
To receive email updates about this page, enter your email address:
CDC Organization
View CDC’s Official Mission Statements/Organizational Charts to learn more about CDC′s organizational structure.
Popular Topics
Birth Defects
Healthy Weight
Travelers’ Health
Sexual Health

Life Stages
Adolescent & School Health
Adolescents & Teens
Infants & Toddlers
Older Adults & Seniors

Specific Populations
American Indians & Alaska Natives
Correctional Health
Family Health History
Immigrant, Refugee, and Migrant Health
Lesbian, Gay, Bisexual & Transgender
Minority Health & Health Equity
People with Disabilities
Persons Who Inject Drugs (PWID)
Women’s Health
Workplace Health Promotion

Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Blog The Education Hub
https://educationhub.blog.gov.uk/2024/03/14/how-supporting-university-students-mental-health/
How we’re supporting university students with their mental health

Going to university is a fun and exciting time for most students – but it comes with unique challenges and stresses. We believe that all students’ mental health and wellbeing should be properly supported during their time at university.
There is a range of mental health support available to students, from online mental health and wellbeing platform Student Space to counselling and one-to-one support. Here’s what you need to know.
What action are you taking to support students’ mental health?
Students struggling with their mental health can access Student Space , a mental health and wellbeing hub supporting students.
Funded by £3.6 million from the Office for Students (OfS), Student Space provides dedicated one-to-one text and web chat support services. It’s also an online platform providing vital mental health and wellbeing resources.
This service is part of the £15 million we have asked the OfS to allocate towards student mental health in 2023/2024. This funding will also be used to give additional support for those making the transition from school or college to university, in particular through counselling services.
It will also be used to address any challenges that students may face in accessing local support services through their university, by establishing better partnerships between universities and local NHS services.
To ensure all the information is readily available for students and young people, we have put together some useful links and sources of mental health support so that everyone can get the advice and help they need. This information is available here .
We are also asking universities to take a whole university approach to mental health by setting a target for all universities to sign up to the University Mental Health Charter Programme by September 2024.
To support this target t he Office for Students ( OfS ) is providing £400,000 additional funding to Student Minds to support expansion of the Programme . You can read more about it on the OfS website .
What is the University Mental Health Charter Programme?
Universities that are part of the University Mental Health Charter programme will be supported to make cultural change so that all aspects of university life promote and support mental health.
Both students and staff will benefit from better support for their mental health and wellbeing as a result.
The Charter Award is given to the universities that are part of the Programme members which demonstrate excellent practice in supporting student mental health.
What is the Department doing to reduce suicides at universities?
Every student death is a tragedy and preventing suicide and self-harm in our student populations is a key priority.
So that students are better protected we have asked universities to fully implement best practice including the Suicide Safer Universities guidance, led by Universities UUK and Papyrus.
This includes guidance for universities on sharing information with family and friends in the event of a mental health crisis and practical advice on compassionate, confident, and timely support when a tragedy occurs.
Understanding student suicide data and risk factors is central to informing preventative action, which is why we have worked with the Office for National Statistics, which has published updated data and analysis .
We appointed Professor Edward Peck as Higher Education Student Support Champion in May 2022 for a two-year term and extended the appointment for another year until 31 May 2025 . Professor Peck has been speaking to bereaved parents to understand where improvements can be made.
To deliver better practice in mental health support across the higher education sector Professor Peck is chairing a Higher Education Mental Health Implementation Taskforce, which will include bereaved parents, students, mental health experts, charities and sector representatives.
It has been asked to deliver a report with a plan for better early identification of students at risk, a University Student Commitment on dealing with students sensitively on disciplinary issues, and a set of clear targets for improvements in practice by providers.
Its first stage report has been published outlining progress so far and setting out new areas of focus, including improving join up between higher education and NHS mental health services. It is due to publish a second stage report by July 2024.
We have also appointed the National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH) to carry out a National Review of Higher Education Suicides.
This will ensure that valuable lessons from past tragedies can be learnt to help us better protect students in future. Its findings report will be published by Spring 2025 outlining good practice and areas for improvement around suicide prevention in higher education.
Providers’ participation in the National Review of HE Suicides will be supported by the additional one-off £10m funding we have asked the OfS to allocate on mental health and hardship, which comes top of the £15 million already distributed this year on HE student mental health.
What should I do if I’m worried about a friend or family member at university?
We understand that helping a friend or family member with mental health issues can be difficult. It is important that students feel supported at this difficult time. There is support in place and people who are available to listen.
If for any reason you have cause to believe that someone you know is struggling with mental health and wellbeing issues at university, we recommend following NHS guidance .
Universities have support services in place for their students which can be accessed via their website, or by looking up your university on the Student Space support pages .
You may also be interested in:
- Mental health resources for children, students, parents, carers and school/college staff
- What we are doing to improve the mental health of children and young people
- Five things you didn’t know about mental health support in schools
Tags: Mental health , mental health resources , Office for Students , Pupil mental health , Universities UK , University , Wellbeing
Sharing and comments
Share this page, related content and links, about the education hub.
The Education Hub is a site for parents, pupils, education professionals and the media that captures all you need to know about the education system. You’ll find accessible, straightforward information on popular topics, Q&As, interviews, case studies, and more.
Please note that for media enquiries, journalists should call our central Newsdesk on 020 7783 8300. This media-only line operates from Monday to Friday, 8am to 7pm. Outside of these hours the number will divert to the duty media officer.
Members of the public should call our general enquiries line on 0370 000 2288.
Sign up and manage updates
Follow us on social media, search by date, comments and moderation policy.
- About the Hub
- Announcements
- Faculty Experts Guide
- Subscribe to the newsletter
Explore by Topic
- Arts+Culture
- Politics+Society
- Science+Technology
- Student Life
- University News
- Voices+Opinion
- About Hub at Work
- Gazette Archive
- Benefits+Perks
- Health+Well-Being
- Current Issue
- About the Magazine
- Past Issues
- Support Johns Hopkins Magazine
- Subscribe to the Magazine
You are using an outdated browser. Please upgrade your browser to improve your experience.

Credit: COURTESY OF LIVE BALTIMORE
An ambitious new annual survey of Baltimore's residents aims to inform local policy
By Sheri Booker
When Johns Hopkins researchers began developing the Baltimore Area Survey —a new annual appraisal of Baltimore City and County residents—they wanted to ask questions on hot-button issues that could inform local and state policy while also gauging the emotional state of the area's residents. For the transportation section of the survey, for instance, that meant asking questions like: Do you feel left out? Do you feel down because you don't have transportation to get to places for social engagement? Have you ever been let down by transportation?
"It's really important to understand whether people can get to the doctor or get to work, but it's also important to know whether you feel like you're left out because you can't get to places to meet folks," explains Michael Bader , faculty director of the Johns Hopkins 21st Century Cities Initiative , which released the survey in late 2023. According to their findings, 1 in 10 Baltimore area residents admitted that they "often" feel down because of transportation issues, while a whopping one-third of residents reported at least one transportation issue. The data also highlighted racial inequality in public transportation: Twice as many Baltimore area residents of color experienced transportation-related issues—like missing an appointment—than white residents in the same areas.
With the Baltimore Area Survey, Bader—an associate professor of sociology who studies the evolution of cities and neighborhoods since the civil rights era—wanted to document what daily life looks like for Baltimore area residents and how experiences and perceptions are impacted by race. Last summer, his team mailed the survey to 6,000 Baltimore City residents and 4,000 Baltimore County residents, along with a crisp $2 bill as an incentive. A total of 1,352 households sent back their responses. A collaboration between Hopkins researchers, community members, and students, the survey zeros in on four broad themes: neighborhoods, connectivity, health, and finance/entrepreneurship.
"One of the things that I think we did was document the ways in which the daily disparities and inequalities exist among white and Black Baltimoreans," he says. "We know it exists, but to be able to put data behind what those disparities are and across different dimensions is valuable, and I think it's something we can contribute as a university to the city."
While some inequities were expected, there were several that surprised the research team. When it came to food insecurity, for example, Bader and his team ran the numbers three or four times before believing that the city's rates are 2 to 3 times higher than the national average. And on the topic of policing, 3 out of 4 Black Baltimoreans feared being arrested or questioned by the police, while only 1 in 4 white residents said they had the same fears.
In the education section, the biggest takeaway for the team was that county residents thought that public schools in the county were better than those in the city.
The survey's results are already being used by local agencies and organizations to support programming and policy changes. Central Baltimore Partnership , for example, is using the data to support its Greenmount Life, Opportunity, and Wellness Initiative , which is focused on examining the social determinants of health along the Greenmount Avenue corridor. "The organization is using data from the Baltimore Area Survey to get additional insight into the needs of the neighborhoods where they work and to identify any disparities such as food or transit insecurity," explains Mac McComas , senior program manager for the 21st Century Cities Initiative.
While Bader hopes the data from this project will inform future policy, he also wants it to serve as a foundation for graduate students and other researchers to build their studies upon.
Raghav Agrawal, a sophomore economics major, was one of two undergraduate students who worked on the study. At first Agrawal, who often uses public transportation, thought questions about being let down by transportation were strange for this type of survey, but after deeper analysis he was able to see how important it is to address these types of questions.
"This project has helped me to view everything through an equity lens," he says. "Now I ask, Is it equitable distribution? … It gives me hope for how it can help the city."
Baltimore ahead of nation in people who have loved ones pass away from overdose
Hopkins survey shows baltimore-area residents’ perceptions on education, transportation, health, and more, few baltimore-area residents trust local government, new survey says.
The questions won't be the same from year to year, but Bader hopes to work closely with a committee of local nonprofits, faith leaders, government officials, and philanthropists to identify important topics to examine. The goal is to ensure that policymakers have the latest and most informed data when making decisions for their constituents. The questions for the 2024 survey are already in the works, with transportation issues remaining at the forefront. This time, the questions will go beyond transportation insecurity and consider the upcoming plans for the Red Line—a major initiative to enhance east-west transit in the city —and Complete Streets—a plan to better consider pedestrians, bicyclists, and transit users in roadway design . The questions will also explore how people are impacted by violence and possible solutions to the problem.
Bader says he wishes the survey would've begun years earlier.
"If we had a survey in 2019 and out every year following, we would've been able to understand some of the impacts of the pandemic as they were happening rather than waiting three years to get the information," he says. "We never know when these things are going to come up, and that's why this project adds value to the Baltimore community."
Posted in Community
You might also like
News network.
- Johns Hopkins Magazine
- Get Email Updates
- Submit an Announcement
- Submit an Event
- Privacy Statement
- Accessibility
Discover JHU
- About the University
- Schools & Divisions
- Academic Programs
- Plan a Visit
- my.JohnsHopkins.edu
- © 2024 Johns Hopkins University . All rights reserved.
- University Communications
- 3910 Keswick Rd., Suite N2600, Baltimore, MD
- X Facebook LinkedIn YouTube Instagram

IMAGES
VIDEO
COMMENTS
A collection of presentations designed for health educators to use in face-to-face sessions with community members to increase environmental health literacy. Promoting Environmental Health in Communities (ATSDR). A guide that includes talking points, PowerPoint presentations, and covers the basic concepts of the environment, toxicology, and health.
Health education strategies are tailored for their intended audience. Health education presents information to audiences on different health topics, including the health benefits or threats they face, and provides tools to build capacity and support behavior change in an appropriate setting. Characteristics of health education strategies include:
A person's community can have a major impact on their health and well-being. Healthy People 2030 focuses on ways organizations, businesses, schools, and residents can help build healthier communities. Community organizations that provide preventive health care services can help improve health and well-being. Businesses can also help keep ...
Public Health is described as the science of protecting and improving the health of communities through education, promotion of healthy lifestyles and research for disease and injury prevention. Professionals in Public Health study health related concerns that are potentially affecting communities and work to find ways to educate individuals to ...
The Community Health Education program will teach you to positively influence the health behavior of individuals, groups and communities. ... This course provides for an in-depth analysis of the array of topics germane to the health field. Each semester one or more topics will be offered through this course. Prerequisite: HED 100 or HED 110.
Health Education Curriculum Analysis Tool (HECAT). This tool helps school and community leaders conduct clear, complete, and consistent analyses of health education curricula across a wide variety of topics (e.g., nutrition, tobacco, mental/emotional health). HECAT Webinars. A series of six videos introducing HECAT and featured health topic ...
Health systems. Infection prevention and control. Conditions. Infertility. Diseases and conditions. Influenza (avian and other zoonotic) Diseases and conditions. Influenza seasonal. Socio-political determinants.
Members of the Educational and Community Based Programs (ECBP) Workgroup have expertise in areas including school-based health centers, K-12 school and workplace health programs and policies, and medical/allied professions training curricula. They developed the objectives related to educational and community-based programs, and they'll provide data to track progress toward achieving these ...
reviews health education theories and definitions, identifies the components of evidence-based health education and outlines the abilities necessary to engage in effective practice. Much has been written over the years about the relationship and overlap between health education, health promotion and other concepts, such as health literacy.
A Community Health Worker Training Manual Resource for Preventing Heart Disease and Stroke. Document. Presents an evidence-based, user-friendly curriculum for CHWs to increase their skills in preventing heart disease, stroke, and the associated risk factors. Organization (s): Centers for Disease Control and Prevention.
The Health 1,2,3,4 program maintains a collaborative partnership with Martin Luther King Jr. Middle School to provide health education to its 6 th-8 th grade student population. Students who pursued the Health 497 King Middle School path developed and facilitated lesson plans on several health-related topics, including nutrition, positive ...
9. Health Promotion and Disease Prevention in Community Settings. Our world—and our neighborhoods—are instrumental in determining our health status. Education, access to services, family life, and work all play a role in shaping individual health and lifestyles. The kinds of health messages that people receive close to home, in their own ...
Health Education, Advocacy and Community Mobilisation Module: 12. Planning Health Education Programmes: 1 ... For example, you wouldn't offer health education to households on the same topic at every visit. Fourthly, planning helps you prioritise needs and activities. This is useful because your community may have a lot of problems, but not ...
This paper strives to present current evidence and examples of how the collaboration between health education and health literacy disciplines can strengthen K-12 education, promote improved health, and foster dialogue among school officials, public health officials, teachers, parents, students, and other stakeholders.
Highlighted Topics. Alzheimer's and Dementia. Brain Health. Caregiving. Clinical Trials and Studies. Exercise and Physical Activity. Healthy Eating. Menopause. NIA provides health information informed by research and reviewed by experts to help you learn about healthy aging and common health conditions in older adults.
Come join us in a rich community engagement talk with Dr. Tyler Derreth, an assistant professor in the Department of Health, Behavior and Society and an associate Director of SOURCE. Dr. Derreth will share with BSPH community tools and resources on how public health professionals can engage in community by building authentic relationships, learning through service, redistributing power, and ...
Community Health Education. We provide community education on a wide array of health topics. These include, but not limited to: Child Health and Safety. Chronic Health Conditions. Communicable Diseases. Emergency Preparedness. Hand Washing & Illness Prevention. Injury Prevention.
Creating a robust community oral health program is more than a goal; it's a commitment to the well-being of a community. Community Oral Health Program, commonly known as COHP, is a public health initiative aimed at improving oral health of a specific community. It incorporates the principles of health education and promotion and extends ...
The CHCE's nine-week education program - now in its second year - immerses Black medical students in one of the six publicly funded community health centres near Toronto that are dedicated ...
This recognition is evident in the first goal of the EFA which is to expand and improve comprehensive early childhood care and education, especially for the most vulnerable and disadvantaged children, and in five of the MDG goals which relate to the health, nutrition and education of children. 1 Other high-ranked solutions were: number 2 ...
The team made their anonymized data set publicly available—including self-reports, surveys, and phone-sensing and brain-imaging data—to help advance research into the mental health of students during their college years.. Andrew Campbell, the paper's senior author and Dartmouth's Albert Bradley 1915 Third Century Professor of Computer Science, says that the study's extensive data ...
The Health Topics A-Z Index lists topics with relevance to a broad cross-section of CDC.gov's audiences. The items are representative of popular topics, frequent inquiries, or have critical importance to CDC's public health mission. The index will continue to evolve as additional topics are added. Last Updated December 29, 2023.
With medical care covered by the Compulsory Health Insurance Fund, financing of social spending in 2020 will make up more than RUB 2 trillion. Spending on state-run educational programs in education will grow by 25.8%, with a 30.4% growth in healthcare, 63.7% in sports, and 18,4% in social support for residents.
Health Days, All-Russia Health Days and memorable occasions, or in connection with the control of major diseases and are held in outpatient clinics or off site; 62 awareness-raising and preventive activities were conducted in 2022. Overall, 8500 health-related activities were held that year with a total of 1 941 400 participants.
The authors also urge the medical community to update their education and training and take steps to combat global warming. UC Davis infectious diseases specialist George Thompson "Clinicians need to be ready to deal with the changes in the infectious disease landscape," said lead author George R. Thompson.
Going to university is a fun and exciting time for most students - but it comes with unique challenges and stresses. We believe that all students' mental health and wellbeing should be properly supported during their time at university. There is a range of mental health support available to students, from online mental health and wellbeing platform Student Space to counselling and one-to ...
The integration of health education and nutrition support nursing can effectively enhance the therapeutic outcomes of patients with pulmonary tuberculosis. This approach not only improves their nutritional status, treatment adherence, and quality of life, but also reduces the incidence of adverse reactions.
And on the topic of policing, 3 out of 4 Black Baltimoreans feared being arrested or questioned by the police, while only 1 in 4 white residents said they had the same fears. In the education section, the biggest takeaway for the team was that county residents thought that public schools in the county were better than those in the city.