Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic

RELATED TOPICS
INTRODUCTION
This topic will review the development, clinical manifestations, and diagnosis of portal hypertension in adults. The causes of portal hypertension and the treatment of its complications are discussed in detail elsewhere:
● (See "Cirrhosis in adults: Etiologies, clinical manifestations, and diagnosis" .)
● (See "Noncirrhotic portal hypertension" .)
● (See "Cirrhosis in adults: Overview of complications, general management, and prognosis", section on 'Preventing complications' .)
Advertisement
Systemic Disease and Portal Hypertension
- Published: 04 March 2024
- Volume 23 , pages 162–173, ( 2024 )
Cite this article

- Talal Khurshid Bhatti 1 &
- Paul Y. Kwo 2
60 Accesses
Explore all metrics
Purpose of Review
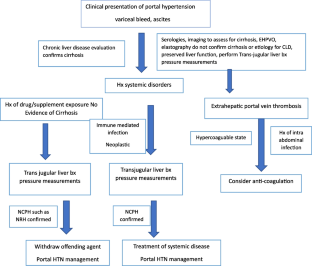
The development of portal hypertension is typically a consequence of liver cirrhosis due mainly to primary liver disorders, whereas non-cirrhotic portal hypertension (NCPH) can be a complication of systemic, primarily extrahepatic diseases. Our purpose was to review the various systemic disorders leading to portal hypertension and provide a pathway for diagnosis and management.
Recent Findings
Non-cirrhotic portal hypertension is a heterogeneous group of liver disorders primarily of vascular origin that may manifest as portal hypertension. The diagnosis of NCPH in the setting of systemic diseases is challenging and a liver biopsy may be required to confirm the diagnosis. Etiologies include those of vascular origin, autoimmune disorders, drug exposures, and infections.
Complications of portal hypertension in the setting of systemic diseases are similar to patients having cirrhosis and should be addressed similarly while addressing the underlying systemic disorder if possible
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Non-Cirrhotic Portal Hypertension: an Overview
Idiopathic non-cirrhotic portal hypertension: a review.

Non-cirrhotic Portal Fibrosis
Papers of particular interest, published recently, have been highlighted as: •• of major importance.
Schouten JN, Garcia-Pagan JC, Valla DC, Janssen HL. Idiopathic noncirrhotic portal hypertension. Hepatology. 2011;54(3):1071–81.
Article PubMed Google Scholar
Gracia-Sancho J, Marrone G, Fernández-Iglesias A. Hepatic microcirculation and mechanisms of portal hypertension. Nat Rev Gastroenterol Hepatol. 2019;16(4):221–34.
Intagliata NM, Caldwell SH, Tripodi A. Diagnosis, development, and treatment of portal vein thrombosis in patients with and without cirrhosis. Gastroenterology. 2019;156(6).
Simonetto DA, Liu M, Kamath PS. Portal hypertension and related complications :diagnosis and management. Mayo Clin Proc. 2019;94(4):714–26.
Khanna R, Sarin SK. Idiopathic portal hypertension and extrahepatic portal venous obstruction. Hepatol Int. 2018;12(Suppl 1):148–67.
Da BL, Surana P, Kapuria D, Vittal A, Levy E, Kleiner DE, Koh C, Heller T. Portal pressure in noncirrhotic portal hypertension: to measure or not to measure. Hepatology. 2019;70(6):2228–30. Of major importance: This study reported in a large cohort of individuals with non-cirrhotic portal hypertension that portal pressures as assessed by HVPH are not typically elevated and also do not correlate with complications of portal hypertension. They suggest that at obtaining a liver biopsy percutaneously may be an appropriate strategy in this population .
Eapen CE, Nightingale P, Hubscher SG, et al. Non-cirrhotic intrahepatic portal hypertension: associated gut diseases and prognostic factors. Dig Dis Sci. 2011;56(1):227–35.
Article CAS PubMed Google Scholar
Sharma P, Agarwal R, Dhawan S, Bansal N, Singla V, Kumar A, Arora A. Transient elastography (fibroscan) in patients with non-cirrhotic portal fibrosis. J Clin Exp Hepatol. 2017;7(3):230–4.
Article PubMed PubMed Central Google Scholar
Sarin SK, Khanna R. Noncirrhotic portal hypertension. Clin Liver Dis. 2014;18:451–76.
Verheij J, Schouten JN, Komuta M, et al. Histological features in western patients with idiopathic non-cirrhotic portal hypertension. Histopathology. 2013;62(7):1083–91.
Lee H, Rehman AU, Fiel MI. Idiopathic noncirrhotic portal hypertension: an appraisal. J Pathol Transl Med. 2016;50(1):17–25.
Nayak NC, Jain D, Saigal S, Soin AS. Non-cirrhotic portal fibrosis: one disease with many names? An analysis from morphological study of native explant livers with end stage chronic liver disease. J Clin Pathol. 2011;64(7):592–8.
Hillaire S, Bonte E, Denninger MH, et al. Idiopathic non-cirrhotic intrahepatic portal hypertension in the west: a re-evaluation in 28 patients. Gut. 2002;51(2):275–80.
Article CAS PubMed PubMed Central Google Scholar
De Gottardi A, Rautou PE, Schouten J, Rubbia-Brandt L, Leebeek F, Trebicka J, Murad SD, Vilgrain V, Hernandez-Gea V, Nery F, Plessier A. Porto-sinusoidal vascular disease: proposal and description of a novel entity. Lancet Gastroenterol Hepatol. 2019;4(5):399–411.
Cerda Reyes E, González-Navarro EA, Magaz M, Muñoz-Sánchez G, Diaz A, Silva-Junior G, et al. Autoimmune biomarkers in porto-sinusoidal vascular disease: potential role in its diagnosis and pathophysiology. Liver Int. 2021;41(9):2171–8.
Sarin SK, Kapoor D. Non-cirrhotic portal fibrosis: current concepts and management. J Gastroenterol Hepatol. 2002;17:526–34.
Madhu K, Avinash B, Ramakrishna B, Eapen CE, Shyamkumar NK, Zachariah U, et al. Idiopathic non-cirrhotic intrahepatic portal hypertension: common cause of cryptogenic intrahepatic portal hypertension in a Southern Indian tertiary hospital. Indian J Gastroenterol. 2009;28:83–7.
Okudaira M, Ohbu M, Okuda K. Idiopathic portal hypertension and its pathology. Semin Liver Dis. 2002;22(1):59–72.
Chang P-E, Miquel R, Blanco J-L, Laguno M, Bruguera M, Abraldes JG, et al. Idiopathic portal hypertension in patients with HIV infection treated with highly active antiretroviral therapy. Am J Gastroenterol. 2009;104:1707–14.
Schouten JN, Van der Ende ME, Koëter T, et al. Risk factors and outcome of HIV associated idiopathic noncirrhotic portal hypertension. Aliment Pharmacol Ther. 2012;36(9):875–85.
Mallet V, Blanchard P, Verkarre V, Vallet-Pichard A, Fontaine H, Lascoux-Combe C, et al. Nodular regenerative hyperplasia is a new cause of chronic liver disease in HIV-infected patients. AIDS. 2007;21:187–92.
Okuda K. Non-cirrhotic portal hypertension versus idiopathic portal hypertension. J Gastroenterol Hepatol. 2002;17(Suppl 3):S204–13.
PubMed Google Scholar
Salzer U, Warnatz K, Peter HH. Common variable immunodeficiency: an update. Arthritis Res Ther. 2012;14:223.
Xiao X, Miao Q, Chang C, Gershwin ME, Ma X. Common variable immunodeficiency and autoimmunity—an inconvenient truth. Autoimmun Rev. 2014;13:858–64.
Bonilla FA, Barlan I, Chapel H, Costa-Carvalho BT, Cunningham-Rundles C, de la Morena MT, Espinosa-Rosales FJ, et al. International consensus document (ICON): common variable immunodeficiency disorders. J Allergy Clin Immunol Pract. 2016;4:38–59.
Resnick ES, Moshier EL, Godbold JH, Cunningham-Rundles C. Morbidity and mortality in common variable immune deficiency over 4 decades. Blood. 2012;119:1650–7.
Gathmann B, Mahlaoui N, Gerard L, Oksenhendler E, Warnatz K, Schulze I, Kindle G, et al. Clinical picture and treatment of 2212 patients with common variable immunodeficiency. J Allergy Clin Immunol. 2014;134:116–26.
Cunningham-Rundles C, Maglione PJ. Common variable immunodeficiency. J Allergy Clin Immunol. 2012;129:1425-1426.e1423.
Fuss IJ, Friend J, Yang Z, et al. Nodular regenerative hyperplasia in common variable immunodeficiency. J Clin Immunol. 2013;33:748–58.
Inagaki H, Nonami T, Kawagoe T, et al. Idiopathic portal hypertension associated with systemic lupus erythematosus. J Gastroenterol. 2000;35(3):235–9.
van Hoek B. The spectrum of liver disease in systemic lupus erythematosus. Neth J Med. 1996;48(6):244–53.
Matsumoto T, Yoshimine T, Shimouchi K, et al. The liver in systemic lupus erythematosus: pathologic analysis of 52 cases and review of Japanese Autopsy Registry Da-ta. Hum Pathology. 1992;23(10):1151–8.
Article CAS Google Scholar
Efe C, Purnak T, Ozaslan E, et al. Autoimmune liver disease in patients with systemic lupus erythematosus retrospective analysis of 147 cases. Scand J Gastroenterol. 2011;46(6):732–7.
Kraaijvanger R, Janssen Bonás M, Vorselaars AD, Veltkamp M. Biomarkers in the diagnosis and prognosis of sarcoidosis: current use and future prospects. Front Immunol. 2020;14(11):1443.
Article Google Scholar
Kennedy PTF, Zakaria N, Modawi SB, et al. Natural history of hepatic sarcoidosis and its response to treatment. European J Gastroenterol Hepatol. 2006;18:721–6.
Bodh V, Chawla YK. Noncirrhotic intrahepatic portal hypertension. Clin Liver Dis. 2014;3:129–32.
Koukounari A, Donnelly CA, Sacko M, Keita AD, Landouré A, Dembelé R, et al. The impact of single versus mixed schistosome species infections on liver, spleen and bladder morbidity within Malian children pre- and post-praziquantel treatment. BMC Infect Dis. 2010;10:227.
Mazigo HD, Nuwaha F, Wilson S, Kinung’hi SM, Morona D, Waihenya R, et al. Epidemiology and interactions of human immunodeficiency virus - 1 and Schistosoma Mansoni+ in sub-Saharan Africa. Infect Dis Poverty. 2013;2(1):2.
Pereira TA, Xie G, Choi SS, Syn WK, Voieta I, Lu J, et al. Macrophage-derived hedgehog ligands promotes fibrogenic and angiogenic responses in human Schistosomiasis mansoni. Liver Int. 2013;33:149–61.
Mallet VO, Varthaman A, Lasne D, Viard JP, Gouya H, Borgel D, Lacroix-Desmazes S. et al. Acquired protein S deficiency leads to obliterative portal venopathy and to compensatory nodular regenerative hyperplasia in HIV-infected patients. AIDS. 2009;23(12):1511–1518.
Lafeuillade A, Alessi MC, Poizot-Martin I, Dhiver C, Quilichini R, Aubert L, et al. Protein S deficiency and HIV infection. N Engl J Med. 1991;324:1220.
Siramolpiwat S, Seijo S, Miquel R, et al. Idiopathic portal hypertension: natural history and long-term outcome. Hepatology. 2014;59(6):2276–85.
Bora D. Epidemiology of visceral leishmaniasis in India. Natl Med J India. 1999;12:62–8.
CAS PubMed Google Scholar
Bryceson A. Visceral leishmaniasis in India. Lancet. 2000;356:1933.
Singh S, Sivakumar R. Recent advances in the diagnosis of leishmaniasis. J Postgrad Med. 2003;49:55–60.
Datta DV, Saha S, Grover SL, Samant A, Singh R, Chakravarti N, et al. Portal hypertension in kalaazar. Gut. 1972;13:147–52.
Agrawal P, Wali JP, Chopra P. Liver in kala-azar. Indian J Gastroenterol. 1990;9:135–6.
Google Scholar
Guevara P, Ramirez JL, Rojas L, Scorza JV, Gonzales N, Anez N. Leishmania braziliensis in blood 30 years after cure. Lancet. 1993;341:1341.
Rogler G. Gastrointestinal and liver adverse effects of drugs used for treating IBD. Best Practice Res Clin Gastroenterol. 2010;24(2):157–65.
Wanless IR, Godwin TA, Allen F, Feder A. Nodular regenerative hyperplasia of the liver in hematologic disorders: a possible response to obliterative portal venopathy. A morphometric study of nine cases with an hypothesis on the pathogenesis. Medicine. 1980;59:367–79.
DeLeve LD, Wang X, Kuhlenkamp JF, et al. Toxicity of azathioprine and monocrotaline in murine sinusoidal endothelial cells and hepatocytes: the role of glutathione and relevance to hepatic venoocclusive disease. Hepatology. 1996;23:589–99.
De Vito C, Tyraskis A, Davenport M, Thompson R, Heaton N, Quaglia A. Histopathology of livers in patients with congenital portosystemic shunts (Abernethy malformation): a case series of 22 patients. Virchows Arch. 2018;474(1):47–57.
Baiges A, Turon F, Simón-Talero M, Tasayco S, Bueno J, Zekrini K, et al. Congenital extrahepatic portosystemic shunts (Abernethy malformation): an international observational study. Hepatology. 2019;71(2):658–69.
Majumdar A, Delatycki MB, Crowley P, et al. with m. J Hepatol. 2015;63(2):525–7.
Besmond C, Valla D, Hubert L, et al. Mutations in the novel gene FOPV are associated with familial autosomal dominant and non-familial obliterative portal venopathy. Liver Int. 2018;38(2):358–64.
Dumortier J, Boillot O, Chevallier M, et al. Familial occurrence of nodular regenerative hyperplasia of the liver: a report on three families. Gut. 1999;45(2):289–94.
Witters P, Libbrecht L, Roskams T, Boeck KD, Dupont L, Proesmans M, et al. Noncirrhotic pre-sinusoidal portal hypertension is common in cystic fibrosis-associated liver disease. Hepatology. 2011;53:1064–5.
Mayer JE, Schiano TD, Fiel MI, Hoffman R, Mascarenhas JO. An association of myeloproliferative neoplasms and obliterative portal venopathy. Dig Dis Sci. 2014;59(7):1638–41.
Valla DC, Cazals-Hatem D. Vascular liver diseases on the clinical side: definitions and diagnosis, new concepts. Virchows Arch. 2018;473(1):3–13.
Schouten JNL, Nevens F, Hansen B, Laleman W, den Born M, Komuta M, et al. Idiopathic noncirrhotic portal hypertension is associated with poor survival: results of a long-term cohort study. Aliment Pharmacol Ther. 2012;35:1424–33.
Cazals-Hatem D, Hillaire S, Rudler M, Plessier A, Paradis V, Condat B, et al. Obliterative portal venopathy: portal hypertension is not always present at diagnosis. J Hepatol. 2011;54:455–61.
Carreras LO, Defreyn G, Machin SJ, Vermylen J, Deman R, Spitz B, et al. Arterial thrombosis, intrauterine death and “lupus” antiocoagulant: detection of immunoglobulin interfering with prostacyclin formation. Lancet. 1981;1:244–6.
O’Leary JG, Cai J, Freeman R, et al. Proposed diagnostic criteria for chronic antibody mediated rejection in liver allografts. Am J Transpl. 2016;16(2):603–14.
Etzion O, Koh C, Heller T. Noncirrhotic portal hypertension: An overview. Clin Liver Dis (Hoboken). 2015;6(3):72–74.
Glatard AS, Hillaire S, d’Assignies G, Cazals-Hatem D, Plessier A, Valla DC, Vilgrain V. Obliterative portal venopathy: findings at CT imaging. Radiology. 2012;263(3):741–50.
Arora A, Sarin SK. Multimodality imaging of obliterative portal venopathy: what every radiologist should know. Br J Radiol. 2015;88(1046):20140653.
Elkrief L, Lazareth M, Chevret S, Paradis V, Magaz M, Blaise L, Rubbia-Brandt L, et al. Liver stiffness by transient elastography to detect porto-sinusoidal vascular liver disease with portal hypertension. Hepatology . 2020.
Sarin SK, Kumar A, Chawla YK, Baijal SS, Dhiman RK, Jafri W, et al. Noncirrhotic portal fibrosis/idiopathic portal hypertension: APASL recommendations for diagnosis and treatment. Hepatol Int. 2007.
Dhiman RK, Chawla Y, Vasishta RK, Kakkar N, Dilawari JB, Trehan MS, et al. Non-cirrhotic portal fibrosis (idiopathic portal hypertension): experience with 151 patients and a review of the literature. J Gastroenterol Hepatol. 2002;17:6–16.
Okuda K, Kono K, Ohnishi K, Kimura K, Omata M, Koen H, et al. Clinical study of eighty-six cases of idiopathic portal hypertension and comparison with cirrhosis with splenomegaly. Gastroenterology. 1984;86:600–10.
Rangari M, Gupta R, Jain M, Malhotra V, Sarin SK. Hepatic dysfunction in patients with extrahepatic portal venous obstruction. Liver Int. 2003;23:434–9.
Bissonnette J, Garcia-Pagán JC, Albillos A, Turon F, Ferreira C, Tellez L, et al. Role of the trans-jugular intrahepatic portosystemic shunt in the management of severe complications of portal hypertension in idiopathic noncirrhotic portal hypertension: liver failure/cirrhosis/portal hypertension. Hepatology. 2016;64(1):224–31.
Lattanzi B, Gioia S, Di Cola S, et al. Prevalence and impact of sarcopenia in non-cirrhotic portal hypertension. Liver Int. 2019;39(10):1937–42. Of major importance: This report notes that the prevalence of sarcopenia in a cohort of patients with non-cirrhotic portal hypertension as assessed by skeletal muscle index (SMI) was similar to those with cirrhosis, decompensated and portal vein thrombosis suggesting that the presence of portal hypertension contributes sarcopenia. In addition, sarcopenia was also associated with a higher rate of variceal bleeding requiring TIPS placement .
Dhiman RK, Behera A, Chawla YK, Dilawari JB, Suri S. Portal hypertensive biliopathy. Gut. 2007;56:1001–8.
Dilawari JB, Chawla YK. Extrahepatic portal venous obstruction. Gut. 1988;29:L554-555.
Maruyama H, Okugawa H, Kobayashi S, Yoshizumi H, Takahashi M, Ishibashi H, et al. Non-invasive porto-graphy: a microbubble-induced three-dimensional sonogram for discriminating idiopathic portal hypertension from cirrhosis. Br J Radiol. 2012;85(1013):587–95.
Lee H, Ainechi S, Singh M, Ells PF, Sheehan CE, Lin J. Histological spectrum of idiopathic noncirrhotic portal hypertension in liver biopsies from dialysis patients. Int J Surg Pathol. 2015;23(6):439–46.
Bioulac-Sage P, Le Bail B, Bernard PH, Balabaud C. Hepatoportal sclerosis. Semin Liver Dis. 1995;15(4):329–39.
Jharap B, van Asseldonk DP, de Boer NKH, et al. Diagnosing nodular regenerative hyperplasia of the liver is thwarted by low interobserver agreement. PLoS ONE. 2015;10:e0120299.
de Franchis R; On behalf of the Baveno V Faculty. Revising consensus in portal hypertension: report of the Baveno V consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2010;53:762–768.
Sarin SK, Gupta N, Jha SK, Agrawal A, Mishra SR, Sharma BC, et al. Equal efficacy of endoscopic variceal ligation and propranolol in preventing variceal bleeding in patients with noncirrhotic portal hypertension. Gastroenterology. 2010;139:1238–45.
Sarin SK, Sollano JD, Chawla YK, Amarapurkar D, Hamid S, Hashizume M, et al. Members of the APASL working party on portal hypertension. Consensus on extra-hepatic portal vein obstruction. Liver Int. 2006;26:512–9.
Romano M, Giojelli A, Capuano G, Pomponi D, Salvatore M. Partial splenic embolization in patients with idiopathic portal hypertension. Eur J Radiol. 2004;49:268–73.
Hirota S, Ichikawa S, Matsumoto S, Motohara T, Fukuda T, Yoshikawa T. Interventional radiologic treatment for idiopathic portal hypertension. Cardiovasc Intervent Radiol. 1999;22:311–4.
Krasinskas AM, Eghtesad B, Kamath PS, Demetris AJ, Abraham SC. Liver transplantation for severe intrahepatic noncirrhotic portal hypertension. Liver Transpl. 2005;11:627–34.
Dumortier J, Bizollon T, Scoazec JY, Chevallier M, Bancel B, Berger F, et al. Orthotopic liver transplantation for idiopathic portal hypertension: indications and outcome. Scand J Gastroenterol. 2001;36:417–22.
Loinaz C, Colina F, Musella M, Lopez-Rios F, Gomez R, Jimenez C, et al. Orthotopic liver transplantation in 4 patients with portal hypertension and non-cirrhotic nodular liver. Hepato-Gastroenterol. 1998.
Download references
Author information
Authors and affiliations.
Shaheed Zulfiqar Ali Bhutto Medical University, Islamabad, Pakistan
Talal Khurshid Bhatti
Stanford University School of Medicine, 430 Broadway, Pavilion C, 3Rd Floor, Redwood City, Palo Alto, CA, USA
Paul Y. Kwo
You can also search for this author in PubMed Google Scholar
Contributions
PK made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; drafted the work or revised it critically for important intellectual content; approved the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. TK made substantial contributions to the acquisition, analysis, or interpretation of data; drafted the work or revised it critically for important intellectual content; approved the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Correspondence to Paul Y. Kwo .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Conflict of Interest
Human and animal rights and informed consent.
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Bhatti, T.K., Kwo, P.Y. Systemic Disease and Portal Hypertension. Curr Hepatology Rep 23 , 162–173 (2024). https://doi.org/10.1007/s11901-024-00645-8
Download citation
Accepted : 15 January 2024
Published : 04 March 2024
Issue Date : March 2024
DOI : https://doi.org/10.1007/s11901-024-00645-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Non-cirrhotic portal hypertension
- Nodular regenerative hyperplasia
- Extrahepatic portal vein thrombosis
- Hepatoportal sclerosis
- Idiopathic portal hypertension
- Find a journal
- Publish with us
- Track your research
- Current Issue
- Supplements
Gastroenterology & Hepatology
January 2021 - volume 17, issue 1, overview of current management of portal hypertension, guadalupe garcia-tsao, md.
Professor of Medicine Yale University School of Medicine New Haven, Connecticut Chief, Digestive Diseases Section VA-CT Healthcare System West Haven, Connecticut
G&H Currently, what are the most common causes of portal hypertension?
GG-T Portal hypertension is high pressure in the portal vein, which is the vein that carries blood to the liver. By far, the most common cause of portal hypertension is cirrhosis. Normally, the liver is a soft organ, and blood flows through it very easily. With cirrhosis, the liver becomes hard and blood cannot flow easily, so it backs up and pressure increases in the portal vein.
The second most common cause is portal vein thrombosis, when there is a clot in a part of the portal vein before the liver. This results in a prehepatic type of portal hypertension. The liver is healthy, but the clot is an obstruction, and pressure increases in the portion of the portal vein that is proximal to the clot. In cirrhosis, the obstruction is the liver itself.
G&H How do patients with portal hypertension typically present?
GG-T A typical presentation involves varices or variceal bleeding. Vessels in the esophagus, known as varices, normally carry blood into the portal system, but with portal hypertension, these vessels enlarge and carry blood away from the portal vein. These vessels may rupture, causing the patient to vomit blood. A more common, but more ominous, presentation of cirrhosis with portal hypertension is the development of fluid in the abdomen, referred to as ascites. Once the patient presents with variceal bleeding or ascites, the patient’s cirrhosis has decompensated.
G&H How is portal hypertension currently measured?
GG-T All of the research to date has measured portal pressure by determining the hepatic venous pressure gradient (HVPG), although this approach is invasive. A needle is placed in the jugular vein, and pressure is measured in the liver sinusoids. This indirect measure is used because accessing the portal vein directly is very difficult.
G&H What is the current understanding of clinically significant portal hypertension?
GG-T Clinically significant portal hypertension is defined as an HVPG equal to or higher than 10 mm Hg, mild portal hypertension as 6 to less than 10 mm Hg, and normal pressure as 3 to 5 mm Hg. Patients with mild portal hypertension are unlikely to decompensate, whereas patients with clinically significant portal hypertension are more likely to decompensate (ie, they develop ascites; bleed from varices; or develop encephalopathy, which is when ammonia is not cleared by the liver because it escapes through collateral veins, causing the patient to become confused).
G&H Have there been any recent changes in the treatment paradigm of patients with cirrhosis and portal hypertension?
GG-T There may now be a new treatment approach. In the past, when cirrhosis was diagnosed, the next step was to perform an endoscopy to determine whether the patient had varices. Patients with large varices were treated via banding of the varices or with nonselective beta blockers because the varices were likely to bleed. The main goal was to prevent variceal hemorrhage, and no measures were used to prevent the other 2 decompensating events, ascites or encephalopathy. A seminal randomized, placebo-controlled study was published last year, the PREDESCI trial, which showed that nonselective beta blockers prevent decompensation (mainly ascites) in patients with clinically significant portal hypertension. This concept will likely lead to a paradigm shift. Now, when a diagnosis of cirrhosis is made, the next step is to determine whether the patient has clinically significant portal hypertension and, if so, to start nonselective beta blockers to prevent decompensation.
G&H How effective are nonselective beta blockers in patients with portal hypertension?
GG-T These agents are very effective, although they do not decrease portal pressure in all patients. In the PREDESCI trial, investigators used the beta blockers propranolol and carvedilol and adjusted their doses based on heart rate and blood pressure. Carvedilol is a much more potent nonselective beta blocker because it has additional alpha-adrenergic blocking effects. In the trial, one-third of patients received carvedilol, while two-thirds received propranolol. Patients who received carvedilol had a greater portal pressure–reducing effect and had better outcomes.
G&H What have other studies reported thus far regarding which nonselective beta blocker is most effective in this setting?
GG-T Several investigational studies have shown that carvedilol is more effective than propranolol at lowering HVPG. However, carvedilol lowers the mean arterial pressure much more than propranolol. Thus, if an individual taking carvedilol has low blood pressure, as is often the case with a decompensated patient, he or she is more likely to become hypotensive. This is the main concern with using carvedilol. On the other hand, there is no issue with carvedilol use in compensated patients, as their blood pressure is typically normal.
G&H What is the current role of portosystemic shunting procedures in patients with portal hypertension?
GG-T It is important to emphasize that portosystemic shunts such as the transjugular intrahepatic portosystemic shunt (TIPS) procedure should never be used in compensated patients, as this will divert blood flow away from the liver and could actually lead to decompensation in a patient who is otherwise doing well. In contrast, decompensated patients may need to urgently decompress portal pressure because they may be bleeding massively from varices. In these decompensated patients, the TIPS procedure could be life-saving.
G&H When should the TIPS procedure be used in decompensated patients?
GG-T In general, the TIPS procedure is second-line therapy for variceal hemorrhage or ascites in patients with decompensated cirrhosis. That is, it is performed when bleeding or ascites are not responding to standard of care. Having said that, doctors probably have been waiting too long to use the TIPS procedure. It should not be used too late, but it should also not be used too early, when it may divert blood flow away from the liver. The ideal timing is still being debated. I think doctors are starting to consider the TIPS procedure earlier on now. I would not wait for a patient to bleed for the third time; once a patient bleeds a second time, I would turn to the TIPS procedure. The current indications and timing of the TIPS procedure were recently discussed at an expert consensus conference by the ALTA (Advancing Liver Therapeutic Approaches) Consortium and are expected to be published soon.
G&H Does there appear to be a role for statins in the management of portal hypertension?
GG-T Statins can dilate the vessels that are inside the liver and that are constricted. There are experimental studies and proof-of-concept studies in patients with cirrhosis showing that statins lower portal pressure while improving flow to the liver. However, there is a lack of randomized clinical trials that show that statins can prevent decompensation. There is currently an ongoing multicenter, randomized, controlled Veterans Affairs study investigating the use of statins in compensated cirrhosis with the objective of preventing decompensation. The National Institutes of Health has recently announced a research project cooperative agreement looking at trials on statins for this use.
G&H What other research is being conducted in this field?
GG-T As previously mentioned, measurement of HVPG is invasive. Many investigations are looking at noninvasive methods to determine who has or does not have clinically significant portal hypertension. For example, some research is examining noninvasive assessment of liver stiffness because the stiffer the liver, the higher the portal pressure. Another method being studied to determine whether a patient has clinically significant portal hypertension is measuring the platelet count in combination with liver stiffness measurement.
In addition to looking for other ways of reducing portal pressure, there has also been much discussion on the preemptive use of the TIPS procedure. This involves placement of the TIPS procedure in patients admitted with variceal bleeding who respond to standard of care but are at a high risk of rebleeding during the admission. In these patients, rather than wait to use the TIPS procedure when the patient rebleeds, it would be used preemptively. There is controversy over which patients are candidates for doing this, so further research is needed.
Finally, we are looking forward to the upcoming Baveno VII Consensus Conference, which will take place in less than a year. New guidelines will be developed for portal hypertension that will include the use of nonselective beta blockers in patients with clinically significant portal hypertension (without having to perform an endoscopy) and the indications for preemptive use of the TIPS procedure.
Disclosures
Dr Garcia-Tsao has no relevant conflicts of interest to disclose.
Suggested Reading
Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the Study of Liver Diseases. Hepatology . 2017;65(1):310-335.
Mandorfer M, Hernández-Gea V, García-Pagán JC, Reiberger T. Noninvasive diagnostics for portal hypertension: a comprehensive review. Semin Liver Dis . 2020;40(3):240-255.
Turco L, Garcia-Tsao G. Portal hypertension: pathogenesis and diagnosis. Clin Liver Dis . 2019;23(4):573-587.
Villanueva C, Albillos A, Genescà J, et al. β blockers to prevent decompensation of cirrhosis in patients with clinically significant portal hypertension (PREDESCI): a randomised, double-blind, placebo-controlled, multicentre trial. Lancet . 2019;393(10181):1597-1608.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Hepatol
- v.2012; 2012

Clinical Manifestations of Portal Hypertension
Said a. al-busafi.
1 Department of Medicine, College of Medicine and Health Sciences, Sultan Qaboos University, P.O. Box 35, 123 Muscat, Oman
2 Department of Gastroenterology, Royal Victoria Hospital, McGill University Health Center, Montreal, QC, Canada H3A 1A1
Julia McNabb-Baltar
Amanda farag.
3 Department of Medicine, Royal Victoria Hospital, McGill University Health Center, Montreal, QC, Canada H3A 1A1
Nir Hilzenrat
4 Department of Gastroenterology, Jewish General Hospital, McGill University, Montreal, QC, Canada
The portal hypertension is responsible for many of the manifestations of liver cirrhosis. Some of these complications are the direct consequences of portal hypertension, such as gastrointestinal bleeding from ruptured gastroesophageal varices and from portal hypertensive gastropathy and colopathy, ascites and hepatorenal syndrome, and hypersplenism. In other complications, portal hypertension plays a key role, although it is not the only pathophysiological factor in their development. These include spontaneous bacterial peritonitis, hepatic encephalopathy, cirrhotic cardiomyopathy, hepatopulmonary syndrome, and portopulmonary hypertension.
1. Introduction
Portal hypertension (PH) is a common clinical syndrome defined as the elevation of hepatic venous pressure gradient (HVPG) above 5 mm Hg. PH is caused by a combination of two simultaneous occurring hemodynamic processes: (1) increased intrahepatic resistance to passage of blood flow through the liver due to cirrhosis and (2) increased splanchnic blood flow secondary to vasodilatation within the splanchnic vascular bed. PH can be due to many different causes at prehepatic, intrahepatic, and posthepatic sites ( Table 1 ). Cirrhosis of the liver accounts for approximately 90% of cases of PH in Western countries.
Causes of portal hypertension (PH).
The importance of PH is defined by the frequency and severity of its complications including variceal bleeding, spontaneous bacterial peritonitis, and hepatorenal syndrome, which represent the leading causes of death and of liver transplantation in patients with cirrhosis. PH is considered to be clinically significant when HVPG exceeds 10 to 12 mm Hg, since this is the threshold for the clinical complications of PH to appear [ 1 ]. Proper diagnosis and management of these complications are vital to improving quality of life and patients' survival. This paper will review the multisystemic manifestations of PH in cirrhosis.
2. Gastrointestinal Manifestations
2.1. gastroesophageal (ge) varices.
Approximately 5–15% of cirrhotics per year develop varices, and it is estimated that the majority of patients with cirrhosis will develop GE varices over their lifetime. The presence of GE varices correlates with the severity of liver disease; while only 40% of child A patients have varices, they are present in 85% of child C patients ( Table 2 ) [ 2 ].
Child-Pugh-Turcotte (CPT) Classification of the Severity of Cirrhosis.
Collaterals usually exist between the portal venous system and the systemic veins. The resistance in the portal vessels is normally lower than in the collateral circulation, and so blood flows from the systemic bed into the portal bed. However, when PH develops, the portal pressure is higher than systemic venous pressure, and this leads to reversal of flow in these collaterals. In addition, the collateral circulatory bed also develops through angiogenesis and the development of new blood vessels in an attempt to decompress the portal circulation [ 3 ]. The areas where major collaterals occur between the portal and systemic venous system are shown in Table 3 . Unfortunately these collaterals are insufficient to decompress the PH, leading to complications including variceal bleeding.
Location and blood vessels of collaterals between the portal and systemic venous circulations.
GE area is the main site of formation of varices [ 4 ]. Esophageal varices (EV) form when the HVPG exceeds 10 mm Hg [ 5 ]. In the lower 2 to 3 cm of the esophagus, the varices in the submucosa are very superficial and thus have thinner wall. In addition, these varices do not communicate with the periesophageal veins and therefore cannot easily be decompressed. These are the reasons why EV bleeds only at this site.
Over the last decade, most practice guidelines recommend to screen known cirrhotics with endoscopy to look for GE varices. Varices should be suspected in all patients with stigmata of chronic liver disease such as spider nevi, jaundice, palmar erythema, splenomegaly, ascites, encephalopathy, and caput medusae. EV are graded as small (<5 mm) and large (>5 mm), where 5 mm is roughly the size of an open biopsy forceps [ 6 ].
The rate of progression of small EV to large is 8% per year [ 2 ]. Decompensated cirrhosis (child B or C), presence of red wale marks (defined as longitudinal dilated venules resembling whip marks on the variceal surface), and alcoholic cirrhosis at the time of baseline endoscopy are the main factors associated with the progression from small to large EV [ 2 ]. EV bleeding occurs at a yearly rate of 5%–15% [ 7 ]. The predictors of first bleeding include the size of varices, severity of cirrhosis (Child B or C), variceal pressure (>12 mm Hg), and the endoscopic presence of red wale marks [ 7 , 8 ]. Although EV bleeding stops spontaneously in up to 40% of patients, and despite improvements in therapy over the last decade, the 6 weeks mortality rate is still ≥20% [ 9 ].
Gastroesophageal varices (GOV) are an extension of EV and are categorized based on Sarin's classification into 2 types ( Figure 1 ). The most common are Type 1 (GOV1) varices, which extend along the lesser curvature. Type 2 GOV (GOV2) are those that extend along the fundus. They are longer and more tortuous than GOV1. Isolated gastric varices (IGV) occur in the absence of EV and are also classified into 2 types. Type 1 (IGV1) are located in the fundus and tend to be tortuous and complex, and type 2 (IVG2) are located in the body, antrum, or around the pylorus. When IGV1 is present, one must exclude splenic vein thrombosis. GV are less common than EV and are present in 5%–30% of patients with PH with a reported incidence of bleeding of about 25% in 2 years, with a higher bleeding incidence for fundal varices [ 10 ]. Predictors of GV bleeding include the size of fundal varices (large (>10 mm) > medium (5–10 mm) > small (<5 mm)), severity of cirrhosis (child class C>B>A), and endoscopic presence of variceal red spots (defined as localized reddish mucosal area or spots on the mucosal surface of a varix) [ 11 ].

Sarin classification of gastric varices.
2.2. Ectopic Varices (EcV)
EcV are best defined as large portosystemic venous collaterals occurring anywhere in the abdomen except for the GE region [ 12 ]. They are an unusual cause of GI bleeding, but account for up to 5% of all variceal bleeding [ 13 ]. Compared to GE varices, EcV are difficult to locate, occur at distal sites, and when identified, the choice of therapy is unclear, therefore representing a clinical challenge [ 12 ]. Furthermore, bleeding EcV may be associated with poor prognosis, with one study quoting mortality reaching 40% [ 14 ]. Different areas of EcV are the duodenum, jejunum, ileum, colon, rectum, peristomal, biliary tree, gallbladder, peritoneum, umbilicus, bare area of the liver, ovary, vagina, and testis [ 15 , 16 ].
The prevalence of EcV varies in the literature and seems to be related to the etiology of the PH and the diagnostic modalities used [ 17 ]. In patients with PH due to cirrhosis, duodenal varices are seen in 40% of patients undergoing angiography [ 18 ]. Results of a survey for EcV conducted over 5 years in Japan identified 57 cases of duodenal varices; they were located in the duodenal bulb in 3.5%, the descending part in 82.5%, and the transverse part in 14.0% [ 15 ].
In contrast to duodenal varices, it appears that most cases of varices in other portions of the small bowel and colonic varices are seen in patients with cirrhosis who have previously undergone abdominal surgery [ 12 ]. Using advanced endoscopic technologies, particularly capsule endoscopy and enteroscopy, the prevalence of small bowel varices is estimated to be approximately 69% in patients with PH [ 19 ]. The prevalence of colonic varices and rectal varices has been found to be 34% to 46% [ 20 , 21 ] and 10% to 40% [ 22 ], respectively, in patients with cirrhosis undergoing colonoscopy. It is important to differentiate rectal varices from hemorrhoids; rectal varices extend more than 4 cm above the anal verge, are dark blue in color, collapse with digital pressure, and do not prolapse into the proctoscope on examination, whereas hemorrhoids do not extend proximal to the dentate line, are purple in color, do not collapse with digital pressure, and often prolapse into the proctoscope [ 22 , 23 ]. Stomal varices are a particularly common cause of EcV and can occur in patients with cirrhosis secondary to primary sclerosing cholangitis (PSC) [ 12 ].
In the west, because the prevalence of noncirrhotic PH is low, most bleeding EcV is usually associated with cirrhotic PH (6,8). Although EcV can occur at several sites, bleeding EcV are most commonly found in the duodenum and at sites of previous bowel surgery including stomas.
In a review of 169 cases of bleeding EcV, 17% occurred in the duodenum, 17% in the jejunum or ileum, 14% in the colon, 8% in the rectum, and 9% in the peritoneum. In the review, 26% bled from stomal varices and a few from infrequent sites such as the ovary and vagina [ 24 ].
Portal biliopathy, which includes abnormalities (stricture and dilatation) of both extra and intrahepatic bile ducts and varices of the gallbladder, is associated with PH, particularly extrahepatic portal vein obstruction [ 25 , 26 ]. They are also seen associated with cirrhosis, non-cirrhotic portal fibrosis, and congenital hepatic fibrosis [ 27 ]. While a majority of these patients are asymptomatic, some present with a raised alkaline phosphatase level, abdominal pain, fever, and cholangitis. Choledocholithiasis may develop as a complication and manifest as obstructive jaundice with or without cholangitis [ 26 ]. On cholangiography, bile-duct varices may be visualized as multiple, smooth, mural-filling defects with narrowing and irregularity resulting from compression of the portal vein and collateral vessels. They may mimic PSC or cholangiocarcinoma (pseudocholangiocarcinoma sign) [ 28 ].
2.3. Portal Hypertensive Intestinal Vasculopathies
Mucosal changes in the stomach in patients with PH include portal hypertensive gastropathy (PHG) and gastric vascular ectasia. PHG describes the endoscopicappearance of gastric mucosa with a characteristic mosaic, or snake-skin-like appearance with or without red spots. It is a common finding in patients with PH [ 29 ]. The prevalence of PHG parallels the severity of PH and it is considered mild when only a mosaic-like pattern is present and severe when superimposed discrete red spots are also seen. Bleeding (acute or chronic) from these lesions is relatively uncommon, and rarely severe [ 30 ]. Patients with chronic bleeding usually present with chroniciron deficiency anemia.
In gastric vascular ectasia, collection of ectatic vessels can be seen on endoscopy as red spots without a mosaic-like pattern [ 31 ]. When the aggregates are confined to the antrum of the stomach, the term gastric antral vascular ectasia (GAVE) is used, and if aggregates in the antrum are linear, the term watermelon stomach is used to describe the lesion. The prevalence of GAVE syndrome in cirrhosis is low [ 32 ] and can be endoscopically difficult to differentiate from severe PHG. Therefore, gastric biopsy may be required to differentiate them as histologically GAVE lesions are completely distinct from PHG ( Table 4 ) [ 33 ].
Comparison of portal hypertensive gastropathy (PHG) and gastric antral vascular ectasia (GAVE).
PH: portal hypertension, TIPS: transjugular intrahepatic portosystemic shunt.
Small bowel might also show mucosal changes related to PH, which is called portal hypertensive enteropathy (PHE). The diagnosis of PHE has been limited in the past due to the difficult access to the small bowel. With advanced endoscopic techniques such as capsule endoscopy and enteroscopy, PHE is now thought to be a frequent finding in patients with cirrhosis, perhaps as common as PHG, and may cause occult GI blood loss [ 34 , 35 ].
Portal hypertensive colopathy (PHC) refers to mucosal edema, erythema, granularity, friability, and vascular lesions of the colon in PH. PHC may be confused with colitis [ 36 , 37 ]. Although they are found in up to 70% of patients with PH and are more common in patients with EV and PHG, they rarely cause bleeding [ 38 , 39 ].

2.4. Ascites and Spontaneous Bacterial Peritonitis (SBP)
Ascites is defined as the accumulation of free fluid in the peritoneal cavity. Cirrhotic PH is the most common cause of ascites, which accounts for approximately 75% patients with ascites. About 60% of patients with cirrhosis develop ascites during 10 years of observation [ 40 ]. The development of ascites is an important event in cirrhosis as the mortality is approximately 50% at 2 years without a liver transplantation [ 41 ]. The formation of ascites in cirrhosis is due to a combination of abnormalities in both renal function and portal and splanchnic circulation. The main pathogenic factor is sodium retention [ 42 ].
The main clinical symptom of patients with ascites is an increase in abdominal girth, often accompanied by lower-limb edema. In some cases, the accumulation of fluid is so severe that respiratory function and physical activity is impaired. In most cases, ascites develop insidiously over the course of several weeks. Patients must have approximately 1500 mL of fluid for ascites to be detected reliably by physical examination. Dyspnea in these patients can occur as a consequence of increasing abdominal distension and/or accompanying pleural effusions. Increased intra-abdominal pressure might favour the development of abdominal hernias (mainly umbilical) in patients with cirrhosis and longstanding ascites [ 43 ].
The current classification of ascites, as defined by the International Ascites Club, divides patients in three groups ( Table 5 ) [ 44 ]. Patients with refractory ascites are those that do not respond to sodium restriction and high doses of diuretics or develop diuretic-induced side effects that preclude their use.
International ascites club grading system for ascites.
Ascites may not be clinically detectable when present in small volumes. In larger volumes, the classic findings of ascites are adistended abdomen with a fluid thrill or shifting dullness. Ascites must be differentiated from abdominal distension due to other causes such as obesity, pregnancy, gaseous distension of bowel, bladder distension, cysts, and tumours. Ultrasonography is used to confirm the presence of minimal ascites and guide diagnostic paracentesis.
Successful treatment depends on an accurate diagnosis of the cause of ascites. Paracentesis with analysis of ascitic fluid is the most rapid and cost-effective method of diagnosis. It should be done in patients with ascites of recent onset, cirrhotic patients with ascites admitted to hospital, or those with clinical deterioration. The most important analyses are cell count, fluid culture, and calculation of the serum: ascites albumin gradient (SAAG), which reflects differences in oncotic pressures and correlates with portal venous pressure. It SAAG is greater or equal to 1.1 g/dL (or 11 g/L), ascites is ascribed to PH with approximately 97% accuracy [ 45 ].
Patients with cirrhosis and ascites are also at risk of developing infections, particularly spontaneous bacterial peritonitis (SBP). SBP occurs in approximately 10% of hospitalized cirrhotic patients [ 46 ], with an associated mortality of 20–40% if untreated [ 47 ]. Many patients are asymptomatic, but clinical signs can include abdominal pain, fever, and diarrhea. The diagnosis of SBP is based on neutrophil count >250 cells/mm 3 in the ascitic fluid.
3. Renal Manifestations
3.1. hepatorenal syndrome.
Hepatorenal syndrome (HRS) is a common complication seen in patients with advanced cirrhosis and PH [ 48 ]. HRS can also be seen in other types of severe chronic liver disease, alcoholic hepatitis, or in acute liver failure. This syndrome generally predicts poor prognosis [ 48 ]. HRS has been defined in the literature as a reversible functional renal impairment in the absence of other causes of renal failure, tubular dysfunction, proteinuria, or morphological alterations in histological studies. Precise and accurate diagnostic criteria have been established in order to clearly define this syndrome ( Table 6 ) [ 49 ]. The diagnosis remains one of exclusion.
Revised diagnostic criteria of Hepatorenal syndrome.
The reported incidence of HRS is approximately 10% among hospitalized patients with cirrhosis and ascites. The probability of occurrence of HRS in patients with cirrhosis is around 20% after 1 year and 40% after 5 years [ 50 ]. The pathogenesis of HRS is not completely understood, but is likely the result of an extreme underfilling of the peripheral arterial circulation secondary to arterial vasodilatation in the splanchnic circulation [ 51 ]. In addition, recent data indicates that a reduction in cardiac output also plays a significant role [ 52 ].
HRS-associated renal failure is seen in late stages of cirrhosis and is marked by severe oliguria, increased sodium and water retention, volume overload, hyperkalemia, and spontaneous dilutional hyponatremia. There are two main subtypes of HRS described [ 49 ]. Type 1 HRS is a rapidly progressive renal failure that is defined by doubling of serum creatinine >2.5 mg/dL (>221 μ moL/L) or a decrease of 50% in creatinine clearance (<20 mL/min) in less than 2 weeks. This form of HRS is usually precipitated by gastrointestinal bleeds, large volume paracenthesis, acute alcoholic hepatitis and SBP [ 53 ]. In addition to renal failure, patients with type 1 HRS present deterioration in the function of other organs, including the heart, brain, liver, and adrenal glands. The median survival of these patients without treatment is <2 weeks, and almost all of them die within 10 weeks after onset of HRS. Type 2 HRS is a moderate and stable renal failure with a serum creatinine of >1.5 mg/dL (>133 μ moL/L) that remains stable over a longer period and is characterized by diuretics resistant ascites [ 49 , 54 ].
4. Neurological Manifestations
4.1. hepatic encephalopathy.
Hepatic encephalopathy (HE) is defined as neurologic and psychiatric dysfunction in a patient with chronic liver disease. The exact mechanism leading to this dysfunction is still poorly understood, but multiple factors appear to play a role in its genesis. The liver normally metabolizes ammonia, produced by enteric bacteria [ 56 ] and enterocytes [ 57 , 58 ]. In a patient with PH, ammonia bypasses the liver through portosystemic shunt and reaches the astrocytes in the brain. Within the astrocyte, ammonia is metabolized into glutamine, which acts as an osmole to attract water, thus causing cerebral edema. In addition, direct ammonia toxicity triggers nitrosative and oxidative stress, which lead to astrocyte mitochondrial dysfunction [ 59 , 60 ]. Another important factor is the enhancement of gamma-aminobutyric acid (GABA-A) receptors through neuroinhibitory steroids (i.e., allopregnanolone) [ 61 ] and benzodiazepine. Benzodiazepine also contributes to astrocyte swelling through a specific receptor [ 62 ]. Finally, tryptophane byproducts indole and oxindole [ 63 ], manganese [ 64 ], inflammation, hyponatremia [ 65 ], and reduced acetylcholine through acetylcholinesterase activity [ 66 ] also contribute to cerebral dysfunction.
The clinical manifestations of HE can be subtle. Minimal hepatic encephalopathy (grade 0) ( Table 7 ) can present with impaired driving ability [ 67 ], minimally impaired psychometric tests, decreased global functioning, and increased risk of falls [ 68 ]. In overt hepatic encephalopathy, diurnal sleep pattern changes will often precede neurologic symptoms. To add to the complexity, HE can be intermittent or persistent.
West Haven Criteria of Severity of Hepatic Encephalopathy (Adapted with permission [ 55 ]).
The severity of presentation is usually classified using the West Haven criteria ( Table 7 ). Grade 1 hepatic encephalopathy represents lack of awareness, anxiety or euphoria, and short attention span. Change of personality, lethargy, and inappropriate behavior can be seen in grade 2 encephalopathy. More advanced features include disorientation, stupor, confusion (grade 3), and can even reach coma (grade 4). Focal neurologic symptoms, including hemiplegia, may also be observed [ 69 ]. Physical examination may be normal, but typical signs include bradykinesia, asterixis, hyperactive deep tendon reflexes and even decerebrate posturing [ 55 ].
5. Pulmonary Manifestations
5.1. hepatopulmonary syndrome.
Hepatopulmonary syndrome (HPS) is a triad of liver disease, pulmonary vascular ectasia and impaired oxygenation. HPS is defined in the literature as a widened alveolar-arterial oxygen difference (A-a gradient) in room air (>15 mm Hg or >20 mm Hg in patients > 64 years of age) with or without hypoxemia due to intrapulmonary vasodilatation in the presence of hepatic dysfunction [ 70 , 71 ]. This syndrome occurs mostly in those with PH (with or without cirrhosis) and indicates poor prognosis and higher mortality. Estimates of the prevalence of HPS among patients with chronic liver disease range from 4 to 47%, depending upon the diagnostic criteria and methods used [ 71 – 73 ].
HPS results in hypoxemia through pulmonary microvascular vasodilatation and intrapulmonary arteriovenous shunting resulting in ventilation-perfusion mismatch [ 74 ], and can occur even with mild liver disease [ 75 ]. Clinically, patients with HPS complain of progressive dyspnea on exertion, at rest, or both. Severe hypoxemia (PaO 2 < 60 mm Hg) is often seen and strongly suggests HPS [ 70 , 71 ]. A classical finding in HPS is orthodeoxia defined as a decreased arterial oxygen tension by more than 4 mm Hg or arterial oxyhemoglobin desaturation by more than 5% with changing position from supine to standing. It is associated with platypnea defined as dyspnea worsened by upright position [ 70 , 71 ]. Platypnea-orthodeoxia is caused by the worsening of diffusion-perfusion matching and increased shunting at the lung bases in the upright position. There are no hallmark signs on physical exam; however, cyanosis, clubbing, and cutaneous telangiectasia (spider nevi) are commonly noted. Furthermore, systemic arterioembolisation may cause stroke, cerebral hemorrhage, or brain abscess, and can present with neurological deficits.
5.2. Portopulmonary Hypertension
Portopulmonary hypertension (PPH), a well-recognized complication of chronic liver disease, refers to pulmonary arterial hypertension (PAH) associated with PH when no alternative causes exist. It is defined by the presence of elevated pulmonary arterial pressure (mean pressure >25 mm Hg at rest and 30 mm Hg on exertion) elevated pulmonary vascular resistance (>240 dyne s −1 cm −5 ) in the presence of a pulmonary capillary wedge pressure <15 mm Hg [ 76 ].
The prevalence of PPH depends on the patient population studies and severity of the liver disease, 0.7–2% and 3.5–16.1% in cirrhotics and patients undergoing liver transplantation, respectively. The development of PPH is independent of the cause of PH, and it is often seen in cirrhosis. It is however, also described in those with PH due to nonhepatic pathologies such as portal venous thrombosis [ 71 , 77 ]. PH seems to be the driving force of PAH. The pathogenesis of PPH is not completely understood; however, several theories have been offered. The most widely accepted theory is that a humoral vasoactive substances (e.g., serotonin, endothelin-1, interleukin-1, thromboxane B2, and secretin), normally metabolized by the liver, is able to reach the pulmonary circulation via portosystemic shunts, resulting in PPH [ 71 , 78 , 79 ].
Clinically, most patients with PPH present with evidence of both PAH and PH. Typically manifestations of PH precede those of PAH. The most common presenting symptom is progressive dyspnea on exertion [ 80 ] and less frequently fatigue, palpitations, syncope, hemoptysis, orthopnea, and chest pain. On physical exam, classical features include edema, an accentuated P2 and a systolic murmur, indicating tricuspid regurgitation [ 71 , 77 , 80 ]. In severe cases, signs and symptoms of right-heart failure can be noted.
5.3. Hepatic Hydrothorax
Hepatic hydrothorax is an uncommon complication of end-stage liver disease. It is defined as a pleural effusion greater than 500 mL in patients with cirrhosis in absence of primary cardiac, pulmonary, or pleural disease [ 81 ]. The underlying pathogenesis of hepatic hydrothorax is incompletely understood. Patients with cirrhosis and PH have abnormal extracellular fluid volume regulation resulting in passage of ascites from the peritoneal space to the pleural cavity via diaphragmatic defects generally in the tendinous portion of the diaphragm [ 82 ]. Negative intrathoracic pressure during inspiration pulls the fluid from the intra-abdominal cavity into the pleural cavity. Hydrothorax develops when the pleural absorptive capacity is surpassed, leading to accumulation of fluid in the pleural space. Multiple studies have shown the passage of fluid from the intra-abdominal space to the pleural space via 99mTc-human albumin or 99mTc-sulphur colloid [ 81 ].
Clinical manifestations of hepatic hydrothorax include shortness of breath, cough, hypoxemia, and chest discomfort [ 81 ]. Ascites may not always be present. Hepatic hydrothorax should always be suspected in patients with cirrhosis or PH and undiagnosed pleural effusion, regardless of the presence of ascites. Serious complications include acute tension hydrothorax with dyspnoea and hypotension [ 83 ] and spontaneous bacterial empyema [ 84 ].
6. Other Organs Manifestations
6.1. cirrhotic cardiomyopathy.
Cirrhotic cardiomyopathy is defined as a chronic cardiac dysfunction in patients with cirrhosis. It occurs in up to 50% of patients with advanced cirrhosis. It is characterized by impaired contractile response and/or altered diastolic relaxation in the absence of other cardiac diseases. The pathophysiology of this condition is complex, and seemingly related to PH and cirrhosis. In advanced liver disease, splanchnic vasodilatation leads to a resting hyperdynamic state [ 85 ]. Plasma volume expands, leading to a relative central volume decrease [ 86 ]. In cirrhosis, the arterial vessel wall thickness and tone decreases, leading to reduced arterial compliance [ 87 , 88 ]. Autonomic dysfunction may also contribute to blunted cardiac response [ 89 ]. Ultimately, these factors lead to systolic and diastolic dysfunction.
Symptoms associated with cirrhotic cardiomyopathy include dyspnea with exertion, impaired exercise capacity, paroxysmal nocturnal dyspnea, peripheral edema, and orthopnea. Less-frequent presentations include long QT on electrocardiography, arrhythmia, and sudden death [ 90 ].
6.2. Hepatic Osteodystrophy
Hepatic osteodystrophy is defined as bone disease (osteomalacia, osteoporosis, and osteopenia) associated with liver disease. Osteomalacia and osteoporosis are frequently seen in cirrhotic patients and can predispose to pathologic fractures. The pathophysiology of osteoporosis in liver disease is relatively complex. The leading hypothesis suggests that it is related to the uncoupling of osteoblastic and osteoclastic activity. Osteoclastogenic proinflammatory cytokines (interleukin 1(Il-1) and tumor necrosis factor α (TNF α )) are increased in hepatic fibrosis. Moreover, TNF α is increased in a rat model of PH [ 91 ]. Decreased osteoblastic activity has also been linked with insulin-like growth factor 1 in a rat model (IGF-1). Increasing IGF-1 levels are associated with liver disease severity [ 92 ]. Finally, vitamin K mediates the carboxylation of glutamyl residues on osteocalcin, stimulating osteoclastic activity [ 93 ].
Patients with osteoporosis are usually asymptomatic. They may present with pain following a nontraumatic fracture of the axial skeleton or bone deformity, including pronounced cervical kyphosis. Osteomalacia presentation is similar and includes proximal muscle weakness [ 94 ].
6.3. Hypersplenism
Hypersplenism is a common complication of massive congestive splenomegaly in patients with cirrhosis and PH. In this condition, splenomegaly is associated with thrombocytopenia, leucopenia, or anemia or a combination of any the three [ 95 , 96 ]. Severe hypersplenism is present in about 1/3 of patients with cirrhosis being assessed for liver transplantation. Most patients have no symptoms related to hypersplenism, however severe thrombocytopenia may increase the risk of bleeding, especially after invasive procedures.
7. Conclusion
Portal hypertension secondary to cirrhosis has multisystem effects and complications. Once a patient develops such complications, they are considered to have decompensated disease with the high morbidity and mortality. The quality of life and survival of patients with cirrhosis can be improved by the prevention and treatment of these complications.
Achieve Mastery of Medical Concepts
Study for medical school and boards with lecturio.
USMLE Step 1 | USMLE Step 2 | COMLEX Level 1 | COMLEX Level 2 | ENARM | NEET
Portal Hypertension
Portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension is increased pressure in the portal venous system. This increased pressure can lead to splanchnic vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs , collateral blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure through portosystemic anastomoses Portosystemic anastomoses Systemic and Special Circulations , and increased hydrostatic pressure Hydrostatic pressure The pressure due to the weight of fluid. Edema . There are a number of etiologies, including cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis , right-sided heart failure Right-Sided Heart Failure Ebstein’s Anomaly , schistosomiasis Schistosomiasis Infection with flukes (trematodes) of the genus schistosoma. Three species produce the most frequent clinical diseases: Schistosoma haematobium (endemic in Africa and the Middle East), Schistosoma Mansoni (in Egypt, northern and southern Africa, some West Indies islands, northern 2/3 of South america), and Schistosoma japonicum (in Japan, China, the Philippines, Celebes, Thailand, Laos). S. mansoni is often seen in Puerto Ricans living in the United States. Schistosoma/Schistosomiasis , portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus , hepatitis, and Budd-Chiari syndrome Budd-Chiari syndrome Budd-Chiari syndrome is a condition resulting from the interruption of the normal outflow of blood from the liver. The primary type arises from a venous process (affecting the hepatic veins or inferior vena cava) such as thrombosis, but can also be from a lesion compressing or invading the veins (secondary type). The patient typically presents with hepatomegaly, ascites, and abdominal discomfort. Budd-Chiari Syndrome . Most individuals are asymptomatic until complications arise, including esophageal varices, portal hypertensive gastropathy gastropathy Damage to the epithelial lining with no or minimal associated inflammation and is technically a separate entity from gastritis Gastritis , ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites , and hypersplenism Hypersplenism Condition characterized by splenomegaly, some reduction in the number of circulating blood cells in the presence of a normal or hyperactive bone marrow, and the potential for reversal by splenectomy. Splenomegaly . The diagnosis is clinical, but it can be supported by ultrasound findings (and hepatic venous pressure gradient Pressure gradient Vascular Resistance, Flow, and Mean Arterial Pressure measurement in unclear cases). Management requires treating the underlying etiology and managing the complications. This can include nonselective beta blockers to prevent bleeding from varices, diuretics Diuretics Agents that promote the excretion of urine through their effects on kidney function. Heart Failure and Angina Medication and sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia restriction for ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites , and transjugular intrahepatic portosystemic shunt Transjugular intrahepatic portosystemic shunt A type of surgical portosystemic shunt to reduce portal hypertension with associated complications of esophageal varices and ascites. It is performed percutaneously through the jugular vein and involves the creation of an intrahepatic shunt between the hepatic vein and portal vein. The channel is maintained by a metallic stent. The procedure can be performed in patients who have failed sclerotherapy and is an additional option to the surgical techniques of portocaval, mesocaval, and splenorenal shunts. It takes one to three hours to perform. Ascites for refractory complications.
Last updated: Jul 7, 2023
Etiology and Pathophysiology
Clinical presentation, clinical relevance.
Share this concept:
The etiologies of portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension can be classified based on the location of increased resistance Resistance Physiologically, the opposition to flow of air caused by the forces of friction. As a part of pulmonary function testing, it is the ratio of driving pressure to the rate of air flow. Ventilation: Mechanics of Breathing to blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure through the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy .
Prehepatic etiologies:
- Portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus
- Splenic vein thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus
- Massive splenomegaly Massive Splenomegaly Splenomegaly
- Splanchnic arteriovenous fistula Arteriovenous fistula An abnormal direct communication between an artery and a vein without passing through the capillaries. An a-v fistula usually leads to the formation of a dilated sac-like connection, arteriovenous aneurysm. The locations and size of the shunts determine the degree of effects on the cardiovascular functions such as blood pressure and heart rate. Vascular Surgery
Hepatic etiologies:
- Schistosomiasis Schistosomiasis Infection with flukes (trematodes) of the genus schistosoma. Three species produce the most frequent clinical diseases: Schistosoma haematobium (endemic in Africa and the Middle East), Schistosoma Mansoni (in Egypt, northern and southern Africa, some West Indies islands, northern 2/3 of South america), and Schistosoma japonicum (in Japan, China, the Philippines, Celebes, Thailand, Laos). S. mansoni is often seen in Puerto Ricans living in the United States. Schistosoma/Schistosomiasis
- Early primary biliary cholangitis Primary Biliary Cholangitis Primary biliary cholangitis (PBC) is a chronic disease resulting in autoimmune destruction of the intrahepatic bile ducts. The typical presentation is that of a middle-aged woman with pruritus, fatigue, and right upper quadrant abdominal pain. Elevated liver enzymes and antimitochondrial antibodies (AMAs) establish the diagnosis. Primary Biliary Cholangitis
- Granulomatous disease Granulomatous disease A defect of leukocyte function in which phagocytic cells ingest but fail to digest bacteria, resulting in recurring bacterial infections with granuloma formation. When chronic granulomatous disease is caused by mutations in the cybb gene, the condition is inherited in an X-linked recessive pattern. When chronic granulomatous disease is caused by cyba, ncf1, ncf2, or ncf4 gene mutations, the condition is inherited in an autosomal recessive pattern. Common Variable Immunodeficiency (CVID) (e.g., sarcoidosis Sarcoidosis Sarcoidosis is a multisystem inflammatory disease that causes noncaseating granulomas. The exact etiology is unknown. Sarcoidosis usually affects the lungs and thoracic lymph nodes, but it can also affect almost every system in the body, including the skin, heart, and eyes, most commonly. Sarcoidosis )
- Congenital Congenital Chorioretinitis hepatic fibrosis Hepatic fibrosis Autosomal Recessive Polycystic Kidney Disease (ARPKD)
- Polycystic liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease
- Idiopathic Idiopathic Dermatomyositis noncirrhotic portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension
- Cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis (most common cause in Western countries)
- Acute alcoholic Alcoholic Persons who have a history of physical or psychological dependence on ethanol. Mallory-Weiss Syndrome (Mallory-Weiss Tear) hepatitis
- Viral hepatitis
- Vitamin A Vitamin A Retinol and derivatives of retinol that play an essential role in metabolic functioning of the retina, the growth of and differentiation of epithelial tissue, the growth of bone, reproduction, and the immune response. Dietary vitamin A is derived from a variety of carotenoids found in plants. It is enriched in the liver, egg yolks, and the fat component of dairy products. Fat-soluble Vitamins and their Deficiencies intoxication
- Postsinusoidal: hepatic veno-occlusive disease
Posthepatic etiologies:
- Right-sided heart failure Right-Sided Heart Failure Ebstein’s Anomaly
- Severe tricuspid regurgitation Regurgitation Gastroesophageal Reflux Disease (GERD)
- Constrictive pericarditis Constrictive pericarditis Inflammation of the pericardium that is characterized by the fibrous scarring and adhesion of both serous layers, the visceral pericardium and the parietal pericardium leading to the loss of pericardial cavity. The thickened pericardium severely restricts cardiac filling. Clinical signs include fatigue, muscle wasting, and weight loss. Pericarditis
- Restrictive cardiomyopathy Restrictive Cardiomyopathy Restrictive cardiomyopathy (RCM) is a fairly uncommon condition characterized by progressive stiffening of the cardiac muscle, which causes impaired relaxation and refilling of the heart during diastole, resulting in diastolic dysfunction and eventual heart failure. Restrictive Cardiomyopathy
- Noncardiac: Budd-Chiari syndrome Budd-Chiari syndrome Budd-Chiari syndrome is a condition resulting from the interruption of the normal outflow of blood from the liver. The primary type arises from a venous process (affecting the hepatic veins or inferior vena cava) such as thrombosis, but can also be from a lesion compressing or invading the veins (secondary type). The patient typically presents with hepatomegaly, ascites, and abdominal discomfort. Budd-Chiari Syndrome
Pathophysiology
- Supplies 25% of the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy ’s blood supply
- Carries oxygenated blood
- Supplies 75% of blood supply
- Formed most commonly by the union of the splenic and superior mesenteric veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology
- Carries oxygen-poor, nutrient-rich blood drained from the abdominal organs
- Venous drainage: sinusoids Sinusoids Liver: Anatomy → central vein of each lobule → hepatic veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology → inferior vena cava Inferior vena cava The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy ( IVC IVC The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy )
- Alternative routes of circulation Circulation The movement of the blood as it is pumped through the cardiovascular system. ABCDE Assessment ensure venous drainage of the abdominal organs even if a blockage occurs in the portal system.
- Left gastric veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology and lower esophageal veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology
- Superior rectal veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology and inferior and middle rectal veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology
- Paraumbilical veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology and small epigastric veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology
- Intraparenchymal hepatic branches of right division of portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy and retroperitoneal Retroperitoneal Peritoneum: Anatomy veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology
- Omental and colonic veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology with retroperitoneal Retroperitoneal Peritoneum: Anatomy veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology
- Ductus venosus Ductus venosus Development of the Heart and the IVC IVC The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy
Portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension :
- Pathologically elevated pressure of the portal venous system (> 5 mm Hg higher than the IVC IVC The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy )
- Varices: ↑ collateral blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure through the portosystemic anastomoses Portosystemic anastomoses Systemic and Special Circulations
- ↑ Hydrostatic pressure Hydrostatic pressure The pressure due to the weight of fluid. Edema in the downstream hepatic vessels → fluid shift Fluid Shift Translocation of body fluids from one compartment to another, such as from the vascular to the interstitial compartments. Fluid shifts are associated with profound changes in vascular permeability and water-electrolyte imbalance. The shift can also be from the lower body to the upper body as in conditions of weightlessness. Volume Depletion and Dehydration from intravascular space to peritoneal cavity Peritoneal Cavity The space enclosed by the peritoneum. It is divided into two portions, the greater sac and the lesser sac or omental bursa, which lies behind the stomach. The two sacs are connected by the foramen of winslow, or epiploic foramen. Peritoneum: Anatomy
- ↑ Splanchnic vasodilation Vasodilation The physiological widening of blood vessels by relaxing the underlying vascular smooth muscle. Pulmonary Hypertension Drugs and blood pooling → ↓ arterial volume → ↓ renal blood flow Renal blood flow The amount of the renal blood flow that is going to the functional renal tissue, i.e., parts of the kidney that are involved in production of urine. Glomerular Filtration → RAAS RAAS A blood pressure regulating system of interacting components that include renin; angiotensinogen; angiotensin converting enzyme; angiotensin i; angiotensin ii; and angiotensinase. Renin, an enzyme produced in the kidney, acts on angiotensinogen, an alpha-2 globulin produced by the liver, forming angiotensin I. Angiotensin-converting enzyme, contained in the lung, acts on angiotensin I in the plasma converting it to angiotensin II, an extremely powerful vasoconstrictor. Angiotensin II causes contraction of the arteriolar and renal vascular smooth muscle, leading to retention of salt and water in the kidney and increased arterial blood pressure. In addition, angiotensin II stimulates the release of aldosterone from the adrenal cortex, which in turn also increases salt and water retention in the kidney. Angiotensin-converting enzyme also breaks down bradykinin, a powerful vasodilator and component of the kallikrein-kinin system. Adrenal Hormones activation → sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia and water retention
- Hypersplenism Hypersplenism Condition characterized by splenomegaly, some reduction in the number of circulating blood cells in the presence of a normal or hyperactive bone marrow, and the potential for reversal by splenectomy. Splenomegaly : ↑ splenic vein pressure
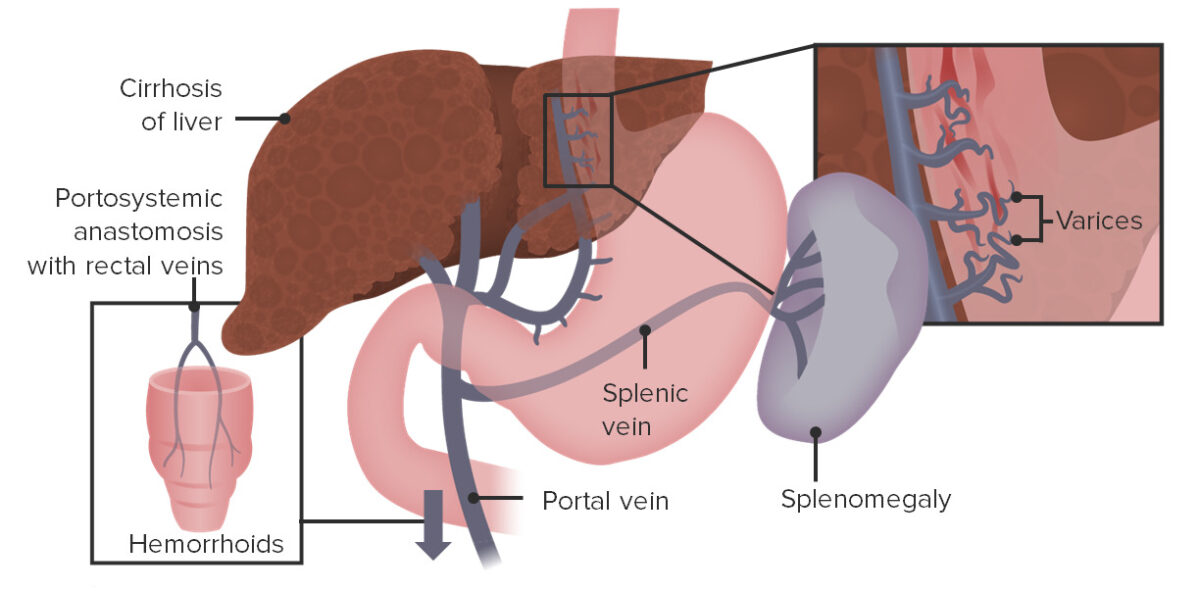
Esophageal varices, splenomegaly, and rectal varices resulting from backup of blood flow due to elevated pressures within the portal vein
Related videos
Portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension itself usually has no symptoms. Clinical manifestations arise as a result of the underlying etiology and/or complications.
Evidence of common complications
- Caput medusae Caput Medusae Abdominal Examination (engorged paraumbilical veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology )
- Esophageal varices (potentially life-threatening)
- Portal hypertensive gastropathy gastropathy Damage to the epithelial lining with no or minimal associated inflammation and is technically a separate entity from gastritis Gastritis (gastric mucosal vascular congestion)
- Bleeding from rectal varices
- Splenomegaly Splenomegaly Splenomegaly is pathologic enlargement of the spleen that is attributable to numerous causes, including infections, hemoglobinopathies, infiltrative processes, and outflow obstruction of the portal vein. Splenomegaly
- Pancytopenia Pancytopenia Deficiency of all three cell elements of the blood, erythrocytes, leukocytes and platelets. Aplastic Anemia
- Abdominal distention Abdominal distention Megacolon
- Shifting dullness Shifting dullness Change of resonance (from dull to tympanic) when patient changes from supine to lateral decubitus position. Ascites
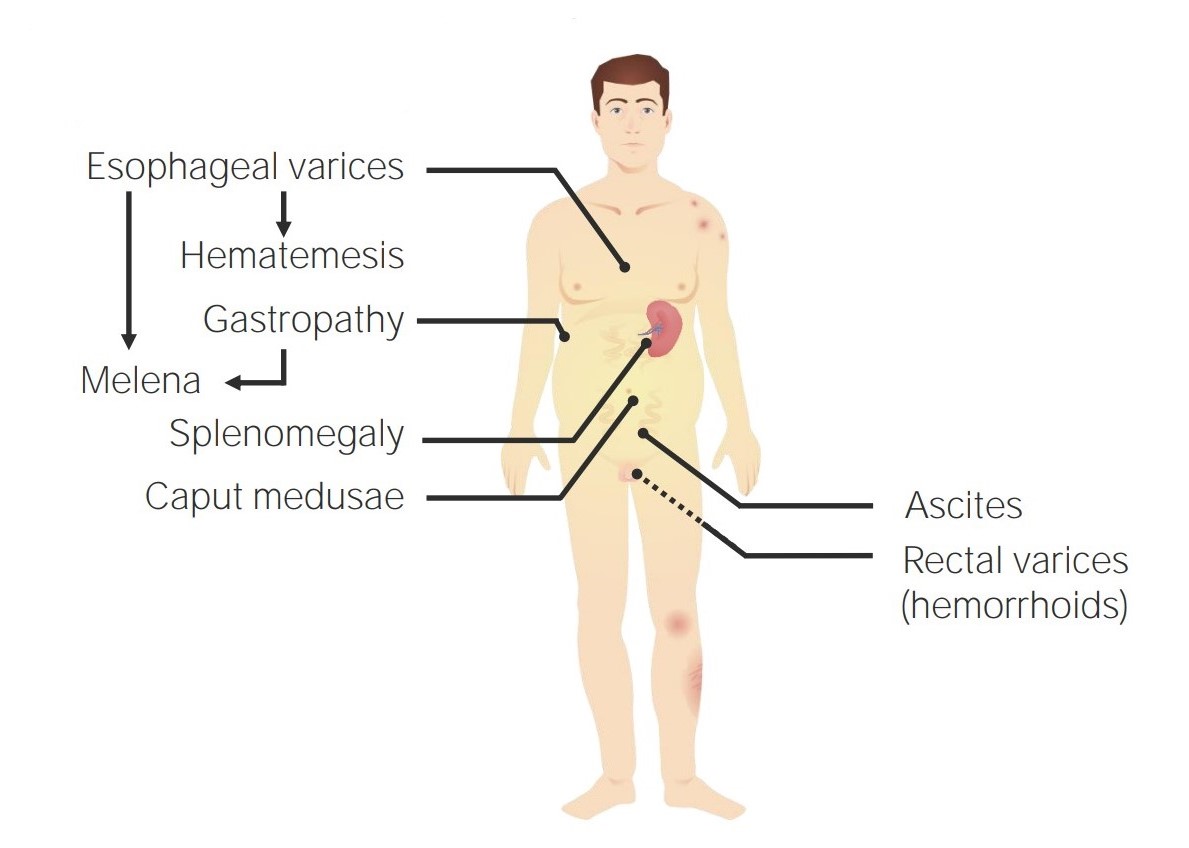
Symptoms resulting from portal hypertension

Ascites secondary to hepatic cirrhosis
Evidence of common etiologies
- Jaundice Jaundice Jaundice is the abnormal yellowing of the skin and/or sclera caused by the accumulation of bilirubin. Hyperbilirubinemia is caused by either an increase in bilirubin production or a decrease in the hepatic uptake, conjugation, or excretion of bilirubin. Jaundice
- Pruritus Pruritus An intense itching sensation that produces the urge to rub or scratch the skin to obtain relief. Atopic Dermatitis (Eczema)
- Gynecomastia Gynecomastia Gynecomastia is a benign proliferation of male breast glandular ductal tissue, usually bilateral, caused by increased estrogen activity, decreased testosterone activity, or medications. The condition is common and physiological in neonates, adolescent boys, and elderly men. Gynecomastia
- Palmar erythema Palmar Erythema Cirrhosis
- Spider Spider Arthropods of the class arachnida, order araneae. Except for mites and ticks, spiders constitute the largest order of arachnids, with approximately 37, 000 species having been described. The majority of spiders are harmless, although some species can be regarded as moderately harmful since their bites can lead to quite severe local symptoms. Spider Bites angiomata
- Asterixis Asterixis Hepatic Encephalopathy
- Peripheral edema Peripheral edema Peripheral edema is the swelling of the lower extremities, namely, legs, feet, and ankles. Edema
- Elevated jugular venous pressure
- Shortness of breath Shortness of breath Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea
- Paroxysmal nocturnal dyspnea Paroxysmal nocturnal dyspnea A disorder characterized by sudden attacks of respiratory distress in at rest patients with heart failure and pulmonary edema. It usually occurs at night after several hours of sleep in a reclining position. Patients awaken with a feeling of suffocation, coughing, a cold sweat, and tachycardia. When there is significant wheezing, it is called cardiac asthma. Pulmonary Edema
Diagnostic evaluation
The diagnosis of portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension is generally based on clinical evaluation, but it may be supported by:
- Should be performed with Doppler Doppler Ultrasonography applying the doppler effect, with frequency-shifted ultrasound reflections produced by moving targets (usually red blood cells) in the bloodstream along the ultrasound axis in direct proportion to the velocity of movement of the targets, to determine both direction and velocity of blood flow. Ultrasound (Sonography) flow Flow Blood flows through the heart, arteries, capillaries, and veins in a closed, continuous circuit. Flow is the movement of volume per unit of time. Flow is affected by the pressure gradient and the resistance fluid encounters between 2 points. Vascular resistance is the opposition to flow, which is caused primarily by blood friction against vessel walls. Vascular Resistance, Flow, and Mean Arterial Pressure
- Can support the diagnosis, but not sensitive
- Reversed blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure in the portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy
- Portosystemic collaterals
- Enlarged portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy diameter
- Ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites
- Nodular/cirrhotic liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy
- Venous thrombosis Venous thrombosis The formation or presence of a blood clot (thrombus) within a vein. Budd-Chiari Syndrome
- Usually done only if the diagnosis is unclear
- Approximates the pressure gradient Pressure gradient Vascular Resistance, Flow, and Mean Arterial Pressure between the portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy and IVC IVC The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy by using a transjugular catheter
- HVPG ≥ 6 mm Hg is diagnostic.
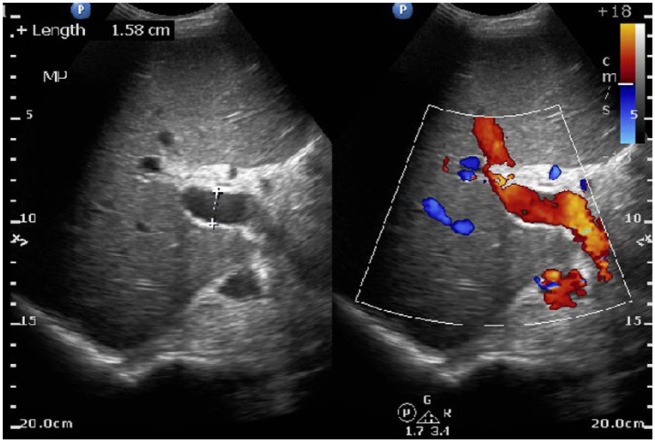
Ultrasound of the liver identifies a large portal vein, consistent with portal hypertension.
Additional evaluation
Additional studies may be performed based on the clinical presentation and presence of complications.
- ↑ Bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism
- ↑ AST AST Enzymes of the transferase class that catalyze the conversion of l-aspartate and 2-ketoglutarate to oxaloacetate and l-glutamate. Liver Function Tests , and ALT ALT An enzyme that catalyzes the conversion of l-alanine and 2-oxoglutarate to pyruvate and l-glutamate. Liver Function Tests (may be normal in advanced cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis )
- ↓ Albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests
- ↑ Ammonia Ammonia A colorless alkaline gas. It is formed in the body during decomposition of organic materials during a large number of metabolically important reactions. Note that the aqueous form of ammonia is referred to as ammonium hydroxide. Acid-Base Balance
- Anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types
- Thrombocytopenia Thrombocytopenia Thrombocytopenia occurs when the platelet count is Thrombocytopenia
- Paracentesis can be considered.
- Serum– ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests gradient: > 1.1 g/dL indicates portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension
- > 2.5 g/dL, consider cardiac causes and Budd-Chiari syndrome Budd-Chiari syndrome Budd-Chiari syndrome is a condition resulting from the interruption of the normal outflow of blood from the liver. The primary type arises from a venous process (affecting the hepatic veins or inferior vena cava) such as thrombosis, but can also be from a lesion compressing or invading the veins (secondary type). The patient typically presents with hepatomegaly, ascites, and abdominal discomfort. Budd-Chiari Syndrome
- < 2.5 g/dL, consider cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis
- Can be performed to screen for esophageal varices
- Diagnostic and therapeutic for acute bleeding from esophageal varices

Endoscopic view of the esophageal varices: The red patches indicate a recent bleed.
The focus of therapy is to prevent and treat the complications of portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus . It is also important to treat the underlying etiology (when possible).
Varices and portal hypertensive gastropathy gastropathy Damage to the epithelial lining with no or minimal associated inflammation and is technically a separate entity from gastritis Gastritis management
- Cause splanchnic vasoconstriction Vasoconstriction The physiological narrowing of blood vessels by contraction of the vascular smooth muscle. Vascular Resistance, Flow, and Mean Arterial Pressure and ↓ portal inflow
- ↓ Risk of bleeding from varices or gastropathy gastropathy Damage to the epithelial lining with no or minimal associated inflammation and is technically a separate entity from gastritis Gastritis
- IV fluid resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome
- Packed red blood cells Red blood cells Erythrocytes, or red blood cells (RBCs), are the most abundant cells in the blood. While erythrocytes in the fetus are initially produced in the yolk sac then the liver, the bone marrow eventually becomes the main site of production. Erythrocytes: Histology
- FFP FFP Transfusion Products
- Platelets Platelets Platelets are small cell fragments involved in hemostasis. Thrombopoiesis takes place primarily in the bone marrow through a series of cell differentiation and is influenced by several cytokines. Platelets are formed after fragmentation of the megakaryocyte cytoplasm. Platelets: Histology
- Octreotide Octreotide A potent, long-acting synthetic somatostatin octapeptide analog that inhibits secretion of growth hormone and is used to treat hormone-secreting tumors; diabetes mellitus; hypotension, orthostatic; hyperinsulinism; hypergastrinemia; and small bowel fistula. Antidiarrheal Drugs : causes splanchnic vasoconstriction Vasoconstriction The physiological narrowing of blood vessels by contraction of the vascular smooth muscle. Vascular Resistance, Flow, and Mean Arterial Pressure → ↓ portal pressure
- Antibiotic prophylaxis Prophylaxis Cephalosporins ( ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins ): ↓ risk of spontaneous bacterial peritonitis Spontaneous Bacterial Peritonitis Ascites
- Endoscopic interventions: endoscopic band ligation Band ligation Mallory-Weiss Syndrome (Mallory-Weiss Tear) or sclerotherapy Sclerotherapy Treatment of varicose veins, hemorrhoids, gastric and esophageal varices, and peptic ulcer hemorrhage by injection or infusion of chemical agents which cause localized thrombosis and eventual fibrosis and obliteration of the vessels. Hemorrhoids for varices
- May be used for recurrent or refractory bleeding
- Creates and maintains (via stenting) a connection between the portal and hepatic vein Hepatic vein Veins which drain the liver. Budd-Chiari Syndrome → ↓ pressure in the portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy
Ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites management
- Sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia restriction (< 2 g/day)
- Furosemide Furosemide A benzoic-sulfonamide-furan. It is a diuretic with fast onset and short duration that is used for edema and chronic renal insufficiency. Loop Diuretics
- Spironolactone Spironolactone A potassium sparing diuretic that acts by antagonism of aldosterone in the distal renal tubules. It is used mainly in the treatment of refractory edema in patients with congestive heart failure, nephrotic syndrome, or hepatic cirrhosis. Its effects on the endocrine system are utilized in the treatments of hirsutism and acne but they can lead to adverse effects. Potassium-sparing Diuretics
- Rapid symptom relief
- Used if ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites is refractory to conservative measures
- Transjugular intrahepatic portosystemic shunt Transjugular intrahepatic portosystemic shunt A type of surgical portosystemic shunt to reduce portal hypertension with associated complications of esophageal varices and ascites. It is performed percutaneously through the jugular vein and involves the creation of an intrahepatic shunt between the hepatic vein and portal vein. The channel is maintained by a metallic stent. The procedure can be performed in patients who have failed sclerotherapy and is an additional option to the surgical techniques of portocaval, mesocaval, and splenorenal shunts. It takes one to three hours to perform. Ascites for refractory ascites Refractory Ascites Ascites
- Cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis : late stage of hepatic necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage and scarring Scarring Inflammation . In cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis , chronic cellular damage causes extensive distortion Distortion Defense Mechanisms of the normal hepatic architecture, which can lead to impairment of normal blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure through the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy and portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension . Signs and symptoms are often nonspecific (e.g., fatigue Fatigue The state of weariness following a period of exertion, mental or physical, characterized by a decreased capacity for work and reduced efficiency to respond to stimuli. Fibromyalgia , anorexia Anorexia The lack or loss of appetite accompanied by an aversion to food and the inability to eat. It is the defining characteristic of the disorder anorexia nervosa. Anorexia Nervosa , weight loss Weight loss Decrease in existing body weight. Bariatric Surgery ). Decompensation manifests as jaundice Jaundice Jaundice is the abnormal yellowing of the skin and/or sclera caused by the accumulation of bilirubin. Hyperbilirubinemia is caused by either an increase in bilirubin production or a decrease in the hepatic uptake, conjugation, or excretion of bilirubin. Jaundice , ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites , and liver failure Liver failure Severe inability of the liver to perform its normal metabolic functions, as evidenced by severe jaundice and abnormal serum levels of ammonia; bilirubin; alkaline phosphatase; aspartate aminotransferase; lactate dehydrogenases; and albumin/globulin ratio. Autoimmune Hepatitis . Diagnosis often requires liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma . Management is mostly supportive, with liver transplantation Liver transplantation The transference of a part of or an entire liver from one human or animal to another. Hepatocellular Carcinoma (HCC) and Liver Metastases being the only curative treatment.
- Budd-Chiari syndrome Budd-Chiari syndrome Budd-Chiari syndrome is a condition resulting from the interruption of the normal outflow of blood from the liver. The primary type arises from a venous process (affecting the hepatic veins or inferior vena cava) such as thrombosis, but can also be from a lesion compressing or invading the veins (secondary type). The patient typically presents with hepatomegaly, ascites, and abdominal discomfort. Budd-Chiari Syndrome : hepatic venous outflow obstruction (from thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus , compression Compression Blunt Chest Trauma , or vascular invasion), which may affect the hepatic veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology and/or IVC IVC The venous trunk which receives blood from the lower extremities and from the pelvic and abdominal organs. Mediastinum and Great Vessels: Anatomy . Typical presentation is with hepatomegaly, ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites , and abdominal discomfort. The diagnosis is confirmed by Doppler Doppler Ultrasonography applying the doppler effect, with frequency-shifted ultrasound reflections produced by moving targets (usually red blood cells) in the bloodstream along the ultrasound axis in direct proportion to the velocity of movement of the targets, to determine both direction and velocity of blood flow. Ultrasound (Sonography) ultrasonography. Treatment involves addressing the underlying condition that caused the venous occlusion.
- Portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus : can occur from a number of causes ( hypercoagulable Hypercoagulable Hypercoagulable states (also referred to as thrombophilias) are a group of hematologic diseases defined by an increased risk of clot formation (i.e., thrombosis) due to either an increase in procoagulants, a decrease in anticoagulants, or a decrease in fibrinolysis. Hypercoagulable States state, surgery, inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation , trauma, malignancy Malignancy Hemothorax ) and results in portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension . Ultrasound with Doppler Doppler Ultrasonography applying the doppler effect, with frequency-shifted ultrasound reflections produced by moving targets (usually red blood cells) in the bloodstream along the ultrasound axis in direct proportion to the velocity of movement of the targets, to determine both direction and velocity of blood flow. Ultrasound (Sonography) showing absent or diminished blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure through the portal vein Portal vein A short thick vein formed by union of the superior mesenteric vein and the splenic vein. Liver: Anatomy is usually diagnostic. Management includes anticoagulation Anticoagulation Pulmonary Hypertension Drugs , thrombolysis in specific cases, and management of complications of portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension .
- Schistosomiasis Schistosomiasis Infection with flukes (trematodes) of the genus schistosoma. Three species produce the most frequent clinical diseases: Schistosoma haematobium (endemic in Africa and the Middle East), Schistosoma Mansoni (in Egypt, northern and southern Africa, some West Indies islands, northern 2/3 of South america), and Schistosoma japonicum (in Japan, China, the Philippines, Celebes, Thailand, Laos). S. mansoni is often seen in Puerto Ricans living in the United States. Schistosoma/Schistosomiasis : infection by the trematode Trematode Class of parasitic flukes consisting of three subclasses, monogenea, aspidogastrea, and digenea. The digenetic trematodes are the only ones found in man. They are endoparasites and require two hosts to complete their life cycle. Schistosoma/Schistosomiasis Schistosoma Schistosoma Schistosomiasis is an infection caused by Schistosoma, a trematode. Schistosomiasis occurs in developing countries with poor sanitation. Freshwater snails are the intermediate host and are transmitted to humans through skin contact with contaminated fresh water. The clinical presentation occurs as a result of the host’s immune response to antigens from the eggs. Schistosoma/Schistosomiasis . Schistosomiasis Schistosomiasis Infection with flukes (trematodes) of the genus schistosoma. Three species produce the most frequent clinical diseases: Schistosoma haematobium (endemic in Africa and the Middle East), Schistosoma Mansoni (in Egypt, northern and southern Africa, some West Indies islands, northern 2/3 of South america), and Schistosoma japonicum (in Japan, China, the Philippines, Celebes, Thailand, Laos). S. mansoni is often seen in Puerto Ricans living in the United States. Schistosoma/Schistosomiasis occurs in developing countries with poor sanitation Sanitation The development and establishment of environmental conditions favorable to the health of the public. Hepatitis E Virus . The clinical presentation is a result of the host’s immune response to antigens from the eggs. Most individuals are asymptomatic, but others may develop acute schistosome dermatitis Acute Schistosome Dermatitis Schistosoma/Schistosomiasis , acute schistosomiasis syndrome Acute Schistosomiasis Syndrome Schistosoma/Schistosomiasis , or chronic schistosomiasis Chronic Schistosomiasis Schistosoma/Schistosomiasis . The diagnosis can be made with microscopic evaluation of the urine or feces, serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus , or PCR PCR Polymerase chain reaction (PCR) is a technique that amplifies DNA fragments exponentially for analysis. The process is highly specific, allowing for the targeting of specific genomic sequences, even with minuscule sample amounts. The PCR cycles multiple times through 3 phases: denaturation of the template DNA, annealing of a specific primer to the individual DNA strands, and synthesis/elongation of new DNA molecules. Polymerase Chain Reaction (PCR) . The treatment for schistosomiasis Schistosomiasis Infection with flukes (trematodes) of the genus schistosoma. Three species produce the most frequent clinical diseases: Schistosoma haematobium (endemic in Africa and the Middle East), Schistosoma Mansoni (in Egypt, northern and southern Africa, some West Indies islands, northern 2/3 of South america), and Schistosoma japonicum (in Japan, China, the Philippines, Celebes, Thailand, Laos). S. mansoni is often seen in Puerto Ricans living in the United States. Schistosoma/Schistosomiasis is praziquantel Praziquantel An anthelmintic used in most schistosome and many cestode infestations. Anthelmintic Drugs .
- Congestive hepatopathy: right-sided heart failure Right-Sided Heart Failure Ebstein’s Anomaly can lead to severe venous congestion, including within the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy . This can progress to cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis . Individuals can have evidence of both heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) and cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis , and the diagnosis is generally clinical. Management involves treating the underlying heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR) .
- Hou, W., Sanyal, A. J. (2009). Ascites: diagnosis and management. Med Clin North Am 93:801–817, vii. reference.medscape.com/medline/abstract/19577115
- Lubel, J. S., Angus, P. W. /2005). Modern management of portal hypertension. Intern Med J 35:45–49. reference.medscape.com/medline/abstract/15667468
- Bleibel, W., Chopra, S., Curry, M. P. (2021). Portal hypertension in adults. UpToDate. Retrieved October 3, 2021, from https://www.uptodate.com/contents/portal-hypertension-in-adults
- Garcia-Pagan, J. C., Pik Eu, J. C. (2021). Noncirrhotic portal hypertension. UpToDate. Retrieved October 3, 2021, from https://www.uptodate.com/contents/noncirrhotic-portal-hypertension
- Oliver, T. I., Sharma, B., John, S. (2021). Portal hypertension. StatPearls. Retrieved October 3, 2021, from https://www.ncbi.nlm.nih.gov/books/NBK507718/
- Carale, J., Azer, S. A., Mekaroonkamol, P. (2017). Portal hypertension. Medscape. Retrieved October 3, 2021, from https://emedicine.medscape.com/article/182098-overview
- Tholey, D. (2021). Portal hypertension. MSD Manual Professional Version. Retrieved October 3, 2021, from https://www.msdmanuals.com/professional/hepatic-and-biliary-disorders/approach-to-the-patient-with-liver-disease/portal-hypertension
Study with Lecturio for
Medical School
Nursing School
- Data Privacy
- Terms and Conditions
- Legal Information
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
Create your free account or log in to continue reading!
Sign up now and get free access to Lecturio with concept pages, medical videos, and questions for your medical education.
Log in to your account
User Reviews
Get Premium to test your knowledge
Lecturio Premium gives you full access to all content & features
Get Premium to watch all videos
Verify your email now to get a free trial.
Create a free account to test your knowledge
Lecturio Premium gives you full access to all contents and features—including Lecturio’s Qbank with up-to-date board-style questions.

IMAGES
VIDEO
COMMENTS
Patients usually have no symptoms until complications arise. Hematemesis from bleeding varices is the most common presentation. Melena without hematemesis can also be present. As cirrhosis is the most common cause of portal hypertension, patients may present with stigmata of cirrhosis.
The first noticeable symptoms of portal hypertension are usually related to new, enlarged, leaky and bleeding veins, such as: Blood in vomit. Blood in poop. Bloated stomach with rapid weight gain (from fluid). Swelling in your legs and feet ( edema ). Mental confusion or disorientation.
Portal hypertension often develops in the setting of cirrhosis, schistosomiasis, or extrahepatic portal vein thrombosis. It is the result of resistance to portal blood flow and may lead to complications such as variceal bleeding and ascites. This topic will review the development, clinical manifestations, and diagnosis of portal hypertension in ...
Request an Appointment. 410-955-5000 Maryland. 855-695-4872 Outside of Maryland. +1-410-502-7683 International. Find a Treatment Center. The most common cause of portal hypertension is cirrhosis (scarring) of the liver.
Portal hypertension is a major complication of cirrhosis, and its consequences, including ascites, esophageal varices, hepatic encephalopathy, and hepatorenal syndrome, lead to substantial morbidity and mortality. The past several decades have seen major improvements in the clinical management of complications of portal hypertension, resulting in substantial gains in patient outcomes. However ...
The most common cause of portal hypertension is cirrhosis of the liver. Cirrhosis is scarring which accompanies the healing of liver injury caused by hepatitis, alcohol, or other less common ...
Many conditions are associated with portal hypertension, with cirrhosis being the most common cause of this disorder. Two important factors—vascular resistance and blood flow—exist in the development of portal hypertension. ... Presentation History. In obtaining the medical history of a patient with portal hypertension, attention should be ...
Cirrhosis is the most common cause of portal hypertension. Cirrhosis is a type of liver disease in which scar tissue replaces healthy liver tissue. This scar tissue can block the blood flow and ...
The most common cause of portal hypertension is cirrhosis. In this setting, there is an increase in intrahepatic resistance leading to an increase in portal pressure. By increasing portal blood flow, splanchnic vasodilation further aggravates portal hypertension. ... Endoscopy should be performed within 12 hour of presentation in patients with ...
Hematemesis from bleeding varices is the most common presentation. Melena without hematemesis can also be present. As cirrhosis is the most common cause of portal hypertension, patients may present with stigmata of cirrhosis. ... The common cause of portal hypertension is cirrhosis in Western countries. Noncirrhotic portal hypertension due to ...
Portal hypertension is a clinical syndrome defined by a portal venous pressure gradient exceeding 5 mm Hg. Cirrhosis is the most common cause of portal hypertension in the Western world. The goal of this review is to provide an overview of the current understanding of the pathophysiology and treatment of portal hypertension.
Abstract. Portal hypertension is a major complication of cirrhosis, and its consequences, including ascites, esophageal varices, hepatic encephalopathy, and hepatorenal syndrome, lead to substantial morbidity and mortality. The past several decades have seen major improvements in the clinical management of complications of portal hypertension ...
The most common cause of portal hypertension is cirrhosis. Vascular resistance and blood flow are the 2 important factors in its development. The images below depict esophageal varices, which are responsible for the main complication of portal hypertension, upper gastrointestinal (GI) hemorrhage. Large esophageal varices with red wale signs ...
Portal hypertension is defined as increased portal venous pressure, with a hepatic venous pressure gradient greater than 5 mmHg. Normal portal pressure is 1-4 mmHg; clinically insignificant portal hypertension is present at portal pressures 5-9 mmHg; clinically significant portal hypertension is present at portal pressures greater than 10 mmHg. The portal vein and its branches supply most ...
Non-cirrhotic portal hypertension is a common presentation in those with hypogammaglobulinemia and/or common variable immunodeficiency with the most common of these etiologies being nodular regenerative hyperplasia (NRH), where there is development of benign small regenerative nodules that may lead to portal hypertension.
GG-T Portal hypertension is high pressure in the portal vein, which is the vein that carries blood to the liver. By far, the most common cause of portal hypertension is cirrhosis. Normally, the liver is a soft organ, and blood flows through it very easily. With cirrhosis, the liver becomes hard and blood cannot flow easily, so it backs up and ...
The most severe and life-threatening presentation of portal hypertension is acute variceal bleeding. Pharmacotherapy with vasoactive agents (terlipressin or somatostatin), endoscopic band ligation and radiological treatment with transjugular intrahepatic portosystemic shunt (TIPSS) are the most common treatment options for variceal bleeding.
Portal hypertension (PH) is a common clinical syndrome defined as the elevation of hepatic venous pressure gradient (HVPG) above 5 mm Hg. PH is caused by a combination of two simultaneous occurring hemodynamic processes: (1) increased intrahepatic resistance to passage of blood flow through the liver due to cirrhosis and (2) increased ...
Clinical Presentation. Portal hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter.