- Credit cards
- View all credit cards
- Banking guide
- Loans guide
- Insurance guide
- Personal finance
- View all personal finance
- Small business
- Small business guide
- View all taxes

You’re our first priority. Every time.
We believe everyone should be able to make financial decisions with confidence. And while our site doesn’t feature every company or financial product available on the market, we’re proud that the guidance we offer, the information we provide and the tools we create are objective, independent, straightforward — and free.
So how do we make money? Our partners compensate us. This may influence which products we review and write about (and where those products appear on the site), but it in no way affects our recommendations or advice, which are grounded in thousands of hours of research. Our partners cannot pay us to guarantee favorable reviews of their products or services. Here is a list of our partners .
How Much Does Gender-Affirming Surgery Cost?

Many or all of the products featured here are from our partners who compensate us. This influences which products we write about and where and how the product appears on a page. However, this does not influence our evaluations. Our opinions are our own. Here is a list of our partners and here's how we make money .
Gender-affirming care encompasses a broad range of psychological, behavioral and medical treatments for transgender, nonbinary and gender-nonconforming people.
The care is designed to “support and affirm an individual’s gender identity” when it is at odds with the sex they were assigned at birth, as defined by the World Health Organization.
What is gender-affirming surgery?
Gender-affirming surgery refers to the surgical and cosmetic procedures that give transgender and nonbinary people “the physical appearance and functional abilities of the gender they know themselves to be,” according to the American Society of Plastic Surgeons. It is sometimes called gender reassignment surgery.
There are three main types of gender-affirming surgeries, per the Cleveland Clinic:
Top surgery , in which a surgeon either removes a person’s breast tissue for a more traditionally masculine appearance or shapes a person’s breast tissue for a more traditionally feminine appearance.
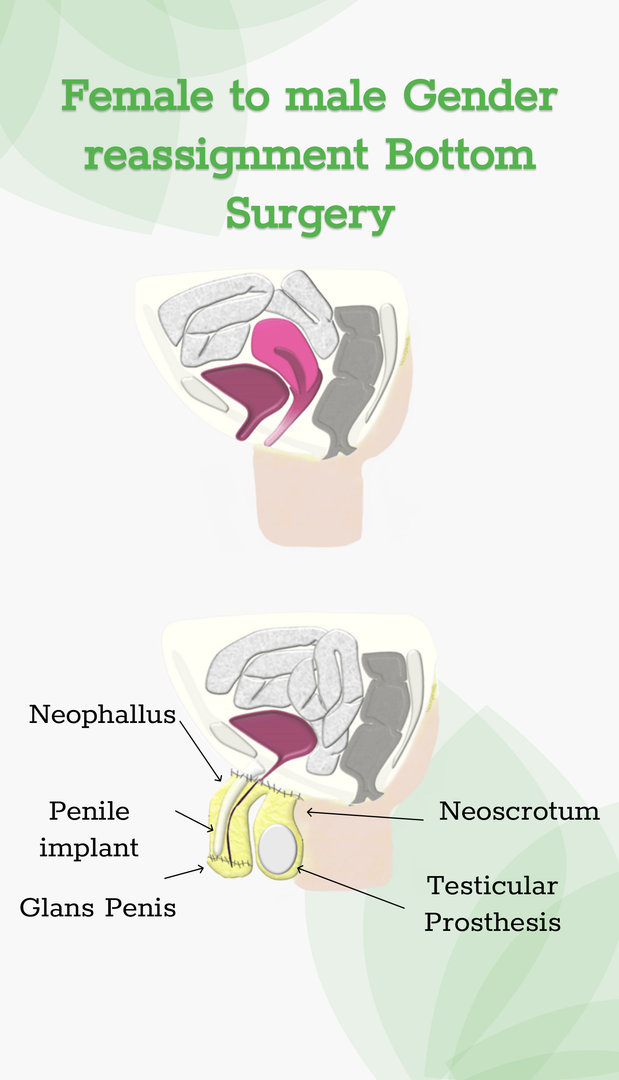
Bottom surgery , or the reconstruction of the genitals to better align with a person’s gender identity.
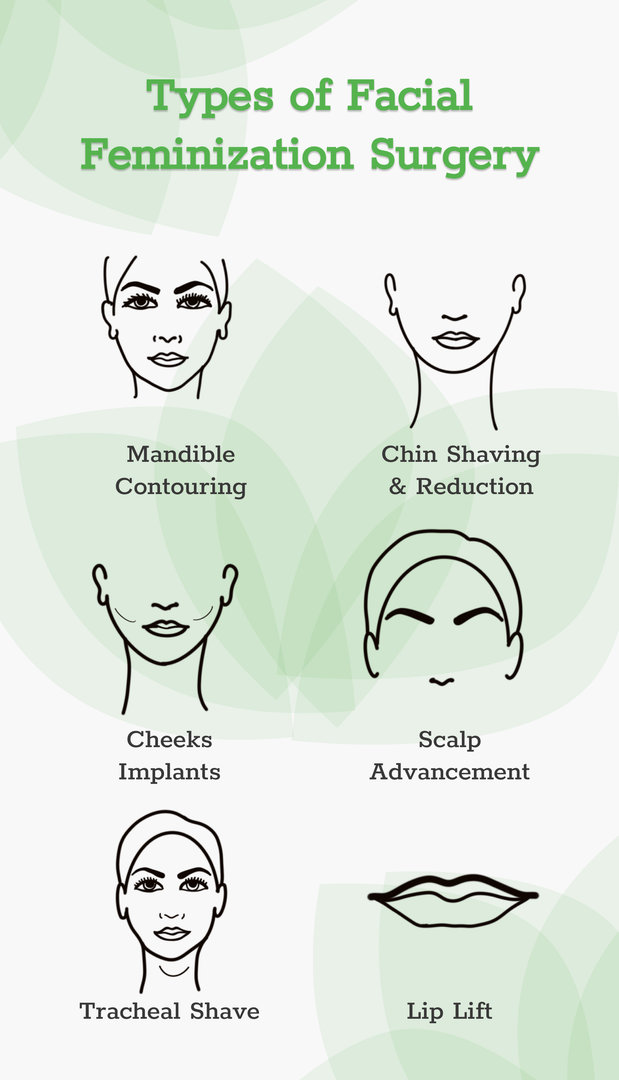
Facial feminization or masculinization surgery , in which the bones and soft tissue of a person’s face are transformed for either a more traditionally masculine or feminine appearance.
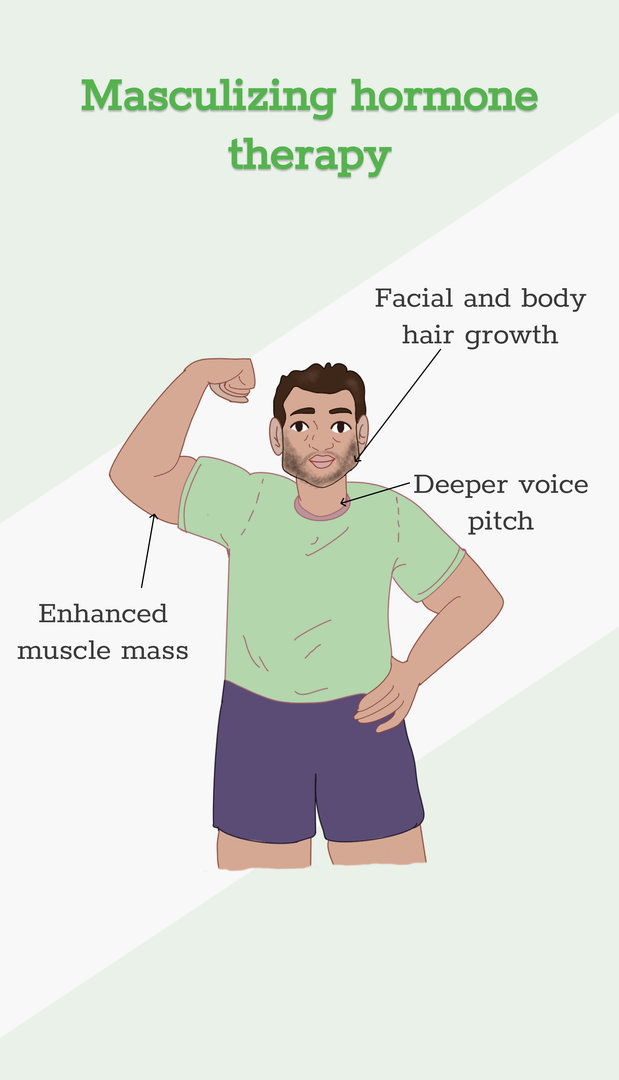
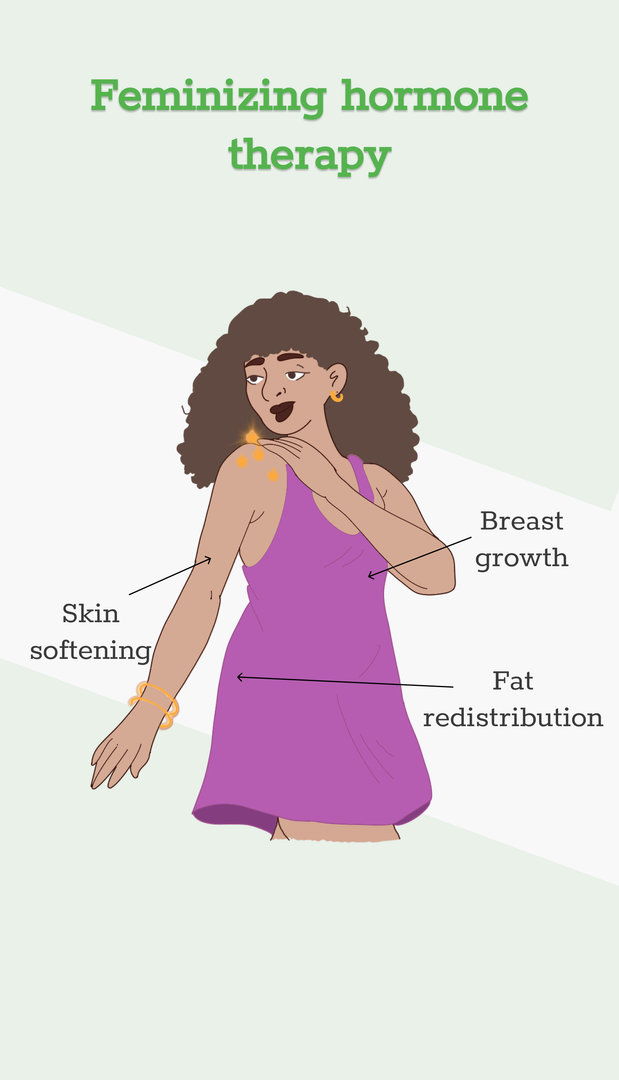
Some people who undergo gender-affirming surgeries also use specific hormone therapies. A trans woman or nonbinary person on feminizing hormone therapy, for example, takes estrogen that’s paired with a substance that blocks testosterone. And a trans man or nonbinary person on masculinizing hormone therapy takes testosterone.
Gender-affirming surgeries and treatments are the recommended course of treatment for gender dysphoria by the American Medical Association. Gender dysphoria is defined as “clinically significant distress or impairment related to gender incongruence, which may include desire to change primary and/or secondary sex characteristics,” according to the American Psychiatric Association.
Some LGBTQ+ advocates and medical professionals feel that gender dysphoria shouldn't be treated as a mental disorder, and worry that gender dysphoria’s inclusion in the DSM-5 — the authoritative source on recognized mental health disorders for the psychiatric industry — stigmatizes trans and nonbinary people.
How much does gender-affirming surgery cost?
Gender-affirming surgery can cost between $6,900 and $63,400 depending on the precise procedure, according to a 2022 study published in The Journal of Law, Medicine and Ethics.
Out-of-pocket costs can vary dramatically, though, depending on whether you have insurance and whether your insurance company covers gender-affirming surgeries.
There are also costs associated with the surgery that may not be represented in these estimates. Additional costs may include:
Surgeons fees
Hospital fees
Consultation fees
Insurance copays
The cost of psychiatric care or therapy, as most insurance companies and surgeons require at least one referral letter prior to the surgery. An hour of therapy can cost between $65 and $250, according to Good Therapy, an online platform for therapists and counselors.
Time off work. After bottom surgery, you can expect to miss six weeks of work while recovering. Most people miss around two weeks of work after top surgery.
Miscellaneous goods that’ll help you recover. For example, after bottom surgery, you might need to invest in a shower stool, waterproof bed sheets, cheap underwear and sanitary towels. Top surgery patients may need, depending on the procedure, a mastectomy pillow, chest binder and baggy clothes.
Is gender-affirming surgery covered by insurance?
It’s illegal for any federally funded health insurance program to deny coverage on the basis of gender identity, sexual orientation or sexual characteristics, per Section 1557, a section of the Affordable Care Act. Section 1557 doesn’t apply to private insurance companies, though, and several U.S. states have passed laws banning gender-affirming care.
The following states have banned gender-affirming surgery for people under 18 years old, according to the Human Rights Campaign: Alabama, Arkansas, Florida, Georgia, Idaho, Indiana, Iowa, Kentucky, Louisiana, Mississippi, Missouri, Montana, Nebraska, North Carolina, North Dakota, Oklahoma, South Dakota, Tennessee, Texas, Utah, West Virginia. In four of these states — Alabama, Arkansas, Florida and Indiana — court injunctions are currently ensuring access to care.
And these states have either passed laws — or have governors who issued executive orders — protecting access to gender-affirming surgery, according to the Movement Advancement Project, a public policy nonprofit: California, Colorado, Connecticut, Illinois, Maryland, Massachusetts, Minnesota, New Jersey, New Mexico, New York, Oregon, Vermont and Washington, D.C.
But even if your state has enshrined protections for gender-affirming care, some private insurance companies may consider surgeries “cosmetic” and therefore “not medically necessary,” according to the Transgender Legal Defense and Education Fund. If you have private insurance or are insured through your employer, contact your insurance company and see if they cover gender-affirming care. Also, ask about any documentation the insurance company requires for coverage.
The Williams Institute estimates that 14% of trans Americans currently enrolled in Medicaid live in states where such coverage is banned, while another 27% of trans Americans live in states where coverage is “uncertain,” because their state laws are “silent or unclear on coverage for gender-affirming care.”
Because of Section 1557, Medicaid is federally banned from denying coverage on the basis of sex or gender; among the roughly 1.3 million transgender Americans, around 276,000 have Medicaid coverage, according to a 2022 report from the Williams Institute.
How to pay for gender-affirming surgery
If your private insurance company won’t cover gender-affirming care, and you’re unable to obtain coverage through the federal marketplace, consider these sources:
Online personal loan.
Credit union personal loan.
Credit card.
CareCredit.
Home equity line of credit.
Family loan.
There are also several nonprofits that offer financial assistance for gender-affirmation surgeries. Those organizations include:
Point of Pride , which offers grants and scholarships to trans and nonbinary people seeking gender-affirming surgery and care.
The Jim Collins Foundation , which raises money to fund gender-affirming surgeries.
Genderbands , which offers grants for gender-affirming surgeries and care.
Black Transmen Inc. , which funds gender-affirming surgeries for Black trans men.
On a similar note...
Get doctor listing on ClinicSpots.
- Gender Reassignment Surgery Cost (MTF & FTM)
Explore the rising demand for gender reassignment surgery worldwide. Learn about the various procedures and their detailed costs in this comprehensive article.
- Transgender Surgery
By Priyanka Dutta Deb
6th June '22
Gender reassignment surgery cost varies depending on the type of transition.
- For male to female (MTF) transition, the cost ranges from $2438 to $6095 and
- For female to male (FTM) transition, the cost falls between $4876 and $9752 .
When considering the cost of gender reassignment surgery, it's important to note that these figures encompass the surgical expenses alone. Additional costs, such as:
- pre-operative consultations
- post-operative care
- hospitalization may also be involved
For a precise cost estimate that aligns with your specific needs, it is highly recommended that you consult reliable healthcare providers or clinics.
Begin with clarity. Contact us for detailed cost insights now.
There are two broad types of gender reassignment surgery : top surgery and bottom surgery. The top surgery is performed for both people assigned female at birth (AFAB) and assigned male at birth (AMAB).
- Male to female or non-binary (MTF/N): This procedure entails using saline or silicone implants to boost chest size and form for a more feminine or female appearance. Male-to-female top surgery is done under general anesthesia.
- Female to male or non-binary (FTM/N): During FTM top surgery, breast tissue is removed and the chest is shaped to give the patient a flat, masculine, or male appearance. Following this, a nipple graft is planted to give a complete look .
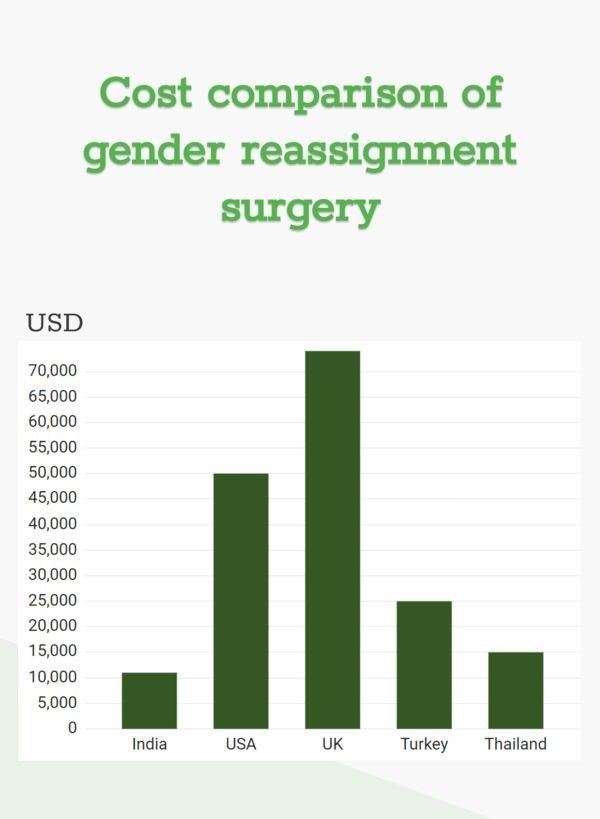
Before we discuss each service's cost, let's take a quick look at overall transgender surgery costs in different countries.
You must be curious to know the gender change surgery cost of different surgical procedures. Let's read.
What is the Cost of Male-to-Female Top Surgery?
Breast augmentation or augmentation mammoplasty is another name for MTF and MTN top surgery.
The MTF/N top surgery or breast augmentation surgery cost in India is around USD 1290 to USD 1940 . The surgeon's expertise and experience are two of the most critical aspects that affect the cost.
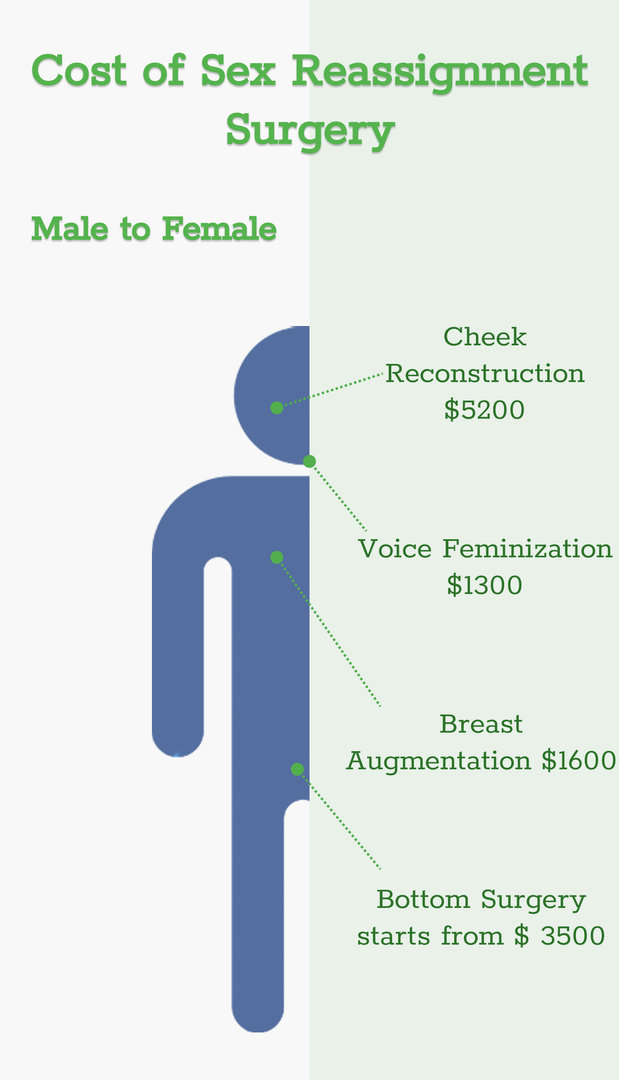
For the duration of the surgery, you will be put under general anesthesia. Your surgeon may choose different breast augmentation methods depending on your desired chest size, implant kind, and incision site. The average time for MTF and MTN top surgery is 1 to 2 hours .
The insertion cost and the implant cost are the two components of the surgery cost.
Navigating your options? Contact us today for more information on cost!
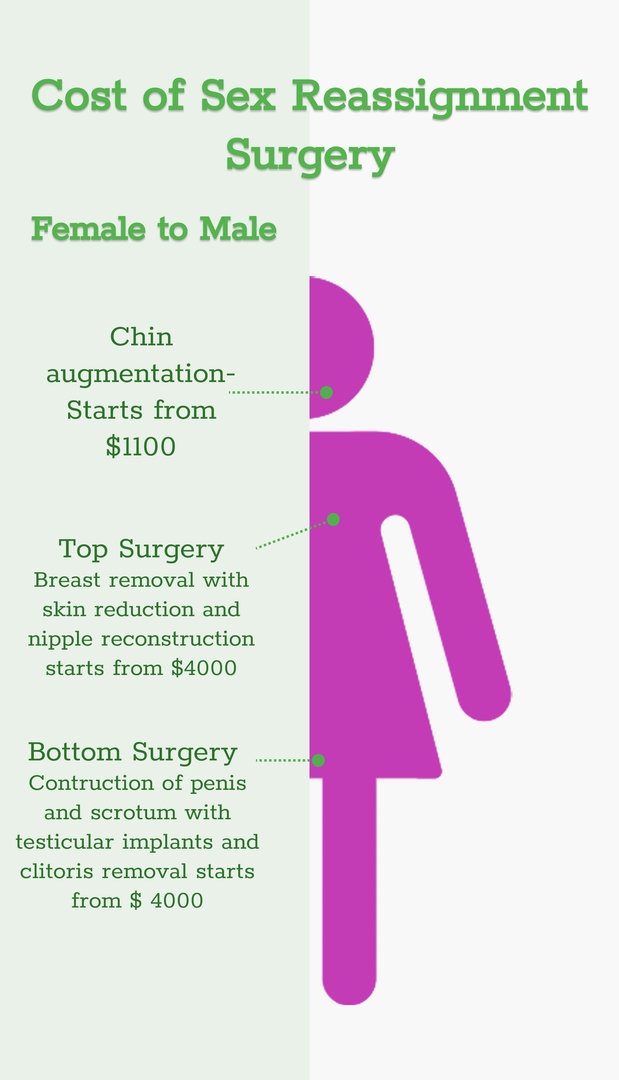
What is the cost of female-to-male top surgery?
An FTM or FTN top surgery procedure takes from 1.5 to 4 hours . Various treatments are performed to get a more flat, masculine, or male-looking chest. Double incision, periareolar, and keyhole are the most popular procedures used by surgeons.
The FTM top surgery cost ranges around USD 3870 .
Now that we have already discussed top surgery costs, let's take a look at how much mtf bottom surgery costs.
AFAB and AMAB people can undergo bottom surgery as part of their gender confirmation process. Bottom surgery involves transforming or reconstructing the bottom or genitalia. This involves Vaginoplasty, penile transplant , phalloplasty, and metoidioplasty.
What is the cost of male-to-female bottom surgery?
Vaginoplasty surgery is the major procedure performed in bottom surgery . There are three main options under Vaginoplasty. Penile inversion, non-penile inversion Vaginoplasty, and recto-sigmoid or colon graft.
The clitoris is moulded from the head/tip of the penis in all three surgical approaches. The Vaginoplasty cost is around USD 3870 to USD 4520.
Now, let's look at female to male bottom surgery cost.
What is the Cost of Female-to-Male Bottom Surgery?
This procedure involves the removal of the female organs in the lower region and reassigning them to male sexual parts. It includes removing the uterus, vaginal remodeling, labia reconstruction, metoidioplasty, and phalloplasty.
The whole procedure may cost somewhere around USD 5160 to USD 10,335 .
To get a clearer picture of gender reassignment surgery cost, connect with us now .
What is the Cost of Facial Feminization Surgery?
Facial feminization surgery is a technique that involves changing your facial characteristics to make them appear more feminine. FFS is concerned with bone structure and nose shape. FFS is distinct for each person and can affect any part of the face or neck.
The facial feminization surgery cost is USD 1350 .
What is Hormonal Replacement Cost?
Hormonal replacement therapy is for both MTF/N and FTM/N transitioning.
MTF/N: The hormones for a male-to-female transition enhance the alignment of your gender identity. It helps induce physical changes in your body produced by female hormones during puberty (gender congruence). Male secondary sex traits can be avoided if feminizing hormone therapy like progesterone is initiated before male puberty. The hormonal replacement therapy cost for MTF/N is USD 12/month.
FTM/N: You'll be administered the male hormone testosterone during masculinizing hormone therapy. It suppresses your menstrual cycles and lowers oestrogen synthesis in your ovaries. The hormonal replacement therapy cost FTM/N is USD 7/month.
To make a more informed decision, talk to us today.
Factors affecting the cost of gender reassignment surgery:
- Hospital charges: It depends on the type of hospital you choose. Moreover, the cost also depends on whether you are admitted to a general ward or a private room.
- Psychiatrist : If you need a psychiatrist to deal with your physical changes, your cost will impact you. A psychiatrist is recommended to understand better the complex procedures and adjustments you will need before and after your surgery.
- Clinical Experts and Surgeons : You will discuss the specifics of your gender change surgery with your doctor. It includes an assessment of your medical health status, discussing your long-term gender confirmation goals, and evaluating which procedures may be most appropriate to assist you in your journey. You can ask for specific details such as risks, benefits, and what to expect from the surgery.
- Medical Insurance: Your medical insurance will play an essential role in the procedure, saving you a lot of money.
- Accommodation Charges: The accommodation charges are included for international patients.
- Medication charges : These charges include all the medication you will receive before and after the procedure ends.
- Pre- and Post-treatment charges: The pre-treatment charges include doctor consultation fees, diagnosis charges, etc. The post-treatment charges may include medicine costs, doctor's revisit charges, etc.
Your health is too important to ignore – schedule your appointment now.
Do Insurance Companies Cover Gender Reassignment Surgery?
Yes, insurance companies that cover gender reassignment surgery! There is no legal prohibition for that. Not all employers provide insurance coverage to unmarried or live-in partners of straight employees. But, several organizations nowadays provide medical insurance to their employees' same-sex partners, including coverage for gender-reassignment surgery.
Some independent companies have made it a goal to try and incorporate this coverage into their medical insurance for employees.
Note: This article is on the cost of gender reassignment surgery, and data about it is only for your informational purposes and is subject to change.
1. Side effects of gender reassignment surgery
- Infections.
- Side effects of anesthesia.
- Difficulty in urinating.
- Severe complications in intestines.
- Leakage of urine through openings.
- Closure of vaginal opening.
2. Who typically undergoes gender reassignment surgery?
Gender reassignment surgery is typically undergone by individuals who experience gender dysphoria, a condition where an individual's gender identity does not match their assigned sex at birth. It is usually recommended as a last resort after other treatments such as therapy, hormone therapy, and social transition have been tried.
3. What are the types of gender reassignment surgery?
The two main types of gender reassignment surgery are "top surgery," which refers to surgeries that alter the chest and breast area, and "bottom surgery," which refers to surgeries that alter the genital area. Top surgery may involve a mastectomy, breast augmentation, or breast reduction. Bottom surgery may involve genital reconstruction, orchiectomy, metoidioplasty, or phalloplasty. 4. Do the costs vary for different types of gender affirmation procedures? Yes, the cost can vary based on the specific surgeries involved, such as chest or breast augmentation, facial feminization, or genital reconstruction. References:
https://my.clevelandclinic.org/
Dr. Josef Hadeed Plastic Surgery | Beverly Hills & Los Angeles (josefhadeedmd.com)
The Economic Times: Business News, Personal Finance, Financial News, India Stock Market Investing, Economy News, SENSEX, NIFTY, NSE, BSE Live, IPO News (indiatimes.com)
Market research reports, consulting: Global Market Insights Inc. (gminsights.com)
Transgender surgery – Knowledge gap among physicians impacti... : Current Urology (lww.com)
https://jamanetwork.com/journals/jamasurgery/fullarticle/2779429
Relevant Blogs
How much does male to female (MTF) surgery cost in 2024?
Explore the interactive cost guide below for detailed pricing information on a range of MTF surgeries and compare costs in different countries.
Female to Male (FTM) Surgery Cost in 2023
Explore managing fibrocystic breast disease post-menopause. Gain insights and support for optimal health beyond this stage.

Transgender Surgery Gone Wrong, How To Reverse It?
Discover solutions for transgender surgery gone wrong. Learn how to reverse complications and regain confidence. Your guide to a corrective journey awaits.

MTF Top Surgery Scars, Are They Normal & How To Treat Them?
Understanding MTF top surgery scars: types, management, and scar reduction techniques. Empowering choices for a smooth transition.

Progesterone Transgender: Effects and Considerations
Explore the use of progesterone in transgender hormone therapy. Learn about its role in feminizing or masculinizing effects and its potential benefits and risks for individuals undergoing gender transition.

Gender Dysphoria in Adults: Understanding and Support
Explore gender dysphoria in adults. Gain insights, support, and resources for understanding and navigating this complex experience with compassion and dignity.
FTM Post Op: Expectations After Transgender Surgery
Explore the transformative journey of FTM post-op experiences. Discover insights, support, and resources for a fulfilling and affirming transition.

Post Op MTF, What You Can Expect Post MTF Surgery For Transgender?
Find out post-operative care for MTF (Male-to-Female) gender confirmation surgery. Learn about recovery, potential complications, and ongoing support for a successful transition journey.
Question and Answers
After sex change body Ex vometing
Female | 20
In case you are experiencing vomiting after a sex change surgery, please consider medical attention. This could be a symptom of the complication, like an infection or medication intolerance. It is advisable to see a gender reassignment surgeon or a doctor who has dealt with transgender patients in the past. Do not delay seeking medical care.
Answered on 21st Feb '24
Dr. Vinod Vij
In ftm hrt, would the physical effects be noticeable? I have family that are very conservative and am just wondering whether they will be able to notice.
Indeed, the physical results of FTM HRT are visible but may differ depending on an individual. It is possible also to identify some physical changes such as a deepening voice, facial and body hair growths, and redistribution of the fatty mass. It is best to consult with a gender-affirming healthcare provider who specializes in trans healthcare
Answered on 29th Jan '24
Can a transgender male have a period?
Men who are transgenders assigned female at birth still possess uterus, and consequently continue to menstruate as normal. Hormone therapy commonly used in the gender transition brings about a significant decrease or cessation of menstrual bleeding. In order to get personalized advice regarding the management of menstrual health for those going through gender transition, a specialist in transgender medicine or endocrinology needs to be consulted.
Answered on 18th Jan '24
Female to male fmga operation cheyinchukuna valaki pillalu putte is there a possibility
FMGA surgery DOES NOT allow for biological pregnancy..
Answered on 13th Dec '23
Hi mai m2f crossdresser ho mai self m2f hormons treatment karna chahti hu khya app mujje guide kar sakte hai ki meri body or breast female jaisi karne ke liye kis name ki hormones tablet pills le sakti ho
For feminization before hormonal therapy few tests has to be done, the eligibility and other health conditions need to check and based on that proper treatment plan can be prescribed.
Answered on 12th Dec '23
Transgender Surgery Hospitals In Other Cities
Top related speciality doctors in other cities.
- Introduction
- Conclusions
- Article Information
Error bars represent 95% CIs. GAS indicates gender-affirming surgery.
Percentages are based on the number of procedures divided by number of patients; thus, as some patients underwent multiple procedures the total may be greater than 100%. Error bars represent 95% CIs.
eTable. ICD-10 and CPT Codes of Gender-Affirming Surgery
eFigure. Percentage of Patients With Codes for Gender Identity Disorder Who Underwent GAS
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Wright JD , Chen L , Suzuki Y , Matsuo K , Hershman DL. National Estimates of Gender-Affirming Surgery in the US. JAMA Netw Open. 2023;6(8):e2330348. doi:10.1001/jamanetworkopen.2023.30348
Manage citations:
© 2024
- Permissions
National Estimates of Gender-Affirming Surgery in the US
- 1 Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, New York, New York
- 2 Department of Obstetrics and Gynecology, University of Southern California, Los Angeles
Question What are the temporal trends in gender-affirming surgery (GAS) in the US?
Findings In this cohort study of 48 019 patients, GAS increased significantly, nearly tripling from 2016 to 2019. Breast and chest surgery was the most common class of procedures performed overall; genital reconstructive procedures were more common among older individuals.
Meaning These findings suggest that there will be a greater need for clinicians knowledgeable in the care of transgender individuals with the requisite expertise to perform gender-affirming procedures.
Importance While changes in federal and state laws mandating coverage of gender-affirming surgery (GAS) may have led to an increase in the number of annual cases, comprehensive data describing trends in both inpatient and outpatient procedures are limited.
Objective To examine trends in inpatient and outpatient GAS procedures in the US and to explore the temporal trends in the types of GAS performed across age groups.
Design, Setting, and Participants This cohort study includes data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. Patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified, and the performance of GAS, including breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures, were identified.
Main Outcome Measures Weighted estimates of the annual number of inpatient and outpatient procedures performed and the distribution of each class of procedure overall and by age were analyzed.
Results A total of 48 019 patients who underwent GAS were identified, including 25 099 (52.3%) who were aged 19 to 30 years. The most common procedures were breast and chest procedures, which occurred in 27 187 patients (56.6%), followed by genital reconstruction (16 872 [35.1%]) and other facial and cosmetic procedures (6669 [13.9%]). The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020. Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged12 to 18 years. When stratified by the type of procedure performed, breast and chest procedures made up a greater percentage of the surgical interventions in younger patients, while genital surgical procedures were greater in older patients.
Conclusions and Relevance Performance of GAS has increased substantially in the US. Breast and chest surgery was the most common group of procedures performed. The number of genital surgical procedures performed increased with increasing age.
Gender dysphoria is characterized as an incongruence between an individual’s experienced or expressed gender and the gender that was assigned at birth. 1 Transgender individuals may pursue multiple treatments, including behavioral therapy, hormonal therapy, and gender-affirming surgery (GAS). 2 GAS encompasses a variety of procedures that align an individual patient’s gender identity with their physical appearance. 2 - 4
While numerous surgical interventions can be considered GAS, the procedures have been broadly classified as breast and chest surgical procedures, facial and cosmetic interventions, and genital reconstructive surgery. 2 , 4 Prior studies 2 - 7 have shown that GAS is associated with improved quality of life, high rates of satisfaction, and a reduction in gender dysphoria. Furthermore, some studies have reported that GAS is associated with decreased depression and anxiety. 8 Lastly, the procedures appear to be associated with acceptable morbidity and reasonable rates of perioperative complications. 2 , 4
Given the benefits of GAS, the performance of GAS in the US has increased over time. 9 The increase in GAS is likely due in part to federal and state laws requiring coverage of transition-related care, although actual insurance coverage of specific procedures is variable. 10 , 11 While prior work has shown that the use of inpatient GAS has increased, national estimates of inpatient and outpatient GAS are lacking. 9 This is important as many GAS procedures occur in ambulatory settings. We performed a population-based analysis to examine trends in GAS in the US and explored the temporal trends in the types of GAS performed across age groups.
To capture both inpatient and outpatient surgical procedures, we used data from the Nationwide Ambulatory Surgery Sample (NASS) and the National Inpatient Sample (NIS). NASS is an ambulatory surgery database and captures major ambulatory surgical procedures at nearly 2800 hospital-owned facilities from up to 35 states, approximating a 63% to 67% stratified sample of hospital-owned facilities. NIS comprehensively captures approximately 20% of inpatient hospital encounters from all community hospitals across 48 states participating in the Healthcare Cost and Utilization Project (HCUP), covering more than 97% of the US population. Both NIS and NASS contain weights that can be used to produce US population estimates. 12 , 13 Informed consent was waived because data sources contain deidentified data, and the study was deemed exempt by the Columbia University institutional review board. This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We selected patients of all ages with an International Statistical Classification of Diseases and Related Health Problems, Tenth Revision ( ICD-10 ) diagnosis codes for gender identity disorder or transsexualism ( ICD-10 F64) or a personal history of sex reassignment ( ICD-10 Z87.890) from 2016 to 2020 (eTable in Supplement 1 ). We first examined all hospital (NIS) and ambulatory surgical (NASS) encounters for patients with these codes and then analyzed encounters for GAS within this cohort. GAS was identified using ICD-10 procedure codes and Common Procedural Terminology codes and classified as breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures. 2 , 4 Breast and chest surgical procedures encompassed breast reconstruction, mammoplasty and mastopexy, or nipple reconstruction. Genital reconstructive procedures included any surgical intervention of the male or female genital tract. Other facial and cosmetic procedures included cosmetic facial procedures and other cosmetic procedures including hair removal or transplantation, liposuction, and collagen injections (eTable in Supplement 1 ). Patients might have undergone procedures from multiple different surgical groups. We measured the total number of procedures and the distribution of procedures within each procedural group.
Within the data sets, sex was based on patient self-report. The sex of patients in NIS who underwent inpatient surgery was classified as either male, female, missing, or inconsistent. The inconsistent classification denoted patients who underwent a procedure that was not consistent with the sex recorded on their medical record. Similar to prior analyses, patients in NIS with a sex variable not compatible with the procedure performed were classified as having undergone genital reconstructive surgery (GAS not otherwise specified). 9
Clinical variables in the analysis included patient clinical and demographic factors and hospital characteristics. Demographic characteristics included age at the time of surgery (12 to 18 years, 19 to 30 years, 31 to 40 years, 41 to 50 years, 51 to 60 years, 61 to 70 years, and older than 70 years), year of the procedure (2016-2020), and primary insurance coverage (private, Medicare, Medicaid, self-pay, and other). Race and ethnicity were only reported in NIS and were classified as White, Black, Hispanic and other. Race and ethnicity were considered in this study because prior studies have shown an association between race and GAS. The income status captured national quartiles of median household income based of a patient’s zip code and was recorded as less than 25% (low), 26% to 50% (medium-low), 51% to 75% (medium-high), and 76% or more (high). The Elixhauser Comorbidity Index was estimated for each patient based on the codes for common medical comorbidities and weighted for a final score. 14 Patients were classified as 0, 1, 2, or 3 or more. We separately reported coding for HIV and AIDS; substance abuse, including alcohol and drug abuse; and recorded mental health diagnoses, including depression and psychoses. Hospital characteristics included a composite of teaching status and location (rural, urban teaching, and urban nonteaching) and hospital region (Northeast, Midwest, South, and West). Hospital bed sizes were classified as small, medium, and large. The cutoffs were less than 100 (small), 100 to 299 (medium), and 300 or more (large) short-term acute care beds of the facilities from NASS and were varied based on region, urban-rural designation, and teaching status of the hospital from NIS. 8 Patients with missing data were classified as the unknown group and were included in the analysis.
National estimates of the number of GAS procedures among all hospital encounters for patients with gender identity disorder were derived using discharge or encounter weight provided by the databases. 15 The clinical and demographic characteristics of the patients undergoing GAS were reported descriptively. The number of encounters for gender identity disorder, the percentage of GAS procedures among those encounters, and the absolute number of each procedure performed over time were estimated. The difference by age group was examined and tested using Rao-Scott χ 2 test. All hypothesis tests were 2-sided, and P < .05 was considered statistically significant. All analyses were conducted using SAS version 9.4 (SAS Institute Inc).
A total of 48 019 patients who underwent GAS were identified ( Table 1 ). Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged 12 to 18 years. Private insurance coverage was most common in 29 064 patients (60.5%), while 12 127 (25.3%) were Medicaid recipients. Depression was reported in 7192 patients (15.0%). Most patients (42 467 [88.4%]) were treated at urban, teaching hospitals, and there was a disproportionate number of patients in the West (22 037 [45.9%]) and Northeast (12 396 [25.8%]). Within the cohort, 31 668 patients (65.9%) underwent 1 procedure while 13 415 (27.9%) underwent 2 procedures, and the remainder underwent multiple procedures concurrently ( Table 1 ).
The overall number of health system encounters for gender identity disorder rose from 13 855 in 2016 to 38 470 in 2020. Among encounters with a billing code for gender identity disorder, there was a consistent rise in the percentage that were for GAS from 4552 (32.9%) in 2016 to 13 011 (37.1%) in 2019, followed by a decline to 12 818 (33.3%) in 2020 ( Figure 1 and eFigure in Supplement 1 ). Among patients undergoing ambulatory surgical procedures, 37 394 (80.3%) of the surgical procedures included gender-affirming surgical procedures. For those with hospital admissions with gender identity disorder, 10 625 (11.8%) of admissions were for GAS.
Breast and chest procedures were most common and were performed for 27 187 patients (56.6%). Genital reconstruction was performed for 16 872 patients (35.1%), and other facial and cosmetic procedures for 6669 patients (13.9%) ( Table 2 ). The most common individual procedure was breast reconstruction in 21 244 (44.2%), while the most common genital reconstructive procedure was hysterectomy (4489 [9.3%]), followed by orchiectomy (3425 [7.1%]), and vaginoplasty (3381 [7.0%]). Among patients who underwent other facial and cosmetic procedures, liposuction (2945 [6.1%]) was most common, followed by rhinoplasty (2446 [5.1%]) and facial feminizing surgery and chin augmentation (1874 [3.9%]).
The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020 ( Figure 1 ). Similar trends were noted for breast and chest surgical procedures as well as genital surgery, while the rate of other facial and cosmetic procedures increased consistently from 2016 to 2020. The distribution of the individual procedures performed in each class were largely similar across the years of analysis ( Table 3 ).
When stratified by age, patients 19 to 30 years had the greatest number of procedures, 25 099 ( Figure 2 ). There were 10 476 procedures performed in those aged 31 to 40 years and 4359 in those aged 41 to 50 years. Among patients younger than 19 years, 3678 GAS procedures were performed. GAS was less common in those cohorts older than 50 years. Overall, the greatest number of breast and chest surgical procedures, genital surgical procedures, and facial and other cosmetic surgical procedures were performed in patients aged 19 to 30 years.
When stratified by the type of procedure performed, breast and chest procedures made up the greatest percentage of the surgical interventions in younger patients while genital surgical procedures were greater in older patients ( Figure 2 ). Additionally, 3215 patients (87.4%) aged 12 to 18 years underwent GAS and had breast or chest procedures. This decreased to 16 067 patients (64.0%) in those aged 19 to 30 years, 4918 (46.9%) in those aged 31 to 40 years, and 1650 (37.9%) in patients aged 41 to 50 years ( P < .001). In contrast, 405 patients (11.0%) aged 12 to 18 years underwent genital surgery. The percentage of patients who underwent genital surgery rose sequentially to 4423 (42.2%) in those aged 31 to 40 years, 1546 (52.3%) in those aged 51 to 60 years, and 742 (58.4%) in those aged 61 to 70 years ( P < .001). The percentage of patients who underwent facial and other cosmetic surgical procedures rose with age from 9.5% in those aged 12 to 18 years to 20.6% in those aged 51 to 60 years, then gradually declined ( P < .001). Figure 2 displays the absolute number of procedure classes performed by year stratified by age. The greatest magnitude of the decline in 2020 was in younger patients and for breast and chest procedures.
These findings suggest that the number of GAS procedures performed in the US has increased dramatically, nearly tripling from 2016 to 2019. Breast and chest surgery is the most common class of procedure performed while patients are most likely to undergo surgery between the ages of 19 and 30 years. The number of genital surgical procedures performed increased with increasing age.
Consistent with prior studies, we identified a remarkable increase in the number of GAS procedures performed over time. 9 , 16 A prior study examining national estimates of inpatient GAS procedures noted that the absolute number of procedures performed nearly doubled between 2000 to 2005 and from 2006 to 2011. In our analysis, the number of GAS procedures nearly tripled from 2016 to 2020. 9 , 17 Not unexpectedly, a large number of the procedures we captured were performed in the ambulatory setting, highlighting the need to capture both inpatient and outpatient procedures when analyzing data on trends. Like many prior studies, we noted a decrease in the number of procedures performed in 2020, likely reflective of the COVID-19 pandemic. 18 However, the decline in the number of procedures performed between 2019 and 2020 was relatively modest, particularly as these procedures are largely elective.
Analysis of procedure-specific trends by age revealed a number of important findings. First, GAS procedures were most common in patients aged 19 to 30 years. This is in line with prior work that demonstrated that most patients first experience gender dysphoria at a young age, with approximately three-quarters of patients reporting gender dysphoria by age 7 years. These patients subsequently lived for a mean of 23 years for transgender men and 27 years for transgender women before beginning gender transition treatments. 19 Our findings were also notable that GAS procedures were relatively uncommon in patients aged 18 years or younger. In our cohort, fewer than 1200 patients in this age group underwent GAS, even in the highest volume years. GAS in adolescents has been the focus of intense debate and led to legislative initiatives to limit access to these procedures in adolescents in several states. 20 , 21
Second, there was a marked difference in the distribution of procedures in the different age groups. Breast and chest procedures were more common in younger patients, while genital surgery was more frequent in older individuals. In our cohort of individuals aged 19 to 30 years, breast and chest procedures were twice as common as genital procedures. Genital surgery gradually increased with advancing age, and these procedures became the most common in patients older than 40 years. A prior study of patients with commercial insurance who underwent GAS noted that the mean age for mastectomy was 28 years, significantly lower than for hysterectomy at age 31 years, vaginoplasty at age 40 years, and orchiectomy at age 37 years. 16 These trends likely reflect the increased complexity of genital surgery compared with breast and chest surgery as well as the definitive nature of removal of the reproductive organs.
This study has limitations. First, there may be under-capture of both transgender individuals and GAS procedures. In both data sets analyzed, gender is based on self-report. NIS specifically makes notation of procedures that are considered inconsistent with a patient’s reported gender (eg, a male patient who underwent oophorectomy). Similar to prior work, we assumed that patients with a code for gender identity disorder or transsexualism along with a surgical procedure classified as inconsistent underwent GAS. 9 Second, we captured procedures commonly reported as GAS procedures; however, it is possible that some of these procedures were performed for other underlying indications or diseases rather than solely for gender affirmation. Third, our trends showed a significant increase in procedures through 2019, with a decline in 2020. The decline in services in 2020 is likely related to COVID-19 service alterations. Additionally, while we comprehensively captured inpatient and ambulatory surgical procedures in large, nationwide data sets, undoubtedly, a small number of procedures were performed in other settings; thus, our estimates may underrepresent the actual number of procedures performed each year in the US.
These data have important implications in providing an understanding of the use of services that can help inform care for transgender populations. The rapid rise in the performance of GAS suggests that there will be a greater need for clinicians knowledgeable in the care of transgender individuals and with the requisite expertise to perform GAS procedures. However, numerous reports have described the political considerations and challenges in the delivery of transgender care. 22 Despite many medical societies recognizing the necessity of gender-affirming care, several states have enacted legislation or policies that restrict gender-affirming care and services, particularly in adolescence. 20 , 21 These regulations are barriers for patients who seek gender-affirming care and provide legal and ethical challenges for clinicians. As the use of GAS increases, delivering equitable gender-affirming care in this complex landscape will remain a public health challenge.
Accepted for Publication: July 15, 2023.
Published: August 23, 2023. doi:10.1001/jamanetworkopen.2023.30348
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Wright JD et al. JAMA Network Open .
Corresponding Author: Jason D. Wright, MD, Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, 161 Fort Washington Ave, 4th Floor, New York, NY 10032 ( [email protected] ).
Author Contributions: Dr Wright had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Wright, Chen.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Wright.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Wright, Chen.
Administrative, technical, or material support: Wright, Suzuki.
Conflict of Interest Disclosures: Dr Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Health Reporting in the States
Bill of the month: a plan for affordable gender-confirmation surgery goes awry.
Emmarie Huetteman

Wren Vetens was promised a significant discount on the cost of her gender-confirmation surgery if she paid in cash upfront, without using her health insurance. Yet afterward, Vetens received an explanation of benefits saying the hospital had billed her insurer nearly $92,000. Lauren Justice for KHN hide caption
Wren Vetens was promised a significant discount on the cost of her gender-confirmation surgery if she paid in cash upfront, without using her health insurance. Yet afterward, Vetens received an explanation of benefits saying the hospital had billed her insurer nearly $92,000.
Wren Vetens thought she'd done everything possible to prepare for her surgery.
She chose a doctoral program in physics at the University of Wisconsin-Madison, a school that not only embraced transgender students like her, but also granted insurance coverage for her gender-confirmation surgery when she enrolled in 2016. When uncertainty over the fate of an Obama-era anti-discrimination rule allowed the state to discontinue such coverage, Vetens and her mother, Kimberly Moreland, an OB-GYN, shopped for another plan.
Deducing the procedure would run from $19,000 to $25,000, based on prices posted online, they purchased insurance from Consolidated Health Plans. It would pay a maximum of $25,000 for the operation.
With that information in hand, Vetens planned ahead: She got her insurer's preapproval and scheduled surgery during winter break of her second year, allowing time for recovery before returning to her studies.
Tell Us Your Billing Story
Do you have a medical bill or explanation of benefits that you'd like us to see? Submit it here and tell us the story behind it .
We may use it, with your permission, in one of our monthly features.
So, she was shocked when a hospital representative called her a couple of months before the long-awaited surgery estimating the bill would be $100,000. That meant she would be on the hook for as much as $75,000 after her insurer's $25,000 payout.
With preparations for the surgery well underway, Vetens was feeling overwhelmed with stress. "There were days when I just couldn't get out of bed for a whole day," she said, describing two weeks of panic attacks.
After mother and daughter complained about the last-minute surprise, a hospital representative offered a solution: If they paid out of pocket and in full before Vetens' surgery — forgoing their use of insurance — the hospital would accept just $20,080, assuring them the hospital would charge nothing to Vetens' insurer. But if they did not decide and pay up right away, the surgery would be canceled.
"I certainly felt that I had no choice," Vetens said.
After Moreland gave the hospital her credit card number for payment, they thought the financial roller coaster was over and Vetens could focus on recovery.
Then the bill came.
Patient: Wren Vetens, then 23, a Ph.D. student at the University of Wisconsin-Madison
Total bill: $91,850.20
Insurance payment: $25,427.91
Vetens owed: $13,191.95 (after $20,080 that was counted as a deposit)
Service provider: University of Wisconsin Hospital in Madison
Medical treatment: Vetens underwent a procedure known as penile inversion vaginoplasty to address her diagnosis of gender dysphoria, a condition resulting from one's sex identified at birth being in conflict with one's gender identity.
The procedure, in which the patient's penile and scrotal tissue is used to create a vagina, generally takes about two to four hours and requires a short inpatient stay, according to Dr. Madeline Deutsch, the medical director for transgender care at the University of California, San Francisco.
Candidates for the procedure must live for at least one year in their identified gender role and undergo at least one year of hormone therapy, Deutsch said. Preparation also includes permanent hair removal.
What gives: Though gender dysphoria is relatively uncommon, many of the billing and insurance issues Vetens encountered are typical for patients planning major surgery. Much of her stress and frustration arose from the vast difference between online price estimates ($19,000-$25,000), the hospital's billed price to the insurer ($91,850) and what it was willing to accept as an upfront cash payment ($20,080).
Hospitals set list prices high because insurers with whom they have contracts typically negotiate them down. In exchange for charging an insurer's members a lower price, doctors and hospitals gain access to those customers, who have incentives to use these in-network providers. Hospitals may offer package deals for procedures to patients, if they pay cash upfront, in part because the hospital avoids the hassle of negotiation.
Officials at University of Wisconsin Hospital said they offered Vetens the option to pay $20,080 for these reasons: to secure extra experience and exposure for the hospital's programs for transgender patients, and to shield Vetens from an even bigger bill. "We were trying to protect the patient," said Dr. Katherine Gast, Vetens' surgeon.

Dr. Kimberly Moreland (left) helped her daughter shop for an insurance plan that would cover Vetens' gender-confirmation surgery. Yet mother and daughter still found themselves caught between the hospital and the insurer. Courtesy of Richard Malatesta/Kimberly Moreland hide caption
Dr. Kimberly Moreland (left) helped her daughter shop for an insurance plan that would cover Vetens' gender-confirmation surgery. Yet mother and daughter still found themselves caught between the hospital and the insurer.
As both parties hedged their bets in trying to determine what a penile inversion vaginoplasty was worth, Vetens was stuck in the middle with the prospect of hugely varying payments.
Lisa Brunette, a hospital spokeswoman, said that, despite having provided Vetens an estimate of $100,000, the hospital really did not know how much it would charge for the procedure because it did not know how much it would be reimbursed by the insurance company. Vetens was the second person to have the procedure at the hospital.
The spokeswoman for the hospital said its contract with Vetens' insurer "relies on a complex formula."
And in an apparent chicken-and-egg quandary, Drew DiGiorgio, president and chief executive of Consolidated Health Plans, said the insurer did not know how much it would reimburse because it did not know how much the hospital would charge.
When Moreland called the hospital to pay the $20,080 price — an option she acknowledged many simply could not afford — she asked for an itemized bill.
The next day, she received a brief letter outlining some of the general services included for the price, such as "physician's fee" and "post surgery labs." Then it simply said: "Penile Inversion Vaginoplasty — $20,080.00."
"How in the world did you come up with a number if you have no idea what it covers?" she asked.
Had Vetens chosen a hospital that did not contract with her insurer, the family could have been reimbursed 60 percent, or about $12,000 of the money paid, since her insurance pays a portion of out-of-network care.
But since Consolidated Health Plans has a contract with the University of Wisconsin Hospital, it said it would not reimburse anything at all. Contracts between insurers and providers discourage such sideline cash transactions, since hospitals can make more money when patients use insurance, as evidenced by Vetens' bill.
Vetens and Moreland appealed to Consolidated Health Plans, feeling that they had been "the victims of a bait-and-switch scam."
The surprises didn't end there. Though multiple hospital representatives reassured Vetens that they wouldn't charge her insurance after her cash payment, Vetens received an explanation of benefits saying the hospital had billed her insurer nearly $92,000.
A hospital bill followed, identifying their $20,080 as "pre-payment," treating it like a partial deposit. Vetens owed more than $13,000, it said.
Studies have shown that more than half of hospital bills contain errors , a problem made worse by the fact that medical bills — with codes and jargon — can be nearly impossible for even savvy patients to understand.
"That was not supposed to happen. That was an error," said Abby Abongwa, a hospital billing official. "That was absolutely an error on our part."
Resolution: After the bill for $91,850 arrived, an alarmed Vetens showed it to her surgeon. The hospital quickly apologized and repaid her insurance company.
Within a few weeks of receiving the appeal — which noted that Vetens and Moreland had contacted a national media outlet — Consolidated Health Plans reimbursed Vetens nearly $18,000, offering her no explanation for why the company had ultimately decided to reverse its earlier judgement that it would not pay anything toward her care.
With their reimbursement, Vetens and Moreland paid about $2,100 for the surgery, all told.
The Takeaway: Be mindful that online pricing estimates frequently represent cash prices, which are often far lower than the price hospitals will bill your insurance.
Ask about a cash price — you may get a better deal. But if you forgo insurance, you're on your own. Your insurer is under no obligation to pay you back for any part of the bill or help you troubleshoot billing, and any payment you make likely will not count toward your deductible.
Enlist your doctor's help. Gast, Vetens' surgeon, proved a powerful advocate for her patient when disputes arose about billing and pricing. Billing representatives might not always be responsive to patients, but it's in the hospital executives' interest to keep staff surgeons happy.
Some of these issues can be settled only through legislation. Right now, there is no legal requirement for hospitals to provide itemized bills to patients. Hospital bills are fraught with errors, and there is little accountability for providers who bill erroneously.
In the meantime, don't be afraid to ask questions and fight back.
Bram Sable-Smith, who contributed to the audio story, is part of NPR's reporting partnership with Side Effects Public Media, member station KBIA and Kaiser Health News.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of the Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
You can follow Emmarie Huetteman on Twitter: @emmarieDC .
- bill of the month
- gender dysphoria
- gender identity
- transgender
- Health Insurance
- Plastic surgery
Thomas Barwick / Getty Images
Advertiser Disclosure
Guide to paying for gender reassignment surgery
Not every trans person opts for surgery, but here's what you need to know if you're considering it
Published: June 3, 2021

Author: Elly Belle

Editor: Adriana Ocañas

Reviewer: Antonio Ruiz-Camacho
How we Choose
With queer and trans people constantly under attack from waves of legislation and discrimination directly targeting them, taking a direct stand against the hate is one of the most impactful actions. Pride month isn’t the only time we should be learning how we can do our part to support people…
The content on this page is accurate as of the posting date; however, some of our partner offers may have expired. Please review our list of best credit cards , or use our CardMatch™ tool to find cards matched to your needs.
With queer and trans people constantly under attack from waves of legislation and discrimination directly targeting them, taking a direct stand against the hate is one of the most impactful actions.
Pride month isn’t the only time we should be learning how we can do our part to support people in the LGBTQIA+ community, including the estimated 1.4 million U.S. adults who identify as transgender, but it is an opportune moment to take stock and understand their experiences.
See related: Guide to LGBT finances: You can live a richer life
A few important things to understand about sex, gender and trans people
Sex and gender are not the same thing – and gender is often more personal and culturally constructed. While sex is someone’s biological and physiological characteristics, a person’s gender is the behaviors, roles, expectations and activities they relate to in society.
Not everyone identifies with the sex they were assigned at birth, and thanks to more exposure in pop culture and the amplifying of trans people’s voices, people are increasingly starting to explore their gender identity.
Another important thing to know and consider is transgender people exist everywhere and come from all kinds of backgrounds. They come from all walks of life and of all ethnicities and races. And what it means and looks like to be trans will be different for each person, which is why it’s so critical not to make blanket assumptions about transness.
In many places, it’s still dangerous to be openly trans, and not all trans people are even remotely safe to present as who they truly are inside. Wearing the clothing, makeup or other external accessories that make them feel most affirmed and like themselves is not always possible.
For this and many other reasons, it’s important to remember that you can’t tell someone’s gender just by looking at them.
Gender reassignment procedures
Those who want to transition physically or externally have many different options, from getting gender reassignment procedures and buying a new wardrobe and accessories that match their gender, to choosing against surgery.
Trans people can also transition without surgery or medical procedures by changing their clothing, pronouns, name and gender presentation. Either way, money can often be a barrier for trans folks, and getting accurate information about the costs of transitioning can be a hurdle in and of itself.
For those who do wish to get surgery to alleviate gender dysphoria and have a body that matches their gender (and are at least 18 years of age, in most cases), the costs vary significantly depending on details like insurance coverage and location.
Types of surgeries and their costs
The types of surgeries that trans people seek are more informally known as top surgery, which is a reconstructive surgery that alters the appearance of the chest, either taking breasts away for a more masculine/flat chest or adding breasts for those who want to appear more feminine. Top surgeries are performed by a plastic surgeon with training in transgender and gender-affirming medical procedures.
Bottom surgery refers to vaginoplasty, phalloplasty or metoidioplasty, all various procedures that change a person’s genitals to match their gender. Trans women might also opt for facial feminization surgery, so their facial features match how they want to see themselves.
Hormone replacement therapy (HRT) is also a popular mode of transitioning and involves using testosterone or estrogen to reach one’s desired gender presentation.
These methods are not just for binary trans people, or trans men and women, either. Non-binary people and genderqueer people might medically or hormonally transition as well.
The cost breakdown includes:
How to budget for the costs of transitioning
Transitioning isn’t limited to medical costs and procedures. Other things to budget for include post-surgery care or even buying new clothes that match your gender presentation and make you feel affirmed in your identity. It might also include makeup and accessories that help you feel like yourself. And of course, for trans women and transfemmes, much of this will include the pink tax .
Everyday costs
“So far, it’s all been relatively manageable. But I will say that trying to cultivate a wardrobe with gender-affirming looks and clothing has been the most expensive,” says Evelyn, a trans woman who began transitioning within the last half-year. “The biggest thing as a trans woman that has surprised me is shoes. Mainly women’s shoes usually only go up to about 11-12. I have a size 14-15, so most of the time, I would have to order from special stores, or places that custom-make shoes for drag queens.”
Buying new clothing and accessories is not the only option, though. You can do clothing swaps with other trans people, go thrifting or ask friends if they have old clothes they want to get rid of that match your new gender presentation.
Clothing and makeup, despite how expensive they can be, have brought the most joy to Evelyn. “My personality is very extra and outgoing and colorful, and my male-passing clothing always were dull and very narrow fitting. Now, I am buying all these flowy cardigans and scarves and really living my Stevie Nicks meets City girl dreams,” she says.
“I feel so powerful and so happy when I walk around, and the wind picks up my long cardigan and I move with a grace I didn’t think I would ever be able to have.” Despite how much costs can weigh you down, the people who spoke with us explain that transition feels freeing.
Sasha, a Latinx non-binary trans woman who began HRT in January 2020, says that her job in tech and excellent health insurance is what’s made it possible for her to afford transitioning. The most expensive part of her transition, she says, has been hair removal.
“I have spent thousands of dollars on both laser and electrolysis. I looked at my credit card history and to date, I’ve spent $5,003.25 on electrolysis (with probably another $1,500 or so before I’m totally clear of facial hair). As for laser for body hair, I have paid around $3,000 for it so far.”
In total, Sasha has spent about $8,000 just on hair removal, and she says she still has $2,000 or more to go. “This has been far and away the most expensive part of transition because insurance won’t cover it. They will only cover electrolysis for preparation for bottom surgery,” Sasha says.
There are some important things she wishes she’d been told earlier, like the costs and benefits of laser versus electrolysis. While electrolysis is more expensive and takes a longer time, it permanently removes hair. Laser is faster and cheaper but not permanent.
“I decided to go with laser early on in my transition because it was cheaper and seemed to be a good option at the time. For facial hair removal, I would’ve liked to have started out with electrolysis because although it is a slower process, the results are for life. So, I wasted some time and some money on laser for my face early on that I wish I hadn’t,” she says.
Although surgeries and other medical necessities have certainly helped Sasha transition, some of the most affirming purchases she has made in the last few years are accessories that help her feel gender euphoric.
“I bought these leather high-heeled boots that I absolutely love. Playing with makeup is something I always wanted to do and since allowing myself the pleasure, I’ve had so much fun trying different eyeshadows and lipsticks,” she says.
Alex, who has been out as a nonbinary trans woman since 2017, says she’s been most surprised by how quickly transition expenses add up. “They are wildly inaccessible to those without disposable income and require maintenance,” she says of things like budgeting for nail and hair appointments and medspa procedures (like laser hair removal, Botox and fillers).
Legal costs
When transitioning, some people choose to legally change their names and some don’t. The costs can vary depending on where you live. For Sasha, it cost $350 to get a court-ordered name change and publish her name change in a local paper, which is a legally required part of the process.
“I wouldn’t have had to pay that if I had had a legal counsel that guided me through the process of waiving those fees, which is totally possible, but I didn’t know how to navigate it,” she says. Once her name change is official, she’ll also have to pay for copies of the court order.
See related: Major issuers slow to adopt Mastercard True Name card
Social costs
The costs of transitioning are also not simply financial. Trans people who choose to live openly often face discrimination, rejection and even violence. Black trans women and trans women of color face these dangers the most. The risk of being fired from a job, bullied or harassed at work or having to move to an entirely new community because of transphobia is also high.
Some of the social costs of transitioning that Alex says she’s experienced include “ongoing stress and hypervigilance when in public, and exhaustion from being hyper-focused on how I’m being perceived by others.”
However, there are also positive, affirming social experiences that come with transition – and that joy is just as important to acknowledge and to be able to look forward to.
The pieces of clothing that Alex has invested in that have made her feel like her truest self include crop tops and big pants, neutral blushes and lipstick and skin tints. And the most affirming experience she’s had related to her transition has been relearning what sex and pleasure feels like in her changing body, she explains.
Options on how to pay
Crowdfunding, loans and credit cards are some of the main ways that trans women who spoke with us said they’ve been able to pay for medical bills.
Like Sasha explained, even if you have insurance or a well-paying job, some costs are just too great, and insurance doesn’t cover everything.
Other options to pay for the numerous costs listed above include:
- Personal loan from a credit union: Although credit unions provide virtually all of the same services and products as banks, their goal is to enable members to borrow at the lowest possible cost.
- Credit cards: A 0% APR credit card may be your best option as many offer introductory APR periods of usually 12 months or longer.
- Home equity line of credit: A HELOC is a variable-rate home equity product that works like a credit card – you have access to a credit line that you can draw from and pay back as needed.
- CareCredit: Instead of an open-ended date to pay off your debt (like with a regular credit card), a CareCredit credit card has fixed monthly payments over a set term ranging from six months to 60 months.
- Online personal loan : A personal loan is best for people who may need more time to pay down their balances. You’ll get a low fixed rate that can last for several years.
- Family loan: If a family member is willing to help, make sure to formalize the deal by writing up a contract that includes terms, dates and conditions.
- Crowdfunding: GoFundMe and Indiegogo are great examples of crowdfunding platforms.
- Surgery grants: Point of Pride, Genderbands and The Jim Collins Foundation are all great places to start when looking at this option.
See related: When should you use medical credit cards?
Allyship to trans people
“It is still a very dangerous thing to be trans in the world. I am extremely privileged and due to my job and the resources I have, I can shield myself from many of the hardships a lot of other trans people face. Most trans folks don’t have that luxury,” Sasha says.
The best way to support trans people is to give to them directly, she explains. Donating to transition funds is crucial. “If you see a way that directly supports a trans person’s housing, surgeries, HRT, food, etc., whether that be through a GoFundMe, Venmo, or whatever, if you have the resources, give! Especially to Black and Indigenous trans folks,” she says.
“For cis allies, I challenge you to really listen to trans people. I find that when I speak to cis allies, they do a lot of talking and not a lot of listening. Listen to what trans people tell you about what their experience is like living in this world. It will help you understand how to be a better ally.”
Speaking out against transphobia, sharing your own pronouns and respecting others’ pronouns is yet another important way to support trans people. Doing all these things even when you don’t think there are any trans people to hear it or see it is especially necessary. Because not everyone is able to be or wants to be openly trans, you never know what these actions might mean to someone.
Cis people as well as trans people can embrace their unique gender identities in many ways by “cultivating self-reflective practices that make space for you to think about your gender instead of taking it for granted,” says Alex.
“Everyone, cis or not, has their own relationships to gender. Not all cis people adhere to gender roles in the same way. We are all unique and it’s misleading to think that only trans people divert from gender expectations.”
Even if you’re cisgender, embracing your own unique gender identity and exploring your gender presentation can be eye-opening. Understanding your own gender could help you care more about understanding and respecting other people’s, and stands to give you deeper self-knowledge.
Editorial Disclaimer
The editorial content on this page is based solely on the objective assessment of our writers and is not driven by advertising dollars. It has not been provided or commissioned by the credit card issuers. However, we may receive compensation when you click on links to products from our partners.
Essential reads, delivered straight to your inbox
Stay up-to-date on the latest credit card news 一 from product reviews to credit advice 一 with our newsletter in your inbox twice a week.
By providing my email address, I agree to CreditCards.com’s Privacy Policy
Your credit cards journey is officially underway.
Keep an eye on your inbox—we’ll be sending over your first message soon.
Learn more about To Her Credit

Texas abortion law: What it means, what happens next
The passage of S.B. 8 in Texas has lead to protests on both sides of the argument, statements from the White House and questions about where this leaves citizens of the state who are seeking a safe abortion. Find out more about the law and how you can provide aid to Texans who are impacted by it.

Navigating financial help when leaving an abusive relationship
Women and food insecurity – and what you can do to help
How chronic migraines have shaped my financial independence
Menstrual products now classified as qualified medical expenses
Women and financial anxiety: How fear impacts financial independence
Explore more categories
- Card advice
- Credit management
Questions or comments?
Editorial corrections policies
CreditCards.com is an independent, advertising-supported comparison service. The offers that appear on this site are from companies from which CreditCards.com receives compensation. This compensation may impact how and where products appear on this site, including, for example, the order in which they may appear within listing categories. Other factors, such as our own proprietary website rules and the likelihood of applicants' credit approval also impact how and where products appear on this site. CreditCards.com does not include the entire universe of available financial or credit offers. CCDC has partnerships with issuers including, but not limited to, American Express, Bank of America, Capital One, Chase, Citi and Discover.
Since 2004, CreditCards.com has worked to break down the barriers that stand between you and your perfect credit card. Our team is made up of diverse individuals with a wide range of expertise and complementary backgrounds. From industry experts to data analysts and, of course, credit card users, we’re well-positioned to give you the best advice and up-to-date information about the credit card universe.
Let’s face it — there’s a lot of jargon and high-level talk in the credit card industry. Our experts have learned the ins and outs of credit card applications and policies so you don’t have to. With tools like CardMatch™ and in-depth advice from our editors, we present you with digestible information so you can make informed financial decisions.
Our top goal is simple: We want to help you narrow down your search so you don’t have to stress about finding your next credit card. Every day, we strive to bring you peace-of-mind as you work toward your financial goals.
A dedicated team of CreditCards.com editors oversees the automated content production process — from ideation to publication. These editors thoroughly edit and fact-check the content, ensuring that the information is accurate, authoritative and helpful to our audience.
Editorial integrity is central to every article we publish. Accuracy, independence and authority remain as key principles of our editorial guidelines. For further information about automated content on CreditCards.com , email Lance Davis, VP of Content, at [email protected] .
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Understanding Insurance Requirements for Gender Affirmation Surgery
- Type of Surgeries
- Barriers to Access
- WPATH Standards
Restrictions to Coverage
Getting started, what you can do.
Insurance coverage for orchiectomy, genitoplasty, and other types of gender-affirmation surgery is largely governed by standards issued by the World Professional Association for Transgender Health (WPATH). Many health insurance providers use these guidelines to direct which procedures are medically necessary. However, not every insurer—or state—does.
Because acceptance of WPATH guidelines can vary, it can sometimes be hard to determine which procedures are covered by your health plan and whether gender affirmation is even affordable.
This article describes the types of surgeries pursued by transgender or gender-nonconforming people as a part of gender affirmation and the barriers they face. It also explains the WPATH standards of care for each type of surgery, how insurance companies use them to determine eligibility, and what restrictions are imposed by providers or states.
Gender-affirmation surgery is the preferred term but gender-confirmation surgery and gender-alignment surgery can also be used. Outdated terms like "sex reassignment" or "sex change" should not be used.
Gender affirmation reflects the process a person goes through when they begin to live as their authentic gender rather than the gender assigned to them a birth.
Medical or surgical procedures are only one facet of gender affirmation.
Types of Gender-Affirmation Surgery
Not all transgender, non-binary , and genderqueer individuals want surgery to align their bodies to their gender identity. Some people are content with social or other medical transition options .
Others want one or more surgeries, including those referred to as " top surgery ” (occurring above the waist) and "bottom surgery" (occurring below the waist).
An extensive national survey of transgender people found that:
- 66% of transgender women either had or wanted vaginoplasty or labiaplasty .
- 51% of transgender women either had or wanted breast augmentation.
- 50% of transgender women either had or wanted facial feminization (surgery to make a face appear more feminine).
- 37% of transgender women either had or wanted a tracheal shave (removal of the Adam’s apple).
- 58% of transgender women either had or wanted orchiectomy (removal of the testicles).
- 22% of transgender men either had or wanted phalloplasty (the creation of a penis).
- 27% of transgender men either had or wanted metoidioplasty (surgery that uses existing genitalia to create a penis).
- 97% of transgender men either had or wanted chest reconstruction or mastectomy (removal of the breasts).
- 71% of transgender men either had or wanted a hysterectomy (removal of the uterus).
Common Barriers to Gender-Affirmation Surgery
Cost, surgeon availability, and a process referred to "gatekeeping" are three major hurdles commonly faced by people undergoing gender affirmation.
Cost is one of the primary reasons people have limited access to gender-affirmation surgeries. Historically, most public or private insurance companies have not covered these procedures. Fortunately, that is changing.
Some public and private insurance companies cover some or all gender-affirmation surgery options. But that coverage often comes with many hoops that people need to jump through. It is also not available to all people in all states.
Surgeon Availability
Another major factor limiting access to surgery is the small number of surgeons trained to perform them. These surgeons, particularly very experienced ones, are often booked months or years in advance.
In addition, many don’t take insurance. Fortunately, as insurance coverage for gender-affirmation surgeries has increased, so too has physician interest in training. Today, there are many hospitals across the country that routinely perform vaginoplasty and accept insurance to pay for them.
"Gatekeeping"
Another barrier is a process called “gatekeeping" currently endorsed by WPATH. Gatekeeping involves undergoing a significant therapy or psychiatric assessment before they are allowed to transition medically.
It is a process that attracted considerable debate given that this level of scrutiny is not required for other major surgeries. It ultimately places the decision in the hands of a psychiatrist who can determine if a person is mentally "fit" to pursue treatment.

Discrimination and Stigma
In addition to barriers like cost and surgeon availability/competency, there is also a long history of discrimination and stigma limiting transgender patients’ access to care.
Insurance and the WPATH Standards
When determining eligibility for gender-affirming surgery coverage, many insurers turn to the WPATH Standards of Care to inform their eligibility guidelines. These are also known as the WPATH criteria or WPATH requirements.
WPATH updates its guidelines every five to 10 years. These standards of care help define which treatments are medically necessary and under which conditions they should be authorized. The standards have become less restrictive over time, reflecting the growing recognition of gender diversity in society.
The standards of care are broadly described as follows:
Standards for Top Surgery
“Top surgery” refers to gender-affirmation surgery of the breast or chest. For transmasculine people, this surgery is called chest reconstruction. For transfeminine people, it is breast augmentation.
The WPATH criteria for top surgery include:
- Persistent, well-documented gender dysphoria (distress caused by the difference between a person’s gender and the gender they were assigned at birth)
- The ability to make an informed decision and consent to treatment
- Any significant medical or mental health conditions are “reasonably well controlled”
Standards for Hormone Therapy
It is important to note that hormone therapy is not required for these surgeries. However, a year of hormone therapy is recommended for transgender women because it allows them to get the maximum possible breast growth without surgery, which improves surgical outcomes.
For transgender men, there is no hormone requirement or recommendation. That’s because some transmasculine people are only dysphoric about their chests. Therefore, they do not want or need testosterone treatment.
There are also several physical and psychological reasons people choose to undergo top surgery without hormone use. That said, people who are taking testosterone and are very active may wish to wait a year for surgery because testosterone and exercise can significantly reshape the chest. Therefore, waiting a year may result in a more aesthetic outcome.
Standards for Orchiectomy, Hysterectomy, and Ovariectomy
These surgeries involve the removal of the testicles (orchiectomy), uterus (hysterectomy), or ovaries (ovariectomy).
WPATH criteria for these surgeries include:
- Persistent, well-documented gender dysphoria
- Any significant medical or mental health conditions are “well controlled”
- At least 12 continuous months of appropriate hormone therapy, unless there are reasons someone can’t or won’t take hormones. The purpose of this guideline is so that people can experience reversible hormone changes before they undergo irreversible ones.
Surgeries to remove the gonads (testes, ovaries) and the uterus may be performed independently. They may also be performed alongside other gender-affirmation surgeries.
Removing the gonads alone can lower the amount of cross-sex hormone therapy required to get results. In addition, removing the uterus or cervix eliminates the need to screen those organs. That’s important because those screening exams can cause dysphoria and discomfort in many transgender men.
Standards for Vaginoplasty, Phalloplasty, and Metoidioplasty
This group of surgeries constructs a vagina (vaginoplasty) or penis (phalloplasty, metoidioplasty). These procedures make a person’s genitalia more in line with their gender identity.
- Any significant medical or mental health conditions are “well controlled”
- Appropriate hormone therapy for 12 continuous months, unless there are reasons why someone can’t or won’t take hormones
- Living in a gender role that is consistent with their gender identity for 12 continuous months
The requirement for a year of living in a gender role is because it gives people time to adjust to their desired gender. In addition, doctors widely believe that a year is a sufficient time for that adjustment before undergoing a complicated, expensive, and irreversible surgery.
Aftercare for these surgeries can be emotionally intense and difficult. For example, following vaginoplasty , consistent vaginal dilation is required to maintain depth and girth and avoid complications. These requirements can sometimes be challenging for people with a history of sexual trauma.
Aftercare Recommendations
Due to these surgeries’ physical and emotional intensity, experts recommend that those considering them have regular visits with a mental or medical health professional.
Standards for Facial Feminization Surgery
There are no formal guidelines for facial feminization surgery. In addition, it has historically been tough to get this procedure covered by insurance due to a lack of research on the benefits.
However, some individuals have been able to have it successfully covered by arguing that it is as medically necessary as genital surgery and has equally positive effects on quality of life.
Standards for Children and Adolescents
WPATH guidelines for children and adolescents include criteria for fully reversible interventions ( puberty blockers that pause puberty, for example) or partially reversible ones (hormones, for example). However, they do not recommend irreversible (surgical) interventions until the age of majority in their given country.
One exception is chest surgery for transmasculine adolescents. WPATH criteria suggest this could be carried out before adulthood, after ample time of living in their gender role, and after being on testosterone treatment for one year.
Despite the increasing uptake of WPATH guidelines by insurers, not every organization embraces them or applies them in the same way. Even WPATH notes that “the criteria put forth in this document... are clinical guidelines. Individual health professionals and programs may modify them.” And many times, they do.
Generally speaking, private insurance companies are more likely to offer coverage for some or all procedures than government agencies like Medicaid and Medicare. Even so, eligibility requirements can vary as can copayment and coinsurance costs.
Medicaid is the U.S. government health coverage program for low-income people, jointly funded by the federal government and states. Of the estimated 1.4 million transgender adults living in the United States, approximately 152,000 have Medicaid coverage, according to the Kaiser Family Foundation.
Many state Medicaid programs cover aspects of gender-affirming health services. But only two states—Maine and Illinois—cover all five WPATH standards of care as of October 2022 (hormone therapy, surgery, fertility assistance, voice and communication therapy, primary care, and behavioral intervention).
Current Medicaid Coverage Status
In terms of gender-affirming surgery, 23 states provide coverage for adults, while nine states (Alabama, Arizona, Florida, Hawaii, Iowa, Kansas, Missouri, Texas, and Wyoming) currently deny coverage. The remaining states either have no policies in place or offer no reporting of coverage.
Medicare is federal health insurance for people 65 or older and some younger people with disabilities. Original Medicare (Part A and Part B) will cover gender-affirmation surgery when it is considered medically necessary. Prior to 2014, no coverage was offered.
The challenge with accessing surgery is that Medicare has no national precedent for approving or denying coverage. As such, approval or denial is based largely on precedents within your state and is conducted on a case-by-case basis.
This suggests that approval may be more difficult in states that deny coverage to Medicaid recipients given that Medicare is administered by a central agency called the Centers for Medicare & Medicaid Services (CMS).
As a general guideline, the CMS states that the following is needed for you to be an eligible candidate for gender-affirmation surgery:
- Have a diagnosis of gender dysphoria
- Provide proof of counseling
- Provide evidence of hormone therapy (for transgender women)
If coverage is denied, there is an appeal process you can undergo to overturn the denial.
Private Insurance
Most private insurance companies in the United States will offer coverage for some—but not necessarily all—gender-affirming surgeries.
According to the Transgender Legal Defense & Education Fund (TLDEF), many of the larger insurers offer coverage for a comprehensive array of surgeries, including providers like:
- Blue Cross/Blue Shield
- UnitedHealthcare
Others have different standards in different states (such as AmeriHealth) or only offer coverage for specific surgeries like facial feminization surgery (Prestige and AmeriHealth New Hampshire).
Though coverage of gender-affirmation surgery is increasing, many private insurers still require you to meet extensive criteria before approval is granted. By way of example, to get approval for breast augmentation, a transgender woman would need to provide a company like Aetna:
- A signed letter from a qualified mental health professional stating their readiness for physical treatment as well as their capacity to consent to a specific treatment
- Documentation of marked and sustained gender dysphoria
- Documentation that other possible causes of gender dysphoria have been excluded
- The completion of six to 12 months of hormone therapy
- A risk assessment of breast cancer screening by a qualified healthcare provider
Even if approval is granted, copayment, coinsurance, and out-of-pocket costs can vary, often considerably.
Out-of-Pocket Costs
According to a 2022 study from Oregon Health & Science University, a transgender person who underwent "bottom" surgery from 2007 to 2019 paid an average of $1,781 out of pocket.
With that said, 50% had to leave their state due to the restriction or unavailability of gender-affirmation surgery and ended up paying an average of $2,645 out of pocket, not including travel or living expenses.
Showing that a person has “persistent, well-documented gender dysphoria” usually requires a letter from a mental health provider. This letter usually states that the person meets the criteria for gender dysphoria, including the length of time that has been true.
This letter often also contains a narrative of the person’s gender history in detail. In addition, the letter should state how long the provider has been working with the person.
Well or Reasonably Controlled
It is important to note that some standards require that medical and mental health problems be well controlled, while others only require them to be reasonably well controlled. Documentation of this is also usually in a letter from the relevant healthcare provider.
This letter should contain information about the history of the condition, how it is controlled, and the length of the clinician’s relationship with the person. Ideally, the phrases “well controlled” or “reasonably well controlled” are used in the letter as appropriate.
Using terminology referenced in the WPTH criteria makes it easier for providers and insurance companies to determine that the conditions of the standards of care have been met.
Of note, mental health conditions are not a contraindication for gender affirmation surgeries. In fact, these procedures can help resolve symptoms in many transgender people and others with gender dysphoria. Symptom relief is true not just for anxiety and depression but for more severe conditions such as psychosis.
Getting insurance coverage for gender confirmation surgery can be a frustrating process. However, it can help to prepare a copy of the WPATH guidelines and any relevant research papers to support your goals. That’s particularly true if they include surgeries other than those listed above.
In addition, it may be a good idea to reach out to your local LGBT health center for assistance. Many health centers are now hiring transgender patient navigators who have extensive experience with the insurance process. They can be a great resource.
Local and national LGBTQ-focused legal organizations often have helplines or access hours where people can seek information.
Gender-affirmation surgery refers to various surgeries that allow people to align their bodies with their gender. WPATH guidelines offer criteria for determining whether someone is a good candidate for gender-affirmation surgery.
Not all insurance offers coverage for gender-affirmation surgery, but some do. First, however, you need to provide the proper documentation to show that you meet specific surgery criteria. This documentation is usually in a letter written by your physician or mental health clinician.
Morrison SD, Capitán-Cañadas F, Sánchez-García A, et al. Prospective quality-of-life outcomes after facial feminization surgery: an international multicenter study . Plast Reconstr Surg . 2020;145(6):1499-1509. doi:10.1097/PRS.0000000000006837
National Center for Transgender Equality. The report of the 2015 U.S. transgender survey .
World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people, 7th version .
Kaiser Family Foundation. Update on Medicaid coverage of gender-affirming health services .
CMS.gov. Gender dysphoria and gender reassignment surgery .
Transgender Legal Defense & Education Fund. Health insurance medical policies: gender dysphoria / gender reassignment .
Aetna. Gender-affirming surgery .
Downing J, Holt SK, Cunetta M, Gore JL, Dy GW. Spending and out-of-pocket costs for genital gender-affirming surgery in the US . JAMA Surg. 2022;157(9):799-806. doi:10.1001/jamasurg.2022.2606
Meijer JH, Eeckhout GM, van Vlerken RH, de Vries AL. Gender dysphoria and co-existing psychosis: review and four case examples of successful gender affirmative treatment . LGBT Health . 2017;4(2):106-114. doi:10.1089/lgbt.2016.0133
By Elizabeth Boskey, PhD Elizabeth Boskey, PhD, MPH, CHES, is a social worker, adjunct lecturer, and expert writer in the field of sexually transmitted diseases.
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Study: Paying for Transgender Health Care Cost-Effective
Most health insurance plans do not cover care associated with transitioning to the opposite sex.
A new analysis led by the Johns Hopkins Bloomberg School of Public Health suggests that while most U.S. health insurance plans deny benefits to transgender men and women for medical care necessary to transition to the opposite sex, paying for sex reassignment surgery and hormones is actually cost-effective.
The researchers, reporting online in the Journal of General Internal Medicine , say that the cost of surgery and hormones is not significantly higher than the cost of treatment for depression, substance abuse and HIV/AIDS, all of which are highly prevalent in those who are transgender but are not in a position to medically transition to the opposite sex. In 2014, the Center for Medicare and Medicaid Services began paying for sex reassignment surgery and other transitional care, after a 33-year-ban on covering those costs was lifted.
“Providing health care benefits to transgender people makes economic sense,” says study leader William V. Padula, PhD, MS, MSc, an assistant professor of health policy and management at the Bloomberg School. “Many insurance companies have said that it’s not worth it to pay for these services for transgender people. Our study shows they don’t have an economic leg to stand on when they decide to deny coverage. This is a small population of people and we can do them a great service without a huge financial impact on society.”
Estimates vary widely but it is believed that between 3,000 and 9,000 Americans undergo sex reassignment surgery each year. Transition medical care can include hormone replacement therapy, mastectomy, plastic surgery, psychotherapy and more.
For their study, Padula and colleagues analyzed data from the 2011 National Transgender Discrimination Survey, which includes information on access to medical care and health outcomes, as well as the Healthcare Bluebook, which outlines the cost of medical services. They also looked at previously published research on the topic.
When determining cost-effectiveness of medical services in the U.S., policymakers consider something cost-effective if the price is below $100,000 per year of quality of life. In the first five years, the researchers found, providing health care for transgender people cost between $34,000 and $43,000 per year of quality of life; after 10 years, the cost dropped to between $7,000 and $10,000 per year of quality of life.
Padula likens the case of paying for transgender care to caring for people with rare diseases. For example, cystic fibrosis affects just 30,000 people in the United States but can be treated as a chronic condition with the availability of new medications at a cost of $300,000 per year. While this is neither cost-effective nor individually affordable, Padula says, society has decided to pay for the treatment out of compassion. The same can be done for transgender people, he says.
Health insurance policies also pay for treatments that can be considered elective, such as breast reduction and spinal fusion as well as medication for erectile dysfunction. Some employers and health insurance companies do offer at least one plan that covers transition care, but that is not the norm, Padula says.
“Most U.S. health insurance policies still contain transgender exclusions, even though treatment of gender identity disorder is neither cosmetic nor experimental,” he says.
The new analysis calculated that the cost to cover transgender people would be fewer than two pennies per month for every person with health insurance coverage in the United States.
“We would be paying a very small incremental amount to improve the quality of life for a population that is extremely disenfranchised from health care and other services we consider a right,” Padula says. “For this small investment for a small number of people, we could improve their lives significantly and make them more productive members of society.”
He says that providing sex-reassignment surgery and other services to transgender people could help mitigate the expenses of treating depression, which often occurs in people who cannot transition, often because they do not have the financial means, as well as drug abuse and HIV/AIDS.
“ Societal Implications of Health Insurance Coverage for Medically Necessary Services in the U.S. Transgender Population: A Cost-Effectiveness Analysis ” was written by William V. Padula, Shiona Heru and Jonathan D. Campbell. Heru worked with the Commonwealth of Massachusetts Group Insurance Commission and Campbell is with the University of Colorado.
Funding for this study includes an F32 National Research Service Award from the Agency for Healthcare Research and Quality, a University of Chicago Medicine Small Grant in Diversity Research and a merit fellowship from Western New England University School of Law in affiliation with the Gender and Sexuality Center.
Media contacts for the Johns Hopkins Bloomberg School of Public Health: Stephanie Desmon at 410-955-7619 or [email protected] and Susan Murrow at 410-955-7624 and [email protected] .
How Much Does Transgender Surgery Cost
With modern technology, nothing seems impossible nowadays – not even changing your gender. Setting aside everyone’s take and belief regarding the procedure, let’s discuss how much does transgender surgery cost ?
Average Cost of Transgender Surgery
Transgender surgery is comprised of several surgical procedures that you can avail individually or as a package. The average transgender surgery cost for each procedure typically ranges from $1,500 to $26,000 but the total for all could be as high as $200,000 to $300,000.
Replacing the core reproductive organ completes the entire sexual reassignment. The male-to-female vaginoplasty is estimated to be somewhere between $20,000 and $50,000 or even higher . For the female-to-male phalloplasty and complete testicular implantation, the total cost could climb up to $25,000 to $35,000 .
Procedures Included
As previously implied, transgender surgery doesn’t only revolve around gender reassignment. It also involves almost the entire anatomy of the person.
This is due to the fact that the people who consider such procedures experience gender dysphoria or the feeling of misalignment between gender and sex. For the same reason, it is crucial to be able to transform every single part of the body into exactly like the gender one is identifying themselves with.
There are two types of gender confirmation surgeries: the transmasculine transition and the transfeminine transition. The following are the procedures you should be expecting to undergo if you decide to totally transform into the gender you want, depending on your current gender assignment.
For the male sex organs (Transfeminine Transition):
- Penectomy – surgical procedure for removing the external genitalia of males.
- Orchiectomy – surgical procedure for removing the testicles or testes.
- Vaginoplasty – surgical procedure that creates a vagina.
- Feminizing genitoplasty – surgical procedure for creating the internal female genitalia.
For the female sex organs (Transmasculine Transition):
- Masculinizing genitoplasty – the surgical creation of external genitalia by using the tissue of the labia in creating the penis.
- Phalloplasty – the surgical creation of a penis through the use of skin graft from the thigh, forearm, or upper back.
- Metoidioplasty – the surgical creation of a penis through the hormonally enlarged clitoris.
- Scrotoplasty – the surgical creation of a scrotum.
Optional Procedures
When it comes to the actual sexual reassignment surgery cost, candidates can determine the expenses based on the core body parts that either require correction based on expert advice or what they opt to undergo by preference . Some of these are the following:
Facial Feminization – this involves plastic surgery in the face to make their faces reflect or suit their gender identity. Again, there are two types for this procedure: facial feminization and facial masculinization.
Under the facial feminization are the following:
- Adam’s apple reduction
- Cheek augmentation
- Chin surgery
- Forehead contouring
- Hairline advancement
- Jaw reduction
- Lip augmentation
- Rhinoplasty
On the other hand, facial masculinization involves the following:
- Adam’s apple enhancement
- Chin contouring
- Forehead lengthening
- Jaw reshaping
- Top Surgery
Torso – Modifying the structure of the torso is another crucial part of the overall transgender surgery cost. The surgery involved in this include the following:
- Breast implants – this is the surgical creation of breast
- Liposuction – this is the surgical removal of unwanted body fats to achieve that feminine or masculine figure that the candidate is aiming for.
- Gluteoplasty – this is the surgical procedure that increases the volume of the buttocks
Prerequisite Investment
Obviously, s ex reassignment is a very extensive process. So p rior to being given the go signal for the surgical operations, both the male and female candidates must be able to meet the prerequisite criteria.
Below are the basic guidelines as presented by the online directory called The Transgender Center:
- Certified psychological diagnosis for ‘gender dysphoria.’
- Consistent opposite sex lifestyle for one year or more.
- Sustained hormone treatment (estrogen or steroids) for two years or more.
- Emotional stability in the midst of gender confusion.
- Medically healthy and clear of any chronic conditions.
- Special recommendation from 2 mental health specialists experienced in gender identity issues.
Other Miscellaneous Costs
Apart from the bulk of the overall sexual reassignment surgery cost , there are other expenses one may consider in line with the successful transformation of the sexual identity.
The cost for hormonal treatment is estimated at roughly $25 to $200 per month or $300 to $2,400 per year . As for the doctor’s visits and laboratory tests for health clearance and certification prior to the operation, the projected cost is somewhere around $500.
- Hair Removal
Some patients undergo hair removal or growth prior to the sexual reassignment procedures. For male-to-female transformation, the average cost for laser hair removal may depend on the scope of the skin area.
T he average cost of laser hair removal can range from around $30 to $400 . On the other hand, just for the face costs around $75 to $150 per session.
When it comes to female-to-male transformation, facial hair is an optional feature. Beard growth for trans males is rather a product of time and the genetic acclimatization resulting from extensive hormone treatment.
- Voice Coaching
Some patients may or may not tend to overlook the importance of natural voice modulation in the course of their sex change journey. In the midst of earlier stages of gender dysphoria, the deep voices of males and shrill petite voices of females may be too much to overcome by sheer effort alone.
Modulating the tone of the voice may be optional, but mismatched vocal gender identification could (at worse) evoke an unusual response in a public audience.
On top of the 2-year hormone treatment, transgender candidates can consider voice lesson s as an important investment in the overall sex change price . Voice coaching costs an average of $30 per session.
- Legal Identity
Another important and often overlooked aspect of complete sex transformation is the legal record of one’s identity. Names are a crucial part of a person’s identity.
Despite the extensive physical modification an individual has gone through, they will still be addressed by their given name on their birth certificate.
O ne key requirement needed in order to obtain a change of name and sex in legal documents is to acquire the services of a lawyer. The overall filling fee may entail a cost range between $150 and $500.
It is important to take note, however, that the exact costs may vary depending on the specific state. An additional fee of $15 to $20 is charged for every copy of the legally certified name change.
Leave a Comment Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Privacy Policy
Terms and Conditions
Amazon Affiliate Disclosure
Card Category Offers
Additional education.
- Best Credit Cards of 2021
- Best Reward Cards
- Best Cards for Bad Credit Scores
- Best Cards for People with No Credit
- Best Business Cards
- Credit Cards 101
- How To Choose The Best Credit Card
- 5 Credit Card Fees To Avoid
- What Is A Credit Card Balance?
- Types Of Credit Cards
- Get The Most From Your Rewards Card
- Pending Transactions Explained
- What's This Charge On My Credit Card Statement?
- Who Accepts Virtual Credit Cards?
- How To Track Credit Card Purchases
Services & Reviews
- Best Credit Repair Companies
- Lexington Law Review
- CreditZo Review
- Creditrepair.com Review
- CreditFirm.net Review
- TotallyMoney Review
- Signs You Need Credit Repair
- Credit Repair vs Credit Counseling
- Sample Credit Letter Templates
- How to Read Your Credit Report
- How to Contact Credit Bureaus
- How to Dispute Items On Credit Report
- How to Remove Something From Credit Report
- Credit Repair Guide
- 5 Ways to Get Your Free Credit Report
- How to Get a Free Experian Credit Report
- Annualcreditreport.com Review
- How to Get a Free Transunion Credit Report
- How to Get a Free Equifax Credit Report
- Credit Karma Credit Report Review
- What is a Credit Score?
- What is Credit Monitoring?
- What Affects Your Credit Score?
- What is a Good Credit Score?
- Credit Score Ranges
- How to Improve Your Credit Score
Additional Education & Learning Centers
- Credit Score and Credit Report Resources
- Credit Card Learning Center
- Small Business Resource Center
- Medical Debt Resources
- Advertiser Disclosure
- Financial Literacy
- News & Economics
Gender Transition Cost — How Much Does Hormone Therapy and Gender Reassignment Surgery Cost?
Gender transition is a process whereby transgender people undergo certain medical, social, and legal steps in order to transition into a gender other than the one that they were assigned at birth. Like many forms of medical treatment, however, gender transition for transgender people often costs money. This article will inform you about how much gender transition costs, how much certain transgender surgeries cost, and more.
The Process of Changing Your Gender
There is no single right way to transition. However, many gender transitions do end up sharing certain similar steps and milestones that will be covered here.
Why Transgender People Transition
Many transgender people are diagnosed with a condition called gender dysphoria, where they feel a level of discomfort — ranging from mild to extreme — with the physical characteristics or social roles of the gender that they were assigned at birth. A literature review by Cornell University looked at publications in medical journals from 1991 to 2017, and found overwhelming evidence that gender transition was an effective treatment for gender dysphoria.
Starting Gender Transition
There is no single right way to begin gender transition, and the best way to access services related to medical transition may vary depending on where you live. However, in general, you should expect to begin medical transition by visiting a trained and licensed therapist. After several sessions, a therapist may officially diagnose you with gender dysphoria and write a referral letter, directing a medical doctor to begin hormone therapy.
Once you have picked out a qualified medical doctor, they will supervise hormone therapy as part of your medical transition. They may also be able to answer any questions you have about other medical aspects of transition, including transgender surgeries.
Milestones for medical transition often include seeing a therapist and getting a hormone prescription from a doctor, but it’s also important to remember to create a budget in order to account for the regular cost of medications and visits to the doctor.
Hormone Therapy
Best practices surrounding access to transgender hormone therapy are still being worked out by doctors and mental health professionals. However, the World Professional Association for Transgender Health recommends in their Standards of Care that individuals seeking hormone therapy:
- Have persistent, well-documented gender dysphoria.
- Have the capacity to make fully informed decisions about medical treatment.
- Are of the age of majority in their country, or otherwise have parental consent to begin hormone therapy.
After starting hormone therapy under the supervision of a qualified medical doctor, a person can expect to take on some secondary sexual characteristics of their target sex over the course of several months, or even years.
According to the Trans Care Project , people who are undergoing hormone therapy as part of a transition from female to male (FtM) should expect to take the hormone testosterone, typically either in the form of a patch or cream that is applied to the skin or an injection of testosterone directly into the muscle. In the United States, testosterone is a schedule III controlled substance, so you will need a doctor’s permission to use it.
Also according to the Trans Care Project , people who are undergoing hormone therapy as part of a transition from male to female (MtF) should expect to take the hormone estrogen, typically in a pill, a patch or cream applied to the skin, or an injection of estrogen directly into the muscle. In addition to estrogen, people transitioning from male to female should also expect to take an anti-androgen, a type of drug that blocks the body’s natural production of testosterone. This will prevent testosterone from overriding the estrogen that a person is taking and allow feminizing effects to take place. There is some anecdotal evidence (but no definitive medical evidence) that the hormone progesterone has feminizing effects as a part of medical transition, so some people will take progesterone in addition to estrogen and an anti-androgen.
Gender Reassignment Surgery
Although the media often focuses on genital surgery as the definitive surgical procedure for gender transition, the reality is not so simple. While genital surgery is an important part of gender transition for many transgender people, it is not always the first surgery that a person might seek out. In fact, some transgender people transition completely without getting genital surgery at all. Which transgender surgeries (if any) are right for you is a discussion for your doctor, but here are some surgical options that some people choose as part of a gender transition.
Genital Surgery
As stated above, surgery in order to reconfigure a person’s genitals into those of their target sex is an important part of medical transition for many people.
Top Surgery
As part of female puberty, many people undergoing an FtM transition have developed unwanted breast tissue. Top surgery is a general term for a variety of surgical procedures that can be used to remove this breast tissue, leading to a quality of life improvement for the patient. Some people who undergo an MtF transition may choose to have breast augmentation surgery if they are unsatisfied by the development of breast tissue as a result of their hormone therapy.
Facial Feminization Surgery and Facial Masculinization Surgery
Facial bone structure often changes as a result of male puberty, and these changes play an important role in the way that we see gender in the world. For example, they are one reason why we can often tell a person’s sex only by looking at their face.
In cases where hormone therapy is not sufficient to alter a person’s face to either appear more feminine (for MtF transitions) or more masculine (for FtM transitions), cosmetic surgery on the face can be used to either reduce bone in certain areas or use surgical implants to add the appearance of new or shaped bone.
How Much Does Transgender Hormone Therapy Cost?
When figuring out the cost of your hormone therapy, you should remember to account for several things:
- Whether or not your insurance will help to cover the cost of hormones, including copay amounts. Many medications used as part of hormone therapy have generic versions, which will often be covered at the lowest copay by your insurance, but some do not. If your insurance covers these medications, then you should ignore the prices given below, which are determined without considering insurance coverage.
- The cost of visits to the doctor and blood tests that are a necessary part of hormone therapy for many people. If possible, ask your doctor to bill hormone blood tests as preventative. This way they are more likely to be covered by insurance and at a better rate.
- Prices below are derived from GoodRX reportings as of September 2018. Keep in mind that the cost of medication may fluctuate depending on availability, the pharmacy that you buy from, and the region where you are located.
FtM Hormone Therapy
How much does testosterone cost.
- Testosterone Cypionate: This popular injectable form of testosterone costs between $40 and $90 per 10 ml bottle of 200 mg/ml solution without insurance. Keep in mind that a single 10 ml bottle can last you for several months, depending on the dosage prescribed by your doctor. Needles and syringes are very inexpensive and can be bought at the pharmacy or online.
- Androgel: The generic equivalent of this topical form of testosterone can cost between $30 and $80 without insurance for a packet of six patches, which may last about a month depending on your dosage. Brand-name patches will cost upwards of $130 for comparable amounts.
MtF Hormone Therapy
How much does estrogen cost.
- Estradiol Pill: Generic estradiol is an incredibly cheap pill form of estradiol that many transgender women take. A bottle of 30, 2-mg tablets costs just $4 at the Walmart pharmacy. Other vendors may charge up to $40, but generic estrace is often covered by insurance at reasonable rates.
- Estradiol Patch: Patches deliver hormones through your skin and a single patch may be worn for up to a week. While patches may be more convenient than pills, since you only have to worry about application once a week, they also cost more. A packet of four generic estradiol patches that deliver 0.1 mg of estradiol per day will cost you between $30 and $60.
- Injectable Estradiol: Hormone injections are, for some people, the most convenient way to administer the medication. Unlike patches, they leave no visible indications on your body of the hormones that you are taking and, as long as you don’t mind injecting yourself or having a nurse or trusted friend do it for you, administration is an easy process that takes 10 to 15 minutes every one or two weeks, depending on the dosage determined by your doctor. However, injectable estradiol is also more expensive than other forms. Generic injectable estradiol (estradiol valerate) has experienced supply shortages in the past, but a 5 ml vial may cost you between $40 or $100. Depending on your dosage, a single vial may last a little over a month. Non-generic injectable estradiol (estradiol cypionate) has a longer half-life inside the body than valerate, meaning that you can go longer between injections, but it also costs more. Estradiol cypionate (or depo-estradiol) may cost around $120.
How Much Do Anti-Androgens Cost?
- Spironolactone: Spironolactone is the most commonly prescribed anti-androgen in the United States, in part because it is cheap and easy to acquire. Without insurance, spironolactone may cost between $4 and $12 per month.
- Cyproterone: Cyproterone is another popular anti-androgen. However, it is more expensive than its counterpart, Spironolactone, at anywhere between $12 to $35 for a monthly supply.
How Much Does Transgender Surgery Cost?
For many transgender people, surgeries are an important part of gender transition that are used in addition to or in lieu of hormone therapy. Although certain surgical procedures are often highlighted in media coverage of transgender people, the reality is that there are many transgender surgeries available, and deciding which ones are right for you and your transition is a personal matter. Below, we will cover some of the more popular transgender surgeries, and how much they cost without help from your insurance provider. With any surgical procedure, make sure that you research your surgeon to find out their qualifications and the prices they charge.
Facial Feminization Surgery (FFS) Surgery Cost
In order to correct certain gendered features in the face, some transgender people will undergo facial cosmetic surgery, called facial feminization surgery (FFS) or facial masculinization surgery (FMS). Neither FFS nor FMS is a single procedure by itself. Instead, they represent a wide variety of procedures that contribute to sexual characteristics in the face. As a result, the price that you can expect to pay for FFS or FMS will vary wildly depending on the surgeon you choose and the procedures they perform. According to individuals that we spoke to who had sought out these procedures, surgery could cost you between $5,000 or $50,000, although most surgeries are likely to fall somewhere in the middle, as few people only get a single small procedure or an extremely large number of procedures.
FtM Top Surgery
Surgical procedures centered around the chest or “top surgery” are designed to either augment or remove breast tissue, depending on the person’s transition goals. For many FtM individuals, top surgery is a very important part of transition and seen as a major milestone.
It may be more optional for those making an MtF transition, as hormone therapy will develop breast tissue in many people. According to individuals that we spoke to who had sought out these procedures, top surgery can cost between $3,000 or $10,000, depending on the surgeon that you choose, and how difficult or time-consuming the procedure will be to perform for them.
Gender Reassignment Surgery Cost
The term “bottom surgery” is used to refer to genital surgery, or gender confirming surgery, for transgender people. Although it is popularized in the media as the most important surgery that a transgender person can get, there are many people who consider their transitions complete without bottom surgery.
Male to Female Surgery
According to individuals that we spoke to who had sought out these procedures, MtF bottom surgery can cost between $10,000 or $30,000. Once again, this depends heavily on the surgeon that you choose and the exact procedures that they perform.
Female to Male Surgery
Bottom surgery for FtM people is often more expensive, as the surgical procedure is more involved. It may cost between $20,000 and $50,000 depending on the surgeon you see and the techniques used.
Fortunately, although many medically necessary surgical procedures as a part of transition are not covered by insurance, bottom surgery is receiving more and more coverage as insurance companies partner with specific surgeons.
How Much Does it Cost to Legally Change Your Gender?
Unfortunately, healthcare costs aren’t the only costs related to gender transition. In order to change you legal sex (for example, the sex marker on your driver’s license), you will have to pay a fee in many states in order to have your legal name and gender changed. For example, in Massachusetts a legal name change costs $185. You should speak with your state government in order to find out how much they will charge. There are also some additional costs that you may or may not have to pay as part of changing your legal name and gender:
- A lawyer’s fee is you’re having difficulty changing your name because of a criminal record .
- The cost of publishing your name change in a local newspaper, which many states require, but which can be waived by a judge.
- The cost of new legal identification documents, such as a new driver’s license or passport.
Paying for Gender Transition
With all of these costs, paying for gender transition isn’t easy. Especially since transgender people are four times more likely to have a make less than $10,000 a year than the average person in the United States. Minorities in general may be more likely to work in jobs that only pay minimum wage . If you’re struggling to figure out how you can pay for your transition, here are some things to consider:
Health Insurance Coverage
Health insurance companies are slow to add on new coverage, especially for minorities who are already the subject of heated political debates. However, insurance coverage for gender transition is slowly beginning to catch up to modern medical science. Many insurance companies will cover hormone therapy at the same rate as any other prescription from your doctor. Surgical procedures, such as bottom surgery and FtM top surgery, are also being covered more widely, and some insurance companies will even cover cosmetic surgery as part of gender transition .
Find a Good Job
Getting on the right insurance plan can be a matter of working for a company with good employee benefits. Finding a job that fits your personality can help you excel. It goes without saying that making more money will help you to pay for transition, although in order to do this, you may have to make a choice between money and job satisfaction .
Paying Medical Bills With Your Roth IRA
Typically, if you have a Roth IRA retirement plan , you will receive a tax penalty if you withdraw money from it before you reach age 59 and a half. However, you can avoid this tax penalty if you’re withdrawing from your Roth IRA in order to pay for a medical procedure that costs more than 7.5 percent of your annual income.
Medical Loan Providers
Some surgeons and doctors will partner with medical loan providers such as CareCredit . They offer loans specifically for the cost of a your surgery or other medical procedures. If you do decide to take out loans to pay for transition, make sure that you have a good credit score so you can receive competitive interest rates . It’s also very important that you pay debt back, so that you can avoid default, wage garnishment, or tanking your credit history.
Using a Credit Card to Pay for Transition
It is possible to use a credit card to pay for gender transition. However, you will need an acceptable credit history to get approved for a credit card in the first place. If you aren’t sure of your credit history, Experian offers free credit score and credit report checks. It’s also unwise to use a credit card to make payments if you won’t be able to afford your credit card bill at the end of the month. Credit cards tend to have very high interest rates compared to other forms of debt and companies tend to slap on credit card fees wherever they can. If you do decide to use a credit card to pay for your gender transition, use is sparingly and pay off your entire balance as quickly as possible.

National Estimates of Gender-Affirming Surgery in the US
Affiliations.
- 1 Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, New York, New York.
- 2 Department of Obstetrics and Gynecology, University of Southern California, Los Angeles.
- PMID: 37610753
- PMCID: PMC10448302
- DOI: 10.1001/jamanetworkopen.2023.30348
Importance: While changes in federal and state laws mandating coverage of gender-affirming surgery (GAS) may have led to an increase in the number of annual cases, comprehensive data describing trends in both inpatient and outpatient procedures are limited.
Objective: To examine trends in inpatient and outpatient GAS procedures in the US and to explore the temporal trends in the types of GAS performed across age groups.
Design, setting, and participants: This cohort study includes data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. Patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified, and the performance of GAS, including breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures, were identified.
Main outcome measures: Weighted estimates of the annual number of inpatient and outpatient procedures performed and the distribution of each class of procedure overall and by age were analyzed.
Results: A total of 48 019 patients who underwent GAS were identified, including 25 099 (52.3%) who were aged 19 to 30 years. The most common procedures were breast and chest procedures, which occurred in 27 187 patients (56.6%), followed by genital reconstruction (16 872 [35.1%]) and other facial and cosmetic procedures (6669 [13.9%]). The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020. Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged12 to 18 years. When stratified by the type of procedure performed, breast and chest procedures made up a greater percentage of the surgical interventions in younger patients, while genital surgical procedures were greater in older patients.
Conclusions and relevance: Performance of GAS has increased substantially in the US. Breast and chest surgery was the most common group of procedures performed. The number of genital surgical procedures performed increased with increasing age.
- Cohort Studies
- Gender Dysphoria* / epidemiology
- Gender Dysphoria* / surgery
- Sex Reassignment Surgery*
- Transsexualism* / epidemiology
- Transsexualism* / surgery

IMAGES
VIDEO
COMMENTS
The cost of transgender surgery can vary by provider and the type of surgery you choose to get. For a female-to-male transition, masculinization chest surgery (also known as top surgery) might ...
Gender-affirming surgery can cost between $6,900 and $63,400 depending on the precise procedure, according to a 2022 study published in The Journal of Law, Medicine and Ethics. Out-of-pocket costs ...
This comprehensive surgery involves a series of procedures, including lip and cheekbone augmentation, hairline adjustment to reduce forehead size, and sculpting of the jaw and chin. The goal is to harmonize and enhance facial traits for a more feminine appearance. The total Male to Female Feminization surgery cost may go up from $9,000 to $12,000.
Transgender Surgery. By Priyanka Dutta Deb. •. 6th June '22. MBBS, MS - General Surgery, MCh - Plastic Surgery. Gender reassignment surgery cost varies depending on the type of transition. For male to female (MTF) transition, the cost ranges from $2438 to $6095 and. For female to male (FTM) transition, the cost falls between $4876 and $9752 ...
Key Points. Question What are the temporal trends in gender-affirming surgery (GAS) in the US?. Findings In this cohort study of 48 019 patients, GAS increased significantly, nearly tripling from 2016 to 2019. Breast and chest surgery was the most common class of procedures performed overall; genital reconstructive procedures were more common among older individuals.
The standard premium for Medicare Part B in 2020 is $144.60 each month, and there is a $198 annual deductible cost. After a person pays the deductible, Medicare pays 80% of the allowable costs ...
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
Hormone therapy can cost anywhere from $25 to $200 a month. That's between $300 and $2,400 a year. What's more, the counseling involved in preparing for a gender transition (and required by many doctors and insurance companies), can cost between $50 and $200 a session. In short, transitioning is expensive.
Patient: Wren Vetens, then 23, a Ph.D. student at the University of Wisconsin-Madison. Total bill: $91,850.20. Insurance payment: $25,427.91. Vetens owed: $13,191.95 (after $20,080 that was ...
The per-episode payer costs of gender-affirming surgeries ranged from $6,927 for orchiectomy to $45,080 for vaginoplasty and $63,432 for phalloplasty (Table 2.3). As vaginoplasty and phalloplasty were frequently multi-episode procedures, the total average cost of these procedures per person was $53,645 and $133,911, respectively.
Gender reassignment procedures. ... Gender affirming surgery costs (includes hospital care and anesthesia) Top surgery: $3,000 - $10,000: Metoidioplasty (bottom surgery) ... In total, Sasha has spent about $8,000 just on hair removal, and she says she still has $2,000 or more to go. "This has been far and away the most expensive part of ...
CMS.gov. Gender dysphoria and gender reassignment surgery. Transgender Legal Defense & Education Fund. Health insurance medical policies: gender dysphoria / gender reassignment. Aetna. Gender-affirming surgery. Downing J, Holt SK, Cunetta M, Gore JL, Dy GW. Spending and out-of-pocket costs for genital gender-affirming surgery in the US.
In 2014, the Center for Medicare and Medicaid Services began paying for sex reassignment surgery and other transitional care, after a 33-year-ban on covering those costs was lifted. "Providing health care benefits to transgender people makes economic sense," says study leader William V. Padula, PhD, MS, MSc, an assistant professor of health ...
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
OOP and Total Costs of Phalloplasties . Among 72 phalloplasties, the median OOP cost was $2120 (IQR, $738-$4371) and the median total cost was $148 540 (IQR, $74 679-$240 844) (Table 3). Out-of-pocket costs were higher for patients residing in the South, patients with less restrictive health plans, and patients who underwent surgery in more ...
The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020. Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged12 to 18 years.
Importance: Genital gender-affirming surgery (GAS) is safe and offers substantial benefits to patients. Geographic accessibility and high out-of-pocket (OOP) costs reportedly hinder access; however, to date, this has not been thoroughly investigated at the national level. Objective: To estimate OOP and total costs for GAS among commercially ...
The average transgender surgery cost for each procedure typically ranges from $1,500 to $26,000 but the total for all could be as high as $200,000 to $300,000. Replacing the core reproductive organ completes the entire sexual reassignment. The male-to-female vaginoplasty is estimated to be somewhere between $20,000 and $50,000 or even higher.
According to individuals that we spoke to who had sought out these procedures, top surgery can cost between $3,000 or $10,000, depending on the surgeon that you choose, and how difficult or time-consuming the procedure will be to perform for them. Gender Reassignment Surgery Cost
The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020. Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged12 to 18 years. When stratified by the type of procedure performed, breast and chest ...
The number of gender-affirming surgeries rose from 4,552 in 2016 to 13,011 in 2019, declining only slightly to 12,818 during the first year of the Covid-19 pandemic, when many hospitals cut back ...
Gender reassignment surgery (GRS) is a procedure that can change the transgender person's physical body to accord with their gender identity. ... 2018). The majority of GRS performed are for male-to-female assignment, with a total cost to the NHS of £3,525,460 in the financial year of 2016/2017 (NHS, e-mail message to author, May 22, 2018 ...