Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
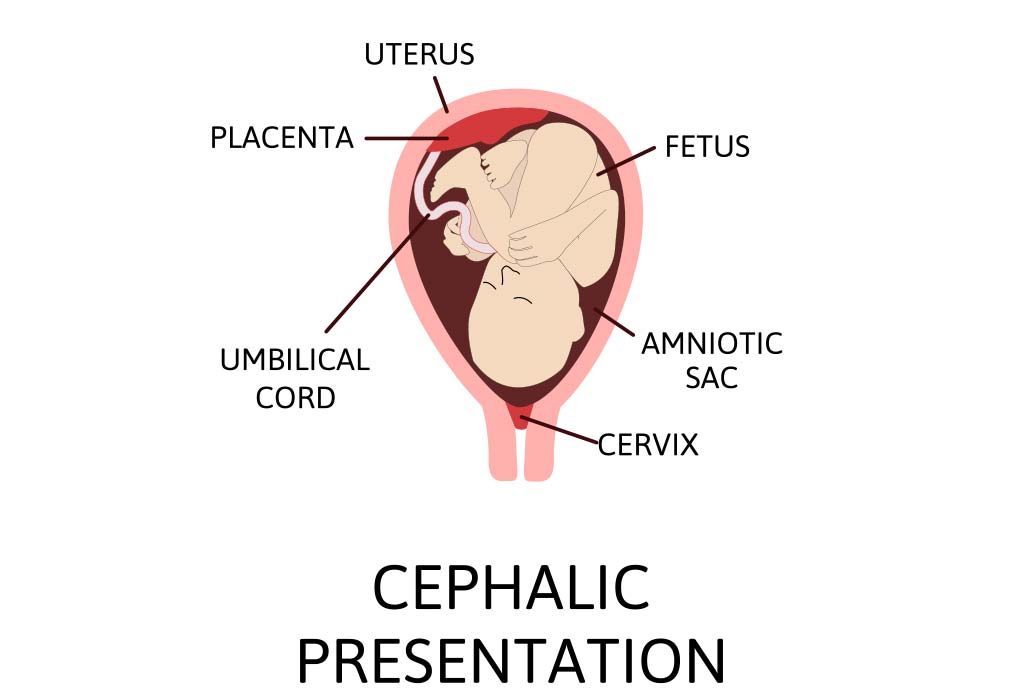
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.

Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What Is Cephalic Position?
The ideal fetal position for labor and delivery
- Why It's Best
Risks of Other Positions
- Determining Position
- Turning a Fetus
The cephalic position is when a fetus is head down when it is ready to enter the birth canal. This is one of a few variations of how a fetus can rest in the womb and is considered the ideal one for labor and delivery.
About 96% of babies are born in the cephalic position. Most settle into it between the 32nd and 36th weeks of pregnancy . Your healthcare provider will monitor the fetus's position during the last weeks of gestation to ensure this has happened by week 36.
If the fetus is not in the cephalic position at that point, the provider may try to turn it. If this doesn't work, some—but not all—practitioners will attempt to deliver vaginally, while others will recommend a Cesarean (C-section).
Getty Images
Why Is the Cephalic Position Best?
During labor, contractions dilate the cervix so the fetus has adequate room to come through the birth canal. The cephalic position is the easiest and safest way for the baby to pass through the birth canal.
If the fetus is in a noncephalic position, delivery becomes more challenging. Different fetal positions have a range of difficulties and varying risks.
A small percentage of babies present in noncephalic positions. This can pose risks both to the fetus and the mother, and make labor and delivery more challenging. It can also influence the way in which someone can deliver.
A fetus may actually find itself in any of these positions throughout pregnancy, as the move about the uterus. But as they grow, there will be less room to tumble around and they will settle into a final position.
It is at this point that noncephalic positions can pose significant risks.
Cephalic Posterior
A fetus may also present in an occiput or cephalic posterior position. This means they are positioned head down, but they are facing the abdomen instead of the back.
This position is also nicknamed "sunny-side up."
Presenting this way increases the chance of a painful and prolonged delivery.
There are three different types of breech fetal positioning:
- Frank breech: The legs are up with the feet near the head.
- Footling breech: One or both legs is lowered over the cervix.
- Complete breech: The fetus is bottom-first with knees bent.
A vaginal delivery is most times a safe way to deliver. But with breech positions, a vaginal delivery can be complicated.
When a baby is born in the breech position, the largest part—its head—is delivered last. This can result in them getting stuck in the birth canal (entrapped). This can cause injury or death.
The umbilical cord may also be damaged or slide down into the mouth of the womb, which can reduce or cut off the baby's oxygen supply.
Some providers are still comfortable performing a vaginal birth as long as the fetus is doing well. But breech is always a riskier delivery position compared with the cephalic position, and most cases require a C-section.
Likelihood of a Breech Baby
You are more likely to have a breech baby if you:
- Go into early labor before you're full term
- Have an abnormally shaped uterus, fibroids , or too much amniotic fluid
- Are pregnant with multiples
- Have placenta previa (when the placenta covers the cervix)
Transverse Lie
In transverse lie position, the fetus is presenting sideways across the uterus rather than vertically. They may be:
- Down, with the back facing the birth canal
- With one shoulder pointing toward the birth canal
- Up, with the hands and feet facing the birth canal
If a transverse lie is not corrected before labor, a C-section will be required. This is typically the case.
Determining Fetal Position
Your healthcare provider can determine if your baby is in cephalic presentation by performing a physical exam and ultrasound.
In the final weeks of pregnancy, your healthcare provider will feel your lower abdomen with their hands to assess the positioning of the baby. This includes where the head, back, and buttocks lie
If your healthcare provider senses that the fetus is in a breech position, they can use ultrasound to confirm their suspicion.
Turning a Fetus So They Are in Cephalic Position
External cephalic version (ECV) is a common, noninvasive procedure to turn a breech baby into cephalic position while it's still in the uterus.
This is only considered if a healthcare provider monitors presentation progress in the last trimester and notices that a fetus is maintaining a noncephalic position as your delivery date approaches.
External Cephalic Version (ECV)
ECV involves the healthcare provider applying pressure to your stomach to turn the fetus from the outside. They will attempt to rotate the head forward or backward and lift the buttocks in an upward position. Sometimes, they use ultrasound to help guide the process.
The best time to perform ECV is about 37 weeks of pregnancy. Afterward, the fetal heart rate will be monitored to make sure it’s within normal levels. You should be able to go home after having ECV done.
ECV has a 50% to 60% success rate. However, even if it does work, there is still a chance the fetus will return to the breech position before birth.
Natural Methods For Turning a Fetus
There are also natural methods that can help turn a fetus into cephalic position. There is no medical research that confirms their efficacy, however.
- Changing your position: Sometimes a fetus will move when you get into certain positions. Two specific movements that your provider may recommend include: Getting on your hands and knees and gently rocking back and forth. Another you could try is pushing your hips up in the air while laying on your back with your knees bent and feet flat on the floor (bridge pose).
- Playing stimulating sounds: Fetuses gravitate to sound. You may be successful at luring a fetus out of breech position by playing music or a recording of your voice near your lower abdomen.
- Chiropractic care: A chiropractor can try the Webster technique. This is a specific chiropractic analysis and adjustment which enables chiropractors to establish balance in the pregnant person's pelvis and reduce undue stress to the uterus and supporting ligaments.
- Acupuncture: This is a considerably safe way someone can try to turn a fetus. Some practitioners incorporate moxibustion—the burning of dried mugwort on certain areas of the body—because they believe it will enhance the chances of success.
A Word From Verywell
While most babies are born in cephalic position at delivery, this is not always the case. And while some fetuses can be turned, others may be more stubborn.
This may affect your labor and delivery wishes. Try to remember that having a healthy baby, and staying well yourself, are your ultimate priorities. That may mean diverting from your best laid plans.
Speaking to your healthcare provider about turning options and the safest route of delivery may help you adjust to this twist and feel better about how you will move ahead.
Glezerman M. Planned vaginal breech delivery: current status and the need to reconsider . Expert Rev Obstet Gynecol. 2012;7(2):159-166. doi:10.1586/eog.12.2
Cleveland Clinic. Fetal positions for birth .
MedlinePlus. Breech birth .
UT Southwestern Medical Center. Can you turn a breech baby around?
The American College of Obstetricians and Gynecologists. If your baby is breech .
Roecker CB. Breech repositioning unresponsive to Webster technique: coexistence of oligohydramnios . Journal of Chiropractic Medicine . 2013;12(2):74-78. doi:10.1016/j.jcm.2013.06.003
By Cherie Berkley, MS Berkley is a journalist with a certification in global health from Johns Hopkins University and a master's degree in journalism.

Cephalic presentation
October 14, 2016
A cephalic presentation or head presentation or head-first presentation is a situation at childbirth where the fetus is in a longitudinal lie and the head enters the pelvis first; the most common form of cephalic presentation is the vertex presentation where the occiput is the leading part (the part that first enters the birth canal). All other presentations are abnormal (malpresentations) which are either more difficult to deliver or not deliverable by natural means.
The movement of the fetus to cephalic presentation is called head engagement. It occurs in the third trimester. In head engagement, the fetal head descends into the pelvic cavity so that only a small part (or none) of it can be felt abdominally. The perineum and cervix are further flattened and the head may be felt vaginally. Head engagement is known colloquially as the baby drop, and in natural medicine as the lightening because of the release of pressure on the upper abdomen and renewed ease in breathing. However, it severely reduces bladder capacity, increases pressure on the pelvic floor and the rectum, and the mother may experience the perpetual sensation that the fetus will “fall out” at any moment.
The vertex is the area of the vault bounded anteriorly by the anterior fontanelle and the coronal suture, posteriorly by the posterior fontanelle and the lambdoid suture and laterally by 2 lines passing through the parietal eminences.
In the vertex presentation the occiput typically is anterior and thus in an optimal position to negotiate the pelvic curve by extending the head. In an occiput posterior position, labor becomes prolonged and more operative interventions are deemed necessary. The prevalence of the persistent occiput posterior is given as 4.7 %
The vertex presentations are further classified according to the position of the occiput, it being right, left, or transverse, and anterior or posterior:
Left Occipito-Anterior (LOA), Left Occipito-Posterior (LOP), Left Occipito-Transverse (LOT); Right Occipito-Anterior (ROA), Right Occipito-Posterior (ROP), Right Occipito-Transverse (ROT);
By Mikael Häggström – Own work, Public Domain
Cephalic presentation. (2016, September 17). In Wikipedia, The Free Encyclopedia . Retrieved 05:18, September 17, 2016, from https://en.wikipedia.org/w/index.php?title=Cephalic_presentation&oldid=739815165
Insert/edit link
Enter the destination URL
Or link to existing content

- Learn /
Why Is Cephalic Presentation Ideal For Childbirth?

5 Dec 2017 | 8 min Read
During labour, contractions stretch your birth canal so that your baby has adequate room to come through during birth. The cephalic presentation is the safest and easiest way for your baby to pass through the birth canal.
If your baby is in a non-cephalic position, delivery can become more challenging. Different fetal positions pose a range of difficulties and varying risks and may not be considered ideal birthing positions.
Two Kinds of Cephalic Positions
There are two kinds of cephalic positions:
- Cephalic occiput anterior , where your baby’s head is down and is facing toward your back.
- Cephalic occiput posterior , where your baby is positioned head down, but they are facing your abdomen instead of your back. This position is also nicknamed ‘sunny-side-up’ and can increase the chances of prolonged and painful delivery.
How to Know if Your Baby is In a Cephalic Position?
You can feel your baby’s position by rubbing your hand on your belly. If you feel your little one’s stomach in the upper stomach, then your baby is in a cephalic position. But if you feel their kicks in the lower stomach, then it could mean that your baby is in a breech position.
You can also determine whether your baby is in the anterior or posterior cephalic position. If your baby is in the anterior position, you may feel their movement underneath your ribs and your belly button could also pop out. If your baby is in the posterior position, then you may feel their kicks in their abdomen, and your stomach may appear rounded up instead of flat.
You can also determine your baby’s position through an ultrasound scan or a physical examination at your healthcare provider’s office.
Benefits of Cephalic Presentation in Pregnancy
Cephalic presentation is one of the most ideal birth positions, and has the following benefits:
- It is the safest way to give birth as your baby’s position is head-down and prevents the risk of any injuries.
- It can help your baby move through the delivery canal as safely and easily as possible.
- It increases the chances of smooth labour and delivery.
Are There Any Risks Involved in Cephalic Position?
Conditions like a cephalic posterior position in addition to a narrow pelvis of the mother can increase the risk of pregnancy complications during delivery. Some babies in the head-first cephalic presentation might have their heads tilted backward. This may, in some rare cases, cause preterm delivery.
What are the Risks Associated with Other Birth Positions?
A small percentage of babies may settle into a non-cephalic position before their birth. This can pose risks to both your and your baby’s health, and also influence the way in which you deliver.
In the next section, we have discussed a few positions that your baby can settle in throughout pregnancy, as they move around the uterus. But as they grow old, there will be less space for them to tumble around, and they will settle into their final position. This is when non-cephalic positions can pose a risk.
Breech Position
There are three types of breech fetal positioning:
- Frank breech : Your baby’s legs stick straight up along with their feet near their head.
- Footling breech: One or both of your baby’s legs are lowered over your cervix.
- Complete breech: Your baby is positioned bottom-first with their knees bent.
If your baby is in a breech position , vaginal delivery is considered complicated. When a baby is born in breech position, the largest part of their body, that is, their head is delivered last. This can lead to injury or even fetal distress. Moreover, the umbilical cord may also get damaged or get wrapped around your baby’s neck, cutting off their oxygen supply.
If your baby is in a breech position, your healthcare provider may recommend a c-section, or they may try ways to flip your baby’s position in a cephalic presentation.
Transverse Lie
In this position, your baby settles in sideways across the uterus rather than being in a vertical position. They may be:
- Head-down, with their back facing the birth canal
- One shoulder pointing toward the birth canal
- Up with their hands and feet facing the birth canal
If your baby settles in this position, then your healthcare provider may suggest a c-section to reduce the risk of distress in your baby and other pregnancy complications.
Turning Your Baby Into A Cephalic Position
External cephalic version (ECV) is a common, and non-invasive procedure that helps turn your baby into a cephalic position while they are in the womb. However, your healthcare provider may only consider this procedure if they consider you have a stable health condition in the last trimester, and if your baby hasn’t changed their position by the 36th week.
You can also try some natural remedies to change your baby’s position, such as:
- Lying in a bridge position: Movements like bridge position can sometimes help move your baby into a more suitable position. Lie on your back with your feet flat on the ground and your legs bent. Raise your pelvis and hips into a bridge position and hold for 5-10 minutes. Repeat several times daily.
- Chiropractic care: A chiropractor can help with the adjustment of your baby’s position and also reduce stress in them.
- Acupuncture: After your doctor’s go-ahead, you can also consider acupuncture to get your baby to settle into an ideal birthing position.
While most babies settle in a cephalic presentation by the 36th week of pregnancy, some may lie in a breech or transverse position before birth. Since the cephalic position is considered the safest, your doctor may recommend certain procedures to flip your baby’s position to make your labour and delivery smooth. You may also try the natural methods that we discussed above to get your baby into a safe birthing position and prevent risks or other pregnancy complications.
When Should A Baby Be In A Cephalic Position?
Your baby would likely naturally drop into a cephalic position between weeks 37 to 40 of your pregnancy .
Is Cephalic Position Safe?
Research shows that 95% of babies take the cephalic position a few weeks or days before their due date. It is considered to be the safest position. It ensures a smooth birthing process.
While most of the babies are in cephalic position at delivery, this is not always the case. If you have a breech baby, you can discuss the available options for delivery with your doctor.
Does cephalic presentation mean labour is near?
Head-down is the ideal position for your baby within your uterus during birth. This is known as the cephalic position. This posture allows your baby to pass through the delivery canal more easily and safely.
Can babies change from cephalic to breech?
The external cephalic version (ECV) is the most frequent procedure used for turning a breech infant.
How can I keep my baby in a cephalic position?
While your baby naturally gets into this position, you can try some exercises to ensure that they settle in cephalic presentation. Exercises such as breech tilt, forward-leaning position (spinning babies program), cat and camel pose can help.
Stitches after a normal delivery : How many stitches do you need after a vaginal delivery? Tap this post to know.
Vaginal birth after caesarean delivery : Learn all about the precautions to consider before having a vaginal delivery after a c-section procedure.
How many c-sections can you have : Tap this post to know the total number of c-sections that you can safely have.
Cover Image Credit: Freepik.com

Related Topics for you
babychakraenglish
cephalicposition
cephalicpresentation
fetaldevelopment
fetalmovement
preganancycare
Suggestions offered by doctors on BabyChakra are of advisory nature i.e., for educational and informational purposes only. Content posted on, created for, or compiled by BabyChakra is not intended or designed to replace your doctor's independent judgment about any symptom, condition, or the appropriateness or risks of a procedure or treatment for a given person.
- Getting pregnant
- Preschooler
- Life as a parent
- Baby essentials
- Find your birth club
- Free antenatal classes
- Meet local parents & parents-to-be
- See all in Community
- Ovulation calculator
- Am I pregnant quiz
- How to get pregnant fast
- Best sex positions
- Signs of pregnancy
- How many days after your period can you get pregnant?
- How age affects fertility
- Very early signs of pregnancy
- What fertile cervical mucus looks like
- Think you're pregnant but the test is negative?
- Faint line on pregnancy test
- See all in Getting pregnant
- Pregnancy week by week
- How big is my baby?
- Due date calculator
- Baby movements week by week
- Symptoms you should never ignore
- Hospital bag checklist
- Signs of labour
- Your baby's position in the womb
- Baby gender predictor
- Vaginal spotting
- Fetal development chart
- See all in Pregnancy
- Baby names finder
- Baby name inspiration
- Popular baby names 2022
- Numerology calculator
- Gender-neutral names
- Old-fashioned names
- See all in Baby names
- Your baby week by week
- Baby milestones by month
- Baby rash types
- Baby poop chart
- Ways to soothe a crying baby
- Safe co-sleeping
- Teething signs
- Growth spurts
- See all in Baby
- Your toddler month by month
- Toddler development milestones
- Dealing with tantrums
- Toddler meals
- Food & fussy eating
- When to start potty training
- Moving from a cot to a bed
- Help your child sleep through
- Games & activities
- Vomiting: what's normal?
- See all in Toddler
- Your child month by month
- Food ideas & nutrition
- How kids learn to share
- Coping with aggression
- Bedtime battles
- Anxiety in children
- Dealing with public tantrums
- Great play ideas
- Is your child ready for school?Top tips for starting school
- See all in Preschooler
- Postnatal symptoms to watch out for
- Stitches after birth
- Postpartum blood clots
- Baby showers
- Sex secrets for parents
- See all in Life as a parent
- Best baby products
- Best formula and bottles for a windy baby
- Best car seats if you need three to fit
- Best nappies
- Best Moses baskets
- Best baby registries
- Best baby sleeping bags
- Best baby humidifier
- Best baby monitors
- Best baby bath seat
- Best baby food
- See all in Baby essentials
- Back pain in pregnancy
- Pelvic girdle pain
- Perineal massage
- Signs you're having a boy
- Signs you're having a girl
- Can you take fish oil while pregnant?
- 18 weeks pregnant bump
- Can you eat salami when pregnant?
- Edwards' syndrome
- Missed miscarriage
- Should I harvest my colostrum?
- Rhesus positive vs. Rhesus negative
- What do contractions feel like?
- Hunger in early pregnancy
- First poop after birth
- When do babies sit up?
- When can babies have salt?
- MMR vaccine rash
- Vaping while breastfeeding
- How to transition from formula to milk
- When do babies start grabbing things?
- Sperm allergy: can sperm cause itching?
- How long after taking folic acid can I get pregnant?
Understanding your maternity notes

What is a personal maternity record?
What's in your maternity notes, what other information might my notes contain, what do all these abbreviations in my notes mean, information about you.
- Your name, address, telephone numbers, hospital number and contact details for your next of kin.
- Your ethnic origin, which helps your midwife check for any conditions that may be common for people with your heritage.
- Your language so your midwife ensures that you receive appropriate support. For example, they can help arrange an interpreter for your appointments if your English language skills are limited or you have a disability such as hearing loss that affects how you communicate.
- Your religious beliefs so the right spiritual care can be arranged when you give birth or if you face an emergency.
- Your health. Your midwife and doctor need to consider any health conditions you've had in the past, or currently have, that might affect your pregnancy and labour. For example, if you had rheumatic fever as a child, you might find pushing difficult when it comes to giving birth. And if you have been experiencing high blood pressure, you will need to be monitored closely. They will also consider any long-term conditions you may have, including epilepsy or asthma . They will also talk about your mental wellbeing and any physical or learning disabilities you may have, so you get the care and support you need to keep you and your baby well.
- Medicines or drugs that you are taking. Your doctor will want to make sure that none of these will harm your unborn baby.
- The health of close family members. This helps your midwife assess whether your baby might inherit a condition that runs in your family and talk to you about close family members' mental health too.
Information about any previous pregnancies
Information about this pregnancy.
- The date of your first antenatal visit and the date your baby is expected.
- The results of blood tests .
- The checks your midwife has carried out at the antenatal clinic. This includes blood pressure readings, urine test results, measurements of your bump and the position in which your baby is lying later in pregnancy.
- Any problems you've experienced during your pregnancy.
- Details of your ultrasound scans .
- A customised growth chart for your baby (which is added after your first ultrasound scan).
- Details of any reasons you had to go to the antenatal ward or day assessment unit at your local hospital.
Your preferences for your baby's birth
- pain relief
- monitoring your baby's heartbeat
- when and how your medical team may intervene to assist your labour
- breastfeeding your baby, using formula milk or combination feeding
- having skin-to-skin with your baby after the birth
- if you have any preferred positions for labour
- who you want your birth partner to be
- how you want the third stage of labour to be managed
- how you would feel about a student midwife being present
- Phone numbers for your midwife, GP, ambulance service, birth suite and hospital switchboard.
- Phone numbers for voluntary and charitable organisations which work with mums, babies and families.
- Names of books and pamphlets that you might find interesting.
- A list of topics that you might want to ask your midwife about.
- What to do if you have vaginal bleeding , severe headaches or pain in your belly during pregnancy.
- The normal size of a baby's head and the length of a baby’s thigh bone for various weeks of pregnancy (as measured on a scan).
- General tips about the health benefits of breastfeeding , stopping smoking and eating well .
- What to expect from your baby’s movements .
Length of pregnancy
- EDD: estimated date of delivery or the date your baby is due
- GA: gestational age, for example, 28+3 (28 weeks and three days pregnant)
- LMP: last menstrual period
Blood pressure (BP)
- PGO: whether your urine sample contains protein, glucose or anything else (other)
- NAD: no abnormalities detected
- MSU: midstream sample of urine
- Tr or trace: tiny amounts of protein or sugar found, also marked with a +, ++ or +++ depending on how much is present
Height of uterus (fundal height)
Position of your baby.
- Cephalic (or ceph): head-down
- BR bottom down or breech
- LOA: the back of your baby's head is on your left-hand side and towards the front of your tummy
- ROA: the back of your baby's head is on your right-hand side and towards the front of your tummy
- LOP: the back of your baby's head is on your left-hand side and towards the back of your tummy
- ROP: the back of your baby's head is on your right-hand side and towards the back of your tummy
Engagement of baby’s head in your pelvis
- NE, NEng, Not Eng: your baby’s head is not engaged
- E or Eng: your baby’s head is engaged
- 5/5: free, meaning your baby’s head has not engaged in to your pelvis
- 4/5: sitting on the pelvic brim
- 3/5: lower but most still above the brim
- 2/5: engaged, as most is below the brim
- 1/5 or 0/5: deeply engaged
Heartbeat or activity
- FHH: fetal heart heard; or FHHR: fetal heart heard and regular
- FMF: fetal movements felt
Ultrasound scan measurements
- AC: abdominal circumference
- BPD: biparietal diameter, which is the measurement of the diameter of your baby's skull, from one side to the other, using the parietal bones either side of the skull
- CRL: crown rump length. Measurement of your baby from head to bottom
- FL: femur length or thigh bone length
- HC: head circumference
- TD: trunk diameter

Pregnancy history
- Multigravida: you have been pregnant before, including pregnancies that ended in a loss
- Para 0: you have had no pregnancies that have gone beyond 24 weeks
- Para 1: you have had one other pregnancy that lasted longer than 24 weeks. Para 2 means two pregnancies and so on
- Primagravida: you are pregnant for the first time
Vaginal examination (VE)
- BS: = Bishop score , which measures the ripeness of your cervix. Your midwife will need to find this out before inducing labour because it helps to tell whether your body is ready.
- Cx: your cervix, which is the neck of your womb.
- RV: your womb is retroverted or tilting backwards.
Was this article helpful?
BabyCentre Community Guidelines

32 month old

Android Software Attribution Notice
How do i get hold of my maternity records.

BabyCentre's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organisations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .

Chess Thomas is a freelance health writer and former research editor at BabyCentre.
Where to go next

Delivery, Face and Brow Presentation
Affiliations.
- 1 Vilnius University, Lithuania, Imperial London Healthcare NHS Trust
- 2 University of Health Sciences, Rawalpindi Medical College
- PMID: 33620804
- Bookshelf ID: NBK567727
The term presentation describes the leading part of the fetus or the anatomical structure closest to the maternal pelvic inlet during labor. The presentation can roughly be divided into the following classifications: cephalic, breech, shoulder, and compound. Cephalic presentation is the most common and can be further subclassified as vertex, sinciput, brow, face, and chin. The most common presentation in term labor is the vertex, where the fetal neck is flexed to the chin, minimizing the head circumference.
Face presentation – an abnormal form of cephalic presentation where the presenting part is mentum. This typically occurs because of hyperextension of the neck and the occiput touching the fetal back. Incidence of face presentation is rare, accounting for approximately 1 in 600 of all presentations.
In brow presentation, the neck is not extended as much as in face presentation, and the leading part is the area between the anterior fontanelle and the orbital ridges. Brow presentation is considered the rarest of all malpresentation with a prevalence of 1 in 500 to 1 in 4000 deliveries.
Both face and brow presentations occur due to extension of the fetal neck instead of flexion; therefore, conditions that would lead to hyperextension or prevent flexion of the fetal neck can all contribute to face or brow presentation. These risk factors may be related to either the mother or the fetus. Maternal risk factors are preterm delivery, contracted maternal pelvis, platypelloid pelvis, multiparity, previous cesarean section, black race. Fetal risk factors include anencephaly, multiple loops of cord around the neck, masses of the neck, macrosomia, polyhydramnios.
These malpresentations are usually diagnosed during the second stage of labor when performing a digital examination. It is possible to palpate orbital ridges, nose, malar eminences, mentum, mouth, gums, and chin in face presentation. Based on the position of the chin, face presentation can be further divided into mentum anterior, posterior, or transverse. In brow presentation, anterior fontanelle and face can be palpated except for the mouth and the chin. Brow presentation can then be further described based on the position of the anterior fontanelle as frontal anterior, posterior, or transverse.
Diagnosing the exact presentation can be challenging, and face presentation may be misdiagnosed as frank breech. To avoid any confusion, a bedside ultrasound scan can be performed. The ultrasound imaging can show a reduced angle between the occiput and the spine or, the chin is separated from the chest. However, ultrasound does not provide much predicting value in the outcome of the labor.
Copyright © 2024, StatPearls Publishing LLC.
- Continuing Education Activity
- Introduction
- Anatomy and Physiology
- Indications
- Contraindications
- Preparation
- Technique or Treatment
- Complications
- Clinical Significance
- Enhancing Healthcare Team Outcomes
- Review Questions
Publication types
- Study Guide
- Trying to Conceive
- Signs & Symptoms
- Pregnancy Tests
- Fertility Testing
- Fertility Treatment
- Weeks & Trimesters
- Staying Healthy
- Preparing for Baby
- Complications & Concerns
- Pregnancy Loss
- Breastfeeding
- School-Aged Kids
- Raising Kids
- Personal Stories
- Everyday Wellness
- Safety & First Aid
- Immunizations
- Food & Nutrition
- Active Play
- Pregnancy Products
- Nursery & Sleep Products
- Nursing & Feeding Products
- Clothing & Accessories
- Toys & Gifts
- Ovulation Calculator
- Pregnancy Due Date Calculator
- How to Talk About Postpartum Depression
- Editorial Process
- Meet Our Review Board
Fetal Positions for Labor and Birth
Knowing your baby's position can you help ease pain and speed up labor
In the last weeks of pregnancy , determining your baby's position can help you manage pain and discomfort. Knowing your baby's position during early labor can help you adjust your own position during labor and possibly even speed up the process.
Right or Left Occiput Anterior
Illustration by JR Bee, Verywell
Looking at where the baby's head is in the birth canal helps determine the fetal position.The front of a baby's head is referred to as the anterior portion and the back is the posterior portion. There are two different positions called occiput anterior (OA) positions that may occur.
The left occiput anterior (LOA) position is the most common in labor. In this position, the baby's head is slightly off-center in the pelvis with the back of the head toward the mother's left thigh.
The right occiput anterior (ROA) presentation is also common in labor. In this position, the back of the baby is slightly off-center in the pelvis with the back of the head toward the mother's right thigh.
In general, OA positions do not lead to problems or additional pain during labor or birth.
Right or Left Occiput Transverse
Illustration by JR Bee, Verywell
When facing out toward the mother's right thigh, the baby is said to be left occiput transverse (LOT). This position is halfway between a posterior and anterior position. If the baby was previously in a posterior position (in either direction), the LOT position indicates positive movement toward an anterior position.
When the baby is facing outward toward the mother's left thigh, the baby is said to be right occiput transverse (ROT). Like the previous presentation, ROT is halfway between a posterior and anterior position. If the baby was previously in a posterior position, ROT is a sign the baby is making a positive move toward an anterior position.
When a baby is in the left occiput transverse position (LOT) or right occiput transverse (ROT) position during labor, it may lead to more pain and a slower progression.
Tips to Reduce Discomfort
There are several labor positions a mother can try to alleviate pain and encourage the baby to continue rotating toward an anterior position, including:
- Pelvic tilts
- Standing and swaying
A doula , labor nurse, midwife , or doctor may have other suggestions for positions.
Right or Left Occiput Posterior
When facing forward, the baby is in the occiput posterior position. If the baby is facing forward and slightly to the left (looking toward the mother's right thigh) it is in the left occiput posterior (LOP) position. This presentation can lead to more back pain (sometimes referred to as " back labor ") and slow progression of labor.
In the right occiput posterior position (ROP), the baby is facing forward and slightly to the right (looking toward the mother's left thigh). This presentation may slow labor and cause more pain.
To help prevent or decrease pain during labor and encourage the baby to move into a better position for delivery, mothers can try a variety of positions, including:
- Hands and knees
- Pelvic rocking
Mothers may try other comfort measures, including:
- Bathtub or shower (water)
- Counter pressure
- Movement (swaying, dancing, sitting on a birth ball )
- Rice socks (heat packs)
How a Doctor Determines Baby's Position
Leopold's maneuvers are a series of hands-on examinations your doctor or midwife will use to help determine your baby's position. During the third trimester , the assessment will be done at most of your prenatal visits. Knowing the baby's position before labor begins can help you prepare for labor and delivery.
Once labor begins, a nurse, doctor, or midwife will be able to get a more accurate sense of your baby's position by performing a vaginal exam. When your cervix is dilated enough, the practitioner will insert their fingers into the vagina and feel for the suture lines of the baby's skull as it moves down in the birth canal. It's important to ensure the baby is head down and moving in the right direction.
Labor and delivery may be more complicated if the baby is not in a head-down position, such as in the case of a breech presentation.
How You Can Determine Baby's Position
While exams by health practitioners are an important part of your care, from the prenatal period through labor and delivery, often the best person to assess a baby's position in the pelvis is you. Mothers should pay close attention to how the baby moves and where different movements are felt.
A technique called belly mapping can help mothers ask questions of themselves to assess their baby's movement and get a sense of the position they are in as labor approaches.
For example, the position of your baby's legs can be determined by asking questions about the location and strength of the kicking you feel. The spots where you feel the strongest kicks are most likely where your baby's feet are.
Other landmarks you can feel for include a large, flat plane, which is most likely your baby's back. Sometimes you can feel the baby arching his or her back.
At the top or bottom of the flat plane, you may feel either a hard, round shape (most likely your baby's head) or a soft curve (most likely to be your baby's bottom).
Guittier M, Othenin-Girard V, de Gasquet B, Irion O, Boulvain M. Maternal positioning to correct occiput posterior fetal position during the first stage of labour: a randomised controlled trial . BJOG: An International Journal of Obstetrics & Gynaecology . 2016;123(13):2199-2207. doi:10.1111/1471-0528.13855
Gizzo S, Di Gangi S, Noventa M, Bacile V, Zambon A, Nardelli G. Women’s Choice of Positions during Labour: Return to the Past or a Modern Way to Give Birth? A Cohort Study in Italy . Biomed Res Int . 2014;2014:1-7. doi:10.1155/2014/638093
Ahmad A, Webb S, Early B, Sitch A, Khan K, MacArthur C. Association between fetal position at onset of labor and mode of delivery: a prospective cohort study . Ultrasound in Obstetrics & Gynecology . 2014;43(2):176-182. doi:10.1002/uog.13189
Nishikawa M, Sakakibara H. Effect of nursing intervention program using abdominal palpation of Leopold’s maneuvers on maternal-fetal attachment . Reprod Health . 2013;10(1). doi:10.1186/1742-4755-10-12
Choi S, Park Y, Lee D, Ko H, Park I, Shin J. Sonographic assessment of fetal occiput position during labor for the prediction of labor dystocia and perinatal outcomes . The Journal of Maternal-Fetal & Neonatal Medicine . 2016;29(24):3988-3992. doi:10.3109/14767058.2016.1152250
Bamberg C, Deprest J, Sindhwani N et al. Evaluating fetal head dimension changes during labor using open magnetic resonance imaging . J Perinat Med . 2017;45(3). doi:10.1515/jpm-2016-0005
Gabbe S, Niebyl J, Simpson J et al. Obstetrics . Philadelphia, Pa.: Elsevier; 2012.
By Robin Elise Weiss, PhD, MPH Robin Elise Weiss, PhD, MPH is a professor, author, childbirth and postpartum educator, certified doula, and lactation counselor.

- Vishal's account
- Prenatal Care
Fetal Cephalic Presentation During Pregnancy

What is Cephalic Position?
Types of cephalic position, when does a foetus get into the cephalic position, how do you know if baby is in cephalic position, how to turn a breech baby into cephalic position.
If your baby is moving around in the womb, it’s a good sign as it tells you that your baby is developing just fine. A baby starts moving around in the belly at around 14 weeks. And their first movements are usually called ‘ quickening’ or ‘fluttering’.
A baby can settle into many different positions throughout the pregnancy and it’s alright. But it is only when you have reached your third and final trimester that the position of your baby in your womb will matter the most. The position that your baby takes at the end of the gestation period will most likely be how your baby will make its appearance into the world. Out of all the different positions that your baby can settle into, the cephalic position at 36 weeks is considered the best position. Read on to know more about it.
A baby is in the cephalic position when he is in a head-down position. This is the best position for them to come out in. In case of a ‘cephalic presentation’, the chances of a smooth delivery are higher. This position is where your baby’s head has positioned itself close to the birth canal, and the feet and bottom are up. This is the best position for your baby to be in for safe and healthy delivery.
Your doctor will begin to keep an eye on the position of your baby at around 34 weeks to 36 weeks. The closer you get to your due date, the more important it is that your baby takes the cephalic position. If your baby is not in this position, your doctor will try gentle nudges to get your baby in the right position.
Though it is pretty straightforward, the cephalic position actually has two types, which are explained below:
1. Cephalic Occiput Anterior
Most babies settle in this position. Out of all the babies who settle in cephalic position, 95% of them will settle this way. This is when a baby is in the head-down position but is facing the mother’s back. This is the preferred position as the baby is able to slide out more easily than in any other position.
2. Cephalic Occiput Posterior
In this position, the baby is in the head-down position but the baby’s face is turned towards the mother’s belly. This type of cephalic presentation is not the best position for delivery as the baby’s head could get stuck owing to its wide position. Almost 5% of the babies in cephalic presentation settle into this position. Babies who come out in this position are said to come out ‘sunny side up’.
When a foetus is moving into the cephalic position, it is known as ‘head engagement’. The baby stars getting into this position in the third trimester, between the 32nd and the 36th weeks, to be precise. When the head engagement begins, the foetus starts moving down into the pelvic canal. At this stage, very little of the baby is felt in the abdomen, but more is felt moving downward into the pelvic canal in preparation for birth.
You may think that in order to find out if your baby has a cephalic presentation, an ultrasound is your only option. This is not always the case. You can actually find out the position of your baby just by touching and feeling their movements.
By rubbing your hand on your belly, you might be able to feel their position. If your baby is in the cephalic position, you might feel their kicks in the upper stomach. Whereas, if the baby is in the breech position, you might feel their kicks in the lower stomach.
Even in the cephalic position, it may be possible to tell if your baby is in the anterior position or in the posterior position. When your baby is in the anterior position, they may be facing your back. You may be able to feel your baby move underneath your ribs. It is likely that your belly button will also pop out.
When your baby is in the posterior position, you will usually feel your baby start to kick you in your stomach. When your baby has its back pressed up against your back, your stomach may not look rounded out, but flat instead.
Mothers whose placentas have attached in the front, something known as anterior placenta , you may not be able to feel the movements of your baby as well as you might like to.
Breech babies can make things complicated. Both the mother and the baby will face some problems. A breech baby is positioned head-up and bottom down. In order to deliver the baby, the birth canal needs to open a lot wider than it has to in the cephalic position. Besides this, your baby can get an arm or leg entangled while coming out.
If your baby is in the breech position, there are some things that you can do to encourage the baby to get into the cephalic position. There are a few exercises that could help such as pelvic tilts , swimming , spending a bit of time upside down, and belly dancing are a few ways you can try yourself to get your baby into the head-down position.
If this is not working either, your doctor will try an ECV (External Cephalic Version) . Here, your doctor will be hands-on, applying some gentle, but firm pressure to your tummy. In order to reach a cephalic position, the baby will need to be rolled into a bottom’s up position. This technique is successful around 50% of the time. When this happens, you will be able to have a normal vaginal delivery.
Though it sounds simple enough to get the fetal presentation into cephalic, there are some risks involved with ECV. If your doctor notices your baby’s heart rate starts to become problematic, the doctor will stop the procedure right away.
Most babies get into the cephalic position on their own. This is the most ideal situation as there will be little to no complications during normal vaginal labour. There are different cephalic positions, but these should not cause a lot of issues. If your baby is in any other position, you may need C-Section . Keep yourself updated on the smallest of progress during your pregnancy so that you are aware of everything that is going on. Go for regular check-ups as your doctor will be able to help you in case a complication arises.
When The Head Of Baby Turns Down in Pregnancy Transverse Lie Position in Pregnancy Belly Mapping
- RELATED ARTICLES
- MORE FROM AUTHOR

Is Cloudy Urine During Pregnancy a Cause of Concern?

Gender Reveal with Egg - Tips and Ideas

10 Common Side Effects of Abortion Pills

Acupuncture in Pregnancy - Benefits and Side Effects

Urinary Tract Infection (UTI) During Pregnancy

Body Odour During Pregnancy - Causes and Remedies
Popular on parenting.

245 Rare Boy & Girl Names with Meanings

Top 22 Short Moral Stories For Kids

170 Boy & Girl Names That Mean 'Gift from God'

800+ Unique & Cute Nicknames for Boys & Girls
Latest posts.
Cookie Monster Coloring Pages - Free Printable Pages For Kids
Robot Coloring Pages - Free Printable Pages For Kids

Cheerleading Coloring Pages - Free Printable Pages For Kids

Essay On Holi - 10 lines, Short and Long Essay for Students and Children
GFMER Geneva Foundation for Medical Education and Research
- Annual reports
- GFMER members
- Country coordinators
- Obstetric fistula
- Cervical cancer
- Emergency and surgical care
- Picture of the week
- Social media
- Free medical journals
Obstetrics Simplified - Diaa M. EI-Mowafi
Face Presentation
It is a cephalic presentation in which the head is completely extended.
About 1:300 labours.
- It is less common.
- It occurs during pregnancy.
- Anencephaly: due to absence of the bony vault of the skull and the scalp while the facial portion is normal.
- Loops of the cord around the neck.
- Tumours of the foetal neck e.g. congenital goitre.
- Hypertonicity of the extensor muscles of the neck.
- Dolicocephaly: long antero-posterior diameter of the head, so as the breadth is less than 4/5 of the length.
- Dead or premature foetus.
- Idiopathic.
- It is more common.
- It occurs during labour.
- Contracted pelvis particularly flat pelvis which allows descent of the bitemporal but not the biparietal diameter leads to extension of the head.
- Pendulous abdomen or marked lateral obliquity of the uterus.
- Further deflexion of brow or occipito - posterior positions.
- Other causes of malpresentations as polyhydramnios and placenta praevia.
- Right mento-posterior (RMP).
- Left mento-posterior (LMP).
- Left mento-anterior (LMA).
- Right mento-anterior (RMA), are the more common positions.
- Right mento-transverse (lateral), left mento-transverse, direct mento-posterior and direct mento-anterior are rare and usually transient positions.
The first position (RMP) corresponds to the first normal position (LOA) as the back should be to the left and anterior in the first position. Mento-anterior are more common than mento-posterior as most cases arise from more deflexion of the head in occipito-posterior position usually in flat contracted pelvis.
During pregnancy (difficult)
- The back is difficult to feel.
- The limbs are felt more prominent in mento-anterior position.
- The chin may be felt on the same side of the limbs as a horseshoe-shaped rim in mento-anterior position.
- In mento-posterior, a groove may be felt between the occiput and the back particularly after rupture of the membranes.
- Second pelvic grip: the occiput is at a higher level than the sinciput.
- The FHS are heard below the umbilicus through the foetal chest wall in mento-anterior position.
- Ultrasound or X-ray: confirms the diagnosis and may identify associated foetal anomalies as anencephaly.
During labour
Vaginal examination shows the following identifying features for face:
- supra-orbital ridges,
- the malar processes,
- the nose (rubbery and saddle shaped),
- the mouth with hard areolar ridges.
Late in labour, the face becomes oedematous (tumefaction) so it can be misdiagnosed as a buttock (breech presentation) where the two cheeks are mistaken with buttocks and the mouth with anus and the malar processes with the ischial tuberosities. The following points can differentiate in-between:
Mechanism of Labour
Mento-anterior position
- Engagement by submento-bregmatic diameter 9.5 cm.
- Increased extension.
- Internal rotation of chin 1/8 circle anteriorly.
- Flexion: is the movement by which the head is delivered in mento-anterior position when the submental region hinges below the symphysis. The vulva is much distended by the submento-vertical diameter 11.5 cm.
- Restitution.
- External rotation.
Engagement is delayed because:
- The biparietal diameter does not pass the plane of pelvic inlet until the chin is below the level of the ischial spines and the face begins to distend the perineum.
- Moulding does not occur as in vertex presentation.
Mento-posterior position
- so the head is delivered as mento-anterior.
- Deep transverse arrest of the face: when the chin rotates 1/8 circle anteriorly.
- Persistent mento-posterior: when no rotation occurs.
- Direct mento-posterior: When the chin rotates 1/8 circle posteriorly.
In the last 3 conditions no further progress occurs and labour is obstructed.
Direct mento-posterior, unlike direct occipito-posterior, cannot be delivered because:
- Delivery should occur by extension while the head is already maximally extended.
- As the length of the sacrum is 10 cm and that of neck is only 5 cm, the shoulders enter the pelvis and become impacted while the head still in the pelvis, thus the labour is obstructed.
Management of Labour
Exclude: - Foetal anomalies and - Contracted pelvis.
Mento-anterior
- First stage: as in occipito-posterior.
- Spontaneous delivery usually occurs.
- Forceps delivery may be indicated in prolonged 2nd stage.
- Episiotomy is necessary because of over distension of the vulva.
Mento-posterior
- First stage: as mento-anterior.
- Wait for long anterior rotation of the mentum 3/8 circle and the head will be delivered as mento-anterior. During this period oxytocin is used to compete inertia which is common in such conditions as long as there is no contraindication. Failure of this long rotation is more common than in occipito-posterior position so earlier interference is usually indicated.
- Caesarean section: which is the safest and the current alternative in modern obstetrics.
- Manual rotation and forceps extraction as mento-anterior, or
- Rotation and extraction by Kielland forceps.
- In the last 2 methods the head should be engaged but they are hazardous to both the mother and foetus so they are nearly out of modern obstetrics.
- Craniotomy: if the foetus is dead.
The face of the foetus is oedematous after delivery so the mother is assured that this will be spontaneously relieved within few days.
Complications
See complications of malpresentations and malposition.
- Dystocia : Guidelines, reviews
- Getting pregnant
- Preschooler
- Life as a parent
- Baby essentials
- Find your birth club
- Free antenatal classes
- Meet local parents & parents-to-be
- See all in Community
- Ovulation calculator
- Am I pregnant quiz
- How to get pregnant fast
- Best sex positions
- Signs of pregnancy
- How many days after your period can you get pregnant?
- How age affects fertility
- Very early signs of pregnancy
- What fertile cervical mucus looks like
- Think you're pregnant but the test is negative?
- Faint line on pregnancy test
- See all in Getting pregnant
- Pregnancy week by week
- How big is my baby?
- Due date calculator
- Baby movements week by week
- Symptoms you should never ignore
- Hospital bag checklist
- Signs of labour
- Your baby's position in the womb
- Baby gender predictor
- Vaginal spotting
- Fetal development chart
- See all in Pregnancy
- Baby names finder
- Baby name inspiration
- Popular baby names 2022
- Numerology calculator
- Gender-neutral names
- Old-fashioned names
- See all in Baby names
- Your baby week by week
- Baby milestones by month
- Baby rash types
- Baby poop chart
- Ways to soothe a crying baby
- Safe co-sleeping
- Teething signs
- Growth spurts
- See all in Baby
- Your toddler month by month
- Toddler development milestones
- Dealing with tantrums
- Toddler meals
- Food & fussy eating
- When to start potty training
- Moving from a cot to a bed
- Help your child sleep through
- Games & activities
- Vomiting: what's normal?
- See all in Toddler
- Your child month by month
- Food ideas & nutrition
- How kids learn to share
- Coping with aggression
- Bedtime battles
- Anxiety in children
- Dealing with public tantrums
- Great play ideas
- Is your child ready for school?Top tips for starting school
- See all in Preschooler
- Postnatal symptoms to watch out for
- Stitches after birth
- Postpartum blood clots
- Baby showers
- Sex secrets for parents
- See all in Life as a parent
- Best baby products
- Best formula and bottles for a windy baby
- Best car seats if you need three to fit
- Best nappies
- Best Moses baskets
- Best baby registries
- Best baby sleeping bags
- Best baby humidifier
- Best baby monitors
- Best baby bath seat
- Best baby food
- See all in Baby essentials
- Back pain in pregnancy
- Pelvic girdle pain
- Perineal massage
- Signs you're having a boy
- Signs you're having a girl
- Can you take fish oil while pregnant?
- 18 weeks pregnant bump
- Can you eat salami when pregnant?
- Edwards' syndrome
- Missed miscarriage
- Should I harvest my colostrum?
- Rhesus positive vs. Rhesus negative
- What do contractions feel like?
- Hunger in early pregnancy
- First poop after birth
- When do babies sit up?
- When can babies have salt?
- MMR vaccine rash
- Vaping while breastfeeding
- How to transition from formula to milk
- When do babies start grabbing things?
- Sperm allergy: can sperm cause itching?
- How long after taking folic acid can I get pregnant?
Cephalic presentation at 28 weeks
I had my first growth scan today, the baby is growing fine but she noted he was in the cephalic position.
Probably overthinking but do I need to be worried or is it normal at this stage for baby to be head down?
- l lucie2014 Posted 21-02-20 It's perfect!
- v Vickyc123 Posted 21-02-20 At this stage your baby will still be able to do full somersaults in there, so he (I'm assuming a baby boy) can move several times into breach or cephalic position. I think, but don't quote me on this, by 36/37 weeks you want baby to finally move into head down position and he's likely to stay this way until birth. But, some babies are breach right up until a day or two before labour. The midwife will keep checking after 32 weeks to check his positioning, at least mine did all those years ago. And they check to see whether they've engaged by 37 weeks.
- l Luluh1985 Posted 21-02-20 Think it's normal. I'm 27 weeks today and my baby has been in that position for about 5 weeks. She moves occasionally but every scan and every hospital check she is like cephalic. Just a comfy position for them I guess
- m Mala93 Posted 21-02-20 Don’t worry, babies keep moving around. At my 27w growth scan the baby was in vertex position. Had another scan at 30w and the baby is breech. My obgyn says it’s too early to be in one position.
- Book your antenatal a course
- Volunteer with us
Pregnancy maternity notes: understanding them
Read time 5 minutes

If you’re feeling a bit confused by it all, here’s what you might want to know about your notes
What are your maternity notes or maternity notes folder?
Maternity notes, or handheld notes, are a record book/folder where your midwife will note down details of each appointment. They’re a standardised, national maternity record and you’ll need to take them with you to each antenatal appointment.
When to take them with you
Take your maternity notes wherever you go (within reason…) including on holidays, in case you need medical attention when you’re away from home. It might not be easy to understand everything in your notes, so it’s a good idea to ask your maternity team to explain anything you’re unsure about.
What’s in your maternity (handheld) notes
Your maternity notes contain the following information:
- Your name, address and hospital number and details.
- Your medical history including any disease you are currently suffering from and medications you are taking.
- Your family medical history, for example if any of your family members suffered from medical conditions like diabetes, blood pressure etc.
- Information about previous pregnancies and births.
- Your appointment times.
- Results of blood tests and investigations including ultrasound scans.
- Phone numbers for your midwife, birth suite and hospital etc.
- Information collected by your midwife during antenatal checks. This includes your blood pressure, urine tests, vaccines taken, foetal movements and foetal heart. It also includes the way your baby is lying in the womb and engagement – how deep the baby’s head is below the brim of the pelvis.
- Assessment of the baby’s growth inside the womb.
- Any problems encountered during pregnancy.
- Preferences for birth, eg where you would like to give birth, who’ll be your birth partner, what pain relief methods you would like.
- When your labour started and how it progressed. This will include foetal heart monitoring, your posture during labour and delivery, what type of birth you had and how the placenta was delivered.
Pamphlets and extra information
As well as all the above information about you, you may be given:
- Phone numbers for charities that work with parents and babies.
- Pamphlets on topics you might find interesting, eg breastfeeding, eating well when you’re pregnant.
- Advice on issues during pregnancy.
Meaning of abbreviations used in maternity notes
Urine test results (for presence of protein or sugar)
NAD: nothing abnormal detected
Nil: none found
Tr (trace): small amount of sugar or protein found
+ , ++ , +++: presence of greater amount or protein
Heartbeat or activity
FHH: foetal heart heard
FHHR: foetal heart heard and regular
FHNH: foetal heart not heard
FMF: foetal movements felt
Position of your baby – the way it is lying in the womb
L: longitudinal (length-wise)
O: oblique (slanting)
T: transverse (sideways)
Which part it presents towards the birth canal
C: cephalic (head first – also called as vertex)
B or Br: bottom first or breech
OA: occiput anterior (head down, facing your back)
OP: occiput posterior (head down, facing your front)
OL: occiput lateral (head down, facing your side)
L or R in front of these tell you which side of your body your baby is.
Engagement of baby’s head in the pelvis
NE, NEng, Not Eng: not engaged
E or Eng = engaged
4/5 = sitting on the pelvic brim
3/5 = lower but most still above the brim
2/5 = engaged, as most is below the brim
1/5 or 0/5 = deeply engaged.
If it’s your first baby, engagement tends to happen in the last weeks. In subsequent pregnancies, it may happen later or even not until labour has started.
This page was last reviewed in May 2018.
Further information.
Our support line offers practical and emotional support with feeding your baby and general enquiries for parents, members and volunteers: 0300 330 0700.
We also offer antenatal courses which are a great way to find out more about birth, labour and life with a new baby.
Make friends with other parents-to-be and new parents in your local area for support and friendship by seeing what NCT activities are happening nearby.
Information you can trust from NCT
When it comes to content, our aim is simple: every parent should have access to information they can trust.
All of our articles have been thoroughly researched and are based on the latest evidence from reputable and robust sources. We create our articles with NCT antenatal teachers, postnatal leaders and breastfeeding counsellors, as well as academics and representatives from relevant organisations and charities.
Read more about our editorial review process .
Related articles

Courses & workshops

In-person NCT Antenatal course

NCT Antenatal refresher course


IMAGES
VIDEO
COMMENTS
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
Engagement. The movement of the fetus to cephalic presentation is called head engagement.It occurs in the third trimester.In head engagement, the fetal head descends into the pelvic cavity so that only a small part (or none) of it can be felt abdominally. The perineum and cervix are further flattened and the head may be felt vaginally. Head engagement is known colloquially as the baby drop ...
Turning a Fetus. The cephalic position is when a fetus is head down when it is ready to enter the birth canal. This is one of a few variations of how a fetus can rest in the womb and is considered the ideal one for labor and delivery. About 96% of babies are born in the cephalic position. Most settle into it between the 32nd and 36th weeks of ...
A cephalic presentation or head presentation or head-first presentation is a situation at childbirth where the fetus is in a longitudinal lie and the head enters the pelvis first; the most common form of cephalic presentation is the vertex presentation where the occiput is the leading part (the part that first enters the birth canal). All other presentations are abnormal (malpresentations ...
Cephalic Presentation is the Best Position. The baby's position in the womb tells a lot about the delivery and the complications it may pose during labor. Cephalic presentation is considered the safest birthing position. The good news is that most babies naturally settle in this position by the 36th week of pregnancy.
Understanding your maternity notes. Your maternity notes show the healthcare professionals taking care of you during your pregnancy how you and your baby are doing. These notes could be on paper, or they could be stored in an app. They include things like information about your baby's growth, your expected due date and results of any checks and ...
In the cephalic presentation, the baby is head down, chin tucked to chest, facing their mother's back. This position typically allows for the smoothest delivery, as baby's head can easily move down the birth canal and under the pubic bone during childbirth. While that's not to say there can't be complications, this is the ideal position ...
Your pregnancy care provider may call it fetal presentation or the presentation of the fetus (although this usually refers to which part of a fetus's body will move into the birth canal first). Knowing the position of the fetus helps a pregnancy care provider determine if it's safe for you to have a vaginal delivery or if they should ...
In the cephalic presentation with a well-flexed head, the largest transverse diameter of the fetal head is the biparietal diameter (9.5 cm). In the breech, the widest diameter is the bitrochanteric diameter. Clinically, engagement can be confirmed by palpation of the presenting part both abdominally and vaginally.
Depending on your condition, the doctor may recommend External Cephalic Version, wherein they'll try to turn the baby to a cephalic presentation by applying calculated pressure to the abdomen. After all, if the baby is in breech position, the possibility of having a Cesarean delivery increases. At home, you may also find yourself browsing ...
Brow presentation is considered the rarest of all malpresentation with a prevalence of 1 in 500 to 1 in 4000 deliveries. Both face and brow presentations occur due to extension of the fetal neck instead of flexion; therefore, conditions that would lead to hyperextension or prevent flexion of the fetal neck can all contribute to face or brow ...
The vertex presentation describes the orientation a fetus should be in for a safe vaginal delivery. It becomes important as you near your due date because it tells your pregnancy care provider how they may need to deliver your baby. Vertex means "crown of the head.". This means that the crown of the fetus's head is presenting towards the ...
When the baby is facing outward toward the mother's left thigh, the baby is said to be right occiput transverse (ROT). Like the previous presentation, ROT is halfway between a posterior and anterior position. If the baby was previously in a posterior position, ROT is a sign the baby is making a positive move toward an anterior position.
External cephalic version (ECV) is a process by which a breech baby can sometimes be turned from buttocks or foot first to head first. It is a manual procedure that is recommended by national guidelines for breech presentation of a pregnancy with a single baby, in order to enable vaginal delivery. It is usually performed late in pregnancy, that is, after 36 gestational weeks, preferably 37 ...
2. Cephalic Occiput Posterior. In this position, the baby is in the head-down position but the baby's face is turned towards the mother's belly. This type of cephalic presentation is not the best position for delivery as the baby's head could get stuck owing to its wide position. Almost 5% of the babies in cephalic presentation settle ...
In a face presentation, the fetal head and neck are hyperextended, causing the occiput to come in contact with the upper back of the fetus while lying in a longitudinal axis. The presenting portion of the fetus is the fetal face between the orbital ridges and the chin. The fetal chin (mentum) is the point designated for reference during an ...
Face Presentation: Frank Breech: The foetal mouth and malar processes form the apexes of a triangle. The anus is on the same line with the ischial tuberosities. The gum is felt hard through the mouth. No hard object through the anus. The examining finger may be sucked by the foetal mouth during vaginal examination. The anus does not suck the ...
Sinciput, brow, and face presentations represent the 3 classical variants of cephalic malpresentation and are characterized by a progressive deflection from vertex presentation. These classic variants of malpresentation are quite rare, with reported incidences of 1 in 600 to 1 in 2000 for face presentation. 1.
Cephalic presentation at 28 weeks. m. Maya19922. Posted 21-02-20. Hi all, (FTM here) I had my first growth scan today, the baby is growing fine but she noted he was in the cephalic position. Probably overthinking but do I need to be worried or is it normal at this stage for baby to be head down?
This includes your blood pressure, urine tests, vaccines taken, foetal movements and foetal heart. It also includes the way your baby is lying in the womb and engagement - how deep the baby's head is below the brim of the pelvis. Assessment of the baby's growth inside the womb. Any problems encountered during pregnancy.
Understanding Cephalic Presentation During Pregnancy • Is your baby in the right position for a safe and smooth delivery? Watch this video to understand ceph...
The most common way for a fetus to present at 38 weeks is with the back of the head closest to the cervix and turned slightly to the mother's left. This is termed left occiput anterior, or loa. Although loa is the most common presentation, roa, or right occiput anterior, is not uncommon and is not associated with any increased complications.