

Step-By-Step Guide to Writing a Nursing Case Study
You now know all the key sections you need to include in a nursing case study. You also know what exactly you need to do in each section. It is now time to know how exactly to write a nursing case study. The process detailed below should be easy to follow because you now know the typical structure of nursing case studies.
When given a nursing case study assignment, the first thing you need to do is to read. You need to read two pieces of information slowly and carefully.
First, you need to read the prompt itself slowly and carefully. This is important because the prompt will have important bits of information that you need to know, including the style, the format, the word count, and the number of references needed. All these bits of information are important to know to ensure what you are writing is the right thing.
Second, you need to read the patient scenario slowly and carefully. You should do this to understand it clearly so that you do not make any mistakes in your analysis.
- Create a rough outline
Failure to plan is a plan to fail. So do not fail to plan. In other words, do not fail to create an outline for your case study analysis. Use the template provided in this essay to create a rough outline for your nursing case study analysis.
Make sure your outline is as detailed as it can be at this stage. You can do light research to achieve this aim. However, this is not exactly necessary because this is just a rough outline.
- Conduct thorough research
After creating a rough outline, you should conduct thorough research. Your research should especially focus on providing a credible and evidence-based nursing assessment on the patient problem(s). The evidence you should use should only be from recent nursing or medical literature.
You will also need to conduct thorough research to come up with an effective intervention or nursing care plan. So when researching the patient’s problem and its diagnosis, you should also research the most suitable intervention or you should do it right after.
When conducting research, you should always note down your sources. So for every piece of information you find and what to use, you should have its reference.
After conducting thorough research, you should enhance your rough outline using the new pieces of information you have discovered. Make sure it is as comprehensive as possible.
- Write your nursing case study
At this stage, you simply need to follow your comprehensive outline to write your case study analysis. If you created a good outline, you should find it very easy to write your nursing case study analysis.
If you did not, you will find it difficult to write your nursing case study. Whenever you are stuck when writing your case study analysis paper, you should re-read the part of this article where we explain what to include in every section of your analysis. Doing so will help you know what exactly to write to continue with your essay. Writing a nursing case study analysis usually takes only a few hours.
- Reference your case study
After writing your case study, make sure you add all in-text citations if you had not added them already. And when adding them, you should make sure you follow the style/format recommended in the assignment prompt (usually APA or Harvard style).
After adding in-text citations exactly where they need to be and in the right format, add all the references you have used in a references page. And you should add them correctly as per the rules of the style you were asked to use.
Do not forget to organize your references alphabetically after you are done creating your references page.
- Thoroughly edit your case study
After STEP 5 above, you need to edit your case study. You should edit it slowly and carefully. Do this by proofreading it twice. Proofread it slowly each time to discover all the grammar, style, and punctuation errors. Remove all the errors you find.
After proofreading your essay twice, check it one more time to make sure every sentence is very easy to understand. This is what will transform your ordinary case study into an A-grade case study. Of course, it must also have all the standard sections expected in a case study.
Just to make sure your case study is absolutely perfect, check it one more time using a grammarly.com or a similar computer grammar checker. Doing this will help you catch and eliminate all the remaining errors in your work.
- Submit your case study analysis
After you are done proofreading and editing your case study analysis, it will be 100% ready for submission. Just convert it into the format it is required in and submit it.
Published by laura
View all posts by laura
Nursing Care Plans (NCP): Ultimate Guide and List
Writing the best nursing care plan requires a step-by-step approach to complete the parts needed for a care plan correctly. This tutorial will walk you through developing a care plan. This guide has the ultimate database and list of nursing care plans (NCP) and nursing diagnosis samples for our student nurses and professional nurses to use—all for free! Care plan components, examples, objectives, and purposes are included with a detailed guide on writing an excellent nursing care plan or a template for your unit.
Table of Contents
Standardized care plans, individualized care plans, purposes of a nursing care plan, three-column format, four-column format, student care plans, step 1: data collection or assessment, step 2: data analysis and organization, step 3: formulating your nursing diagnoses, step 4: setting priorities, short-term and long-term goals, components of goals and desired outcomes, types of nursing interventions, step 7: providing rationale, step 8: evaluation, step 9: putting it on paper, basic nursing and general care plans, surgery and perioperative care plans, cardiac care plans, endocrine and metabolic care plans, gastrointestinal, hematologic and lymphatic, infectious diseases, integumentary, maternal and newborn care plans, mental health and psychiatric, musculoskeletal, neurological, pediatric nursing care plans, reproductive, respiratory, recommended resources, references and sources, what is a nursing care plan.
A nursing care plan (NCP) is a formal process that correctly identifies existing needs and recognizes a client’s potential needs or risks. Care plans provide a way of communication among nurses, their patients, and other healthcare providers to achieve healthcare outcomes. Without the nursing care planning process, the quality and consistency of patient care would be lost.
Nursing care planning begins when the client is admitted to the agency and is continuously updated throughout in response to the client’s changes in condition and evaluation of goal achievement. Planning and delivering individualized or patient-centered care is the basis for excellence in nursing practice.
Types of Nursing Care Plans
Care plans can be informal or formal: An informal nursing care plan is a strategy of action that exists in the nurse ‘s mind. A formal nursing care plan is a written or computerized guide that organizes the client’s care information.
Formal care plans are further subdivided into standardized care plans and individualized care plans: Standardized care plans specify the nursing care for groups of clients with everyday needs. Individualized care plans are tailored to meet a specific client’s unique needs or needs that are not addressed by the standardized care plan.
Standardized care plans are pre-developed guides by the nursing staff and health care agencies to ensure that patients with a particular condition receive consistent care. These care plans are used to ensure that minimally acceptable criteria are met and to promote the efficient use of the nurse’s time by removing the need to develop common activities that are done repeatedly for many of the clients on a nursing unit.
Standardized care plans are not tailored to a patient’s specific needs and goals and can provide a starting point for developing an individualized care plan .
Care plans listed in this guide are standard care plans which can serve as a framework or direction to develop an individualized care plan.
An individualized care plan care plan involves tailoring a standardized care plan to meet the specific needs and goals of the individual client and use approaches shown to be effective for a particular client. This approach allows more personalized and holistic care better suited to the client’s unique needs, strengths, and goals.
Additionally, individualized care plans can improve patient satisfaction . When patients feel that their care is tailored to their specific needs, they are more likely to feel heard and valued, leading to increased satisfaction with their care. This is particularly important in today’s healthcare environment, where patient satisfaction is increasingly used as a quality measure.
Tips on how to individualize a nursing care plan:
- Perform a comprehensive assessment of the patient’s health, history, health status, and desired goals.
- Involve the patient in the care planning process by asking them about their health goals and preferences. By involving the client, nurses can ensure that the care plan is aligned with the patient’s goals and preferences which can improve patient engagement and compliance with the care plan.
- Perform an ongoing assessment and evaluation as the patient’s health and goals can change. Adjust the care plan accordingly.
The following are the goals and objectives of writing a nursing care plan:
- Promote evidence-based nursing care and render pleasant and familiar conditions in hospitals or health centers.
- Support holistic care, which involves the whole person, including physical, psychological, social, and spiritual, with the management and prevention of the disease.
- Establish programs such as care pathways and care bundles. Care pathways involve a team effort to reach a consensus regarding standards of care and expected outcomes. In contrast, care bundles are related to best practices concerning care for a specific disease.
- Identify and distinguish goals and expected outcomes.
- Review communication and documentation of the care plan.
- Measure nursing care.
The following are the purposes and importance of writing a nursing care plan:
- Defines nurse’s role. Care plans help identify nurses’ unique and independent role in attending to clients’ overall health and well-being without relying entirely on a physician’s orders or interventions.
- Provides direction for individualized care of the client. It serves as a roadmap for the care that will be provided to the patient and allows the nurse to think critically in developing interventions directly tailored to the individual.
- Continuity of care. Nurses from different shifts or departments can use the data to render the same quality and type of interventions to care for clients, therefore allowing clients to receive the most benefit from treatment.
- Coordinate care. Ensures that all members of the healthcare team are aware of the patient’s care needs and the actions that need to be taken to meet those needs preventing gaps in care.
- Documentation. It should accurately outline which observations to make, what nursing actions to carry out, and what instructions the client or family members require. If nursing care is not documented correctly in the care plan, there is no evidence the care was provided.
- Serves as a guide for assigning a specific staff to a specific client. There are instances when a client’s care needs to be assigned to staff with particular and precise skills.
- Monitor progress. To help track the patient’s progress and make necessary adjustments to the care plan as the patient’s health status and goals change.
- Serves as a guide for reimbursement. The insurance companies use the medical record to determine what they will pay concerning the hospital care received by the client.
- Defines client’s goals. It benefits nurses and clients by involving them in their treatment and care.
A nursing care plan (NCP) usually includes nursing diagnoses, client problems, expected outcomes, nursing interventions, and rationales. These components are elaborated on below:
- Client health assessment , medical results, and diagnostic reports are the first steps to developing a care plan. In particular, client assessment relates to the following areas and abilities: physical, emotional, sexual, psychosocial, cultural, spiritual/transpersonal, cognitive, functional, age-related, economic, and environmental. Information in this area can be subjective and objective.
- Nursing diagnosis . A nursing diagnosis is a statement that describes the patient’s health issue or concern. It is based on the information gathered about the patient’s health status during the assessment.
- Expected client outcomes. These are specific goals that will be achieved through nursing interventions. These may be long and short-term.
- Nursing interventions . These are specific actions that will be taken to address the nursing diagnosis and achieve expected outcomes . They should be based on best practices and evidence-based guidelines.
- Rationales. These are evidence-based explanations for the nursing interventions specified.
- Evaluation . These includes plans for monitoring and evaluating a patient’s progress and making necessary adjustments to the care plan as the patient’s health status and goals change.
Care Plan Formats
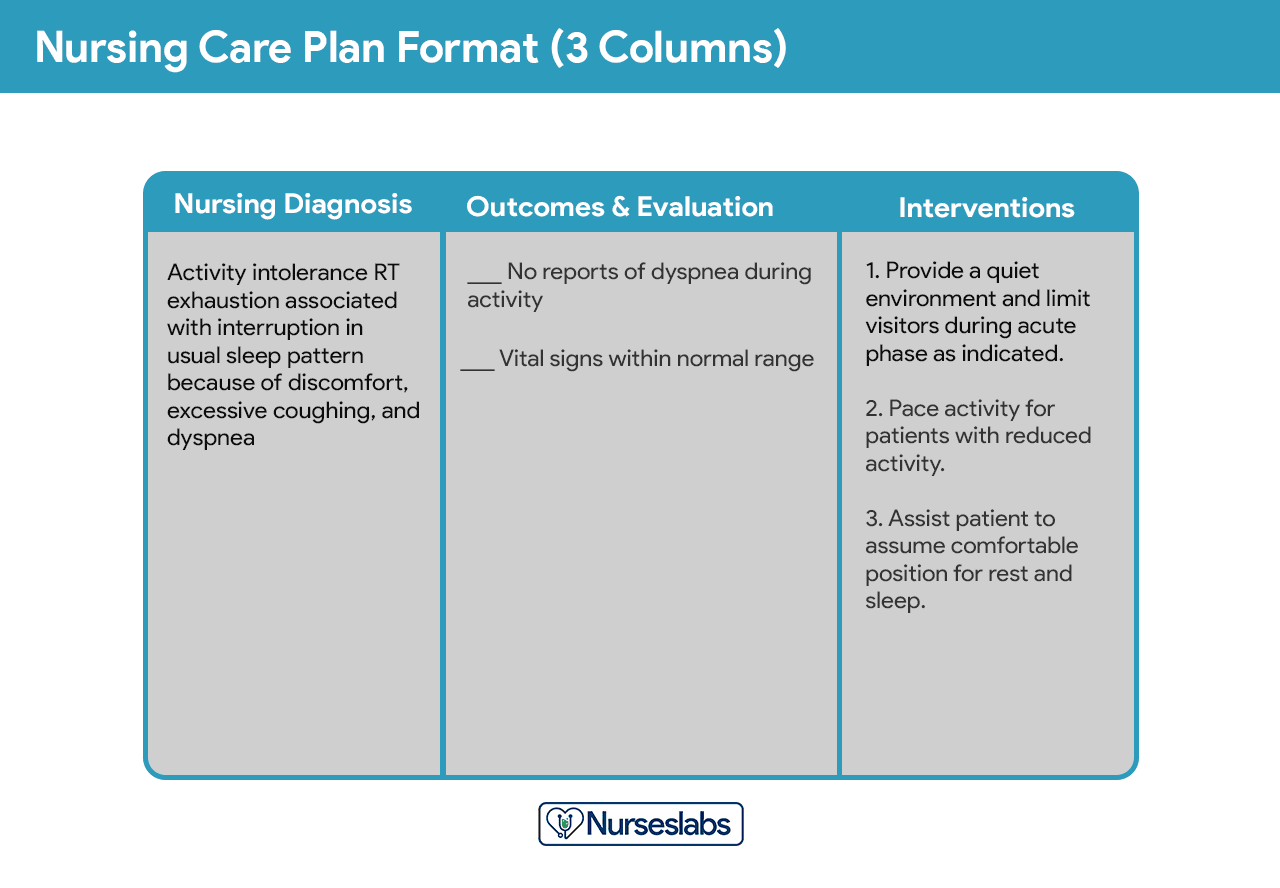
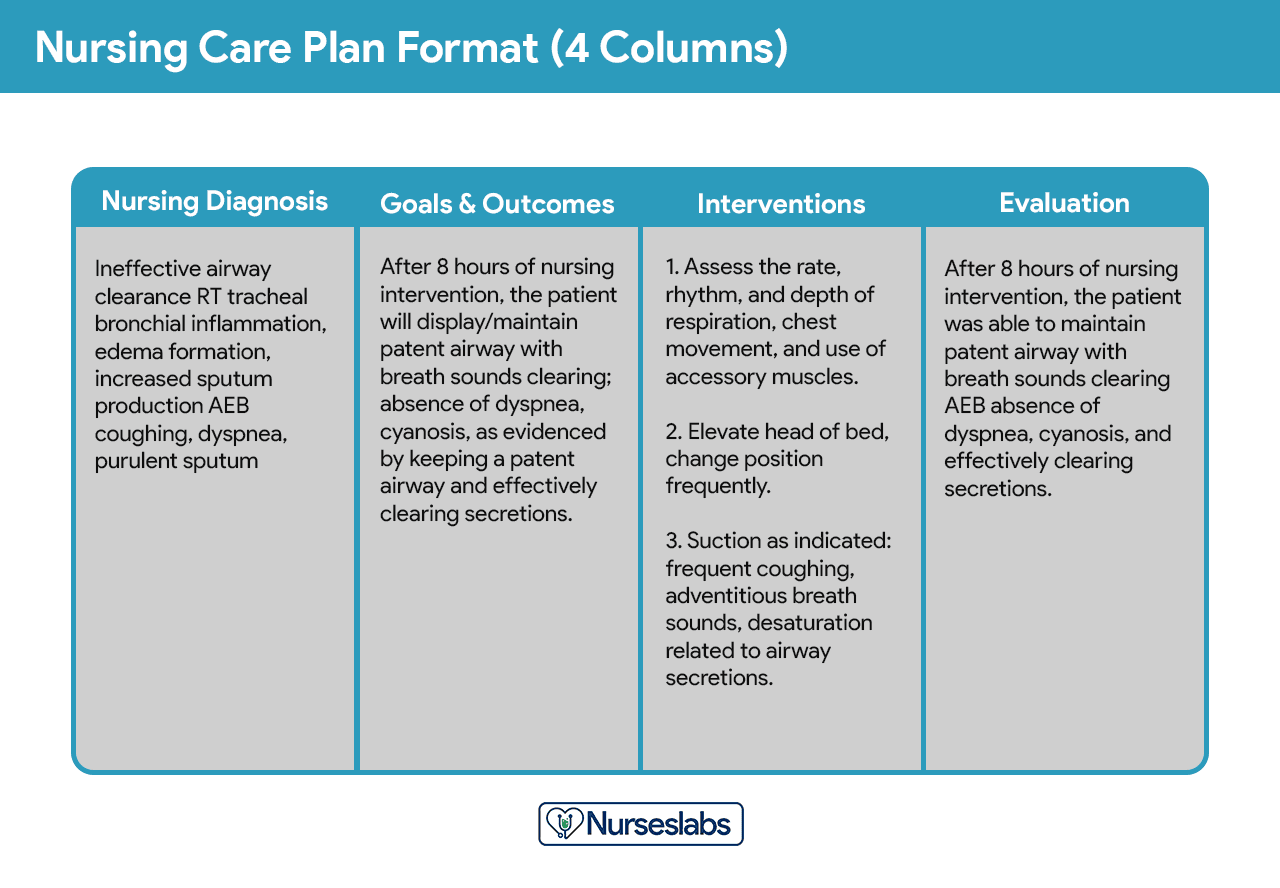
Nursing care plan formats are usually categorized or organized into four columns: (1) nursing diagnoses, (2) desired outcomes and goals, (3) nursing interventions, and (4) evaluation. Some agencies use a three-column plan where goals and evaluation are in the same column. Other agencies have a five-column plan that includes a column for assessment cues.
The three-column plan has a column for nursing diagnosis, outcomes and evaluation, and interventions.
This format includes columns for nursing diagnosis, goals and outcomes, interventions, and evaluation.
Below is a document containing sample templates for the different nursing care plan formats. Please feel free to edit, modify, and share the template.
Download: Printable Nursing Care Plan Templates and Formats
Student care plans are more lengthy and detailed than care plans used by working nurses because they serve as a learning activity for the student nurse.
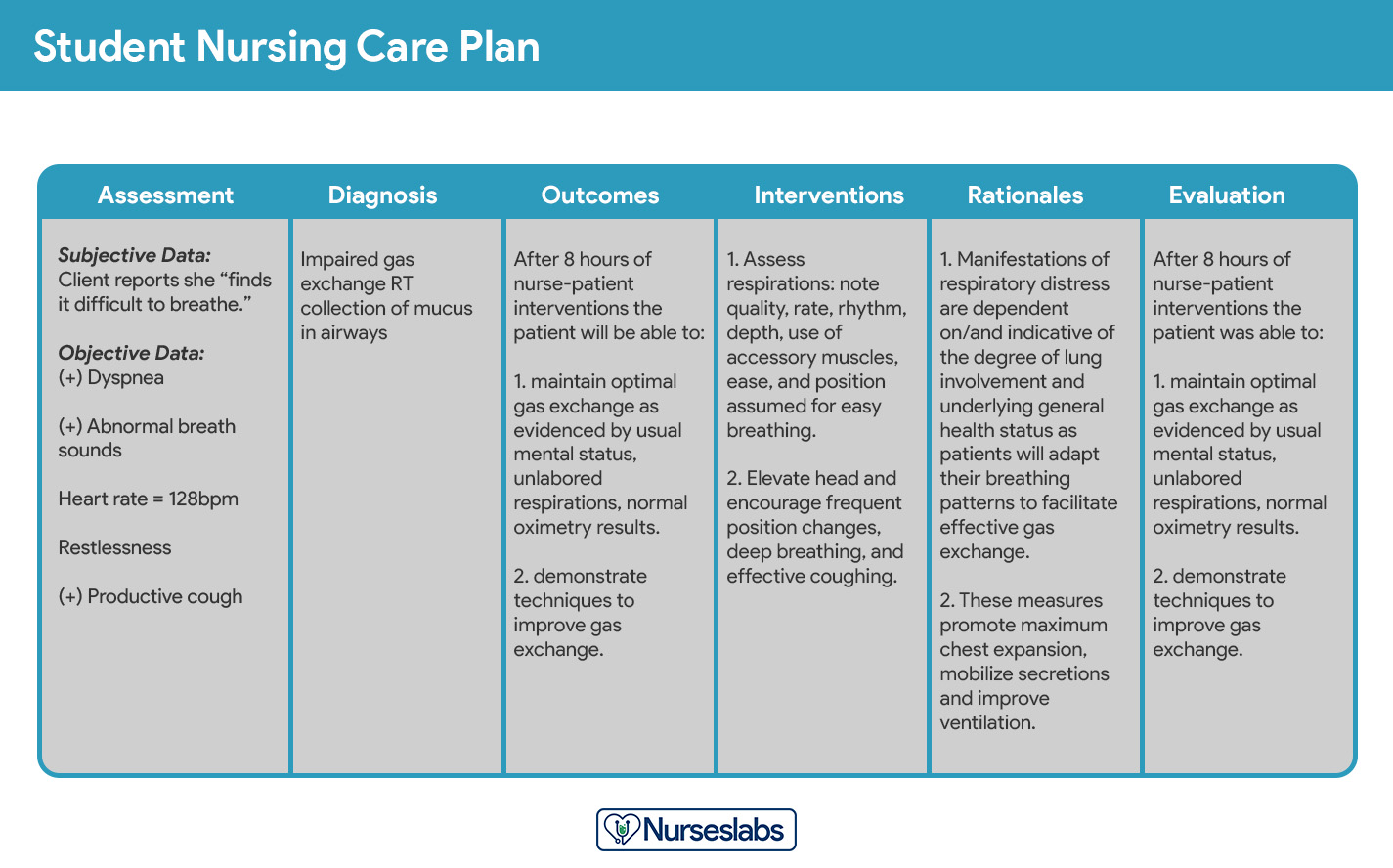
Care plans by student nurses are usually required to be handwritten and have an additional column for “Rationale” or “Scientific Explanation” after the nursing interventions column. Rationales are scientific principles that explain the reasons for selecting a particular nursing intervention.
Writing a Nursing Care Plan
How do you write a nursing care plan (NCP)? Just follow the steps below to develop a care plan for your client.
The first step in writing a nursing care plan is to create a client database using assessment techniques and data collection methods (physical assessment, health history, interview, medical records review, and diagnostic studies). A client database includes all the health information gathered . In this step, the nurse can identify the related or risk factors and defining characteristics that can be used to formulate a nursing diagnosis. Some agencies or nursing schools have specific assessment formats you can use.
Critical thinking is key in patient assessment, integrating knowledge across sciences and professional guidelines to inform evaluations. This process, crucial for complex clinical decision-making, aims to identify patients’ healthcare needs effectively, leveraging a supportive environment and reliable information
Now that you have information about the client’s health, analyze, cluster, and organize the data to formulate your nursing diagnosis, priorities, and desired outcomes.
Nursing diagnoses are a uniform way of identifying, focusing on and dealing with specific client needs and responses to actual and high-risk problems. Actual or potential health problems that can be prevented or resolved by independent nursing intervention are termed nursing diagnoses.
We’ve detailed the steps on how to formulate your nursing diagnoses in this guide: Nursing Diagnosis (NDx): Complete Guide and List .
Setting priorities involves establishing a preferential sequence for addressing nursing diagnoses and interventions. In this step, the nurse and the client begin planning which of the identified problems requires attention first. Diagnoses can be ranked and grouped as having a high, medium, or low priority. Life-threatening problems should be given high priority.
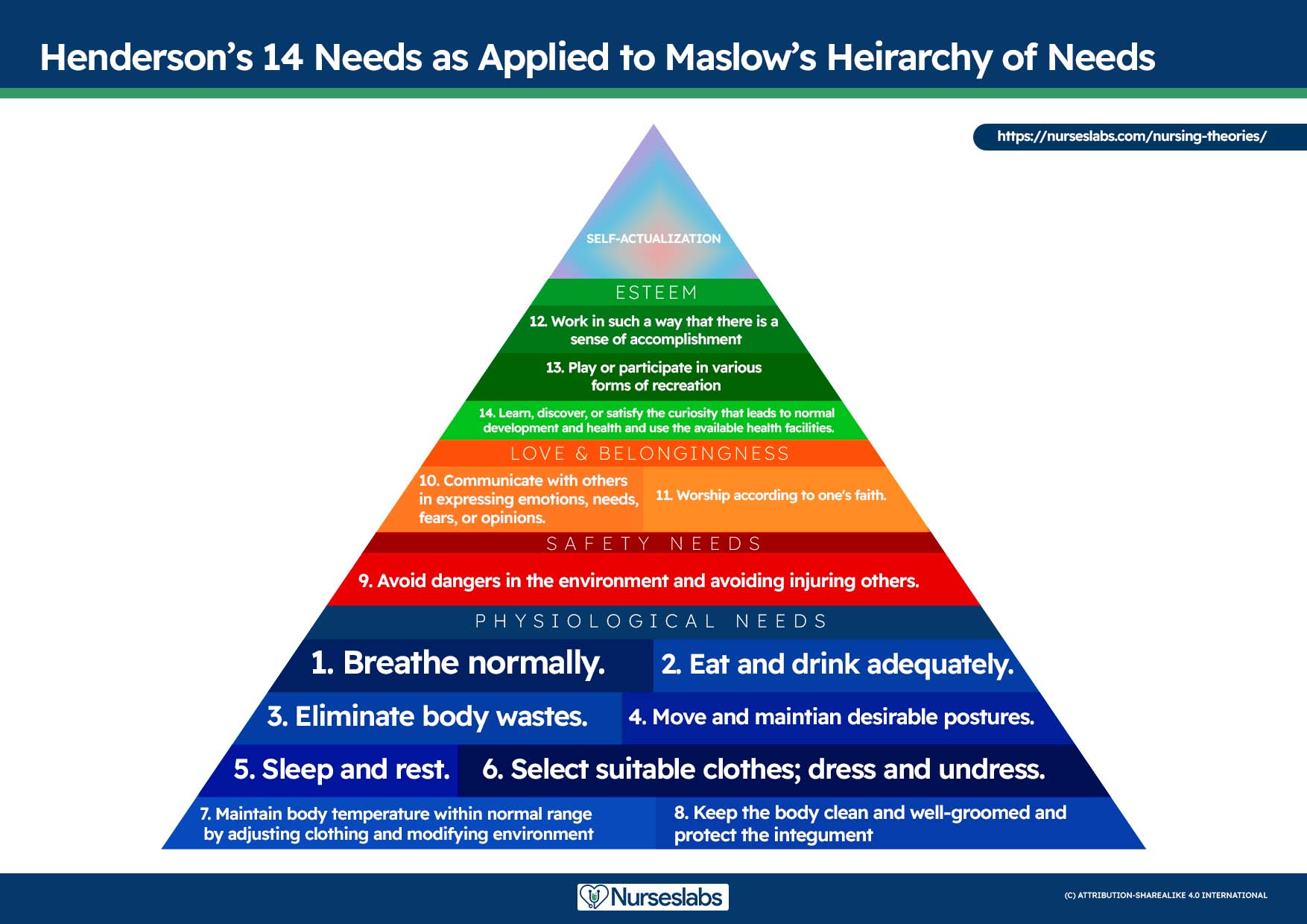
A nursing diagnosis encompasses Maslow’s Hierarchy of Needs and helps to prioritize and plan care based on patient-centered outcomes. In 1943, Abraham Maslow developed a hierarchy based on basic fundamental needs innate to all individuals. Basic physiological needs/goals must be met before higher needs/goals can be achieved, such as self-esteem and self-actualization. Physiological and safety needs are the basis for implementing nursing care and interventions. Thus, they are at the base of Maslow’s pyramid, laying the foundation for physical and emotional health.
Maslow’s Hierarchy of Needs
- Basic Physiological Needs: Nutrition (water and food), elimination (Toileting), airway (suction)-breathing (oxygen)-circulation (pulse, cardiac monitor, blood pressure) (ABCs), sleep , sex, shelter, and exercise.
- Safety and Security: Injury prevention ( side rails , call lights, hand hygiene , isolation , suicide precautions, fall precautions, car seats, helmets, seat belts), fostering a climate of trust and safety ( therapeutic relationship ), patient education (modifiable risk factors for stroke , heart disease).
- Love and Belonging: Foster supportive relationships, methods to avoid social isolation ( bullying ), employ active listening techniques, therapeutic communication , and sexual intimacy.
- Self-Esteem: Acceptance in the community, workforce, personal achievement, sense of control or empowerment, accepting one’s physical appearance or body habitus.
- Self-Actualization: Empowering environment, spiritual growth, ability to recognize the point of view of others, reaching one’s maximum potential.
The client’s health values and beliefs, priorities, resources available, and urgency are factors the nurse must consider when assigning priorities. Involve the client in the process to enhance cooperation.
Step 5: Establishing Client Goals and Desired Outcomes
After assigning priorities for your nursing diagnosis, the nurse and the client set goals for each determined priority. Goals or desired outcomes describe what the nurse hopes to achieve by implementing the nursing interventions derived from the client’s nursing diagnoses. Goals provide direction for planning interventions, serve as criteria for evaluating client progress, enable the client and nurse to determine which problems have been resolved, and help motivate the client and nurse by providing a sense of achievement.
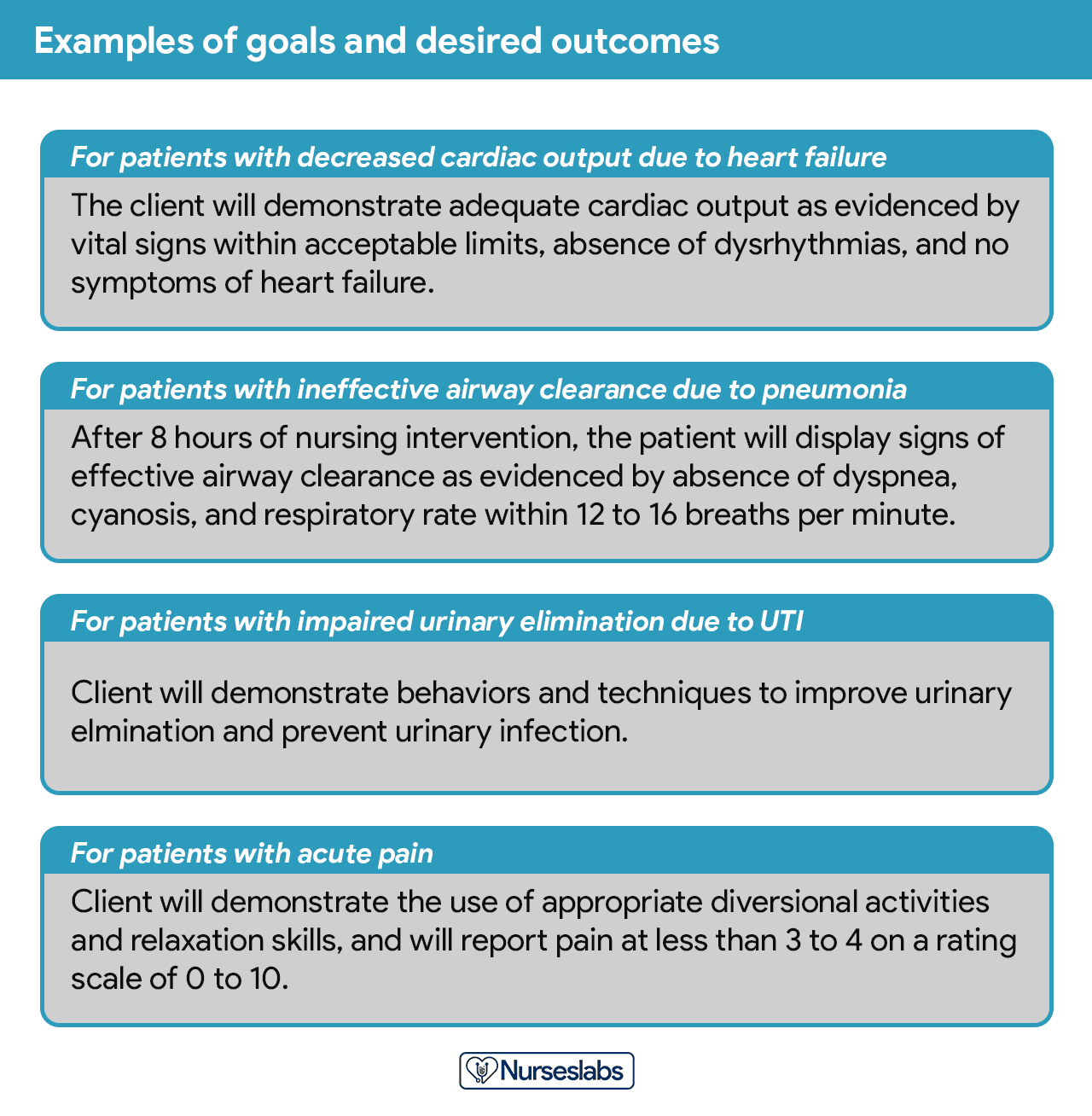
One overall goal is determined for each nursing diagnosis. The terms “ goal outcomes “ and “expected outcome s” are often used interchangeably.
According to Hamilton and Price (2013), goals should be SMART . SMART stands for specific, measurable, attainable, realistic, and time-oriented goals.
- Specific. It should be clear, significant, and sensible for a goal to be effective.
- Measurable or Meaningful. Making sure a goal is measurable makes it easier to monitor progress and know when it reaches the desired result.
- Attainable or Action-Oriented. Goals should be flexible but remain possible.
- Realistic or Results-Oriented. This is important to look forward to effective and successful outcomes by keeping in mind the available resources at hand.
- Timely or Time-Oriented. Every goal needs a designated time parameter, a deadline to focus on, and something to work toward.
Hogston (2011) suggests using the REEPIG standards to ensure that care is of the highest standards. By this means, nursing care plans should be:
- Realistic. Given available resources.
- Explicitly stated. Be clear about precisely what must be done, so there is no room for misinterpretation of instructions.
- Evidence-based. That there is research that supports what is being proposed.
- Prioritized. The most urgent problems are being dealt with first.
- Involve. Involve both the patient and other members of the multidisciplinary team who are going to be involved in implementing the care.
- Goal-centered. That the care planned will meet and achieve the goal set.
Goals and expected outcomes must be measurable and client-centered. Goals are constructed by focusing on problem prevention, resolution, and rehabilitation. Goals can be short-term or long-term . Most goals are short-term in an acute care setting since much of the nurse’s time is spent on the client’s immediate needs. Long-term goals are often used for clients who have chronic health problems or live at home, in nursing homes, or in extended-care facilities.
- Short-term goal . A statement distinguishing a shift in behavior that can be completed immediately, usually within a few hours or days.
- Long-term goal . Indicates an objective to be completed over a longer period, usually weeks or months.
- Discharge planning . Involves naming long-term goals, therefore promoting continued restorative care and problem resolution through home health, physical therapy, or various other referral sources.
Goals or desired outcome statements usually have four components: a subject, a verb, conditions or modifiers, and a criterion of desired performance.
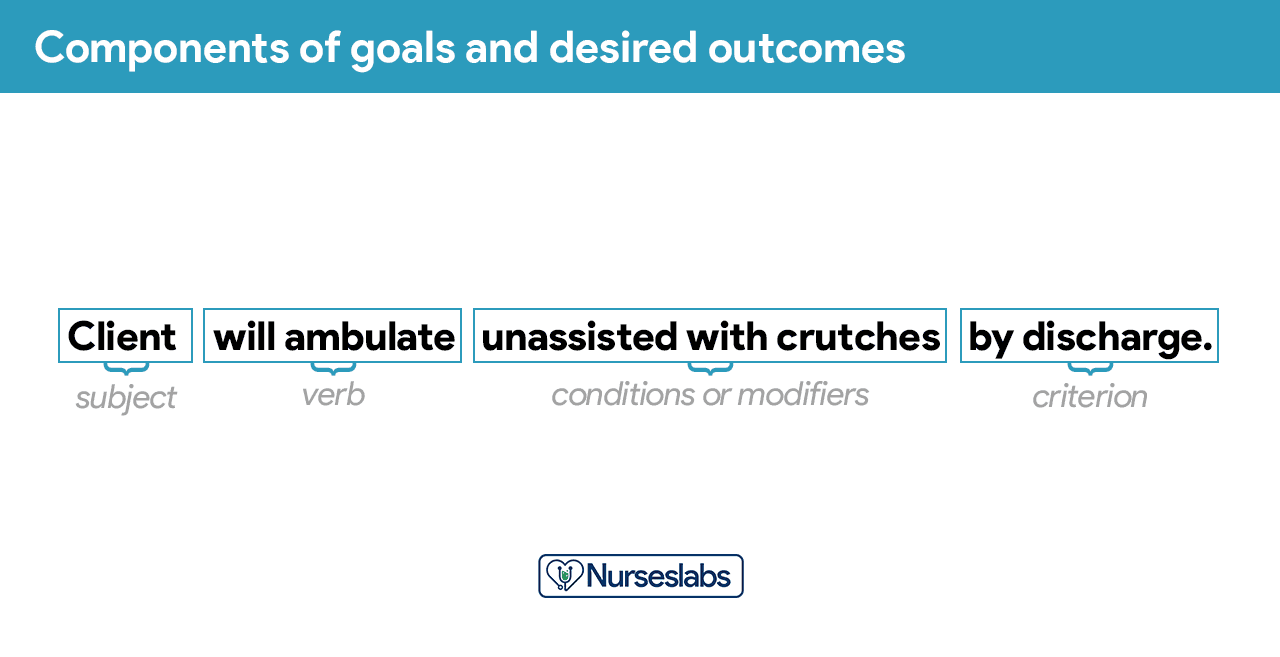
- Subject. The subject is the client, any part of the client, or some attribute of the client (i.e., pulse, temperature, urinary output). That subject is often omitted in writing goals because it is assumed that the subject is the client unless indicated otherwise (family, significant other ).
- Verb. The verb specifies an action the client is to perform, for example, what the client is to do, learn, or experience.
- Conditions or modifiers. These are the “what, when, where, or how” that are added to the verb to explain the circumstances under which the behavior is to be performed.
- Criterion of desired performance. The criterion indicates the standard by which a performance is evaluated or the level at which the client will perform the specified behavior. These are optional.
When writing goals and desired outcomes, the nurse should follow these tips:
- Write goals and outcomes in terms of client responses and not as activities of the nurse. Begin each goal with “Client will […]” help focus the goal on client behavior and responses.
- Avoid writing goals on what the nurse hopes to accomplish, and focus on what the client will do.
- Use observable, measurable terms for outcomes. Avoid using vague words that require interpretation or judgment of the observer.
- Desired outcomes should be realistic for the client’s resources, capabilities, limitations, and on the designated time span of care.
- Ensure that goals are compatible with the therapies of other professionals.
- Ensure that each goal is derived from only one nursing diagnosis. Keeping it this way facilitates evaluation of care by ensuring that planned nursing interventions are clearly related to the diagnosis set.
- Lastly, make sure that the client considers the goals important and values them to ensure cooperation.
Step 6: Selecting Nursing Interventions
Nursing interventions are activities or actions that a nurse performs to achieve client goals. Interventions chosen should focus on eliminating or reducing the etiology of the priority nursing problem or diagnosis. As for risk nursing problems, interventions should focus on reducing the client’s risk factors. In this step, nursing interventions are identified and written during the planning step of the nursing process ; however, they are actually performed during the implementation step.
Nursing interventions can be independent, dependent, or collaborative:
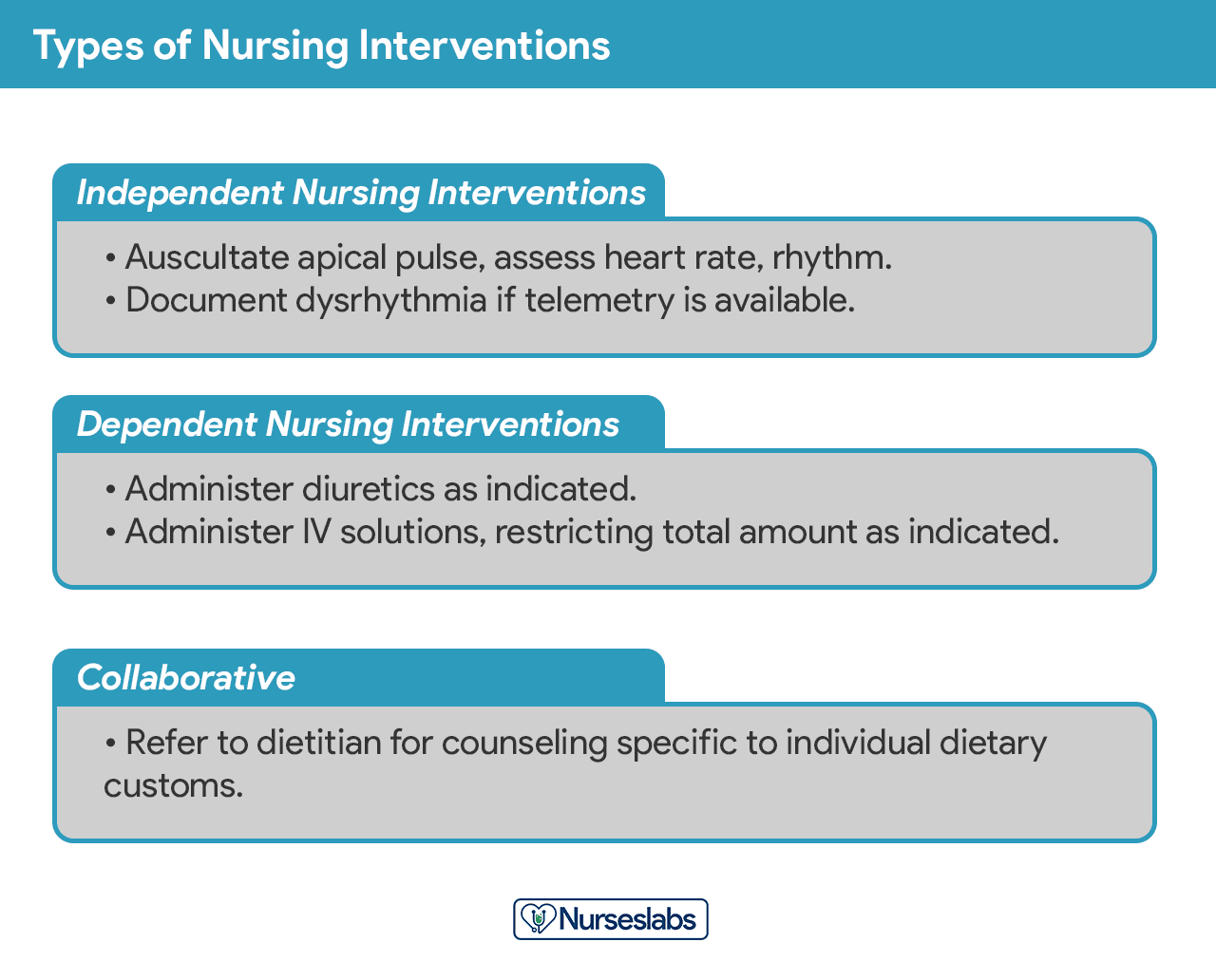
- Independent nursing interventions are activities that nurses are licensed to initiate based on their sound judgement and skills. Includes: ongoing assessment, emotional support, providing comfort, teaching, physical care, and making referrals to other health care professionals.
- Dependent nursing interventions are activities carried out under the physician’s orders or supervision. Includes orders to direct the nurse to provide medications, intravenous therapy , diagnostic tests, treatments, diet, and activity or rest. Assessment and providing explanation while administering medical orders are also part of the dependent nursing interventions.
- Collaborative interventions are actions that the nurse carries out in collaboration with other health team members, such as physicians, social workers, dietitians, and therapists. These actions are developed in consultation with other health care professionals to gain their professional viewpoint.
Nursing interventions should be:
- Safe and appropriate for the client’s age, health, and condition.
- Achievable with the resources and time available.
- Inline with the client’s values, culture, and beliefs.
- Inline with other therapies.
- Based on nursing knowledge and experience or knowledge from relevant sciences.
When writing nursing interventions, follow these tips:
- Write the date and sign the plan. The date the plan is written is essential for evaluation, review, and future planning. The nurse’s signature demonstrates accountability.
- Nursing interventions should be specific and clearly stated, beginning with an action verb indicating what the nurse is expected to do. Action verb starts the intervention and must be precise. Qualifiers of how, when, where, time, frequency, and amount provide the content of the planned activity. For example: “ Educate parents on how to take temperature and notify of any changes,” or “ Assess urine for color, amount, odor, and turbidity.”
- Use only abbreviations accepted by the institution.
Rationales, also known as scientific explanations, explain why the nursing intervention was chosen for the NCP.
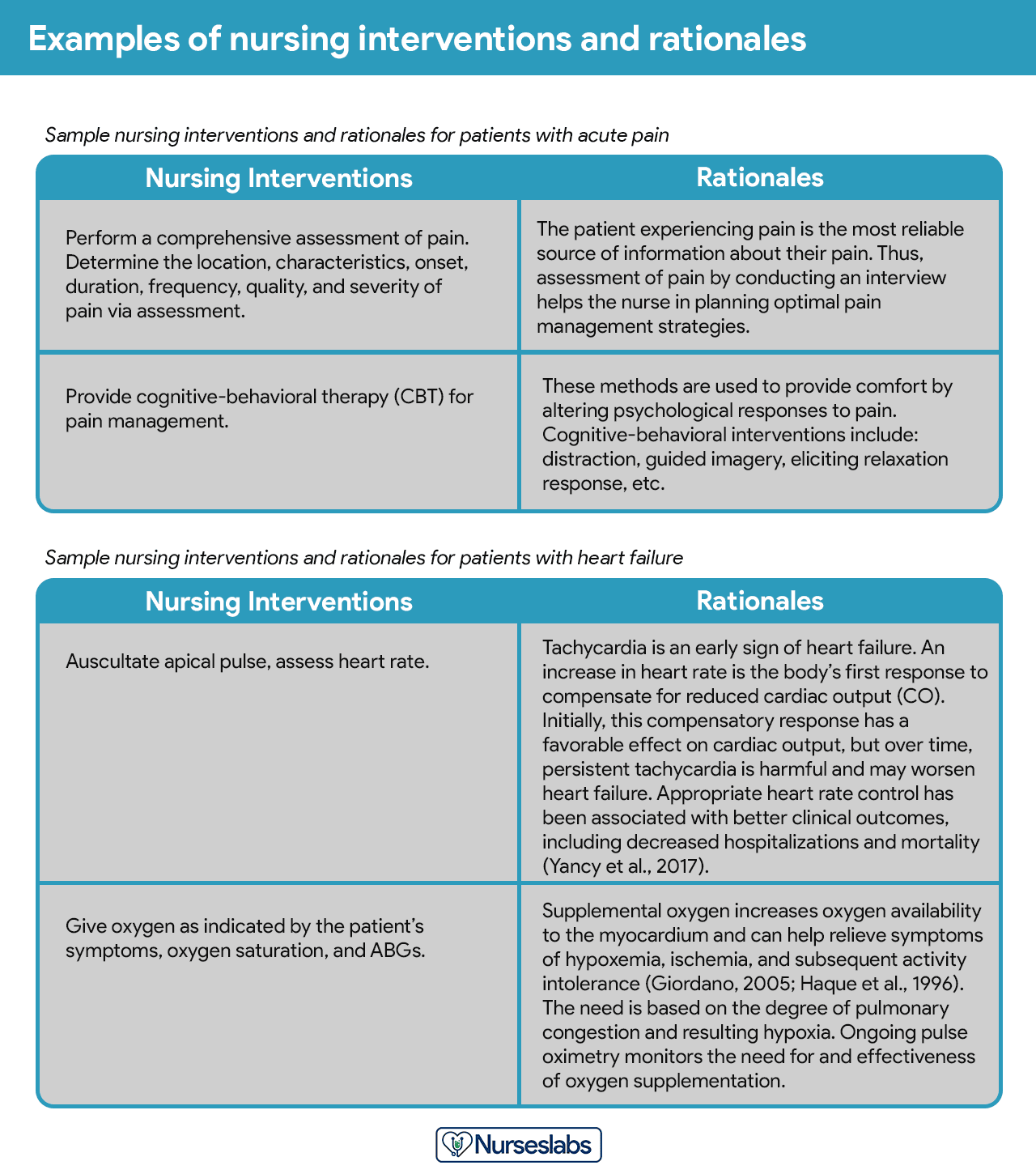
Rationales do not appear in regular care plans. They are included to assist nursing students in associating the pathophysiological and psychological principles with the selected nursing intervention.
Evaluation is a planned, ongoing, purposeful activity in which the client’s progress towards achieving goals or desired outcomes is assessed, and the effectiveness of the nursing care plan (NCP). Evaluation is an essential aspect of the nursing process because the conclusions drawn from this step determine whether the nursing intervention should be terminated, continued, or changed.
The client’s care plan is documented according to hospital policy and becomes part of the client’s permanent medical record, which may be reviewed by the oncoming nurse. Different nursing programs have different care plan formats. Most are designed so that the student systematically proceeds through the interrelated steps of the nursing process , and many use a five-column format.
Nursing Care Plan List
This section lists the sample nursing care plans (NCP) and nursing diagnoses for various diseases and health conditions. They are segmented into categories:
Miscellaneous nursing care plans examples that don’t fit other categories:
Care plans that involve surgical intervention.
Nursing care plans about the different diseases of the cardiovascular system :
Nursing care plans (NCP) related to the endocrine system and metabolism:
Care plans (NCP) covering the disorders of the gastrointestinal and digestive system :
Care plans related to the hematologic and lymphatic system :
NCPs for communicable and infectious diseases:
All about disorders and conditions affecting the integumentary system :
Nursing care plans about the care of the pregnant mother and her infant. See care plans for maternity and obstetric nursing:
Care plans for mental health and psychiatric nursing:
Care plans related to the musculoskeletal system:
Nursing care plans (NCP) for related to nervous system disorders:
Care plans relating to eye disorders:
Nursing care plans (NCP) for pediatric conditions and diseases:
Care plans related to the reproductive and sexual function disorders:
Care plans for respiratory system disorders:
Care plans related to the kidney and urinary system disorders:
Recommended nursing diagnosis and nursing care plan books and resources.
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care We love this book because of its evidence-based approach to nursing interventions. This care plan handbook uses an easy, three-step system to guide you through client assessment, nursing diagnosis, and care planning. Includes step-by-step instructions showing how to implement care and evaluate outcomes, and help you build skills in diagnostic reasoning and critical thinking.

Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition) Includes over two hundred care plans that reflect the most recent evidence-based guidelines. New to this edition are ICNP diagnoses, care plans on LGBTQ health issues, and on electrolytes and acid-base balance.

Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales Quick-reference tool includes all you need to identify the correct diagnoses for efficient patient care planning. The sixteenth edition includes the most recent nursing diagnoses and interventions and an alphabetized listing of nursing diagnoses covering more than 400 disorders.

Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care Identify interventions to plan, individualize, and document care for more than 800 diseases and disorders. Only in the Nursing Diagnosis Manual will you find for each diagnosis subjectively and objectively – sample clinical applications, prioritized action/interventions with rationales – a documentation section, and much more!

All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health Includes over 100 care plans for medical-surgical, maternity/OB, pediatrics, and psychiatric and mental health. Interprofessional “patient problems” focus familiarizes you with how to speak to patients.

Recommended reading materials and sources for this NCP guide:
- Björvell, C., Thorell-Ekstrand, I., & Wredling, R. (2000). Development of an audit instrument for nursing care plans in the patient record. BMJ Quality & Safety , 9 (1), 6-13. [ Link ]
- DeLaune, S. C., & Ladner, P. K. (2011). Fundamentals of nursing: Standards and practice . Cengage learning.
- Freitas, F. A., & Leonard, L. J. (2011). Maslow’s hierarchy of needs and student academic success . Teaching and learning in Nursing , 6 (1), 9-13.
- Hamilton, P., & Price, T. (2007). The nursing process, holistic. Foundations of Nursing Practice E-Book: Fundamentals of Holistic Care , 349.
- Lee, T. T. (2004). Evaluation of computerized nursing care plan: instrument development . Journal of Professional Nursing , 20 (4), 230-238.
- Lee, T. T. (2006). Nurses’ perceptions of their documentation experiences in a computerized nursing care planning system . Journal of Clinical Nursing , 15 (11), 1376-1382.
- Rn, B. O. C., Rn, H. M., Rn, D. T., & Rn, F. E. (2000). Documenting and communicating patient care: Are nursing care plans redundant?. International Journal of Nursing Practice , 6 (5), 276-280.
- Stonehouse, D. (2017). Understanding the nursing process . British Journal of Healthcare Assistants , 11 (8), 388-391.
- Yildirim, B., & Ozkahraman, S. (2011). Critical thinking in nursing process and education . International journal of humanities and social science , 1 (13), 257-262.
65 thoughts on “Nursing Care Plans (NCP): Ultimate Guide and List”
This page is helpful!
Thank you! Hope we’ve helped you write better nursing care plans!
Will definitely use this site to help write care plans. How should I cite this link when using APA format. Thank You
HI Can some one help me to do assignment on Impaired renal perfusion. 1.Goal 2.Related Action 3.Rational 4.Evaluate outcome
Wow God bless plenty Nurseslabs really relieve my burdens 😊😊
Thank you for all this useful info! I have been looking for something like this online.
You’re welcome! :)
Quite educative thank you
The notes were indeed useful
I hope to learn more and improve my skills towards nursing
Thank you so so much! This website is of great assistance to me. God bless you.
It’s so great for nursing student
Very beautiful ,Good work keep it up
Nice work. Well done
Very helpful
Great job,thank you
Thanks so much , it’s of much support for students .
Risk for ineffective thermoregulation would be a good one for you to do next for newborn.
Hi, i have learnt a lot THANK YOU. i would kindly like to learn more on paper 1 since am yet to sit for my nursing council exams and feel challenged on the paper.please do assist me thank you.
This site is a total lifesaver!
What is a nursing care plan a mother in second stage of labour?
Please see: 36 Labor Stages, Induced and Augmented Labor Nursing Care Plans
What is the nursing care plan for pulmonary oedema?
I m interest in receiving a blank nursing care plan template for my students to type on. I was wondering if it was available and if so can you please direct me on where to find it?
Hi! You can download it here: Nursing Care Plan Template
I love this website!!! Is there a textbook version of the Nurseslabs that I can purchase??
Thank you Nurseslabs. This is a wonderful note you’ve prepared for all nurses. I would like a pdf of this. Thanks.
I wish I had had this resource when i was in nursing school 2008!!
Yeah! It’s nice
Thanks for this information!
God bless you sis…Thank you for all this useful info!
This is the kind of step-by-step guidance that I needed. Thank you!
Thank you. I have learned a lot!
Wow! This is a hidden treasure!
Thanks a lot for this, it is really helpful!
Hi Matt! I would like to purchase a textbook of your nursing care plan. Where I can purchase pls help!
Hi Criselda,
Sorry, we don’t have a textbook. All of our resources are here on the website and free to use.
Good day, I would like to know how can I use your website to help students with care plans.
Sincerely, Oscar A. Acosta DNP, RN
Oh I love your works. Your explanations
I’m glad I’ve met your website. It helps me a lot. Thank you
I love this, so helpful.
These care plans are great for using as a template. I don’t have to reinvent the wheel, and the information you provided will ensure that I include the important data without leaving things out. Thanks a million!
Hi, I have learnt a lot, this is a wonderful note you’ve prepared for all nurses thank you.
Matt, this page is very informative and I especially appreciate seeing care plans for patients with neurological disorders. I notice, though, that traumatic brain injury is not on your list. Might you add a care plan page for this?
Thanks alot I had gained much since these are detailed notes 🙏🙏
OMG, this is amazing!
Wow very helpful.thank you very much🙏🙏
Hi, is there a downloadable version of this, pdf or other files maybe this is awesome!
Hi Paul, on your browser go to File > Print > Save as PDF. Hope that helps and thanks for visiting Nurseslabs!
Matt, I’m a nursing instructor looking for tools to teach this. I am interested in where we can find “rules” for establishing “related to” sections…for example –not able to utilize medical diagnosis as a “related to” etc. Also, resources for nursing rationale.
Hello, please check out our guide on how to write nursing diagnoses here: https://nurseslabs.com/nursing-diagnosis/
Nursing care plan is very amazing
Thanks for your time. Nursing Care Plan looks great and helpful!
complete knowledge i get from here
great resource. puts it all together. Thank for making it free for all
Hello Ujunwa, Thanks a lot for the positive vibes! 🌟 It’s super important to us that everyone has access to quality resources. Just wondering, is there any specific topic or area you’d love to see more about? We’re always looking to improve and add value!
Great work.
Hi Abbas, Thank you so much! Really glad to hear you found the nursing care plans guide useful. If there’s a specific area or topic you’re keen on exploring more, or if you have any suggestions for improvement, feel free to share. Always aiming to make our resources as helpful as possible!
It has been good time me to use these nursing guides.
What is ncp for acute pain
For everything you need to know about managing acute pain, including a detailed nursing care plan (NCP), definitely check out our acute pain nursing care plan guide . It’s packed with insights on assessment, interventions, and patient education to effectively manage and alleviate acute pain.
Good morning. I love this website
Leave a Comment Cancel reply
Nursing Care Plans Explained
NurseJournal.org is committed to delivering content that is objective and actionable. To that end, we have built a network of industry professionals across higher education to review our content and ensure we are providing the most helpful information to our readers.
Drawing on their firsthand industry expertise, our Integrity Network members serve as an additional step in our editing process, helping us confirm our content is accurate and up to date. These contributors:
- Suggest changes to inaccurate or misleading information.
- Provide specific, corrective feedback.
- Identify critical information that writers may have missed.
Integrity Network members typically work full time in their industry profession and review content for NurseJournal.org as a side project. All Integrity Network members are paid members of the Red Ventures Education Integrity Network.
Explore our full list of Integrity Network members.

This page can help you understand nursing care plans, how they improve nursing team communication and patient care, and how to develop nursing care plans for your patients. Nursing care plans are individualized and ensure consistency for nursing care of the patient, document patient needs and potential risks, and help patients and nurses work collaboratively toward optimal outcomes.
What Is a Nursing Care Plan?
Nursing care plans are a vital part of the nursing process. They provide a centralized document of the patient’s condition, diagnosis, the nursing team’s goals for that patient, and measure of the patient’s progress. Nursing care plans are structured to capture all the important information for the nursing team in one place.
Because they centralize this information and updates, they ensure that everything important is documented and available to all team members. This also makes patient education easier, since all nursing staff members know and can reinforce what the patient needs to learn.
Without nursing care plans, communication can become disjointed, patient information might be scattered across different patient records and databases, or nursing staff might have to rely on verbal handoffs that the new nurse may mishear or even forget if they are dealing with multiple crises at once.
Developing a Nursing Care Plan
Nursing care plans include the initial patient assessment and diagnosis, the desired outcomes and how to achieve them, and an evaluation of the patient’s results. While the names of the individual parts may vary from organization to organization (for example, “implementation” in one plan might be called “intervention” in another), all nursing care plans include these fundamental components.
Many, but not all, nursing care plans include rationales, the reasons for an intervention, while others require them only if there is some reason not to provide the standard intervention.
Nursing plans should be holistic and take account of nonclinical needs where possible, such as preferences for chaplain services or other ways to support the patient’s mental well-being.
Patient Assessment
Patient assessment includes a thorough evaluation of subjective and objective symptoms and vital signs. Nurses are responsible for collecting and maintaining this data, although certified nursing assistants may help collect vital signs.
Nursing Diagnoses
A nursing diagnosis is created by a nurse based on the subjective and objective data collected during the patient assessment. This is separate from a medical diagnosis which must be provided by a physician or nurse practitioner. Nurses select standardized diagnoses approved by the North American Nursing Diagnosis Association (NANDA) that are relevant to the patient’s condition, symptoms, and risks.
Anticipated Outcomes/Goals
This section describes the goals for the patient, usually both short-term goals, such as reduction of pain or improvement in symptoms or vital signs, as well as long-term goals, such as recovery within a certain time frame. The goals are directly related to the nursing diagnosis.
Implementation
Implementation describes how the nursing team can work to achieve these goals. Specific nursing interventions are planned based on the goals. This section also documents what nursing-specific care the nursing team has performed for the patient.
This section describes how well the patient’s condition responded to the nursing interventions or, in other words, how the goals were or were not met. If the goals were not met, the nurse revises the plan. If the goals were met, the nurse may decide to add more goals and interventions.
Popular Online RN-to-BSN Programs
Learn about start dates, transferring credits, availability of financial aid, and more by contacting the universities below.
Nursing Care Plan Do’s and Don’ts
While nursing care plans are created to document the care you are providing for your patient, there are “Do’s and Don’ts” to writing an effective care plan. Here are a few:
Using a Nursing Care Plan
In addition to centralizing information, nursing care plans are one of the most effective tools for nurses to uphold the nursing code of ethics and to document that they did so in case of lawsuits or accusations of failure to adhere to care standards. This is one of the many reasons for all nurses and nursing assistants to understand and update each patient’s nursing care plan when necessary.
Unlike most electronic health records systems, nursing care plans are designed to address the patient’s holistic needs which helps provide a better patient experience. When all members of a care team have access to all the information about a patient’s needs and preference, everyone stays on the same page.
Many organizations have their own preferred formats for nursing care plans, but if you are looking for models to update your existing nursing care plan or implement a new one, you can find samples and templates from Craig Hospital and Nursing Home Help .
Page last reviewed July 26, 2021
You might be interested in

11 Great Nursing Careers in a Patient Care Setting
There are many great opportunities for patient-focused nursing care that are unique and not often considered by new graduates.

The 20 Best Nursing Career Specialties Based On Salary
Interested in nursing, but unsure which career track is best for you? This guide describes the 20 best nursing career specialties and how to get started in these fields.

Primary Care Nurse Practitioner Career Overview
Learn more about primary care nurse practitioners, how to become one, and the important role they play in delivering quality healthcare.

How to Write a Nursing Case Study Paper (A Guide)

Most nursing students dread writing a nursing case study analysis paper, yet it is a mandatory assignment; call it a rite of passage in nursing school. This is because it is a somewhat tricky process that is often overwhelming for nursing students. Nevertheless, by reading this guide prepared by our best nursing students, you should be able to easily and quickly write a nursing case study that can get you an excellent grade.
How different is this guide from similar guides all over the internet? Very different!
This guide provides all the pieces of information that one would need to write an A-grade nursing case study. These include the format for a nursing case study, a step-by-step guide on how to write a nursing case study, and all the important tips to follow when writing a nursing case study.
This comprehensive guide was developed by the top nursing essay writers at NurseMyGrade, so you can trust that the information herein is a gem that will catapult your grades to the next level. Expect updates as we unravel further information about writing a nursing case study.
Now that you know you’ve discovered a gold mine , let’s get right into it.
What Is a Nursing Case Study?
A nursing case study is a natural or imagined patient scenario designed to test the knowledge and skills of student nurses. Nursing case study assignments usually focus on testing knowledge and skills in areas of nursing study related to daily nursing practice.
As a nursing student, you must expect a nursing case study assignment at some point in your academic life. The fact that you are reading this post means that point is now.
While there is no standard structure for writing a nursing case study assignment, some things or elements must be present in your nursing assignment for your professor to consider it complete.
In the next section, you will discover what your instructor n expects in your nursing case study analysis. Remember, these are assignments where you are given a case study and are expected to write a case analysis report explaining how to handle such scenarios in real-life settings.
The Nursing Case Study Template
The typical nursing case study has nine sections. These are:
- Introduction
- Case presentation (Patient info, history, and medical condition)
- Diagnosis/Nursing assessment
- Intervention/Nursing care plan
- Discussion and recommendations
The Structure of a Nursing Case Study Analysis
You now know what nursing professors expect in a nursing case study analysis. In this section, we will explain what to include in each section of your nursing case study analysis to make it an excellent one.
1. Title page
The title page is essential in all types of academic writing. You must include it in your nursing case study analysis or any other essay or paper. And you must include it in the format recommended by your college.
If your college has no specific title page format, use the title page format of the style requested in the assignment prompt. In nursing college, virtually all assignments should be written in Harvard or APA format .
So, check your assignment prompt and create your title page correctly. The typical title page should include the topic of your paper, your name, the name of your professor, the course name, the date you are submitting the paper, and the name of your college.
2. Abstract
Most nursing professors require you to include an abstract in your nursing case study analysis. And even when you are not explicitly required to write one, it is good to do so. Of course, you should consult with your professor before doing so.
When writing an abstract for your paper, make sure it is about 200 words long. The abstract should include a brief summary of the case study, including all the essential information in the patient presentation, such as the history, age, and current diagnosis.
The summary should also include the nursing assessment, the current interventions, and recommendations.
3. Introduction
After writing the title page and the abstract, start writing the introduction. The introduction of a nursing case study analysis must briefly include the patient’s presentation, current diagnosis and medication, and recommendations. It must also include a strong thesis statement that shows what the paper is all about.
You shouldn’t just write an introduction for the sake of it. If you do so, your introduction will be bland. You need to put in good effort when writing your introduction. The best way to do this is to use your introduction to show you understand the case study perfectly and that you will analyze it right.
You can always write your introduction last. Many students do this because they believe writing an introduction last makes it more precise and accurate.
4. Case Presentation (Status of the Patient)
After introducing your nursing case study analysis, you should present the case where you outline the patient's status. It is usually straightforward to present a case.
You must paraphrase the patient scenario in the assignment prompt or brief. Focus on the demographic data of the patient (who they are, age, race, height, skin tone, occupation, relationships, marital status, appearance, etc.), why they are in the case study or scenario, reasons they sought medical attention, chief complaint, and current diagnosis and treatment. You should also discuss the actions performed on the patient, such as admission to the ICU, taking vital signs, recommending tests, etc.
In short, everything necessary in the patient scenario should be in your case presentation. You only need to avoid copying the patient scenario or case study word-for-word when writing your case presentation.
5. Diagnosis and Assessment
After the case presentation, you should explain the diagnosis. In other words, you should explain the condition, disease, or medical situation highlighted in the case presentation. For example, if the patient is a heavy smoker and he has COPD, it is at this point that you explain how COPD is linked to heavy smoking.
This is the section where you thoroughly discuss the disease process (pathophysiology) by highlighting the causes, symptoms, observations, and treatment methods. You should relate these to the patient’s status and give concrete evidence. You should describe the progression of the disease from when the client was admitted to a few hours or days after they were stabilized. Consider the first indication of the disease that prompted the patient to seek further medical assistance.
Your paper should also elucidate the diagnostic tests that should be conducted and the differential diagnosis. Ensure that each is given a well-founded rationale.
When explaining the condition, go deep into the pathophysiology. Focus specifically on the patient’s risk factors. Ensure you get your explanation from recent nursing literature (peer-reviewed scholarly journals published in the last 5 years). And do not forget to cite all the literature you get your facts from.
In short, this section should explain the patient’s condition or suffering.
6. Nursing Intervention
After the diagnosis and nursing assessment section, your nursing case study analysis should have an intervention section. This section is also known as the nursing care planning section. What you are supposed to do in this section is to present a nursing care plan for the patient presented in the patient scenario. You should describe the nursing care plan and goals for the patient. Record all the anticipated positive changes and assess whether the care plan addresses the patient's condition.
A good nursing care plan details the patient’s chief complaints or critical problems. It then describes the causes of these problems using evidence from recent medical or nursing literature. It then details the potential intervention for each problem. Lastly, it includes goals and evaluation strategies for the measures. Most professors, predominantly Australian and UK professors, prefer if this section is in table format.
Some nursing professors regard the intervention section (or nursing care plan section) as the most critical part of a nursing case study. This is because this part details precisely how the student nurse will react to the patient scenario (which is what the nursing professors want to know). So, ensure you make a reasonable effort when developing this section to get an excellent grade.
7. Discussion and Recommendations
The intervention section in a nursing case study is followed by a discussion and recommendations section. In this section, you are supposed to expound on the patient scenario, the diagnosis, and the nursing care plan. You should also expound on the potential outcomes if the care plan is followed correctly. The discussion should also explain the rationale for the care plan or its significant bits.
Recommendations should follow the discussion. Recommendations usually involve everything necessary that can be done or changed to manage a patient’s condition or prevent its reoccurrence. Anything that enhances the patient’s well-being can be a recommendation. Just make sure your key recommendations are supported by evidence.
8. Conclusion
This is the second last section of a typical nursing case study. What you need here is to summarize the entire case study. Ensure your summary has at least the case presentation, the nursing assessment/diagnosis, the intervention, and the key recommendations.
At the very end of your conclusion, add a closing statement. The statement should wrap up the whole thing nicely. Try to make it as impressive as possible.
9. References
This is the last section of a nursing case study. No nursing case study is complete without a references section. You should ensure your case study has in-text citations and a references page.
And you should make sure both are written as recommended in the assignment. The style section is usually Harvard or APA. Follow the recommended style to get a good grade on your essay.
Step-By-Step Guide to Writing a Nursing Case Study
You know all the key sections you must include in a nursing case study. You also know what exactly you need to do in each section. It is time to learn how to write a nursing case study. The process detailed below should be easy to follow because you know the typical nursing case study structure.
1. Understand the Assignment
When given a nursing case study assignment, the first thing you need to do is to read. You need to read two pieces of information slowly and carefully.
First, you need to read the prompt itself slowly and carefully. This is important because the prompt will have essential bits of information you need to know, including the style, the format, the word count, and the number of references needed. All these bits of information are essential to ensure your writing is correct.
Second, you need to read the patient scenario slowly and carefully. You should do this to understand it clearly so that you do not make any mistakes in your analysis.
2. Create a Rough Outline
Failure to plan is a plan to fail. That is not what you are in it for anyway! In other words, do not fail to create an outline for your case study analysis. Use the template provided in this essay to create a rough outline for your nursing case study analysis.
Ensure your outline is as detailed as it can be at this stage. You can do light research to achieve this aim. However, this is not exactly necessary because this is just a rough outline.
3. Conduct thorough research
After creating a rough outline, you should conduct thorough research. Your research should especially focus on providing a credible and evidence-based nursing assessment of the patient problem(s). You should only use evidence from recent nursing or medical literature.
You must also conduct thorough research to develop an effective intervention or nursing care plan. So when researching the patient’s problem and its diagnosis, you should also research the most suitable intervention or do it right after.
When conducting research, you should always note down your sources. So for every piece of information you find, and what to use, you should have its reference.
After conducting thorough research, you should enhance your rough outline using the new information you have discovered. Make sure it is as comprehensive as possible.
4. Write your nursing case study
You must follow your comprehensive outline to write your case study analysis at this stage. If you created a good outline, you should find it very easy to write your nursing case study analysis.
If you did not, writing your nursing case study will be challenging. Whenever you are stuck writing your case study analysis paper, you should re-read the part where we explain what to include in every section of your analysis. Doing so will help you know what to write to continue your essay. Writing a nursing case study analysis usually takes only a few hours.
5. Reference your case study
After writing your case study, ensure you add all in-text citations if you have not already. And when adding them, you should follow the style/format recommended in the assignment prompt (usually APA or Harvard style).
After adding in-text citations exactly where they need to be and in the correct format, add all the references you have used in a references page. And you should add them correctly as per the rules of the style you were asked to use.
Do not forget to organize your references alphabetically after creating your references page.
6. Thoroughly edit your case study
After STEP 5 above, you need to edit your case study. You should edit it slowly and carefully. Do this by proofreading it twice. Proofread it slowly each time to discover all the grammar, style, and punctuation errors. Remove all the errors you find.
After proofreading your essay twice, recheck it to ensure every sentence is straightforward. This will transform your ordinary case study into an A-grade one. Of course, it must also have all the standard sections expected in a case study.
Recheck your case study using a grammarly.com or a similar computer grammar checker to ensure it is perfect. Doing this will help you catch and eliminate all the remaining errors in your work.
7. Submit your case study analysis
After proofreading and editing your case study analysis, it will be 100% ready for submission. Just convert it into the format it is required in and submit it.
Nursing Case Study Tips and Tricks
The guide above and other information in this article should help you develop a good nursing case study analysis. Note that this guide focuses entirely on nursing case scenario-based papers, not research study-based nursing case studies. The tips and tricks in this section should help you ensure that the nursing case study analysis you create is excellent.
1. Begin early
The moment you see a nursing case study assignment prompt, identify a date to start writing it and create your own deadline to beat before the deadline stated in the prompt.
Do this and start writing your case study analysis early before your deadline. You will have plenty of time to do excellent research, develop an excellent paper, and edit your final paper as thoroughly as you want.
Most student nurses combine work and study. Therefore, if you decide to leave a nursing case study assignment until late to complete it, something could come up, and you could end up failing to submit it or submitting a rushed case study analysis.
2. Use the proper terminology
When writing an essay or any other academic paper, you are always encouraged to use the most straightforward language to make your work easy to understand. However, this is not true when writing a nursing case study analysis. While your work should certainly be easy to understand, you must use the right nursing terminology at every point where it is necessary. Failure to do this could damage your work or make it look less professional or convincing.
3. Avoid copying and pasting
If you are a serious nursing student, you know that copying and pasting are prohibited in assignments. However, sometimes copying and pasting can seem okay in nursing case studies. For example, it can seem okay to copy-paste the patient presentation. However, this is not okay. You are supposed to paraphrase the verbatim when presenting the patient presentation in your essay. You should also avoid copy-pasting information or texts directly. Every fact or evidence you research and find should be paraphrased to appear in your work. And it should be cited correctly.
4. Always ask for help if stuck
This is very important. Students are usually overwhelmed with academic work, especially a month or two to the end of the semester. If you are overwhelmed and think you will not have the time to complete your nursing case study analysis or submit a quality one, ask for help. Ask for help from a nursing assignment-help website like ours, and you will soon have a paper ready that you can use as you please. If you choose to get help from us, you will get a well-researched, well-planned, well-developed, and fully edited nursing case study.
5. Format your paper correctly
Many students forget to do proper formatting after writing their nursing case study analyses. Before you submit your paper, make sure you format it correctly. If you do not format your paper correctly, you will lose marks because of poor formatting. If you feel you are not very confident with your APA or Harvard formatting skills, send your paper to us to get it correctly formatted and ready for submission.
Now that you are all set up …
Our company has been among the best-rated nursing homework help companies in the last few years. Thousands of students have benefitted from our many academic writing guides. Many more have benefitted from direct help given by our experts.
- How to write a nursing philosophy statement.
- Writing an abstract poster presentation.
We have experienced nursing experts available every day of the week to provide nursing assignment help. They can easily research and write virtually any nursing assignment, including a nursing case study. So, if the information provided in this article isn’t making you feel any optimistic about writing an excellent nursing case study, get help from us.
Get help by ordering a custom nursing case study through this very website. If you do so, you will get a 100% original paper that is well-researched, well-written, well-formatted, and adequately referenced. Since the paper is original, you can use it anywhere without problems.
Thousands of students trust our company every week, month, and year. Be like them! Trust us for 100% confidentiality and speedy delivery.
Struggling with
Related Articles
Nursing Student's Ultimate Guide to Writing a Nursing Care Plan

Nursing Topics for Research plus Ideas

Writing Nursing Dissertations, Theses, & Scholarly Projects (Step-by-Step Guide)
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
The Ultimate Guide to Nursing Care Plans
What is a nursing care plan, types of nursing care plans.
- Nursing Care Plan Components
How to Write a Nursing Care Plan
Sample nursing care plans.

If you aspire to become a nurse, you'll want to familiarize yourself with what nursing care plans (NCPs) are all about. Nursing care plans provide a means of communication among nurses, their patients, and other healthcare providers to achieve healthcare outcomes.
A nursing care plan contains relevant information about a patient’s diagnosis, the goals of treatment, the specific nursing orders (including what observations are needed and what actions must be performed), and an evaluation plan.
Over the course of the patient’s stay, the plan is updated with any changes and new information as it presents itself. In fact, most hospitals require nurses to update the care plan during and after each shift.
Get 10% OFF Nursing School Study Guides From nurseinthemaking.com ! Fill out the form to get your exclusive discount.
What is the Purpose of a Nursing Care Plan?
Nursing care plans help define nursing guidelines and some treatment guidelines (as ordered) for a specific patient.
Essentially, it is a plan of action. It helps guide nurses throughout their shift in caring for the patient. It also allows nurses to provide attentive and focused care.
>> Show Me Online RN-to-BSN Programs
There are four main types of nursing care plans.
- Informal - A care plan that exists in the nurse’s mind and is actions the nurse wishes to accomplish during their shift.
- Formal - This is a written or computerized plan that organizes and coordinates the patient’s care information and plan.
- Standardized - Nursing care for groups of patients with everyday needs.
- Individualized - A care plan tailored to the specific needs of the patient.
What are the Components of a Nursing Care Plan?
Nursing care plans follow a five-step process:
- Expected outcomes
- Interventions
- Rationale and Evaluation
>> Related: The Nursing Process Explained
When writing a nursing care plan, you first have to determine what type of care plan you are interested in. If it is for your own use throughout the shift, then an informal one may be beneficial; however, if it is for the patient’s chart and required during your shift then an individualized care plan is the way to go.
Get 5 FREE study guides from Simplenursing.com - fill out the form for instant access! 1. Fluid & Electrolytes study guide 2. EKG Rhythms study guide 3. Congestive Heart Failure study guide 4. Lab Values study guide 5. Metabolic Acidosis & Alkalosis study guide

By clicking download, you agree to receive email newsletters and special offers from Nurse.org & Simplenursing.com. You may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.
Your request has been received. Thanks!
Step 1: Assessment
The first step in writing an organized care plan includes gathering subjective and objective nursing data . This information can come from,
- Verbal statements from patient and family
- Vital signs
- Physical complaints
- Body conditions
- Medical history
- Height and weight
- Intake and output
Step 2: Diagnosis
Using the information and data collected in Step 1, a nursing diagnosis is chosen that best fits the patient, the goals, and objectives for the patient’s hospitalization.
According to North American Nursing Diagnosis Association (NANDA), defines a nursing diagnosis as “a clinical judgment about the human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group or community.”
A nursing diagnosis is based on Maslow’s Hierarchy of Needs pyramid and helps prioritize treatments. Based on the nursing diagnosis chosen, the goals to resolve the patient’s problems through nursing implementations are determined in the next step.
Step 3: Outcomes and Planning
After determining the nursing diagnosis, it is time to create a SMART goal based on evidence-based practices. SMART goals stands for Specific, Measurable, Achievable, Relevant, and Time-Bound . It is important to consider the patient’s medical diagnosis, overall condition, and all of the data collected.
It is also during this time you will consider goals for the patient and outcomes for the short and long term. These goals must be realistic and desired by the patient. For example, if a goal is for the patient to seek counseling for alcohol dependency during the hospitalization but the patient is currently detoxing and having mental distress - this might not be a realistic goal.
Step 4: Implementation
Now that the goals have been set, you must put the actions into effect to help the patient achieve the goals. While some of the actions will show immediate results (ex. giving a patient with constipation a suppository to elicit a bowel movement) others might not be seen until later on in the hospitalization.
The implementation phase means performing the nursing interventions outlined in the care plan. Interventions are classified into seven categories:
- Physiological
- Complex physiological
- Health system interventions
Some interventions will be patient or diagnosis-specific, but there are several that are completed each shift for every patient:
- Pain assessment
- Position changes
- Fall prevention
- Providing cluster care
- Infection control
Step 5: Evaluation
The fifth and final step of the nursing care plan is the evaluation phase. This is when you evaluate if the desired outcome has been met during the shift. There are three possible outcomes,
Based on the evaluation, it can determine if the goals and interventions need to be altered.
Nursing Diagnosis: Ineffective breathing pattern related to right pulmonary agenesis as evidenced by high carbon dioxide levels and absent breath sounds on right side of the chest.
Assessment:
- Vital signs: Monitor the patient’s heart rate, respiratory rate and SpO2 levels. Signs of respiratory distress include tachypnea, dyspnea and an SpO2 <95%.
- Breathing patterns: If the patient shows signs of respiratory distress, it should alarm the nurse, and interventions should take place. Signs of respiratory distress include nasal flaring, accessory muscles, grunting, shortness of breath, and retractions.
- CO2 lab values: When the body has an ineffective breathing pattern, inadequate gas exchange will take place. During this, the body retains CO2 and can enter into a stage of respiratory acidosis. Monitor for respiratory acidosis with blood gas lab values.
- Skin assessment: A person experiencing respiratory distress may experience pallor, cyanotic, and/or mottled skin.
SMART Goal: The patient will maintain a SpO2 level of >95%, RR of 30 to 55 breaths per minute, and heart rate of 80 to 140 beats per minute until the end of the shift.
Interventions:
- Check manual heart rate and respiratory rate every four hours.
- Check patient is on continuous SpO2 monitor with pulse oximetry on the same extremity throughout shift.
- Obtain blood gases as ordered.
- Monitor for signs and symptoms of increased work of breathing and respiratory distress.
- The patient is observed and/or documented to have SpO2, HR, and RR all within normal limits by end of the shift.
- The patient is documented to have received blood gas results that contain a CO2 value that is within the normal range.
- The patient is observed and documented to not experience any symptoms of respiratory distress throughout the shift.
Find Nursing Programs
Nursing care plan faqs, how do you write a nursing care plan.
- Writing a nursing care plan takes time and practice. It is something you will learn during nursing school and will continue to use throughout your nursing career. First, you must complete an assessment of your patient to determine the nursing diagnosis and include relevant patient information. Next, utilize a NANDA-approved diagnosis and determine expected and projected outcomes for the patient. Finally, implement the interventions and determine if the outcome was met.
What is the purpose of the nursing care plan?
- Nursing care plans provide a means of communication among nurses, their patients, and other healthcare providers to achieve healthcare outcomes.
What are the 5 main components of a care plan?
- There are five main components to a nursing care plan including; assessment, diagnosis, expected outcomes, interventions, and rationale/evaluation.
What is included in a nursing care plan?
- Nursing care plans include relevant information about the patient’s assessment, goals of treatment, interventions that need to occur, and observations. These observations may include subjective and objective data.
*This website is provided for educational and informational purposes only and does not constitute providing medical advice or professional services. The information provided should not be used for diagnosing or treating a health problem or disease.

Kathleen Gaines (nee Colduvell) is a nationally published writer turned Pediatric ICU nurse from Philadelphia with over 13 years of ICU experience. She has an extensive ICU background having formerly worked in the CICU and NICU at several major hospitals in the Philadelphia region. After earning her MSN in Education from Loyola University of New Orleans, she currently also teaches for several prominent Universities making sure the next generation is ready for the bedside. As a certified breastfeeding counselor and trauma certified nurse, she is always ready for the next nursing challenge.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. We will not sell or distribute your email address to any third party, and you may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.
How to Write a Nursing Case Study [Examples, Format, & Tips]
✒️ case study topics for nursing students.
- 🩺️ The Basics
- 💉 Nursing Case Study: Writing Rules
📑 Nursing Case Study Format
📝 nursing case study examples.
- ⏱️ Tips on Quick Writing
🔗 References
A nursing case study is an in-depth analysis of the health situation of an individual patient.
The analysis is based on:
- medical history,
- other relevant criteria.
In most cases, you will be asked to diagnose to suggest the first aid measures. Alternatively, nurses can be asked to describe a patient in their practice and analyze the correctness of their actions. The purpose is to recreate a realistic hospital setting in the classroom and make students reflect on the treatment process from diagnosis to treatment.
- Anaphylactic shock in a teenager with peanut allergy.
- Non-compliant patient with diabetes: ways to improve adherence.
- Telehealth intervention for managing chronic disease.
- Communication strategies to address vaccine hesitancy in a rural community.
- Postpartum hemorrhage in a new mother: risk factors and interventions.
- Ways to improve recognition of dehydration in aging adults.
- The effective ways of maintaining work-life balance for nurses.
- Cultural competency in providing care to migrants and refugees.
- Why should every patient’s medical history remain confidential?
- The use of massage therapy in relieving pain.
- The challenges facing medicine in 2024.
- How does modern technology impact nursing?
- The significance of regular follow-up appointments with the healthcare provider.
- What are the primary treatments for postpartum depression?
- The use of steroids in cancer treatment.
🩺️ Nursing Case Study: What Is It About?
As a nursing student, you should understand that no two patients are the same. Each has a unique clinical record and condition. And although most nursing case study tasks will ask you to suggest a diagnosis or treatment, your focus should rest on the patient.
Busy nurses can sometimes see their patients in the framework of an illness to be treated or a procedure to be fulfilled. But you should do your best to remember that each patient is a living person with a complex set of needs, emotions, and preferences. A ready-made textbook answer is rarely the best solution for them. Moreover, it rarely helps to analyze a condition in isolation from the patient.
In a nursing case study, your task is to analyze a disorder or illness as a part of a specific medical situation. If you don’t do that, your case study becomes an essay (theoretical and generalized). It is the difference between the two assignment types.
Once again:
A case study in nursing emphasizes the particular patient’s condition. Meanwhile, a nursing essay will explore the disease, prevention methods, treatment, or possible consequences of the disease.
Even if the case is hypothetical, it should focus on the suggested reality. On the other hand, essays are usually literature-based. You are expected to do some reading for a case study too, but you should research and present the information within the context of the patient. In simple terms, a case study uses information in the actual application, and an essay uses it for the sake of generalized suggestions.
💉 How to Write a Nursing Case Study: 3 Key Rules
- Do the fieldwork. Before setting your hands to writing, you should collect all of the available materials: clinical notes, results of medical tests, x-rays, sickness records, etc. Use this information to draw a clear picture of the story. It is always helpful to ask yourself, “What is interesting or unusual about this patient’s condition?” In the course of writing, recall your answer from time to time not to get lost in words. It will help you to convey a definite and appropriate message.
- Stick to the facts. A nursing case study should be an accurate description of the actual situation. Restrain from speculating about the inherent mechanisms of the illness or the general treatment methodology. In fact, students are rarely prepared enough to discuss pathology and physiology. Leave this to reputable experts. The best result you can provide in a case study is an honest account of clinical events.
- Concentrate on the patients and their progress. Remember that a nursing case study is a story of a patient’s progress and not a narrative about their nurse. No matter how efficiently the medical specialist acted, it would be incorrect to add any praiseful remarks. The optimal way is to tell the story in its logical and time order and outline the result of treatment. In this case, the outcome will speak for itself.
Introduction
It is where you should tell the reader why this case is interesting . Place your study in a social or historical context. If, during your preliminary research, you found some similar cases, describe them briefly. If you had a hard time diagnosing the patient or your proposed treatment is complicated, mention it here. Don’t forget to cite the references to each of them!
The introduction should not exceed several paragraphs. The purpose is to explain why the reader will benefit from reading about the case.
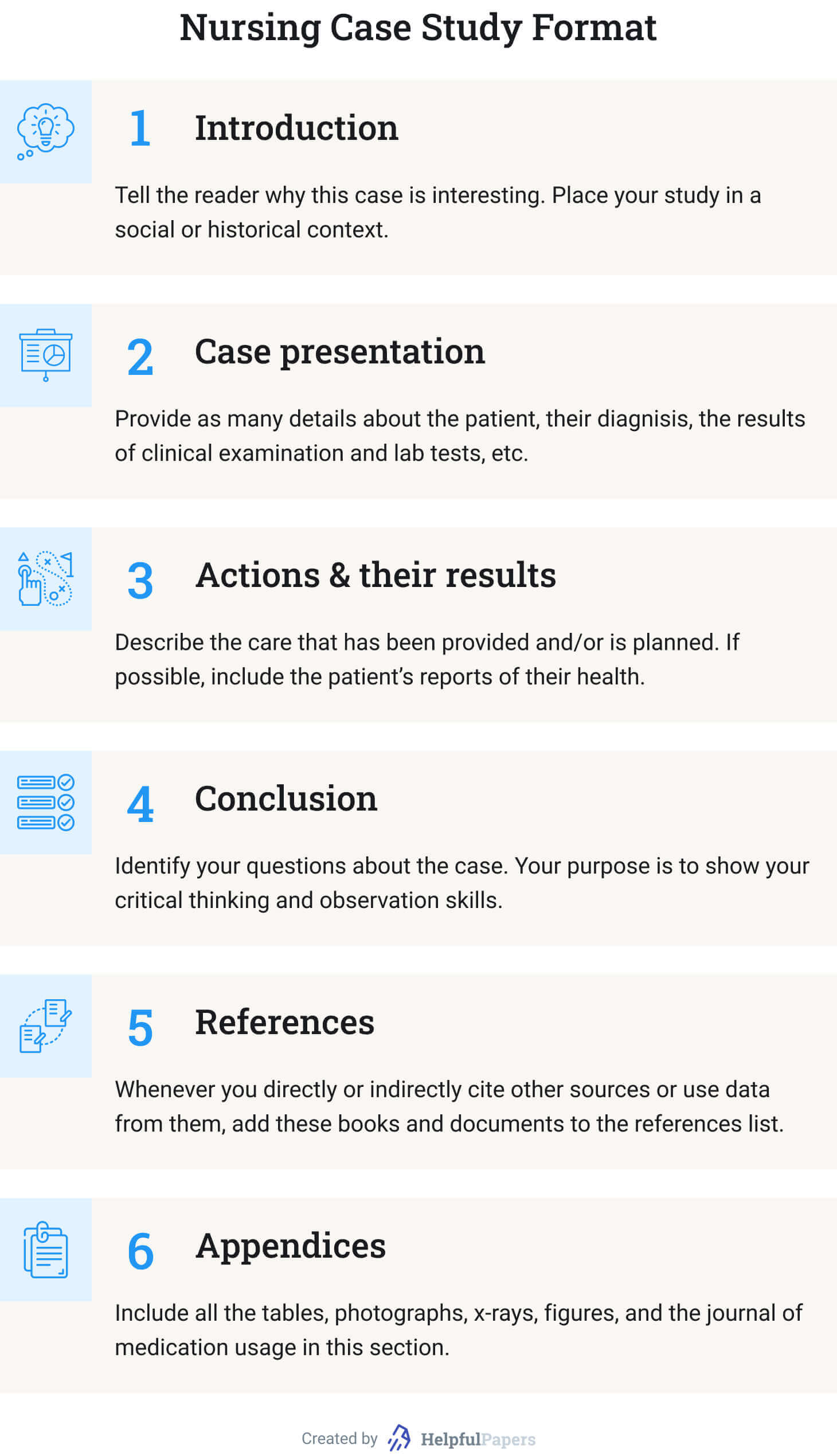
Case Presentation
- Why did the patient seek medical help? (Describe the symptoms.)
- What is known about the patient? (Mention only the information that influenced your diagnosis. Otherwise, explain why some information is irrelevant to the diagnosis.)
- Stick to the narrative form. (Make it a story!)
- What are the variants for diagnosis? (Make a shortlist of possible disorders that fall under the patient’s symptoms. But make it specific: not just “pneumonia” but “bilateral pneumonia,” for example. Besides, this point is optional.)
- What were the results of your clinical examination? (If you saw the patient in person.)
- Explain the results of lab tests. (The words “positive” or “negative” are not always clear.)
Actions and Their Results
This section describes the care that has been provided and/or is planned. You can answer the following questions in narrative form . If some information is missing, skip the point:
- What preliminary actions have been taken? (Be specific: not just “wound care,” but “wound cleaning and dressing.”)
- How long has the patient been under care?
- Has the previous treatment given any visible result?
- Why was it suspended or finished?
- Why did the patient withdraw from treatment (if applicable)?
- How could you improve the patient’s condition if the result was negative?
- If the disease is incurable (like in the case of diabetes), which activities would stabilize the patient’s condition?
- If possible, include the patient’s reports of their own physical and mental health.
In this section, you should identify your questions about the case. It is impossible to answer all of them in one case study. Likewise, it is unreal to suggest all the relevant hypotheses explaining the patient’s condition. Your purpose is to show your critical thinking and observation skills. Finalize your conclusion by summarizing the lessons you learned from the nursing case study.
Whenever you directly or indirectly cite other sources or use data from them, add these books and documents to the references list. Follow the citation style assigned by your professor. Besides, 15 items are already too much. Try to make a list of up to 10. Using textbooks as references can be viewed as bad manners.
Include all the tables, photographs, x-rays, figures, and the journal of medication usage in this section. Unless required otherwise in the assignment, start each item from a new page, naming them “Appendix A,” “Appendix B…”.
Below you will find case study samples for various topics. Using them as a reference will improve your writing. If you need more ideas, you are welcome to use our free title-generating tool .
- Case study: healing and autonomy.
- Sara’s case study: maternal and child nursing.
- COPD medical diagnostics: case study.
- Care standards in healthcare institutions: case study.
- Acute bacterial prostatitis: case study analysis.
- Alzheimer disease: the patient case study.
- The treatment of foot ulcers in diabetic patients: case study.
- Hypertension: C.D’s case study.
- Myocardial infarction: cardiovascular case study.
- Major depressive disorder case.
- Case study of the patient with metabolic syndrome .
- Pulmonary analysis case study .
- Older adults isolation: Case study .
- The holistic care: Case study .
- Medical ethics: Case study .
- Patient diagnoses and treatment: Case study .
- Obesity case study: Mr. C .
- Nurse Joserine: Case study problems .
- Chronic stable angina: Case study .
- Fetal abnormality: Case study .
- Researching SOAP: Case study .
- Case study for a patient with hormonal disorders .
- Obesity in the elderly: The case study .
- “Walking the Tightrope”: A case study analysis .
- ARNP approach: Case study analysis .
- Case study on biomedical ethics in the Christian narrative .
- Thermal injury: Case study .
- Ethical dilemma in nursing: Case study .
- Asthma: A case study of the patient .
- Asthma discharge plan: Mini case study .
- Case study: An ethics of euthanasia .
- Case study: Head-to-toe assessment steps .
- Pain management strategies: Case study .
- Case study: Inflammatory bowel disease .
- Sleep deprivation and insomnia: The case study .
- The case study of a heart failure .
- Porphyria cutanea tarda: Disease case study .
- Case study: Hardy Hospital case summary .
- Obesity and its complications: Case study .
- Angina disease case study .
- Nursing ethics case study .
- Case study of a patient: Assessment and treatment plan .
- Cecile case study: Mrs. J .
- Nursing power in the emergency department: Case study .
- Heart failure case study: Mrs. J .
- Application of ethics in nursing: Case study .
- Sudden visual impairment: Case study .
- Epidemiology case study: Outbreak at Watersedge — Public health discovery game .
- Wellness of senior citizens: Case study .
- Healthcare organization evaluation: Case study of Banner Health .
⏱️ Bonus: Tips on Writing a Case Study in Record Time
Need to prepare a case study on nursing or in another field? Below you’ll find a collection fo tips that will help you do it as quickly as possible!
3 Shortcuts for a Quick Start
If you’re about to start writing a case study, you should check yourself if you’re not doing any of the following:
- spending too much time on selecting a topic;
- reading too much before selecting a topic;
- making conclusions too early – creating bias.
Instead of killing time doing the three useless things discussed above, consider these:
- Choose approach. Note that there are 2 major approaches to case studies: the analytical approach (investigating possible reasons without making any conclusions) and problem-oriented approach (focusing on a particular problem and investigating it).
- Skim some sources (DON’T READ THEM). Select several sources. Simply skim abstracts and conclusions.
- Start making notes early. Simply reading is ineffective unless you’re lucky to have a phenomenal memory. Always make notes of any useful arguments.
4 Shortcuts Not to Get Stuck in the Middle
Even if you kick started your case study, it’s too early to celebrate it. Consider the following traps in the middle of the project:
- Watch the structure. The classic logical structure is your formula of success. It will help you move from one point to another without the unnecessary procrastination:
- Respect the logic. Make your case study flow – make logical transitions between the different parts and make it consistent. Avoid changing your position throughout the paper.
- Be detail-oriented. Any trifle deserves attention when you write a case study.
- Avoid bias. Be sure that all your opinions are based on the specific arguments form the case study. Avoid pouring your biased views into the project.
3 Shortcuts for a Happy Ending
- Offer a realistic solution. College case study is a rehearsal of real-life situations. Take the responsibility for your suggestions.
- Keep your conclusion short. Avoid repeating the details and don’t include any new information.
- Consider creating a Power Point. If your task is not only writing a case study, but also presenting it – why not create PowerPoint slides to help you?
As the last step on your way to a perfect nursing case study, prepare the title page. Its format usually depends on the professor’s requirements. But if you know the citation style, our Title Page Maker is a perfect tool to apply the right formatting and accelerate the process. And if you have any know-how on how to write a medical case study, you are very welcome to share it with other students in the comments below.
❓ Nursing Case Study: FAQ
What is a case study in nursing.
A nursing case study explores the condition of a patient. It is based on previous clinical records, lab reports, and other medical and personal information. A case study focuses on the patient and describes the treatment that was (or should be) applied and its (expected) outcome.
How to Write a Nursing Case Study?
- Collect the bulk of data available about the patient.
- Read literature about the diagnosed condition.
- Focus on the individual patient and their symptoms.
- Describe the situation and outline its development in time.
- Analyze the actions of the medical personnel that have been done.
- Plan further treatment of the patient.
Why Are Case Studies Good for Nursing Students?
Nursing case studies offer you a priceless opportunity to gain experience of different patient conditions and cure methods without visiting the clinic. You can think about whether the proposed treatment was appropriate or wrong and suggest a better solution. And the best thing, your teacher will indicate your mistakes (and no patient will be hurt in the process).
Why Are Case Studies Important in Nursing?
- You learn to distinguish the relevant data and analyze it.
- You learn to ask the right questions.
- You learn to evaluate the severity of symptoms.
- You learn to make better diagnoses.
- You train your critical thinking in terms of treatment methods
- Case studies are in-class simulators of authentic atmosphere in a clinical ward.
- What is a case study? | Evidence-Based Nursing
- Case Studies – Johns Hopkins Medicine
- Case Study Research Design in Nursing
- Case study report for Nursing | Learning Lab – RMIT University
- Case Study or Nursing Care Study? – jstor
Research Paper Analysis: How to Analyze a Research Article + Example
Film analysis: example, format, and outline + topics & prompts.
- Upcoming Issues
- Archive Issues
- Press Releases
- Case Studies
- Industry Reports
- Research Insight
- Techno Trends
- White Papers
- Health & Wellness
- Organizations
- Target Market
- Target Audience
- E-Newsletters
Featured News
Transforming pathology labs: the role of laboratory information systems in hospitals, hospital discharge care intervention reduces readmissions, healthcare ai transparency – onc finalises sweeping rule, advances in the patient care and system capability with ai, leveraging iot for more effective management at hospitals, livedata periop tools recognized as a top hospital it solution for…, increasing emr system satisfaction through personalisation, intersystems expands the intersystems iris data platform with vector search to…, meeting patients’ digital expectations with systems that put safety first, an ai future where healthtech merges with the human touch, building trust in healthcare through digital engagement, latest press releases, intersystems named as a strong performer in forrester wave for enterprise data fabrics, andaman7 launches ai supercharged personal health record v5, improve cancer care through automated ct analysis: oncoshield – ct, intersystems fhir for indonesia roadshow with dto, persi and arssi empowers healthcare providers to be satusehat compliant, featured press releases, intersystems and ecosystm study reveals data synergy would improve analytics insights…, intersystems reimagines clinician workflow with trakcare assistant, greiner bio-one celebrates its 60th anniversary.
- Knowledge Bank
How to Write a Case Study Paper for Nursing
Case studies are an evitable part of nursing education. These projects allow nursing students to understand the concepts of health assessment better, define factual information about the patient, and prepare for the licensure examination.
A case study will teach you how to conduct a comprehensive health assessment, including physical, psychological, and social evaluations. To complete the case study successfully, you must combine your theoretical knowledge and practical skills to advance as a professional nurse. For example, spinal stenosis is a term that expresses low back pain. But knowing the term is not enough; you must understand the main symptoms, how this condition occurs, and related conditions that may clarify your patient’s health.
As a nursing student, you may feel confused with case studies, as it requires in-depth and critical analysis thinking from you. If you have faced this type of assignment for the first time, you can use a case study writing service to get a clear idea of how the paper should be written. A licensed nurse will perform writing and deliver a professional-looking paper.
You will be assigned to solve various case studies during your nursing course. Typically, there are two types of nursing case studies:
• Traditional case study. This kind often comprises a patient’s scenario as well as a list of questions that need to be addressed.
• Unfolding case study. It’s quite a new type of case study. The task usually presents a patient scenario with evolution details. Students must evaluate and re-evaluate the patient’s condition based on the offered scenario, care plan, and rationale.
7 Steps to Write a Nursing Case Study
Read out the case carefully. Just after you have read the text, think about the situation. How does the case influence your patient? Does it influence the care plan? How does the received information affect the priorities of care and implementation?
Evaluate the case. Don’t rush into writing a practice section. You need to analyze subjective and objective data to be able to make a patient’s health assessment and draw up a plan. You may be able to see possible difficulties and advantages in the treatment of the patient by thinking back on the scenario described in the case. Your capacity for critical thinking and the quality of your patient care decision-making may be improved by proper evaluation.
Understand the questions. You need to figure out every word to receive the correct answer. Try to rephrase the question and underline keywords to grasp the main idea. Moreover, you may need to clarify and search for more information to understand the question better. It can also be beneficial to divide difficult questions into manageable chunks and respond to each separately.
Answer a “So what” question. It’s essential to improve your critical thinking skills and retention of key information. We advise you to additionally use external resources such as textbooks or evidence-based search engines to clarify any uncertainties and deepen your understanding of the subject matter. Take notes while evaluating to identify key moments to consider when answering the question and be helpful when making conclusions.
Take a new stance. Now it’s time to reread the text of the case and relate all information you have to the situation. Do new key points influence the health care plan? What has changed? After responding to questions, thinking back on the patient description may offer fresh perspectives that weren’t initially obvious. This task can help improve patient care and develop your clinical reasoning abilities.
Consider future outcomes. After you have driven the conclusion, it’s time to reflect on how the care plan will influence the trajectory of patients’ care. How will it affect your patient? To avoid problems and enhance results, you must proactively adapt your care strategy by predicting possible changes in the patient’s state.
Organize your answers. Some nursing schools and colleges give templates that students should just fill in. At the same time, others ask for more formal writing. To write answers to your case study, read out the requirements for paper design. It might include the referencing style (typically APA), length, and required sections.
Tips for Writing a Nursing Case Study
Plan your time. Dedicate enough time to work on the case study. You may need to do additional research and organize your writing.
Don’t get frustrated. When you don’t know the answer, don’t try to find the perfect or ideal solution. Define the room for your growth and define your knowledge gaps.
Format your paper. Organize your references and citations according to the required formatting style.
Proofread and edit. Spelling and grammar errors can spoil even a perfect answer. Some professors don’t mind mistakes, while others may lower your mark.
Self-evaluate your performance on the case . It’s highly important to find your areas of strength and weakness. If you wish to grow personally and professionally, take some time to reflect on your case performance.
Wrapping Up
Working on case studies may be overwhelming, but it will be much easier with the proper guidance and your effort. Keep in mind to take pauses and get assistance when necessary. Don’t be afraid to edit and rewrite your work to get the best results.
RELATED ARTICLES MORE FROM AUTHOR
Livedata periop tools recognized as a top hospital it solution for 2024, recent posts, why consult an atlanta-based injury lawyer for your accident claims, know your heart: reducing the risk of cardiovascular disease, when robotics meet surgery: the future of operative medicine.
Select Country Algeria (+213) Andorra (+376) Angola (+244) Anguilla (+1264) Antigua & Barbuda (+1268) Argentina (+54) Armenia (+374) Aruba (+297) Australia (+61) Austria (+43) Azerbaijan (+994) Bahamas (+1242) Bahrain (+973) Bangladesh (+880) Barbados (+1246) Belarus (+375) Belgium (+32) Belize (+501) Benin (+229) Bermuda (+1441) Bhutan (+975) Bolivia (+591) Bosnia Herzegovina (+387) Botswana (+267) Brazil (+55) Brunei (+673) Bulgaria (+359) Burkina Faso (+226) Burundi (+257) Cambodia (+855) Cameroon (+237) Canada (+1) Cape Verde Islands (+238) Cayman Islands (+1345) Central African Republic (+236) Chile (+56) China (+86) Colombia (+57) Comoros (+269) Congo (+242) Cook Islands (+682) Costa Rica (+506) Croatia (+385) Cuba (+53) Cyprus North (+90392) Cyprus South (+357) Czech Republic (+42) Denmark (+45) Djibouti (+253) Dominica (+1809) Dominican Republic (+1809) Ecuador (+593) Egypt (+20) El Salvador (+503) Equatorial Guinea (+240) Eritrea (+291) Estonia (+372) Ethiopia (+251) Falkland Islands (+500) Faroe Islands (+298) Fiji (+679) Finland (+358) France (+33) French Guiana (+594) French Polynesia (+689) Gabon (+241) Gambia (+220) Georgia (+7880) Germany (+49) Ghana (+233) Gibraltar (+350) Greece (+30) Greenland (+299) Grenada (+1473) Guadeloupe (+590) Guam (+671) Guatemala (+502) Guinea (+224) Guinea - Bissau (+245) Guyana (+592) Haiti (+509) Honduras (+504) Hong Kong (+852) Hungary (+36) Iceland (+354) India (+91) Indonesia (+62) Iran (+98) Iraq (+964) Ireland (+353) Israel (+972) Italy (+39) Jamaica (+1876) Japan (+81) Jordan (+962) Kazakhstan (+7) Kenya (+254) Kiribati (+686) Korea North (+850) Korea South (+82) Kuwait (+965) Kyrgyzstan (+996) Laos (+856) Latvia (+371) Lebanon (+961) Lesotho (+266) Liberia (+231) Libya (+218) Liechtenstein (+417) Lithuania (+370) Luxembourg (+352) Macao (+853) Macedonia (+389) Madagascar (+261) Malawi (+265) Malaysia (+60) Maldives (+960) Mali (+223) Malta (+356) Marshall Islands (+692) Martinique (+596) Mauritania (+222) Mayotte (+269) Mexico (+52) Micronesia (+691) Moldova (+373) Monaco (+377) Mongolia (+976) Montserrat (+1664) Morocco (+212) Mozambique (+258) Myanmar (+95) Namibia (+264) Nauru (+674) Nepal (+977) Netherlands (+31) New Caledonia (+687) New Zealand (+64) Nicaragua (+505) Niger (+227) Nigeria (+234) Niue (+683) Norfolk Islands (+672) Northern Marianas (+670) Norway (+47) Oman (+968) Palau (+680) Panama (+507) Papua New Guinea (+675) Paraguay (+595) Peru (+51) Philippines (+63) Poland (+48) Portugal (+351) Puerto Rico (+1787) Qatar (+974) Reunion (+262) Romania (+40) Russia (+7) Rwanda (+250) San Marino (+378) Sao Tome & Principe (+239) Saudi Arabia (+966) Senegal (+221) Serbia (+381) Seychelles (+248) Sierra Leone (+232) Singapore (+65) Slovak Republic (+421) Slovenia (+386) Solomon Islands (+677) Somalia (+252) South Africa (+27) Spain (+34) Sri Lanka (+94) St. Helena (+290) St. Kitts (+1869) St. Lucia (+1758) Sudan (+249) Suriname (+597) Swaziland (+268) Sweden (+46) Switzerland (+41) Syria (+963) Taiwan (+886) Tajikstan (+7) Thailand (+66) Togo (+228) Tonga (+676) Trinidad & Tobago (+1868) Tunisia (+216) Turkey (+90) Turkmenistan (+7) Turkmenistan (+993) Turks & Caicos Islands (+1649) Tuvalu (+688) Uganda (+256) UK (+44) Ukraine (+380) United Arab Emirates (+971) Uruguay (+598) USA (+1) Uzbekistan (+7) Vanuatu (+678) Vatican City (+379) Venezuela (+58) Vietnam (+84) Virgin Islands - British (+1284) Virgin Islands - US (+1340) Wallis & Futuna (+681) Yemen (North)(+969) Yemen (South)(+967) Zambia (+260) Zimbabwe (+263)

7 steps to successful nursing case study writing.
A nursing case study is a detailed study of a patient that is encountered during a nurse’s daily practice. They are usually written by nurses in training as part of their coursework, but they can also be written by experienced nurses as a way of sharing best practice.
Case studies are an important part of the nursing curriculum as they provide students with a real-life insight into the complexities of patient care. They also allow nurses to reflect on their own practice and identify areas where they could make improvements.
When writing a nursing case study, it is important to follow the instructions provided by your tutor. This will ensure that your case study is relevant and meets the required academic standards. It is also important to be clear and concise in your writing, and to use evidence-based sources to support your claims.
If you are struggling to write a nursing case study, there are a number of resources that can help you. The following books are all recommended reading for anyone wanting to write a case study:
- The Complete Guide to Case Study Research by Elaine M. Hubbell
- Nursing Case Studies: A Guide to Understanding and Writing Them by Jennifer R. Gray
- Writing Nursing Case Studies by Sally G. Reed
Once you have a good understanding of how to write a nursing case study, you will be able to produce high-quality studies that will be of benefit to both yourself and your patients.
Importance of nursing case study writing.
Nursing case studies are an important part of your nursing education. They provide you with the opportunity to apply the knowledge and skills you have learned in the classroom to real-world scenarios. Nursing case studies also allow you to develop critical thinking and problem-solving skills.
The nursing case study should be a detailed and accurate account of the care that was provided to the patient. It should be used to evaluate the outcome of that care and to identify any areas where improvements can be made.
Steps when writing a nursing case study paper.
There are various steps you should keep in mind in order to help you write a successful nursing case study.
These important steps include:
- Define the problem.
- Gathering information.
- Developing alternatives.
- Analyzing the alternatives.
- Selecting the best alternative.
- Implementing the solution.
- Evaluating the outcome.
Defining the Problem
When writing a nursing case study, it is important to first define the problem. The problem should be something that can be solved through nursing interventions. Once the problem is defined, the nursing case study can be written to discuss the interventions that were used to solve the problem.
Nursing case studies are a great way to learn about different nursing interventions and how they can be used to solve problems. By reading nursing case studies, nurses can learn about different diseases and conditions and how to treat them. Nursing case studies can also be used to teach other nurses about different interventions.

Gathering Information
When it comes to writing a nursing case study, the first and most important step is gathering information. This is where you will need to do your research and collect data from a variety of sources. Once you have all of the information you need, you can begin to write your case study.
It is crucial to gather information before starting to write your nursing case study. This ensures that you include all of the relevant information. This means including details about the patient’s medical history, symptoms, and treatment.
Developing Alternatives
Once you have all of the necessary information, you can begin developing alternatives for the patient’s treatment. This will involve looking at the different options and deciding which is best based on the specific case. You will need to consider the risks and benefits of each option before making a recommendation.
Once you have developed a few different options, you can then start writing the case study. This should include an overview of the patient’s history, their current condition, and the different treatment options that were considered. Be sure to explain why you ultimately recommended the chosen course of treatment.
Analyzing the Alternatives
When you are given a nursing case study to write, the first step is to read the case thoroughly. Make sure you understand the situation and the patient’s history. Once you have a good understanding of the case, you can start to analyze the alternatives.
There are usually three alternatives in a nursing case study: nursing intervention, medical intervention, and no intervention. You will need to evaluate each alternative and decide which is best for the patient.
Nursing intervention is usually the first choice because it is the least invasive and has the least risk. Medical intervention is usually the next choice because it is more invasive but has a higher chance of success. No intervention is usually the last choice because it means doing nothing and letting the patient’s condition worsen.
Once you have evaluated the alternatives, you can start to write your case study. Remember to include all of the important information, such as the patient’s history, the alternatives you considered, and your recommendation.
Selecting the Best Alternative
When you are presented with a nursing case study, the first thing you need to do is identify the problem. Once you have identified the problem, you need to gather information about the patient. This information will help you to develop a plan of care. Once you have developed a plan of care, you need to select the best alternative.
The best alternative is the one that will best meet the needs of the patient. When selecting the best alternative, you need to consider the patient’s preferences, the severity of the problem, the risks and benefits of each alternative, and the resources available.
Implementing the Solution
Once you have selected the best alternative, you need to implement the plan of care. After you have implemented the plan of care, you need to evaluate the patient’s response. If the patient’s condition improves, you need to continue the plan of care. If the patient’s condition does not improve, you need to reevaluate the plan of care and select a different alternative.
Evaluating the Outcome
A nursing case study is a detailed account of a patient’s medical history and treatment. It is used to evaluate the outcome of a patient’s care and to identify any areas where improvements can be made.
When writing a nursing case study, it is important to include a detailed description of the patient’s symptoms and medical history. The case study should also include a discussion of the treatment that was provided and the outcome of that treatment.
It is also important to discuss any areas where improvements could be made in the care that was provided. This could include changes to the treatment plan, changes to the way that the patient was monitored, or changes to the way that the patient’s symptoms were managed.
Conclusion.
Writing a successful nursing case study can be a challenging task. However, by following the steps provided in this blog that is, first defining the problem, gathering information, developing alternatives., analyzing the alternatives, selecting the best alternative, implementing the solution and evaluating the outcome. You will be able to write a top-notch nursing case study that meets your requirements.
If you need professional assistance, place your order right here to get help from expert nursing paper writers.

Work with professional online writers

- Affordable Nursing Papers
- Nursing Coursework Writing
- Nursing Essay Writing Service
- Nursing Essay Assignments
- Nursing Assignment Writing
- Nursing Case Study Writing
- Nursing Process Essay Writing
- Nursing Capstone Project
- BSN Capstone Project
- Reliable Nursing Writers
- PICO Question Examples
- Nursing Speeches
- Nursing PowerPoint Presentations
- Online Nursing Essay Writers
- Nursing Thesis
- Nursing Coursework
- Nursing Term Papers
- Legit Nursing Writers
- Best Nursing Writing Company
- Nursing Students Writing Help
- Cheap Nursing Term Paper

- Refund Guarantee
- On time delivery
- Plagiarism-free papers
- Safe and Confidential
- Trained Writers
- Nursing Essay Writing
- Nursing Coursework Help
- Nursing Dissertations
- Nursing Case Studies
- Nursing Assignment Help
Contact Info
- 123 Fifth Ave, New York, NY 12004, United States.
- +1(413) 798-7210
- [email protected]
- AI Content Shield
- AI KW Research
- AI Assistant
- SEO Optimizer
- AI KW Clustering
- Customer reviews
- The NLO Revolution
- Press Center
- Help Center
- Content Resources
- Facebook Group
How to Write a Thorough Nursing Case Study
Table of Contents
Case studies are common requirements for nursing schools and healthcare institutions. But learning how to write a nursing case study can be challenging. If you’re stuck on how to get started, we’ve got your back! In this article, we’ll be guiding you through all the necessary elements you should include ensuring your study is clear and thorough. We’ll also share some key tips to make your work more professional. When done right, a case study can enhance your knowledge base and help identify better healthcare practices. And this can greatly improve overall healthcare standards.
What is a Nursing Case Study?
A nursing case study is a detailed assessment of a patient’s medical history, diagnosis, and treatment . It seeks to identify the causes of an illness or injury and analyze how they have been addressed. This helps assess the overall quality of care given. These case studies aim to understand the cause of certain illnesses, how to prevent them, and how to best treat them. The data gathered from these studies can inform policy changes and develop effective strategies for improving patient outcomes.

How to Write a Nursing Case Study
Writing a nursing case study requires thoughtful consideration of relevant information and resources. You must select a single subject, conduct research on it, interview experts, analyze the data collected, and present your findings. That may seem like a lot, but let us break it down for you. Here’s a look at the key elements that your case study structure should cover:
A title page should be concise yet informative, helping readers understand what the focus of the study is. It includes the following elements:
- Title of the case study
- Author’s name
- Any collaborators or contributors to the work
- An abstract summarizing the contents
An abstract is a summary of the content of the case study, which outlines its purpose, methods used, results, and conclusions. It aims to provide readers with a clear overview of the studied topic without reading through the entire document.
Introduction
The introduction sets the stage for the case study by introducing the main subject and providing background information. It should include the research question(s) or hypothesis that will guide the investigation.
Case Presentation
Your case presentation needs to include as much relevant detail as possible while maintaining clarity and brevity. It details the following:
- Patient’s history
- Physical exam findings
- Laboratory values
- Imaging studies
- Treatments received
- Clinical course
Pathophysiology
Pathophysiology discusses how diseases affect normal body processes and functions. Try to explain the pathology behind the observed symptoms to understand how they can be managed. This may involve discussing anatomy, physiology, biochemistry, genetics, pharmacology, immunology, and pathogenesis.
Nursing Care Plan
A nursing care plan should provide an overview of the patient’s current condition, including any pre-existing medical conditions. It should also outline the desired goals for the patient’s health, such as stabilizing vital signs or reducing pain levels. The plan will usually include a list of interventions to be carried out by nurses. It can also outline monitoring steps to evaluate whether these interventions are effective in achieving the desired outcomes.
Discussion and Recommendations
This section provides an opportunity to discuss any issues or suggestions related to the patient’s case study. Experienced professionals can provide valuable input regarding the best strategies to improve the treatment outcome.
The conclusion is where you can summarize all the findings from the study and provide your final thoughts regarding the results. It should draw attention to any successes achieved during the investigation and identify areas for improvement. Your conclusion should also make clear how the results relate to the overall objective of providing quality care for the patient.
The references section is where sources used throughout the case study are listed. These may include textbooks, reports, journal entries, and other forms of documentation that were consulted for the project. All entries must adhere to proper citation standards (e.g., APA style) and appear alphabetically according to the author’s name.
Final Words
Learning how to write a nursing case study has far more applications than just fulfilling a course requirement. These case studies can be invaluable tools in advocating for improved healthcare for individuals and communities. Hopefully, this quick guide has helped you better understand how to write a more comprehensive and clearer work. Good luck!

Abir Ghenaiet
Abir is a data analyst and researcher. Among her interests are artificial intelligence, machine learning, and natural language processing. As a humanitarian and educator, she actively supports women in tech and promotes diversity.
Explore All Write A Case Study Articles
How to write a leadership case study (sample) .
Writing a case study isn’t as straightforward as writing essays. But it has proven to be an effective way of…
- Write A Case Study
Top 5 Online Expert Case Study Writing Services
It’s a few hours to your deadline — and your case study college assignment is still a mystery to you.…
Examples Of Business Case Study In Research
A business case study can prevent an imminent mistake in business. How? It’s an effective teaching technique that teaches students…
How to Write a Multiple Case Study Effectively
Have you ever been assigned to write a multiple case study but don’t know where to begin? Are you intimidated…
How to Write a Case Study Presentation: 6 Key Steps
Case studies are an essential element of the business world. Understanding how to write a case study presentation will give…
How to Write a Case Study for Your Portfolio
Are you ready to showcase your design skills and move your career to the next level? Crafting a compelling case…
Connect on WhatsApp: +91 74786 38563 , Uninterrupted Access, 24x7 Availability, 100% Confidential. Connect Now
Writing Tips
A comprehensive nursing case study writing guide.
Aug. 4, 2023 • 7 min read
Nursing Case Study Writing Step-By-Step Guide
Nursing case studies play a vital role in the education and training of aspiring nurses in the USA, UK, UAE, and Canada. These real-life scenarios provide students with a unique opportunity to apply theoretical knowledge to practical situations, enhancing their critical thinking, clinical reasoning, and decision-making skills. In this guide, we'll walk you through the essential steps to creating effective and insightful nursing case studies that meet the academic standards of these countries.
1. Choosing a Relevant Case
The foundation of a successful nursing case study is the selection of an appropriate case. Look for scenarios that align with your course's learning objectives and reflect the wide range of healthcare challenges that nurses may face. Select cases involving ethical quandaries, complex patient interactions, or situations requiring interdisciplinary collaboration.
2. Gathering Information
Thorough research is key to crafting a detailed and accurate nursing case study. Collect data from reputable sources such as medical journals, textbooks, and evidence-based practice guidelines. Ensure that the patient's medical history, current condition, and relevant clinical data are well-documented. Protect patient confidentiality by de-identifying information.
3. Setting the Stage
Introduce the case by providing basic details on the patient, the healthcare setting, and any other relevant information. Describe the patient's demographics, medical history, current symptoms, and reason for seeking medical help. This establishes the context for readers to comprehend the situation and its significance.
4. Clinical Assessment
Detail the nursing assessment process, including physical examinations, diagnostic tests, and the collection of subjective and objective data. Highlight the nurse's role in observing, interviewing, and evaluating the patient's condition. Discuss the data collected and its implications for the patient's care.
5. Diagnosis and Planning
Based on the assessment, outline the nursing diagnoses and collaborative problems. Clearly explain the rationale behind each diagnosis and present a well-reasoned plan of care. Discuss short-term and long-term goals, potential interventions, and the expected outcomes of nursing interventions.
6. Implementation and Evaluation
Describe how the nursing care plan was executed and the interventions that were implemented. Include details about the nurse's interactions with the patient, families, and other healthcare team members. Evaluate the effectiveness of the interventions, discussing any changes in the patient's condition, responses to treatment, and unexpected challenges.
7. Reflection and Learning
Encourage critical thinking by incorporating a reflection section. Invite students to analyze the case, consider alternative approaches, and reflect on what they have learned from the experience. Discuss the ethical, cultural, and emotional aspects of the case, promoting a holistic understanding of patient care.
8. References and Citations
Maintain academic integrity by properly citing all sources used in your case study. Follow the appropriate citation style (such as APA, MLA, or Chicago) as required by your institution.
Writing nursing case studies is an essential skill for nursing students in the USA, UK, and Canada. Through these case studies, students can bridge the gap between theory and practice, preparing them for the complex and dynamic healthcare environments they will encounter in their careers. By carefully selecting cases, conducting thorough research, and presenting well-structured and reflective analyses, nursing students can create case studies that not only meet academic standards but also contribute to their growth as competent and compassionate healthcare professionals.
Our platform has been giving quality services to our students from the very beginning, all thanks to our highly-trained and professional Nursing case study helpers, who complete every task with utmost sincerity and dedication by applying all their knowledge to your projects so that you can raise your head confidently while presenting in front of your class. TutorGenix has always been ranked as the Best Nursing Case Study help in the USA, the UK, Canada, and the UAE. Our Nursing project writers will complete your academic reports, essays, homework, and whatnot, so just order us and we will help with everything we’ve got. You will get instant solutions for nursing homeworks or any other subject homework you need help with, as we have 24/7 available tutors.
Stuck With Your Homework? Get Your Homework Done From Our Expert Writers
Is there any desired work length (in words)?
No. of pages (1 page = 250 words)
Fill Your Mobile Number & Get 5$
I accept the T&C and other policies of the website and agree to receive offers and updates.
Useful Links:
- Homework Help
- Assignment Help
- Live Session Help
- Lab Report Writing
- Project Report Writing
- PowerPoint Presentation
- Case Study Writing
- Essay Writing
- Coursework Writing
Related Articles

How to Write a Freedom Essay in 9 Steps
June 23, 2023 • 10 min read
What are the 4 types of sentences?
June 13, 2023 • 10 min read
How to write a Lab Report?
Nov. 28, 2022 • 10 min read
- General Nursing
- Nursing Specialties
- Nursing Students
- United States Nursing
- World Nursing
- Boards of Nursing
- Breakroom / Clubs
- Nurse Q&A
- Student Q&A
- Fastest BSN
- Most Affordable BSN
- Fastest MSN
- Most Affordable MSN
- Best RN to BSN
- Fastest RN to BSN
- Most Affordable RN to BSN
- Best LPN/LVN
- Fastest LPN/LVN
- Most Affordable LPN/LVN
- Fastest DNP
- Most Affordable DNP
- Medical Assistant
- Best Online Medical Assistant
- Best Accelerated Medical Assistant
- Most Affordable Medical Assistant
- Nurse Practitioner
- Pediatric NP
- Neonatal NP
- Oncology NP
- Acute Care NP
- Aesthetic NP
- Women's Health NP
- Adult-Gerontology NP
- Emergency NP
- Best RN to NP
- Psychiatric-Mental Health NP
- RN Specialties
- Best RN Jobs and Salaries
- Aesthetic Nurse
- Nursing Informatics
- Nurse Case Manager
- Forensic Nurse
- Labor and Delivery Nurse
- Psychiatric Nurse
- Pediatric Nurse
- Travel Nurse
- Telemetry Nurse
- Dermatology Nurse
- Best NP Jobs and Salaries
- Family NP (FNP)
- Orthopedic NP
- Psychiatric-Mental Health NP (PMHNP)
- Nurse Educator
- Nurse Administrator
- Certified Nurse Midwife (CNM)
- Clinical Nurse Specialist (CNS)
- Certified Registered Nurse Anesthetist (CRNA)
- Best Free Online NCLEX-RN Study Guide
- The Nursing Process
- Question Leveling
- NCLEX-RN Question Identification
- Expert NCLEX-RN Test-Taking Strategies
- Best Scrubs for Nurses
- Best Shoes for Nurses
- Best Stethoscopes for Nurses
- Best Gifts for Nurses
- Undergraduate
- How to Become an LPN/LVN
- How to Earn an ADN
- Differences Between ADN, ASN, AAS
- How to Earn a BSN
- Best MSN Concentrations
- Is an MSN Worth It?
- How to Earn a DNP
- MSN vs. DNP
What's the difference between case study and care plan?
Nursing Students General Students Nursing Q/A

HI, I'm in block one,
I have my first case study next week. What is the difference between a case study and care plan ?
We are told to use various formats such as;
A assessment
D diagnosis/with at least two (NANDA) diagnoses
I implementation
E evaluation
I'm aware of the info and concept, but I wish I could see an example of a case study just to assure myself I'm on the right track.
I do have a nursing care plan book/mosby.
More Like This
- + Add a Comment
- Sort by votes
- Sort by date
- Good answer?

A case study is when u analyze or report about the status of the patient. It includes the assessment, patho-physio of the disease, etc. It's more general. Care plan includes the ones that you put above. U can incorporate the care plan in the case study.

llg, PhD, RN
13,469 Posts
You may already know this, but as you are a new nursing student, I'll offer this friendly warning. As different schools and different instructors may use the terms in a slightly different way, it's risky to rely on other people for the answer to your question. Your school/instructor probably has specific requirements for its case studies (or care plans ) and someone outside that school would not be aware of that.
A lot of students hesitate to ask questions in class because they don't like drawing attention to themselves. I see this all the time. I'll teach a class and then say, "Does anybody have any questions?" and everyone sits there silently. Then, as soon as I release them from class, a small crowd gathers around me with the questions they SHOULD have asked when given the chance. Many of them have the same question and it would have saved us all a lot of time and trouble if one of them would have the gumption to ask it publically so that we could clear it up for everyone at the same time.
Books, articles, strangers on the internet, etc. can give you some information about the topic in general (that might be correct or incorrect). But even the best general sources can't know the particular preferences of your faculty.
So ... Talk to your instructor first. If you still have questions, tell her that you need a little more clarification. If you are still having questions after that, seek help within your school -- upperclassmen are often a good source of information and many schools have tutoring services, etc. The general information you'll get from outside sources may be helpful in broadening your understanding of the big picture, it may add to your confusion if your faculty has specific requirements that don't exactly match those of the author.
Good luck with school.
Daytonite, BSN, RN
1 Article; 14,604 Posts
Hi, iggyangel! Block one! And already a case study ! I'm assuming you've had no patients, am I right? Therefore, what is going to happen is you'll most likely be given information about a hypothetical "Patient" for you to do a care plan on just as if they really existed. The difference is that you won't have the opportunity to actually see and assess a real person. So, parts of the normal data gathering process are going to come from information you will glean from a variety of textbooks to help you out. This is generally the way most case studies in nursing school are done in order to help nursing students develop an appreciation of how the nursing process works as well as to learn something about the treatment and care of specific illnesses that people have.
I do think you may have gotten a bit confused about what you have in your notes. Adpie is the nursing process. Each letter of the acronym, adpie, stands for one part of the care planning process. A care plan is merely the written result of putting all those elements together. However, in actuality, a nurse on the job is constantly thinking about a patient's care in terms of the entire nursing process all the time. It's just that committing it to paper seems to be the monkey wrench that fouls up the works for most people! Part of the reason is because it forces you to slow your thinking down to break this process down into it's component parts.
Your nursing care plan book, the one written by betty ackley isn't it, is a good one. Ackley updated all her care plan books in 2005 to reflect the newest changes from nanda (north american nursing diagnosis association). In the very first chapters should be a discussion about the care planning process and adpie. I strongly recommend that you read those early chapters in the book that discuss this. Don't just read them once, but several times at different seating sessions until you get an inkling of what is being said. That information will help you as you go through this necessary process in nursing school of writing case studies and care plans . After all, your grades are going to depend on how well you do these assignments.
The early chapter discussions in your care plan book will guide you as to how your assessment is used to determine the nursing diagnoses you pick, which leads to the nursing interventions (plan) you decide upon and implement and, finally, the evaluation of the plan.
Generally, in case studies where you don't have an actual patient, the assessment data comes from the information that you are given in the scenario your instructor presents you as well as information (signs, symptoms, treatment) you will look up about the actual medical disease, if you are given the name of an actual medical disease to work with. Sometimes you will need to look up the pathophysiology of a disease to include with the presentation. This is an instructor's choice, so you need to find out if that is something your instructor will want or not.
As the previous poster wrote in reply to you, check with your instructor for specifics about this assignment. In fact, start making a list of questions today to take into class with you. Don't leave class until they have all been answered satisfactorily. Remember, it's your grade, not mine. I can help you with putting a care plan together, but I'm not the one sitting in your classroom getting the instructions you have to follow.
Thank you all for your input and help.
I will read up more and talk to my teacher and upper class students.'
Nursing Case Study for Breast Cancer
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Natasha is a 32-year-old female African American patient arriving at the surgery oncology unit status post left breast mastectomy and lymph node excision. She arrives from the post-anesthesia unit (PACU) via hospital bed with her spouse, Angelica, at the bedside. They explain that a self-exam revealed a lump, and, after mammography and biopsy, this surgery was the next step in cancer treatment, and they have an oncologist they trust. Natasha says, “I wonder how I will look later since I want reconstruction.”
What assessments and initial check-in activities should the nurse perform for this post-operative patient?
- Airway patency, respiratory rate (RR), peripheral oxygen saturation (SpO2), heart rate (HR), blood pressure (BP), mental status, temperature, and the presence of pain, nausea, or vomiting are assessed upon arrival. Medication allergies, social questioning (i.e. living situation, religious affiliation), as well as education preference are also vital. An admission assessment MUST include an examination of the post-op dressing and any drains in place. This should be documented accordingly.
- The hand-off should be thorough and may be standardized. Some institutions have implemented a formal checklist to provide a structure for the intrahospital transfer of surgical patients. Such instruments help to standardize processes thereby ensuring that clinicians have critical information when patient care is transferred to a new team. The nurse should also prepare to provide education based on surgeon AND oncologist guidance
What orders does the nurse expect to see in the chart?
- Post-op medications, dressing change and/or drain management, strict I&O, no BP/stick on the operative side (rationale is to help prevent lymphedema – Blood pressure (BP) measurement with a cuff on the ipsilateral arm has been posed as a risk factor for the development of LE after-breast cancer therapy for years, regardless of the amount of lymph node excision.)
- Parameters for calling the surgeon are also important. The nurse should also check for an oncology service consult.
After screening and assessing the patient, the nurse finds she is AAOx4 (awake, alert and oriented to date, place, person and situation). The PACU staff gave her ice due to dry mouth which she self-administers and tolerates well. She has a 20G IV in her right hand. She states her pain is 2 on a scale of 1-10 with 10 being the highest. Her wife asks when the patient can eat and about visiting hours. Natasha also asks about a bedside commode for urination and why she does not have a “pain medicine button”. Another call light goes off and the nurse’s clinical communicator (unit issued cell phone) rings.
The nurse heard in report about a Jackson-Pratt drain but there are no dressing change instructions, so she does not further assess the post-op dressing situation in order deal with everything going on at the moment. She then sits down to document this patient.
Medications ordered in electronic health record but not yet administered by PACU: Tramadol 50 mg q 6 hrs. Prn for mild to moderate pain. Oxycodone 5 mg PO q 4 hrs. Prn for moderate to severe pain (5-7 on 1-10 scale) Fentanyl 25 mcg IV q3hrs. Prn For breakthrough pain (no relieve from PO meds or greater than 8 on 1-10 scale) Lactated Ringers 125 mL/hr IV infusion, continuous x 2 liters Naloxone 0.4-2 mg IV/IM/SC; may repeat q2-3min PRN respiratory rate less than 6 bpm; not to exceed 10 mg
BP 110/70 SpO2 98% on Room Air HR 68bpm and regular Ht 157 cm RR 14 bpm Wt 53 kg Temp 36.°5C EBL 130mL CBC -WNL BMP Potassium – 5.4 mEq/L
What education should be conducted regarding post-op medications?
- New post-op pain guidelines rely less on patient-controlled analgesia (aka “pain medicine button”) than in previous years. Most facilities will have an approved standing protocol (i.e., “Multimodal analgesia and Opioid Prescribing recommendation” guideline) or standing orders. The patient must be instructed on how to rate pain using facility-approved tools (aka “pain scales”). She should also report any medication-related side effects and reinforce there is a reversal medication in case of an opioid overdose.
What are some medical and/or non-medical concerns the nurse may have at this point? If there are any, should they be brought up to the surgeon?
- The nurse may request an anti-emetic such as ondansetron 4 mg IV q 6 hrs prn nausea vomiting (N&V) since it is not uncommon post-op for the patient to have N&V. The rate of LR is a little high for such a small patient and could cause electrolyte imbalances. The nurse may also inquire about the oncologist being on the case and ask if the surgeon has discussed reconstruction with the patient yet. She may also want to ask about dressing change orders.
Natasha sleeps through the night with no complaints of pain. Lab comes to draw the ordered labs and the CNA takes vital signs. See below.
CBC HGB 7.2 g/dl HCT 21.6%
BMP Sodium 130 mEq/L Potassium 6.0 mEq/L BUN 5 mg/dL
BP 84/46 SpO2 91% on Room Air HR 109 RR 22 bpm
What should the nurse do FIRST? Is the nurse concerned about the AM labs? AM vital signs? Why or why not?
- Check the dressing and drain for bleeding (assess the patient). The patient should also sit up and allow staff to check the bed for signs of bleeding. Reinforce the dressing as needed. Record output from the drain (or review documentation of all the night’s drain output). Labs and vital signs indicate she may be losing blood.
Check the dressing and drain for BLEEDING (assess the patient). The patient should also sit up and allow staff to check the bed for signs of bleeding. Reinforce the dressing as needed. Record output from the drain (or review documentation of all the night’s drain output). Labs and vital signs indicate she may be losing blood.
What orders does the nurse anticipate from the surgeon?
- The nurse should expect an order to transfuse blood for this patient. Also, dressing reinforcement or change instructions are needed in the case of saturation)
How should the nurse address Natasha’s declaration? What alerts the nurse to a possible complication?
- First, the complication is that “Kingdom Hall” is the site of worship for Jehovah’s Witnesses. They do not accept ANY blood product, not even in emergencies. It is vital the nurse determines the patient’s affiliation and religious exceptions for medical care before moving forward. Next, employ therapeutic communication to elicit more details about Natasha’s concerns. Say things like, “tell me why you think you’re not attractive?” She may discuss reconstruction options or ask the patient to write down specific questions about this option to ask the provider later. Ask about getting family in to provide support. Seek information to give the patient about support groups and other resources available (as appropriate, ie. prosthetics, special undergarments/accessories, etc)
The surgeon orders 1 unit packed red blood cells to be infused. The nurse then goes to the patient to ask about religious affiliation and to discuss the doctor’s order. After verifying that Natasha is not a practicing Jehovah’s Witness, the nurse proceeds to prepare the transfusion.
What is required to administer blood or blood products?
- First, the patient’s CONSENT is required to give blood products. The nurse must also prepare to stay with the patient for at least the first 15 minutes of the transfusion taking a baseline set of V/S prior to infusion. Then, V/S per protocol (frequent). Education is also required. The patient should report feeling flushed, back or flank pain, shortness of breath, chest pain, chills, itching, hives. Normal saline ONLY for infusion setup and flushing: size IV 20g or higher. Always defer infusion time limits to “per policy” because this can differ vastly
How should the nurse respond to this question?
- Planning for post-op cancer treatment should have begun prior to the surgery. Ask the patient if she has discussed plans with her oncologist. Refer to any specialist documentation to see if this is mentioned. Remind the patient of the specialist’s assessment and planning information. Reinforce that testing of the tissue may change the course of treatment as well. Provide education AS PER THE PATIENT’S STATED PREFERENCE and/or resources based on what the plan includes (ie. chemotherapy, radiation, further surgery. Continually assess and reassess patient understanding. Include family and/or support with the patient’s approval.
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
References:
View the full transcript, nursing case studies.

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Europe PMC Author Manuscripts
Care plans and care planning in long term conditions: a conceptual model
The prevalence and impact of long term conditions continues to rise. Care planning for people with long term conditions has been a policy priority for chronic disease management in a number of health care systems. However, patients and providers appear unclear about the formulation and implementation of care planning. Further work in this area is therefore required to inform the development, implementation and evaluation of future care planning initiatives. We distinguish between ‘care planning’ (the process by which health care professionals and patients discuss, agree and review an action plan to achieve the goals or behaviour change of most relevance and concern to the patient) and a ‘care plan’ (a written document recording the outcome of a care planning process). We propose a typology of care planning and care plans with three core dimensions: perspective (patient or professional), scope (a focus on goals or on behaviours) and networks (confined to the professional-patient dyad or extending to the entire care network). In addition, we draw on psychological models of mediation and moderation to outline potential mechanisms through which care planning and care plans may lead to improved outcomes for both patients and the wider health care system. The proposed typology of care planning and care plans offered here, along with the model of the process by which care planning may influence outcomes, provide a useful framework for future policy developments and evaluations. Empirical work is required to explore the degree to which current care planning approaches and care plans can be described according to these dimensions, and the factors that determine which types of patients and professionals use which type of care plans.
With the burden of disease shifting to long term conditions, health systems are tasked to deliver effective, efficient, accessible and patient-centred care ( Singh and Ham, 2006 , Wagner et al., 1996 , Department of Health, 2006 ). The Chronic Care Model was developed in response to concerns about the effectiveness of primary care for people with long term conditions ( Wagner et al., 1996 , Wagner, 2001 ). The model sets out a vision in which informed patients and proactive health care teams work together within highly organised systems to achieve the highest quality of care. It has been influential in the organization of long term condition care internationally ( Bodenheimer et al., 2002b ). It recognises that all long term conditions present a “common set of challenges” to individuals and their families. It aims to support management of the “physical, psychological, and social demands” of conditions through “productive interactions” between practice teams and patients that consistently provide (a) assessments, (b) support for self-management, (c) optimisation of therapy; and (d) proactive follow-up ( Wagner et al., 1996 ).
Key potential outcomes of the Chronic Care Model include reduction in health care use and costs, and improved clinical outcomes and patient experience. For example, a broad overview of 39 studies in diabetes found that the vast majority (82%) demonstrated that interventions based on Chronic Care Model components impacted on at least one process or outcome measure, such as glycaemic control ( Bodenheimer et al., 2002b ), while a smaller number of studies (67%) found reductions in health care utilisation or costs.
There is significant interest in assessment of which aspects of the Chronic Care Model are ‘active ingredients’ ( Bodenheimer et al., 2002a ). Effective collaboration between patients and providers may be crucial, involving “providers and patients working together to define problems, set priorities, establish goals, create treatment plans and solve problems along the way” (Improving Chronic Illness Care). Such collaboration is the essence of good family practice, but achieving this consistently is a challenge, reflecting professional/patient power disparities ( May, 1992 ), differences in ‘models’ of disease and illness ( Cohen et al., 1994 ), different priorities ( Tuckett et al., 1985 ), and the varying challenges associated with different long term conditions and comorbidities.
A number of methods have been used to improve collaboration ( Lorig et al., 1999 , Kennedy et al., 2004 , Lewin et al., 2001 ). One is a formal process of ‘care planning’ and production of written ‘care plans’ recording discussions between patients and professionals, a specific element recommended within the Chronic Care Model. Broadly, care planning involves:
- Anticipatory rather than reactive discussions about patient care
- Defining roles and tasks among team members, including the patient
- Negotiating agreements that facilitate care within and across organisation
- Supporting patients to manage their own health
- Promoting shared decision making
- Promoting care that is consistent with scientific evidence and the patient’s preferences
Care planning and care plans have been implemented in health care systems including Australia, Canada, the United States, and the United Kingdom, and in contexts including respiratory disorders ( Partridge, 2004 , Gibson and Powell, 2004 ), mental health ( Department of Health, 2008 ), and palliative care ( Epstein et al., 2011 ). However, despite widespread policy interest, empirical research suggests that patients and providers are uncertain as to the exact nature of care planning and plans ( Burt et al., 2012 , Newbould et al., 2012 ). Greater conceptual clarity in this area would benefit both those implementing care planning and care plans, and researchers attempting evaluations in this field ( Craig et al., 2008 ). The aim of this review is to (a) develop a typology of care planning and care plans; (b) present a model of mechanisms by which care planning and care plans may benefit patients, and (c) clarify the outcomes which care planning and care plans might be expected to impact on, to inform future service developments and evaluations.
Scope and approach of the review
As part of a mixed methods evaluation of care planning for long term conditions in England, we undertook two different approaches to literature reviews. Firstly, we conducted a systematic search to explore current empirical knowledge in this field. We developed a search strategy including terms related to care plans and planning and long term conditions. We searched PubMed, Cochrane Library, EMBASE, CINAHL and PsycINFO for studies published up until 2011 of (a) interventions for either patients or health care providers which were intended to promote shared decision-making or any aspect of shared decision making (e.g. patient participation), and (b) interventions which included the provision of a care or action plan (whether stand-alone or as part of a wider self-management intervention). See Appendix 1 for details of our search strategy. We do not report the results here, but use located studies (both empirical and theoretical) to support the ideas outlined in this paper.
Secondly, we conducted an additional literature review to explore further how and why care planning might work or fail. Through this, we were seeking key drivers of successful care planning and underlying mechanisms through which care planning may impact on outcomes. To this end, we supplemented the findings of our systematic review by conducting searches to locate relevant additional literature (including grey literature such as policy documents from the UK, US, Canada and Australia on the implementation or evaluation of care planning and care plans; and theory and discussion papers relevant to the management of long term conditions and care planning approaches). Thus, in addition to the databases already mentioned, we searched OpenGrey ( http://www.opengrey.eu , a European repository including research reports , dissertations , and official publications), NTIS ( www.ntis.gov/ , a repository of US government-funded scientific and other information), PsycEXTRA ( www.apa.org/psycextra/ , a repository for research reports, conference presentations and policy statements in the fields of psychology, behavioral science, and health) and HMIC (a UK database combining data from the Department of Health’s Library and Information Services and the King’s Fund Information and Library Service) using terms related to “care planning” and “long term conditions”, for publications up until 2011.
Our focus was limited to care planning for long term conditions within primary care. Definitions of long term conditions vary. For example, the definition used by the English Department of Health focuses on the incurable nature of such conditions: “the definition of a long term condition is any condition that cannot be cured but can be managed by medication and/or therapy” (Department of Health). We defined long term conditions as those which require ongoing management over a period of years, including non-communicable diseases (e.g. cancer and cardiovascular disease), communicable diseases (e.g. HIV/AIDS), certain mental disorders (e.g. schizophrenia, depression), and ongoing impairments in structure (e.g. blindness, joint disorders). This definition acknowledges the work often required for people to manage such conditions.
In this paper, we present a ‘theory map’ of care planning which focuses on the identification of:
- types of care plans and care planning
- anticipated relationships between mechanisms and outcomes of care planning, and
- potential outcomes of care planning
Types of care planning
‘care planning’ and ‘care plans’.
We make a distinction between ‘care planning’ (verb: the process by which health care professionals and patients discuss, agree and review an action plan to achieve the goals or behaviour change of most relevance and concern to the patient), and a ‘care plan’ (noun: a written document recording the outcome of a care planning process). Data from the English National GP Patient Survey suggest that 84% of patients with a long-term condition report some care planning discussion during the last 12 months, but only 12% report being told they had a care plan ( Burt et al., 2012 ).
Care plans may function as extensions of the medical record, as a guide to action, and/or as a contract between patients, providers and the health care system. As an extension of conventional medical records, they may be used to record additional relevant details for long term condition care. For example, the Australian Team Care Arrangement records details of treatment decisions to ensure all those involved in care are aware of their basis, which may improve management and informational continuity ( Haggerty et al., 2003 ). As guides to action, they may stimulate forward thinking and a focus on goals for patients and professionals. As a contract, they may include mechanisms to ensure actions are undertaken, for example by providing incentives to act. Examples include advance decisions within end of life care, which might be legally binding, and care plans enabling access to resources e.g. personal health budgets in the United Kingdom ( Harvey, 2010 ).
As noted above, the process of care planning may not necessarily result in a written care plan. From a policy perspective, the distinction between ‘care plans’ and ‘care planning’ can be represented in a 2×2 typology ( Figure 1 ) ( Burt et al., 2012 ). Quadrant D represents poor quality care, with no care planning and no care plan. In Quadrant C, care planning has taken place but there is no formal ‘care plan’. This probably represents the majority of care for long term conditions in England at present. Quadrant A represents the ‘gold standard’; care planning supports production of a written care plan, which in turn feeds back into care planning. Box B might reflect ‘gaming’: ( Doran et al., 2008 ) a ‘care plan’ is produced, but without a full care planning process. This behaviour may occur if care plans are poorly defined, if they lack clarity of purpose or if their implementation is not supported by suitable training and guidance. Additionally, if care plans are mandated or incentivised (either financially or through access to other resources), but are perceived unfavourably by professionals, care plans may be produced without care planning. A further influence may be the use of standardised care plan templates, which could constrain the recording of a comprehensive and personalised care planning discussion.

The use of care plans
‘Care plans’ or ‘action plans’ have been described in a number of contexts. In respiratory disorders, patient-held care plans are focussed on responses to exacerbations, and provide specific instructions for daily treatment, step-up treatment in the event of deterioration, and seeking urgent medical consultation ( Gibson and Powell, 2004 ). In severe mental illness, care plans combine both instruction and needs assessment, focussing particularly on anticipation of crisis situations ( Department of Health, 2007 ). In diabetes, the use of care plans has a more open-ended aim to encourage partnership-building, emphasising the importance of both the professional perspective on ‘disease’ and the ideas and concerns of the patient ( Zwar et al., 2007 ).
Care plans are used in health care systems including the UK, US, Canada and Australia. In Australia, care plans have a needs assessment focus, and were originally defined as “a written, comprehensive and longitudinal plan of action that sets out the health service needs of a patient and the types of services and supports needed to meet those needs” ( Zwar et al., 2008 ). Some types of care plans in Australia (“Team Care Arrangements”) were modified to focus on coordination and team-working for patients under multidisciplinary care ( Vagholkar et al., 2007 , Zwar et al., 2008 ). In the US, Medicare and Medicaid certified nursing homes have Minimum Data Set requirements that include the development and modification of care plans describing how to meet each resident’s needs ( Unwin et al., 2010 ). Within the UK, care plans form part of the patient choice agenda; all patients with long term conditions are expected to participate in explicit care planning discussions to enhance self-management, including the setting of personal goals and action planning ( Department of Health, 2009 ).
A typology of care planning and care plans
In an effort to develop conceptual clarity in this area, we present a typology which can be used to categorise and describe care planning and care plans ( Figure 2 ). Firstly, it is important to make the distinction between care planning for conditions and care planning for people . Care planning policy often emphasises the importance of taking account of the entirety of a person’s conditions, circumstances, attitudes and preferences in developing an effective care plan. Multimorbidity among long term conditions is common ( Valderas et al., 2009 ). Patients with multiple long term conditions report difficulties in determining priorities among conditions and their management, and managing multiple conditions can lead to a significant treatment burden ( Bayliss et al., 2007b , Lin et al., 2006 , Fried et al., 2008b ). Whilst such concerns may drive the formulation of care planning policy, in practice, care plans have often been developed and implemented on a condition-specific basis (e.g. for diabetes). We propose a typology with three core dimensions that takes into account these differences in emphasis.

1. Perspective: Is the focus on the patient’s or the professional’s perspective?
2. Scope: Is the focus on discrete behaviours or on broader goals and values?
3. Network: Is the focus on patient-professional dyad or the wider care system?
The first dimension ( perspective ) represents the degree to which the process of development and the content of the care plan reflects the perspective of the professional (with the patient as the ‘target’) or the perspective of the patient (with the professional as the ‘target’). In Australia, patient accounts suggest care plans were seen as being about the professional, and frequently documented ‘clinical goals and activities about which they had no expertise’ ( Shortus et al., 2007 ). Self-management policies aimed at empowering patients have been criticised for ignoring the complexities and impact of professional power and the gatekeeping role within the doctor-patient relationship ( Tang and Anderson, 1999 , Wilson, 2001 ). Whilst care planning policy sets out a patient-driven process, supported by the professional, the Australian example shows questions may be asked about leads the decision-making. It cannot be assumed that introduction of care plans or care planning will immediately impact on existing and longstanding power relationships.
The second dimension ( scope ) reflects the degree to which the plan is focused on discrete behaviours and items (e.g. steps to take in an exacerbation), or on broader goals (such as a reduction in HbA1C at the next diabetes review). The content of care plan templates may be a key driver of their scope. An analysis of primary care consultations in the UK suggested that the use of standardised computer templates led to self-management dialogue being framed around discrete behaviours ( Blakeman et al., 2011 ).
Combining these two dimensions creates four types of care plans:
- Professional-centred/behaviour-focussed: e.g. written asthma self-management plans
- Professional-centred/goal-focussed: e.g. depression treatment goals in stepped care
- Patient-centred/goal-focussed: e.g. advance directives in end of life care, attending a key social event
- Patient-centred/behavior-focussed: e.g. healthy eating plans, talking to family about the impact of a condition
A third dimension ( network ) can be added to this typology. This describes whether care plans are focused on the core professional-patient dyad (e.g. patient and GP), or a wider care network (e.g. a multi-disciplinary team, and/or social networks) ( Rogers et al., 2011 ).
Mechanisms of care planning
To explore mechanisms, we drew on the mediation-moderation model from psychology. In Baron and Kenny’s influential formulation, a mediator is a “transformation process” by which the effects of stimuli impact on a behaviour or health outcome ( Baron and Kenny, 1986 ). A mediator variable explains, in full or part, the relationship between two other variables. For example, care plans may improve health outcomes if they increase shared decision making. A moderator is “a qualitative (e.g. sex, race, class) or quantitative (e.g., level of reward) variable that affects the direction and/or strength of the relation between an independent or predictor variable and a dependent or criterion variable” ( Baron and Kenny, 1986 ). The definition and investigation of moderators requires understanding the circumstances or groups where an explanatory variable most strongly influences an outcome variable. For example, care planning may be more effective in patients with long term conditions with a significant burden of treatment ( Department of Health, 2006 ). Mediators and moderators may interact in various complex ways; identification and understanding of even the basic underlying relationships has the potential to optimise the design of care plans of most utility and relevance to patients and professionals.
Mediators of change in care planning
We suggest three core mediators of relevance to care planning: participation and shared decision-making, supporting self-management behaviour change, and coordinating treatment ( Figure 3 ).

Participation and shared decision making
Patient-centred care encourages (a) shared control of the consultation, decisions about interventions or management of the health problems with the patients, and/or (b) a focus in the consultation on the patient as a whole person who has individual preferences situated within social contexts ( Lewin et al., 2001 ). There may be different approaches to patient-centredness, and evidence suggests variable associations with patient outcomes: for example, approaches which seek to “activate” the patient rather than simply take their perspective have been more consistently associated with good health outcomes ( Michie et al., 2003 ). Some innovations to promote patient-centred care have been criticised for superficiality, with insufficient grounding in the key aims of improving patient-doctor relationships and facilitating participation and shared-decision making ( Epstein and Street, 2011 ).
Decision-making may be seen as a staged sequence of “information exchange, deliberation or discussion of treatment preferences, and deciding on the treatment to implement” ( Levinson et al., 2005 ). Key components of patient participation include: 1) the patient’s contribution to the direction of dialogue, 2) their influence in setting the agenda, 3) their share in the reasoning process, 4) their influence in the decision-making, and the 5) emotional reciprocity within encounters ( Perakyla and Ruusuvuori, 2007 ). Care planning initiatives such as Year of Care in the UK have been specifically built on a patient-centred approach, with the aim of fostering patient participation and shared decision making through system re-design and practitioner and patient training ( National Diabetes Support Team, 2008 ). Research suggests, however, that many decisions in health care are still not shared ( Levinson et al., 2005 , Murray et al., 2007 ), and there remain a number of questions about peoples’ desire to assume an identity of the active, informed patient ( Sinding et al., 2010 ).
Supporting self- management behaviour change
Care planning should support changes in behavior that result from patients being more involved in management of their conditions. Incorporating theories of behavior change strengthens the design, implementation and evaluation of interventions such as care planning ( Abraham et al., 2009 , Cane et al., 2012 ). Care planning involves a number of potential influences on behavior, and may require a variety of techniques of behavior change. For example, the United Kingdom introduced health trainers to improve the delivery of preventive care and health behaviour change in deprived communities. Those focussed on individual behaviour change often use Personal Health Plans, designed to list core client goals which can be worked on with the trainer. These plans were explicitly linked with behaviour change techniques developed from a psychological framework, including goal-setting, self-monitoring and building social support ( British Psychological Society, 2008 ). There is developing interest in other techniques to support people with long-term conditions to sustain behavior change, such as motivational interviewing ( Scott, 2010 ). However, the efficacy, skills and competencies required to facilitate a meaningful and comprehensive care planning process leading to effective behavior change may be challenging for health professionals to develop without sufficient support and time.
Coordinating treatment
Care coordination is the need to process and integrate information relevant to patient care. It reflects both variability and complexity ( Perrow, 1967 ). Variability refers to the diversity of patient problems that present; complexity is the degree to which decision making algorithms can be used to determine necessary actions for task performance. Tasks which demand high levels of information processing are best performed by teams in which there is a high level of interdependent working among members ( Thompson, 1967 ). However, co-ordination of care is often poor, and teams may need processes and structures to facilitate sharing of information. Care planning might provide the basis for shared patient information systems that allow each person to access information on the care provided by others.
Moderators of the effects of care planning
Potential moderators of the effect of care planning include patient level factors (clinical, psychosocial and socio-demographic) as well as system level issues (clinical information systems, templates and protocols; and health care team climate).
Clinical issues
There are significant commonalities between long term conditions in decision making, self-management, and treatment co-ordination requirements. However, important differences may moderate the impact of care planning. For example, diabetes can remain asymptomatic for many years: a lack of explicit symptoms may make care planning appear of low priority for both patients and professionals. In symptomatic disease, the greater ‘visibility’ of the condition may stimulate interest in methods to improve self-management. Care planning approaches may move in and out of perceived relevance, depending on the current stage and severity of a condition: for example, COPD management plans are usually invoked only for acute exacerbations ( Turnock et al., 2005 ). Perhaps the most important clinical moderator for care planning is in meeting the needs of patients with multimorbidity, who represent a large proportion of the workload in primary care ( Salisbury et al., 2011 ). Such patients frequently face difficult decisions about priorities among conditions ( Bayliss et al., 2007a , Fried et al., 2008a ), and time restrictions in primary care may make it difficult to meet their needs for support and information ( Bower et al., 2011 ). Care planning approaches implemented to date are frequently disease-specific: completing a diabetes care plan template for someone with multimorbidity may not be the most appropriate way of meeting their needs.
Psychosocial issues
There is extensive evidence that preferences for shared decision making vary by patient demography ( Cullati et al., 2011 , Say et al., 2006 , Protheroe et al., 2012 ). It remains a key research question whether the effectiveness of care plans will be lower in those groups who routinely prefer professionals to lead, or whether intervention in these groups will lead to enhanced outcomes, as they have greatest capacity to benefit. Variations in patient competency to participate in care planning processes may affect uptake and outcomes.
Much of the consideration of care planning focuses on the individual patient, in consultation with individual or teams of professionals. However, support for long term conditions does not occur at an individual level alone, and often involves significant ‘networks of support’ including family, friends, professionals outside health services, and community groups ( Rogers et al., 2011 ). Effective care planning may therefore place a greater emphasis on events and support outside of formal health care services.
Sociodemographic issues
A number of sociodemographic issues may moderate the effect of care planning on outcomes. In an analysis of whether care planning discussions had helped improve management of a health problem, benefits of care planning were reported more by men and older patients, as well as those reporting better access to and continuity of care ( Burt et al., 2012 ). Other relevant factors may include level of deprivation, ethnic background, language, and carer responsibilities, although empirical evidence is currently lacking.The capacity of patients to benefit may also be moderated by health literacy ( Nutbeam, 2008 ). Health literacy is the “degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions” ( Institute of Medicine, 2004 ). Low health literacy is associated with a range of markers of poor health including: higher rates of long-term conditions, poor self-management, poorer understanding of one’s medical condition and adherence to medical instructions, reduced responsiveness to health education and higher health care costs ( Berkman, 2011 ). In addition, low health literacy may be associated with higher mortality in older adults. This may have important implications for the delivery and impact of care planning in those with poorer health literacy ( Bostock and Steptoe, 2012 ).
Clinical information systems, templates and protocols
Potential constraints on the process of care planning and the production of care plans arising from the use of templates or particular clinical information systems have already been mentioned. Patient data systems may be organized around service needs and data monitoring requirements rather than patient experience of illness ( Procter et al., 2013 ). An ethnography of computer templates in chronic disease management concluded that their use in consultations contributes to “how disease is defined; how care is delivered; what it means to be a patient; and what it means to be a clinician” ( Swinglehurst et al., 2012 ). Effective individualized care planning and care plans are likely to be influenced by the nature of the clinical system, including for example whether clinicians are prompted to review the implementation of the plan at a later date.
Health care team climate
Climate has been defined as a team’s shared perceptions of organisational policies, practices and procedures ( Anderson and West, 1998 ). There is evidence that strong team orientation and perceptions of supportive team interactions in primary care teams may impact on health status of older patients, with stronger effects in more serious diagnoses (e.g. cancer, COPD) ( Roblin et al., 2011 ). Studies of primary care teamwork highlight that developing trust and respect is necessary for co-operation, and there are potentially problematic issues within groups of GPs, and between GPs and other health professionals, concerning the distribution of practice workload and conflicts about roles ( Belanger and Rodriguez, 2008 ). The effective uptake and implementation of care planning and care plans may in part be moderated by the quality of teamwork within a provider, especially in patients with multimorbidity and significant multidisciplinary input.
Process and health outcomes of care planning
Quality of health care for individuals has been defined as “whether individuals can access the health structures and processes of care which they need and whether the care received is effective” ( Campbell et al., 2000 ). This approach clearly differentiates the structure of health care (through which care is delivered and received) from the process of health care (the care that is given). Outcome of care is a result of the interaction between individuals and the health care system; a consequence rather than a part of care ( Campbell et al., 2000 ). Through improving the processes of care, it is anticipated that care planning could contribute to improved health outcomes including health status, user experience and costs of care. However, there is currently little evidence on the impact of the care planning process as a whole on health or other outcomes, although the beneficial effects of many of the components of care planning are better understood ( Graffy et al., 2009 ). Mapping aspects of care planning onto the framework of the Chronic Care Model, we highlight five measurable outcomes of interest that may support the development of an evidence base (Improving Chronic Illness Care).
Firstly, supporting self-management is at the core of care planning. The Chronic Care Model highlights the importance of empowering and preparing patients to manage their health. Measurable outcomes of care planning for self-management may therefore include an assessment of engagement in healthy behaviours, self-efficacy (a perception of confidence to complete activities) ( Lorig et al., 1989 ), management of medication regimes, and perceived barriers to self-management.
Secondly, care planning involves the provision of support for decision-making. Within the Chronic Care Model, the aspiration is to promote care which is consistent with scientific evidence and patient preferences, including the sharing of guidelines and information with patients to encourage participation. Measurable outcomes of care planning in this domain could include patient perceptions of the degree to which their health care professional is ‘autonomy supportive’ as opposed to ‘controlling’. Autonomy support has been defined as providing patients with effective options for treatment, supporting patient initiatives, and minimising professional judgment ( Williams et al., 1996 ).
Thirdly, care plans that are focussed on multiple professionals may make explicit the roles and tasks of each ( Zwar et al., 2008 , Zwar et al., 2007 ). The planning aspect of care plans may facilitate follow up, and including values and preferences may make care more responsive to patient’s background and preferences. This highlights the Chronic Care Model’s call for careful design of the delivery system, including the clear definition of roles and distribution of tasks among team members (including the patient), and regular follow-up by the health care team. Assessment of the impact of care planning on this domain may include patient experience of care, including in particular perceptions of continuity, coordination and follow-up (see Haggerty et. al 2012 for a recent generic measure of continuity of care ( Haggerty et al., 2012 )).
Fourthly, care plans that are focussed on multiple professionals may lead to the development of mechanisms to co-ordinate care at an organisational level ( Zwar et al., 2008 , Zwar et al., 2007 ). The Chronic Care Model suggests that there is a need to foster the right culture, organization and mechanisms to promote safe, high quality care, which includes the development of agreements to facilitate coordination in and across organisations. Assessment of changes in team effectiveness and cross-organisational working (using, for example, the Team Climate Inventory ( Anderson and West, 1998 , Anderson and West, 1999 )) and overall patient experience (such as assessed by the GP Patient Survey (Department of Health)) could be useful here.
Finally, the Chronic Care Model requires high quality clinical information systems, which are also needed to facilitate care planning, via the effective recording, retrieval and sharing of the content of plans over time. The developing field of electronic health records has clear implications for care planning processes; as already noted, templates may restrict discussions between providers and patients, but electronic data shared across health care teams and organisations may also streamline the recording and reviewing of care planning discussions and care plans. Measurable outcomes of the impact of care planning on effective use of clinical systems could include patient assessment of information provision and coordination of care, for example as in the follow up/coordination scales of the PACIC (Patient Assessment of Chronic Illness Care) instrument ( Glasgow et al., 2005 , Rick et al., 2012 ).
There is significant policy interest in the potential of care plans and care planning. However, empirical evidence suggests that, at ground level, there remains a lack of specificity concerning the nature of care plans and care planning, as well as insufficient consideration of their likely influence on processes; anticipated outcomes; and factors which might influence benefit. The proposed typology of care planning offered here, along with the model of the process by which care planning may influence outcomes, provide a useful framework for future policy developments and evaluations. Empirical work is required to explore the degree to which current care plans can be described according to these dimensions, and the factors that determine which types of patients and professionals use which type of care plans.
Acknowledgements
We thank Anne Rogers and Anne Kennedy for their advice throughout this project. We also thank two reviewers for their extremely thoughtful suggestions, which greatly improved the manuscript.
Financial Support: Funding body: Department of Health Policy Research Programme Reference Number: 077/0016. This is an independent report commissioned and funded by the Policy Research Programme in the Department of Health. The views expressed are not necessarily those of the Department of Health.
Appendix 1. Search strategy
The following is the specific search strategy used in PubMed. This search strategy was applied to the other databases (Cochrane Library, EMBASE, CINAHL and PsycINFO).
#1 patient care planning[mh:noexp] or advance care planning[mh:noexp] or patient participation[mh:noexp] or care plan*[tiab] or care-plan*[tiab] or action plan*[tiab] or action-plan*[tiab] or management plan*[tiab] or management-plan*[tiab] or management program*[tiab] or personal health plan*[tiab] or personal-health-plan*[tiab] or self manag*[tiab] or self-manag*[tiab] or self car*[tiab] or self-car*[tiab]
#2 chronic disease [mh] or chronic disease[tiab] or chronic-disease[tiab] or (ongoing[tiab] adj (illness*[tiab] or disease[tiab] or condition*[tiab])) or (ongoing[tiab] adj health adj (illness*[tiab] or disease[tiab] or condition*[tiab])) or (persistent[tiab] adj (illness*[tiab] or disease[tiab] or condition*[tiab])) or (long[tiab] adj term adj (illness*[tiab] or disease[tiab] or condition*[tiab]))
Conflicts of Interest: None.
This article has been accepted for publication and will appear in a revised form, subsequent to or editorial input by Cambridge University Press, in Primary Health Care Research & Development published by Cambridge University Press. Copyright is held by Cambridge University Press. The definitive version will be available from Primary Health Care Research & Development
- ABRAHAM C, KELLY M, WEST R, MICHIE S. The UK National Institute for Health and Clinical Excellence public health guidance on behaviour change: A brief introduction. Psychology Health Med. 2009; 14 :1–8. [ PubMed ] [ Google Scholar ]
- ANDERSON NR, WEST MA. Measuring climate for work group innovation: development and validation of the team climate inventory. Journal of organizational behavior. 1998; 19 :235–258. [ Google Scholar ]
- ANDERSON NR, WEST MA. Manual and Users’ Guide. NFER-Nelson; Windsor, UK: 1999. The Team Climate Inventory (Revised) [ Google Scholar ]
- BARON RM, KENNY DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986; 51 :1173–82. [ PubMed ] [ Google Scholar ]
- BAYLISS EA, BOSWORTH HB, NOEL PH, WOLFF JL, DAMUSH TM, MCIVER L. Supporting self-management for patients with complex medical needs: recommendations of a working group. Chronic Illness. 2007a; 3 :167–175. [ PubMed ] [ Google Scholar ]
- BAYLISS EA, ELLIS JL, STEINER JF. Barriers to self-management and quality-of-life outcomes in seniors with multimorbidities. Ann Fam Med. 2007b; 5 :395–402. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- BELANGER E, RODRIGUEZ C. More than the sum of its parts? A qualitative research synthesis on multi-disciplinary primary care teams. J Interprof Care. 2008; 22 :587–97. [ PubMed ] [ Google Scholar ]
- BERKMAN ND, SHERIDAN SL, DONAHUE KE, HALPERN DJ, VIERA A, CROTTY K, VISWANATHAN M. Health literacy interventions and outcomes: An updated systematic review. Agency for Healthcare Research and Quality; Rockville, MD: 2011. (Evidence Report/Technology Assessment, No. 199). [ PMC free article ] [ PubMed ] [ Google Scholar ]
- BLAKEMAN T, CHEW-GRAHAM C, REEVES D, ROGERS A, BOWER P. The Quality and Outcomes Framework and self-management dialogue in primary care consultations: a qualitative study. British Journal of General Practice. 2011; 61 :e666–e673. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- BODENHEIMER T, WAGNER EH, GRUMBACH K. Improving primary care for patients with chronic illness. JAMA. 2002a; 288 :1775–1779. [ PubMed ] [ Google Scholar ]
- BODENHEIMER T, WAGNER EH, GRUMBACH K. Improving primary care for patients with chronic illness - The chronic care model, part 2. JAMA. 2002b; 288 :1909–1914. [ PubMed ] [ Google Scholar ]
- BOSTOCK S, STEPTOE A. Association between low functional health literacy and mortality in older adults: longitudinal cohort study. BMJ. 2012; 344 :e1602. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- BOWER P, MACDONALD W, HARKNESS E, GASK L, KENDRICK T, VALDERAS JM, DICKENS C, BLAKEMAN T, SIBBALD B. Multimorbidity, service organization and clinical decision making in primary care: a qualitative study. Family Practice. 2011; 28 :579–87. [ PubMed ] [ Google Scholar ]
- BRITISH PSYCHOLOGICAL SOCIETY . Improving Health: Changing Behaviour. Department of Health; London: 2008. (NHS Health Trainer Handbook). [ Google Scholar ]
- BURT J, ROLAND M, PADDISON C, REEVES D, CAMPBELL J, ABEL G, BOWER P. Prevalence and benefits of care plans and care planning for people with long-term conditions in England. J Health Serv Res Policy. 2012; 17 (Suppl 1):64–71. [ PubMed ] [ Google Scholar ]
- CAMPBELL SM, ROLAND MO, BUETOW SA. Defining quality of care. Soc Sci Med. 2000; 51 :1611–25. [ PubMed ] [ Google Scholar ]
- CANE J, O’CONNOR D, MICHIE S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implementation Science. 2012; 7 :37. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- COHEN MZ, TRIPP-REIMER T, SMITH C, SOROFMAN B, LIVELY S. Explanatory models of diabetes: patient practitioner variation. Soc Sci Med. 1994; 38 :59–66. [ PubMed ] [ Google Scholar ]
- CRAIG P, DIEPPE P, MACINTYRE S, MICHIE S, NAZARETH I, PETTICREW M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008; 337 :a1655. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- CULLATI S, COURVOISIER DS, CHARVET-BERARD AI, PERNEGER TV. Desire for autonomy in health care decisions: a general population survey. Patient Educ Couns. 2011; 83 :134–8. [ PubMed ] [ Google Scholar ]
- DEPARTMENT OF HEALTH [Accessed 18 December 2012]; The GP Patient Survey [Online] Available: http://www.gp-patient.co.uk/
- DEPARTMENT OF HEALTH [Accessed 07/06/2012]; Millions of patients set to beenfit from a modern NHS [Online] Available: http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/MediaCentre/Pressreleases/DH_125042 .
- DEPARTMENT OF HEALTH . Our health, our care, our say: a new direction for community services. Department of Health; London: 2006. [ PubMed ] [ Google Scholar ]
- DEPARTMENT OF HEALTH . Making the CPA work for you. Department of Health; London: 2007. [ Google Scholar ]
- DEPARTMENT OF HEALTH . Refocusing the Care Programme Approach: Policy and Positive Practice Guidance. Department of Health; London: 2008. [ Google Scholar ]
- DEPARTMENT OF HEALTH . Supporting People with Long Term Conditions : Commissioning Personalised Care Planning - a guide for commissioners. Department of Health; London: 2009. [ Google Scholar ]
- DORAN T, FULLWOOD C, REEVES D, GRAVELLE H, ROLAND M. Exclusion of patients from pay-for-performance targets by English physicians. N Engl J Med. 2008; 359 :274–84. [ PubMed ] [ Google Scholar ]
- EPSTEIN AS, VOLANDES AE, O’REILLY EM. Building on Individual, State, and Federal Initiatives for Advance Care Planning, an Integral Component of Palliative and End-of-Life Cancer Care. J Oncol Pract. 2011; 7 :355–9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- EPSTEIN RM, STREET RL. The Values and Value of Patient-Centered Care. Ann Fam Med. 2011; 9 :100–103. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- FRIED TR, MCGRAW S, AGOSTINI JV, TINETTI ME. Views of older persons with multiple morbidities on competing outcomes and clinical decision-making. Journal of the American Geriatrics Society. 2008a; 56 :1839–1844. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- FRIED TR, MCGRAW S, AGOSTINI JV, TINETTI ME. Views of older persons with multiple morbidities on competing outcomes and clinical decision-making. J Am Geriatr Soc. 2008b; 56 :1839–44. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- GIBSON PG, POWELL H. Written action plans for asthma: an evidence-based review of the key components. Thorax. 2004; 59 :94–99. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- GLASGOW RE, WAGNER EH, SCHAEFER J, MAHONEY LD, REID RJ, GREENE SM. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC) Med Care. 2005; 43 :436–44. [ PubMed ] [ Google Scholar ]
- GRAFFY J, EATON S, STURT J, CHADWICK P. Personalized care planning for diabetes: policy lessons from systematic reviews of consultation and self-management interventions. Primary Health Care Research & Development. 2009; 10 :210–222. [ Google Scholar ]
- HAGGERTY JL, REID RJ, FREEMAN GK, STARFIELD BH, ADAIR CE, MCKENDRY R. Continuity of care: a multidisciplinary review. BMJ. 2003; 327 :1219–1221. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- HAGGERTY JL, ROBERGE D, FREEMAN GK, BEAULIEU C, BRÉTON M. Validation of a Generic Measure of Continuity of Care: When Patients Encounter Several Clinicians. Ann Fam Med. 2012; 10 :443–451. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- HARVEY J. Key elements of personalised care planning in long term conditions and personal health budgets. NHS; London: 2010. [ Google Scholar ]
- IMPROVING CHRONIC ILLNESS CARE [Accessed 08/08/12]; The Chronic Care Model [Online] Available: http://www.improvingchroniccare.org/index.php?p=The_Chronic_Care_Model&s=2 .
- INSTITUTE OF MEDICINE . Health literacy: a prescription to end confusion. Institute of Medicine; Washington DC: 2004. [ Google Scholar ]
- KENNEDY AP, NELSON E, REEVES D, RICHARDSON G, ROBERTS C, ROBINSON A, ROGERS AE, SCULPHER M, THOMPSON DG. A randomised controlled trial to assess the effectiveness and cost of a patient orientated self management approach to chronic inflammatory bowel disease. Gut. 2004; 53 :1639–1645. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- LEVINSON W, KAO A, KUBY A, THISTED RA. Not all patients want to participate in decision making. A national study of public preferences. J Gen Intern Med. 2005; 20 :531–5. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- LEWIN SA, SKEA ZC, ENTWISTLE V, ZWARENSTEIN M, DICK J. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database of Systematic Reviews. 2001:CD003267. [ PubMed ] [ Google Scholar ]
- LIN EH, KATON W, RUTTER C, SIMON GE, LUDMAN EJ, VON KORFF M, YOUNG B, OLIVER M, CIECHANOWSKI PC, KINDER L, WALKER E. Effects of enhanced depression treatment on diabetes self-care. Ann Fam Med. 2006; 4 :46–53. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- LORIG K, SELEZNICK M, LUBECK D, UNG E, CHASTAIN R, HOLMAN H. The beneficial outcomes of the arthritis self-management course are not adequately explained by behaviour change. Arthritis Rheum. 1989; 32 :91–95. [ PubMed ] [ Google Scholar ]
- LORIG KR, SOBEL DS, STEWART AL, BROWN BW, JR., BANDURA A, RITTER P, GONZALEZ VM, LAURENT DD, HOLMAN HR. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999; 37 :5–14. [ PubMed ] [ Google Scholar ]
- MAY C. Individual Care? Power and Subjectivity in Therapeutic Relationships. Sociology. 1992; 26 :589–602. [ Google Scholar ]
- MICHIE S, MILES J, WEINMAN J. Patient-centredness in chronic illness: what is it and does it matter? Patient Educ Couns. 2003; 51 :197–206. [ PubMed ] [ Google Scholar ]
- MURRAY E, POLLACK L, WHITE M, LO B. Clinical decision-making: Patients’ preferences and experiences. Patient Educ Couns. 2007; 65 :189–96. [ PubMed ] [ Google Scholar ]
- NATIONAL DIABETES SUPPORT TEAM . Getting to Grips with the Year of Care: A Practical Guide. National Diabetes Support Team; London: 2008. [ Google Scholar ]
- NEWBOULD J, BURT J, BOWER P, BLAKEMAN T, KENNEDY A, ROGERS A, ROLAND M. Experiences of care planning in England: interviews with patients with long term conditions. BMC Family Practice. 2012:13. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- NUTBEAM D. The evolving concept of health literacy. Soc Sci Med. 2008; 67 :2072–8. [ PubMed ] [ Google Scholar ]
- PARTRIDGE MR. Written asthma action plans. Thorax. 2004; 59 :87–8. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- PERAKYLA A, RUUSUVUORI J. Components of participation in health care consultations: A conceptual model for research. In: COLLINS S, BRITTEN N, RUUSUVUORI J, THOMPSON A, editors. Patient Participation in Health Care Consultations: Qualitative Perspectives. Open University Press; Maidenhead: 2007. [ Google Scholar ]
- PERROW C. A framework for the comparative analysis of complex organizations. American Sociological Review. 1967; 32 :194–208. [ Google Scholar ]
- PROCTER S, WILSON PM, BROOKS F, KENDALL S. Success and failure in integrated models of nursing for long term conditions: Multiple case studies of whole systems. Int J Nurs Stud. 2013; 50 :632–43. [ PubMed ] [ Google Scholar ]
- PROTHEROE J, BROOKS H, CHEW-GRAHAM C, GARDNER C, ROGERS A. ‘Permission to participate?’ : A qualitative study of participation in patients from differing socio-economic backgrounds. J Health Psychol. 2012 [ PubMed ] [ Google Scholar ]
- RICK J, ROWE K, HANN M, SIBBALD B, REEVES D, ROLAND M, BOWER P. Psychometric properties of the patient assessment of chronic illness care measure: acceptability, reliability and validity in United Kingdom patients with long-term conditions. BMC Health Serv Res. 2012; 12 :293. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- ROBLIN DW, HOWARD DH, JUNLING REN, BECKER ER. An evaluation of the influence of primary care team functioning on the health of Medicare beneficiaries. Med Care Res Rev. 2011; 68 :177–201. [ PubMed ] [ Google Scholar ]
- ROGERS A, VASSILEV I, SANDERS C, KIRK S, CHEW-GRAHAM C, KENNEDY A, PROTHEROE J, BOWER P, BLICKEM C, REEVES D, KAPADIA D, BROOKS H, FULLWOOD C, RICHARDSON G. Social networks, work and network-based resources for the management of long-term conditions: a framework and study protocol for developing self-care support. Implement Sci. 2011; 6 :56. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- SALISBURY C, JOHNSON L, PURDY S, VALDERAS J, MONTGOMERY A. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. British Journal of General Practice. 2011; 61 :e12–e21. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- SAY R, MURTAGH M, THOMSON R. Patients’ preference for involvement in medical decision making: a narrative review. Patient Educ Couns. 2006; 60 :102–14. [ PubMed ] [ Google Scholar ]
- SCOTT G. Motivational interviewing. 2: How to apply this approach in nursing practice. Nursing Times. 2010; 106 :21–2. [ PubMed ] [ Google Scholar ]
- SHORTUS TD, MCKENZIE SH, KEMP LA, PROUDFOOT JG, HARRIS MF. Multidisciplinary care plans for diabetes: how are they used? Med J Aust. 2007; 187 :78–81. [ PubMed ] [ Google Scholar ]
- SINDING C, HUDAK P, WIERNIKOWSKI J, ARONSON J, MILLER P, GOULD J, FITZPATRICK-LEWIS D. “I like to be an informed person but…” negotiating responsibility for treatment decisions in cancer care. Soc Sci Med. 2010; 71 :1094–1101. [ PubMed ] [ Google Scholar ]
- SINGH D, HAM C. Improving care for people with long-term conditions: a review of UK and international frameworks. University of Birmingham; NHS Institute for Innovation and Improvement; Birmingham: 2006. [ Google Scholar ]
- SWINGLEHURST D, GREENHALGH T, ROBERTS C. Computer templates in chronic disease management: ethnographic case study in general practice. BMJ Open. 2012; 2 :e001754. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- TANG SY, ANDERSON JM. Human agency and the process of healing: lessons learned from women living with a chronic illness--‘re-writing the expert’ Nurs Inq. 1999; 6 :83–93. [ PubMed ] [ Google Scholar ]
- THOMPSON JD. Organizations in Action. McGraw-Hill; New York: 1967. [ Google Scholar ]
- TUCKETT D, BOULTON M, OLSON C, WILLIAMS A. Meetings Between Experts: An Approach to Sharing Ideas in Medical Consultations. Tavistock Publications; London: 1985. [ Google Scholar ]
- TURNOCK A, WALTERS H, WALTERS J, WOOD-BAKER R. Action plans for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews [Online] 2005 Available: http://www.mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD005074/frame.html . [ PubMed ]
- UNWIN BK, PORVAZNIK M, SPOELHOF GD. Nursing home care: part I. Principles and pitfalls of practice. Am Fam Physician. 2010; 81 :1219–27. [ PubMed ] [ Google Scholar ]
- VAGHOLKAR S, HERMIZ O, ZWAR NA, SHORTUS T, COMINO EJ, HARRIS M. Multidisciplinary care plans for diabetic patients: what do they contain? Aust Fam Physician. 2007; 36 :279–82. [ PubMed ] [ Google Scholar ]
- VALDERAS JM, STARFIELD B, SIBBALD B, SALISBURY C, ROLAND M. Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009; 7 :357–63. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- WAGNER EH. Meeting the needs of chronically ill people. BMJ. 2001; 323 :945–6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- WAGNER EH, AUSTIN BT, MICHAEL VON K. Organizing Care for Patients with Chronic Illness. The Milbank Quarterly. 1996; 74 :511–544. [ PubMed ] [ Google Scholar ]
- WILLIAMS GC, GROW VM, FREEDMAN ZR, RYAN RM, DECI EL. Motivational predictors of weight loss and weight-loss maintenance. J Pers Soc Psychol. 1996; 70 :115–26. [ PubMed ] [ Google Scholar ]
- WILSON PM. A policy analysis of the Expert Patient in the United Kingdom: Self-care as an expression of pastoral power? Health and Social Care in the Community. 2001; 9 :134–142. [ PubMed ] [ Google Scholar ]
- ZWAR N, HASAN I, HERMIZ O, VAGHOLKAR S, COMINO E, HARRIS M. Multidisciplinary care plans and diabetes--benefits for patients with poor glycaemic control. Aust Fam Physician. 2008; 37 :960–2. [ PubMed ] [ Google Scholar ]
- ZWAR NA, HERMIZ O, COMINO EJ, SHORTUS T, BURNS J, HARRIS M. Do multidisciplinary care plans result in better care for patients with type 2 diabetes? Aust Fam Physician. 2007; 36 :85–9. [ PubMed ] [ Google Scholar ]

NurseStudy.Net
Nursing Education Site
Multiple Sclerosis MS Nursing Diagnosis and Nursing Care Plan
Last updated on April 30th, 2023 at 12:36 am
Multiple Sclerosis MS Nursing Care Plans Diagnosis and Interventions
Multiple Sclerosis MS NCLEX Review and Nursing Care Plans
Multiple sclerosis (MS) is a chronic condition involving the central nervous system. It is an autoimmune disease characterized by the demyelination or degeneration of myelin sheaths which are protective covering of nerve cells.
The damage causes problems in the communication between the brain and the rest of the body.
There are three types of multiple sclerosis, namely: relapsing MS, secondary progressive MS, and primary progressive MS.
- Relapsing MS – the most common type, accounting for about 85% of all the MS cases. Relapsing MS is characterized by a relapsing and remitting cycle.
- Secondary progressive MS – starts off as relapsing MS but symptoms get steadily worse.
- Primary progressive MS – described as the gradual worsening of MS symptoms over time.
Signs and Symptoms of Multiple Sclerosis MS
Multiple sclerosis involves a range of different signs and symptoms.
These symptoms may vary depending on the location of affected nerve fibers, and may include:
- Numbness or weakness on one or both sides of the body
- Lhermitte sign – sensations of electric shocks when moving the neck
- Tremors and unsteady gait
- Partial/complete vision loss – typically occurs one eye at a time
- Prolonged double vision
- Blurred vision
- Slurring of speech
- Tingling sensation
- Issues with sexual, bowel, and bladder function
Causes of Multiple Sclerosis MS
Multiple sclerosis is considered an autoimmune condition although the exact etiology of the disease is still unknown.
In the case of MS, the body attacks the protective covering of nerve fibers of the brain and spinal cord called myelin sheaths.
The risk factors for developing the condition are as follows:
- Age – the onset of MS commonly occurs between 20-40 years of age. However, all ages can develop the condition
- Sex – women are reported to be more susceptible to the disease
- Family history – having immediate family members diagnosed with MS increases the risk of developing the condition
- Some infections – there are infections associated with the development of MS such as Epstein-Barr infection
- Race – those with Northern European descent are at higher risk of developing MS
- Climate – MS is more common in countries with a temperate climate such as the US, New Zealand, and Europe
- Vitamin D – low level of vitamin D is linked with the development of MS
- Autoimmune diseases – those with pre-existing autoimmune diseases are slightly at risk of developing MS
Complications of Multiple Sclerosis MS
- Muscle spasms
- Problems related to bladder, bowel, and sexual functions
- Mental changes
Diagnosis of Multiple Sclerosis MS
A neurologist typically makes the diagnosis of multiple sclerosis. The diagnosis for this condition may not be straightforward and may require a series of tests, which may include:
- Neurological exam – questions about health problems at present and in the past may be asked as part of the assessment. The medical history may help explain the symptoms and rule out other possible diagnoses. A neurological exam may include physical tests to assess for changes and weaknesses in movement, vision, balance, sensation, speech, and reflexes.
- Magnetic resonance imaging (MRI) – an MRI of the brain and spinal cord is performed to identify the exact location of damage to the nerve tissues. MRI has been successful in providing a definite diagnosis in 90% of cases.
- Evoked potential test – this procedure involves the attachment of electrodes on the head to record brain patterns while stimuli are presented.
- Spinal tap – also known as lumbar puncture, this test involves the insertion of a needle into the space surrounding the spinal cord to take a small sample of the spinal fluid. In people with MS, the fluid will show the presence of antibodies.
- Blood tests – blood tests are performed to help rule out other conditions that are similar to MS.
Treatment for Multiple Sclerosis MS
Multiple sclerosis has no cure; however, several therapies and treatment options are available to help manage the disease.
- Disease-Modifying Therapies (DMTs). DMTs are known to be effective in relapsing MS. They work by slowing down the progression of symptoms and damage caused by the condition. There are a variety of DMTs available in the market in the form of tablets, injections, and infusions.
- Hematopoietic Stem Cell Transplantation (HSCT). HSCT is an intensive treatment involving the use of chemotherapy to wipe out and regrow the immune system with the use of stem cells. It is most effective in the early stages of the disease.
- Physiotherapy. Physiotherapists can help deal with physical difficulties associated with the disease. They can advise on movements and exercises to deal with the problematic area of the body.
- Complementary and Alternative Therapies. Also known as complementary and alternative medicine (CAMs), this therapy option involves the use of a variety of “natural” medicine such as acupuncture, yoga, and aromatherapy.
Nursing Diagnosis for Multiple Sclerosis MS
Nursing care plan for multiple sclerosis 1.
Impaired physical mobility related to neurological impairment secondary to multiple sclerosis, as evidenced by numbness or weakness on one or both sides of the body, Lhermitte sign, tremors, and unsteady gait
Desired Outcome: The patient will be able to perform activities of daily living within the limits of the disease.
Nursing Care Plan for Multiple Sclerosis 2
Nursing Diagnosis: Fatigue related to body weakness secondary to multiple sclerosis as evidenced by numbness and weakness on one side of the body or both, inability to do activities of daily living (ADLs) as normal, and verbalization of overwhelming tiredness
Desired Outcome: The patient will demonstrate active participation in necessary and desired activities and demonstrate increase in activity levels.
Nursing Care Plan for Multiple Sclerosis 3
Nursing Diagnosis: Disturbed Sensory Perception (Visual) related to visual impairment secondary to multiple sclerosis as evidenced by verbal complaint of vision problems such as blurry vision, prolonged double vision, or partial/total loss of vision
Desired Outcome: The patient will regain optimal vision while being able to cope with and accept permanent vision changes.
Nursing Care Plan for Multiple Sclerosis 4
Impaired Urinary Elimination
Nursing Diagnosis: Impaired Urinary Elimination related to neuromuscular impairment (i.e., spinal cord lesions, neurogenic bladder) secondary to multiple sclerosis as evidenced by nocturia, frequency, incontinence, urinary retention with overflow, and recurrent urinary tract infections (UTIs)
Desired Outcomes :
- The patient will express their knowledge of the situation.
- The patient will exhibit infection-prevention/minimization habits and procedures.
- The patient will routinely and fully empty his bladder (voluntarily or by catheter as appropriate).
- The patient will demonstrate the absence of urine leakage.
Nursing Care Plan for Multiple Sclerosis 5
Low Self-Esteem
Nursing Diagnosis: Low Self-Esteem related to structure/function modification, disturbance in the patient’s perception of his or her own body, reversal of roles, and dependence secondary to multiple sclerosis as evidenced by confusion over one’s identity, purpose and life path, denial, retreat, rage, self-destructive/negative behavior, using ineffective coping strategies, and changes in one’s/others’ perceptions of their role/physical ability to resume it.
Desired Outcomes:
- The patient will express a realistic view of the body and acceptance of it as it is.
- The patient will see himself/herself as a capable individual.
- The patient will take part in and be responsible for satisfying his or her own needs.
- The patient will notice and incorporate changes in self-concept/role without compromising self-esteem.
- The patient will make realistic preparations for adjusting to new roles.
Nursing Care Plan for Multiple Sclerosis 6
Self-Care Deficit
Nursing Diagnosis: Self-Care Deficit related to motor impairment, tremors, neuromuscular/perceptual impairment, intolerance to exertion, diminished strength and endurance, pain, discomfort and exhaustion, memory problems, and depression secondary to multiple sclerosis as evidenced by frustration, inability to execute self-care activities, and poor personal hygiene.
- The patient will identify individual aspects of weakness/needs.
- The patient will exhibit self-care practices and lifestyle improvements.
- The patient will execute self-care activities to the best of his or her abilities.
- The patient will discover personal and community resources that can help.
More Multiple Sclerosis Nursing Diagnosis
- Impaired Verbal Communication
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care . St. Louis, MO: Elsevier. Buy on Amazon
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, & outcomes . St. Louis, MO: Elsevier. Buy on Amazon
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2020). Medical-surgical nursing: Concepts for interprofessional collaborative care . St. Louis, MO: Elsevier. Buy on Amazon
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination . St. Louis, MO: Elsevier. Buy on Amazon
Disclaimer:
Please follow your facilities guidelines and policies and procedures.
The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes.
This information is not intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.
Leave a Comment Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .

IMAGES
VIDEO
COMMENTS
Writing a nursing case study analysis usually takes only a few hours. Reference your case study. After writing your case study, make sure you add all in-text citations if you had not added them already. And when adding them, you should make sure you follow the style/format recommended in the assignment prompt (usually APA or Harvard style).
1. Assessment. The first step of writing a nursing care plan is to practice critical thinking skills and perform data collection. During this phase, you collect subjective and objective data. The source of subjective data is an interview with the caretakers, family members, or friends of the patient and the patient.
Step 1: Assessment. The first step in writing an organized care plan includes gathering subjective and objective nursing data. Subjective data is what the patient tells us their symptoms are, including feelings, perceptions, and concerns. Objective data is observable and measurable. This information can come from,
Step 1: Data Collection or Assessment. The first step in writing a nursing care plan is to create a client database using assessment techniques and data collection methods (physical assessment, health history, interview, medical records review, and diagnostic studies). A client database includes all the health information gathered.
We'll discuss the steps involved, from selecting a patient to presenting the case study, and provide tips to ensure a comprehensive and informative analysis. Step 1: Selecting the Patient. The first step in completing a nursing case study with an actual patient scenario is to select an appropriate patient.
It is best to simply tell the story and let the outcome speak for itself. With these points in mind, let's begin the process of writing the case study: Title page: Title: The title page will contain the full title of the article. Remember that many people may find our article by searching on the internet.
Nursing care plans are a vital part of the nursing process. They provide a centralized document of the patient's condition, diagnosis, the nursing team's goals for that patient, and measure of the patient's progress. Nursing care plans are structured to capture all the important information for the nursing team in one place.
Ensure your summary has at least the case presentation, the nursing assessment/diagnosis, the intervention, and the key recommendations. At the very end of your conclusion, add a closing statement. The statement should wrap up the whole thing nicely. Try to make it as impressive as possible. 9.
Nursing care plans help define nursing guidelines and some treatment guidelines (as ordered) for a specific patient. Essentially, it is a plan of action. It helps guide nurses throughout their shift in caring for the patient. It also allows nurses to provide attentive and focused care.
The nurse can evaluate if interventions are effective by evaluating goal progression. 4. Communication and continuity between nurses. The plan of care is a document that assists nurses in providing continuous and consistent care, working toward shared goals. 5. Coordinates other disciplines.
Nursing ethics case study. Case study of a patient: Assessment and treatment plan. Cecile case study: Mrs. J. Nursing power in the emergency department: Case study. Heart failure case study: Mrs. J. Application of ethics in nursing: Case study. Sudden visual impairment: Case study.
• Unfolding case study. It's quite a new type of case study. The task usually presents a patient scenario with evolution details. Students must evaluate and re-evaluate the patient's condition based on the offered scenario, care plan, and rationale. 7 Steps to Write a Nursing Case Study. Step 1. Read out the case carefully. Just after you ...
Writing a successful nursing case study can be a challenging task. However, by following the steps provided in this blog that is, first defining the problem, gathering information, developing alternatives., analyzing the alternatives, selecting the best alternative, implementing the solution and evaluating the outcome.
Writing a nursing case study requires thoughtful consideration of relevant information and resources. You must select a single subject, conduct research on it, interview experts, analyze the data collected, and present your findings. That may seem like a lot, but let us break it down for you. Here's a look at the key elements that your case ...
A case report is a detailed report of the symptoms, signs, diagnosis, treatment, and follow-up of an individual patient. Case reports usually describe an unusual or novel occurrence and as such, remain one of the cornerstones of medical progress and provide many new ideas in medicine. Some reports contain an extensive review of the relevant ...
A nursing care plan (NCP) is a document that contains relevant information about a patient's diagnosis, treatment goals, and nursing orders, as well as an evaluation plan. Nursing care plans may ...
In this guide, we'll walk you through the essential steps to creating effective and insightful nursing case studies that meet the academic standards of these countries. 1. Choosing a Relevant Case. The foundation of a successful nursing case study is the selection of an appropriate case. Look for scenarios that align with your course's learning ...
kalayaan. 109 Posts. A case study is when u analyze or report about the status of the patient. It includes the assessment, patho-physio of the disease, etc. It's more general. Care plan includes the ones that you put above. U can incorporate the care plan in the case study.
Outline. Natasha is a 32-year-old female African American patient arriving at the surgery oncology unit status post left breast mastectomy and lymph node excision. She arrives from the post-anesthesia unit (PACU) via hospital bed with her spouse, Angelica, at the bedside. They explain that a self-exam revealed a lump, and, after mammography and ...
Care planning policy often emphasises the importance of taking account of the entirety of a person's conditions, circumstances, attitudes and preferences in developing an effective care plan. Multimorbidity among long term conditions is common ( Valderas et al., 2009 ). Patients with multiple long term conditions report difficulties in ...
The nurse can promote adherence to Mich's asthma treatment regimen by providing education and resources, such as written instructions and referrals to support groups. The nurse can also encourage open communication with Mich and his family and address any barriers to adherence, such as cost or access to medications. 5.
The nursing process consists of four stages, the assessment, planning, implementing and evaluation. This problem solving approach will be adopted to structure, organise, and present the nursing intervention. A fully detailed client's profile will be given. The "mental health assessment and plan" process will also be addressed.
Helpful in building an individualized treatment plan to fulfill a patient's specific needs using the most up-to-date procedures and continence supplies. As directed, catheterize. If the patient is unable to empty their bladder or holds urine, this test may be required as a treatment and for evaluation.