Treatment Research
In a new study in mice, researchers showed they could enhance radiation therapy by boosting levels of the BAMBI protein in MDSC immune cells in the tumor microenvironment. After radiation, T cells flooded into the tumor and killed tumors elsewhere in the body.
In a clinical trial, people being treated for cancer who participated in virtual mind–body fitness classes were less likely to be hospitalized, and had shorter stays when they were hospitalized, than people who did not take the classes.
NCI’s James H. Doroshow, M.D., reflects on the accomplishments of NCI-MATCH, a first-of-its-kind precision medicine cancer trial, and gives an overview of three new successor trials: ComboMATCH, MyeloMATCH, and iMATCH.
A new study, conducted largely in mice, may help explain why a currently used molecular marker—called mismatch repair deficiency—doesn’t always work to predict which patients will respond to immunotherapies called immune checkpoint inhibitors.
New approach may increase the effectiveness of T-cell-based immunotherapy treatments against solid tumors.
A cancer-infecting virus engineered to tamp down a tumor’s ability to suppress the immune system shrank tumors in mice, a new study shows. The modified oncolytic virus worked even better when used along with an immune checkpoint inhibitor.
Despite recommendations, a new analysis shows few people with cancer undergo germline testing to learn if their cancer may have been caused by gene changes inherited from a parent. Germline testing can help doctors determine the best treatments for a patient and help identify people whose family members may be at higher risk of cancer.
ComboMATCH will consist of numerous phase 2 cancer treatment trials that aim to identify promising drug combinations that can advance to larger, more definitive clinical trials.
A new study has compared three formulations of an mRNA vaccine designed to treat cancers caused by human papillomavirus (HPV) infections. All three vaccines showed promise in mice.
Researchers have identified a mechanism by which cancer cells develop specific genetic changes needed to become resistant to targeted therapies. They also showed that this process, called non-homologous end-joining (NHEJ), can potentially be disrupted.
For some people with cancer, is 6 months of immunotherapy the only treatment they might ever need? Or 4 weeks of immunotherapy followed by minor surgery? Results from several small clinical trials suggest these scenarios may be bona fide possibilities.
Two research teams have developed ways of overcoming barriers that have limited the effectiveness of CAR T-cell therapies, including engineering ways to potentially make them effective against solid tumors like pancreatic cancer and melanoma.
In people with cancer treated with immune checkpoint inhibitors, a rare, but often fatal, side effect is inflammation in the heart, called myocarditis. Researchers have now identified a potential chief cause of this problem: T cells attacking a protein in heart cells called α-myosin.
Researchers have modified a chemo drug, once abandoned because it caused serious gut side effects, so that it is only triggered in tumors but not normal tissues. After promising results in mice, the drug, DRP-104, is now being tested in a clinical trial.
Two research teams have developed a treatment approach that could potentially enable KRAS-targeted drugs—and perhaps other targeted cancer drugs—flag cancer cells for the immune system. In lab studies, the teams paired these targeted drugs with experimental antibody drugs that helped the immune system mount an attack.
Inflammation is considered a hallmark of cancer. Researchers hope to learn more about whether people with cancer might benefit from treatments that target inflammation around tumors. Some early studies have yielded promising results and more are on the horizon.
NCI researchers are developing an immunotherapy that involves injecting protein bits from cytomegalovirus (CMV) into tumors. The proteins coat the tumor, causing immune cells to attack. In mice, the treatment shrank tumors and kept them from returning.
FDA has approved the combination of the targeted drugs dabrafenib (Tafinlar) and trametinib (Mekinist) for nearly any type of advanced solid tumor with a specific mutation in the BRAF gene. Data from the NCI-MATCH trial informed the approval.
People with cancer who take immunotherapy drugs often develop skin side effects, including itching and painful rashes. New research in mice suggests these side effects may be caused by the immune system attacking new bacterial colonies on the skin.
Researchers have developed tiny “drug factories” that produce an immune-boosting molecule and can be implanted near tumors. The pinhead-sized beads eliminated tumors in mice with ovarian and colorectal cancer and will soon be tested in human studies.
Women are more likely than men to experience severe side effects from cancer treatments such as chemotherapy, targeted therapy, and immunotherapy, a new study finds. Researchers hope the findings will increase awareness of the problem and help guide patient care.
Research to improve CAR T-cell therapy is progressing rapidly. Researchers are working to expand its use to treat more types of cancer and better understand and manage its side effects. Learn how CAR T-cell therapy works, which cancers it’s used to treat, and current research efforts.
Experts say studies are needed on how to best transition telehealth from a temporary solution during the pandemic to a permanent part of cancer care that’s accessible to all who need it.
Removing immune cells called naive T cells from donated stem cells before they are transplanted may prevent chronic graft-versus-host disease (GVHD) in people with leukemia, a new study reports. The procedure did not appear to increase the likelihood of patients’ cancer returning.
A specific form of the HLA gene, HLA-A*03, may make immune checkpoint inhibitors less effective for some people with cancer, according to an NCI-led study. If additional studies confirm the finding, it could help guide the use of these commonly used drugs.
The success of mRNA vaccines for COVID-19 could help accelerate research on using mRNA vaccine technology to treat cancer, including the development of personalized cancer vaccines.
Aneuploidy—when cells have too many or too few chromosomes—is common in cancer cells, but scientists didn’t know why. Two new studies suggest that aneuploidy helps the cells survive treatments like chemotherapy and targeted therapies.
New research suggests that fungi in the gut may affect how tumors respond to cancer treatments. In mice, when bacteria were eliminated with antibiotics, fungi filled the void and impaired the immune response after radiation therapy, the study found.
FDA has approved belumosudil (Rezurock) for the treatment of chronic graft-versus-host disease (GVHD). The approval covers the use of belumosudil for people 12 years and older who have already tried at least two other therapies.
In lab studies, the antibiotic novobiocin showed promise as a treatment for cancers that have become resistant to PARP inhibitors. The drug, which inhibits a protein called DNA polymerase theta, will be tested in NCI-supported clinical trials.
A drug called avasopasem manganese, which has been found to protect normal tissues from radiation therapy, can also make cancer cells more vulnerable to radiation treatment, a new study in mice suggests.
While doctors are familiar with the short-term side effects of immune checkpoint inhibitors, less is known about potential long-term side effects. A new study details the chronic side effects of these drugs in people who received them as part of treatment for melanoma.
Cholesterol-lowering drugs known as PCSK9 inhibitors may improve the effectiveness of cancer immune checkpoint inhibitors, according to studies in mice. The drugs appear to improve the immunotherapy drugs’ ability to find tumors and slow their growth.
Researchers have developed a nanoparticle that trains immune cells to attack cancer. According to the NCI-funded study, the nanoparticle slowed the growth of melanoma in mice and was more effective when combined with an immune checkpoint inhibitor.
A comprehensive analysis of patients with cancer who had exceptional responses to therapy has revealed molecular changes in the patients’ tumors that may explain some of the exceptional responses.
Researchers are developing a new class of cancer drugs called radiopharmaceuticals, which deliver radiation therapy directly and specifically to cancer cells. This Cancer Currents story explores the research on these emerging therapies.
FDA has recently approved two blood tests, known as liquid biopsies, that gather genetic information to help inform treatment decisions for people with cancer. This Cancer Currents story explores how the tests are used and who can get the tests.
Cancer cells with a genetic feature called microsatellite instability-high (MSI-high) depend on the enzyme WRN to survive. A new NCI study explains why and reinforces the idea of targeting WRN as a treatment approach for MSI-high cancer.
Efforts to contain the opioid epidemic may be preventing people with cancer from receiving appropriate prescriptions for opioids to manage their cancer pain, according to a new study of oncologists’ opioid prescribing patterns.
The gene-editing tool CRISPR is changing the way scientists study cancer, and may change how cancer is treated. This in-depth blog post describes how this revolutionary technology is being used to better understand cancer and create new treatments.
FDA’s approval of pembrolizumab (Keytruda) to treat people whose cancer is tumor mutational burden-high highlights the importance of genomic testing to guide treatment, including for children with cancer, according to NCI Director Dr. Ned Sharpless.
Patients with acute graft-versus-host disease (GVHD) that does not respond to steroid therapy are more likely to respond to the drug ruxolitinib (Jakafi) than other available treatments, results from a large clinical trial show.
NCI is developing the capability to produce cellular therapies, like CAR T cells, to be tested in cancer clinical trials at multiple hospital sites. Few laboratories and centers have the capability to make CAR T cells, which has limited the ability to test them more broadly.
An experimental drug may help prevent the chemotherapy drug doxorubicin from harming the heart and does so without interfering with doxorubicin’s ability to kill cancer cells, according to a study in mice.
In people with blood cancers, the health of their gut microbiome appears to affect the risk of dying after receiving an allogeneic hematopoietic stem cell transplant, according to an NCI-funded study conducted at four hospitals across the globe.
A novel approach to analyzing tumors may bring precision cancer medicine to more patients. A study showed the approach, which analyzes gene expression using tumor RNA, could accurately predict whether patients had responded to treatment with targeted therapy or immunotherapy.
Bone loss associated with chemotherapy appears to be induced by cells that stop dividing but do not die, a recent study in mice suggests. The researchers tested drugs that could block signals from these senescent cells and reverse bone loss in mice.
Some experts believe that proton therapy is safer than traditional radiation, but research has been limited. A new observational study compared the safety and effectiveness of proton therapy and traditional radiation in adults with advanced cancer.
In people with cancer, the abscopal effect occurs when radiation—or another type of localized therapy—shrinks a targeted tumor but also causes untreated tumors in the body to shrink. Researchers are trying to better understand this phenomenon and take advantage of it to improve cancer therapy.
An experimental drug, AMG 510, that targets mutated forms of the KRAS protein completely shrank tumors in cancer mouse models and data from a small clinical trial show that it appears to be active against different cancer types with a KRAS mutation.
Researchers have engineered an oncolytic virus to kill cancer cells and boost the immune response against tumors. In a new study, the virus provided T cells around tumors with a hormone they need for their own cell-killing functions.
FDA has approved entrectinib (Rozlytrek) for the treatment of children and adults with tumors bearing an NTRK gene fusion. The approval also covers adults with non-small cell lung cancer harboring a ROS1 gene fusion.
A new NCI-supported study showed that altering cancer cell metabolism by feeding mice a diet very low in the nutrient methionine improved the ability of chemotherapy and radiation therapy to shrink tumors.
An NCI-funded clinical trial is testing the immunotherapy drug nivolumab (Opdivo) in people who have advanced cancer and an autoimmune disease, such as rheumatoid arthritis, lupus, or multiple sclerosis, who are often excluded from such trials.
Researchers have identified a protein called CD24 that may be a new target for cancer immunotherapy. The protein is a ‘don’t eat me’ signal that prevents immune cells called macrophages from engulfing and eating cells.
Injecting cells undergoing necroptosis, a form of cell death, into tumors in mice kickstarted an immune response against the tumors, researchers have found. When combined with immunotherapy, the treatment was effective at eliminating tumors in mice.
Researchers have identified proteins that may play a central role in transforming T cells from powerful destroyers to depleted bystanders that can no longer harm cancer cells. The findings could lead to strategies for boosting cancer immunotherapies.
Did you know that NCI supports clinical trials of new treatments for pet dogs with cancer? Learn more about NCI’s comparative oncology studies and how they may also help people with cancer.
Researchers have discovered a potential way to turn on one of the most commonly silenced tumor-suppressor proteins in cancer, called PTEN. They also found a natural compound, I3C, that in lab studies could flip the on switch.
New findings from a clinical trial suggest that a single dose of radiation therapy may control painful bone metastases as effectively as multiple lower doses of radiation therapy.
The expanding use of cancer immunotherapy has revealed a variety of side effects associated with this treatment approach. Researchers are now trying to better understand how and why these side effects occur and develop strategies for better managing them.
The investigational immunotherapy drug bintrafusp alfa (also called M7824), a bifunctional fusion protein, shrank the tumors of some patients with advanced HPV-related cancers, according to results from a phase 1 clinical trial.
A new study provides insight into how cancer immunotherapy works and suggests ways to enhance the treatment’s effectiveness. The NCI-led study, published in Science, examined the effect of high potassium levels on T cells.
Pain is a common and much-feared symptom among people with cancer and long-term survivors. As more people survive cancer for longer periods, there is a renewed interest in developing new, nonaddictive approaches for managing their chronic pain.
Advertisement

Clinical Cancer Research | American Association for Cancer Research
- Online First
- Collections
- Online ISSN 1557-3265
- Print ISSN 1078-0432
AACR Journals
- Blood Cancer Discovery
- Cancer Discovery
- Cancer Epidemiology, Biomarkers & Prevention
- Cancer Immunology Research
- Cancer Prevention Research
- Cancer Research
- Cancer Research Communications
- Clinical Cancer Research
- Molecular Cancer Research
- Molecular Cancer Therapeutics
- Info for Advertisers
- Information for Institutions/Librarians
- Privacy Policy
- Copyright © 2023 by the American Association for Cancer Research.
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Journal of Experimental & Clinical Cancer Research
Featured article : preclinical models as patients’ avatars for precision medicine in colorectal cancer: past and future challenges.
Colorectal cancer (CRC) is a complex and heterogeneous disease, characterized by dismal prognosis and low survival rate in the advanced (metastatic) stage. During the last decade, the establishment of novel preclinical models, leading to the generation of translational discovery and validation platforms, has opened up a new scenario for the clinical practice of CRC patients. To bridge the results developed at the bench with the medical decision process, the ideal model should be easily scalable, reliable to predict treatment responses, and flexibly adapted for various applications in the research. As such, the improved benefit of novel therapies being tested initially on valuable and reproducible preclinical models would lie in personalized treatment recommendations based on the biology and genomics of the patient’s tumor with the overall aim to avoid overtreatment and unnecessary toxicity.
In this review , we summarize different in vitro and in vivo models, which proved efficacy in detection of novel CRC culprits and shed light into the biology and therapy of this complex disease. Even though cell lines and patient-derived xenografts remain the mainstay of colorectal cancer research, the field has been confidently shifting to the use of organoids as the most relevant preclinical model. Prioritization of organoids is supported by increasing body of evidence that these represent excellent tools worth further therapeutic explorations. In addition, novel preclinical models such as zebrafish avatars are emerging as useful tools for pharmacological interrogation. Finally, all available models represent complementary tools that can be utilized for precision medicine applications.
Aims and scope
Journal of Experimental & Clinical Cancer Research is an online peer-reviewed journal that provides a high-quality forum for all aspects of basic, clinical and translational work in oncology.
Please click here to read more.
Editor-in-Chief
Mauro Castelli, Regina Elena National Cancer Institute, Italy
If you would like to contact Journal of Experimental & Clinical Cancer Research, please send an email to:
- Most accessed
GPR65 sensing tumor-derived lactate induces HMGB1 release from TAM via the cAMP/PKA/CREB pathway to promote glioma progression
Authors: Chaolong Yan, Zijiang Yang, Pin Chen, Yuyang Yeh, Chongjing Sun, Tao Xie, Wei Huang and Xiaobiao Zhang
RBM10 C761Y mutation induced oncogenic ASPM isoforms and regulated β-catenin signaling in cholangiocarcinoma
Authors: Jiang Chang, Yaodong Zhang, Tao Zhou, Qian Qiao, Jijun Shan, Yananlan Chen, Wangjie Jiang, Yirui Wang, Shuochen Liu, Yuming Wang, Yue Yu, Changxian Li and Xiangcheng Li
Mesothelin promotes brain metastasis of non-small cell lung cancer by activating MET
Authors: Shengkai Xia, Wenzhe Duan, Mingxin Xu, Mengqi Li, Mengyi Tang, Song Wei, Manqing Lin, Encheng Li, Wenwen Liu and Qi Wang
Oncolytic adenovirus encoding apolipoprotein A1 suppresses metastasis of triple-negative breast cancer in mice
Authors: Jie Dong, Lingkai Kong, Shiqun Wang, Mao Xia, Yenan Zhang, Jingyi Wu, Fuming Yang, Shuguang Zuo and Jiwu Wei
Transcriptional regulation of cancer stem cell: regulatory factors elucidation and cancer treatment strategies
Authors: Zhengyue Zhang and Yanjie Zhang
Most recent articles RSS
View all articles
Apoptosis in cancer: from pathogenesis to treatment
Authors: Rebecca SY Wong
High-dose intravenous vitamin C, a promising multi-targeting agent in the treatment of cancer
Authors: Franziska Böttger, Andrea Vallés-Martí, Loraine Cahn and Connie R. Jimenez
Ivermectin reverses the drug resistance in cancer cells through EGFR/ERK/Akt/NF-κB pathway
Authors: Lu Jiang, Pan Wang, Ying-Jian Sun and Yi-Jun Wu
Effects of short-term fasting on cancer treatment
Authors: Stefanie de Groot, Hanno Pijl, Jacobus J. M. van der Hoeven and Judith R. Kroep
Iron and leukemia: new insights for future treatments
Authors: Fang Wang, Huanhuan Lv, Bin Zhao, Liangfu Zhou, Shenghang Wang, Jie Luo, Junyu Liu and Peng Shang
Most accessed articles RSS
Springer Nature Oncology Portfolio

Colorectal Cancer Awareness Month
Call for papers: Liquid Biopsy in Precision Oncology
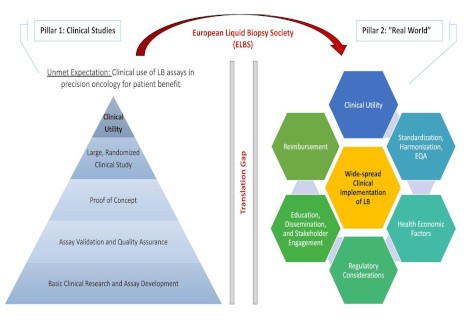
Journal of Experimental & Clinical Cancer Research is delighted to announce a new thematic series focused on:
Liquid Biopsy in Precision Oncology
The Special Issue will accept Research Articles and Reviews in this topic. Submit here .
- Submission opens: 1 st February 2024
- Submission deadline: 31 st January 2025
Click here to view this collection. Click here to access all thematic series published to date in Journal of Experimental & Clinical Cancer Research .
Call for papers: CRISPR-Cas9 system, the next generation in cancer therapy and target discovery

Journal of Experimental & Clinical Cancer Research is delighted to announce a new thematic series focused on:
CRISPR-Cas9 system, the next generation in cancer therapy and target discovery
The Special Issue will accept Research Articles and Review in this topic. Submit here .
- Submission opens: 1 st April 2023
- Submission deadline: 30 th June 2024
Click here to view this collection. Click here to access all thematic series published to date in Journal of Experimental & Clinical Cancer Research.
Follow JECCR on Social Media

Follow JECCR's social media accounts to be kept up-to-date with the latest articles, collections and journal news!
Recognising Editorial Excellence

Reviewer Acknowledgement and New Recruitment
The Editor-in-Chief of Journal of Experimental & Clinical Cancer Research would like to thank all of our reviewers who have contributed to the journal and is looking for new reviewers to assess manuscripts. For consideration, please send your CV with keywords and expertise to [email protected]
Archival content
Journal of Experimental & Clinical Cancer Research has been publishing since 1982. Prior to publishing with BioMed Central from 2008, Journal of Experimental & Clinical Cancer Research was published in print. For enquiries about previous content, please contact us on:

Owned by the Association for International Promotion & Study in Tumors (APSIT)

Official journal of the Regina Elena National Cancer Institute , Scientific Director Gennaro Ciliberto, Rome, Italy
- Editorial Board
- Manuscript editing services
- Instructions for Editors
- Sign up for article alerts and news from this journal
- Submit manuscript
Annual Journal Metrics
2022 Citation Impact 11.3 - 2-year Impact Factor 11.5 - 5-year Impact Factor 1.870 - SNIP (Source Normalized Impact per Paper) 2.413 - SJR (SCImago Journal Rank)
2023 Speed 4 days submission to first editorial decision for all manuscripts (Median) 100 days submission to accept (Median)
2023 Usage 3,003,080 downloads 3,022 Altmetric mentions
- More about our metrics
ISSN: 1756-9966
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

- Find a Clinical Trial
- Find a Physician
- Find a Location
- Cancers We Treat
- Chemotherapy & Medical Infusion Services
- Clinical Trials
- Genetic Screening & Testing
- Gynecologic Oncology
- Immunotherapy
- Bispecific Therapy
- Radiation Oncology
- Care Coordination
- FCS Foundation
- Insurance & Financial Navigation
- Rx To Go (Oral Oncolytic Pharmacy)
- Nutrition & Wellness
- Supportive Care
- Patient Education
- Patient Education Videos
- Your First Visit
- Masks & Visitors
- Patient Stories
- Patient Experience Portal
- Supporting a Loved One Living with Cancer
- Time To Treat
- Refer a Patient
- Clinical Research Associates
- FCS Hematology Oncology Review
- Insurance & Financial Counseling
- Radiology Non-FCS Scans
- Telehealth Services
- Case Studies
- Our Partners
- Mission Vision Values
- Locations by County
- Accreditations
- Executive and Senior Management
- Physician Leadership
- Clinical Trials Team
- FCS Publications

FCS Clinical Research Driving Progress to Cure Cancer

Florida Cancer Specialists & Research Institute Clinical Research Driving Progress to Cure Cancer
Clinical trials showcased at global gathering.
Fort Myers, Fla., April 5, 2024 – Clinical research conducted at Florida Cancer Specialists & Research Institute, LLC (FCS) will be highlighted at the American Association for Cancer Research 2024 Annual Meeting in San Diego as scientists, clinicians and other health care professionals and stakeholders from all over the world gather to share the latest advances in cancer science and medicine.
“Finding cancer cures requires diligence and collaboration among the greatest minds in cancer research,” noted Lucio N. Gordan, MD , FCS President & Managing Physician. “Through our extensive and growing clinical trials research program, FCS is proud to be part of global efforts that are saving lives and enhancing the quality of life for patients and their families.”
FCS provides ongoing access to more than 160 clinical trials within 32 FCS clinics and three Drug Development Units (early-phase) across Florida, in Sarasota, Lake Mary and Lake Nona. In recent years, the majority of new cancer drugs approved for use in the U.S. were studied in clinical trials with FCS participation, prior to approval.
FCS physician investigators will present findings during oral and poster sessions at the ACCR 2024 Annual Meeting.
FCS abstracts at AACR 2024 Annual Meeting: 068, 075, 132, 141, 156, 163, 291, 6552, 7172, 099, 077, 2565
FCS Director of Drug Development Manish Patel, MD , co-author of nine abstracts:
- Interim results of the ongoing phase 1-2 clinical trial of KVA12123, an engineered IgG1 targeting VISTA, as monotherapy and in combination with pembrolizumab in patients with advanced solid tumors
- Phase 1 trial evaluating AC699, an orally bioavailable chimeric estrogen receptor degrader, in patients with advanced or metastatic breast cancer
- Phase I/IIa clinical trial (TranStar101) to evaluate the safety, tolerability and pharmacokinetics of OSEMITAMAB administered as monotherapy or in combination with nivolumab or standard of care in patients with locally advanced or metastatic solid tumors
- mRNA-4157 (V940) individualized neoantigen therapy (INT) + pembrolizumab (pembro) in advanced unresectable HPV- head & neck carcinoma (HNSCC): Clinical & translational analysis
- Phase I study evaluating AC676, an innovative BTK chimeric degrader, in patients with relapsed and refractory B-cell malignancies
- Phase 1 clinical trial of the farnesyl transferase inhibitor KO-2806 alone or as part of combination therapy for advanced solid tumors
- Phase 1/2, first-in-human study of DS-3939a in patients with advanced solid tumors: A new DXd ADC targeting TA-MUC1
- Intratumoral (ITu) delivery of mRNA-2752 encoding human OX40L/IL-23/IL-36γ in combination with durvalumab induces an immunostimulatory effect within the tumor microenvironment (TME) of patients with advanced solid tumors
- Pharmacokinetic/biomarker (PK/BMx) analysis of the toll-like receptor 7 and 8 (TLR7/8) agonist EIK1001 in phase 1 studies in participants (Pts) with solid tumors
FCS Associate Director of Drug Development Judy Wang, MD first author:
- NGM707 in combination with pembrolizumab in advanced or metastatic solid tumors: Preliminary results from dose escalation
FCS Scientific Director of Research and Associate Professor of Medicine, Wake Forest University School of Medicine Lowell Hart, MD, FACP , first author:
- Vitamin D deficiency and outcomes in prostate cancer patients-A real world database
Co-authors include FCS Trial Match Specialist and Medical Oncologist and Hematologist (retired) James Reeves Jr., MD, FCS Nurse Specialist Stacey Garofalo RN and members of the FCS Real-World Evidence Team, IT Director Data Science Derek Hall and Informatics Data Scientist Parth Kothiya.
FCS Director of Drug Development, Lake Nona DDU, Cesar Augusto Perez, MD , co-author:
- Open-label phase 1 study to investigate SGN-CEACAM5C in adults with advanced solid tumors
“Our clinical trials research contributes daily to the discovery of ground-breaking new drugs and therapies that are accelerating our understanding of cancer and transforming the standard of care,“ said FCS Director of Late-Phase Clinical Research Bradley Monk, MD .
Dr. Monk is co-author of a study conducted at HonorHealth University of Arizona College of Medicine and Creighton University School of Medicine prior to being named to his leadership position at FCS earlier this year, “Tumor microenvironment (TME) biomarkers of TIGIT and PD-L1 immune checkpoint blockade in cervical cancer: An exploratory biomarker analysis from SKYSCRAPER-04 (SKY04) study.”
Abstracts will be published in the AACR journal, Cancer Research , following the annual meeting. The American Association for Cancer Research (AACR), the first and largest cancer research organization dedicated to accelerating the conquest of cancer, represents 58,000 members residing in 141 countries.

FCS is pleased to share that its financial performance for the first two months of 2024 has surpassed the statewide practice’s budget.
Pharmacy leaders from Florida Cancer Specialists & Research Institute share expertise and best practices at the NCODA 2024 Spring Forum.
Core Ventures, Florida Cancer Specialists & Research Institute’s MSO, announces the formation of a new real-world evidence and analytics company, Vita Nova Insights(SM).

You are using an outdated browser. Please upgrade your browser to improve your experience.
Press Office
Clinical Academic Training Programme
Funding boost for next generation of clinical cancer scientists.
Published on: 5 April 2024
Clinical academics specialising in cancer research in Newcastle can now access support at every stage of their career development journey.
Newcastle University has secured almost £1.5m from Cancer Research UK to continue its prestigious Clinical Academic Training Programme over the next five years. This will provide five fully funded PhD clinical fellowships and five bursaries for undergraduates looking to intercalate and to do a Masters of Research (MRes) degree, aligned with cancer focused research.
Academics on the programme will be supported throughout their training pathway by the Newcastle Health Innovation Partners (NHIP) Academy, which provides career development support and mentoring to the next generation of health and care researchers.

NHIP Academy is the academic career development arm of NHIP, the Newcastle Academic Health Science Centre (AHSC). The Academy acts as both a physical and an intellectual hub for academic trainees, facilitating interaction between peers and creating a community of research active professionals, which is key for effective translational research. It provides guidance with funding applications and interview preparation, and also offers hotdesking and meeting spaces.
Professor Jones added: “By embedding the Clinical Academic Training Programme into NHIP Academy, we can provide a fully comprehensive training programme for aspiring clinical academics in cancer that ensures our fellows are under the support and oversight of a single organised structure.
“In addition to this, it provides a strong collegiate culture among the trainees at the different stages of their career development, with invaluable peer-to-peer support.”
Transforming training
Cancer Research UK’s Clinical Academic Training Programme Award will continue to transform clinical research training at nine of its research centres over the next five years. It builds on the five-year £50.7 million investment awarded by the charity in 2019.
In total, Cancer Research UK will have invested more than £109 million in this programme over 10 years, signalling the critical role the charity plays in supporting the UK’s life sciences ecosystem, funding around 50% of all publicly-funded research in the UK.
Michelle Mitchell , Cancer Research UK’s Chief Executive, said: “Clinician scientists have a very important role to play by bringing their knowledge and experience of treating people with cancer to scientific research.
“We need all our doctors and scientists to be able to reach their full potential, no matter their background. That’s why we are continuing to provide flexible training options for early-career clinician scientists.
“After the success of the first five years of this programme, we want to encourage even more clinicians to get involved in cancer research to help us get closer to a world where everybody lives longer, better lives free from the fear of cancer.”
Latest News
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Ecancermedicalscience


Innovative approaches for cancer treatment: current perspectives and new challenges
Carlotta pucci.
1 Smart Bio-Interfaces, Istituto Italiano di Tecnologia, 56025 Pisa, Italy
a https://orcid.org/0000-0002-8976-3711
Chiara Martinelli
b https://orcid.org/0000-0001-9360-1689
Gianni Ciofani
2 Department of Mechanical and Aerospace Engineering, Politecnico di Torino, 10129 Torino, Italy
c https://orcid.org/0000-0003-1192-3647
Every year, cancer is responsible for millions of deaths worldwide and, even though much progress has been achieved in medicine, there are still many issues that must be addressed in order to improve cancer therapy. For this reason, oncological research is putting a lot of effort towards finding new and efficient therapies which can alleviate critical side effects caused by conventional treatments. Different technologies are currently under evaluation in clinical trials or have been already introduced into clinical practice. While nanomedicine is contributing to the development of biocompatible materials both for diagnostic and therapeutic purposes, bioengineering of extracellular vesicles and cells derived from patients has allowed designing ad hoc systems and univocal targeting strategies. In this review, we will provide an in-depth analysis of the most innovative advances in basic and applied cancer research.
Introduction
Cancer is one of the main causes of death worldwide, and in the past decade, many research studies have focused on finding new therapies to reduce the side effects caused by conventional therapies.
During cancer progression, tumours become highly heterogeneous, creating a mixed population of cells characterised by different molecular features and diverse responsivity to therapies. This heterogeneity can be appreciated both at spatial and temporal levels and is the key factor responsible for the development of resistant phenotypes promoted by a selective pressure upon treatment administration [ 1 ]. Usually, cancer is treated as a global and homogeneous disease and tumours are considered as a whole population of cells. Thus, a deep understanding of these complex phenomena is of fundamental importance in order to design precise and efficient therapies.
Nanomedicine offers a versatile platform of biocompatible and biodegradable systems that are able to deliver conventional chemotherapeutic drugs in vivo , increasing their bioavailability and concentration around tumour tissues, and improving their release profile [ 2 ]. Nanoparticles can be exploited for different applications, ranging from diagnosis to therapy [ 2 ].
Recently, extracellular vesicles (EVs), responsible for cancer development, microenvironment modification and required for metastatic progression, have been widely investigated as efficient drug delivery vehicles [ 3 ].
Natural antioxidants and many phytochemicals have been recently introduced as anti-cancer adjuvant therapies due to their anti-proliferative and pro-apoptotic properties [ 4 , 5 ].
Targeted therapy is another branch of cancer therapy aiming at targeting a specific site, such as tumour vasculature or intracellular organelles, leaving the surroundings unaffected. This enormously increases the specificity of the treatment, reducing its drawbacks [ 6 ].
Another promising opportunity relies on gene therapy and expression of genes triggering apoptosis [ 7 ] and wild type tumour suppressors [ 8 ], or the targeted silencing mediated by siRNAs, currently under evaluation in many clinical trials worldwide [ 9 ].
Thermal ablation of tumours and magnetic hyperthermia are opening new opportunities for precision medicine, making the treatment localised in very narrow and precise areas. These methods could be a potential substitute for more invasive practices, such as surgery [ 10 , 11 ].
Furthermore, new fields such as radiomics and pathomics are contributing to the development of innovative approaches for collecting big amounts of data and elaborate new therapeutic strategies [ 12 , 13 ] and predict accurate responses, clinical outcome and cancer recurrence [ 14 – 16 ].
Taken all together, these strategies will be able to provide the best personalised therapies for cancer patients, highlighting the importance of combining multiple disciplines to get the best outcome.
In this review, we will provide a general overview of the most advanced basic and applied cancer therapies, as well as newly proposed methods that are currently under investigation at the research stage that should overcome the limitation of conventional therapies; different approaches to cancer diagnosis and therapy and their current status in the clinical context will be discussed, underlining their impact as innovative anti-cancer strategies.
Nanomedicine
Nanoparticles are small systems (1–1,000 nm in size) with peculiar physicochemical properties due to their size and high surface-to-volume ratio [ 17 ]. Biocompatible nanoparticles are used in cancer medicine to overcome some of the issues related to conventional therapies, such as the low specificity and bioavailability of drugs or contrast agents [ 2 ]. Therefore, encapsulation of the active agents in nanoparticles will increase their solubility/biocompatibility, their stability in bodily fluids and retention time in the tumour vasculature [ 18 – 20 ]. Furthermore, nanoparticles can be engineered to be extremely selective for a precise target [ 21 , 22 ] (see the “Targeted therapy and immunotherapy” section) and to release the drug in a controlled way by responding to a specific stimulus [ 18 , 23 – 25 ]. This is the case of ThermoDox, a liposomal formulation that can release doxorubicin as a response to an increment of temperature [ 26 ].
Inorganic nanoparticles are generally used as contrast agents for diagnosis purposes. Among them, quantum dots are small light-emitting semiconductor nanocrystals with peculiar electronic and optical properties, which make them highly fluorescent, resistant to photobleaching and sensitive for detection and imaging purposes [ 27 ]. Combined with active ingredients, they can be promising tools for theranostic applications [ 27 ]. In a recent study, quantum dots coated with poly(ethylene glycol) (PEG) were conjugated to anti-HER2 antibody and localised in specific tumour cells [ 28 ].
Superparamagnetic iron oxide nanoparticles (SPIONs) are usually exploited as contrast agents in magnetic resonance imaging (MRI) because they interact with magnetic fields [ 29 , 30 ]. Five types of SPIONs have been tested for MRI: ferumoxides (Feridex in the US, Endorem in Europe), ferucarbotran (Resovist), ferucarbotran C (Supravist, SHU 555 C), ferumoxtran-10 (Combidex) and NC100150 (Clariscan). Ferucarbotran is currently available in few countries, while the others have been removed from the market [ 25 ]. SPIONs have also been studied for cancer treatment by magnetic hyperthermia (see the “Thermal ablation and magnetic hyperthermia” section), and a formulation of iron oxide coated with aminosilane called Nanotherm has been already approved for the treatment of glioblastoma [ 31 ].
Gold nanoparticles have raised interest because of their optical and electrical properties and low toxicity [ 32 – 34 ]. They are mainly used as contrast agents for X-ray imaging, computed tomography [ 25 ], photoacoustic imaging [ 35 ] and photodynamic therapy [ 36 ]. A nanoshell made of a silica core and a gold shell coated with PEG was approved by the Food and Drug Administration (FDA) in 2012 and commercialised as AuroShell (Nanospectra) for the treatment of breast cancer by photodynamic therapy [ 25 ].
Organic nanoparticles are mainly used as delivery systems for drugs. Liposomes and micelles are both made of phospholipids, but they differ in their morphology. Liposomes are spherical particles having at least one lipid bilayer, resembling the structure of cell membranes. They are mainly used to encapsulate hydrophilic drugs in their aqueous core, but hydrophobic drugs can also be accommodated in the bilayer or chemically attached to the particles [ 37 ]. Micelles, instead, own a hydrophobic core that can encapsulate hydrophobic drugs [ 38 ]. Doxil, doxorubicin-loaded PEGylated liposomes, were the first nanoparticles approved by the FDA in 1995 to treat AIDS-associated Kaposi’s sarcoma [ 39 ]. This formulation drastically reduces doxorubicin side effects. Since then, other liposomal formulations have been approved by the FDA for cancer therapy, such as Myocet and DaunoXome [ 40 – 42 ]. Polymeric nanoparticles are made of biocompatible or natural polymers, such as poly(lactide-co-glycolide), poly(ε-caprolactone), chitosan, alginate and albumin [ 43 ]. Some formulations have already been accepted by the FDA, such as Abraxane (albumin-paclitaxel particles for the treatment of metastatic breast cancer and pancreatic ductal adenocarcinoma) and Ontak (an engineered protein combining interleukin-2 and diphtheria toxins for the treatment of non-Hodgkin’s peripheral T-cell lymphomas).
As well as these systems, which have been either accepted or are under clinical investigation, it is worth mentioning some new nanoparticles currently undergoing testing at the research level, which should improve treatment performance. For example, solid lipid nanoparticles, made of lipids that are solid at body temperature [ 44 ], and fabricated to load hydrophobic drugs [ 45 ] have been demonstrated to give a higher drug stability and prolonged release compared to other systems; however, the encapsulation efficiency is often low because of their high crystallinity [ 46 ]. To overcome this issue, one or more lipids, liquid at room temperature (like oleic acid, for example), are included in the formulation [ 47 ]. Lipid nanoparticles are good candidates for brain tumour therapy as they are able to cross the blood–brain barrier (BBB) [ 48 ]. A recent work showed that lipid nanoparticles loaded with SPIONs and temozolomide are efficient to treat glioblastoma since they combine the effect of the conventional chemotherapy and hyperthermia [ 49 , 50 ]. Dendrimers are another family of nanoparticles composed of polymers with a repetitive branched structure and characterised by a globular morphology [ 51 , 52 ]. Their architecture can be easily controlled, making their structure extremely versatile for many applications. For example, some recent studies show that poly-L-lysine (PLL) dendrimers loaded with doxorubicin induce anti-angiogenic responses in in vivo tumour models [ 53 ]. Currently, there is only one clinical trial for a formulation named ImDendrim based on a dendrimer and on a rhenium complex coupled to an imidazolium ligand, for the treatment of inoperable liver cancers that do not respond to conventional therapies [ 54 ].
Extracellular vesicles for cancer diagnosis and therapy
EVs are classified in two categories based on their biogenesis. Specifically, exosomes are small vesicles of around 30–150 nm originated from endosomes in physiological and pathological conditions and released by a fusion of multivesicular bodies (MVBs) to the cell membrane [ 55 , 56 ], while shed microvesicles (sMVs), with a typical size of 50–1,300 nm, are present in almost any extracellular bodily fluid and are responsible for the exchange of molecular materials between cells [ 57 , 58 ]. Exosomes are involved in cancer development and spreading [ 3 , 59 , 60 ], in the bidirectional communication between tumour cells and surrounding tissues, and in the construction of the microenvironment needed for pre-metastatic niche establishment and metastatic progression [ 61 ]. Hence, circulating vesicles are clinically relevant in cancer diagnosis, prognosis and follow up. Exosomes are actually recognised as valid diagnostic tools, but they can also be isolated and exploited as anti-cancer vaccines or nanosized drug carriers in cancer therapy [ 62 ].
Nowadays, one of the main issues in cancer diagnosis is the early identification of biomarkers by non-invasive techniques. Obtaining a significant amount of information, before and during tumour treatment, should allow the monitoring of cancer progression and the efficacy of therapeutic regimens. Liquid biopsies to detect circulating tumour cells, RNAs, DNAs and exosomes have been used as indicators for personalised medicine [ 63 ]. In recent years, exosomes detection has been validated as a reliable tool for preclinical practice in different cancer types [ 64 ], thanks to the identification of their content: double-stranded DNA (dsDNA) [ 65 , 66 ], messenger RNA (mRNA), micro RNA (miRNA), long non-coding RNA (lncRNA) [ 67 ], proteins and lipids [ 68 ]. DsDNA has been detected in exosomes isolated from plasma and serum of different cancer cell types, and mutated genes involved in tumorigenesis, such as mutated KRAS and TP53 [ 69 , 70 ], have been identified as disease predictors. Similarly, exosomal AR-V7 mRNA has been used as a prognostic marker of resistance to hormonal therapy in metastatic prostate cancer patients [ 71 ]. Gene expression profiling of multiple RNAs from urinary exosomes has been adopted as an efficient diagnostic tool [ 72 ]. LncRNAs isolated from serum exosomes have been exploited for disease prognosis in colorectal cancer patients [ 73 ], and multiple miRNAs allow one to distinguish between different lung cancer subtypes [ 74 ]. GPC1-positive exosomes have been employed to detect pancreatic cancer [ 75 ], while circulating exosomal macrophage migration inhibitory factor (MIF) was able to predict liver metastasis onset [ 76 ]. Finally, multiple lipids present in urinary exosomes have been approved as prostate cancer indicators [ 77 ]. Due to the high variability of patient classes and sample size, and in order to obtain clinically significant results for a fast and effective diagnosis, huge investments in exosome research will be required in the near future.
Exosomes could also be exploited as natural, biocompatible and low immunogenic nanocarriers for drug delivery in cancer therapy. They can be passively loaded by mixing purified vesicles with small drugs [ 78 – 82 ], or actively loaded by means of laboratory techniques, such as electroporation and sonication [ 83 , 84 ]. Superparamagnetic nanoparticles conjugated to transferrin have been tested for the isolation of exosomes expressing transferrin receptor from mice blood. After incubation with doxorubicin, they have been used to target liver cancer cells in response to external magnetic fields, inhibiting cell growth both in vitro and in vivo [ 80 ]. Kim et al. [ 83 ] engineered mouse macrophage-derived exosomes with aminoethyl anisamide-PEG to target sigma receptor, overexpressed in lung cancer cells and passively loaded them with paclitaxel. These systems acted as targeting agents able to suppress metastatic growth in vivo .
Three clinical trials with loaded exosomes are currently ongoing for the treatment of different tumours [ 85 – 87 ]: a phase I trial is evaluating the ability of exosomes to deliver curcumin to normal and colon cancer tissues [ 85 ]; a phase II trial is investigating the in vivo performance of autologous tumour cell-derived microparticles carrying methotrexate in lung cancer patients [ 86 ] and a clinical inquiry is focusing on autologous erythrocyte-derived microparticles loaded with methotrexate for gastric, colorectal and ovarian cancer treatment [ 87 ].
Recently, new strategies to produce ad hoc exosomes have been developed. Cells releasing exosomes have been genetically engineered to overexpress specific macromolecules, or modified to release exosomes with particular targeting molecules [ 88 – 90 ].
Exosomes derived from different cancer cells have already been exploited as cancer vaccines. Autologous dendritic cell-derived exosomes with improved immunostimulatory function have been tested in a phase II clinical trial for the activation of CD8 + T cells [ 91 ] in non-small cell lung cancer (NSCLC) patients, observing disease stabilisation and a better overall survival [ 92 ]. In a phase I trial, ascites-derived exosomes supplemented with granulocyte-macrophage colony stimulating factor (GM-CSF) have been administered to colorectal cancer patients, soliciting a tumour-specific immune response [ 93 ].
Many issues related to exosomes clinical translation remain open and are mostly connected to the definition of preclinical procedures for isolation, quantification, storage and standard protocols for drug loading. It is becoming even more necessary to distinguish between tumour and healthy blood cell-derived vesicles to characterise their post-isolation half-life and to perform standard content analyses. For these purposes, innovative approaches and technologies have been set up, such as microarrays and specific monoclonal antibodies and RNA markers amplification strategies [ 94 ].
Natural antioxidants in cancer therapy
Every day, the human body undergoes several exogenous insults, such as ultraviolet (UV) rays, air pollution and tobacco smoke, which result in the production of reactive species, especially oxidants and free radicals, responsible for the onset of many diseases, including cancer. These molecules can also be produced as a consequence of clinical administration of drugs, but they are also naturally created inside our cells and tissues by mitochondria and peroxisomes, and from macrophages metabolism, during normal physiological aerobic processes.
Oxidative stress and radical oxygen species are able to damage DNA (genetic alterations, DNA double strand breaks and chromosomal aberrations [ 95 , 96 ]) and other bio-macromolecules [ 97 ], such as lipids (membrane peroxidation and necrosis [ 98 ]) and proteins (significantly changing the regulation of transcription factors and, as a consequence, of essential metabolic pathways [ 99 ]).
The protective mechanisms our body has developed against these molecules are sometimes insufficient to counteract the huge damages produced. Recently, in addition to research into the roles of the physiological enzymes superoxide dismutase (SOD), catalase (CAT) and glutathione peroxidase (GP), natural antioxidants such as vitamins, polyphenols and plant-derived bioactive compounds are being studied in order to introduce them as preventive agents and potential therapeutic drugs [ 100 , 101 ]. These molecules have anti-inflammatory and anti-oxidant properties and are found in many vegetables and spices [ 102 ]. Vitamins, alkaloids, flavonoids, carotenoids, curcumin, berberine, quercetin and many other compounds have been screened in vitro and tested in vivo , displaying appreciable anti-proliferative and pro-apoptotic properties, and have been introduced as complementary therapies for cancer [ 4 , 5 , 103 ].
Despite the advantages of using natural drugs, their translation into clinical practice remains difficult due to their limited bioavailability and/or toxicity. Curcumin, a polyphenolic compound extracted from turmeric ( Curcuma longa ), is a traditional Southeast Asian remedy with anti-inflammatory, anti-oxidant and chemopreventive and therapeutic activities [ 104 ]. It has been shown to have cytotoxic effects in different kinds of tumours, such as brain, lung, leukaemia, pancreatic and hepatocellular carcinoma [ 105 , 106 ], with no adverse effects in normal cells at the effective therapeutic doses [ 107 ]. Curcumin can modulate a plethora of cellular mechanisms [ 108 , 109 ]; however, its biological properties, and as a consequence, the treatment duration and the efficient therapeutic doses, have not been completely elucidated yet. This molecule is highly lipophilic, poorly soluble in water and not very stable [ 110 ]. Different strategies and specific carriers, such as liposomes and micelles [ 111 , 112 ], have been developed to improve its bioavailability. Currently, 24 clinical trials involving curcumin are ongoing and 23 have been already completed [ 113 ].
Berberine is an alkaloid compound extracted from different plants, such as Berberis . Recently, it has been demonstrated to be effective against different tumours and to act as a chemopreventive agent, modulating many signalling pathways [ 114 , 115 ]. Like curcumin, it is poorly soluble in water; therefore, different nanotechnological strategies have been developed to facilitate its delivery across cell membranes [ 116 – 119 ]; six clinical trials are open and one has been completed [ 120 ].
Quercetin, a polyphenolic flavonoid found in fruits and vegetable, has been proven to be effective to treat several tumours, such as lung, prostate, liver, colon and breast cancers [ 121 – 123 ], by binding cellular receptors and interfering with many signalling pathways [ 124 ]. Interestingly, it has been shown to be effective also in combination with chemotherapeutic agents [ 125 ]. Presently, seven clinical trials are open and four have been completed [ 126 ].
Targeted therapy and immunotherapy
One of the main problems of conventional cancer therapy is the low specificity of chemotherapeutic drugs for cancer cells. In fact, most drugs act both on healthy and diseased tissues, generating severe side effects. Researchers are putting a lot of effort into finding a way to target only the desired site. Nanoparticles have raised great interest for their tendency to accumulate more in tumour tissues due to the enhanced permeability and retention effect (EPR) [ 127 ]. This process, called passive targeting, relies on the small size of nanoparticles and the leaky vasculature and impaired lymphatic drainage of neoplastic tissues [ 6 ]. Passive targeting, however, is difficult to control and can induce multidrug resistance (MDR) [ 128 ]. Active targeting, on the other hand, enhances the uptake by tumour cells by targeting specific receptors that are overexpressed on them [ 129 , 130 ]. Nanoparticles, for example, can be functionalized with ligands that univocally bind particular cells or subcellular sites [ 6 ]. Several kinds of ligands can be used, such as small molecules, peptides, proteins, aptamers and antibodies.
Folic acid and biotin are small molecules, whose receptors are overexpressed in tumour tissues. Several nanocarriers have been functionalized with folic acid to target ovarian and endometrial cancers [ 131 ]: folic acid-conjugated polyethylene glycol-poly(lactic-co-glycolic acid) nanoparticles delivering docetaxel increased drug cellular uptake by human cervical carcinoma cells [ 132 ]. Small ligands are cheap and can be linked to nanoparticles by simple conjugation chemistry [ 133 , 134 ].
Different kinds of small peptides and proteins are also effective in active targeting. Angiopep-2 is a peptide that has raised great interest in the treatment of brain cancer [ 135 ], because it binds to low-density lipoprotein receptor-related protein-1 (LRP1) of endothelial cells in the BBB, and it is also overexpressed in glioblastoma cancer cells [ 136 ]. Bombesin peptide conjugated to poly(lactic-co-glycolic acid) (PLGA) nanoparticles loaded with docetaxel was used to target the gastrin-releasing peptide receptor, overexpressed on cell surface of prostate, breast, ovarian, pancreatic and colorectal cancer cells [ 137 , 138 ]. Transferrin is a serum glycoprotein overexpressed on many solid tumours, especially on glioblastoma multiforme cells [ 139 ], and on epithelial cells of the BBB [ 6 , 140 ]. Transferrin-conjugated chitosan-PEG nanoparticles delivering paclitaxel exhibited a higher cytotoxicity towards transferrin-overexpressing human non-small cell lung cancer cells (NSCLCs) (HOP-62) [ 141 ].
Aptamers are small synthetic single-stranded RNA or DNA oligonucleotides folded into specific shapes that make them capable of binding specific targets [ 142 ]. Farokhzad et al. [ 143 ] reported that the use of A10 RNA aptamer conjugated to docetaxel-loaded nanoparticles significantly enhances in vitro cytotoxicity. The same aptamer has been also used to prepare quantum dot-doxorubicin conjugates [ 144 ].
Antibodies are currently the most exploited ligands for active targeting. These proteins have a typical ‘Y’ shape, where the two arms are responsible for the selective interaction with the antigen [ 145 ]. Antibodies can be used as immunoconjugates, when conjugated to a drug or nanoparticle, or naked. In the first case, their function is mainly to target a specific antigen overexpressed on cancer cells. Antibodies used for this purpose include those ones that bind to the human epidermal growth factor receptor 2 (HER2), the epidermal growth factor receptor (EGFR), the transferrin receptor (TfR) and the prostate-specific membrane antigen (PSMA) [ 6 ]. Rapamycin-PLGA nanoparticle conjugated to EGFR antibody exhibited higher cellular uptake by human breast adenocarcinoma cells (MCF-7), with enhanced apoptotic activity [ 146 ]. Loperamide-loaded human serum albumin nanoparticles conjugated to antibodies that specifically bind transferrin receptor successfully crossed the BBB and delivered the drug to the desired site [ 147 ].
Naked antibodies or immunoconjugates can also be used in immunotherapy, which is a cancer treatment that aims at stimulating or restoring the immune system of the patient against cancer cells [ 148 ]. Antibodies can act as markers for cancer cells to make them more vulnerable to the immune system response (non-specific immune stimulation), or as inhibitors for immune checkpoint proteins on cancer cell surface, that can modulate the action of T-cells [ 148 ]. Several antibodies have been already tested and accepted by FDA for immunotherapy, such as rituximab (1997, [ 149 ]), ibritumomab tiuxetan (2002, [ 150 ]), trastuzumab emtansine (2013, [ 151 ]), nivolumab (2014, [ 152 ]) and pembrolizumab (2014, [ 153 ]).
Immunotherapy can be achieved by another strategy called adoptive cell transfer (ACT) and it consists of isolating T-lymphocytes (T-cells) with the highest activity against cancer directly from the patient’s blood, expanding them ex vivo , and reinfusing them again into the patient [ 154 ]. Autologous T-cells can be genetically engineered in vitro to express a chimaeric antigen receptor (CAR), which makes them more specific against cancer cell antigens [ 148 ]. Different CARs can be designed to be directed against a certain cancer antigen. The genetic modification of T-cells can be achieved by different methods such as viral transduction, non-viral methods like DNA-based transposons, CRISPR/Cas9 or other plasmid DNA and mRNA transfer techniques (i.e., electroporation, encapsulation in nanoparticles) [ 155 ]. ACT protocols have been already adopted in clinical practice for advanced or recurrent acute lymphoblastic leukaemia and for some aggressive forms of non-Hodgkin’s lymphoma [ 148 ]. For example, it has been shown that the treatment of end-stage patients affected by acute lymphocytic leukaemia with CAR T-cells led to a full recovery in up to 92% of patients [ 155 ]. Despite these very promising results, much research is currently devoted to understanding the long-term side effects of CAR T-cell therapies and their fate within tumours, and to improving CAR T-cell expansion technologies.
Gene therapy for cancer treatment
Gene therapy is intended as the introduction of a normal copy of a defective gene in the genome in order to cure specific diseases [ 156 ]. The first application dates back to 1990 when a retroviral vector was exploited to deliver the adenosine deaminase (ADA) gene to T-cells in patients with severe combined immunodeficiency (SCID) [ 157 ]. Further research demonstrated that gene therapy could be applied in many human rare and chronic disorders and, most importantly, in cancer treatment. Approximately 2,900 gene therapy clinical trials are currently ongoing, 66.6% of which are related to cancer [ 158 ]. Different strategies are under evaluation for cancer gene therapy: 1) expression of pro-apoptotic [ 159 , 160 ] and chemo-sensitising genes [ 4 ]; 2) expression of wild type tumour suppressor genes [ 5 ]; 3) expression of genes able to solicit specific antitumour immune responses and 4) targeted silencing of oncogenes.
One approach relied on thymidine kinase (TK) gene delivery, followed by administration of prodrug ganciclovir to activate its expression and induce specific cytotoxicity [ 161 ]. This has been clinically translated for the treatment of prostate cancer and glioma [ 162 – 164 ]. In recent decades, different vectors carrying the p53 tumour suppressor gene have been evaluated for clinical applications. ONYX-015 has been tested in NSCLC patients and gave a high response rate when administered alone or together with chemotherapy [ 165 ]. Gendicine, a recombinant adenovirus carrying wild-type p53 in head and neck squamous cell cancer had a similar success, inducing complete disease regression when combined with radiotherapy [ 166 ].
Despite many achievements, there are still some challenges to face when dealing with gene therapy, such as the selection of the right conditions for optimal expression levels and the choice of the best delivery system to univocally target cancer cells. Gene therapy also presents some drawbacks linked to genome integration, limited efficacy in specific subsets of patients and high chances of being neutralised by the immune system. Therefore, particular interest has been elicited by targeted gene silencing approaches.
RNA interference (RNAi) has been recently established as an efficient technology both for basic research and medical translation. Small interfering RNAs (siRNAs) consist of double-stranded RNAs [ 167 ] able to produce targeted gene silencing. This process is intracellularly mediated by the RNA-induced silencing complex (RISC), responsible for cleaving the messenger RNA (mRNA), thus leading to interference with protein synthesis [ 168 ]. This physiological mechanism has been demonstrated in many eukaryotes, including animals. A few years after RNAi discovery, the first clinical application for wet-age related macular degeneration treatment entered phase I clinical trial [ 169 ]. Since cancer is triggered by precise molecular mechanisms, siRNAs can be rationally designed to block desired targets responsible for cell proliferation and metastatic invasion. This strategy relies on siRNA-mediated gene silencing of anti-apoptotic proteins [ 170 ], transcription factors (i.e., c-myc gene) [ 171 , 172 ] or cancer mutated genes (i.e., K-RAS ) [ 173 ]. Most of the clinical trials currently ongoing are based on local administration of siRNA oligonucleotides in a specific tissue/organ or on systemic delivery throughout the entire body [ 9 , 174 ]. Using siRNA-based drugs has several advantages: 1) safety, since they do not interact with the genome; 2) high efficacy, because only small amounts can produce a dramatic gene downregulation; 3) possibility of being designed for any specific target; 4) fewer side effects when compared to conventional therapies and 5) low costs of production [ 175 , 176 ]. However, siRNAs are relatively unstable in vivo and can be phagocytosed during blood circulation, excreted by renal filtration, or undergo enzymatic degradation [ 177 ]. Occasionally, they can induce off-target effects [ 178 ] or elicit innate immune responses, followed by specific inflammation [ 179 , 180 ]. Since naked siRNAs are negatively charged hydrophilic molecules, they cannot spontaneously cross cell membranes. Consequently, different delivery strategies are currently under study, such as chemical modification, encapsulation into lipid or polymeric carriers or conjugation with organic molecules (polymers, peptides, lipids, antibodies, small molecules [ 181 ], for efficient targeting [ 182 , 183 ]). Chemical modifications include the insertion of a phosphorothioate at 3’ end to reduce exonuclease degradation [ 184 ], the introduction of 2’ O-methyl group to obtain longer half-life in plasma [ 185 ] and the modification by 2,4-dinitrophenol to favour membrane permeability [ 186 ]. Nevertheless, the degradation of modified siRNAs often elicits cytotoxic effects; therefore, it is preferable to design ad hoc nanocarriers.
Different cationic lipid nanoparticles, such as liposomes, micelles and solid lipid nanoparticles [ 183 ], have been exploited for siRNA loading. Cationic liposomes interact with negatively charged nucleic acids, which can be easily transfected by simple electrostatic interactions [ 187 , 188 ]. They can be constituted by 1,2-dioleoyl-3-trimethylammonium propane (DOTAP) and N-{1-(2,3-dioleoyloxy) propyl]-N,N,N-trimethylammonium methyl sulphate (DOTMA) [ 189 ]. A theranostic agent consisting of an anticancer survivin siRNA entrapped in PEGylated liposomes has been developed to achieve simultaneous localisation inside tumour cells by means of entrapped MR agents and fluorophores and reduction of proliferation in vivo [ 190 ].
Neutral liposomes based on 1,2-dioleoyl-sn-glycero-3-phosphatidylcholine (DOPC) have shown high efficacy in mice models of ovarian carcinoma and colorectal cancer [ 191 , 192 ]. A phase I clinical trial is currently recruiting patients for evaluating the safety of siRNA-EphA2-DOPC when administered to patients with advanced and recurrent cancer [ 193 ].
Stable nucleic acid lipid particles (SNALPs) have been evaluated in non-human primates [ 194 ]. SiRNAs have been encapsulated in a mixture of cationic lipids coated with a shell of polyethylene glycol (PEG) [ 195 ]. SNALPs entered a phase I clinical trial in patients affected by advanced solid tumours with liver involvement [ 196 ] and a phase I/II trial for treating neuroendocrine tumours and adrenocortical carcinoma patients refractory to standard therapy [ 197 ].
SiRNAs can be condensed in cationic polymers such as chitosan, cyclodextrin and polyethylenimine (PEI). Chitosan is a natural polysaccharide that, due to its cationic charge, has been exploited as carrier for nucleic acids in vitro and in vivo [ 198 ]. Specifically, a targeted siRNA has been delivered in mice xenografts of breast cancer [ 199 ]. Cyclodextrin polymers coated with PEG, conjugated with human transferrin and carrying a siRNA called CALAA-01, inhibit tumour growth by reducing the expression of M2 subunit of ribonucleotide reductase (R2), and have entered a phase I clinical trial [ 200 ]. PEI is able to form small cationic nanoparticles containing siRNAs and it has been exploited as antitumoural, upon loading with HER-2 receptor-specific siRNA [ 201 ]. A phase II clinical trial is presently starting to evaluate siG12D LODER directed to mutated KRAS oncogene and encapsulated into a biodegradable polymeric matrix for locally treating advanced pancreatic cancer patients in combination with chemotherapy [ 202 ].
SiRNAs may be conjugated to peptides, antibodies and aptamers in order to improve their stability during circulation and to enhance cellular uptake [ 203 ]. A success is represented by siRNAs targeting PSMA, overexpressed in this type of cancer [ 204 ].
The introduction of nanocarriers has largely improved siRNAs stability, pharmacokinetics and biodistribution properties, and the targeting specificity [ 205 , 206 ]. Smart nanomaterials responsive to external (i.e., magnetic field, ultrasounds) and tumour-specific stimuli (i.e., acidic pH, redox conditions) are currently under the development for controlled release and reduction of undesired negative effects [ 207 , 208 ]. Nanocarriers delivering siRNAs undergo a series of pH variations from blood circulation to intracellular environment and, for this reason, many pH responsive materials have been designed to favour cargo release under specific pH conditions [ 209 ]. Poly(allylamine) phosphate nanocarriers, stable at physiological pH, have been developed to release siRNAs in the cytoplasm after disassembly at low endosomal pH [ 210 ].
Although there have been many successes, some questions remain open and make the clinical translation of the siRNA-based approach very challenging, such as the correct doses to be delivered to patients and the many variabilities observed between individuals and different stages of disease. Further research towards controlled release to reach only specific targets, and the set-up of the best personalised therapy for cancer patients will be necessary in the near future.
Thermal ablation and magnetic hyperthermia
Thermal ablation of tumours includes a series of techniques that exploit heat (hyperthermia) or cold (hypothermia) to destroy neoplastic tissues [ 13 ]. It is known that cell necrosis occurs at temperatures lower than -40°C or higher than 60°C. Long exposures to temperatures between 41°C and 55°C are also effective for tumour cell damage. Moreover, it has been shown that cancer cells are more sensitive to high temperatures than healthy ones [ 211 ].
Hypothermic ablation is due to the formation of ice crystals upon cooling, which destroy cell membranes and finally kill cells. Argon gas is the preferred cooling agent because it can cool down the surrounding tissues to -160°C. Also, gases at their critical point, such as nitrogen, can be exploited since they have a higher heat capacity than argon. However, the technology to control and direct them is not well developed yet [ 10 ].
Hyperthermic ablation currently comprises radiofrequency (RF), microwave and laser ablation [ 10 ].
RF ablation is the most used in clinics, because it is effective and safe [ 212 ]. An alternated current of RF waves is applied to a target zone by an insulated electrode tip, while a second electrode, needed to close the circuit, is placed on the skin surface [ 10 ]. The interaction with the current causes the oscillation of ions in the extracellular fluid, which, in turns, produces heat. The more conductive the medium, the more effective the process. For this reason, RF ablation works very well in the liver and in other areas with a high content of water and ions, whereas it has a poor effect in lungs [ 10 ]. Moreover, the efficiency of the treatment decreases with the size of the lesion, giving the best results for areas not larger than 3 cm 2 [ 213 , 214 ].
Microwave ablation is based on the electromagnetic interaction between microwaves and the polar molecules in tissues, like water, that causes their oscillation and the consequent increase in temperature. Unlike the electrical current in RF ablation, microwaves can propagate through any kind of tissue [ 215 , 216 ], and this allows high temperatures to be reached in a short amount of time, to have a deeper penetration and to treat larger areas of tumours [ 217 ].
Laser therapy exploits the properties of laser beams of being very narrow and extremely focused at a specific wavelength. This makes the treatment very powerful and precise, thus a promising alternative to conventional surgery [ 218 ]. The absorption of the light emitted by the laser results in the heating and subsequent damage of the treated area [ 219 ]. Depending on the specific application, different kinds of lasers can be used. Neodymium:yttrium-aluminium-garnet (Nd:YAG) lasers (wavelength of 1064 nm) and diode lasers (wavelength of 800–900 nm) are used to treat internal organs, since they have a penetration depth up to 10 cm [ 218 ]. Conversely, CO 2 lasers (10,600 nm), with a penetration depth of 10 μm up to 1 mm maximum are used for superficial treatments. Laser therapy is receiving a lot of attention in research because of its advantages compared to other ablation techniques, such as a higher efficacy, safety and precision, and a shorter treatment session needed to achieve the same results [ 220 , 221 ]. Moreover, the fibres to transmit laser light are compatible with MRI, allowing for a precise measure of the temperature and the thermal dose [ 222 ]. However, there are still some limitations to overcome, such as the need of a very skilled operator to place the fibre in the correct position [ 218 ].
Finally, a new way to heat tumour tissues, currently under study, is through magnetic hyperthermia. This technique exploits superparamagnetic or ferromagnetic nanoparticles that can generate heat after stimulation with an alternating magnetic field. The most studied systems in nanomedicine are SPIONs [ 11 ]. The production of heat, in this case, is due to the alignment of magnetic domains in the particles when the magnetic field is applied, and the subsequent relaxation processes (Brownian and/or Neel relaxations) during which heat is released, when the magnetic field is removed and the magnetisation of the particles reverts to zero [ 223 ]. Magnetic hyperthermia can reach any area of the body and SPIONs can also act as MRI contrast agents to follow their correct localisation before the stimulation. The particles can be coated with biocompatible polymers and/or lipid and functionalized with specific ligands to impart targeting properties [ 224 ]. As already mentioned, until now, just a formulation of 15-nm iron oxide nanoparticles coated with aminosilane (Nanotherm) obtained approval for the treatment of glioblastoma [ 31 ]. SPIONs have also been successfully encapsulated in lipid nanocarriers together with a chemotherapeutic agent to combine chemotherapy and hyperthermia [ 49 , 50 ].
Recent innovations in cancer therapy: Radiomics and pathomics
Efficient cancer therapy currently relies on surgery and, in approximately 50% of patients, on radiotherapy, that can be delivered by using an external beam source or by inserting locally a radioactive source (in this case, the approach is named brachytherapy), thus obtaining focused irradiation. Currently, localisation of the beam is facilitated by image-guided radiotherapy (IGRT), where images of the patient are acquired during the treatment allowing the best amount of radiation to be set. Thanks to the introduction of intensity-modulated radiotherapy (IMRT), radiation fields of different intensities can be created, helping to reduce doses received by healthy tissues and thus limiting adverse side effects. Finally, by means of stereotactic ablative radiotherapy (SABR), it has become feasible to convey an ablative dose of radiation only to a small target volume, significantly reducing undesired toxicity [ 225 ].
Unfortunately, radioresistance can arise during treatment, lowering its efficacy. This has been linked to mitochondrial defects; thus, targeting specific functions have proven to be helpful in restoring anti-cancer effects [ 226 ]. A recent study has shown, for example, that radioresistance in an oesophageal adenocarcinoma model is linked to an abnormal structure and size of mitochondria, and the measurement of the energy metabolism in patients has allowed discrimination between treatment resistant and sensitive patients [ 227 ]. Targeting mitochondria with small molecules acting as radiosensitizers is being investigated for gastrointestinal cancer therapy [ 228 ].
Cancer is a complex disease and its successful treatment requires huge efforts in order to merge the plethora of information acquired during diagnostic and therapeutic procedures. The ability to link the data collected from medical images and molecular investigations has allowed an overview to be obtained of the whole tridimensional volume of the tumour by non-invasive imaging techniques. This matches with the main aim of precision medicine, which is to minimise therapy-related side effects, while optimising its efficacy to achieve the best individualised therapy [ 229 ].
Radiomics and pathomics are two promising and innovative fields based on accumulating quantitative image features from radiology and pathology screenings as therapeutic and prognostic indicators of disease outcome [ 12 , 13 , 230 ]. Many artificial intelligence technologies, such as machine learning application, have been introduced to manage and elaborate the massive amount of collected datasets and to accurately predict the treatment efficacy, the clinical outcome and the disease recurrence. Prediction of the treatment response can help in finding an ad hoc adaptation for the best prognosis and outcome. Nowadays, personalised medicine requires an integrated interpretation of the results obtained by multiple diagnostic approaches, and biomedical images are crucial to provide real-time monitoring of disease progression, being strictly correlated to cancer molecular characterisation.
Radiomics is intended as the high throughput quantification of tumour properties obtained from the analysis of medical images [ 14 , 15 , 231 ]. Pathomics, on the other side, relies on generation and characterisation of high-resolution tissue images [ 16 , 232 , 233 ]. Many studies are focusing on the development of new techniques for image analysis in order to extrapolate information by quantification and disease characterisation [ 234 , 235 ]. Flexible databases are required to manage big volumes of data coming from gene expression, histology, 3D tissue reconstruction (MRI) and metabolic features (positron emission tomography, PET) in order to identify disease phenotypes [ 236 , 237 ].
Currently, there is an urgent need to define univocal data acquisition guidelines. Some initiatives to establish standardised procedures and facilitate clinical translation have been already undertaken, such as quantitative imaging network [ 238 ] or the German National Cohort Consortium [ 239 ]. Precise description of the parameters required for image acquisition and for the creation and use of computational and statistical methods are necessary to set robust protocols for the generation of models in radiation therapy. According to the US National Library of Medicine, approximately 50 clinical trials involving radiomics are currently recruiting patients, and a few have already been completed [ 240 ].
Conclusions and future perspectives
In recent years, research into cancer medicine has taken remarkable steps towards more effective, precise and less invasive cancer treatments ( Figure 1 ). While nanomedicine, combined with targeted therapy, helped improving the biodistribution of new or already tested chemotherapeutic agents around the specific tissue to be treated, other strategies, such as gene therapy, siRNAs delivery, immunotherapy and antioxidant molecules, offer new possibilities to cancer patients. On the other hand, thermal ablation and magnetic hyperthermia are promising alternatives to tumour resection. Finally, radiomics and pathomics approaches help the management of big data sets from cancer patients to improve prognosis and outcome.

At the moment, the most frequent entries concerning cancer therapies in the database of clinical trials ( www.clinicaltrials.gov ) involve the terms targeted therapy, immunotherapy and gene therapy, highlighting that these are the most popular methodologies under investigation, especially because, as already mentioned before, they have been shown to be very promising and effective ( Figure 2A ). However, Figure 2B shows that the clinical trials started in the past decade on different therapies mentioned in this review (except for liposomes-based therapies) have increased in number, showing how the interest on these new approaches is quickly growing in order to replace and/or improve conventional therapies. In particular, radiomics, immunotherapy and exosomes are the entries whose number has increased the most in the last 10 years.

The current scenario for cancer research is wide, offering many possibilities for the constant improvement of treatment, considering not only patient recovery but also caring for their well-being during therapy. As summarised in Table 1 , these new approaches offer many advantages compared to conventional therapies. However, some disadvantages still have to be overcome to improve their performances. Much progress has been made, but many others are likely to come in the near future, producing more and more ad hoc personalised therapies.
Conflicts of interest
The authors declare that they have no conflict of interest.
Funding declaration
This work was partially supported by the Fondazione CaRiPLo, grant no. 2018-0156 (Nanotechnological countermeasures against Oxidative stress in muscle cells Exposed to Microgravity—NOEMI) and by the European Research Council (ERC) under the European Union’s Horizon 2020 Research and Innovation Programme (grant agreement N°709613, SLaMM).
Authors’ contributions
Carlotta Pucci and Chiara Martinelli contributed equally to this work.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 23 September 2014
Clinical cancer research: the past, present and the future
- Vincent T. DeVita Jr 1 ,
- Alexander M. M. Eggermont 2 ,
- Samuel Hellman 3 &
- David J. Kerr 4
Nature Reviews Clinical Oncology volume 11 , pages 663–669 ( 2014 ) Cite this article
3666 Accesses
25 Citations
20 Altmetric
Metrics details
- Cancer immunotherapy
- Clinical trials
- Drug development
- Targeted therapies
In the past decade, we have witnessed unprecedented changes and some remarkable advances that have enabled true personalized medicine. Nevertheless, many challenges in clinical cancer research remain and need to be overcome if we are to witness similar progress in the next decade. Such hurdles include, but are not limited to, clinical development and testing of multiple agents in combination, design of clinical trials to best accommodate the ever increasing knowledge of heterogeneity of the disease, regulatory challenges relating to drug development and trial design, and funding for basic research. With this in mind, we asked four leading cancer researchers from around the world, and who have been associated with the journal since its launch in November 2004 what, in their opinion, we have learnt over the past 10 years and how we should progress in the next 10 years.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Evolutionary trajectories of small cell lung cancer under therapy
Julie George, Lukas Maas, … Roman K. Thomas

Antibody drug conjugate: the “biological missile” for targeted cancer therapy
Zhiwen Fu, Shijun Li, … Yu Zhang

Optimizing the safety of antibody–drug conjugates for patients with solid tumours
Paolo Tarantino, Biagio Ricciuti, … Sara M. Tolaney
Kochenderfer, J. N. et al . Eradication of B-lineage cells and regression of lymphoma in a patient treated with autologous T cells genetically engineered to recognize CD19. Blood 116 , 4099–4102 (2010).
Article CAS Google Scholar
Tran, E. et al . Cancer immunotherapy based on mutation-specific CD4+ T cells in a patient with epithelial cancer. Science 344 , 641–645 (2014).
Simeone, E. & Ascierto, P. A. Immunomodulating antibodies in the treatment of metastatic melanoma: the experience with anti-CTLA-4, anti-CD137 and anti-PD1. J. Immunotoxicol. 9 , 241–247 (2012).
Ascierto, P. A. et al . Clinical experiences with anti-CD137 and anti-PD1 therapeutic antibodies. Semin. Oncol. 37 , 508–516 (2010).
Flaherty, K. T., Puzanov, I. & Chapman, P. B. Inhibition of mutated, activated BRAF in metastatic melanoma. N. Engl. J. Med. 363 , 809–819 (2010).
Lynch, T. J. et al . Activating mutations in the epidermal growth factor receptor underlying responsiveness on non-small-cell lung cancer to gefitinib. N. Engl. J. Med. 350 , 2129–2139 (2004).
Shaw, A. T. et al . Effect of crizotinib on overall survival in patients with advanced non-small-cell lung cancer harbouring ALK gene rearrangement: a retrospective analysis. Lancet Oncol. 12 , 1004–1012 (2011).
Eggermont, A. M., Spatz, A. & Robert, C. Cutaneous melanoma. Lancet 383 , 816–827 (2014).
Hodi, F. S. et al . Improved survival with ipilimumab in patients with metastatic melanoma. N. Engl. J. Med. 363 , 711–723 (2010).
Topalian, S. L. et al . Survival, durable tumour remission, and long-term safety in patients with advanced melanoma receiving nivolumab. J. Clin. Oncol. 32 , 1020–1030 (2014).
Robert, C. et al . Anti-programmed-death-receptor-1 treatment with pembrolizumab in ipilimumab-refractory advanced melanoma: a randomised dose-comparison cohort of a phase 1 trial. Lancet http://dx.doi.org/10.1016/S0140-6736(14)60958-2 (2014).
Brahmer, J. R. et al . Survival and long-term follow-up of the phase I trial of nivolumab (anti-PD-1; BMS-936558; ONO-4538) in patients (pts) with previously treated advanced non-small cell lung cancer (NSCLC) [abstract]. J. Clin. Oncol. 31 (Suppl.), a8030 (2013).
Google Scholar
Powles, T. et al . Inhibition of PD-L1 by MPDL3280A and clinical activity in pts with metastatic urothelial bladder cancer (UBC) [abstract]. J. Clin. Oncol. 32 (Suppl.), a5011 (2014).
Article Google Scholar
Wolchok, J. D. et al . Nivolumab plus ipilimumab in advanced melanoma. N. Engl. J. Med. 369 , 122–133 (2013).
Eggermont, A. M. & Robert, C. Melanoma: smart therapeutic strategies in immuno-oncology. Nat. Rev. Clin. Oncol. 11 , 181–182 (2014).
Peggs, K. S., Quezada, S. A., Chambers, C. A., Korman, A. J. & Allison, J. P. Blockade of CTLA-4 on both effector and regulatory T cell compartments contributes to the antitumour activity of anti-CTLA-4 antibodies. J. Exp. Med. 206 , 1717–1725 (2009).
Kraman, M. et al . Suppression of antitumour immunity by stromal cells expressing fibroblast activation protein-alpha. Science 330 , 827–830 (2010).
Hinrichs, C. S. & Rosenberg, S. A. Exploiting the curative potential of adoptive T-cell therapy for cancer. Immunol. Rev. 257 , 56–71 (2014).
Lee, Y. et al . Therapeutic effects of ablative radiation on local tumour require CD8+ T cells: changing strategies for cancer treatment. Blood 114 , 589–595 (2009).
Garcia-Barros, M. et al . Tumour response to radiotherapy regulated by endothelial cell apoptosis. Science 300 , 1155–1159 (2003).
Lussier, Y. A. et al . Oligo and polymetastatic progression in lung metastasis(es) patients is associated with specific microRNAs. PLoS ONE 7 , e50141 (2012).
La Thangue, N. B. & Kerr, D. J. Predictive biomarkers: a shift towards personalised cancer medicine. Nat. Rev. Clin. Oncol. 8 , 587–596 (2011).
Kerr, D. J. & Kakil, I. R. Targeted therapies: cetuximab plus chemotherapy in patients with advanced cancer. Nat. Rev. Clin. Oncol. 6 , 499–500 (2009).
Ou, S.-H. I. et al . Efficacy and safety of crizotinib in patients with advanced ROS1 -rearranged non-small cell lung cancer (NSCLC) [abstract]. J. Clin. Oncol. 31 (Suppl.), a8032 (2013).
Dilts, D. M. et al . Development of clinical trials in a cooperative group setting: The Eastern Cooperative Oncology Group. Clin. Cancer Res. 14 , 3427–3433 (2008).
Lacombe, D. et al . European perspective for effective cancer drug development. Nat. Rev. Clin. Oncol. 11 , 492–498 (2014).
Edwards, A. M., Bountra, C., Kerr, D. J. & Willson, T. M. Open access chemical and clinical probes to support drug discovery. Nat. Chem. Biol. 5 , 436–440 (2009).
Prahallad, A. et al . Unresponsiveness of colon cancer to BRAF(V600E) inhibition through feedback activation of EGFR. Nature 483 , 100–103 (2012).
Ward, P. S. & Thompson, C. B. Metabolic reprogramming: a cancer hallmark even warburg did not anticipate. Cancer Cell 21 , 297–308 (2012).
Heimann, R. & Hellman, S. Clinical progression of breast cancer malignant behaviour: what to expect and when to expect it. J. Clin. Oncol. 18 , 591–599 (2000).
Coussens, L. & Werb, Z. Inflammation and cancer. Nature 420 , 860–867 (2002).
Cogent Study Group. Meta-analysis of genome-wide association data identifies four new susceptibility loci for colorectal cancer. Nat. Genet. 40 , 1426–1435 (2008).
Liao, M. et al . Aspirin use, PIK3C mutation and colorectal cancer survival. N. Engl. J. Med. 367 , 1596–1606 (2012).
Domingo, E. et al . Evaluation of PIK3CA mutation as a predictor of benefit from nonsteroidal anti-inflammatory drug therapy in colorectal cancer. J. Clin. Oncol. 31 , 4297–4305 (2013).
Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell 144 , 646–674 (2011).
Hanahan, D. & Weinberg, R. A. Hallmarks of Cancer: an organizing principle for cancer medicine. Cancer: Principles & Practice of Oncology . 10th edn, Ch. 2 (in press, November 2014).
Dunn, G. P., Old, L. J. & Schreiber, R. D. The three Es of cancer immunoediting. Annu. Rev. Immunol. 22 , 329–360 (2004).
Grey, R. et al . Validation study of a quantitative multi-gene RT-PCR assay as a predictor of recurrence in stage II colon cancer patient. J. Clin. Oncol. 12 , 4611–4619 (2011).
Church, D. et al . Toxgnostics: an unmet need in cancer medicine. Nat. Rev. Cancer 14 , 440–445 (2014).
Download references
Author information
Authors and affiliations.
Yale Comprehensive Cancer Center, FMP 117, 333 Cedar Street, New Haven, 06519, CT, USA
Vincent T. DeVita Jr
Cancer Institute, Gustave Roussy Cancer Campus, Grand Paris, 114 rue Édouard Vaillant, Villejuif, 94805, France
Alexander M. M. Eggermont
Department of Radiation and Cellular Oncology, The Ludwig Center for Metastasis Research, The University of Chicago Medical Center, 5758 South Maryland Avenue, Chicago, 60637, IL, USA
Samuel Hellman
Radcliffe Department of Medicine, University of Oxford, Headley Way, Oxford, OX3 9DU, UK
David J. Kerr
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Vincent T. DeVita Jr , Alexander M. M. Eggermont , Samuel Hellman or David J. Kerr .
Ethics declarations
Competing interests.
A.M.M.E. is on the scientific advisory board and receives honoraria from Bristol–Myers Squibb and Merck Sharp & Dohme Limited. D.J.K. is Director of the Oxford University spin out company, Oxford Cancer Biomarkers. The other authors declare no competing interests.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
DeVita, V., Eggermont, A., Hellman, S. et al. Clinical cancer research: the past, present and the future. Nat Rev Clin Oncol 11 , 663–669 (2014). https://doi.org/10.1038/nrclinonc.2014.153
Download citation
Published : 23 September 2014
Issue Date : November 2014
DOI : https://doi.org/10.1038/nrclinonc.2014.153
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Fasting to enhance cancer treatment in models: the next steps.
- Yanlin Deng
- Bee Luan Khoo
Journal of Biomedical Science (2020)
Feasibility and first reports of the MATCH-R repeated biopsy trial at Gustave Roussy
- Gonzalo Recondo
- Linda Mahjoubi
- Luc Friboulet
npj Precision Oncology (2020)
Fasting and cancer: molecular mechanisms and clinical application
- Alessio Nencioni
- Irene Caffa
- Valter D. Longo
Nature Reviews Cancer (2018)
Unsolved challenges of clinical whole-exome sequencing: a systematic literature review of end-users’ views
- Gabrielle Bertier
- Martin Hétu
BMC Medical Genomics (2016)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

IMAGES
COMMENTS
About the Journal. Clinical Cancer Research publishes articles that focus on innovative clinical and translational research bridging the laboratory and the clinic. Topics include targeted therapies; mechanisms of drug sensitivity and resistance; pharmacogenetics and pharmacogenomics; personalized medicine; immunotherapy; gene therapy; diagnostic biomarkers; innovative imaging, and clinical ...
Targeted therapies have swiftly taken a prominent position in cancer research and clinical oncology in recent decades, thanks to the molecular insights into oncogenic processes and mechanisms ...
According to the International Agency for Research on Cancer (IARC), in 2020 there were approximately 19.3 million new cases of cancer, and 10 million deaths by this disease, 6 while 23.8 million cases and 13.0 million deaths are projected to occur by 2030. 73 In this regard, it is clear the increasing role that environmental factors ...
Find research articles on cancer treatment, including news stories, clinical trials, blog posts, and descriptions of active studies. ... NCI is developing the capability to produce cellular therapies, like CAR T cells, to be tested in cancer clinical trials at multiple hospital sites. Few laboratories and centers have the capability to make CAR ...
ASCO's Clinical Cancer Advances report highlights current trends in the field and identifies cancer research priorities that have great potential to advance progress against cancer. The report, now in its 16th edition, is developed by a 26-member editorial board of experts in a range of cancer types, subspecialties, and care issues.
F. Castinetti and F. Borson-ChazotN Engl J Med 2023;389:1916-1918. Although medullary thyroid cancer accounts for less than 5% of thyroid cancers, it deserves attention because of its phenotypic ...
The 100 most downloaded cancer research articles published in Scientific Reports in 2022. ... A cross-sectional study of clinical, dermoscopic, histopathological, and molecular patterns of scalp ...
The 100 most downloaded cancer research articles published in Scientific Reports in 2021. ... Real-world outcomes versus clinical trial results of immunotherapy in stage IV non-small cell lung ...
Clinical Cancer Research has also become an important forum for critical discussions in clinical oncology. Field-leading experts are invited to deliberate on the progress made in a given therapeutic area, focusing on the lessons to be learned from recent successes and failures. Authors from the FDA provide detailed insights into the data that ...
The cancer research community has a shared goal: to improve patient lives through basic, translational, and clinical research. ... and clinical cancer research, come together to further push the boundary, expanding this framework to emphasize the complexity of cancer that extends beyond tumor microenvironment. In doing so, they direct our ...
Cancer, an international interdisciplinary journal of the American Cancer Society, publishes high-impact, peer-reviewed original articles and solicited content on the latest clinical research findings.Spanning the breadth of oncology disciplines, Cancer delivers something for everyone involved in cancer research, risk reduction, treatment, and patient care.
Cancer is a global health problem responsible for one in six deaths worldwide. Treating cancer has been a highly complex process. Conventional treatment approaches, such as surgery, chemotherapy, and radiotherapy, have been in use, while significant advances are being made in recent times, including stem cell therapy, targeted therapy, ablation therapy, nanoparticles, natural antioxidants ...
Ke Chen, Jingcheng Zhang, Lei Meng, Lingshang Kong, Ming Lu, Zhengguang Wang and Wenbin Wang. Journal of Experimental & Clinical Cancer Research 2024 43 :78. Correction Published on: 12 March 2024. The original article was published in Journal of Experimental & Clinical Cancer Research 2024 43 :44. Full Text.
This site uses cookies. By continuing to use our website, you are agreeing to our privacy policy.
Cancer is a leading contributor to health and economic burdens [1, 2], highlighting an ongoing need for therapeutic advancement.However, the expansion of global clinical research has been ...
With the diagnosis of an estimated 19,292,789 cases and the incidence 9,958,133 deaths globally, cancer is considered the leading cause of death in 2020 [].Smoking, alcohol abuse and high body mass index (BMI) are the leading risk factors for risk-attributable cancer deaths and (disability-adjusted life-years) DALYs in 2019 [].The dissemination of cancer cells from the tissue of origin to a ...
Summary: Pablo Meyer and Ross Cagan discuss the main themes emerging from a recent workshop 'Rethinking Cancer', highlighting the key challenges faced by the research community and outlining potential strategies to promote translation of basic findings. In November 2016, a unique workshop titled 'Rethinking Cancer' was hosted by The ...
Journal of Experimental & Clinical Cancer Research is delighted to announce a new thematic series focused on: CRISPR-Cas9 system, the next generation in cancer therapy and target discovery. The Special Issue will accept Research Articles and Review in this topic. Submit here. Submission opens: 1 st April 2023; Submission deadline: 30 th June 2024
Cancer-vaccine trials give reasons for optimism. Therapeutic vaccines could provide a transformative shot in the arm for cancer treatment. Most people think of immunization as a way to prevent ...
Clinical Trials Showcased at Global Gathering. Fort Myers, Fla., April 5, 2024 - Clinical research conducted at Florida Cancer Specialists & Research Institute, LLC (FCS) will be highlighted at the American Association for Cancer Research 2024 Annual Meeting in San Diego as scientists, clinicians and other health care professionals and stakeholders from all over the world gather to share the ...
Newcastle University has secured almost £1.5m from Cancer Research UK to continue its prestigious Clinical Academic Training Programme over the next five years. This will provide five fully funded PhD clinical fellowships and five bursaries for undergraduates looking to intercalate and to do a Masters of Research (MRes) degree, aligned with ...
Approximately 2,900 gene therapy clinical trials are currently ongoing, 66.6% of which are related to cancer [ 158 ]. Different strategies are under evaluation for cancer gene therapy: 1) expression of pro-apoptotic [ 159, 160] and chemo-sensitising genes [ 4 ]; 2) expression of wild type tumour suppressor genes [ 5 ]; 3) expression of genes ...
Read the latest Research articles from Nature Cancer. ... Palmer and colleagues present a computational model of drug additivity that can predict clinical efficacy for the majority of combination ...
The full-time faculty of more than 3,100 is responsible for groundbreaking medical advances and is committed to translating science-driven research quickly to new clinical treatments. UT Southwestern physicians provide care in more than 80 specialties to more than 120,000 hospitalized patients, more than 360,000 emergency room cases, and ...
Abstract. In the past decade, we have witnessed unprecedented changes and some remarkable advances that have enabled true personalized medicine. Nevertheless, many challenges in clinical cancer ...