Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals

Neurosurgery articles from across Nature Portfolio
Neurosurgery is a surgical procedure that uses invasive techniques to diagnose, investigate and/or treat a neurological disorder, disease or injury. For example, to remove a brain tumour or insert a deep brain stimulation device.
Latest Research and Reviews

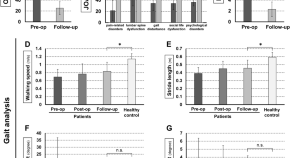
Short-term and mid-term evaluation of three types of minimally invasive lumbar fusion surgery for treatment of L4/L5 degenerative spondylolisthesis
- Zhaojun Song
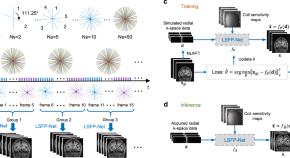
A deep unrolled neural network for real-time MRI-guided brain intervention
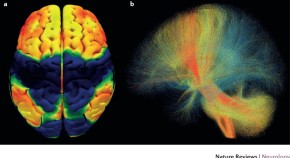
Real-time MRI provides accurate navigation and targeting for neurological interventions. Here, the authors propose a deep unrolled neural network for MRI reconstruction that enables real-time monitoring of remote-controlled brain interventions and can be integrated into diagnostic scanners.
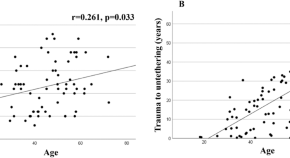
Spinal cord tethering and syringomyelia after trauma: impact of age and surgical outcome
- Denis Bratelj
- Susanne Stalder
- Michael Fiechter
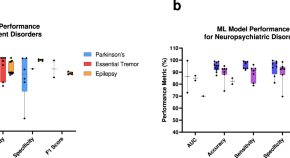
Landscape and future directions of machine learning applications in closed-loop brain stimulation
- Anirudha S. Chandrabhatla
- I. Jonathan Pomeraniec
- Alexander Ksendzovsky
Clinical impact of short limited lumbar fusion for adult spinal deformity with postural and radiological abnormalities
- Hideaki Nakajima
- Hideaki Matsuo
- Akihiko Matsumine

Probabilistic prediction of increased intracranial pressure in patients with severe traumatic brain injury
- Priyantha Wijayatunga
- Lars-Owe D. Koskinen
- Nina Sundström
News and Comment
Ultra-high-field mri improves detection of epileptic lesions.
- Heather Wood

Teamwork aids management and raises new issues in epilepsy
Publications on epilepsy in 2018 have shed light on the aetiology and management of the condition and raised new questions. Translation from mechanisms to clinical practice, driven by cooperation among multiple fields, will be crucial to further advances.
Circuits of Parkinson’s disease
- Anne-Marike Schiffer

Precision medicine drives epilepsy classification and therapy
2017 saw the publication of new classifications for epilepsy and seizure types, which emphasize the importance of understanding the underlying disease mechanisms. This aetiology-based approach is already beginning to inform developments in therapies and trial design in the epilepsies.
- Sameer M. Zuberi
- Andreas Brunklaus
Deep brain stimulation — making the right connections
- Charlotte Ridler
Long-term outcomes in MRI-negative patients with epilepsy
Patients with drug-resistant focal epilepsy who lack structural abnormalities on MRI constitute a challenge in presurgical work-up. A longitudinal single-centre study of long-term seizure outcomes in patients with nonlesional epilepsy showed that 59% of the cohort was free from disabling seizures 10 years after resective epilepsy surgery. These results are encouraging and valuable for patient counselling.
- Kristina Malmgren
- David Krýsl
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Neurosurgery
Explore the latest in neurosurgery, including recent advances in surgical management of epilepsy, CNS tumors, spinal disorders, and more.
Publication
Article type.
In this Medical News article, Edward Chang, MD, chair of the department of neurological surgery at the University of California, San Francisco Weill Institute for Neurosciences joins JAMA Editor in Chief Kirsten Bibbins-Domingo, PhD, MD, MAS, to discuss the potential for AI to revolutionize communication for those unable to speak due to aphasia.
This cohort study assesses the 6-month functional outcomes of patients with traumatic brain injury who undergo early (within 24 hours of injury) vs late extremity fixation.
This cross-sectional study uses UK Biobank and All of Us Research Program data to assess whether APOE ε4 is associated with higher risk of intracerebral hemorrhage among patients with known brain arteriovenous malformation.
This cohort study describes the clinical outcomes of salvage microsurgery following failed primary stereotactic radiosurgery or fractionated stereotactic radiotherapy among patients with sporadic vestibular schwannoma.
This prespecified analysis of the SELECT2 trial assesses endovascular thrombectomy treatment effects in transferred vs directly presenting patients and evaluates the association between transfer times and neuroimaging changes with endovascular thrombectomy clinical outcomes.
This clinical trial assesses the efficacy and adverse events of adjunctive intravenous low-dose methylprednisolone to endovascular thrombectomy for patients with acute ischemic stroke secondary to large-vessel occlusion.
- Adjunctive Steroids as Stroke Reperfusion Strategy JAMA Opinion February 8, 2024 Stroke Cerebrovascular Hemorrhage Cerebrovascular Infarction Cerebrovascular Disease Emergency Medicine Full Text | pdf link PDF
This exploratory analysis of the SELECT2 trial assesses the relationship between imaging estimates of irreversibly injured brain (core) and at-risk regions (mismatch) and the association of mismatch with clinical outcomes and endovascular treatment effect in adult patients with acute ischemic stroke due to occlusion of the internal carotid or middle cerebral artery and large ischemic core in 31 global centers between October 2019 and September 2022.
- Thrombectomy in Medium to Large Ischemic Core: Do Patients Still Need to Be SELECTed? JAMA Opinion February 7, 2024 Neurology Neuroimaging Radiology Cerebrovascular Disease Cerebrovascular Infarction Full Text | pdf link PDF
This individual participant data meta-analysis assesses treatment time from stroke symptom onset and disability level after treatment with intravenous thrombolysis plus thrombectomy vs thrombectomy alone among patients who presented directly at thrombectomy-capable stroke centers.
This cohort study compares the clinical and radiological outcomes of direct oral anticoagulant (DOAC)–associated intracerebral hemorrhage (ICH) treated with prothrombin complex concentrate vs conservative management among patients in Hong Kong.
- Is Nighttime Bracing Enough to Prevent Curve Progression of Adolescent Idiopathic Scoliosis? JAMA Network Open Opinion January 29, 2024 Orthopedics Physical Activity Surgery Spinal Cord Disorders Nutrition, Obesity, Exercise Full Text | pdf link PDF open access
The randomized clinical trial assesses whether self-mediated physical activity combined with either nighttime bracing or scoliosis-specific exercise is superior to self-mediated physical activity alone for preventing Cobb angle progression in moderate-grade adolescent idiopathic scoliosis.
This systematic review and meta-analysis describes the association between preoperative depression and postoperative patient-reported disability, pain, and physical function after spine surgery among adults enrolled in 44 studies.
This economic evaluation assesses the cost utility of introducing a standardized program of awake craniotomies.
This nonrandomized controlled trial of patients with advanced Parkinson disease examines the long-term effects of subthalamic nucleus deep brain stimulation, compared with standard-of-care medication, on quality of life.
This article discusses use of intraoperative MRI in convective gene therapy perfusion.
This randomized clinical trial evaluates whether thrombectomy for large vessel occlusion stroke with the pRESET stent retriever is noninferior to treatment with the Solitaire stent retriever.
This cohort study evaluates variations in center-level decisions to withdraw life-sustaining treatment for pediatric patients with severe traumatic brain injury.
- Deep Brain Stimulation Might Improve Cognition Years After TBI JAMA News December 13, 2023 Traumatic Brain Injury Neurology Psychiatry and Behavioral Health Surgery Psychiatric Surgery and Procedures Full Text | pdf link PDF
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Meetings Overview
- 2024 Annual Meeting
- Search Past Annual Meeting Abstracts
- Past Honored Guests
- Annual Meeting Archives
- Joint Section Meetings
- Request to Add a Meeting
- Code of Conduct
- Neurosurgery
- Operative Neurosurgery
- Clinical Neurosurgery
- Neurosurgery Practice
- Journal Subscription Request
- Publications Resident Fellowship
- Journal Club Podcasts
- Congress Quarterly
- Essential Papers in Neurosurgery
- Featured Education
- Online Education Subscription
- Browse Education Catalog
- Oral Board Exam Preparation Resources
- Primary Board Exam Preparation Resources
- SANS for Individual Learners
- SANS for Residency Program Coordinators
- Request for Seal of Approval
- Joint Accreditation Program
Explore Online Education
- Membership Overview
- Online Learning Subscription
- 2022 Annual Meeting Recordings
- New Members
- Submit Obituary
- Member Spotlight
- Active Duty Military
- International
- International Resident
- Medical Student
- Residency Program Coordinator Corner
- Applications in Progress
Apply for Membership
- Guidelines Overview
- Nominate a Guideline
- Archived Guidelines
- Nominate a Practice Parameter
- Practice Parameter Development Methodology
- About Practice Parameters
- Guideline Development Methodology
- Position Statement on Clinical Practice Guidelines
- Product Endorsement Policy
- Guidelines Podcasts
- CNS Guidelines Fellows
Access CNS Guidelines on the CNS+ App
- Advocacy Overview
- Statements and Releases
- Letters to the Editor
- Neurosurgery in the News
- Neurosurgery Blog
- Position Statements
- Legislative Affairs Archives
- Other Resources
- Washington E-Newsletter
- About the Washington Office
Visit the D.C. Press Room
- Leadership & Careers Overview
- Leadership Fellows & Faculty
- Leadership Committee Members
- Leadership Institute Podcast Series
- Career Center
- About Overview
- Mission and Vision
- Diversity, Equity, and Inclusion Committee
- Annual Reports
- Governance & Policies
- Executive Committee
- Other CNS Committees
- Joint Committees
- Past Presidents
- Family History
- Walter E. Dandy Letters
- Our Valued Partners
- Partnership Opportunities
- Careers at the CNS
- Annual Meeting Media Registration and Guidelines
- Sections and Affiliates
- Social Media
CNS Annual Meeting
- Cerebrovascular
- Neurotrauma & Critical Care
- Spine and Peripheral Nerves
- Stereotactic and Functional Neurosurgery
- Women In Neurosurgery
- Council of State Neurosurgical Societies
Neurosurgery is the official publication of the Congress of Neurological Surgeons. Neurosurgery provides multimedia, prompt publication of scientific articles on clinical or experimental surgery topics important for the brain, spine, and peripheral nerves, reviews, and other information of interest to readers across the world!
Follow Neurosurgery
Current Issue
Submit a Manuscript
Instructions for Authors
Neurosurgery supplements are available at neurosurgery-online.com .
Latest Articles
Neurosurgery - latest articles.
In Reply: Commentary: Letter: Visual Field Defects in the Setting of Suprasellar Lesions: Could Vascularization Patterns of the Optic Chiasm Play a Role?
Gender Differences in the Pediatric Neurosurgical Workforce: Professional Practice, Work-Life Balance, and Beyond
Impact of Procedure Time on First Pass Effect in Mechanical Thrombectomy for Anterior Circulation Acute Ischemic Stroke
Preoperative Opioid Use and Postoperative Outcomes in Patients Undergoing Microvascular Decompression for Trigeminal Neuralgia
MRI-Based Vertebral Bone Quality Score Can Predict the Imminent New Vertebral Fracture After Vertebral Augmentation
Receive access to world-class publications with a CNS membership!
CNS Members receive a 20% discount on Open Access Article Processing Charges in Neurosurgery Practice .

Neurosurgery Speaks!
Neurosurgery is proud to offer audio abstracts in 11 different languages, translated and read by native speakers. Each is the scientific abstract from a published article.
Explore Now
Contact the Editorial Office
Contact NEUROSURGERY Publications
The CNS Mission: Enhancing health and improving lives through the advancement of neurosurgical education and scientific exchange
Get involved.
Associated CNS Websites
- Neurosurgery Publications
- SANS Lifelong Learning
- Activity Center
Connect With Us
- Industry Support Options

Find answers
Find answers to frequently asked questions.
- Reset my password
- Pay my dues
- Get to my abstracts
- Go to the Annual Meeting
- Access the online journals
We use cookies to improve the performance of our site, to analyze the traffic to our site, and to personalize your experience of the site. You can control cookies through your browser settings. Please find more information on the cookies used on our site. Privacy Policy
Innovations and new technologies in pediatric neurosurgery
- Focus Session
- Published: 23 March 2021
- Volume 37 , pages 1471–1472, ( 2021 )
Cite this article
- Mostafa M. E. Atteya ORCID: orcid.org/0000-0001-5205-2660 1
243 Accesses
1 Altmetric
Explore all metrics
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Author information
Authors and affiliations.
Free-lance Consultant Pediatric Neurosurgeon, Alexandria, Egypt
Mostafa M. E. Atteya
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Mostafa M. E. Atteya .
Ethics declarations
Conflict of interest, additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Atteya, M.M.E. Innovations and new technologies in pediatric neurosurgery. Childs Nerv Syst 37 , 1471–1472 (2021). https://doi.org/10.1007/s00381-021-05144-5
Download citation
Received : 15 March 2021
Accepted : 17 March 2021
Published : 23 March 2021
Issue Date : May 2021
DOI : https://doi.org/10.1007/s00381-021-05144-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
Neurologic Surgery
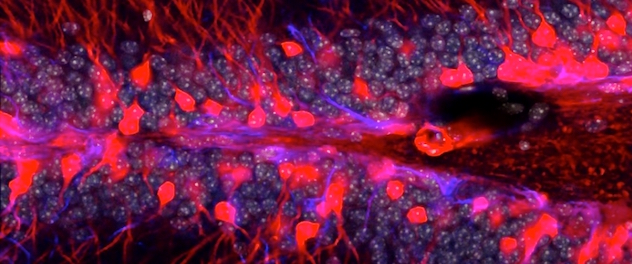
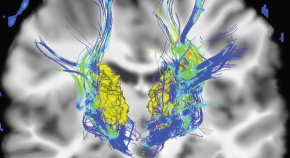
The hippocampus is one of the few brain regions where new neurons (red) are born throughout life. These not only are important for learning and memory but also are impacted by neurological diseases and many cancer therapies. Research in the department helps preserve neurogenesis and cognitive function in people with neurological diseases.
Neurosurgery investigators at Mayo Clinic are dedicated to advancing patient care through cutting-edge research spanning from discovery science and translation to clinical care. Inspired by our patients, Mayo Clinic researchers aim to improve patient care through a multifaceted and multidisciplinary approach, including:
- Basic science research. Several National Institutes of Health-funded laboratories within the department study and model human neurological diseases to discover tomorrow's therapies.
- Clinical studies. Neurosurgery clinicians and researchers at Mayo Clinic perform hundreds of clinical trials to translate new findings from bench to bedside. Find neurosurgery-related clinical trials .
- Informatics. Scientists' efforts to harness and advance informatics technology through new analytic tools and machine learning allows epidemiologic and individual patient data to yield increasingly individualized therapies.
- Neural engineering research. Researchers are developing new devices and technology for advanced management of neurological diseases.
- Outcomes research. Investigators' rigorous attention to how current therapies impact outcomes and quality of life continually refines and improves patient care.
Highly collaborative research efforts span Mayo Clinic's campuses in Phoenix/Scottsdale, Arizona; Jacksonville, Florida; Rochester, Minnesota; and dozens of collaborating institutions throughout the world. Collectively, this work enables the neurosurgery researchers at Mayo Clinic to pioneer technology aimed toward prevention and treatment of stroke, epilepsy, brain tumors, injuries of the brain and spinal cord, and neurodegenerative diseases.
Specific areas of neurosurgery research excellence at Mayo Clinic include:
- Awake brain surgery
- Brachial plexus and peripheral nerve disorders
- Cerebrovascular and skull base neurosurgery
- Informatics and data science
- Neural engineering
- Neuro-oncology
- Regenerative neuroscience
- Spine and spinal disorders
To learn more, explore laboratories and faculty in Mayo Clinic's Department of Neurologic Surgery.
Educational activities
Faculty members in the department train and mentor residents and fellows in Mayo Clinic School of Graduate Medical Education's neurosurgery training programs .
Department leadership
- Bernard R. Bendok, M.D. , is chair of the Department of Neurologic Surgery and a professor of neurosurgery at Mayo Clinic College of Medicine and Science at Mayo Clinic's campus in Arizona.
- Alfredo Quinones-Hinojosa, M.D. , is chair of the Department of Neurologic Surgery and a professor of neurosurgery in the College of Medicine and Science at Mayo Clinic's campus in Florida.
- Robert J. Spinner, M.D. , is chair of the Department of Neurologic Surgery and a professor of anatomy, neurosurgery and orthopedics at Mayo Clinic College of Medicine and Science at the Rochester, Minnesota, campus.
Contact Mayo Clinic with inquiries about investigations in the Department of Neurologic Surgery, patient appointments or supporting neurosurgery research.
- Contact the Department
- Patient Appointments
Neurosurgery research labs at Mayo Clinic's campuses in Arizona, Florida and Minnesota are investigating brain tumors, epilepsy, neurological diseases and neurological trauma.
- Laboratories - Research Laboratories
- Collaborators - Research Collaborators
Clinical Studies
Mayo Clinic is currently enrolling participants in clinical trials related to neurosurgery. Studies help to evaluate gene therapies and integrative medicine to supplement treatments, as well as develop patient registries, and more.
Keep up to date with the latest discoveries from researchers in Mayo Clinic's Department of Neurologic Surgery.
- Advancing the Science - News Advancing the Science
- Discovery's Edge - News Discovery's Edge
- Mayo Clinic News Network - News Mayo Clinic News Network
- Mayo Clinic Proceedings - News Mayo Clinic Proceedings
More about research at Mayo Clinic
- Research Faculty
- Laboratories
- Core Facilities
- Centers & Programs
- Departments & Divisions
- Clinical Trials
- Institutional Review Board
- Postdoctoral Fellowships
- Training Grant Programs
- Publications
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Sovrem Tekhnologii Med
- v.12(5); 2020

Artificial Intelligence in Neurosurgery: a Systematic Review Using Topic Modeling. Part I: Major Research Areas
G.v. danilov.
Scientific Board Secretary; N.N. Burdenko National Medical Research Center for Neurosurgery, Ministry of Health of the Russian Federation, 16, 4 th Tverskaya-Yamskaya St., Moscow, 125047, Russia;
M.A. Shifrin
Scientific Consultant, Laboratory of Biomedical Informatics and Artificial Intelligence; N.N. Burdenko National Medical Research Center for Neurosurgery, Ministry of Health of the Russian Federation, 16, 4 th Tverskaya-Yamskaya St., Moscow, 125047, Russia;
Physics Engineer, Laboratory of Biomedical Informatics and Artificial Intelligence; N.N. Burdenko National Medical Research Center for Neurosurgery, Ministry of Health of the Russian Federation, 16, 4 th Tverskaya-Yamskaya St., Moscow, 125047, Russia;
T.A. Ishankulov
Engineer, Laboratory of Biomedical Informatics and Artificial Intelligence; N.N. Burdenko National Medical Research Center for Neurosurgery, Ministry of Health of the Russian Federation, 16, 4 th Tverskaya-Yamskaya St., Moscow, 125047, Russia;
Yu.N. Orlov
Head of the Department of Computational Physics and Kinetic Equations; Keldysh Institute of Applied Mathematics, Russian Academy of Sciences, 4 Miusskaya Sq., Moscow, 125047

A.S. Kulikov
Staff Anesthesiologist; N.N. Burdenko National Medical Research Center for Neurosurgery, Ministry of Health of the Russian Federation, 16, 4 th Tverskaya-Yamskaya St., Moscow, 125047, Russia;
A.A. Potapov
Professor, Academician of the Russian Academy of Sciences, Scientific Supervisor N.N. Burdenko National Medical Research Center for Neurosurgery, Ministry of Health of the Russian Federation, 16, 4 th Tverskaya-Yamskaya St., Moscow, 125047, Russia;
Authors' contributions. G.V. Danilov, concept and draft writing, research protocol development, using R program for PubMed access, selection of publications, thematic modeling using the LDA algorithm; A.A. Potapov, reviewing and editing the draft in terms of neurosurgery; M.A. Shifrin, reviewing and editing the draft in terms of medical informatics; K.V. Kotik, thematic modeling using the ARTM algorithm; Yu.N. Orlov, reviewing and editing the draft in terms of artificial intelligence; T.A. Ishankulov, using Python program for PubMed access; A.S. Kulikov, reviewing and editing the draft in terms of neuroanesthesiology.
In recent years, the number of scientific publications on artificial intelligence (AI), primarily on machine learning, with respect to neurosurgery, has increased.
The aim of the study was to conduct a systematic literature review and identify the main areas of AI applications in neurosurgery.
Using the PubMed search engine, we found and analyzed 327 original articles published in 1996–2019. The key words specific to each topic were identified using topic modeling algorithms LDA and ARTM, which are part of the AI-based natural language processing.
Five main areas of neurosurgery, in which research into AI methods are underway, have been identified: neuro-oncology, functional neurosurgery, vascular neurosurgery, spinal neurosurgery, and surgery of traumatic brain injury. Specifics of these studies are characterized.
Conclusion.
The information presented in this review can be instrumental in planning new research projects in neurosurgery.
Introduction
The concept of “artificial intelligence” is currently widely used in various fields of science and medicine. In society’s minds, the understanding of artificial intelligence (AI) is formed by the mass media, science fiction, and scientific literature. Still, often this perception does not fully reflect the reality [ 1 ]. Technically, AI is a mathematical technology that automates the solution of an intellectual problem traditionally solved by a human [ 2 ]. At the same time, the term AI denotes the section of computer science within which such solutions are developed [ 3 ]. In the latter case, AI refers to a number of mathematical and software technologies that imitate human cognitive functions to a certain extent.
The most common examples of such technologies are “computer vision” (identification of objects in images), voice and speech recognition, analysis of natural language in texts, and machine translation. In all these examples, the computer (AI) exhibits the abilities inherent to humans: i.e., seeing, listening, reading, and understanding information. However, can this imitation of human intellectual capabilities be used in medicine? The potential of these technologies lies in the automation of medical procedures, primarily in diagnosing diseases, making clinical decisions, or predicting the treatment outcome. Like machine tools automated manual labor during the industrial revolution in the 18 th –19 th centuries, the computer “at the patient’s bedside” is expected to speed up clinical decisions, increase their reliability, and improve the quality and safety of medical care. The above humanistic considerations drive researchers to develop and apply AI technologies in medicine [ 4 – 7 ].
Methods of classical mathematical statistics, developed under conditions of data shortage, enable making scientifically based assumptions about global patterns based on a small number of observations. A large amount of data potentially hides more complex patterns — digital fingerprints of phenomena that cannot be detected without using special technologies. These technologies are being developed with the help of AI. Since the ability to process large amounts of information perceived by sensory organs is a natural function of the human brain, we intuitively call the computer programs capable of extracting and analyzing data from visual, acoustic, and tactile signals artificial intelligence.
How do AI technologies work? The mathematical apparatus of AI allows one to find and remember characteristic patterns of data that humans cannot always interpret. This process is called machine learning (ML), which is actually the mathematical search for the best solutions to systems of equations. The ML process results in a mathematical model, i.e., a function with independent variables (predictors) and parameters learned from the ML. For example, many models use the patient’s age and the severity of his/her disease as independent variables, while the output of the model is a prediction of the treatment outcome (in numeric or categorical terms). ML “learns” the parameters of such a model from a large amount of representative data.
The most promising advantages of AI technologies are their abilities to use the maximum available information (even in an unstructured form — images or text) and find complex and important patterns in it.
Neurosurgery is a field of clinical medicine that generates a large amount of data due to the routine use of high-tech medical equipment and medical information systems. These factors predispose the field of neurosurgery to the successful adaptation of AI technologies. To conceive an AI-based project in neurosurgery, it is important to understand the current demand and implementation of these technologies, as well as to identify research areas promising for using AI. This literature review aims to characterize the problems in neurosurgery that can be solved by AI technologies and to identify the areas in which these technologies are demanded.
The literature review was carried out with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyzes) guidelines and the additional use of topic modeling to objectify the selection of topics in the publications [ 8 , 9 ].
The articles from journals and international conference proceedings that met the following criteria were included in the analysis:
- the publication was an original research article;
- the publication described a disease and/or treatment methods directly related to neurosurgery;
- the paper described the use of AI technology for solving a clinical problem related to diagnosis, treatment, prognosis, rehabilitation, or prevention of a nervous system disorder;
- neurosurgery is a potential or current field of application of the AI technology studied.
Literature search strategy.
Search for the literature was performed in PubMed — the US National Library of Medicine search engine (https://www.ncbi.nlm.nih.gov/pubmed/). The search query was phrased so that all documents containing the terms “neurosurgery” or “neurosurgical procedures” and terms denoting individual AI technologies (including the analysis of large data arrays and machine learning) would appear in the search results. The exact query for the PubMed search was as follows: “neurosurgical procedures”[MeSH Terms] OR (“neurosurgical”[All Fields] AND “procedures”[All Fields]) OR “neurosurgical procedures”[All Fields] OR “Neurosurgery”[All Fields] OR “neurosurgery”[MeSH Terms]) AND (“artificial intelligence”[All Fields] OR “machine learning”[All Fields] OR “natural language processing”[All Fields] OR NLP[All Fields] OR “text mining”[All Fields] OR “fuzzy logic”[All Fields] OR “data mining”[All Fields] OR “big data”[All Fields] OR “topic model”[All Fields].
We reviewed the search results and selected original articles that met the above inclusion criteria. The selected articles were classified by specific areas of neurosurgery; preliminary topics of these studies were worded (using professional expertise), and their number was counted.
Topic modeling.
The expert-provided classification of publications by topics was then objectified using topic modeling technologies: the Latent Dirichlet Allocation (LDA) algorithm and the Additive Regularization of Topic Models (ARTM) algorithm [ 10 , 11 ]. Using these methods, specific sets of words characterizing each research topic (selected by experts) were identified in these article’s abstracts. By slightly varying the number of topics (a parameter of the topic model), we selected sets of words that best characterized specific topics. Finally, the results of the above two algorithms were compared, and the research topics were interpreted in accordance with the identified key words.
Software for data acquisition and analysis.
The primary selection and statistical analysis of the data were carried out using original software developed by the authors in the R (version 3.5.0) programming language for statistical analysis assisted with the integrated development environment RStudio. The PubMed query was performed through the programming interface (https://www.ncbi.nlm.nih.gov/books/NBK25501) from the R environment using the rentrez package (https://cran.r-project.org/web/packages/rentrez/vignettes/rentrez_tutorial.html).
We also applied the software packages XML, fulltext, tibble, dplyr, stringr, tidyr, tidytext, and topicmodels to retrieve the data on publications and analyze them in the R environment using the LDA algorithm. The ARTM model was developed using the Python programming language (version 3.6) in the Jupyter Notebook environment.
The process of selecting research articles for subsequent analysis of their topics is shown in Figure 1 . The query made on July 24, 2019 in PubMed databases, produced 731 results. In accordance with the criteria for inclusion in expert analysis and topic modeling, 327 articles published from 1996 to 2019 were selected.

General characteristics of the publications analyzed.
Figure 2 shows the number of selected papers arranged by the year of publication. In 2018 and the first half of 2019, there was a significant increase in the number of papers on the use of AI technologies in neurosurgery.

Most of the analyzed studies were conducted within 5 major areas of neurosurgery and one combined area:
- neuro-oncology (n=133; 41%);
- functional neurosurgery (n=62; 19%);
- vascular neurosurgery (n=44; 14%);
- spinal neurosurgery (n=29; 8%);
- surgery for trauma brain injury (n=26; 8%);
- other and related areas of neurosurgery (n=33; 10%).
For publications from the first 5 sections, a topic modeling analysis was carried out. The number of topics was initially selected using LDA (so that the topics differ as much as possible when interpreting the key words). Then the ARTM algorithm was applied with the same number of topics. The topics resulted from the LDA and ARTM were compared with each other. In the cases where the ARTM algorithm created two or more similar (and not separable) topics, they were assigned to the same topic under the LDA. The results of topic modeling with the LDA and ARTM algorithms (main specific key words and interpretation of topics) are presented in the Table . The complete list of 327 analyzed publications is presented in the Appendix.
Key topics and related key words from publications in neuro-oncology, functional, vascular and spinal neurosurgery, and surgery for traumatic brain injury identified using the LDA and ARTM topic modeling algorithms
As shown in Table , the two algorithms largely lead to similar discrimination between the topics by key words. The application of AI technologies for each major area of neurosurgery will be described in more detail in the second part of this work.
Despite the recent development of AI technologies, machine learning, and related big data analysis methods, these technologies are yet to earn large-scale and systematic applications in neurosurgery. An objective limitation for the rapid progress in this area is, of course, the insufficient volume of high-quality data (so traditional for medicine).
Due to the increased interest in this research, the base of evidence on the performance, safety, and economic feasibility of AI methods in neurosurgery is being created. Thus, in a systematic review by Senders et al. [ 12 ], the authors described 23 studies that assessed the utility of AI technologies for solving diagnostic and prognostic tasks compared to the accuracy of medical judgments in neurosurgery. In 14 of these studies, diagnostic (classification) problems were approached using primarily neuroimaging data and electroencephalography. Seven studies addressed the methods of preoperative planning based on image analysis. In 3 studies, predicting the outcomes of neurosurgical treatment was attempted. The quoted review shows that ML can help in solving clinical problems. In 29 out of 50 (58%) tests conducted in a total of 23 studies, the results of ML were significantly better than the accuracy of conclusions made by clinical experts (p<0.05); in 18 out of 50 (36%) cases, no significant difference was found between the ML and the experts’ results; in 3 out of 50 (6%) clinical experts solved problems better than ML (p<0.05). In 4 studies assessing the performance of ML as an addition to the expert’s work, this combination was more effective than the performance of the ML or the clinician alone. This result rather confirms the hypothesis about the potential use of AI in neurosurgery.
At present, there is no enough evidence to decide on the utility, safety, and economic feasibility of AI techniques in neurosurgery; therefore, one cannot assume that AI technology is now able to replace the traditional, routine methods of medicine totally. However, given the powerful potential of AI, one can definitely suggest the need for the development and widespread testing of these methods in medical science and practice.
In the present review, methods of topic modeling are used to identify the key topics in publications. As an example of AI technologies, these methods are used to analyze texts written in a natural language. Using topic modeling, from 4 to 9 major topics (research areas) were identified for each section of neurosurgery. This approach is required for the subsequent automatic tracking of trends in a given research area and can exemplify the use of AI in biomedical science.
Below we discuss the limitations of the present work, which are important for interpreting its results. The systematic review is aimed at studying the topics and trends in using the AI solely in neurosurgery. At the same time, in related fields (for example, neuroimaging), the range of tasks solvable by AI can be much wider.
Here, we do not analyze systematic reviews on the use of AI in neurosurgery published by others since most of these papers were focused on a specific design of original studies or a specific disease and therefore had narrow inclusion criteria.
To date, research into the use of AI technologies in neurosurgery has been carried out in five major areas: neuro-oncology, functional, vascular, and spinal neurosurgery, and traumatic brain injury. Using topic modeling, we identified major research topics in each of these areas. In the second part of this review, we will discuss the tasks in neurosurgery approached by AI technologies.
Funding Statement
Financial support. This work was supported by the Russian Foundation for Basic Research (grant 19-2901174).
- See us on facebook
- See us on twitter
- See us on youtube
- See us on linkedin
- See us on instagram
Medical students unseal their futures on Match Day
Nerves turn to celebration as Stanford School of Medicine students discover where they are headed for the final phase of their medical training.
March 19, 2024 - By Nina Bai

Jamasb Sayadi (wearing necktie), matched in neurosurgery at Stanford Medicine. Steve Fisch
As the countdown clock ticked down, the Stanford School of Medicine class of 2024 milled about the Li Ka Shing Center with nervous energy — quite literally not knowing where they were going. Soon they would learn where they had matched for their residencies and which cities they would move to for the most advanced phase of their medical training.
Around the country, graduating medical students engaged in the same Match Day ritual . After dozens of applications and months of interviews, students and residency programs submit their preferences to the National Resident Matching Program, which uses an algorithm to make the optimal matches. The results are unveiled on Match Day.
[Read Match Day 101: How does the medical residency match work? ]
“It’s such a privilege to recognize this incredibly distinguished class,” said Lloyd Minor , MD, dean of the School of Medicine and vice president for medical affairs at Stanford University, offering a moment of reflection amid the excitement. “You bring such vibrancy, such intellectual rigor and passion to the work that you do, and that’s what makes it so meaningful for us as faculty and what makes our research and our patient care mission more meaningful as well.”
Not just MDs
In this year’s graduating class of 73 students, only 17 enrolled four years ago, in the early, uncertain months of the pandemic; 28 have been here for five years; and another 28 have called Stanford home for six years or more. Many will be collecting multiple degrees, including 15 MD-PhD students in the Medical Scientist Training Program. Altogether they matched in 20 specialties, ranging from orthopaedic surgery to psychiatry to radiation oncology.

Grace Li (in blue shirt) is headed to Boston for a residency in emergency medicine at Mass General Brigham. Steve Fisch
Minutes before 9 a.m. Pacific time, each student was handed a sealed red envelope with their destination inside. Their family, friends and mentors gathered around. Everyone counted down the final seconds. After a brief pause of rustling paper, shouts of elation and relief filled the room.
“This is just a surreal feeling,” said Jamasb Sayadi, who matched in neurosurgery at Stanford Medicine. He was surrounded by close friends and family, including his brother and father, and his uncle on video call.
The moment represented years of dedication and sacrifice, especially for his parents, he said, who immigrated from Iran in the aftermath of the 1979 revolution. He was inspired to go into neurosurgery after seeing his father’s transformation from deep brain stimulation for Parkinson’s disease, and after his mother’s death from glioblastoma in August.
Sayadi was grateful that he could continue working with his mentors at Stanford and stay close to his father and brother, who live in California. “It’s going to be the best possible outcome,” he said.
Grace Li, holding a large bouquet of flowers, learned she had matched in emergency medicine at Mass General Brigham, her first choice. Li said she was drawn to emergency medicine because it’s an opportunity to see patients from every walk of life and help them through enormously stressful moments.
Her entire family flew in from Texas, New York City and Boston to celebrate the first physician in the family. “I feel very, very lucky. Just being here on Match Day, surrounded by loved ones, is a dream come true,” she said. She thought about the journey ahead. “I’m going to need a winter coat.”

Sofia Essayan-Perez and Francisco Galdos matched as a couple at Stanford Medicine, Essaya-Perez as a pediatric neurologist and Galdos as a pediatric physician-scientist. Steve Fisch
Sofia Essayan-Perez and Francisco Galdos met nearly 10 years ago during medical school interviews. “The funny things is, the first person I saw when I moved in was Sofia,” Galdos said.
Neighbors and lab partners
They had both been accepted into the Medical Scientist Training Program and, by chance, were moving into adjacent apartment buildings. Then they were taking the same classes and working side by side dissecting the same cadaver in anatomy lab. Soon they were a couple — it didn’t hurt that Galdos always had a good sense of humor, even in anatomy lab, Essayan-Perez said — and have shared every milestone in their nine years at Stanford Medicine.
At Match Day, they made sure to open their envelopes and unfold their letters at exactly the same time. They were thrilled to be matched at Stanford Medicine, Essayan-Perez in pediatric neurology and Galdos in the pediatric physician-scientist program — which means they’ll be at Stanford for at least another five years.
“We’re really excited,” Essayan-Perez said. “We’ve had really amazing support from both of our fields as medical students, and it was the network of mentors that convinced us to stay.”
Galdos plans to continue his research on single ventricle heart defects, a condition in which children are born with part of the heart severely underdeveloped. His younger brother, Luis, died from the condition at age 8, when Galdos was 11. “He’s always been with me on this journey,” Galdos said. “He’s been my inspiration for my whole life.”
With a clear view of the road ahead, the students also took stock of how far they’ve come. “At the beginning of medical school, I remember thinking, ‘Will I still be this excited at the end?’” Galdos said. “Now I can say this path has just reaffirmed that excitement.”
About Stanford Medicine
Stanford Medicine is an integrated academic health system comprising the Stanford School of Medicine and adult and pediatric health care delivery systems. Together, they harness the full potential of biomedicine through collaborative research, education and clinical care for patients. For more information, please visit med.stanford.edu .
Artificial intelligence
Exploring ways AI is applied to health care

Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

Aspirin cuts liver fat in trial

First-ever transplant of pig kidney to patient a success
Parkinson’s warning in skin biopsy

John Moore/Getty Images
Treat addiction with psychedelics?
Despite promise of success stories from patients in recovery, Law School panel cautions that research is lacking on benefits vs. risks
Harvard Staff Writer
Mark Guckel had struggled with crack addiction since high school. Despite numerous attempts to overcome his substance use disorder, nothing helped. That is, until he tried psychedelic plants, such as ayahuasca , psilocybin , and ibogaine . The experience changed his life. Now a professional recovery coach, Guckel said psychedelics might hold a promise to treat addiction disorders.
Guckel shared his story of addiction and recovery during an online panel sponsored by the Petrie-Flom Center at Harvard Law School on Tuesday afternoon, “New Ideas for Substance Use Condition Treatment: Could Psychedelics Help?” But he warned that psychedelics is just one of many other treatments for substance-use disorders. Psilocybin and ibogaine are federally illegal in the U.S., with some exceptions for medical research.
“I can say that while psychedelics helped me to stop using substances, I’d like to reflect that these aren’t a cure,” said Guckel, a founder of a company that offers psychedelic-assisted recovery. “They are catalysts. They’re sacraments, they’re medicines, they’re tools. They’re one of many pathways. There are many other treatment modalities that are out there, from regular treatment to medication-assisted recovery to other holistic modalities that can help us live better lives.”
17% Of Americans over the past year have struggled with substance use disorder yet only 10% have accessed treatment
Accounts like Guckel’s and the idea that psychedelics might prompt a neurochemical reset in the brain have many looking to the approach as a promising treatment for addiction disorders. Around 17 percent of Americans have met criteria for a substance use disorder in the past year, said Stephanie Tabashneck , the event’s moderator. Yet fewer than 10 percent get treatment, she said.
“We have a treatment shortage. We also know that a lot of the treatments that we have are not particularly effective,” said Tabashneck, senior fellow of law and applied neuroscience, a collaboration between the Center for Law, Brain & Behavior and the Petrie-Flom Center.
After reminding the audience that none of the information shared in the panel should be considered legal or medical advice, Tabashneck offered a word of caution about psychedelics.
“Psychedelic therapy is not a replacement for medication treatments, like methadone for opioid-use disorder. All of our panelists will also agree that these are not first-line treatments. If someone has a substance-use disorder and it’s early, no one is recommending or suggesting that you should go ahead and try the psychedelics first as a method of treatment.”
Conventional treatments for addiction include behavioral therapies, such as contingency management and medication compliance therapy. There are also medication-assisted recovery treatments for opioid, alcohol, cocaine, and cannabis-use disorders. But the enthusiasm for psilocybin and ibogaine for treating substance-use conditions has been gradually increasing.
Panelist Mark Guckel describes how psychedelics helped him overcome an addiction to crack.
Jon Chase/Harvard Staff Photographer
Panelist Mason Marks , visiting professor of law, Harvard Law School, and senior fellow and lead of the Project on Psychedelics Law and Regulation at Petrie-Flom, highlighted the legal and medical concerns about psilocybin, also known as magic mushrooms, and ibogaine, a psychoactive substance found in iboga, a shrub that’s native to Central West Africa.
“Unlike psilocybin, there’s no clinical ibogaine research in the U.S. right now, and that’s likely due in part to the risk of cardiovascular adverse events,” said Marks. “Ibogaine has been linked to heart attacks and some deaths.”
Marks said there are efforts in some cities and states across the U.S. to decriminalize psilocybin. Last year, Oregon opened a state-regulated program for supervised administration of psilocybin, and next year, Colorado will open a similar program for psilocybin and possibly ibogaine to be used as a treatment for addiction under medical supervision, he said. But it won’t be without concerns.
“In light of the federal illegality of psilocybin and ibogaine, there are many unresolved legal questions, some challenging legal questions and questions of potential liability, as well for licensed healthcare professionals who choose to get involved in these programs,” Marks said.
Neuroscientist Deborah Mash , professor of neurology and molecular and cellular pharmacology, Leonard M. Miller School of Medicine, has been studying the effects of ibogaine in substance-use disorders for more than three decades. She warned that it is not for everyone.
“I saw patients exhibit a remarkable recovery for a longstanding heroin abuse, cocaine-dependency disorder, including a young man who was on methadone maintenance who remarkably had no withdrawals, no cravings, and put their desire to go out and get and use drugs in remission,” said Mash, also the director of the Brain Endowment Bank at the University of Miami and chief executive officer and founder of DemeRx. “It’s a very powerful addiction interrupter.”
And yet, for people who may have an underlying psychiatric comorbidity like schizophrenia or a bipolar disorder diagnosis, psychedelics might pose a serious health risk, said Mash. She also warned against self-medication with psychedelics obtained through online distributors. “We want these molecules to be used in a medical way by qualified clinicians and therapists who understand these types of therapies and how they can work best.”
Despite all the craze around psychedelics, little research has been done to prove their efficacy treating addiction disorders. Mash pleaded for more evidence-based research that could lead to regulatory approval and make such treatments safely available to those who are “suffering the most.” So far, what researchers have is anecdotal. “And we know that data are not the plural of anecdote,” she said.
Share this article
You might like.
10 percent reduction seen in small study of disease that affects up to a third of U.S. adults

Genetic editing improves compatibility, marks advance in organ shortage crisis
Medical office procedure identifies key biomarker that may lead to more reliable diagnosis of neurodegenerative disorders
Maria Ressa named 2024 Commencement speaker
Nobel Prize-winning defender of press freedom will deliver principal address
The 20-minute workout
Pressed for time? You still have plenty of options.
So what exactly makes Taylor Swift so great?
Experts weigh in on pop superstar's cultural and financial impact as her tours and albums continue to break records.
Related News

Scholarly Project Profile: Jahnavi Shriram

Scholarly Project Profile: Chung Yon John Lin, PhD

Scholarly Project Profile: Ashley Guest
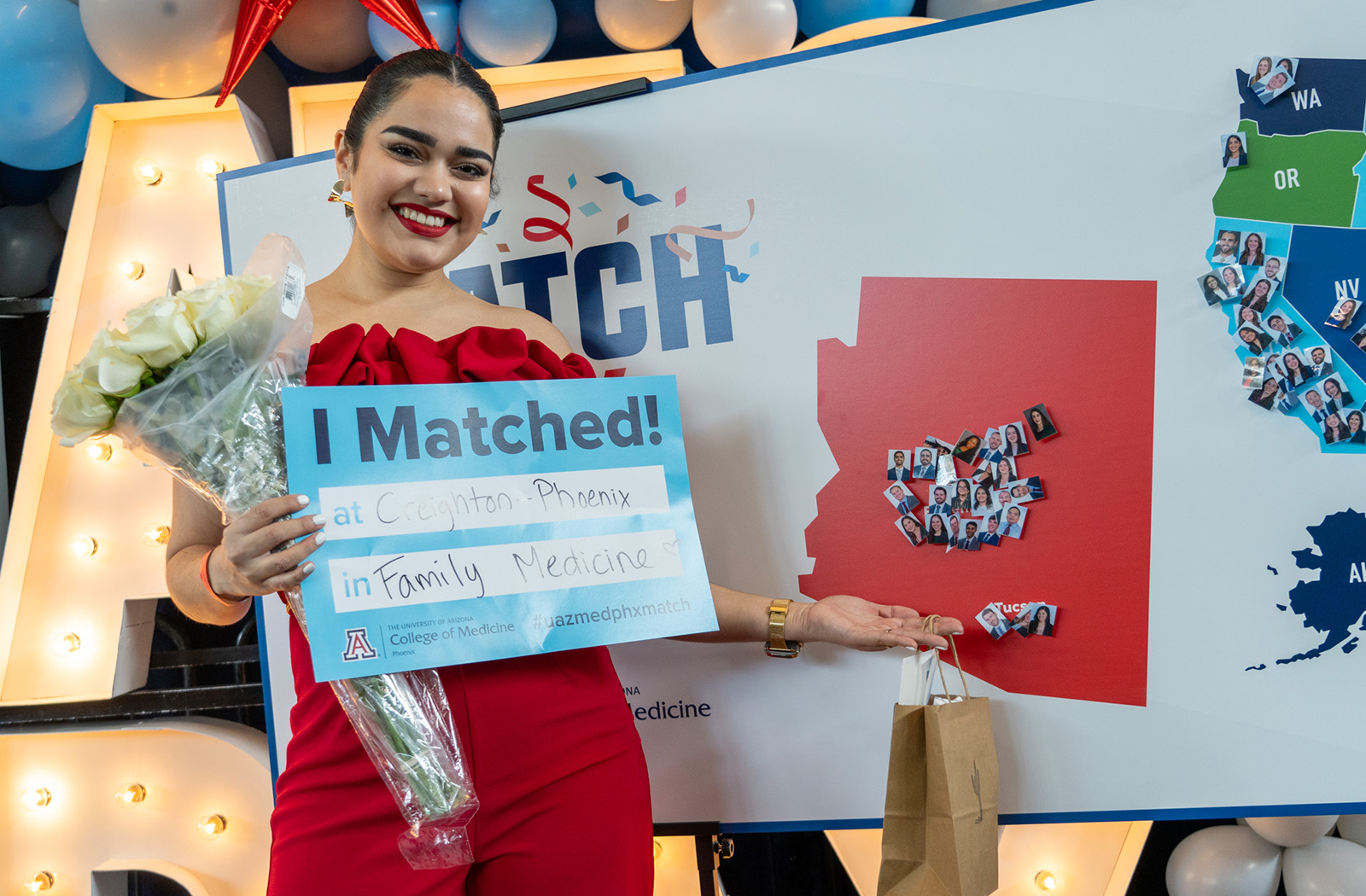
From Uncertainty to Elation, the Class of 2024 Matches
Thomas Kelly
When the Class of 2024 entered medical school at the University of Arizona College of Medicine – Phoenix, they did so with an unclear vision of how their four years would unfold.

The COVID-19 pandemic upended the first year of their studies, forcing most of their learning to be conducted virtually and even postponing their White Coat Ceremony more than a year. Ultimately, though, they endured and prospered.
That perseverance paid off Friday, March 15, at their Match Day . Surrounded by family and friends at the Arizona Science Center, the Class of 2024 soaked in the joyous moment, eagerly ripping open custom award-style envelopes to reveal where the next step in their medical journey would take them.
Stephanie Briney, DO , associate dean of Student Affairs, spoke to their resilience and power of spirit. “This class walked in virtually and didn’t let change or uncertainty hold them back from their aspirations and commitment to medicine,” she said. “The Class of 2024 are fighters, in the best possible way, and they will make excellent future physicians in their chosen specialties.”
And they matched into exceptional programs — such as UArizona College of Medicine – Phoenix, UCLA Medical Center, Barrow Neurological Institute, Walter Reed Medical Center, Yale and USC. They excelled in securing positions in competitive specialties — including dermatology, psychiatry, diagnostic radiology, orthopedic surgery, anesthesiology and more.
As they prepared to announce where they would be headed for residency, an overwhelming sense of happiness swept the room. It was soon to be accompanied by raucous cheers and applause as they shared their matches with the crowd.

Their jubilation was well earned, and in his remarks, Dean Fred Wondisford, MD, MS, MBA , took time to remind them to soak it all in. “There are moments in life that you never forget — when you meet the love of your life, when, or if, you have children,” he said. “I guarantee you: This Match Day will become one of those moments. So, take a breath. Savor the moment.”
The more than 90 medical students from the college were among 50,413 applicants from around the country who registered in the 2024 Main Residency Match. That number was a record high — 2,257 more than last year, a 4.7% increase. U.S. allopathic seniors, osteopathic students, Canadian students, U.S. citizens who studied abroad to obtain their education, as well as non-U.S. citizens vying for residency slots in the U.S. comprised the impressive total.
As the pool of applicants has grown, so have the residency openings they vie for. The additional residency positions afforded applicants access to 125 more programs and 1,128 positions, 2.8% more than the 2023 Main Residency Match.

The UArizona College of Medicine – Phoenix is a central part of that Graduate Medical Education growth , expanding three of its existing programs in 2024. By 2027, 16 new programs will be launched in specialties including anesthesiology, dermatology, neurosurgery, ophthalmology and otolaryngology, among others.
This ensures more of the college’s students will stay in-state to serve Arizonans, and it will also attract more outstanding physicians from around the country to help provide health care to the state’s growing population.
The culmination of a complex, year-long process, the Match is about finding the right fit. Future physicians seek the specialty, residency program and mentors who will help them complete their professional training. Residency programs search for talented physicians who will advance the specialty and improve patient outcomes.
Match results are released nationally by the National Resident Matching Program ™ and announced at Match Day ceremonies coordinated to occur each year on the same date (the third Friday in March) at the same time.
Photos and Video
- Class of 2024 Match Day Recap .
- Photos from the event .
Class of 2024 Fast Facts
- Thirty-six students will complete at least one year of training in Arizona.
- Thirty-three students will complete all years of their residency training in Arizona.
- Twenty matched at UArizona College of Medicine – Phoenix.
- Three matched at UArizona College of Medicine – Tucson.
- Eight matched at Creighton University-affiliated hospitals.
- Four matched at Mayo Clinic School of Graduate Medical Education.
- One matched at another training site in the state.
- The other students will be spread out across the U.S., spanning 23 states in total.
- Almost 32% of the graduates are entering primary care specialties — areas of immense need — including family medicine, internal medicine, pediatrics and Med-Peds.
Class of 2024 Match Day Profiles

About the College
Founded in 2007, the University of Arizona College of Medicine – Phoenix inspires and trains exemplary physicians, scientists and leaders to optimize health and health care in Arizona and beyond. By cultivating collaborative research locally and globally, the college accelerates discovery in a number of critical areas — including cancer, stroke, traumatic brain injury and cardiovascular disease. Championed as a student-centric campus, the college has graduated more than 800 physicians, all of whom received exceptional training from nine clinical partners and more than 2,700 diverse faculty members. As the anchor to the Phoenix Bioscience Core , which is projected to have an economic impact of $3.1 billion by 2025, the college prides itself on engaging with the community, fostering education, inclusion, access and advocacy.
Read our research on: TikTok | Podcasts | Election 2024
Regions & Countries
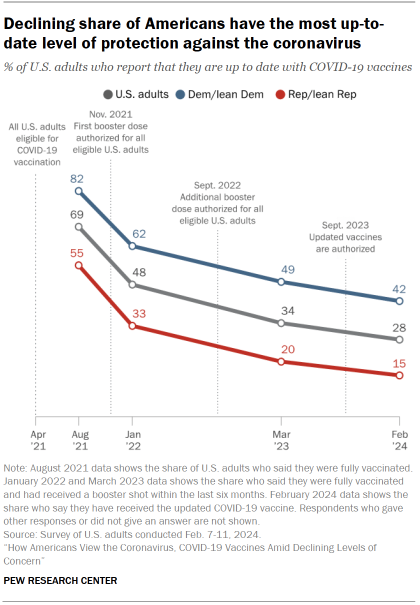
How americans view the coronavirus, covid-19 vaccines amid declining levels of concern, continued decline in share of u.s. adults with up-to-date vaccination.

Pew Research Center conducted this study to understand Americans’ views of the coronavirus and COVID-19 vaccines. For this analysis, we surveyed 10,133 U.S. adults from Feb. 7 to 11, 2024.
Everyone who took part in the survey is a member of the Center’s American Trends Panel (ATP), an online survey panel that is recruited through national, random sampling of residential addresses. This way, nearly all U.S. adults have a chance of selection. The survey is weighted to be representative of the U.S. adult population by gender, race, ethnicity, partisan affiliation, education and other categories. Read more about the ATP’s methodology .
Here are the questions used for this report , along with responses, and its methodology .
A new Pew Research Center survey finds that just 20% of Americans view the coronavirus as a major threat to the health of the U.S. population today and only 10% are very concerned they will get it and require hospitalization. This data represents a low ebb of public concern about the virus that reached its height in the summer and fall of 2020, when as many as two-thirds of Americans viewed COVID-19 as a major threat to public health.
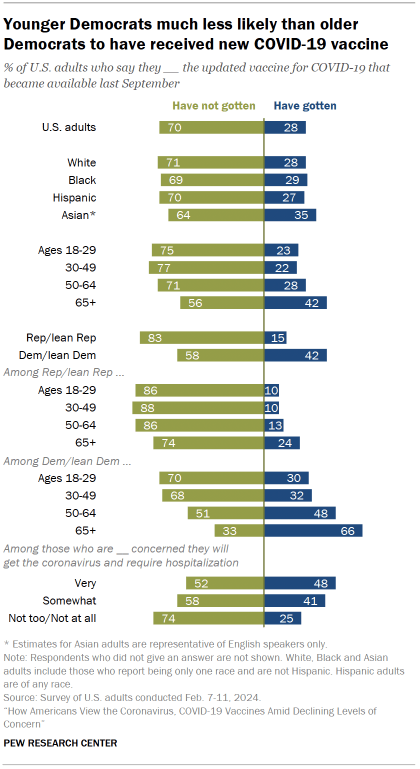
Just 28% of U.S. adults say they have received the updated COVID-19 vaccine, which the Centers for Disease Control and Prevention (CDC) recommended last fall to protect against serious illness. This stands in stark contrast to the spring and summer of 2021, when long lines and limited availability characterized the initial rollout of the first COVID-19 vaccines. A majority of U.S. adults (69%) had been fully vaccinated by August 2021.
Underscoring the limited demand for the updated COVID-19 vaccines, a larger share of U.S. adults say they’ve gotten a flu shot in the last six months than the updated coronavirus vaccine (44% vs. 28%). And despite a public health push encouraging adults to get both vaccines at the same time, almost half of those who received a flu shot from a health care provider chose not to get the updated COVID-19 vaccine.
The vast majority of Americans have some level of protection from the coronavirus because of vaccination, prior infection or a combination of the two. This has led to a decline in severe illness from the disease.
Still, the virus continues to circulate widely in the United States , with wastewater data suggesting that cases in the early part of 2024 were among the highest they have been since the first omicron wave in 2022.
Long COVID ranks among the concerns of public health experts. Long COVID refers to a variety of symptoms such as fatigue and brain fog that last longer than a month after a COVID-19 infection.
The survey – conducted among 10,133 U.S. adults from Feb. 7 to 11, 2024 – finds that 50% of Americans say it is extremely or very important for medical researchers and health care providers to understand and treat long COVID; 27% see this as a less important issue and 22% of Americans say they haven’t heard of long COVID.
Continuity and change: Partisan views of COVID-19
Partisanship remains one of the most powerful factors shaping views about COVID-19 vaccines and the virus. But the size and nature of differences between Republicans and Democrats have evolved since earlier stages of the outbreak.
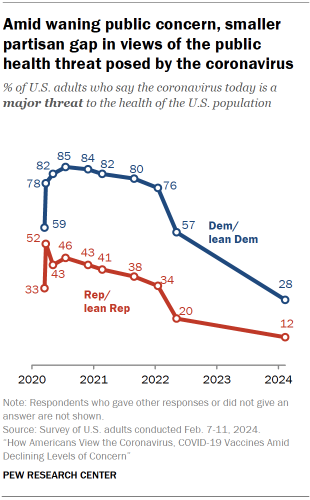
For instance, the gap between the shares of Democrats and Republicans who view the coronavirus as a major threat to public health has fallen from 37 percentage points in May 2022 to 16 points today. In the pandemic’s first year, Democrats were routinely about 40 points more likely than Republicans to view the coronavirus as a major threat to the health of the U.S. population. This gap has waned as overall levels of concern have fallen.
When it comes to vaccination, Democrats and Democratic-leaning independents remain more likely than Republicans and GOP leaners to say they’ve received an updated COVID-19 vaccine (42% vs. 15%). This 27-point gap in recent vaccination is about the same as in January 2022 when 62% of Democrats and 33% of Republicans said they were up to date (i.e., fully vaccinated and recently boosted).
In addition to partisanship, age continues to matter a great deal in attitudes and behaviors tied to the coronavirus. And the intersection of partisanship and age reveals one of the biggest recent changes in the public’s response to the outbreak: a growing divergence between the oldest Republicans and oldest Democrats in vaccine uptake, which is explored below.
COVID-19 vaccination among adults ages 65 and older, by party
Older adults continue to be one of the most at-risk groups for severe illness and death from COVID-19.
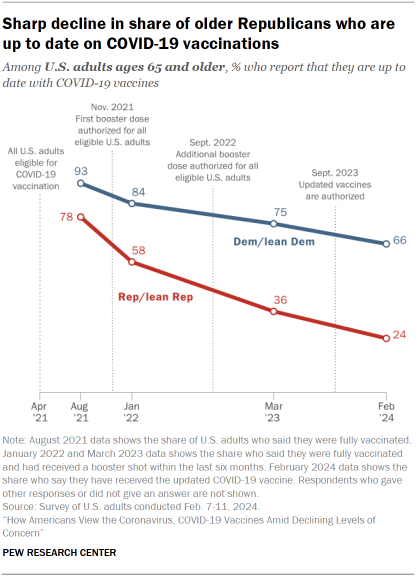
When vaccines first became available in 2021, large majorities of both Republicans and Democrats ages 65 and older said they had received the vaccine. But as additional doses have become available, uptake among older Republicans has declined at a faster rate than among older Democrats.
In the current survey, 66% of Democrats ages 65 and older say they have received the updated COVID-19 vaccine, compared with 24% of Republicans ages 65 and older.
This 42-point partisan gap is much wider now than at other points since the start of the outbreak. For instance, in August 2021, 93% of older Democrats and 78% of older Republicans said they had received all the shots needed to be fully vaccinated (a 15-point gap). Go to the Appendix for more details .
How COVID-19 vaccination varies by age within parties
The impact of age is also striking when looking within political parties.
Among Democrats, about three-in-ten adults under 50 have received an updated COVID-19 vaccine, compared with 48% of those ages 50 to 64 and 66% of Democrats ages 65 and older.
Age differences within the GOP run in the same direction, but are much more modest, reflecting, in part, low overall levels of vaccine uptake.
How COVID-19 vaccination varies by race and ethnicity
Similar shares of White (28%), Black (29%) and Hispanic (27%) adults say they have gotten the updated vaccine. English-speaking Asian adults (35%) are slightly more likely to report receiving the updated vaccine.
As in past Center surveys, there are racial and ethnic differences in vaccine uptake among Democrats.
For instance, 50% of White Democrats and 42% of English-speaking Asian Democrats report having received the updated vaccine, compared with somewhat smaller shares of Black and Hispanic Democrats (32% each).
Views of long COVID
Half of Americans say it is extremely or very important for medical researchers and health care providers to understand and treat long COVID, considering all the different priorities they face.
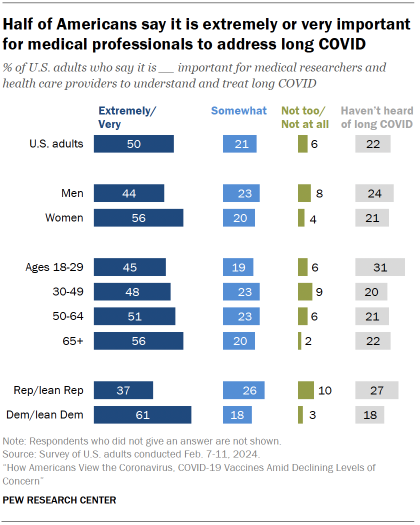
About two-in-ten (21%) say it’s somewhat important for those in medicine to address long COVID, while 6% say it is not too or not at all important. Another 22% say they haven’t heard of long COVID.
More Democrats (61%) than Republicans (37%) say it is extremely or very important for medical researchers and health care providers to understand and treat long COVID.
A majority of women (56%) consider this extremely or very important; a smaller share of men (44%) say the same. The CDC has reported that women are more likely than men to develop long COVID symptoms.
Awareness of long COVID also shapes views on its importance: Those who have heard a lot about long COVID are more likely than those who have heard a little about it to say it’s extremely or very important for medical professional to address it (76% vs. 60%).
Views of the threat posed by the coronavirus
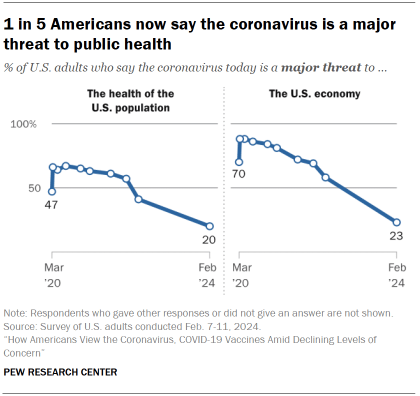
One-in-five Americans now say the coronavirus is a major threat to the health of the U.S. population, down from a high of 67% in July 2020.
Concern about the coronavirus as a major threat to the U.S. economy has also declined dramatically. Today, 23% of Americans say it’s a major threat to the economy, compared with 88% in May 2020. The pandemic spurred an economic recession in 2020 and a spike in unemployment that reached the highest levels since the Great Recession.
Federal policy on the coronavirus has changed as public concern – and the incidence of severe illness – has fallen. The Biden administration ended the public health emergency for the coronavirus pandemic in May 2023. And the CDC recently released updated guidelines with shorter isolation periods for adults testing positive for the disease.
While large partisan gaps characterized views of the coronavirus as a major threat to public health for much of the pandemic, those gaps were far smaller on views of the virus as a major threat to the economy. In the current survey, just a 6-point gap separates Republicans and Democrats with this view (20% vs. 26%, respectively) – similar to the 9-point party gap seen in May 2022.
Personal concern about getting or spreading COVID-19
About a quarter of Americans (27%) are very or somewhat concerned about getting a serious case of COVID-19 that would require hospitalization. A somewhat higher share (40%) say they are very or somewhat concerned they might spread the coronavirus to other people without knowing it.

Levels of concern for getting or spreading the coronavirus are about the same as they were in March 2023 and remain down dramatically from early in the pandemic.
The share of Americans who are very or somewhat concerned about getting a serious case is 26 points lower than in November 2020, before a COVID-19 vaccine was available to the public. And the share of Americans who are at least somewhat concerned about spreading COVID-19 without knowing it is down 24 points since November 2020.
Still, the current data shows how the virus remains a concern in daily life for many Americans, more than four years after the first confirmed coronavirus cases appeared in the U.S.
Consistent with past Center surveys, there are demographic and political differences in personal concern about getting a serious case of COVID-19 and unknowingly spreading the virus:
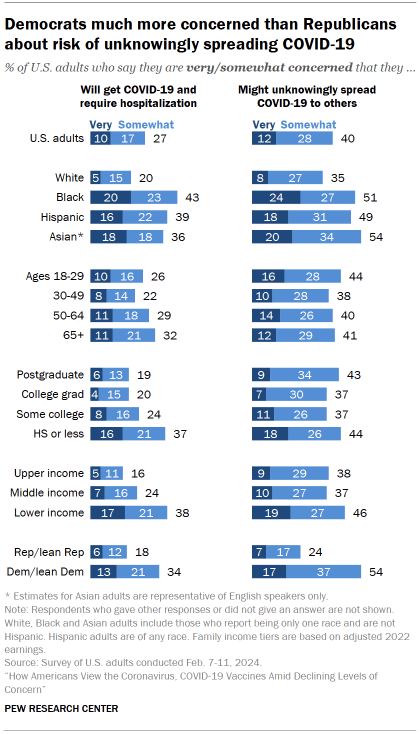
- Income: Lower-income Americans continue to be particularly concerned (38%) about getting a serious case of COVID-19. They’re also more likely than middle- and upper-income Americans to worry about unknowingly spreading COVID-19, but the differences are more modest.
- Party: Democrats (54%) are more than twice as likely as Republicans (24%) to be very or somewhat concerned about unknowingly spreading COVID-19. And they’re 16 points more likely to express concern about getting a serious case of the disease.
- Race and ethnicity: White Americans (20%) are less likely to be concerned about getting a serious case of COVID-19 than Black (43%), Hispanic (39%) and English-speaking Asian Americans (36%).
Some of the groups most personally concerned about getting a severe case of COVID-19 are also among the groups most concerned about the public health threat from the coronavirus. For example, Black adults and adults with lower incomes express more concern about the personal health and public health impact of the coronavirus than White adults and those with upper incomes.
Uptake of the flu shot
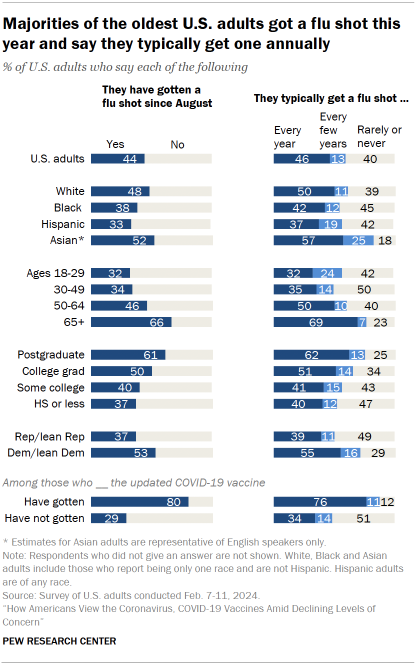
The survey finds 44% of U.S. adults say they have gotten a flu shot since August. This share is down slightly from last March, when 49% of Americans said they had recently gotten a flu shot.
Uptake varies by the following factors:
- Age: Older Americans continue to be more likely to report getting the flu shot. Two-thirds of Americans ages 65 and older say they have gotten the flu shot since August. By comparison, only about a third of those under age 50 say the same. These large age differences are seen among both Democrats and Republicans.
- Race and ethnicity: English-speaking Asian Americans (52%) and White Americans (48%) are more likely than Black Americans (38%) and Hispanic Americans (33%) to say they have gotten a flu shot since August. These racial and ethnic differences are consistent with past Center surveys.
- Partisan affiliation: Democrats are more likely than Republicans to say they got a flu shot this year (53% vs. 37%). This 16-point gap is twice as big now as it was in November 2020, during the pandemic’s first year. The current partisan difference in flu shot uptake is similar to the one recorded in March 2023.
The flu shot and updated COVID-19 vaccines are both recommended to protect against severe illness, but Americans approach these vaccines differently.
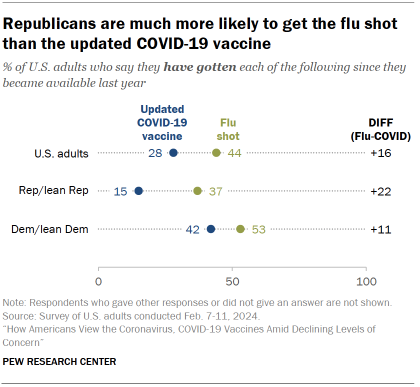
Americans are more likely to report that they received a flu shot than the updated COVID-19 vaccine this year (44% vs. 28%).
This gap in uptake between the flu shot and updated COVID-19 vaccine is more pronounced among Republicans than Democrats.
Republicans are more than twice as likely to say they’ve gotten a flu shot since August as to say they’ve received an updated COVID-19 vaccine (37% vs. 15%). Among Democrats, this difference is more modest (53% vs. 42%).
Add Pew Research Center to your Alexa
Say “Alexa, enable the Pew Research Center flash briefing”
Report Materials
Table of contents, how the pandemic has affected attendance at u.s. religious services, mental health and the pandemic: what u.s. surveys have found, partisan differences are common in the lessons americans take away from covid-19, what we know about online learning and the homework gap amid the pandemic, americans who relied most on trump for covid-19 news among least likely to be vaccinated, most popular.
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Case Reports in Neurosurgery: 2021
Loading... Editorial 06 June 2022 Editorial: Sharing One’s Experience and Advancing Medicine through Case Reports Philipp Taussky 964 views 0 citations
Loading... Case Report 16 March 2022 Coexistence of Pituitary Adenoma and Primary Pituitary Lymphoma: A Case Report and Review of the Literature Shangjun Ren , 5 more and Mengyou Li 1,064 views 4 citations
Case Report 24 January 2022 Internal Maxillary Artery-Radial Artery-Middle Cerebral Artery Bypass and STA-MCA Bypass for the Treatment of Complex Middle Cerebral Artery Bifurcation Aneurysm: A Case Report Chaojue Huang , 3 more and Yongjia Yu 1,665 views 2 citations
Loading... Case Report 14 December 2021 Case Report: Creeping Growth in Lymphoplasmacyte-Rich Meningioma—A Radiologic Variant Jiuhong Li , 4 more and Wenke Liu 1,533 views 5 citations
Loading... Case Report 22 September 2021 Case Report: Whole-Exome Sequencing of Hypothalamic Hamartoma From an Infant With Pallister-Hall Syndrome Revealed Novel de novo Mutation in the GLI3 Yue Yang , 11 more and Han-Song Sheng 2,455 views 4 citations
Case Report 21 September 2021 Technical Case Report of a Cranioplasty With ex vivo Frozen Ostoblastic Bone Graft From Large Skull Metastasis Pang-Shuo Perng , 4 more and Jung-Shun Lee 1,865 views 1 citations
Loading... Case Report 23 August 2021 Ventriculosternal Shunt for the Treatment of Idiopathic Normal Pressure Hydrocephalus: A Case Report Xinxia Guo , 8 more and Junming Zhu 2,374 views 2 citations
Loading... Case Report 06 August 2021 Case Report: High-Definition 4K-3D Exoscope for Removal of an Orbital Cavernous Hemangioma Using a Transpalpebral Approach Stefano Peron , 1 more and Roberto Stefini 2,112 views 4 citations
Case Report 19 July 2021 Case Report: A 62-Year-Old Woman With Contrast-Induced Encephalopathy Caused by Embolization of Intracranial Aneurysm Ying Zhang , 7 more and Ping Liu 2,579 views 1 citations
Case Report 08 July 2021 Case Report: A Rare Case of Fourth Ventricle to Spinal Subarachnoid Space Shunt Migration: Surgical Pearl and Literature Review Nicolas Serratrice , 3 more and Georges Naïm Abi Lahoud 1,573 views 2 citations
Case Report 07 July 2021 Radiological and Clinical Findings of Multiple Cerebellar Liponeurocytoma: A Case Report Shan Wang , 1 more and Chao Wang 2,198 views 1 citations
Case Report 25 May 2021 Anterior Inferior Cerebellar Aneurysm Treated by Aneurysm Resection and Intracranial Artery Anastomosis in situ: A Case Report and Literature Review Chaojue Huang , 2 more and Yongjia Yu 2,143 views 1 citations
Most new doctors face some form of sexual harassment, even after #MeToo
Pair of new studies in first-year residents shows some encouraging trends, variation in experiences, and increased recognition of what constitutes harassment.
More than half of all new doctors face some form of sexual harassment in their first year on the job, including nearly three-quarters of all new female doctors and a third of males, a new study finds.
That's actually down somewhat from the percentage of new doctors who experienced the same five or six years before, according to the paper published in JAMA Health Forum by a team from the University of Michigan Medical School and Medical University of South Carolina.
And today's new doctors are more likely than their predecessors to recognize that what they experienced qualifies as harassment, whether it was gender-biased comments or jokes, persistent unwanted romantic overtures, or pressure to engage in sexual activity for job-related reasons.
But the new study and another paper published recently in JAMA Network Open suggest that medical schools and hospitals need to do more to educate about, and address, all forms of sexual harassment. Some institutions and specific medical specialties have more work to do than others, the research shows.
That's especially true for profession-related sexual coercion, which increased across the six years studied, though it was much rarer than gender-based verbal or work environment harassment.
In all, more than 5% of female first-year residents, also called interns, said in 2023 that they had been in a situation where they felt pressured to engage in a sexual activity in order to get favorable professional treatment. That was more than double the percentage who said so in 2017. The rate in men stayed the same, at less than 2%.
"The overall decrease in sexual harassment incidence over recent years suggests a move in the right direction, however rates of sexual harassment experienced by physician trainees are still alarmingly high," said Elena Frank, Ph.D., lead author of the new study and an assistant research scientist at the Michigan Neuroscience Institute.
The findings come from surveys of thousands of doctors who took part in the Intern Health Study, based at the institute. Each summer, the study enrolls thousands of recent medical school graduates who volunteer to take a variety of smartphone-based surveys and wear activity trackers for their entire intern year.
Recognizing harassment
The new JAMA Health Forum study includes data from nearly 4,000 doctors who finished intern year in 2017, 2018 or 2023. In addition to being asked a general question about whether they had experienced sexual harassment, they were also asked whether and how often they had had specific experiences that qualify as gender-based harassment, unwanted sexual attention and sexual coercion.
That allowed the researchers to measure interns' recognition of what constitutes sexual harassment. To do so, they analyzed how many interns said they had had at least one of those specific experiences, and compared that with each person's answer on the general question of whether they'd experienced sexual harassment.
In all, 55% of the interns in the 2023 group had experienced at least one form of sexual harassment. But only about 18% of that group recognized that they had experienced sexual harassment, and there was a big gap between women and men in recognition.
Recognition of what constitutes sexual harassment has improved, the study shows; in 2017 less than 9% of those who had a sexual harassment experience recognized it as such. Recognition improved fivefold in surgical specialties.
"The persistent gap between the experience and recognition of sexual harassment identified in our study illustrates the importance of looking beyond policy compliance, to challenge the deeply entrenched cultural norms that have enabled sexual and gender-based harassment to continue largely unquestioned in medicine for so long," said Frank, who directs the Intern Health Study team. The society-wide #MeToo movement for sexual harassment awareness and prevention has likely made a difference too.
Variation in experiences
The team explored differences between types and locations of medical training in their JAMA Network Open paper, which is based on 2,000 interns who finished intern year at 28 institutions in 2017.
Interns training in surgery and emergency medicine were 20% more likely than those training in pediatrics or neurology to have experienced sexual harassment in 2017. And interns at some hospitals were 20% more likely to have experienced sexual harassment than those at hospitals with the lowest number of interns reporting any sexual harassment.
Elizabeth Viglianti, M.D., M.P.H., M.Sc., lead author of the JAMA Network Open study and an assistant professor of internal medicine at U-M, notes that the variation between specialties and institutions seen in the study she led suggests that residency programs and hospitals play a key role in combating harassment.
She notes that surgical training programs, which include general surgery and specialties that include surgical training such as gynecology, urology, otolaryngology, neurosurgery, plastic surgery and orthopedic surgery, have the most work to do.
"Until administrators, faculty, and trainees truly understand that sexual harassment is not and should not be an expected or accepted part of the training experience, an equitable and safe learning environment for physicians cannot be achieved," Frank said.
In addition to Frank and Viglianti, the authors of the two papers include Intern Health Study co-investigator Constance Guille, M.D., of the Medical University of South Carolina; Intern Health Study principal investigator Srijan Sen, M.D., Ph.D., who is also the director of the Eisenberg Family Depression Center and a professor of psychiatry and neuroscience at U-M; other U-M faculty Amy Bohnert, Ph.D., M.H.S., Andrea Oliverio, M.D., M.Sc., and Lisa Meeks, Ph.D. as well as Intern Health Study team members Zhuo Joan Zhao, M.S., Yu Fang, M.S.E., Jennifer Cleary, a doctoral student in psychology at U-M, and Karina Pereira-Lima, a Ph.D. student at the University of Sao Paolo.
The Intern Health Study is funded by the National Institute of Mental Health (MH101459). Additional NIH funding was also used for the two studies.
- Gender Difference
- Relationships
- Disorders and Syndromes
- Educational Psychology
- Public Health
- Education and Employment
- Popular Culture
- Educational Policy
- Delusions of parasite infestation
- Sex education
- Homosexuality
- Platonic love
- Bisexuality
- Synesthesia
Story Source:
Materials provided by Michigan Medicine - University of Michigan . Original written by Kara Gavin. Note: Content may be edited for style and length.
Journal References :
- Elena Frank, Zhuo Zhao, Yu Fang, Jennifer L. Cleary, Elizabeth M. Viglianti, Srijan Sen, Constance Guille. Trends in Sexual Harassment Prevalence and Recognition During Intern Year . JAMA Health Forum , 2024; 5 (3): e240139 DOI: 10.1001/jamahealthforum.2024.0139
- Elizabeth M. Viglianti, Andrea L. Oliverio, Karina Pereira-Lima, Elena Frank, Lisa M. Meeks, Srijan Sen, Amy S. B. Bohnert. Variation by Institution in Sexual Harassment Experiences Among US Medical Interns . JAMA Network Open , 2023; 6 (12): e2349129 DOI: 10.1001/jamanetworkopen.2023.49129
Cite This Page :
Explore More
- Complex Biochemical Communication in Plants
- Next-Gen Solar Cells: Perovskite Semiconductors
- When Faces Appear Distorted: Rare Condition
- End of Planet Formation
- Enormous Ice Loss from Greenland Glacier
- Signs of Life Detectable in Single Ice Grain
- Tudor Era Horse Cemetery
- When Do Babies Become Conscious?
- Secrets of the Van Allen Belt Revealed
- Robotic Prostheses, Exoskeletons
Trending Topics
Strange & offbeat.

IMAGES
VIDEO
COMMENTS
Neurosurgery is a surgical procedure that uses invasive techniques to diagnose, investigate and/or treat a neurological disorder, disease or injury. For example, to remove a brain tumour or insert ...
The CNS Neurosurgery Journal publishes top research on clinical and experimental neurosurgery, and the latest developments in science, technology, and medicine. Current Issue : Neurosurgery ... Get new journal Tables of Contents sent right to your email inbox Get New Issue Alerts. Browse Journal Content. Most Popular; For Authors;
N Engl J Med 2024;390:1129-1139. An 84-year-old man was evaluated at the hospital for a fall and admitted for treatment of a presumed urinary tract infection. On hospital day 4, severe chest pain ...
Recent research from the Department of Neurosurgery spans the gamut — from the laboratory to patients' bedsides and beyond, says Chetan Bettegowda, the department's vice chair for research. The aim of the science is to identify biological underpinnings of disease, showcasing new imaging technology and reviewing treatment outcomes in a ...
Explore the latest in neurosurgery, including recent advances in surgical management of epilepsy, CNS tumors, spinal disorders, and more. ... This cross-sectional study uses UK Biobank and All of Us Research Program data to assess whether APOE ε4 is associated with higher risk of intracerebral hemorrhage among patients with known brain ...
Latest Articles : Neurosurgery. Latest Articles. The editors of this journal are pleased to offer electronic publication of accepted papers prior to print publication. These papers can be cited using the date of access and the unique DOI number. Any final changes in manuscripts will be made at the time of print publication and will be reflected ...
The CNS Neurosurgery Journal publishes top research on clinical and experimental neurosurgery, and the latest developments in science, technology, and medicine. ... Get new journal Tables of Contents sent right to your email inbox Get New Issue Alerts. Browse Journal Content. Most Popular; For Authors;
Urology. Urologist - Top $ and Work Life Balance - H1B. The Neurology Neurosurgery page contains articles and information from the New England Journal of Medicine.
Read the latest specialty reports in neurology and neurosurgery, including new research topics, articles, studies, and more at Mount Sinai. Neurology and Neurosurgery . Curing VOGM From Day 6 to Year 6: Baby H has 16 Neuroendovascular Embolizations to Cure a Vein of Galen Malformation .
Neurosurgery is the official publication of the Congress of Neurological Surgeons. Neurosurgery provides multimedia, prompt publication of scientific articles on clinical or experimental surgery topics important for the brain, spine, and peripheral nerves, reviews, and other information of interest to readers across the world! Follow Neurosurgery.
Insights in Neurosurgery: 2021. With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
The first ML approach used in the field of neurosurgery spans about a century ago, in a research published in 1900, that used artificial neural networks (ANNs) to develop structural databases. Since then, there has been great advancement in the field, while in the past 2-3 decades, we can see the implementation of AI and ML algorithms in ...
5,223 views. 5 articles. A platform for the global neurosurgical community to foster innovation and improve patient management across neuro-oncology, skull base surgery, peripheral nerve neurosurgery and neuro-critical care.
Moreover, topic selection in research usually handles already discussed subjects and builds on already existing literature to add new perspectives. But we rarely encounter innovative ideas or out-of-the-box attitudes. ... Atteya, M.M.E. Innovations and new technologies in pediatric neurosurgery. Childs Nerv Syst 37, 1471-1472 (2021). https ...
Basic science research. Several National Institutes of Health-funded laboratories within the department study and model human neurological diseases to discover tomorrow's therapies. Clinical studies. Neurosurgery clinicians and researchers at Mayo Clinic perform hundreds of clinical trials to translate new findings from bench to bedside.
With their unique mixes of varied contributions from Original Research to Review Articles, Research Topics unify the most influential researchers, the latest key findings and historical advances in a hot research area! Find out more on how to host your own Frontiers Research Topic or contribute to one as an author.
In the present review, methods of topic modeling are used to identify the key topics in publications. As an example of AI technologies, these methods are used to analyze texts written in a natural language. Using topic modeling, from 4 to 9 major topics (research areas) were identified for each section of neurosurgery.
Neurology and Neurosurgery Research. Johns Hopkins neurology and neurosurgery research brings together some of the world's most creative and curious minds who are working toward cures for devastating diseases such as brain cancer, Parkinson's disease, ALS and dementia, while broadening our understanding of the most complex organ system in ...
Research finds a direct communication path between the lungs and the brain. ScienceDaily . Retrieved March 24, 2024 from www.sciencedaily.com / releases / 2024 / 03 / 240321155335.htm
Morbidity and Function Loss After Resection of Malignant Peripheral Nerve Sheath Tumors. Martin E, Pendleton C, Verhoef C, Spinner RJ, Coert JH, on behalf of MONACO collaborators. Neurosurgery. 2022;90 (3):354-364, doi: 10.1093/neuros/nyab342.
Mor matched into neurosurgery, Cruz into general surgery, and Robles into anesthesiology — all at UC Davis. Gaeta matched into general surgery at the University of Illinois, Peoria. Proud parents snapped photos of their newly matched students, who posed proudly while holding celebratory signs and balloons.
Her entire family flew in from Texas, New York City and Boston to celebrate the first physician in the family. "I feel very, very lucky. Just being here on Match Day, surrounded by loved ones, is a dream come true," she said. She thought about the journey ahead. "I'm going to need a winter coat."
Despite all the craze around psychedelics, little research has been done to prove their efficacy treating addiction disorders. Mash pleaded for more evidence-based research that could lead to regulatory approval and make such treatments safely available to those who are "suffering the most." So far, what researchers have is anecdotal.
The course, co-developed with the departments of pathology and neurosurgery, will focus on the molecular and genetic foundations of adult primary central nervous system tumors, applying those concepts to the care of patients with brain tumors through the lenses of neuroradiology, neurosurgery, neuropathology, neuro-oncology and radiation
Lily Sandblom revels in the moment after announcing her match. The UArizona College of Medicine - Phoenix is a central part of that Graduate Medical Education growth, expanding three of its existing programs in 2024.By 2027, 16 new programs will be launched in specialties including anesthesiology, dermatology, neurosurgery, ophthalmology and otolaryngology, among others.
A new Pew Research Center survey finds that just 20% of Americans view the coronavirus as a major threat to the health of the U.S. population today and only 10% are very concerned they will get it and require hospitalization. This data represents a low ebb of public concern about the virus that reached its height in the summer and fall of 2020, when as many as two-thirds of Americans viewed ...
This Research Topic was developed in order to highlight high-quality case reports in areas of neurosurgery, including spine, vascular/endovascular management of vascular disease and stroke, neuro-oncology, skull base surgery, functional neurosurgery, pediatric neurosurgery, peripheral nerve neurosurgery, and trauma/neuro critical care. />Case reports aim to highlight unique cases of patients ...
Dec. 16, 2019 — Casual flirting with colleagues at work is relatively harmless and can even be beneficial, according to a new study. The research focuses on the little studied area of positively ...
Research in Neurological Surgery. Neurosurgical research is a fundamental driver of understanding and continues to improve care across the biomedical sciences. Neurosurgeons from around the world have the distinct opportunity to obtain physiologic data, access normal/diseased neural tissues, make direct clinical-operative correlations, develop ...