- Advanced search

Deposit your research
- Open Access
- About UCL Discovery
- UCL Discovery Plus
- REF and open access
- UCL e-theses guidelines
- Notices and policies
UCL Discovery download statistics are currently being regenerated.
We estimate that this process will complete on or before Mon 06-Jul-2020. Until then, reported statistics will be incomplete.
Improving The Diagnosis And Risk Stratification Of Prostate Cancer

The current diagnostic and stratification pathway for prostate cancer has led to over-diagnosis and over- treatment. This thesis aims to improve the prostate cancer diagnosis pathway by developing a minimally invasive blood test to inform diagnosis alongside mpMRI and to understand the true Gleason 4 burden which will help better stratify disease and guide clinicians in treatment planning. To reduce the number of patients who have to undergo prostate biopsy after indeterminate or false positive prostate mpMRI, we aimed to develop a new panel of mRNA detectable in blood or urine that was able to improve the detection of clinical significant prostate cancer (Gleason 4+3 or ≥6mm) in combination with prostate mpMRI. mRNA expression of 28 potential genes was studied in four prostate cancer cell lines and, using publicly available datasets, a new seven gene biomarker panel was developed using machine learning techniques. The signature was then validated in blood and urine samples from the ProMPT, PROMIS and INNOVATE trials. To redefine the classification of Gleason 4 disease in prostate cancer patients, digital pathology was used to contour and accurately assess the burden and spread of Gleason 4 in a cohort of PROMIS patients compared to the gold standard manual pathology. There was a significant difference between observed and objective Gleason 4 burden that has implications in patient risk stratification and biomarker discovery. The work presented in this thesis makes a significant step toward improving the patient diagnostic and risk classification pathways by ensuring only the right patients are biopsied when necessary, improving the current pathological reference standard.

Archive Staff Only
- Freedom of Information
- Accessibility
- Advanced Search
- Original Research
- Open access
- Published: 07 November 2020
Assessment of knowledge, practice and attitude towards prostate cancer screening among male patients aged 40 years and above at Kitwe Teaching Hospital, Zambia
- Sakala Gift ORCID: orcid.org/0000-0003-0438-6804 1 ,
- Kasongo Nancy 2 &
- Mwanakasale Victor 1
African Journal of Urology volume 26 , Article number: 70 ( 2020 ) Cite this article
9244 Accesses
5 Citations
Metrics details
Prostate cancer is a leading cause of cancer death in men. Evaluating knowledge, practice and attitudes towards the condition is important to identify key areas where interventions can be instituted.
This was a hospital-based descriptive cross-sectional study aimed at assessing knowledge, practice and attitude towards prostate cancer screening among male patients aged 40 years and above at Kitwe Teaching Hospital, Zambia.
A total of 200 men took part in the study (response rate = 100%). Of the 200 respondents, 67 (33.5%) had heard about prostate cancer and 58 (29%) expressed knowledge of prostate cancer out of which 37 (63.8%) had low knowledge. Twenty-six participants (13%) were screened for prostate cancer in the last 2 years. 98.5% of the participants had a positive attitude towards prostate cancer screening. Binary logistic regression results showed that advanced age ( p = 0.017), having secondary or tertiary education ( p = 0.041), increased knowledge ( p = 0.023) and family history of cancer ( p = 0.003) increased prostate cancer screening practice. After multivariate analysis, participants with increased knowledge ( p = 0.001) and family history of cancer ( p = 0.002) were more likely to practice prostate cancer screening.
The study revealed low knowledge of prostate cancer, low prostate cancer screening practice and positive attitude of men towards prostate cancer screening. These findings indicate a need for increased public sensitization campaigns on prostate cancer and its screening tests to improve public understanding about the disease with the aim of early detection.
1 Background
Prostate cancer, or adenocarcinoma of the prostate as it is called in some settings, can be described as cancer of the prostate gland.
The prostate is a small fibromuscular accessory gland of male reproductive system weighing about 20 g. It is located posterior to the pubic symphysis, superior to the perineal membrane, inferior to the bladder and anterior to the rectum. It produces and secretes proteolytic enzymes into semen, to facilitate fertilization [ 1 , 2 ].
Prostate cancer is characterized by both physical and psychological symptoms [ 3 ]. Early-stage prostate cancer is usually asymptomatic [ 4 ]. More advanced disease has similar symptoms with benign prostate conditions such as weak or interrupted urine flow, hesitancy, frequency, nocturia, hematuria or dysuria. Late-stage prostate cancer commonly spreads to bones and cause pain in the hips, spine or ribs [ 4 ]. The 2 commonly used screening methods for prostate cancer are digital rectal examination (DRE) and prostate-specific antigen (PSA) test.
Prostate cancer is one of the leading causes of cancer-related deaths among males globally [ 4 ]. The 2018 Global Cancer Project (GLOBOCAN) report estimated 1 276 106 new cases in 2018, representing 7.1% of all cancers worldwide [ 5 ]. The report further estimated the number of deaths due to prostate cancer at 358 989, representing 3.8% of all cancers globally. It was thus ranked the second most common cancer and the fifth leading cause of cancer death in men. The American Cancer Society 2019 report showed that an estimated 174,650 new cases of prostate cancer would be diagnosed in the USA during 2019 [ 4 ]. The report further stated that an estimated 31,620 deaths from prostate cancer would occur in 2019. It further put the incidence of prostate cancer to about 60% higher in blacks than in whites suggesting a genetic predilection to the cancer.
Africa is no exception to this global trend of high incidence and mortality of prostate cancer with age-standardized incidence and mortality rates of 26.6 and 14.6 per 100 000 men, respectively [ 5 ]. This placed prostate cancer as the third most common cancer among both sexes and the fourth leading cause of all cancer deaths among both sexes in the region. Current statistics on Zambia indicate that Zambia has one of the world’s highest estimated mortality rates from prostate cancer [ 6 , 7 ]. The age standardized incidence and mortality rates from prostate cancer are at 45.6 and 28.4 per 100,000 men, respectively [ 5 ].
Although the causes of prostate cancer are not yet fully understood, it is thought that advanced age (above 50 years), positive family history of prostate cancer and an African-American ethnic background are risk factors [ 4 , 8 ].
In mitigating the effects of diseases like prostate cancer, evaluating knowledge, practice and attitudes towards the condition is important to identify key areas where interventions can be instituted. For instance, studies in other countries that accessed these factors were able to identify the role that health workers and political will could play in increasing knowledge and screening for prostate cancer [ 8 , 9 , 10 ]. Furthermore, low level of awareness about prostate cancer or the complete lack of it has been identified as the cause of late presentation and poor prognosis [ 11 , 12 ].
Despite Zambia having one of the world’s highest estimated mortality rates from prostate cancer [ 6 , 7 ] coupled with an increased suggested genetic predilection to the cancer [ 4 ], since the majority of the male population are black, no studies assessing knowledge, practice and attitude towards prostate cancer screening have been done. This study therefore sought to address the gap.
The aims of the study were to determine the knowledge, practice and attitude towards prostate cancer screening at Kitwe Teaching Hospital (KTH). In addition, the study also aimed to determine the association between demographics of participants and knowledge, knowledge of participants and attitude towards prostate cancer screening, knowledge of participants and prostate cancer screening practice as well as attitude of participants towards prostate cancer screening and prostate cancer screening practice.
2.2 Study site and design
The study was done at KTH in the Copperbelt province of Zambia. It is a tertiary referral hospital in the region whose catchment area includes Copperbelt, Luapula and North-western provinces. It has a bed capacity of 630 [ 13 ].
This was a descriptive cross-sectional study of knowledge, practice and attitude towards prostate cancer screening among male patients aged 40 years and above at KTH. The study design was chosen because it is simple to use, cost-effective and time economic.
2.3 Study participants
The sample size was ascertained using the ‘Stalcalc’ function of Epi Info Version 7.1.5. In a month, nearly 419 male patients presented to the target areas for this study at KTH, namely Out-Patient Department (OPD), medical and surgical admission wards. Since data for this study were collected in 1 month, 419 was used as the total population size. A confidence level was 95% and a confidence limit was 5% (at 95% confidence level) and the expected frequency was 50%. Therefore, a sample size of 200 was calculated for this study. Study participants were randomly selected from target areas. All consenting male patients aged 40 years and above in the target areas for this study at KTH were enrolled until the targeted sample size was reached. Male patients aged less than 40 years and participants who did not give consent were excluded from the study.
2.4 Study duration
The study was done in a period of 6 months from April to September 2019.
2.5 Data collection and analysis
The study objectives were explained to participants, and written and informed consent was obtained. Participants were enrolled utilizing a well-structured questionnaire as shown in “Appendix”. The questionnaire collected demographic information including age, marital status, education and occupation. It also collected data on family history of cancer as well as knowledge, practice and attitudes towards prostate cancer screening. Translations to the questionnaire were done from English to a suitable local language according to the participant’s preference. The responses were recorded as given by the participants.
Data collected during the study were checked for completeness and double-entered into the Epi Info version 7 software. Frequency tables and graphs were generated for relevant variables. The data were analysed using Statistical Package for Social Sciences (SPSS) version 23. For comparing associations between variables, Pearson Chi-square test was performed. A p value of equal or less than 0.05 was considered significant. Binary logistic regression, as well as multivariate analysis, was done. Low knowledge was defined as scoring 1–3 correct responses in the knowledge section, moderate knowledge as scoring 4–6 correct responses and high knowledge as scoring 7–9. Positive attitude was defined as scoring 2 or more correct responses in the section assessing attitudes, while negative was defined as scoring less than 2 correct responses. Practice was assessed with a closed-ended question in the practice section.
A total of 200 participants were enrolled.
3.1 Background characteristics
As illustrated in Table 1 , more than half, 149 (74.5%), of the participants in the study were in the 40–60 years age range. All participants were Christians, 161 (80.5%) had no formal education or had primary education, and 198 (99%) were in informal employment or unemployed.
3.2 Knowledge of prostate cancer
Of the 200 participants enrolled, 67 (33.5%) had heard about prostate cancer, while 133 (66.5%) had never heard about it. Majority, 55.3%, of the participants who had had heard about prostate cancer pointed to a doctor or nurse as a source of information as shown in Table 2 .
Of the 200 participants enrolled in the study, 58 (29%) expressed knowledge on prostate cancer. Among participants who had knowledge, majority of them, 37 (63.8%) had low knowledge as shown in Fig. 1 .
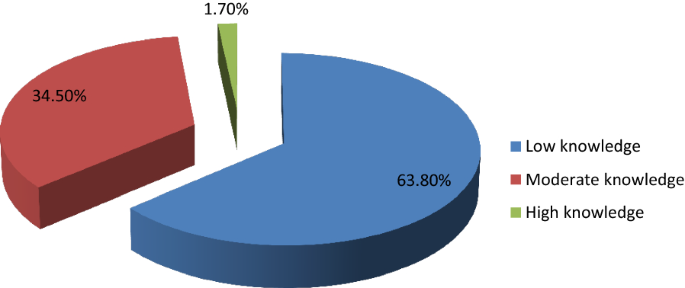
Levels of knowledge
Participants who had secondary school or tertiary education were more knowledgeable about prostate cancer than those who did not have ( p < 0.001). Participants who had heard about prostate cancer were more knowledgeable than those who had not ( p < 0.001). Participants who had heard about prostate cancer had high levels of knowledge compared to those who had not ( p = 0.009). Participants older than 60 years had more knowledge on prostate cancer compared with those below 60 years ( p = 0.026).
3.3 Practice of prostate cancer screening
Of the 200 participants, only 26 (13%) had been screened in the last 2 years. Among participants who had screened, 20 (76.9%) pointed out DRE as the method used, while 3 (11.5%) pointed out PSA, 2 (7.69%) reported both DRE and PSA, and 1 (3.85%) did not know which screening method was used. Among the 26 participants that had screened in the last 2 years, 18 (69.2%) had a positive prostate cancer outcome, while 8 (30.8%) had a negative prostate cancer outcome. 199 (99.5%) of the participants expressed intentions to screen in future.
Age above 60 years was associated with a positive prostate cancer outcome ( p = 0.002). The study also found that participants who were knowledgeable about prostate cancer were more likely to undergo prostate cancer screening ( p < 0.001) and that high level of knowledge was associated with prostate cancer screening practice ( p = 0.024). Increasing age of participants (over 60) was also associated with prostate cancer screening practice in the last 2 years ( p < 0.001).
3.4 Attitude towards prostate cancer screening
Among 200 participants enrolled in the study, 197 (98.5%) had a positive attitude towards prostate cancer screening, while 3 (1.5%) had a negative attitude. There were no statistically significant associations between age and attitude towards prostate cancer screening ( p = 0.099), knowledge and attitude towards prostate cancer screening ( p = 0.868) as well as between practice in the last 2 years and attitude towards prostate cancer screening ( p = 0.291).
3.5 Factors affecting prostate cancer screening practice
Binary logistic regression analysis was performed to identify factors that affect prostate cancer screening. As shown in Table 3 , prostate cancer screening practice was associated with age ( p = 0.017), education ( p = 0.041), knowledge ( p = 0.023) and family history of cancer ( p = 0.003).
All factors that were significant in binary logistic analysis (with p < 0.05) were analysed using multivariate logistic regression. A backward step-by-step elimination method was employed to manually eliminate factors with insignificant p values. As illustrated in Table 4 , only two factors remained statistically significant, namely knowledge and family history of cancer. Participants who had knowledge about prostate cancer were nearly 11 times more likely to practice prostate cancer screening than those who did not have ( p = 0.001). Participants who had a family history of cancer were 26 times more likely to practice prostate cancer screening than those who had a negative family history of cancer ( p = 0.002).
4 Discussion
The study targeted male patients aged 40 years and above due to available literature which indicates that prostate cancer screening should start at 40 years [ 4 , 14 ]. Literature indicates that the average age of a man to be diagnosed with prostate cancer is about 66 years and above [ 4 , 15 ]. Since the majority of the participants in the study, 149 (74.5%), were in the 40–60 years age group, as also observed by Mofolo and colleagues in their study [ 16 ], there was an over representation of participants at the lowest risk of prostate cancer.
The study found low levels of awareness and knowledge. This is similar to findings of other studies done in other countries [ 10 , 17 ]. This implies that there is little sensitization being done to the public and expresses the need for more public sensitization campaigns utilizing both electronic and print media with the aim of early detection and treatment to improve the prognosis [ 7 , 8 , 11 ]. However, other studies found high levels of awareness [ 9 , 18 , 19 , 20 ]. Of the studies that found high levels of knowledge, one of them was done on a group of public servants who were educated, had good access to health information and this was not a reflection of the general population who are mostly uneducated [ 9 ]. The study also demonstrated that majority of the participants who were knowledgeable about prostate cancer had low level of knowledge which was consistent with findings by other studies [ 10 , 18 , 19 , 21 , 22 , 23 ]. This indicates a need for comprehensive knowledge on prostate cancer to promote early detection.
Participants with higher level of education were more knowledgeable about prostate cancer than those who had lower level of education or no formal education at all consistent with findings by similar studies done in other countries [ 16 , 17 , 21 , 24 ]. However, some studies done in Nigeria and Kenya in 2018 did not find such an association [ 10 , 19 ]. In one of the studies that did not find an association between higher education and knowledge, the sample was drawn from a rural part of the country with more than 60% having no formal education or had primary education [ 19 ]. This could have resulted in the finding.
Participants older than 60 years had more knowledge on prostate cancer than those below 60 years as also demonstrated by Adibe et al. [ 24 ]. This highlights a possible bias that might be present in the provision of information on prostate cancer where individuals who are at an advanced age are educated about it because of their increased risk. It could also indicate the natural history of how older patients are more likely to have information about prostate cancer as they visit healthcare centres for urologic problems like benign prostate hyperplasia which are quiet frequent [ 4 , 15 ].
In addition to health workers contributing to the increase in knowledge of prostate cancer, utilizing media platforms that are widely accessible such as radio presents a great opportunity to achieve this. A 2018 study by Kinyao and Kishoyian which assessed attitudes, perceived risk and intention in a rural county found that over 60% of the participants learnt about prostate cancer from the radio [ 19 ]. This shows how much more applicable this media platform can be in developing regions like Africa.
The low level of prostate cancer screening practice demonstrated in the study is consistent with findings from similar studies [ 10 , 11 , 19 , 21 , 25 ] though majority of participants in this study were willing to be screened after discussing about the condition with them consistent with a study done in Kenya [ 21 ]. However, it is inconclusive whether increased knowledge would increase screening as other factors apart from knowledge on prostate cancer appear to influence this practice. A similar study by Kinyao and Kishoyian in 2018 found that many participants had strong fatalistic attitudes towards screening such as “if I am meant to get prostate cancer, I will get it” and these appeared to influence screening [ 19 ]. Thus in sharing information on prostate cancer, cultural beliefs and fatalistic attitudes must also be addressed.
DRE was the most commonly used method of prostate cancer screening contrary to findings by similar studies done in Nigeria that found PSA to be the most commonly used method [ 24 , 25 ]. This suggests a possible cost barrier to utilization of the PSA screening method in our sample.
The finding demonstrated in the study that participants were more likely to screen for prostate cancer if they were older than 60 years is consistent with findings of similar studies done in Uganda and Nigeria [ 11 , 25 ]. This implies that there is a risk of late presentation and consequently poor prognosis. As such, intensified public sensitization campaigns are needed to attain early detection and treatment as well as good prognosis. Participants who were more educated were more likely to undergo prostate cancer screening consistent with findings from a Nigerian study [ 25 ]. The statistically significant association between knowledge on prostate cancer and prostate cancer screening practice is consistent with other similar studies done [ 10 , 11 , 21 ]. This is another indication of the need to intensify prostate cancer sensitization campaigns.
The high positive attitude level demonstrated in the study was similar to findings from other studies done [ 9 , 23 , 24 ]. However, a Ugandan study found a negative attitude towards prostate cancer screening [ 11 ]. This could be because the study explored other factors under attitude that our study did not. The lack of any statistically significant association between age of participants and attitude towards prostate cancer screening concurs with findings from a study done in Uganda [ 11 ]. However, a 2017 study done in Nigeria found an association between age and attitude [ 24 ].
5 Limitations of Study
Generalizability of findings of this study must be done with caution since this was a hospital-based study. There is thus a need for more studies to be done in other institutions such as universities and colleges, urban and rural communities, district, general, central and other teaching hospitals to have comprehensive knowledge. In addition, certain aspects of knowledge were not assessed, for example, that prostate cancer can present without symptoms. As such, the study findings were limited to comparisons with studies that also did not assess the asymptomatic presentation of prostate cancer.
6 Conclusion
The study revealed low knowledge of prostate cancer, low prostate cancer screening practice and positive attitude of men towards prostate cancer screening. Practice of prostate cancer screening was associated with age, education level, knowledge and family history of cancer.
Being the first study to assess knowledge, practice and attitude towards prostate cancer screening in Zambia, it has bridged the knowledge gap and has also provided valuable information for healthcare intervention.
Availability of data and material
Data used in the study is available in additional file 1 captioned ‘Dataset for AFJU-D-19-00041R2 manuscript’ and authors agree to share it.
Abbreviations
- Digital rectal examination
- Prostate-specific antigen
Out-Patient Department
Tropical Diseases Research Centre
National Health Research Authority
Kitwe Teaching Hospital
Global Cancer Project
Blandy J, Kaisary A (2009) Lecture notes urology, 6th edn. Wiley, Hoboken
Google Scholar
Shenoy KR, Shenoy A (2019) Manipal manual of surgery, 4th edn. CBS Publishers Pvt Ltd., Shenoy Nagar
Desousa A, Sonavane S, Mehta J (2012) Psychological aspects of prostate cancer. Prostate Cancer and Prostatic Dis 15(2):120–127
Article CAS Google Scholar
American Cancer Society (2019) Cancer facts and figures, 2019. American Cancer Society, Atlanta
GloboCan (2018). http://globocan.iarc.fr
GloboCan (2012). http://globocan.iarc.fr
National Cancer Control Strategic Plan 2016–2021. Ministry of Health Zambia
So WK, Choi KC, Tang WP, Lee PC, Shiu AT, Ho SS et al (2014) Uptake of prostate cancer screening and associated factors among Chinese men aged 50 or more: a population-based survey. Cancer Biol Med 11(1):56–63
PubMed PubMed Central Google Scholar
Oranusi CK, Mbieri UT, Oranusi IO, Nwofor AME (2012) Prostate cancer awareness and screening among male public servants in Anambra State Nigeria. Afr J Urol 18(2):72–74
Article Google Scholar
Awosan KJ, Yunusa EU, Agwu NP, Taofiq S (2018) Knowledge of prostate cancer and screening practices among men in Sokoto, Nigeria. Asian J Med Sci 9(6):51–56
Nakandi H, Kirabo M, Semugabo C, Kittengo A, Kitayimbwa P, Kalungi S, Maena J (2013) Knowledge, attitudes and practices of Ugandan men regarding prostate cancer. Afr J Urol 19(4):165–170
Ito K (2014) Prostate cancer in Asian men. Nat Rev Urol 11:197
Sichula M, Kabelenga E, Mwanakasale V (2018) Factors influencing malnutrition among under five children at Kitwe Teaching Hospital, Zambia. Int J Curr Innov in Adv Res 1(7):9–18
Canadian National Institute of Health (2013)
Cancer Diseases Hospital (2013) Annual report
Mofolo N, Betshu O, Kenna O, Koroma S, Lebeko T, Claassen FM, Joubert Gina (2015) Knowledge of prostate cancer among males attending a Urology clinic, a South African study. SpringerPlus 4:67
Kabore FA, Kambou T, Zango B, Ouédraogo A (2014) Knowledge and awareness of prostate cancer among the general public in Burkina Faso. J Cancer Educ 29:69–73. https://doi.org/10.1007/s13187-013-0545-2
Article PubMed Google Scholar
Muhammad FHMS, Soon LK, Azlina Y (2016) Knowledge, awareness and perception towards prostate cancer among male public staffs in Kelantan. Int J of Public Health Clin Sci 3(6):105–115
Kinyao M, Kishoyina G (2018) Attitude, perceived risk and intention to screen for prostate cancer by adult men in Kasikeu sub location, Makueni County, Kenya. Ann Med Health Sci Res 8(3):125–132
Agbugui JO, Obarisiagbon EO, Nwajei CO, Osaigbovo EO, Okolo JC, Akinyele AO (2013) Awareness and knowledge of prostate cancer among men in Benin City, Nigeria. J Med Biomed Res 12(2):42–47
Wanyagah P (2013) Prostate cancer awareness, knowledge, perception on self-vulnerability and uptake of screening among men in Nairobi. Kenyatta University, Kenya
Arafa MA, Rabah DM, Wahdan IH (2012) Awareness of general public towards cancer prostate and screening practice in Arabic communities: a comparative multi-center study. Asian Pac J Cancer Prev 13:4321–4326
Makado E, Makado RK, Rusere MT (2015) An assessment of knowledge of and attitudes towards prostate cancer screening among men aged 40 to 60 years at Chitungwiza Central Hospital in Zimbabwe. Int J Humanit Soc Stud 3(4):45–55
Adibe MO, Oyine DA, Abdulmuminu I, Chibueze A (2017) Knowledge, attitudes and perceptions of prostate cancer among male staff of the University of Nigeria. Asian Pac J Cancer Prev 18(7):1961–1966
Ebuechi OM, Otumu IU (2011) Prostate screening practices among male staff of the University of Lagos, Lagos, Nigeria. Afr J Urol 17(4):122–134
Download references
Acknowledgements
First and foremost, I express my sincere, heartfelt and profound gratitude to the Almighty God for guiding, protecting and seeing me through the entire process of conducting this study. I am also grateful to my supervisor Prof. Victor Mwanasakale for his zeal and tireless efforts in seeing to it that this work becomes a reality. Let me also express my gratitude to Prof. Seter Siziya and the entire public health team for all the advice, encouragement. I would also like to thank the entire management at the Copperbelt University Michael Chilufya Sata School of Medicine for a friendly atmosphere. I would also like to thank my family back home for all the support and trust vested in me as well as my friends, roommates and class mates for the moral support.
A thesis submitted in partial fulfilment for the award of the Bachelors degree in medicine and surgery (MBChB).
This work was funded by the Government of the Republic of Zambia through the Ministry of Higher Education through its Higher Education Loans and Scholarships Board. As part of policy, the Ministry of Higher Education through its Higher Education Loans and Scholarships Board finances students in Higher Education institutions whose training demands the carrying out of research. Funding given covers for such expenses incurred during research such as printing and photocopying of data collection tools, transport charges for the researcher during the whole process and ethical clearance charges.
Author information
Authors and affiliations.
Michael Chilufya Sata School of Medicine, The Copperbelt University, P.O. Box 71191, Ndola, Zambia
Sakala Gift & Mwanakasale Victor
Pan - African Organization for Health, Education and Research (POHER), Lusaka, Zambia
Kasongo Nancy
You can also search for this author in PubMed Google Scholar
Contributions
SG is the corresponding author, and KN and MV are the contributing authors. SG constructed the manuscript, collected data, analysed and interpreted data and also edited the manuscript. KN constructed the manuscript, analysed and interpreted data and extensively edited the manuscript. MV constructed the manuscript, extensively edited the manuscript and supervised this thesis study. All authors read and approved the final manuscript.
Author’s information
The corresponding author (S.G) is currently pursuing his Bachelors degree in Medicine and Surgery (MBChB) at the Copperbelt University Michael Chilufya Sata School of Medicine in Zambia. K.N is a Pan African Organization for Health, Education and Research (POHER) scholar with a rich research background, who has presented at so many conferences. She was a recipient of the international research elective which took place at University of Missouri School of Medicine, USA, for 2–3 months. She holds a Bachelors Degree of Medicine and Surgery (MBChB) and graduated as the Best student. M.V was also the supervisor of this work. He holds BSc Human Biology, MBChB, MSc and a PhD in Parasitology and is an Associate Professor of Parasitology at the Copperbelt University Michael Chilufya Sata School of Medicine, Zambia.
Corresponding author
Correspondence to Sakala Gift .
Ethics declarations
Ethics approval and consent to participate.
A request to conduct the study was sought from the Tropical Diseases Research Centre (TDRC) research ethics committee (IRB Registration Number: 00002911, FWA Number: 00003729) as well as the National Health Research Authority (NHRA). Management at Kitwe Teaching Hospital was assured that confidentiality would not be breached and that the data obtained in the study would not be used for any other purpose besides that specified in the study protocol. Informed and written consent was obtained from participants. During data collection, no identifying images or other personal or clinical details of participants were collected. They were treated with at-most respect and dignity and their rights to privacy and confidentiality were not violated at any point.
Consent for publication
In this study, no data that could compromise the anonymity of participants such as images or other personal or clinical details were collected. As such, it was not applicable.
Competing interest
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:.
Dataset for AFJU-D-19-00041R2 manuscript.
Appendix: Questionnaire
Topic: assessment of knowledge, practice and attitude towards prostate cancer screening among male patients aged 40 years and above at Kitwe Teaching Hospital.
NAME OF INTERVIEWER:…………………………………………………………
SERIAL NUMBER OF PARTICIPANT:…………………………………………….
DATE:…………………………………………………………………………………
1.1 Section A: demographic characteristics
Instruction: Please, tick as appropriate.
1. Age:…………years
2. Marital status: Single [] Married [] Divorced [] Separated []
3. Religion: Christian [] Muslim [] Traditional []
4. Educational level: Primary [] Secondary [] Tertiary [] No formal education []
5. Occupation: Trader [] Civil servant [] Taxi driver [] Businessman [] Electrician [] Mechanic [] Barber [] Other (please specify)
1.2 Section B: family history of cancer
6. Does anyone in your family have cancer? Yes [] No []
i) What type of cancer………………………………………………………
ii) What is their relation to you………………………………………………
7. Has anyone in your family died of Cancer Yes [] No []
i) What type of cancer……………………………………………………..
ii) What is their relation to you……………………………………………
1.3 Section C: knowledge
8. Have you heard of prostate cancer before: Yes [] No []
i) Where did you hear it from Friends [] Read about it [] TV [] Radio [] Doctor [] Nurse [] Relative []
ii) Which gender does prostate cancer affect Men only [] Women only [] Both men and women [] I do not know []
iii) Which of the following factors could make a person more likely to develop prostate cancer. Please tick as many as possible
a) Family history of the disease [] b) Drinking alcohol [] c) Age [] d)Exercise [] e) Diet [] f) Smoking []
9. Do you know symptoms of prostate cancer Yes [] No []
If Yes, what are they? Tick as many as possible. a) Excessive urination at night [] b)Headache [] c) blood in urine [] d) High temperature [] e) Bone pain [] f) Painful sex [] g) Loss of sex drive [] h) Infertility [] i) cough []
10. Is prostate cancer preventable Yes [] No [] I do not know []
a) How can it be prevented? Genital hygiene [] regular screening [] condom use [] use of right diet [] avoiding many sexual partners []
11. Is prostate cancer curable Yes [] No [] I don’t know []
1.4 Section D: practice
12. Have you been screened for prostate cancer within the last two years? Yes [] No []
a) Which method was used Prostate Specific Antigen (PSA) [] Digital Rectal Examination (DRE) [] I do not know []
b) What was the outcome of the screening? Positive [] Negative []
13. Do you have any intention of getting screened in the nearest future? Yes [] No []
1.5 Section E: attitude towards prostate cancer screening
14. Prostate cancer screening is good Yes [] No []
15. Going for prostate cancer screening is a waste of time Yes [] No []
16. Prostate cancer screening has side effects that can cause harmful effects to the body Yes [] No []
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Gift, S., Nancy, K. & Victor, M. Assessment of knowledge, practice and attitude towards prostate cancer screening among male patients aged 40 years and above at Kitwe Teaching Hospital, Zambia. Afr J Urol 26 , 70 (2020). https://doi.org/10.1186/s12301-020-00067-0
Download citation
Received : 01 November 2019
Accepted : 16 September 2020
Published : 07 November 2020
DOI : https://doi.org/10.1186/s12301-020-00067-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Prostate cancer screening
- Open access
- Published: 06 May 2021
Knowledge of prostate cancer presentation, etiology, and screening practices among women: a mixed-methods systematic review
- Ebenezer Wiafe ORCID: orcid.org/0000-0002-0496-5737 1 , 2 ,
- Kofi Boamah Mensah 1 , 3 ,
- Adwoa Bemah Boamah Mensah 3 ,
- Varsha Bangalee 1 &
- Frasia Oosthuizen 1
Systematic Reviews volume 10 , Article number: 138 ( 2021 ) Cite this article
2877 Accesses
5 Citations
2 Altmetric
Metrics details
With the burden of prostate cancer, it has become imperative to exploit cost-effective ways to tackle this menace. Women have demonstrated their ability to recognize early cancer signs, and it is, therefore, relevant to include women in strategies to improve the early detection of prostate cancer. This systematic review seeks to gather evidence from studies that investigated women’s knowledge about (1) the signs and symptoms, (2) causes and risk factors, and (3) the screening modalities of prostate cancer. Findings from the review will better position women in the fight against the late detection of prostate cancer.
The convergent segregated approach to the conduct of mixed-methods systematic reviews was employed. Five databases, namely, MEDLINE (EBSCOhost), CINAHL (EBSCOhost), PsycINFO (EBSCOhost), Web of Science, and EMBASE (Ovid), were searched from January 1999 to December 2019 for studies conducted with a focus on the knowledge of women on the signs and symptoms, the causes and risk factors, and the screening modalities of prostate cancer.
Of 2201 titles and abstracts screened, 22 full-text papers were retrieved and reviewed, and 7 were included: 3 quantitative, 1 qualitative, and 3 mixed-methods studies. Both quantitative and qualitative findings indicate that women have moderate knowledge of the signs and symptoms and the causes and risk factors of prostate cancer. However, women recorded poor knowledge about prostate cancer screening modalities or tools.
Conclusions
Moderate knowledge of women on the signs and symptoms and the causes and risk factors of prostate cancer was associated with education. These findings provide vital information for the prevention and control of prostate cancer and encourage policy-makers to incorporate health promotion and awareness campaigns in health policies to improve knowledge and awareness of prostate cancer globally.
Systematic review registration
Open Science Framework (OSF) registration DOI: https://doi.org/10.17605/OSF.IO/BR456
Peer Review reports
Prostate cancer (PCa) is the most common non-skin cancer occurring in men and is accountable for 3.8% of all mortality caused by cancer in men [ 1 , 2 ]. According to the GLOBOCAN, 2018 database, it is estimated that it is the fifth primary cause of cancer death in men globally. It further reported that the highest mortality rate is found in the Caribbean and Southern African men worldwide [ 1 , 3 ]. A recent study by Yeboah-Asiamah et al. reported that PCa was the second most common cancer in areas such as Australia, the USA, and New Zealand [ 4 ]. Though fewer than 30% of all incidence of PCa are from developing countries, these countries have previously been estimated to have the highest mortality from PCa due to late diagnosis [ 5 , 6 ]. Although sub-Saharan Africa (SSA) has a low rate of the disease, the incidence is projected to increase if screening is encouraged [ 7 ]. Hence, PCa remains a vital public health concern in both developed and developing countries.
The Centers for Disease Control and Prevention (CDC) in North America organized a workshop with the motive to explore strategies to control and prevent the disease based on the increasing incidence and mortality rate of PCa [ 8 ]. To address mortality rates related to the disease, participants recommended strategies to improve PCa awareness [ 8 ]. Also, as documented by many studies, PCa incidence is a direct reflection of the rate at which high-risk groups screen for the disease [ 4 , 9 ]. In Europe, early screening was attributed to a 20% reduction in PCa mortality rate [ 10 ]. Although there is evidence suggesting a reduction in PCa mortality due to early screening, a United States (US) study did not highlight a reduction in mortality [ 11 ]. The prostate-specific antigen (PSA) test and the digital rectal examination (DRE) are useful screening tools, although initial controversies were surrounding the use of these tools [ 12 ]. Because of overlap in PSA levels in men with prostatitis, benign prostatic hyperplasia, and PCa, it was assumed that PCa cannot be screened using the PSA test [ 13 ]. Catalona et al. demonstrated that PSA could be utilized as a screening tool for PCa, and it has widely been adopted [ 14 ]. DRE is the only procedure whereby physicians can examine part of the prostate gland [ 15 ]. The findings are only based on the physician impression, hence poor inter-rater reliability and also a limitation to the palpable region of the prostate gland [ 15 ]. However, DRE sometimes detects PCa in men with PSA, 4.0 ng/mL [ 16 ]. Regardless of the controversial nature of screening and the potential for early screening to reduce mortality, studies support the need to encourage screening [ 4 , 12 ].
Women have essential characteristics that make them better managers of family health as compared to men. Therefore, it is not surprising that there is evidence positioning women as individuals who make adequate observations about the health of their partners [ 9 , 17 ]. In promoting the early detection of PCa, women have been documented to observe the slightest symptoms presented by their partners and push them to seek medical attention [ 9 , 18 ]. In a study conducted by Blanchard et al., it was recommended that efforts must be made to actively involve women in improving the timely detection of PCa through the closure of knowledge gaps [ 19 ].
Also, men admit seeking out their wives’ opinions as sources of health information [ 20 ]. In the context of the early detection of PCa, women can play various roles such as information seekers, advocates, health advisors, and support persons [ 21 ]. Therefore, there is the need to gather current evidence about women’s knowledge of PCa as the findings will be vital in equipping women to contribute towards the early detection of the disease.
In light of the availability of limited evidence addressing the awareness of women on prostate cancer, this review will seek to combine quantitative and qualitative data to increase the validity of findings through data triangulation as recommended by Caruth and supported by Lizarondo et al. [ 22 , 23 ]. Thus, this review seeks to map out current evidence regarding women’s awareness of PCa under the scopes of (1) signs and symptoms, (2) risk factors and causes, and (3) screening guidelines.
Review question
Do women have adequate knowledge about prostate cancer?
Methodology
The Joanna Briggs Institute (JBI) reviewer’s manual for the conduct of mixed-methods critical appraisal and synthesis formed the backbone of the study [ 23 ]. With guidance from the JBI manual, a protocol was developed to guide the review process according to the convergent segregated approach [ 23 ]. The respective DOIs of the review protocol and review, registered with the Open Science Framework (OSF), are https://doi.org/10.17605/OSF.IO/EYHF2 and https://doi.org/10.17605/OSF.IO/BR456 . The review protocol is readily available to the scientific community [ 24 ].
Inclusion criteria
The following were grounds for the inclusion of studies:
Studies that were conducted among women aged 18 years and above.
Studies that were conducted among women of all racial backgrounds.
Studies published from January 1999 to December 2019.
Studies that were conducted among women of all geographical locations.
Studies of all research designs.
Studies that were conducted to investigate the knowledge of women on the signs and symptoms of prostate cancer as highlighted in the review protocol.
Studies that were conducted to investigate the knowledge of women on the causes and risk factors of prostate cancer as highlighted in the review protocol.
Studies that were conducted to investigate the knowledge of women on the screening recommendations of prostate cancer as highlighted in the review protocol.
Studies that were published in the English language.
Studies with abstract and full text available.
Exclusion criteria
The following were grounds for the exclusion of studies:
Studies that were published before January 1999 or after December 2019.
Studies that were not published in the English language.
Studies that include women below the age of 18 years.
Studies in which the age of included women cannot be established.
Studies that did not indicate the number/percentage of included women.
Studies that exclusively included men without any women component (18 years and above).
Studies conducted among women who were previously given education on prostate cancer.
Studies that exclusively involved lesbian, gay, bisexual, transsexual/transgender, and queer/questioning (LGBTQ) participants.
Studies that exclusively included healthcare professionals.
Studies that exclusively involved healthcare and college/university students.
Studies that do not include the outcome of interest.
Book chapters.
Reviews and overviews.
Abstracts and conference papers.
Dissertations and thesis.
Commentaries and letters to editors.
Studies published without abstracts.
Information sources and search strategy
An initial explorative search in PubMed founded search terms in preparation for comprehensive electronic search. The selected search terms, applied as MeSH terms, were combined with Boolean operators for a comprehensive electronic search in MEDLINE (EBSCOhost), CINAHL (EBSCOhost), PsycINFO (EBSCOhost), Web of Science, and EMBASE (Ovid) as “(prostate cancer ) AND (awareness OR knowledge) AND (signs OR symptoms) AND (risk factors OR causes) AND (screening) AND (women)”. The search strategy (Additional file 1 ), so developed, was utilized by the first (EW) and second (KBM) reviewers to independently conduct a literature search as outlined in the review protocol e24].
Selection of studies
The first and second reviewers, being guided by the developed review protocol, singularly screened and compared the titles and abstracts of the literature search outcomes to a developed standard (the inclusion and exclusion criteria). Studies that successfully passed the initial stage of screening were subjected to the independent full-text reading by EW and KBM before consideration for data extraction. Lastly, hand-searching and snowballing on references of selected articles were done to find eligible studies in the grey area. There were no disagreements between EW and KBM. Hence, the third reviewer (ABBM) assessed the studies before data extraction was conducted by the lead author according to the JBI data extraction tools outlined in the review protocol [ 24 ]. The characteristic of studies that successfully went through the data extraction, the key findings that were extracted, and a summary of the study selection process are detailed respectively (Tables 1 and 2 and Fig. 1 ).
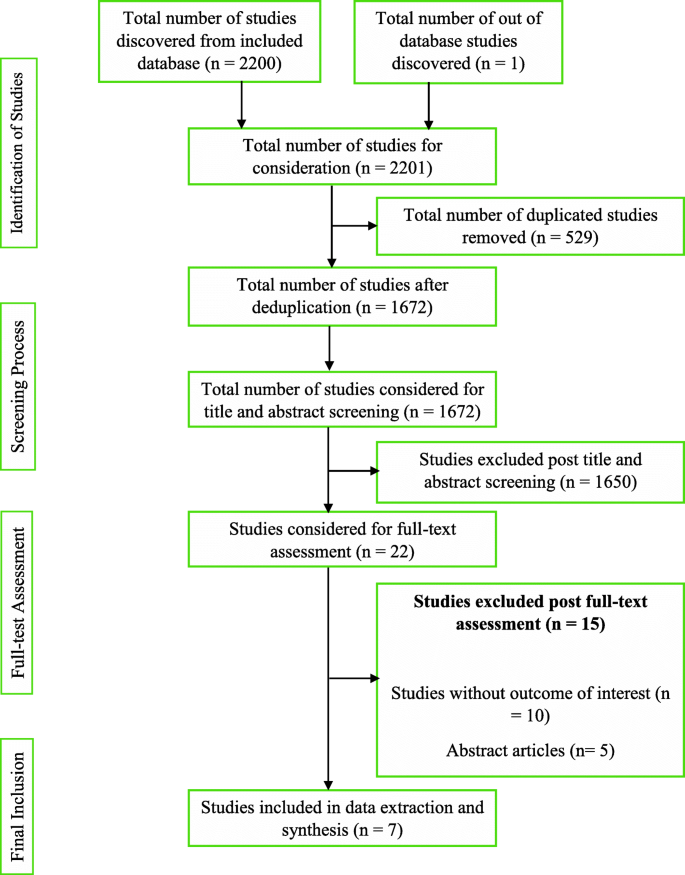
Summary of study selection process
Quality assessment
As described in the review protocol [ 24 ], the methodological quality assessment tool (Additional file 2 ) was adopted and modified for this review due to the similarities this review shares with the study conducted by Mensah et al. [ 30 ]. The tool appraised the studies’ quality based on the study sample representativeness, response rate, reliability, and validity of the data collection tool. The tool was modified to suit the results from the included studies. A score was calculated, and the quality of the studies was classified as weak (0 to 33.9%), moderate (34 to 66.9%), or strong (67 to 100%). Eligible records were subjected to independent quality assessment by EW and KBM. Methodological quality outcomes were not grounds for exclusion.
Synthesis and integration of findings
The review findings were subjected to the convergent segregated approach to synthesis and integration according to the developed review protocol [ 24 ]. A narrative synthesis was separately performed for qualitative and quantitative findings. The heterogeneous nature of the review findings did not support the conduct of a meta-analysis. The results were finally integrated.
Conducting the review, according to the developed protocol, yielded 2200 study results. A detailed citation screening led to an additional study, which increased the total number of studies to 2201. Regarding the summary of the study selection process (Fig. 1 ), 1672 studies were obtained after 529 duplicates were removed from the pool of data. Post-titles and abstract review excluded 1650 studies leaving 22 studies. The 22 studies were further reduced to 7 after a full-text reading resulted in the exclusion of 15 studies.
Characteristics of included studies
The data extracted from the seven (7) studies are detailed (Table 1 ). The publication years ranged from 2003 to 2018 with 5 studies having been conducted in the USA. One of the studies was a multicenter study that involved multinationals [ 28 ]. The study with the highest female participants (4040 women) was conducted in Spain [ 26 ]. Webb et al. recruited the lowest sample size, 14 women [ 29 ]. A total of 5634 women were involved in the 7 studies. Two studies were solely conducted in women, three included other diseases, and two did not disclose study duration.
Quality of included studies
According to the scoring scheme of the quality assessment tool (Additional file 2 ), two studies [ 26 , 29 ] were evaluated as moderate quality whilst five studies were evaluated as strong quality. None of the studies was excluded based on methodological quality assessment outcomes. There was no disagreement between EW and KBM.
Review findings
Study findings, presented in Table 2 , were heterogeneous. Quantitative studies indicate that women knew about the existence of PCa. In exploring qualitative evidence, women exhibited knowledge of PCa. Therefore, both arms of the review are supportive of each other.
Women had moderate knowledge about the signs and symptoms of PCa drawing from quantitative findings. Women knew about the asymptomatic nature of the early stages of PCa. They also moderately knew urinary symptoms such as urinary frequency, difficulty in urinating, and dysuria. Qualitative studies indicate that women were aware prostate cancer patients, usually in advanced stages, could present with signs and symptoms such as urinary frequency, difficulty in urinating, glandular enlargement of the prostate, and erectile dysfunction. Hence, quantitative and qualitative findings revealed that women moderately knew the urinary symptoms of PCa.
Quantitative studies indicate an average score of women on knowledge of risk factors of PCa. Risk factors women knew were increasing age, presence of a first-degree relative, being genetically linked to Africa, and excessive truncal obesity. Qualitative evidence recognized all risk factors documented by the quantitative findings except truncal obesity. Also, identified risk factors included poor diet, inadequate exercise, stressful lifestyle, poor screening habits, cigarette smoking, and poor access to quality healthcare. Women wrongly reported sexual orientation and frequent sexual activity as risk factors. Therefore, qualitative findings confirm the quantitative claim that women have shared knowledge about the risk factors of PCa.
Quantitative studies indicate that women had poor knowledge about PCa screening guidelines, appropriate screening samples, and tools. Although it was reported that women knew about PSA and DRE, the proportions of women who had correct responses to screening knowledge items were not appreciable. Women poorly recognized urine as a screening sample, PSA as an exclusive diagnostic tool (where only 17.5% answered correctly), and failed to identify more than one screening tool (between 41 and 71% of women failed). Qualitative studies respectively reported PSA and blood as a screening tool and sample. Colonoscopy was wrongly reported as a PCa screening tool. Conclusively, both arms of the review reported women knew about PSA and had poor knowledge about PCa screening.
The heterogeneity of the study findings warranted the synthesis as a narrative [ 23 , 31 ]. The convergent segregated approach was employed according to the recommendation of the JBI reviewer’s manual [ 23 ].
Generally, from the quantitative evidence, women knew about prostate cancer [ 19 , 25 , 27 , 28 ]. The knowledge of women was found to have increased with educational and financial status [ 19 ], and disease familiarity [ 19 , 25 ]. The awareness of women about the existence of PCa increased when the disease was mentioned compared to an initial request for women to list cancers [ 28 ]. Qualitative evidence showed that women were aware of PCa [ 18 , 27 ]. They appreciated and specifically requested for PCa education partly because they could not tell the location of the prostate gland [ 18 ]. Thus, quantitative and qualitative evidence indicates that women know about PCa. Women’s awareness could be due to their role in family health management and the possible health-seeking behavior of educated and financially strong women. As persons are faced with the experiences of a health condition, they will seek to make sense of this illness by acquiring knowledge [ 32 ], experiences, and beliefs; hence, this theory might explain the improved awareness of women who were familiar with the disease.
Most of the quantitative studies indicate that women are aware of the asymptomatic nature of early-stage PCa [ 19 , 25 , 27 ]. Symptoms that women had a fair knowledge about included urinary frequency, difficulty in urinating, and dysuria [ 25 ]. Findings from one of the qualitative studies indicate that women fairly recognized urinary frequency, difficulty in urinating, glandular enlargement of the prostate, and erectile dysfunction as signs and symptoms of PCa [ 18 ]. Being familiar with the disease may explain the awareness of women of the urinary symptoms associated with PCa.
According to Okoro and colleagues’ quantitative study, although knowledge of PCa was not adequate, women knew associated risk factors such as being a first-degree relative, being a man of African descent, and excessive truncal obesity [ 27 ]. Blanchard et al. also documented women’s recognition of increasing age as a PCa risk factor [ 19 ]. One of the qualitative studies indicates women knew increasing age could increase a man’s chance for PCa development [ 18 , 29 ]. Other causes and risk factors women identified included poor diet, inadequate exercise, stressful lifestyle, family history of the disease, being of African descent, poor screening habits, cigarette smoking, and poor access to quality healthcare [ 18 ]. Erroneously, one study reported that women perceived sexual orientation and frequent sexual activity as risk factors [ 18 ]. Both quantitative and qualitative findings documented women knew increasing age, family history, and African descent as PCa risk factors.
Quantitatively, women’s responses to queries about PCa screening were poor [ 25 , 28 ]. Some women were unable to recognize at least a PCa screening tool whilst others mistakenly recognized urine as a suitable sample for PCa screening [ 28 ]. According to Okoro et al., the majority of women exclusively tagged PSA elevation as a basis for PCa diagnosis [ 27 ]. This, therefore, calls for extensive education because benign prostatic hyperplasia, prostatitis, and PCa usually present with elevated PSA [ 13 ]. Evidence from qualitative findings indicated women knew physical examination must augment blood analysis [ 29 ]. Also, women mentioned PSA and colonoscopy as screening tools [ 18 ]. The results from included qualitative studies confirmed that women had poor knowledge about PCa screening. The mention of colonoscopy as a screening tool further supports a lack of adequate knowledge about PCa screening.
This critical appraisal and synthesis revealed over the 20 years of study search, only four studies out of the seven included studies investigated all the outcomes of interest. Two studies did not investigate women’s awareness of the signs and symptoms [ 26 , 29 ] and the causes and risk factors [ 25 , 26 ] of PCa. Therefore, although quantitative and qualitative findings were supportive of each other, studies investigating the causes and risk factors, as well as the signs and symptoms of PCa, were lacking.
Recommendations for practice
From the review findings, it is recommended that PCa control programs should also focus on educating women. Clinicians and public health practitioners should include women in prostate cancer health promotion. Women should be encouraged to attend PCa clinics with their male significant others suffering from the disease, and the effect of this strategy in reducing PCa mortality rate must be investigated.
Recommendations for research
Further studies are recommended to investigate the knowledge of women living in low- and middle-income countries (LMIC) about PCa. Such studies should focus extensively on the knowledge of women on PCa screening. Also, it is recommended for research to develop and pilot a PCa educational intervention model, applicable to women to reduce the burden of the disease. This tool should be culturally specific for easy acceptance and recognition. Also, current evidence on the willingness of women to offer social support to men with PCa should be investigated.
Study limitations
The various restrictions that were imposed on the literature search included a search range from January 1999 to December 2019, a search into only 5 databases, and the outright exclusion of non-English publications. These constitute selection bias. Therefore, some important studies could have been left out of the review.
Although five (5) out of the seven (7) included studies explicitly indicated recruiting participants of African backgrounds, none of the studies were conducted in Africa. Hence, the global generalizability of the review findings, to most importantly cover low and middle-income countries, cannot be documented.
The exclusion of studies conducted in women who received education on prostate cancer, healthcare professionals, healthcare students, and college/university students, and further exclusion of studies that involved (LGBTQ) participants further constitute selection bias.
It is imperative to note that the various limitations, in connection to the included studies, documented in Table 2 have an effect on this review and, as such, could be considered as potential limitations.
Availability of data and materials
Data and other pieces of information are available at https://doi.org/10.17605/OSF.IO/BR456
Abbreviations
Centers for disease control and prevention
Digital rectal examination
Global cancer incidence, mortality and prevalence
Joanna briggs institute
Lesbian, gay, bisexual, transsexual/transgender, and queer/questioning
Open science framework
Low- and middle-income countries
- Prostate cancer
Prostate-specific antigen
Sub-Saharan Africa
United States
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492 .
Article PubMed Google Scholar
James LJ, Wong G, Craig JC, Hanson CS, Ju A, Howard K, et al. Men’s perspectives of prostate cancer screening: a systematic review of qualitative studies. PloS One. 2017;12(11):e0188258. https://doi.org/10.1371/journal.pone.0188258 .
Article CAS PubMed PubMed Central Google Scholar
GLOBOCAN. GLOBOCAN 2008: Ghana Fact Sheets. 2018. Available from: file:///C:/Users/user-pc/Downloads/288-ghana-fact-sheets.pdf.
Yeboah-Asiamah B, Yirenya-Tawiah D, Baafi D, Ackumey M. Perceptions and knowledge about prostate cancer and attitudes towards prostate cancer screening among male teachers in the Sunyani Municipality, Ghana. Afr J Urol. 2017;23(4):184-91.
Rebbeck TR, Devesa SS, Chang B-L, Bunker CH, Cheng I, Cooney K, et al. Global patterns of prostate cancer incidence, aggressiveness, and mortality in men of African descent. Prostate Cancer. 2013;2013:1–12. https://doi.org/10.1155/2013/560857 .
Article Google Scholar
Mofolo N, Betshu O, Kenna O, Koroma S, Lebeko T, Claassen FM, et al. Knowledge of prostate cancer among males attending a urology clinic, a South African study. SpringerPlus. 2015;4(1):67. https://doi.org/10.1186/s40064-015-0824-y .
Article PubMed PubMed Central Google Scholar
Jemal A, Bray F, Forman D, O'Brien M, Ferlay J, Center M, et al. Cancer burden in Africa and opportunities for prevention. Cancer. 2012;118(18):4372–84. https://doi.org/10.1002/cncr.27410 .
Dimah KP, Dimah A. Prostate cancer among African American men: a review of empirical literature. Journal of African American Studies. 2003;7(1):27–46. https://doi.org/10.1007/s12111-003-1001-x .
Rashid P, Denham J, Madjar I. Do women have a role in early detection of prostate cancer? Lessons from a qualitative study. Aust Fam Phys. 2007;36(5):375.
Google Scholar
Schröder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V, et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med. 2009;360(13):1320–8. https://doi.org/10.1056/NEJMoa0810084 .
Andriole GL, Crawford ED, Grubb RL III, Buys SS, Chia D, Church TR, et al. Mortality results from a randomized prostate-cancer screening trial. N Engl J Med. 2009;360(13):1310–9. https://doi.org/10.1056/NEJMoa0810696 .
Nakandi H, Kirabo M, Semugabo C, Kittengo A, Kitayimbwa P, Kalungi S, et al. Knowledge, attitudes and practices of Ugandan men regarding prostate cancer. Afr J Urol. 2013;19(4):165–70. https://doi.org/10.1016/j.afju.2013.08.001 .
Catalona WJ. Prostate cancer screening. Med Clin. 2018;102(2):199–214. https://doi.org/10.1016/j.mcna.2017.11.001 .
Catalona WJ, Smith DS, Ratliff TL, Dodds KM, Coplen DE, Yuan JJ, et al. Measurement of prostate-specific antigen in serum as a screening test for prostate cancer. N Engl J Med. 1991;324(17):1156–61. https://doi.org/10.1056/NEJM199104253241702 .
Article CAS PubMed Google Scholar
Wilbur J. Prostate cancer screening: the continuing controversy. Am Fam Phys. 2008;78(12):1377–84.
Federman DG, Pitkin P, Carbone V, Concato J, Kravetz JD. Screening for prostate cancer: are digital rectal examinations being performed? Hosp Pract. 2014;42(2):103–7. https://doi.org/10.3810/hp.2014.04.1108 .
Karim R, Lindberg L, Wamala S, Emmelin M. Men’s perceptions of women’s participation in development initiatives in rural Bangladesh. Am J Mens Health. 2018;12(2):398–410. https://doi.org/10.1177/1557988317735394 .
Owens OL, Friedman DB, Hebert J. Commentary: Building an evidence base for promoting informed prostate cancer screening decisions: an overview of a cancer prevention and control program. Ethn Dis. 2017;27(1):55–62. https://doi.org/10.18865/ed.27.1.55 .
Blanchard K, Proverbs-Singh T, Katner A, Lifsey D, Pollard S, Rayford W. Knowledge, attitudes and beliefs of women about the importance of prostate cancer screening. J Natl Med Assoc. 2005;97(10):1378–85.
PubMed PubMed Central Google Scholar
Taylor KL, Turner RO, Davis JL III, Johnson L, Schwartz MD, Kerner J, et al. Improving knowledge of the prostate cancer screening dilemma among African American men: an academic-community partnership in Washington, DC. Public Health Rep. 2016;116(6):590–8.
Miller SM, Roussi P, Scarpato J, Wen KY, Zhu F, Roy G. Randomized trial of print messaging: the role of the partner and monitoring style in promoting provider discussions about prostate cancer screening among African American men. Psychooncol. 2014;23(4):404–11. https://doi.org/10.1002/pon.3437 .
Caruth GD. Demystifying mixed methods research design: a review of the literature. Mevlana Int J Educ. 2013;3(2):112–22. https://doi.org/10.13054/mije.13.35.3.2 .
Lizarondo L, Stern C, Carrier J, Godfrey C, Rieger K, Salmond S, et al. Chapter 8: Mixed methods systematic reviews.: The Joanna Briggs Institute; 2017 [Available from: https://wiki.joannabriggs.org/display/MANUAL/Chapter+8%3A+Mixed+methods+systematic+reviews .
Wiafe E, Mensah KB, Mensah ABB, Bangalee V, Oosthuizen F. The awareness of women on prostate cancer: a mixed-methods systematic review protocol. Syst Rev. 2020;9(1):1–6.
Brown N, Naman P, Homel P, Fraser-White M, Clare R, Browne R. Assessment of preventive health knowledge and behaviors of African-American and Afro-Caribbean women in urban settings. J Natl Med Assoc. 2006;98(10):1644–51.
Carrasco-Garrido P, Hernandez-Barrera V, Lopez de Andres A, Jimenez-Trujillo I, Gallardo Pino C, Jimenez-Garcıa R. Awareness and uptake of colorectal, breast, cervical and prostate cancer screening tests in Spain. Eur J Public Health. 2014;24(2):264–70. https://doi.org/10.1093/eurpub/ckt089 .
Okoro ON, Rutherford CA, Witherspoon SF. Leveraging the family influence of women in prostate cancer efforts targeting African American Men. J Racial Ethnic Health Disparities. 2018;5(4):820–30. https://doi.org/10.1007/s40615-017-0427-0 .
Article CAS Google Scholar
Schulman CC, Kirby R, Fitzpatrick JM. Awareness of prostate cancer among the general public: findings of an independent international survey. European Urology. 2003;44(3):294–302. https://doi.org/10.1016/S0302-2838(03)00200-8 .
Webb CR, Kronheim L, Williams JE, Hartman TJ. An evaluation of the knowledge, attitudes, and beliefs of African-American men and their female significant others regarding prostate cancer screening. Ethn Dis. 2006;16(1):234–8.
PubMed Google Scholar
Mensah KB, Oosthuizen F, Bonsu AB. Cancer awareness among community pharmacist: a systematic review. BMC Cancer. 2018;18(1):299. https://doi.org/10.1186/s12885-018-4195-y .
Lockwood C, Porritt K, Munn Z, Rittenmeyer L, Salmond S, Bjerrum M, et al. Chapter 2: Systematic reviews of qualitative evidence: the Joanna Briggs Institute; 2017 [Available from: https://wiki.joannabriggs.org/display/MANUAL/Chapter+2%3A+Systematic+reviews+of+qualitative+evidence .
Petrie K, Weinman J. Why illness perceptions matter. Clin Med. 2006;6(6):536–9. https://doi.org/10.7861/clinmedicine.6-6-536 .
Download references
Acknowledgements
The review team gives recognition to Dr. Richard Ofori-Asenso.
Author information
Authors and affiliations.
University of KwaZulu-Natal, Durban, South Africa
Ebenezer Wiafe, Kofi Boamah Mensah, Varsha Bangalee & Frasia Oosthuizen
Ho Teaching Hospital, Ho, Ghana
Ebenezer Wiafe
Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
Kofi Boamah Mensah & Adwoa Bemah Boamah Mensah
You can also search for this author in PubMed Google Scholar
Contributions
EW is credited with the conception of the review, the coordination of the systematic review, the development of the search strategy, the search and selection of studies to be included in the review, the extraction and management of quantitative and qualitative data, the assessment of methodological quality, the filtering of all reference materials, the integration and interpretation of the data, and the drafting of the manuscript, and is the principal reviewer. KBM is credited with the conception of the review, the review of the search strategy, the search and selection of studies to be included in the review, the extraction and management of quantitative and qualitative data, the assessment of methodological quality, the integration and interpretation of the data, and the review of the manuscript. ABBM is credited with the review of the search strategy, the assessment of the studies before data extraction, and the review of the manuscript. VB is credited with the review of the manuscript, the coordination of the systematic review, and the as co-supervisor of the review. FO is credited with the conception of the review, the review of the manuscript, and the overall supervision of the review. All authors have reviewed and accepted the final manuscript of the review for publication. The authors read and approved the final manuscript.
Corresponding author
Correspondence to Ebenezer Wiafe .
Ethics declarations
Ethics approval and consent to participate.
Ethical permission was not required since the study did not involve the enrollment of humans or animals as study subjects.
Consent for publication
Competing interests, additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:..
Proposed search strategy using Medline via EBSCOhost
Additional file 2:.
Assessment of methodological quality of included studies
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wiafe, E., Mensah, K.B., Mensah, A.B.B. et al. Knowledge of prostate cancer presentation, etiology, and screening practices among women: a mixed-methods systematic review. Syst Rev 10 , 138 (2021). https://doi.org/10.1186/s13643-021-01695-5
Download citation
Received : 01 December 2020
Accepted : 29 April 2021
Published : 06 May 2021
DOI : https://doi.org/10.1186/s13643-021-01695-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Signs and symptoms
- Causes and risk factors
- Screening recommendations
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Men’s perspectives of prostate cancer screening: A systematic review of qualitative studies
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Sydney School of Public Health, The University of Sydney, Sydney, Australia, Centre for Kidney Research, The Children’s Hospital at Westmead, Westmead, Australia
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing – review & editing
Affiliations Sydney School of Public Health, The University of Sydney, Sydney, Australia, Centre for Kidney Research, The Children’s Hospital at Westmead, Westmead, Australia, Centre for Transplant and Renal Research, Westmead Hospital, Westmead, Australia
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Writing – review & editing
Roles Conceptualization, Data curation, Formal analysis, Methodology, Software, Writing – review & editing
Roles Conceptualization, Data curation, Formal analysis, Methodology, Writing – review & editing
Affiliation Centre for Kidney Research, The Children’s Hospital at Westmead, Westmead, Australia
Affiliations Department of General Practice, Westmead Clinical School, The University of Sydney, Sydney, Australia, The George Institute for Global Health, Sydney, Australia
Affiliation Department of Urology, Westmead Hospital, Westmead, Australia
Roles Conceptualization, Data curation, Formal analysis, Methodology, Software, Supervision, Writing – review & editing
- Laura J. James,
- Germaine Wong,
- Jonathan C. Craig,
- Camilla S. Hanson,
- Angela Ju,
- Kirsten Howard,
- Tim Usherwood,
- Howard Lau,
- Allison Tong

- Published: November 28, 2017
- https://doi.org/10.1371/journal.pone.0188258
- Reader Comments
Prostate cancer is the most commonly diagnosed non-skin cancer in men. Screening for prostate cancer is widely accepted; however concerns regarding the harms outweighing the benefits of screening exist. Although patient’s play a pivotal role in the decision making process, men may not be aware of the controversies regarding prostate cancer screening. Therefore we aimed to describe men’s attitudes, beliefs and experiences of prostate cancer screening.
Systematic review and thematic synthesis of qualitative studies on men’s perspectives of prostate cancer screening. Electronic databases and reference lists were searched to October 2016.
Sixty studies involving 3,029 men aged from 18–89 years, who had been screened for prostate cancer by Prostate Specific Antigen (PSA) or Digital Rectal Examination (DRE) and not screened, across eight countries were included. Five themes were identified: Social prompting (trusting professional opinion, motivation from family and friends, proximity and prominence of cancer); gaining decisional confidence (overcoming fears, survival imperative, peace of mind, mental preparation, prioritising wellbeing); preserving masculinity (bodily invasion, losing sexuality, threatening manhood, medical avoidance); avoiding the unknown and uncertainties (taboo of cancer-related death, lacking tangible cause, physiological and symptomatic obscurity, ambiguity of the procedure, confusing controversies); and prohibitive costs.
Conclusions
Men are willing to participate in prostate cancer screening to prevent cancer and gain reassurance about their health, particularly when supported or prompted by their social networks or healthcare providers. However, to do so they needed to mentally overcome fears of losing their masculinity and accept the intrusiveness of screening, the ambiguities about the necessity and the potential for substantial costs. Addressing the concerns and priorities of men may facilitate informed decisions about prostate cancer screening and improve patient satisfaction and outcomes.
Citation: James LJ, Wong G, Craig JC, Hanson CS, Ju A, Howard K, et al. (2017) Men’s perspectives of prostate cancer screening: A systematic review of qualitative studies. PLoS ONE 12(11): e0188258. https://doi.org/10.1371/journal.pone.0188258
Editor: Jo Waller, UCL, UNITED KINGDOM
Received: December 28, 2016; Accepted: November 1, 2017; Published: November 28, 2017
Copyright: © 2017 James et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: LJJ and JCC are supported by the National Health and Medical Research Council Program Grant (APP1092957). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Prostate cancer is the most commonly diagnosed non-skin cancer in men and accounts for 48 deaths per 100,000 men per year in the UK.[ 1 ] One in seven men in Australia and the UK will develop prostate cancer by age 75 years.[ 2 , 3 ] The overall age-standardised incidence is 182 per 100,000 men per year in the UK,[ 4 ] and 163 and 129 per 100,000 men per year in Australia and US respectively.[ 5 , 6 ]
Screening for prostate cancer using prostate-specific antigen (PSA) is widely used in the general population, contributing to a threefold increase in the incidence of diagnosed prostate cancer.[ 7 ] However, screening remains controversial, in part due to conflicting results from recent large randomised controlled trials. One large-scale trial, conducted in the US, found no difference in prostate cancer mortality between the screened and control group after 13 years,[ 8 ] whereas another European trial, with a similar follow up, demonstrated a 21% relative reduction in the risk of prostate cancer-specific death.[ 9 ]
More recently, concerns about overdiagnosis have also been raised.[ 10 – 12 ] Early detection through screening can lead to overdiagnosis, which consequently may require further unnecessary investigations, including prostatectomy and radiation therapy.[ 10 ] It remains uncertain whether screening confers appreciable survival benefits, and treatment of screen detected disease can lead to adverse events including urinary incontinence, erectile dysfunction, bowel problems, and unwarranted anxiety.[ 10 , 13 ] As a result, current guidelines for PSA testing vary worldwide.
The conflicting trial results, potential harms associated with the screening algorithm, and the inconsistent recommendations regarding PSA testing in clinical practice guidelines,[ 2 , 11 , 14 – 16 ] highlights the critical role of patient preference. Shared informed decision making is widely advocated to ensure men can understand and weigh the benefits and harms of prostate cancer screening.[ 2 , 11 , 12 , 14 , 16 – 18 ] However, men may not be aware of the potential risks of treating screen-detected prostate cancer.[ 19 – 21 ] Although a clinician’s recommendation to screen is associated with higher uptake of prostate cancer screening[ 22 – 25 ], embarrassment,[ 26 – 29 ] perceived low risk,[ 28 , 30 ] and fear of cancer [ 28 , 31 , 32 ] explain men’s decisions not to undergo screening. We aimed to describe the beliefs, attitudes and experiences of men on prostate cancer screening. A broader range of insights across populations and healthcare settings will provide a comprehensive understanding of men’s perspectives on prostate cancer screening, and may also enable comparisons across demographic characteristics. This may inform strategies for informed, shared-decision making that explicitly considers their values and preferences.
This study follows the Enhancing Transparency of Reporting the Synthesis of Qualitative research (ENTREQ) framework.[ 33 ] ENTREQ covers five main domains for reporting the systematic review of primary qualitative studies: introduction, methods and methodology, literature search and selection, appraisal, and synthesis of findings.
Selection criteria
We included qualitative studies that used interviews or focus groups which elicited perspectives of adult men, of any age, on prostate cancer screening. To obtain a broad range of perspectives on attitudes to screening, studies of men with no previous history of screening or had been screened for prostate cancer using PSA or digital rectal examination (DRE) were included. We excluded studies that only included men diagnosed with prostate cancer, or that included health professionals. Studies published in non-English language were excluded to prevent cultural and linguistic bias in translations. We also excluded studies if they used structured surveys and reported only quantitative data, or were epidemiological studies, editorials or reviews.
Data sources and searches
We searched MEDLINE, Embase, PsycINFO and Cumulative Index to Nursing and Allied Health Literature (CINAHL) from inception to October 2016 ( S1 Text ), as well as Google Scholar and the reference lists of relevant studies and reviews. Author (LJJ) screened titles and abstracts of search results and excluded those that did not meet the selection criteria. Full texts of the remaining articles were assessed for study eligibility by LJJ.
Quality of reporting assessment
Three authors (LJJ/CSH/AJ) independently evaluated the transparency of reporting of each included study using the Consolidated Criteria for Reporting Qualitative Research (COREQ) framework.[ 34 ] The COREQ items addresses the research team, relationship with participants, participant selection, setting, data collection, data analysis and reporting. Discrepancies were discussed and resolved among the reviewers.
We synthesised the results from all included studies using thematic synthesis, as described by Thomas and Harden.[ 35 ] All text and quotations included within the “Results” or “Discussion/Conclusion” section from the included studies were imported into HyperRESEARCH (ResearchWare, INC. 2015, version 3.7.1) software for qualitative data management. LJJ read each study, conducted line-by-line coding of the findings, and inductively identified concepts relating to prostate cancer screening perspectives and grouped similar concepts into themes and subthemes. Three authors (LJJ, CSH, AJ) read the papers independently to ensure that the range and depth of data reported in the included studies were included in the analytical framework. Conceptual links among these themes were identified and mapped into a thematic schema.
Literature search
Of the 2,752 articles retrieved, 68 eligible studies involving 3,029 participants were identified ( Fig 1 ). The characteristics of the studies are provided in Table 1 and S1 Table . Forty studies (59%) included men with and without a history of screening. Nine (13%) studies included men who had not been screened, and 4 (6%) studies included men who had been previously screened. Fifteen (22%) studies did not report participant’s history of screening. Both methods for screening, PSA or DRE, were used, however the number of men that used either method was not reported in most studies. The studies were conducted in nine countries, including the United States (49 [72%]; of which 26 (38%) only included African American men), United Kingdom (7 [10%]), Australia (6 [9%]), Barbados, Belgium, Canada, Germany, Nigeria and Uganda (1 study each).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0188258.g001
https://doi.org/10.1371/journal.pone.0188258.t001
Comprehensiveness of reporting of included studies
The comprehensiveness of reporting was variable, with studies reporting 7 to 23 of the 25 items in the adapted COREQ checklist ( Table 2 ). The participant selection strategy was described in 58 (85%) studies, and data saturation was reported in 28 (41%) studies. The use of software to facilitate data analysis was reported in 41 (60%) studies, and 52 (76%) reported on the use of researcher triangulation. Almost all studies (66 [97%]) provided participant quotations.
https://doi.org/10.1371/journal.pone.0188258.t002
We identified five themes on men’s perspectives on prostate cancer screening: social prompting, gaining decisional confidence, preserving masculinity, avoiding the unknown and uncertainties, and prohibitive costs. The respective subthemes are described below. Table 3 provides selected participant quotations from the included studies, and indicates the studies that contributed to each theme. A thematic schema to illustrate the conceptual links among themes is provided in Fig 2 .
https://doi.org/10.1371/journal.pone.0188258.g002
https://doi.org/10.1371/journal.pone.0188258.t003
Social prompting.
Trusting professional opinion –Some participants had “confidence in doctors” to initiate and make recommendations about prostate cancer screening.[ 19 , 27 , 28 , 38 , 47 , 49 , 52 , 54 , 59 , 60 , 78 , 81 , 83 , 91 , 93 ] Many felt overwhelmed by the complicated medical information and thus did not feel competent enough to “evaluate the pros and cons or the risks” on their own.[ 38 , 52 ] Having a strong relationship with their health care provider allowed participants to make this important health decision for them.[ 78 ]
Motivation from family and friends – Family and friends motivated men to be screened for prostate cancer.[ 40 , 41 , 47 , 55 – 57 , 71 , 72 , 79 , 83 , 91 , 92 , 99 ] Participants appreciated their spouses’ encouragement, their constant “nagging”[ 79 ] to pursue screening and “for sticking by”,[ 47 ] during the decision making and screening process. Having a family member who had prostate-related problems (e.g. benign prostatic hyperplasia) also prompted them to undergo screening, as they “wouldn’t have started checking”[ 69 ] otherwise.[ 65 , 69 , 83 , 91 , 98 ]
Proximity and prominence of cancer – Participants who had seen the devastating impact of cancer among their family or friends felt acutely aware of cancer, and were prompted to undergo prostate cancer screening.[ 21 , 42 , 47 , 51 , 60 , 65 , 66 , 69 , 75 , 83 , 85 , 91 , 100 ] The death of family members due to cancer and “seeing what [they] went through”[ 51 ] as well as understanding the potential of cancer “running in the family,”[ 66 ] caused participants to become proactive about cancer screening, including for prostate cancer. Some believed their family members had cancer detected “too late”.[ 75 ]
Gaining decisional confidence.
Overcoming fears – Preparing to screen for prostate cancer was described by participants as a “psychological game”[ 19 ] that required them to overcome the stigma surrounding the screening procedure.[ 19 , 27 , 55 , 61 , 81 , 82 ] Prostate cancer screening was initially perceived as “embarrassing,”[ 81 ] “uncomfortable,”[ 82 ] and “dreaded,”[ 61 ] which was later on accepted as “necessary,” [ 82 ] and “routine.”[ 61 ]
Survival imperative –Improving their chance of survival through early detection motivated men to undergo prostate cancer screening.[ 20 , 21 , 28 , 36 , 42 , 43 , 60 , 71 , 74 , 77 , 85 , 91 , 92 ] Early detection was perceived as imperative to prevent severe morbidity or mortality, so they could continue to live a “normal life.”[ 21 ] They believed that cancers detected early had a “higher chance”[ 20 ] of cure.
Peace of mind – The possibility of prostate cancer was often “constantly nagging at the back of their mind”[ 79 ] particularly for men with increased risk due to family history of the cancer. Some participants believed they had “nothing to lose”[ 36 ] by going ahead with the screening. By doing so, they felt reassured and their “mind was at ease.”[ 36 , 39 , 48 , 52 , 71 , 79 , 92 ] Prostate cancer screening provided “peace of mind for family and loved ones too.”[ 71 ]
Mental preparation – Preparing for the procedure of screening was psychologically confronting and overwhelming for men.[ 19 , 49 , 79 ] The fear of having an invasive procedure required men to be mentally prepared as they were hesitant to commit.[ 79 ] [ 19 , 79 ] After the test, many men felt “anxious”[ 49 ] awaiting the results and left with a “great void of uncertainty”[ 79 ] as they were terrified to receive a positive result.
Prioritising wellbeing – Men valued survival and family: “I want to live as long as I can and be around for my children and grandchildren.”[ 47 ] For those who had not experienced severe health problems, they “did not want to run the risk”[ 77 ] and instead “wanted to be preventive, instead of regretting”[ 77 ] their decision in the future. Some regarded prostate cancer screening as a “win-win situation”[ 36 ], and regardless of the outcome, they could “not go wrong.”[ 36 ] Some men strived to maintain a sense of control of their body, and were “curious”[ 54 ] and wanted to know “what is really going on in my body”[ 54 ], and thus were inclined to participate in prostate cancer screening.
Preserving masculinity.
Bodily invasion – Some men felt a loss of personal dignity after undergoing the invasive procedure of screening.[ 20 , 27 , 53 , 55 , 60 , 61 , 81 , 82 , 88 , 94 , 97 , 100 ] For men who had not previously been screened for prostate cancer they were fearful of the procedure and did not like the idea of a doctor “messing with me there.”[ 87 ] For men who had participated they felt the procedure was “violating”[ 97 ] and some “felt invaded,”[ 27 , 81 , 82 , 97 ] and therefore were unwilling to complete the screening again.[ 78 , 82 ] Some persevered through the unpleasantness of the procedure by focussing on the necessity–“if I need it I’ll get it done”.[ 82 ]
Losing sexuality – Men were fearful that consequences of screening may cause sexual dysfunction,[ 19 , 20 , 27 , 57 , 58 , 60 , 65 , 68 , 71 – 75 , 77 , 78 , 92 , 94 , 100 ] and this was a “major concern.”[ 19 ] Being unable to perform sexually would be “devastating.”[ 27 ] Prostate cancer and subsequent prostatectomy was seen as “taking the manhood away”[ 71 ] and thus men were reluctant to undergo screening. They wanted to avoid diagnosis of prostate cancer as they did “not want to end up impotent,”[ 77 ] which some had observed in other men who had been treated for prostate cancer.
Threatening manhood – Being diagnosed with prostate cancer was perceived to potentially jeopardise a man’s manhood or masculinity.[ 19 , 39 , 41 , 42 , 51 , 53 , 55 , 57 , 60 , 63 – 66 , 69 , 70 , 72 , 74 , 75 , 78 , 82 , 84 , 88 , 89 , 94 , 96 , 97 ] Their “macho man”[ 53 ] image would be compromised, as “being unhealthy is a sign of being unmanly.”[ 66 ] Some men were uneasy and reluctant to be screened as the DRE was perceived to have “homosexual implications.”[ 19 , 51 , 69 , 74 , 89 ] Some also feared being diagnosed with prostate cancer as they would have to relinquish their role as “the rock”[ 66 ] of their family.
Medical avoidance – Some participants were generally averse to interacting with the medical system, particularly if it was seen as unnecessary given the absence of symptoms or perceptible health problems.[ 19 – 21 , 27 , 28 , 37 , 42 , 45 , 53 , 55 , 63 , 64 , 69 , 72 , 86 , 88 , 89 , 92 ] They reasoned that “if it don’t hurt don’t fix it.”[ 20 ] Even after been advised by a doctor to undergo further tests or examinations they would “postpone and postpone”[ 28 ] as they refused to be seen as vulnerable and were terrified of potentially receiving bad news. Some men believed that it was “not socially acceptable”[ 69 ] to go to the doctor like women,[ 55 , 64 , 69 , 70 , 86 ] which they attributed to their macho mentality[ 21 , 63 , 72 ]–that they were “tough”[ 72 ] and “infallible.”[ 21 ]
Avoiding the unknown and uncertainties.
Taboo of cancer-related death – Fears of being potentially diagnosed with prostate cancer and dying caused men to ignore the matter.[ 19 , 20 , 28 , 36 , 37 , 39 , 41 , 42 , 54 , 56 , 62 , 63 , 77 – 79 , 88 , 92 , 96 , 99 , 100 ] In one study, African American men felt that “anything that a Black man thinks is gonna kill him, he ain’t gonna want to talk about”.[ 41 ] Cancer was considered to be “a death sentence,”[ 28 ] and men expressed that they would “rather not know”.[ 27 ] For men who had previous or ongoing health problems, they were particularly concerned that another diagnosis i.e. of prostate cancer would increase the burden of living with the disease to beyond what they could cope with.
Lacking tangible cause – The absence of signs and symptoms made it difficult for men to understand the value of screening.[ 20 , 36 , 43 , 50 , 58 , 62 , 64 , 69 , 74 , 84 – 86 , 89 , 98 ] Some felt they were healthy and were convinced that “if it’s not affecting me, why bother with it?”[ 86 ] as there was “nothing wrong…no pain or disease.”[ 50 ]
Physiological and symptomatic obscurity– Although participants indicated their awareness of prostate cancer, some did not know “what the gland’s there for, we don’t know what it does, so we don’t know what to do.”[ 44 ] One participant highlighted that he was “pretty ignorant“[ 46 ] as he “didn’t even know women didn’t get it.”[ 46 ] Some younger men felt there was no need to spend time and money for screening as prostate cancer was an “old man”[ 50 ] cancer. Further, participants had lack of awareness of the symptoms of prostate cancer.
Ambiguity of the procedure – Some men described having a vague understanding of the procedures of prostate cancer screening, which caused them to feel concerned and anxious about undergoing screening.[ 36 , 42 , 54 , 65 , 88 , 91 ] Screening was at times acted upon because they received instruction by their doctor, although they had little knowledge regarding the PSA testing.[ 91 ] Due to lack of knowledge and awareness, some men stated there was “too much confusion” and assumed that all prostate cancer screening was “invasive”[ 36 ] and “painful.”[ 88 ] However, some became aware that a blood test was available, and were relieved that they would not have to undergo a DRE.[ 36 ]
Confusing controversies – The controversies regarding the accuracy of prostate cancer screening caused some men to feel confused and uncertain.[ 21 , 36 , 38 , 46 , 52 , 62 , 65 , 67 , 69 , 83 , 92 , 95 ] They questioned “what’s the point of getting a test if it might not be reliable?”[ 62 ] For others, they found the procedure “not that reassuring,”[ 46 ] as there was still a chance they could have prostate cancer. Thus, decision making was complex as they had to “evaluate the pros and cons”[ 38 ] in the context of such uncertainties. Some men also disclosed that the potential risks involved in prostate cancer screening were not addressed by doctors, despite highlighting the benefits of the procedure. [ 93 ]
Prohibitive costs.
The cost of prostate cancer screening created difficulty for men seeking participation[ 19 , 20 , 27 , 40 , 54 , 60 , 64 , 80 , 89 , 90 ] as many were not “able to afford the doctors.”[ 40 ] However, concerns regarding costs were only identified among African American and African-Caribbean participants in the United States. In 14 studies involving African American men, men disclosed that they could not afford health insurance and therefore were unable to be screened for prostate cancer despite their increased risk.[ 19 , 20 , 27 , 39 , 40 , 54 , 62 , 64 , 71 , 73 , 76 , 80 , 87 , 89 ] African-Caribbean men also articulated that “health insurance is probably the biggest impediment”[ 60 ] for men to regularly partake in screening.
Our findings demonstrate that men’s expectations and values regarding prostate cancer screening reflects a complex decisional matrix. Active recommendation to screen from health care providers, persuasion from their close social networks, and exposure to personal experience of cancer supported men’s acceptance and willingness to undergo prostate cancer screening. Further, men believed that early detection could improve chances of survival, which was also a strong motivator to participate in screening. However, some men refused or delayed prostate cancer screening as risks such as erectile dysfunction were regarded as a threat to their masculinity and bodily dignity, Also, men were reluctant to contemplate mortality as it was too confronting (or perceived as irrelevant by younger men), or were anxious about the unknowns and uncertainties of the procedure and the potential distress if screened positive for prostate cancer.
Our review also highlights differences in men’s perspectives of prostate cancer screening by age, ethnicity and family history of prostate cancer. Some younger men felt they had less knowledge about the risk of prostate cancer, and assumed that screening was not relevant at their age as prostate cancer was thought to be more prevalent in older men. Although African American men have an increased risk of prostate cancer, they felt their knowledge of the disease was limited compared to other populations, and identified cost as a major barrier to screening. Many men who had a family history of prostate cancer were acutely aware of the consequences on health and quality life, and were thus motivated to participate in screening. However, we did not identify any clear differences by country.
The decision making process for prostate cancer screening align with the domains of the Integrated Behaviour Model, which has been commonly used to explain decision making in cancer screening.[ 102 , 103 ] The model theorises that intentions (founded by attitudes, subjective norms and perceived self-efficacy) are the predominant determinants of enacting behaviour; while ability, environmental constraints and habit directly enable or constrain the resulting action.[ 104 , 105 ] Thus, our findings demonstrate that men’s decision making for prostate cancer screening is influenced by knowledge obtained through support networks and other means, the personal impact of knowing someone who has suffered from cancer, and their motivation to maintain their wellbeing. However, the only environmental constraint identified in the review was the out-of-pocket costs of screening, which varied by jurisdiction.
Our findings are consistent with similar studies for other cancers. Receiving a direct recommendation from a health care provider to undergo screening has also been found to prompt and reinforce motivation for participation in bowel,[ 106 , 107 ] breast,[ 108 – 110 ] and cervical cancer screening.[ 111 , 112 ] Other facilitators of screening also include early detection and prevention of cancer,[ 109 , 112 , 113 ] peace of mind,[ 114 – 116 ] and being in control of own health.[ 113 , 114 ] Studies have also shown that patients are conscious of their own lack of awareness about the risk and harms of screening, which contributes to uncertainties in decision making.[ 117 – 119 ] In terms of barriers, concerns about invasion of privacy in screening have also been documented in the context of cervical cancer.[ 120 ] In prostate cancer screening, sexual impotence was identified as a major concern in our study. However in contrast, findings from a discrete choice experiment suggests that the risk of erectile dysfunction did not significantly influence men’s preferences for screening, and men were more willing to accept this potential harm to avoid prostate cancer related death.[ 121 ]
Our review involved a systematic and comprehensive literature search, and we synthesized 68 qualitative studies, with 3,029 participants from nine countries to develop a new analytical framework reflecting the complexities in decision-making about prostate cancer screening among men. We also conducted an independent assessment of the transparency of study reporting. However, there are some potential limitations. Although one author coded the studies, the preliminary findings and coding were discussed with multiple investigators who had read the papers, to enhance the analytical framework and to ensure that the full spectrum of perspectives reported in the primary studies were included in the final analysis. We excluded non-English articles to minimise cultural and linguistic misinterpretation. Also, we were unable to delineate differences between types of screening modality as these were not specified in most studies, and whether perspectives varied according to whether men had actually experienced screening.
The lack of understanding about the process and risk of screening, and the potential threat to masculinity as a consequence of further interventions if screened positive, compound the complexities of men’s decision-making about prostate cancer screening. This suggests the need for accessible and comprehensive information about the screening procedure, the potential benefits and harms of screening; particularly as shared decision making about prostate cancer screening is still not being widely implemented in primary healthcare settings.[ 122 ] Current guidelines for prostate cancer screening recommend against prostate cancer screening or suggest a shared decision making approach that address the benefits and harms for specific ages or high risk groups.[ 11 , 14 – 16 ] They also suggest consideration of men’s preferences and values; however they do not explicitly mention the values that are important to men which were disclosed in our review, and includes invasion of privacy, masculinity and impotence.
Decision aids may be beneficial for presenting population based evidence on benefits and harms of screening, but implementation can be challenging. Randomised controlled trials have shown that decision aids can improve informed decisions, communication between patients and health can providers, and therefore facilitate informed decision making.[ 123 – 125 ] Further, trials specific to prostate cancer screening, have found decision aids improve knowledge of PSA testing and reduced men’s desire to undergo screening.[ 126 ] However, at present, information on the harms of overdiagnosis and overtreatment is rarely presented.[ 127 ] Further, decision aids have not been widely implemented,[ 128 ] due to barriers including insufficient practitioner time, unawareness of and access to decision aids, and possibly lack of skills to utilise with patients in a clinical environment.[ 129 – 132 ]
Our findings demonstrate that participation in prostate cancer screening is informed by an individual’s subjective norms. Although routine screening for prostate cancer screening is not recommended, many men participate and remain enthusiastic about screening, as they believe that early detection prevents cancer.[ 133 ] In light of the potential harms of screening, addressing individual and community perceptions of prostate cancer screening through communication and health messages is important to normalise the decision to forgo prostate cancer screening.[ 134 ]
Therefore we suggest further work to gain understanding about what men understand about overdiagnosis as this does not appear to be explicitly addressed in existing studies. This could include eliciting their attitudes, reactions and choices made when provided with such information, and the harms and risks men prioritise, and how these potentially impact the decision making process, as has been done in the context of breast cancer.[ 135 ] As in other previous work in breast cancer screening,[ 134 ] assessing the impact of recent policy changes to prostate cancer screening uptake and understanding awareness of the guidelines changes, the controversy, and what formulates decision making is imperative to develop interventions that can improve the decision making process regarding prostate cancer screening.
As clinician recommendation is an important contributor to prostate cancer screening decisions, an understanding of how pre-screening discussions are conducted in clinical practice is important. Future studies are needed to promote shared decision making about prostate cancer screening. Further, research regarding shared decision making should focus not only on shared decision making as an outcome but also through understanding the processes of formulating a decision, delivering of information of the procedure and associated benefits and harms, and patient’s emotional experience and attitudes towards the decision making process. This will facilitate identification of best practices to disseminate shared decision making interventions.
Prostate cancer screening is sourced and accepted by men in order to prevent cancer-related morbidity and mortality and gain reassurance about their health. Their willingness to screen is informed by their primary care providers and support networks. However fears regarding their masculinity and invasiveness of the procedure, and hesitation relating to the ambiguities of the effectiveness, necessity and costs of screening, also contribute to their decision-making. Addressing the concerns and priorities of men regarding prostate cancer screening may empower men to make more informed decisions that reflect their personal priorities, preferences and values, and improve patient satisfaction and outcomes.
Transparency declaration: LJJ affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Supporting information
S1 text. search strategy..
https://doi.org/10.1371/journal.pone.0188258.s001
S1 Table. Study characteristics.
https://doi.org/10.1371/journal.pone.0188258.s002
S2 Table. ENTREQ checklist.
https://doi.org/10.1371/journal.pone.0188258.s003
S3 Table. PRISMA checklist.
https://doi.org/10.1371/journal.pone.0188258.s004
- 1. Cancer Research UK. Prostate cancer mortality statistics 2015. Available from: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer/mortality-heading-Zero , Accessed August 2016.
- 2. Prostate Cancer Foundation of Australia and Cancer Council Australia PSA Testing Guidelines Expert Advisory Panel. Clinical practice guidelines for PSA testing and early management of test-detected prostate cancer. Sydney: Cancer Council Australia.
- 3. Cancer Research UK. Prostate cancer statistics. Available from: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer-heading-Zero , Accessed August 2016.
- 4. Cancer Research UK. Prostate cancer incidence statistics. Available from: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer/incidence , Accessed August 2016.
- 5. Howlader N, Noone A, Krapcho M, Miller D, Bishop K, Altekruse S, et al. SEER cancer statistics review, 1975–2013, National Cancer Institute. Bethesda, MD http://seer.cancer.gov/csr/1975_2013/ , based on November 2015 SEER data submission, posted to the SEER web site, April 2016.
- 6. Australian Institute of Health and Welfare (AIHW). Australian cancer incidence and mortality (ACIM) books: prostate cancer. Canberra: AIHW2016. Available from: http://www.aihw.gov.au/acim-books .
- View Article
- PubMed/NCBI
- Google Scholar
- 54. Taylor MC. The impact of community health centers on prostate cancer screening behaviors of African American males: A mixed methods study [Dissertation Empirical Study; Interview; Qualitative Study; Quantitative Study]2013.
- 78. Hill KS. An exploratory case study of African American men on the decision making of prostate cancer screening [Dissertation Clinical Case Study; Empirical Study; Qualitative Study]2013.
- 82. Edwards QT. Differentiation of health behavior patterns related to prostate cancer screening among African-American men in military settings: Catholic University of America; 2000.
- 110. Wu T-Y, Bancroft J, editors. Filipino American Women's Perceptions and Experiences With Breast Cancer Screening. Oncology nursing forum; 2006.
- Open supplemental data
- Reference Manager
- Simple TEXT file
People also looked at
Original research article, causal relationship between immune cells and prostate cancer: a mendelian randomization study.

- 1 State Key Laboratory of Oncology in South China, Guangdong Provincial Clinical Research Center for Cancer, Sun Yat-Sen University Cancer Center, Guangzhou, China
- 2 Department of Oncology, The First Affiliated Hospital of Jinan University, Guangzhou, China
Introduction: Despite the abundance of research indicating the participation of immune cells in prostate cancer development, establishing a definitive cause-and-effect relationship has proven to be a difficult undertaking.
Methods: This study employs Mendelian randomization (MR), leveraging genetic variables related to immune cells from publicly available genome-wide association studies (GWAS), to investigate this association. The primary analytical method used in this study is inverse variance weighting (IVW) analysis. Comprehensive sensitivity analyses were conducted to assess the heterogeneity and horizontal pleiotropy of the results.
Results: The study identifies four immune cell traits as causally contributing to prostate cancer risk, including CD127- CD8+ T cell %CD8+ T cell (OR = 1.0042, 95%CI:1.0011–1.0073, p = 0.0077), CD45RA on CD39+ resting CD4 regulatory T cell (OR = 1.0029, 95%CI:1.0008–1.0050, p = 0.0065), CD62L− Dendritic Cell Absolute Count (OR = 1.0016; 95%CI:1.0005–1.0026; p = 0.0039), CX3CR1 on CD14+ CD16− monocyte (OR = 1.0024, 95%CI:1.0007–1.0040, p = 0.0060). Additionally, two immune cell traits are identified as causally protective factors: CD4 on monocyte (OR = 0.9975, 95%CI:0.9958–0.9992, p = 0.0047), FSC-A on plasmacytoid Dendritic Cell (OR = 0.9983, 95%CI:0.9970–0.9995, p = 0.0070). Sensitivity analyses indicated no horizontal pleiotropy.
Discussion: Our MR study provide evidence for a causal relationship between immune cells and prostate cancer, holding implications for clinical diagnosis and treatment.
Introduction
Prostate cancer is a prevalent malignant tumor in elderly men, ranking as the most common solid malignancy in men in western countries, with an increasing incidence year by year ( Rebello et al., 2021 ). Current research indicates that the occurrence of prostate cancer is primarily associated with factors such as age, hormones, race, and genetics ( Bergengren et al., 2023 ). However, its etiology and pathogenesis are not fully understood. Treatment for prostate cancer primarily includes surgery, radiation therapy, and androgen deprivation therapy ( Cha et al., 2020 ). Emerging treatment modalities have provided patients with a greater range of options. For example, the use of nanomaterials in conjunction with circRNA enhance the sensitivity of tumor cells to treatment ( Ghorbani et al., 2023 ; Su et al., 2023 ; Wang et al., 2023 ; Xie et al., 2023 ; Zetrini et al., 2023 ; Zhou et al., 2023 ). However, currently the efficacy for recurrent, drug-resistant, and metastatic prostate cancer is limited ( Antonarakis et al., 2010 ; Gao et al., 2023 ; Guo et al., 2023 ; Sooi et al., 2023 ; Su et al., 2023 ). Therefore, it is imperative to investigate the etiology, pathogenesis, and explore new treatment methods for prostate cancer.
Increasing research indicates that immune cells were involved in the development of prostate cancer. Various cell types involved in the regulation of prostate cancer have been identified ( Fridlender et al., 2009 ; Sagnak et al., 2011 ; Shi et al., 2023 ). NK cells and CD8 + T lymphocytes are pivotal forces in anti-tumor immunity, effectively eliminating cancer cells. Conversely, tumor-associated macrophages and other cells exert inhibitory effects on anti-tumor immunity, and their excessive activation may be associated with the occurrence and progression of tumors ( Luo et al., 2021 ; Shi et al., 2023 ). While there is a preliminary understanding of the roles of certain immune cell types in the pathogenesis of prostate cancer, the specific functions of various subtypes of immune cells and whether there is a causal relationship between these cells and tumor development remain unclear. Clarifying the causal relationship between immune cells and the onset of prostate cancer is a critical topic in current prostate cancer research.
However, the majority of research methods currently employed still face significant limitations in establishing a causal relationship between these factors. Mendelian randomization (MR), utilizing genetic variations as instrumental variables, is a valuable tool for establishing causal relationships. MR improves study validity by reducing bias and enabling causal inference in experimental designs. Mendelian randomization analysis offers advantages over randomized controlled trials (RCTs) by utilizing genetic variants as instrumental variables, providing insights into long-term exposures and outcomes, reducing confounding bias inherent in observational studies, and offering cost-effective alternatives in situations where RCTs are impractical or unethical ( Smith and Ebrahim, 2003 ; Larsson and Burgess, 2022 ). In this study, we employ MR to investigate the causal relationship between immune cells and prostate cancer. This approach is advantageous for illustrating the relationship between immune cells and prostate cancer, laying the groundwork for immunotherapeutic interventions in prostate cancer.
Data sources
This study utilized a population-based immune profiling analysis reported in the Nature Genetics journal. The research included a cohort of 3,757 individuals from the Sardinian population. The comprehensive investigation encompassed a wide range of 731 immunophenotypes, comprising absolute cell counts (n = 118), median fluorescence intensities (n = 389), morphological parameters (n = 32), and relative cell counts (n = 192) ( Orru et al., 2020 ).
The prostate cancer data used in this study were sourced from the Integrative Epidemiology Unit Open GWAS database ( https://gwas.mrcieu.ac.uk/ ). The study included 9,132 European male prostate cancer patients as the study group and 173,493 European males without prostate cancer as the control group. A total of 12,097,504 SNPs were screened for their impact on prostate cancer. The diagnostic criteria for prostate cancer are derived from ICD-10 code C61 and ICD-9 code 185 ( Kimberley Burrows, 2021 ). Figure 1 illustrates the study’s specific research approach, while Table 1 provides specific details on data sources and features.
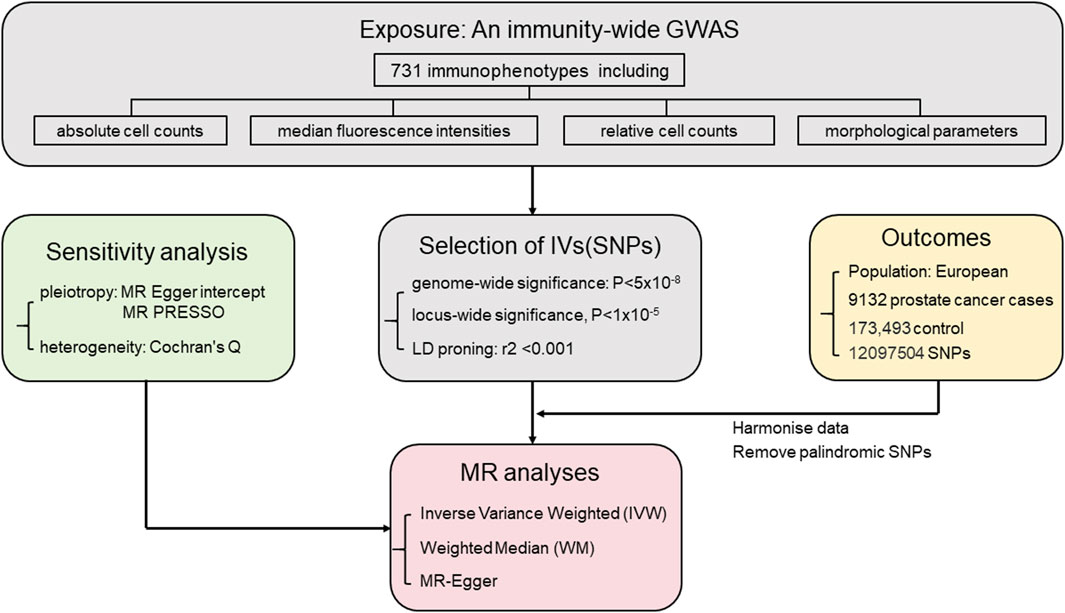
FIGURE 1 . Mendelian randomization study workflow on the association between immune cell types and prostate cancer.

TABLE 1 . Detailed information on the analyzed data.
Instrumental variables (IVs)
MR employs genetic variants as instrumental variables. The selection of instrumental variables needs to satisfy three assumptions: 1) the genetic variants have strong association with the exposure factor; 2) the genetic variants were independent from confounding factors. 3) the genetic variants affect the outcome through the exposure factor ( Smith and Ebrahim, 2004 ; Richmond and Davey Smith, 2022 ). The process of selecting genetic variants as instrumental variables is illustrated in Figure 2 .
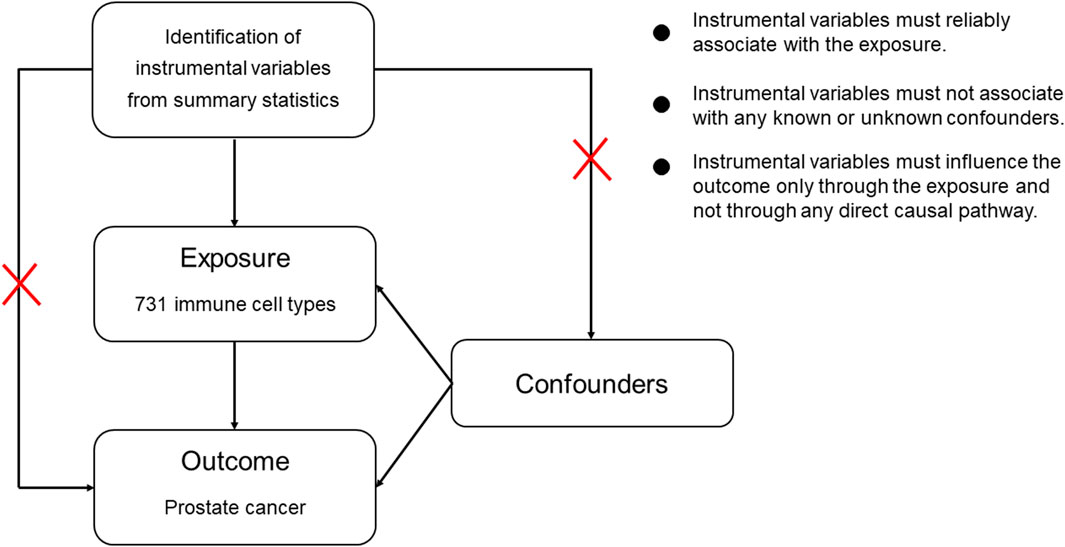
FIGURE 2 . Assumptions in MR studies: a brief overview.
The selection and analysis of IVs for immune traits were conducted meticulously, employing a significance level of 1 × 10 −5 . To ensure the independence of loci, a clumping window of 10,000 kb and a linkage disequilibrium (LD) threshold of r2 < 0.001 were employed. The implementation was carried out using the “TwoSampleMR” package and 1,000 Genomes EUR data. Palindrome SNPs may introduce uncertainty regarding the effect allele in GWAS. To ensure reliability, we excluded palindrome SNPs with effect allele frequencies between 0.3 and 0.7. Additionally, instrument strength was assessed using F-statistics, where a variance ratio (b 2 /se 2 ) exceeding 10 indicates minimal weak instrument bias ( Burgess et al., 2011 ).
Statistical analysis
In this research, various analytical methods including the Inverse Variance Weighted (IVW) method, weighted median method, and MR-Egger regression analysis were employed. The IVW method, widely used in MR studies for its excellent accuracy in effect estimation, was applied in this study with a higher screening threshold ( p -value <0.01) to ensure result accuracy. Random-effects IVW provides an unbiased estimate by considering heterogeneity among studies and appropriately weighting the effects based on their precision. The IVW method was chosen as the primary research method used in this study ( Hemani et al., 2018b ). The MR Egger method accurately evaluates causal relationships, effectively addresses sample selection bias, and enhances statistical power and robustness of data ( Verbanck et al., 2018 ). The weighted median approach provides a reliable estimate by accounting for the distribution of weights assigned to each data point ( Hemani et al., 2018b ). Cochran’s Q test was used to assess heterogeneity ( Bowden et al., 2019 ). MR Egger intercept analysis serves to assess and correct for potential bias caused by horizontal pleiotropy. MR-PRESSO analysis method is designed to detect and correct for horizontal pleiotropy ( Verbanck et al., 2018 ). The application of multiple statistical techniques contributes to the reliability and rigor of the study, facilitating a deeper understanding of the intricate relationship between immune cells and prostate cancer ( Hemani et al., 2018a ). All analyses were conducted with the “TwoSampleMR” package (v.0.5.7) in R (v.4.3.0).
The main results of the analysis of the association between 731 immune cell types and the risk of prostate cancer.
F-statistics were calculated for all 731 immune cell types, ranging from 19.55 to 2381.77. The F-values for all results exceeded 10, surpassing the minimum threshold for weak instrument bias, indicating that they are all strong instrument variables. Detailed information on single nucleotide polymorphisms (SNPs) for each immune cell type is provided in Supplementary Table S1 . The MR results for all features and their associations with prostate cancer are summarized in Supplementary Table S3 , revealing six immune cell types with potential correlations detected using the IVW method, as shown in Figure 1 . The IVs used for immune traits are presented in Supplementary Tables S1, S2 . This MR analysis identified a causal relationship between six immune cell types and the risk of prostate cancer, as illustrated in Figure 3 and detailed in Supplementary Table S4 . The study provides additional evidence to establish potential connections between specific types of immune cells and the risk of prostate cancer.
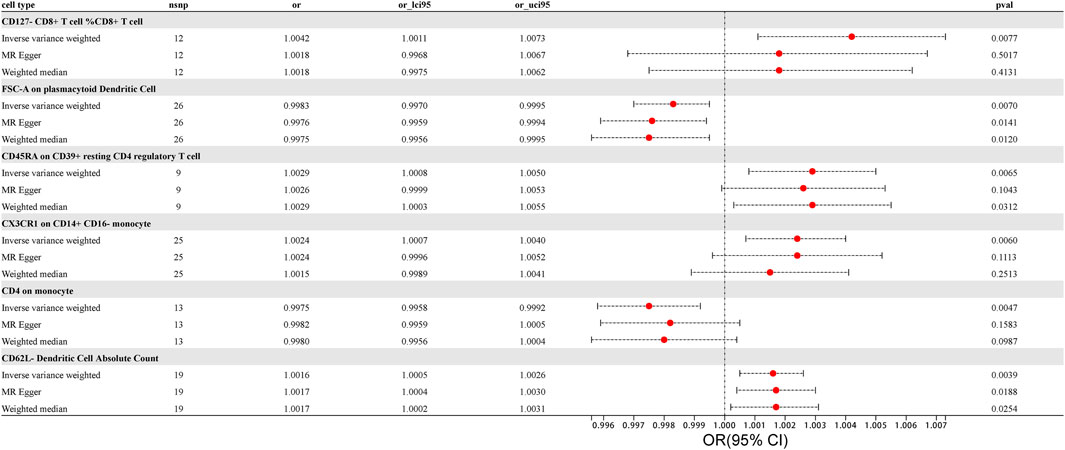
FIGURE 3 . Forest Plot: Associations of Genetically Determined immune traits with prostate cancer risk.
Using the IVW method, we found a clear association between T lymphocytes, monocytes-macrophages, dendritic cells, and the occurrence of prostate cancer. The IVW analysis revealed a positive correlation between CD127 - CD8 + T cell %CD8 + T cell and the risk of prostate cancer (OR = 1.0042, 95%CI:1.0011–1.0073, p = 0.0077). The MR-Egger and weighted median analysis methods did not reveal specific association. Both the MR-Egger intercept assessment ( p = 0.2416) and MR-PRESSO global test ( p = 0.3970) analysis did not indicate horizontal pleiotropy ( Supplementary Tables S5, S6 ).
Similarly, CD45RA on CD39 + resting CD4 regulatory T cell, belonging to T cells, was confirmed to be positively correlated with prostate cancer risk through IVW analysis (OR = 1.0029, 95% CI: 1.0008–1.0050, p = 0.0065), with no significant association in weighted median and MR-Egger. No evidence of horizontal pleiotropy in the MR-Egger intercept assessment ( p = 0.7244) and MR-PRESSO global test analysis ( p = 0.8420) ( Supplementary Tables S5, S6 ).
CX3CR1 on CD14 + CD16 − monocyte was identified through IVW analysis to be positively associated with the risk of prostate cancer (OR = 1.0024, 95%CI:1.0007–1.0040, p = 0.0060). This association was not significant in MR-Egger and weighted median analyses. Both the MR-Egger intercept assessment ( p = 0.9813) and MR-PRESSO global test analysis ( p = 0.8660) did not reveal horizontal pleiotropy ( Supplementary Tables S5, S6 ).
For dendritic cells, CD62L − Dendritic Cell Absolute Count was confirmed to be positively correlated with the risk of prostate cancer through IVW analysis (IVW: OR = 1.0016; 95%CI:1.0005–1.0026; p = 0.0039), with no significant association in MR-Egger and weighted median, and no evidence of horizontal pleiotropy in the MR-Egger intercept assessment ( p = 0.7088) as well as MR-PRESSO global test analysis ( p = 0.4650). The results, analyzed and tested using various methods while excluding outliers and heterogeneity, provided more accurate causal associations and offered new evidence in exploring which immune cells may promote the occurrence of prostate cancer ( Supplementary Tables S5, S6 ).
In contrast to the cells positively correlated with the risk of prostate cancer mentioned above, we also identified immune cells negatively correlated with prostate cancer risk using the IVW method. In monocytes-macrophages, CD4 on monocyte was found to be negatively correlated with prostate cancer risk through IVW testing (OR = 0.9975, 95%CI:0.9958–0.9992, p = 0.0047). This correlation was not significant in MR-Egger and weighted median analyses, and the MR-Egger intercept assessment ( p = 0.3962) as well as MR-PRESSO global test analysis ( p = 0.7580) did not reveal horizontal pleiotropy. Similarly, in dendritic cells, FSC-A on plasmacytoid Dendritic Cell was identified through IVW testing to be negatively correlated with the risk of prostate cancer (OR = 0.9983, 95%CI:0.9970–0.9995, p = 0.0070). However, MR Egger and weighted median analyses did not find a significant association between these immune cells and the risk of prostate cancer, and intercept of MR-Egger analysis ( p = 0.3206) as well as MR-PRESSO global test ( p = 0.4020) analysis did not reveal horizontal pleiotropy in both cases ( Supplementary Tables S5, S6 ).
Scatterplot of genetic association between immune traits and prostate cancer were shown in Figure 4 . We found no significant heterogeneity among immune cells instrumental variables, which further indicates that immune cells play a complex and crucial role in the development of prostate cancer ( Supplementary Table S7 ). Some cells promote the occurrence of prostate cancer, while others have the potential to inhibit the onset of prostate cancer. These findings provide new insights into the pathogenesis and treatment of prostate cancer.
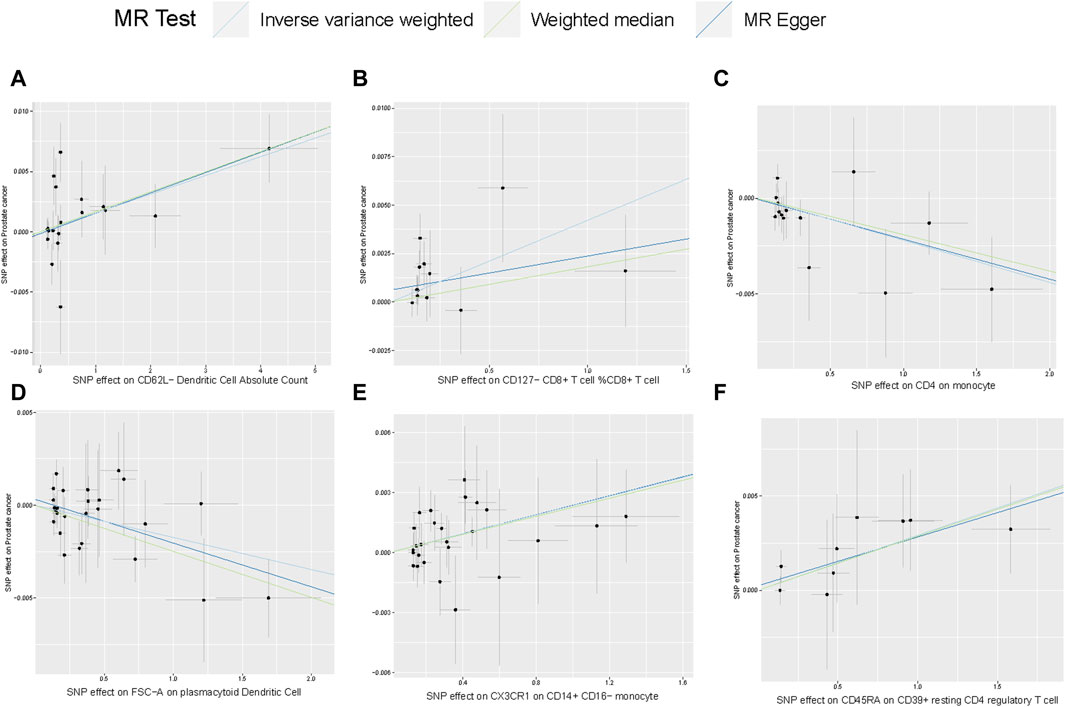
FIGURE 4 . Scatterplot of genetic association between immune traits and prostate cancer. (A) Genetic association of CD62L− Dendritic Cell Absolute Count with prostate cancer Causal effect of Desulfovibrionales on CKD; (B–F) Potential causal effect of five other immune traits on prostate cancer.
In this MR analysis, we identified six types of immune cells related to the risk of prostate cancer, primarily including T cells, monocytes, and dendritic cells. These three categories exhibit different phenotypes and causal relationships with prostate cancer.
The study revealed a positive correlation between CD127 - CD8 + T cell %CD8 + T cell and the development of prostate cancer. CD127, also known as the IL-7 receptor alpha chain, is a component of the IL-7 receptor ( Aloufi et al., 2021 ). IL-7 assumes a vital role in the progression of lymphocyte development ( Lundstrom et al., 2012 ). In normal circumstances, immune cells, especially T cells, receive IL-7 signals through CD127, enhancing their survival and functionality to combat abnormal cells, including cancer cells. CD127 - cells, lacking the ability to receive IL-7 signals, result in immune cells becoming inactive or ineffective in the tumor microenvironment, leading to immune tolerance ( Joshi et al., 2007 ). Therefore, the research findings indicating a positive correlation between CD127 - CD8 + T cell %CD8 + T cell and prostate cancer development are mechanistically reasonable. This provides a favorable basis for further exploring the exact role of CD127 in tumors.
In investigating the interplay between T cells and prostate cancer, we uncovered another intriguing result: CD45RA on CD39 + resting CD4 regulatory T cells is also positively correlated with prostate cancer development. CD45RA is typically expressed on unactivated, resting immune cells, especially unstimulated T cells ( Hermiston et al., 2003 ). CD39, also known as NTPDase1, degrades extracellular ATP. Since ATP has pro-inflammatory effects outside the cells, CD39, by converting ATP to ADP and AMP, indirectly reduces extracellular ATP concentration, thus inhibiting inflammatory reactions ( Timperi and Barnaba, 2021 ). Regulatory T cells (Tregs) suppress the activity of immune cells through various mechanisms.
In the tumor microenvironment, an excessive presence of Tregs may restrict the attack of other immune cells on tumor cells, promoting tumor escape ( Ji et al., 2020 ). Therefore, CD45RA on CD39 + resting CD4 regulatory T cells, by degrading the pro-inflammatory factor ATP and inhibiting the anti-tumor effects of other immune cells, creates a more permissive immune environment for tumor cells. This allows tumor cells to evade immune system surveillance and attacks.
In the analysis of the interaction between immune cells and prostate cancer using MR analysis, a complex relationship was identified, such as a positive correlation between CX3CR1 on CD14 + CD16 − monocytes and the development of prostate cancer, and a negative correlation between CD4 on monocytes and prostate cancer development. CX3CR1 is a chemokine receptor that, by influencing monocyte chemotaxis and tumor angiogenesis ( Pawelec et al., 2020 ), can alter the tumor immune microenvironment, thereby affecting tumor development and immune responses ( Schmall et al., 2015 ). On the other hand, CD14 can interact with receptors such as TLR4, recognizing and binding to molecular patterns of bacteria ( Marchesi et al., 2010 ). However, the role of CD14 in tumor development may be more complex. They can participate in anti-tumor immune responses ( Pallett et al., 2023 ) and produce inhibitory cytokines that promote immune escape by tumors ( Cheah et al., 2015 ). CD16 can bind to the Fc region of antibodies, forming complexes with antibodies. When these complexes bind to antigens on the surface of target cells, they activate natural killer cells, triggering ADCC ( Bhatnagar et al., 2014 ). Based on the above, it is speculated that the possible mechanism by which CX3CR1 on CD14 + CD16 − monocytes promotes prostate cancer development is through the CX3CR1/CX3CL1 signaling pathway, promoting tumor angiogenesis, migration, and infiltration, while inhibiting ADCC, thereby weakening the body’s anti-tumor effects.
The expression of CD4 on monocytes is likely a marker of monocyte activation. Activated monocytes may participate in regulating immune responses, limiting tumor growth. However, as the tumor microenvironment changes ( Zhen et al., 2014 ), the immune regulatory function of monocytes may be inhibited. The exact role of CD4 on monocytes in tumor development depends on the specific tumor type and individual differences among patients. Therefore, further experimental and clinical studies are needed. In summary, the MR analysis revealed complex interactions between monocytes and prostate cancer. This MR analysis is crucial for understanding the role of monocytes in cancer development and exploring new treatment methods.
Dendritic cells, a subset of antigen-presenting cells (APCs), play a crucial role in initiating and activating T cells, enhance the immune regulation of natural killer cells, and exhibit cytotoxic capabilities ( Laginha et al., 2022 ). Presently, there have been encouraging outcomes observed in the use of immunotherapy utilizing dendritic cells for the management of prostate cancer ( Jahnisch et al., 2010 ). This MR analysis provides the first confirmation that CD62L − Dendritic Cell Absolute Count is positively correlated with the development of prostate cancer, while FSC-A on plasmacytoid Dendritic Cell shows a negative correlation. CD62L, also known as L-selectin, is a cell adhesion molecule that participates in leukocyte rolling, adhesion, and migration by binding to ligands on endothelial cells ( Ivetic et al., 2019 ). Decreased expression of CD62L results in reduced chemotactic ability of dendritic cells, leading to a weakened anti-tumor inflammatory response. FSC-A is a crucial parameter used in flow cytometry to measure forward scatter signals and estimate cell size. Plasmacytoid dendritic cells are among the most potent regulators of antiviral immune responses in the body, producing large amounts of type I interferons ( Mitchell et al., 2018 ), such as IFN-α. However, there is currently no experimental data supporting the negative correlation between FSC-A on plasmacytoid Dendritic Cell and prostate cancer. This finding provides new experimental avenues for exploring the relationship between dendritic cells and prostate cancer.
The intricate complexity lies in the interplay between prostate cancer and immune cells. These findings provide important insights into the roles of T cells, monocytes, and dendritic cells in the risk of prostate cancer, contributing to the advancement of immunotherapy for prostate cancer. However, there are certain limitations to consider. Firstly, the causal relationship between the identified six immune cells and prostate cancer was not strong. The causality links’ low power may result from the heterogeneity of the outcomes such as prostate cancer’s stage, severity, and duration. However, at this stage, there is still a lack of data on prostate cancer GWAS sequencing with specific clinical characteristics. Secondly, the population included in the Genome-Wide Association Study (GWAS) mainly comprises individuals of European ancestry. Genetic differences between populations may result in variations in the relationship between immune cells and prostate cancer, introducing a potential ethnic bias to the MR study results. Thirdly, the use of a low threshold value ( p < 1.0 × 10 −5 ) during the tool variable selection may lead to false positives or overlook important genetic variations related to immune cell features. Fourthly, the lack of independent cohort studies to validate the research findings. Fifthly, our research has only demonstrated partial correlation between immune cells and the development of prostate cancer, lacking experimental evidence to further explore and uncover the underlying mechanisms. In the future, we will conduct biological experiments to delve deeper into our findings and investigate potential mechanisms.
Data availability statement
The original contributions presented in the study are included in the article/ Supplementary Material , further inquiries can be directed to the corresponding authors.
Author contributions
ZY: Conceptualization, Data curation, Formal Analysis, Writing–original draft, Writing–review and editing. XD: Data curation, Writing–original draft, Writing–review and editing. JinZ: Data curation, Writing–original draft. RS: Formal Analysis, Writing–original draft. CS: Formal Analysis, Writing–original draft. JiaZ: Conceptualization, Project administration, Writing–review and editing, Writing–original draft. HT: Conceptualization, Project administration, Writing–review and editing, Writing–original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.

Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcell.2024.1381920/full#supplementary-material
Aloufi, N. A., Ali, A. K., Burke Schinkel, S. C., Molyer, B., Barros, P. O., Mcbane, J. E., et al. (2021). Soluble CD127 potentiates IL-7 activity in vivo in healthy mice. Immun. Inflamm. Dis. 9, 1798–1808. doi:10.1002/iid3.530
PubMed Abstract | CrossRef Full Text | Google Scholar
Antonarakis, E. S., Carducci, M. A., and Eisenberger, M. A. (2010). Novel targeted therapeutics for metastatic castration-resistant prostate cancer. Cancer Lett. 291, 1–13. doi:10.1016/j.canlet.2009.08.012
Bergengren, O., Pekala, K. R., Matsoukas, K., Fainberg, J., Mungovan, S. F., Bratt, O., et al. (2023). 2022 update on prostate cancer epidemiology and risk factors-A systematic review. Eur. Urol. 84, 191–206. doi:10.1016/j.eururo.2023.04.021
Bhatnagar, N., Ahmad, F., Hong, H. S., Eberhard, J., Lu, I. N., Ballmaier, M., et al. (2014). FcγRIII (CD16)-mediated ADCC by NK cells is regulated by monocytes and FcγRII (CD32). Eur. J. Immunol. 44, 3368–3379. doi:10.1002/eji.201444515
Bowden, J., Del Greco, M. F., Minelli, C., Zhao, Q., Lawlor, D. A., Sheehan, N. A., et al. (2019). Improving the accuracy of two-sample summary-data Mendelian randomization: moving beyond the NOME assumption. Int. J. Epidemiol. 48, 728–742. doi:10.1093/ije/dyy258
Burgess, S., Thompson, S. G., and Collaboration, C. C. G. (2011). Avoiding bias from weak instruments in Mendelian randomization studies. Int. J. Epidemiol. 40, 755–764. doi:10.1093/ije/dyr036
Cha, H. R., Lee, J. H., and Ponnazhagan, S. (2020). Revisiting immunotherapy: a focus on prostate cancer. Cancer Res. 80, 1615–1623. doi:10.1158/0008-5472.CAN-19-2948
Cheah, M. T., Chen, J. Y., Sahoo, D., Contreras-Trujillo, H., Volkmer, A. K., Scheeren, F. A., et al. (2015). CD14-expressing cancer cells establish the inflammatory and proliferative tumor microenvironment in bladder cancer. Proc. Natl. Acad. Sci. U. S. A. 112, 4725–4730. doi:10.1073/pnas.1424795112
Fridlender, Z. G., Sun, J., Kim, S., Kapoor, V., Cheng, G., Ling, L., et al. (2009). Polarization of tumor-associated neutrophil phenotype by TGF-beta: "N1" versus "N2" TAN. Cancer Cell 16, 183–194. doi:10.1016/j.ccr.2009.06.017
Gao, K., Li, X., Ni, J., Wu, B., Guo, J., Zhang, R., et al. (2023). Non-coding RNAs in enzalutamide resistance of castration-resistant prostate cancer. Cancer Lett. 566, 216247. doi:10.1016/j.canlet.2023.216247
Ghorbani, R., Gharbavi, M., Sharafi, A., Rismani, E., Rezaeejam, H., Mortazavi, Y., et al. (2023). Targeted anti-tumor synergistic effects of Myc decoy oligodeoxynucleotides-loaded selenium nanostructure combined with chemoradiotherapy on LNCaP prostate cancer cells. Oncol. Res. 32, 101–125. doi:10.32604/or.2023.044741
Guo, X., Gao, C., Yang, D. H., and Li, S. (2023). Exosomal circular RNAs: a chief culprit in cancer chemotherapy resistance. Drug Resist Updat 67, 100937. doi:10.1016/j.drup.2023.100937
Hemani, G., Bowden, J., and Davey Smith, G. (2018a). Evaluating the potential role of pleiotropy in Mendelian randomization studies. Hum. Mol. Genet. 27, R195–R208. doi:10.1093/hmg/ddy163
Hemani, G., Zheng, J., Elsworth, B., Wade, K. H., Haberland, V., Baird, D., et al. (2018b). The MR-Base platform supports systematic causal inference across the human phenome. Elife 7, e34408. doi:10.7554/eLife.34408
Hermiston, M. L., Xu, Z., and Weiss, A. (2003). CD45: a critical regulator of signaling thresholds in immune cells. Annu. Rev. Immunol. 21, 107–137. doi:10.1146/annurev.immunol.21.120601.140946
Ivetic, A., Hoskins Green, H. L., and Hart, S. J. (2019). L-Selectin: a major regulator of leukocyte adhesion, migration and signaling. Front. Immunol. 10, 1068. doi:10.3389/fimmu.2019.01068
Jahnisch, H., Fussel, S., Kiessling, A., Wehner, R., Zastrow, S., Bachmann, M., et al. (2010). Dendritic cell-based immunotherapy for prostate cancer. Clin. Dev. Immunol. 2010, 517493. doi:10.1155/2010/517493
Ji, D., Song, C., Li, Y., Xia, J., Wu, Y., Jia, J., et al. (2020). Combination of radiotherapy and suppression of Tregs enhances abscopal antitumor effect and inhibits metastasis in rectal cancer. J. Immunother. Cancer 8, e000826. doi:10.1136/jitc-2020-000826
Joshi, N. S., Cui, W., Chandele, A., Lee, H. K., Urso, D. R., Hagman, J., et al. (2007). Inflammation directs memory precursor and short-lived effector CD8(+) T cell fates via the graded expression of T-bet transcription factor. Immunity 27, 281–295. doi:10.1016/j.immuni.2007.07.010
Kimberley Burrows, P. H. (2021). Genome-wide association study of cancer risk in UK biobank. Available: http://www.nealelab.is/uk-biobank/ .
Google Scholar
Laginha, P. A., Arcoverde, F. V. L., Riccio, L. G. C., Andres, M. P., and Abrao, M. S. (2022). The role of dendritic cells in endometriosis: a systematic review. J. Reprod. Immunol. 149, 103462. doi:10.1016/j.jri.2021.103462
Larsson, S. C., and Burgess, S. (2022). Appraising the causal role of smoking in multiple diseases: a systematic review and meta-analysis of Mendelian randomization studies. EBioMedicine 82, 104154. doi:10.1016/j.ebiom.2022.104154
Lundstrom, W., Fewkes, N. M., and Mackall, C. L. (2012). IL-7 in human health and disease. Semin. Immunol. 24, 218–224. doi:10.1016/j.smim.2012.02.005
Luo, Z. W., Xia, K., Liu, Y. W., Liu, J. H., Rao, S. S., Hu, X. K., et al. (2021). Extracellular vesicles from akkermansia muciniphila elicit antitumor immunity against prostate cancer via modulation of CD8(+) T cells and macrophages. Int. J. Nanomedicine 16, 2949–2963. doi:10.2147/IJN.S304515
Marchesi, F., Locatelli, M., Solinas, G., Erreni, M., Allavena, P., and Mantovani, A. (2010). Role of CX3CR1/CX3CL1 axis in primary and secondary involvement of the nervous system by cancer. J. Neuroimmunol. 224, 39–44. doi:10.1016/j.jneuroim.2010.05.007
Mitchell, D., Chintala, S., and Dey, M. (2018). Plasmacytoid dendritic cell in immunity and cancer. J. Neuroimmunol. 322, 63–73. doi:10.1016/j.jneuroim.2018.06.012
Orru, V., Steri, M., Sidore, C., Marongiu, M., Serra, V., Olla, S., et al. (2020). Complex genetic signatures in immune cells underlie autoimmunity and inform therapy. Nat. Genet. 52, 1036–1045. doi:10.1038/s41588-020-0684-4
Pallett, L. J., Swadling, L., Diniz, M., Maini, A. A., Schwabenland, M., Gasull, A. D., et al. (2023). Tissue CD14(+)CD8(+) T cells reprogrammed by myeloid cells and modulated by LPS. Nature 614, 334–342. doi:10.1038/s41586-022-05645-6
Pawelec, P., Ziemka-Nalecz, M., Sypecka, J., and Zalewska, T. (2020). The impact of the cx3cl1/cx3cr1 Axis in neurological disorders. Cells 9, 2277. doi:10.3390/cells9102277
Rebello, R. J., Oing, C., Knudsen, K. E., Loeb, S., Johnson, D. C., Reiter, R. E., et al. (2021). Prostate cancer. Nat. Rev. Dis. Prim. 7, 9. doi:10.1038/s41572-020-00243-0
Richmond, R. C., and Davey Smith, G. (2022). Mendelian randomization: concepts and scope. Cold Spring Harb. Perspect. Med. 12, a040501. doi:10.1101/cshperspect.a040501
Sagnak, L., Topaloglu, H., Ozok, U., and Ersoy, H. (2011). Prognostic significance of neuroendocrine differentiation in prostate adenocarcinoma. Clin. Genitourin. Cancer 9, 73–80. doi:10.1016/j.clgc.2011.07.003
Schmall, A., Al-Tamari, H. M., Herold, S., Kampschulte, M., Weigert, A., Wietelmann, A., et al. (2015). Macrophage and cancer cell cross-talk via CCR2 and CX3CR1 is a fundamental mechanism driving lung cancer. Am. J. Respir. Crit. Care Med. 191, 437–447. doi:10.1164/rccm.201406-1137OC
Shi, W., Wang, Y., Zhao, Y., Kim, J. J., Li, H., Meng, C., et al. (2023). Immune checkpoint B7-H3 is a therapeutic vulnerability in prostate cancer harboring PTEN and TP53 deficiencies. Sci. Transl. Med. 15, eadf6724. doi:10.1126/scitranslmed.adf6724
Smith, G. D., and Ebrahim, S. (2003). Mendelian randomization': can genetic epidemiology contribute to understanding environmental determinants of disease? Int. J. Epidemiol. 32, 1–22. doi:10.1093/ije/dyg070
Smith, G. D., and Ebrahim, S. (2004). Mendelian randomization: prospects, potentials, and limitations. Int. J. Epidemiol. 33, 30–42. doi:10.1093/ije/dyh132
Sooi, K., Walsh, R., Kumarakulasinghe, N., Wong, A., and Ngoi, N. (2023). A review of strategies to overcome immune resistance in the treatment of advanced prostate cancer. Cancer Drug Resist 6, 656–673. doi:10.20517/cdr.2023.48
Su, Y., Jin, G., Zhou, H., Yang, Z., Wang, L., Mei, Z., et al. (2023). Development of stimuli responsive polymeric nanomedicines modulating tumor microenvironment for improved cancer therapy. Med. Rev. 3, 4–30. doi:10.1515/mr-2022-0048
CrossRef Full Text | Google Scholar
Timperi, E., and Barnaba, V. (2021). CD39 regulation and functions in T cells. Int. J. Mol. Sci. 22, 8068. doi:10.3390/ijms22158068
Verbanck, M., Chen, C. Y., Neale, B., and Do, R. (2018). Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat. Genet. 50, 693–698. doi:10.1038/s41588-018-0099-7
Wang, H., Liu, J., Zhu, X., Yang, B., He, Z., and Yao, X. (2023). AZGP1P2/UBA1/RBM15 cascade mediates the fate determinations of prostate cancer stem cells and promotes therapeutic effect of docetaxel in castration-resistant prostate cancer via TPM1 m6A modification. Res. (Wash D C) 6, 0252. doi:10.34133/research.0252
Xie, J., Ye, F., Deng, X., Tang, Y., Liang, J. Y., Huang, X., et al. (2023). Circular RNA: a promising new star of vaccine. J. Transl. Int. Med. 11, 372–381. doi:10.2478/jtim-2023-0122
Zetrini, A. E., Lip, H., Abbasi, A. Z., Alradwan, I., Ahmed, T., He, C., et al. (2023). Remodeling tumor immune microenvironment by using polymer-lipid-manganese dioxide nanoparticles with radiation therapy to boost immune response of castration-resistant prostate cancer. Res. (Wash D C) 6, 0247. doi:10.34133/research.0247
Zhen, A., Krutzik, S. R., Levin, B. R., Kasparian, S., Zack, J. A., and Kitchen, S. G. (2014). CD4 ligation on human blood monocytes triggers macrophage differentiation and enhances HIV infection. J. Virol. 88, 9934–9946. doi:10.1128/JVI.00616-14
Zhou, Z., Qin, J., Song, C., Wu, T., Quan, Q., Zhang, Y., et al. (2023). circROBO1 promotes prostate cancer growth and enzalutamide resistance via accelerating glycolysis. J. Cancer 14, 2574–2584. doi:10.7150/jca.86940
Keywords: prostate cancer, immune cells, Mendelian randomization, single nucleotide polymorphism, genome-wide association studies
Citation: Ye Z, Deng X, Zhang J, Shao R, Song C, Zhao J and Tang H (2024) Causal relationship between immune cells and prostate cancer: a Mendelian randomization study. Front. Cell Dev. Biol. 12:1381920. doi: 10.3389/fcell.2024.1381920
Received: 04 February 2024; Accepted: 08 March 2024; Published: 19 March 2024.
Reviewed by:
Copyright © 2024 Ye, Deng, Zhang, Shao, Song, Zhao and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianfu Zhao, [email protected] ; Hailin Tang, [email protected]
† These authors have contributed equally to this work
This article is part of the Research Topic
Perspectives on Omics Analysis in Solid Tumors: Advancing Cancer Research
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
March 30, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Prostate cancer is the second-leading cancer among men. Here's what to know about it
by Erin Kayata, Northeastern University

Cancer rates, especially among young people, are on the rise. There's expected to be 2 million new cancer diagnoses in the United States in 2024.
Among these diagnoses is a rise in prostate cancer.
Prostate cancer is one of the most common cancers in the United States, making up about 29% of cancer cases diagnosed among men in 2023 and 11% of cancer deaths. It's also the second-leading cancer among men.
Prostate cancer originates in the prostate, a gland located between a man's bladder and rectum. It is responsible for producing fluid in semen and helps with its ejection. This organ is only found in men.
Doctors test for prostate cancer in one of two ways. One is through a rectal exam in which a doctor feels the gland and for any issues with it. The other way to test for prostate cancer is through prostate-specific antigen testing, a blood test commonly known as PSA.
Screenings can be uncomfortable
However, one of the barriers is getting men to these screenings.
"They're uncomfortable," says Susan Mello, an associate professor of communication studies at Northeastern University who specializes in health communications. "They can be embarrassing. If you know what's involved, (that can be) a barrier to going and getting screened."
Health literacy can also be a barrier, Mello says.
"People not understanding what they should be screening for," she says, "or if they should be getting tested. If they're not going for a regular annual physical … they're not getting those traditional reminders."
Mello added that many men also don't know the risk factors for cancer and whether those weigh into when they should be screened.
What are the risk factors?
Risk factors for prostate cancer include older age (cases before 40 are rare), family history and race. Black men are at a higher risk of developing prostate cancer with one in six Black men being diagnosed in his lifetime versus men of other races who are diagnosed at a rate of one in eight.
"Having an understanding of what your personal risk factors are can be tricky," Mello says.
The American Cancer Society recommends men at an average risk for prostate cancer begin being screened at 50, while Black men and men with a family history (a father or brother diagnosed before age 65) be screened at 45. Men with more than one first-degree relative diagnosed at an early age should be screened as early as 40.
Prostate cancer overall has a strong five-year survival rate, thanks in part to these treatment methods. If the cancer hasn't spread to other parts of the body, the chance of recovery is about 99%.
The usual approach to treating cancer is to remove it from the body, whether through surgery, radiation, or chemotherapy.
This is often the case with prostate cancer, says Asieh Golozar, director of clinical research at Northeastern's Observational Health Data Sciences and Informatics Center. Doctors can remove the gland and treat the patient with radiation to ensure there are no tumors in the surrounding organs. Hormonal therapy is also an option.
Diagnosis can be a double-edged sword
Diagnosis through PSA testing allows for early cancer detection. This can be a double-edged sword. With early detection come challenges when it comes to the treatment of prostate cancer.
"There's questions about how to treat them," says Golozar, who has done research into prostate cancer treatment options. "When it comes to cancer, it's scary. You got to treat fast and you've got to take it out. … (With prostate cancer), you get a lot of patients that are diagnosed way, way early on because they had an abnormal PSA. Some of them could have just lived with their prostate cancer until they die without the disease causing them any problem. And that happens quite a lot."
Not only are these treatment methods painful, but they can also affect the patient's ability to function sexually and can also cause incontinence.
"Being radical means there's consequences for the patients," Golozar says. "You have to go through surgery. Radiotherapy is extremely painful. … It's not the easiest thing. … A good proportion of these patients when they're diagnosed early on, they're young. They might be diagnosed in their 50s and 60s. Theoretically, they could live with that minimally growing tumor for decades without being symptomatic."
Negative side effects vs. risk of spread
Older patients who are diagnosed when they're already in poor health face the same dilemma: doctors have to decide whether the negative side effects from treatment outweigh the risk of the tumor spreading and becoming symptomatic.
Prostate cancer symptoms include trouble urinating, blood in the urine or semen, weight loss, bone pain and erectile dysfunction.
Golozar says that often patients with later-stage disease benefit from treatment, but very young patients and very old patients benefit from "active surveillance" where doctors monitor the prostate and act if there are signs of it worsening.
"The idea of active surveillance (is) … so if we catch the cancer at the time that it's becoming something dangerous," Golozar says. "That might be 20 years or something that this patient can be treatment-free."
This story is republished courtesy of Northeastern Global News news.northeastern.edu .
Explore further
Feedback to editors

Person is diagnosed with bird flu after being in contact with cows in Texas
5 hours ago

'Pathogen prospecting': Mosquito researchers track malaria's history by examining its epidemiology

Pilot study shows ketogenic diet improves severe mental illness

Chatbot outperforms physicians in clinical reasoning, but also underperforms against residents on many occasions
6 hours ago

Reducing late-night alcohol sales curbed all violent crimes by 23% annually in a Baltimore neighborhood: Study

Scientists pioneer immunotherapy technique for autoimmune diseases

Researchers develop more broadly protective coronavirus vaccine

Scientists discover speed of visual perception ranges widely in humans
7 hours ago

Move more, sleep better: Study finds physical activity lengthens REM latency
8 hours ago

Siris tree leaves hold promise for stopping spread of breast cancer cells, say researchers
9 hours ago
Related Stories

Prostate cancer: Screening and treatment options
Jan 25, 2024

What factors affect patients' decisions regarding active surveillance for low-risk prostate cancer?
Jan 22, 2024

Q&A: Combating prostate cancer stigma
Feb 27, 2024

Video: What Black men need to know about prostate cancer
Sep 20, 2023

Prostate cancer: Screening and treatment
Sep 19, 2022

Should men be concerned about prostate cancer?
Nov 19, 2020
Recommended for you

Using cryo-shocked tumor cells to fight lung cancer
11 hours ago

Enhanced melanoma vaccine offers improved survival for men
Mar 29, 2024

Researchers develop AI-based tool paving the way for personalized cancer treatments

Researchers demonstrate technique for identifying single cancer cells in blood for the first time
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

An official website of the United States government
- Approved Projects
- Master's Thesis on Mathematical Modeling of Prost…
- Early Phase Prevention Trials
- HIP Breast Cancer Screening Trial
- Memorial Sloan-Kettering Lung Study
- Minnesota Colon Cancer Control Study
- Lung Screening Study
- Johns Hopkins Lung Project
- Mayo Lung Project
- Browse Approved Projects
- Browse All Publications
Master's Thesis on Mathematical Modeling of Prostate Cancer
The data will be used for model validation particular to Chapter 5 from the book mentioned on "Prostate Cancer: PSA, AR, and ADT Dynamics". Models include the Swanson, Vollmer and Humphrey, Jackson, and Ideta et al models in the textbook. We may also look at models provided in the references section at the end of the chapter.
M.A. student: Greyson Navarro, California State University San Bernardino.
- Search this Site
- Accessibility
- HHS Vulnerability Disclosure
- U.S. Department of Health and Human Services
- National Institutes of Health
- National Cancer Institute
NIH... Turning Discovery Into Health ®
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley-Blackwell Online Open

Prostate cancer and supportive care: a systematic review and qualitative synthesis of men's experiences and unmet needs
A.j.l. king.
1 Centre for Academic Primary Care, School of Social and Community Medicine, University of Bristol, Bristol, UK
T.H.M. Moore
C. paterson.
2 Urology, Bristol Urological Institute Southmead Hospital, Bristol, UK
A.L. Huntley
Prostate cancer is the second most common cancer in men worldwide, accounting for an estimated 1.1 million new cases diagnosed in 2012 ( www.globocan.iarc.fr ). Currently, there is a lack of specific guidance on supportive care for men with prostate cancer. This article describes a qualitative systematic review and synthesis examining men's experience of and need for supportive care. Seven databases were searched; 20 journal articles were identified and critically appraised. A thematic synthesis was conducted in which descriptive themes were drawn out of the data. These were peer support, support from partner, online support, cancer specialist nurse support, self‐care, communication with health professionals, unmet needs (emotional support, information needs, support for treatment‐induced side effects of incontinence and erectile dysfunction) and men's suggestions for improved delivery of supportive care. This was followed by the development of overarching analytic themes which were: uncertainty, reframing, and the timing of receiving treatment, information and support. Our results show that the most valued form of support men experienced following diagnosis was one‐to‐one peer support and support from partners. This review highlights the need for improved access to cancer specialist nurses throughout the care pathway, individually tailored supportive care and psychosexual support for treatment side effects.
Introduction
Prostate cancer is the second most common cancer in men worldwide, accounting for an estimated 1.1 million new cases diagnosed in 2012 (Globocan, 2012 ). This figure has been rising due to increased use of Prostate Specific Antigen (PSA) testing (Ferlay et al . 2008 ). Men with prostate cancer are likely to have a long illness pathway, and as well as the individual burden to patients, this also represents a burden on healthcare resources. One way of managing this is to provide good supportive care for men which ‘helps the patient and their family to cope with cancer and treatment of it … helps the patient to maximise the benefits of treatment and to live as well as possible with the effects of the disease’ (NICE 2008 ). Supportive care will ideally involve strong elements of self‐care, in order to encourage independence in managing symptoms and side effects (Cockle‐Hearne & Faithfull 2010 ). However, the available guidance on supportive care and self‐management tends to be generic to all cancer patients (NCSI 2013 ).
A recent survey in seven European countries and involving over 1000 men found that 81% of the respondents had some unmet supportive care needs (Cockle‐Hearne et al . 2013 ). These findings echoes earlier surveys in Australia and the UK showing that the areas of greatest need were for psychological distress, sexuality‐related issues and managing of enduring lower urinary tract symptoms (Steginga et al . 2001 ; Ream et al . 2008 ). Other studies highlight the need for the provision of information to patients and carers throughout the disease pathway (Gulavita et al . 2000 ; Sinfield et al . 2009 ). The psychological distress that many men with prostate cancer experience is not always assessed or managed well. A study from Germany looked at adjustment to disease and suggested that up to 20% of patients might benefit from mental health support following prostatectomy (Kohler et al . 2014 ). Research also reveals that post‐treatment care from nurses had a significant positive impact on health outcomes (Cockle‐Hearne et al . 2013 ).
Surveys of unmet need make a case for improving supportive care but an important step is to clarify men's experiences of support using qualitative research methods. Many qualitative studies have been carried out looking at men's experiences of prostate cancer and the impact of the disease on their sense of masculinity (Gray et al . 2002 ; Arrington 2003 ; Maliski et al . 2008 ) but less has been written about men's experiences of supportive care provision. The ideal study design for bringing these data together and creating an overview of men's experiences and needs is to conduct a qualitative systematic review and synthesis.
The parent search strategy was devised and run in Medline and Medline in process ( Appendix 1 ). Modified search strategies based on this search were run in Embase, Psych Info, CINAHL, British Nursing Index, IBSS and Sociological Abstracts. All searches were run from inception to July 2013.
Inclusion and exclusion criteria
Inclusion criteria for full‐text articles were: qualitative studies that included men with a diagnosis of prostate cancer who were undergoing or had undergone any type of standard treatment (including active surveillance) that explored their needs for, attitude toward or experience of supportive care. These qualitative studies included ethnographic and observational studies, involving interviews and focus groups with men with prostate cancer. Two of the studies were longitudinal surveys that included qualitative data. Exclusion criteria were men at risk from prostate cancer, and men in end of life care.
References were screened by title and abstract by two reviewers and differences were resolved by discussion with a third person if necessary, and full articles were obtained that met the above criteria. The reference list of papers retrieved as full text were hand searched and key authors contacted.
Data extraction and synthesis
A thematic synthesis of the evidence in the qualitative papers was conducted, taking an interpretive approach. The reviewers adopted a ‘thematic synthesis’ approach (Thomas & Harden 2008 ). ‘Descriptive themes’ were drawn out of the data followed by the development of ‘analytic themes’ identified by the reviewers. The identification of themes was partly driven by the research question and partly grounded in the data. Data were extracted independently by at least two reviewers using customised forms and any discrepancies were resolved by discussion. All papers were reviewed by AJLK and additional reviewers including co‐authors, members of the advisory group and patients with prostate cancer from a local support group. All included papers were critically appraised independently by two reviewers using the Critical Appraisal Skills Programme quality appraisal tool as an integral part of the systematic review (CASP 2014 ). Disagreements around critical appraisal were resolved by discussion between the reviewers.
Findings were organised into ‘first‐order constructs’ (the verbatim views and experiences of research participants) and ‘second‐order constructs’ (the interpretations of the authors). Patient quotes (‘first‐order constructs’) provide a significant voice of patient experience of supportive care in the analysis and discussion of the secondary qualitative data derived from the review papers. A framework was constructed in Excel with columns for first‐ and second‐order constructs and a row for each article. Members of the research team met to identify and agree consensus on descriptive themes emerging across papers, incorporating all the first‐ and second‐order constructs. The themes were summarised and mapped to show which articles had contributed to each theme. The development of descriptive themes remained very close to the constructs in the primary studies. Overarching analytic themes were subsequently identified, enabling synthesis of themes across studies and the development of new ideas.
The searches yielded 1684 articles excluding duplicates ( Appendix 2 ). Twenty papers describing 20 individual qualitative studies were included in the synthesis, all published between 2004 and 2013 in Europe, the USA, Canada, Australia and the UK (Matsunaga & Gotay 2004 ; Boehmer & Babayan 2005 ; Broom 2005 ; Wallace & Storms 2007 ; Tarrant et al . 2008 ; Milne et al . 2008 ; Oliffe et al . 2009 ; Ream et al . 2009 ; Nanton et al . 2009 ; Ervik et al . 2010 ; O'Brien et al . 2010 ; Walsh & Hegarty 2010 ; Carter et al . 2011 ; Nanton & Dale 2011 ; O'Brien et al . 2011 ; Chambers et al . 2012 ; Galbraith et al . 2012 ; O'Shaughnessy et al . 2013 ; Rivers et al . 2012 ; Thomas 2013 ). Dual critical appraisal revealed that the papers were generally of good quality and none were excluded due to poor quality overall (see Appendix 3 ). Negative scoring on reflexivity and ethical considerations were not sufficient to warrant rejection of individual papers. If the papers had scored poorly on the other criteria, the reviewers would then have conducted a sensitivity analysis (Dixon‐Woods et al . 2007 ). The study characteristics are included in Table 1 .
Study characteristics of review studies
AC: African‐Caribbean; AA: African‐American; A: Asian; W: White; L: Latino; O: Other.
Twelve descriptive themes emerged across the papers. They fall into three groups: (1) prostate cancer patients' experience of supportive care; (2) their accounts of unmet needs; and (3) their suggestions about how to improve supportive care. Table 2 lists the papers that contributed to each of the 12 themes. The reviewers then developed three overarching themes that cut across the 12 descriptive themes. These were uncertainty, reframing and timing.
Reviewers' themes
Authors: (1) Matsunaga and Gotay 2004 ; (2) Boehmer and Babayan 2005 ; (3) Broom 2005 ; (4) Wallace and Storms 2007 ; (5) Tarrant et al . 2008 ; (6) Milne et al . 2008 ; (7) Oliffe et al . 2009 ; (8) Ream et al . 2009 ; (9) Nanton et al . 2009 ; (10) Ervik et al . 2010 ; (11) O'Brien et al . 2010 ; (12) Walsh and Hegarty 2010 ; (13) Carter et al . 2011 ; (14) Nanton and Dale 2011 ; (15) O'Brien et al . 2011 ; (16) Chambers et al . 2012 ; (17) Galbraith et al . 2012 ; (18) O'Shaughnessy et al . 2013 ; (19) Rivers et al . 2012 ; (20) Thomas 2013 .
Prostate cancer patients' experience of supportive care
There were seven themes in this group: peer support, support from church communities, trusted other support, online support, communication with health professionals, the role of the prostate cancer specialist nurse and self‐care. The analysis revealed that men's experience of supportive care was predominantly provided and influenced by informal networks of peer support or ‘trusted others’, and that formal support from health professionals was lacking.
Peer support
This was the most frequent theme to emerge, discussed in 10 of the 20 papers (Table 3 ). Peer support took different forms: support groups led by peers or by health professionals, and one‐to‐one peer support. Men were generally proactive in accessing this kind of support. Three papers described referral or signposting by health professionals (Table 3 ). Wallace and Storms ( 2007 ) describe that one study in which participant was told of support services by his urologist. The other papers referred mainly to one‐to‐one informal peer support found within patients' friendship networks, families, work colleagues, church group or leisure clubs.
I was fortunate in that I knew two or three men who had prostate cancer, so I found it very helpful to talk to them. ( Wallace & Storms 2007 : participant quotation)
Types of peer support
Men's experience of peer support lifted them out of a sense of isolation and enabled them to talk about their illness experience, share information and exchange tips and ideas on dealing with treatment side effects. The reciprocal nature of talking and sharing was experienced as empowering. Galbraith et al . ( 2012 ) describes how it provided a sense of meaning in men's experience of the disease. However, he does not distinguish between informal one‐to‐one support or group support. Matsunaga and Gotay ( 2004 ) highlight the importance of reciprocity in such support. This had a positive effect on helping men to adjust to their diagnosis.
Many participants desired to help others who had been diagnosed and treated for prostate cancer as a way to provide meaningful outcome from their challenges with prostate cancer and its treatment. ( Galbraith et al . 2012 : author quotation) Once you go through the procedure, you feel like you could be of assistance, especially about the operation and what to expect. ( Matsunaga & Gotay 2004 : participant quotation)
The value of peer support was evident at all stages of prostate cancer with diagnosis, treatment decision making and advanced disease being three critical times.
[diagnosis was] such an emotional thing that I needed to be with people who had gone through this or were going through it. ( Wallace & Storms 2007 : participant quotation) Participants felt that the ideal support programme should be made available immediately after diagnosis so that they could literally ‘walk out of the urologist's office and begin to discuss options'. The participants were most interested in meeting with other men with the disease, not a physician or a nurse. ( Wallace & Storms 2007 : author quotation) I finally found a fellow around the corner from me and he came over to my house. We had coffee; we got to be pretty good friends and he kind of sold me on the laparoscopic. ( Milne et al . 2008 : participant quotation)
Being in a mixed group with men at different stages of prostate cancer helped men confront and accept disease progression:
For me, who was newly diagnosed in the middle of treatment, to people who had been diagnosed for 15 or 16 years … it may have been confronting but I didn't find it so because they seemed to be able to cope with it and that was reassuring. ( Chambers et al . 2012 : participant quotation)
Carter's study focuses on men with advanced disease in which men were looking for information rather than emotional support. However, not all men found it useful, and some men stopped going when they felt they were no longer learning new information (Carter et al . 2011 ).
Support accessed within a church community
Two papers referred specifically to peer support accessed through their local church. One paper reports the experience of African‐Caribbean men in the UK (Nanton & Dale 2011 ) and another focuses on African‐American men in the USA (Rivers et al . 2012 ). They recount how participants attended church services more frequently and became more involved in church activities after diagnosis. Their church community facilitated access to other men with prostate cancer from whom patients could get information on diagnosis and treatment. This networking helped some men to ‘find their voice’ and become advocates for others:
… there's been several men within my church and in my community that has … (prostate cancer) … when I found out that he was goin’ through it, I went up … we sat down and talked about it and so it's … it's made me somewhat of an advocate. ( Rivers et al . 2012 : participant quotation)
Support from a partner or ‘trusted other’
Wives, partners, friends and families were described as significant sources of support by men in six papers (Matsunaga & Gotay 2004 ; Boehmer & Babayan 2005 ; Ervik et al . 2010 ; Walsh & Hegarty 2010 ; O'Shaughnessy et al . 2013 ; Rivers et al . 2012 ). Boehmer and Babayan ( 2005 ) coined the phrase ‘trusted other’ in recognition that other key individuals, apart from a spouse, may fulfill this role. Ambivalence was expressed about how much to disclose to close family. Men recognised that family members have their own emotional reactions to cope with. For some men the need to retain their ‘normal’ lifestyle despite their diagnosis was paramount.
… and our son, he doesn't say much, he doesn't show a lot of feelings, but our daughter had a hard time … I don't know maybe men are more tough in such cases … now I have a more open attitude towards illness and that sort of question. Earlier in life, I had a much more tough attitude. … ( Ervik et al . 2010 : participant quotation) I mean I only told my wife and nobody else from the day I was informed … So my lifestyle didn't change one iota … because we didn't want to upset them. We could handle it. ( Walsh & Hegarty 2010 : participant quotation)
Ervik et al . ( 2010 ) stresses the importance of support from spouses but several papers highlight the need for spouses to also receive support. For example, concern was raised about spouses' ongoing ability to adequately care for and support them during and after treatment (Boehmer & Babayan 2005 ; Rivers et al . 2012 ):
Some of the women expressed feeling overwhelmed by the caretaker role. … Some feared how this were to change their relationship, were they cast in the nurse role. ( Boehmer & Babayan 2005 : author quotation)
Online support
The internet was cited as a source of information by men in five studies ( Boehmer & Babayan 2005 ; Wallace & Storms 2007 ; Milne et al . 2008 ; Carter et al . 2011 ; Rivers et al . 2012 ). Milne highlights the need for nurses to guide patients to reliable information sources. One article focuses on the experience of men using online support groups in Australia (Broom 2005 ). Men described how engaging with others online as opposed to face‐to‐face reduced their inhibition; they valued the anonymity in accessing and receiving support and information.
Some men don't want to be face to face. Maybe they're frightened of it … maybe they're scared of being ridiculed … maybe they're a bit anxious about having the problem and not wanting to share it. I think that's men for you. ( Broom 2005 : participant quotation)
Some men took a passive role, observing how others responded to prostate cancer and how they were coping without divulging their own experience. Some men found that the online medium enabled them to distance themselves from their disease.
Communication with health professionals
Several papers describe patients' difficulties in talking to health professionals about important issues early on post diagnosis, when many appeared not to have a clear understanding of PSA testing or what a biopsy is.
I think GPs should make a point of saying what it is about and why it's being done at a particular time. ( Walsh & Hegarty 2010 : participant quotation)
Walsh and Hegarty ( 2010 ) highlight that several men in her study did not feel that their general practitioner (GP) had communicated adequately on what the PSA test was and its significance.
So he came up to me and said he was going to do blood tests the next day. Now no one ever told me not even my GP that the blood test was called a PSA. ( Walsh & Hegarty 2010 : participant quotation)
When looking back at their diagnostic appointment (given in some cases by a hospital consultant, a GP or sometimes by specialist nurses) patients singled out that this was not handled with sufficient sensitivity (Wallace & Storms 2007 ; Nanton & Dale 2011 ). Communication difficulties also continued long term after treatments (Ervik et al . 2010 ; Thomas 2013 ).
Men also reported poor communication with health professionals about the potential severity and duration of side effects of treatment, so patients felt unclear about what to expect (Ream et al . 2009 ; Thomas 2013 ), USA (Galbraith et al . 2012 ), Norway (Ervik et al . 2010 ) and Australia (Broom 2005 ).
Three reasons for this difficulty in communication emerged across papers. First, patients felt unable to talk about changes in sexual function, because for the most part, they were not asked about this at an appropriate time or in a suitable context.
Men can be reluctant to volunteer information on erectile function but generally respond with relief when the question is asked. ( Milne et al . 2008 : author quotation)
Second, men said that they could not easily discuss psychological issues with health professionals owing partly to their experience of a lack of continuity of care.
I think if you saw the same person each time you would probably build up a rapport with that person. But seeing a stranger every time you're thinking ‘oh my God I'm not going to walk in there and start talking about my sex life with someone I've never seen in my life before …. I think I glossed over it [the psychological impact]. ( O'Brien et al . 2011 : participant quotation) It was quite a shock when you go there and it's somebody else … I don't think I spoke about my psychological problems. ( O'Brien et al . 2011 : participant quotation)
Third, men felt that there was a lack of empathy shown by health professionals, leaving then feeling depersonalised.
Cavalier attitudes expressed by the treatment team were disquieting … We were treated liked test subjects, not equals. ( Galbraith et al . 2012 : participant quotation)
This prevalent finding may be summed up by Ervik et al . ( 2010 ) who describe what he calls the ‘ silence of the healthcare system ’. This patient is referring to his follow‐up appointment with a physician:
It is never really time for it … he was not that good with words. ( Ervik et al . 2010 : participant quotation)
Thomas's ( 2013 ) article suggests that participants perceived GPs to be more empathetic than urologists:
In marked contrast to the perception of the urologists, most participants were satisfied with the role of their general practitioner in the prostate cancer journey. The local GPs … were thought to be empathetic to the experiences of the participants. ( Thomas 2013 : author quotation)
Experience of a cancer specialist nurse
Men who had received care from a cancer specialist nurse reported a positive experience of enabling them to discuss non‐medical aspects of their illness (Tarrant et al . 2008 ; Ream et al . 2009 ). This was exemplified by the way nurses communicated the diagnosis (Ream et al . 2009 ) and could act as patient advocates by accessing appropriate care and support. Another key element of the specialist nurse role was in terms of long‐term and ongoing care (O'Shaughnessy et al . 2013 ), and the fact that contact could be initiated by the patient.
… men with prostate cancer would utilize the services of a specialist prostate cancer nurse at all stages of the prostate cancer journey. ( O'Shaughnessy et al . 2013 : author quotation)
Key stages when men valued specialist nurse input was around treatment decision making and treatment choice after initial hormone therapy has failed (O'Shaughnessy et al . 2013 ). Specialist nurses sometimes arranged or referred patients to support groups (Tarrant et al . 2008 ) and played a role in helping men reframe their illness experience in a positive way, enabling better adaptation and coping skills.
She's the link, the liaison and to me the liaison officer, or whatever you want to call it … the surgeon, the consultant is very important but only at a specific time. The one you are relying on most is the (prostate cancer specialist nurse). ( Ream et al . 2009 : participant quotation) It worried me to death..I felt I had to ring (the specialist nurse) … I was asking myself questions I couldn't answer … after I spoke to her I felt a lot better. Oh, I can ring (the specialist nurse) up any time I want to. ( Tarrant et al . 2008 : participant quotation)
Tarrant states that patients who saw a specialist nurse were more likely to have received written information and clear explanations about their tests, treatment options and sources of support (Tarrant et al . 2008 ).
Self‐care
Self‐care is discussed in nine of the papers. Several authors discuss the empowerment and sense of control that comes from self‐care and making lifestyle changes such as diet and exercise.
[By] taking an active part in their own health management [through making changes in their diet and/or exercise] men were taking control of their illness. ( Nanton et al . 2009 : author quotation)
This was particularly true for men with advanced hormone‐resistant cancer who were most likely to have changed their diet and lifestyle (O'Shaughnessy et al . 2013 ).
For the last four years, … eating better, exercising more … and living life more fully. ( O'Shaughnessy et al . 2013 : participant quotation)
Other aspects of self‐care include taking an ‘active problem solving approach’ to illness by, for example, joining a support group (Nanton et al . 2009 ), returning to work or seeking out social and emotional support from family, friendship and faith networks (Rivers et al . 2012 ; Nanton & Dale 2011 ).
Self‐care is particularly important for prostate cancer patients who are under active surveillance. They tried to combine ‘ living a normal life ’ with ‘ doing something extra ’, using strategies similar to men at other stages of disease and treatment such as making dietary or lifestyle changes, and engaging with their partner, family and friends (Oliffe et al . 2009 ; O'Shaughnessy et al . 2013 ). The authors emphasise the significance of men's wives and partners in helping men to make lifestyle changes.
Patients' accounts of unmet supportive care needs
There were three themes in this group: need for emotional support, need for support to deal with treatment side effects, in particular changes in sexual function and urinary incontinence, and need for information. A major concern is the difficulty that men experienced in actually broaching sensitive subjects with health professionals (Milne et al . 2008 ; Ream et al . 2009 ; Ervik et al . 2010 ; Galbraith et al . 2012 ; Thomas 2013 ).
Need for emotional support
Men described their long‐term need for emotional or psychological support, beginning at diagnosis and continuing through treatment into survivorship (Oliffe et al . 2009 ; Ream et al . 2009 ; Ervik et al . 2010 ; O'Brien et al . 2010 ; Galbraith et al . 2012 ; O'Shaughnessy et al . 2013 ; Thomas 2013 ). They felt that there was a lack of understanding by health professionals in primary and secondary care of the emotional impact of prostate cancer particularly in the longer term (Matsunaga & Gotay 2004 ; Boehmer & Babayan 2005 ; Oliffe et al . 2009 ; O'Brien et al . 2010 ; Thomas 2013 ). O'Shaughnessy et al . ( 2013 ) define ‘psychosocial’ needs as men's fears around treatment, anxiety and depression, changes in sexuality, masculinity and relationships. O'Shaughnessy et al . ( 2013 ) and Boehmer and Babayan ( 2005 ) highlight that men's distress and need for psychological support is especially evident when they are first diagnosed and Boehmer and Babayan refer to a later peak of distress if their cancer reoccurs.
The estrangement of men from ‘softer’ psychosocial healthcare services was especially evident in how few ideas or recommendations were offered by the study participants when directly asked about what services and how services might best support them. ( Oliffe et al . 2009 : author quotation)
Carter et al . ( 2011 ) highlight the need for psychological support to be ongoing. O'Brien et al . ( 2010 ) and Galbraith et al . ( 2012 ) talk about the need for support through the psycho‐emotional responses to survivorship.
Participants strongly expressed the need for the health care team to acknowledge their experiences of uncertainty, anger, and grief or loss. ( Galbraith et al . 2012 : author quotation)
Need for support to deal with treatment side effects – changes in sexual function and urinary incontinence
Several of the papers highlighted the need for emotional and psychological support for treatment side effects, primarily urinary incontinence and erectile dysfunction.
The follow‐ups (at the hospital) … have been more concerned with the physical side of things, not the mental side of it … there could have been more emphasis on (that). ( O'Brien et al . 2011 : participant quotation)
O'Brien et al . ( 2011 ) highlight that assessment of psychosexual needs has to take place throughout the follow‐up period, not only at the time of initial treatment, particularly because ‘patients may take time to identify that they have a need for psychosexual support’. O'Brien points out that there may be a role for GPs in assessing wider psychosexual needs and signposting where to get help, and to include patients' partners in this. Galbraith suggests that specialist nurses are in a key position to offer support for men's relational and emotional needs.
Men in several studies expressed a need for information on the severity and duration of incontinence and erectile dysfunction side effects, as well as practical support (Milne et al . 2008 ; Walsh & Hegarty 2010 ; Carter et al . 2011 ; Nanton & Dale 2011 ; O'Brien et al . 2011 ; Thomas 2013 ). Men said they lacked help and support in dealing with these. Difficult reactions to surgery were common:
If I had known what was gonna happen, they'd never have done it … They must have cut muscles and everything. And I'll tell you, your sex life is gone. … I should have been filled in. ( Carter et al . 2011 : participant quotation) Immediately postoperatively the question of impotence doesn't really come into your head … I think it's only later on that you have to … face up psychologically to how you handle that … There's not a lot of counselling form either the primary care or the hospital in terms of the psychological aspect. ( O'Brien et al . 2010 : participant quotation)
Need for information
Information can help empower patients to feel more in control of their disease through increased understanding.
Acquiring knowledge allows patients to be in control because it increases their level of understanding'. He highlights the importance of acquiring first‐hand knowledge from other men with prostate cancer. ( Milne et al . 2008 )
Across the articles, men reported receiving information about prostate cancer and its treatment from a variety of sources including oncologists, urologists, nurses, GPs, cancer charities, the internet, friends and family members. A major and valued source of information is through peer networks (Matsunaga & Gotay 2004 ; Wallace & Storms 2007 ; Milne et al . 2008 ; Walsh & Hegarty 2010 ).
In relation to information from health professionals, there were two issues: content and timing. In Matsunaga and Gotay's ( 2004 ) study, men said that physicians did not give them enough information about treatment options and assumed they understood more than they really did. In three studies (Wallace & Storms 2007 ; Tarrant et al . 2008 ; Nanton et al . 2009 ), men expressed a need for information after diagnosis on what the PSA test was and what changes in it meant, and on appropriateness of treatment and treatment options. Timing was sometimes felt to be inappropriate, e.g. when they received information on treatment side effects, it was often too little too late. As a result, men felt unprepared for the severity and duration of these side effects (Milne et al . 2008 ; Carter et al . 2011 ; Nanton & Dale 2011 ). One study participant highlighted that it is hard to absorb information directly upon diagnosis:
No you can't absorb it and that's in a way one little criticism of (the specialist) nurse … ‘you've got prostate cancer’ … and she carts you off into a tiny little cubicle of a room..and I don't know what the hell she said because … that was too soon. … I was in a state of numbness..at that point and so I don't really know what she was trying to achieve. ( Tarrant et al . 2008 : participant quote) .
The importance of including both men and their partners in information provision on treatment and side effects was highlighted by Rivers et al . ( 2012 ) and O'Shaughnessy et al . ( 2013 ). The ‘need for information’ theme highlights the lack of communication between patients and health professionals particularly in relation to who communicates it, and at what point in the care pathway.
Men's suggestions for improved delivery of supportive care
There were two themes in this group: need for information and need for more time with a specialist cancer nurse (to provide practical, emotional and psychological support). Suggestions were forthcoming from the men themselves, across many articles, as to priority areas for targeting improvements. In terms of information, they suggested making more disease‐related information available at or shortly after diagnosis (Tarrant et al . 2008 ). They also suggested that assistance be provided in interpreting the information (Matsunaga & Gotay 2004 ).
Another suggestion was to make more contact time available with a cancer specialist nurse, particularly after diagnosis and after active treatment (Tarrant et al . 2008 ). Emotional and psychological support for both patients and their partners was flagged up as an important area for improvement (Wallace & Storms 2007 ; Carter et al . 2011 ). Ervik et al . ( 2010 ) stated that when asked directly, half of the men in his study would consider organised counselling if this were an option.
Overarching themes
The reviewers developed overarching analytic themes that cut across the 12 descriptive themes within the papers: uncertainty, reframing and timing of support.
Uncertainty
Men's experience of the prostate cancer pathway was full of uncertainty and anxiety (Milne et al . 2008 ; Oliffe et al . 2009 ; Nanton et al . 2009 ; Ervik et al . 2010 ; O'Brien et al . 2010 ; Walsh & Hegarty 2010 ; Carter et al . 2011 ; Nanton & Dale 2011 ; Galbraith et al . 2012 ; O'Shaughnessy et al . 2013 ; Rivers et al . 2012 ; Thomas 2013 ). Uncertainty was associated with a perceived lack of information provision linked to treatment options and outcomes, about the extent and severity of treatment side effects, and likely prognosis. Uncertainty was particularly pronounced in men under active surveillance (Oliffe et al . 2009 ) particularly around the time leading up to PSA testing, and for those with advanced or recurrent disease (Nanton et al . 2009 ). Even the care pathway seemed to be uncertain for some men who did not fully understand the link between their illness experience and the process of care, for example, not knowing when events in their care were going to take place and who was responsible for particular aspects of their care (Nanton et al . 2009 ).
The theme of ‘reframing’ arises as a means of coping with uncertainty. The term ‘reframing’ was used in two of the articles (Nanton et al . 2009 ; Thomas 2013 ), but the concept was relevant across many more. Galbraith's description of men adapting to a ‘new normal’ is conceptually similar. Reframing can be a positive way whereby patients dealing with uncertainty about a prostate cancer prognosis determine a positive reconstruction of the situation, thus giving mental shape to an uncertain future. Reframing can also help allay unrealistic hopes to return to a pre‐treatment level of functioning (Galbraith et al . 2012 ).
Over half the participants found a new appreciation for living in the ‘Now’ and expressed an appreciation of the love and support of those close to them. There was a re‐evaluation as to what was really important in the lives of a number of these men. ( Thomas 2013 : author quotation)
A participant in this study felt that his diagnosis had given him the opportunity to reframe his sense of his sexuality and of being a gay man.
The process of reappraisal and reframing was evident across all patient groups including older men and whose with advanced disease, although it was harder for patients with metastatic disease (Nanton et al . 2009 ). Reframing can be facilitated by support from an individual or a group. For example, the specialist nurse can play a role in the process:
[the nurse] was instrumental in making me feel positive about everything rather than feeling negative … instead of ‘dying of cancer’ you are ‘living with it. ( Ream et al . 2009 : participant quotation)
Reframing also took place during patients’ experience of a peer support group by using the information they had gained through their illness experience to help others in the group.
… through participation in support group activities for example, anxiety over their own situation was displaced … by the process of doing something useful. … men demonstrated the possibility of a positive response in the face of an uncertain future. ( Matsunaga & Gotay 2004 : author quotation)
Timing of support
A trajectory becomes evident in the included studies, from early information needs to later psychological needs, and ongoing support for psychosexual needs. Many articles portray men as relatively uninformed about prostate cancer before and after their diagnosis, and even post‐treatment in some cases (Wallace & Storms 2007 ; Walsh & Hegarty 2010 ; Nanton & Dale 2011 ). A key time for information provision is between testing and diagnosis and before a consultant appointment. Men reported failing to gain a good understanding of treatment and side effects, their severity and longevity. Information at this stage would help patients to realistically appraise or ‘reframe’ their experience and put plans in place to effectively deal with the consequences of treatment. Diagnosis is inevitably a difficult time and for some men their psychological support needs begin here. It can be difficult to retain information given out at this stage (Thomas 2013 ).
The provision of supportive care must be carefully targeted in terms of its content and the timing of delivery. Men experienced uncertainty, lack of information and poor communication with their medical team about the nature of diagnostic tests, the extent of treatment side effects and the likely progression of the disease. Communication with their medical team about these issues was limited and difficult. This was ameliorated if a specialist nurse was in the team. Some of the uncertainty experienced by men reflected inherent problems in treating prostate cancer, such as the uncertainty around disease progression and clinical equipoise around treatments.
There appears to be a strong link between patients' need for information and individual levels of uncertainty. Information to ameliorate uncertainty and its consequent anxiety was not forthcoming, and men reported a lack of information about any support that might be available. Men received most of their information and support from peer groups or individuals but not all managed to access these resources.
Uncertainty as a theme has emerged in previous studies of prostate cancer patients where it has been shown to ‘adversely influence patients' and their spouses’ quality of life (Bailey et al . 2007 ; Shaha et al . 2008 ). Some men deal with uncertainty by focusing their attention on their work life or engaging in self‐care strategies, such as using complementary medicines (Bailey et al . 2007 ). Uncertainty also emerges as a theme in the literature of health and illness more widely. Mishel ( 1990 ) defines uncertainty as ‘ the inability to determine the meaning of illness‐related events. It is a cognitive state created when the individual cannot adequately structure or categorize an illness because of insufficient cues ’. Mishel proposes that managing uncertainty is critical to adapting to illness and that people cognitively process events linked to illness and construct meaning from them. Uncertainty is reappraised over time; it may not be resolved but may become part of people's reality (Mishel 1990 ; Bailey et al . 2007 ). Open discussion between patients and health professionals in a one‐to‐one or group setting may facilitate this process. This theme highlights the need for individual assessment of levels of uncertainty and coping in patients, in order for health professionals to identify areas of need, support and information for patients and families.
Reframing is one possible way of supporting men with prostate cancer around uncertainty. There is a link between reframing and self‐care in that some men in the studies (Milne et al . 2008 ; O'Shaughnessy et al . 2013 ) who felt an overwhelming need to regain control of their lives by returning to pre‐operative activities, and a need to develop a renewed sense of self. The wider literature on prostate cancer also discusses peoples' experience of reframing their illness experience (Lepore & Helgeson 1998 ; Bailey et al . 2007 ). In discussing the reframing process, Bailey et al . ( 2007 ) refers to cognitive reframing, which helps men as ‘ they attempt to incorporate the experience of prostate cancer and watchful waiting in to their life structure ’. Bailey highlights the importance of positive appraisal of the disease in order to enhance quality of life and stresses the ways in which nurses can help men with prostate cancer with this process. This review reveals that men can experience reframing of their illness experience directly for themselves or be encouraged to do this by health professionals in a more formal context (referred to in the wider literature as cognitive reframing (Bailey et al . 2007 ).
Information on the process of care, the timing of events and treatment and responsibility for care has also been highlighted as an unmet need (Nanton et al . 2009 ). To facilitate the delivery and retention of information, the presence of a partner or ‘trusted other’ at the appointment could be encouraged; information could be given in written form and reinforced at subsequent appointments along the disease pathway, for example by a specialist nurse (Tarrant et al . 2008 ). While some men need specialised support such as psycho‐sexual counseling, for many men peer support meets their needs.
Strengths and limitations to the study
The strengths of this study are that it is to our knowledge the first qualitative review and synthesis to be conducted on the experience of, and need for supportive care for men with prostate cancer in the literature and uses rigorous systematic review and qualitative synthesis methodology. Thematic synthesis was chosen as it addresses questions of intervention need, appropriateness and acceptability.
A limitation of this review was that articles focusing specifically on diagnosis and treatment decision making were excluded from this review. The included review papers were predominantly from North America so the authors' findings may not be universally applicable. The overall quality of the papers was good and contributed significantly to the discussion on prostate cancer and supportive care. The review identifies that there are few papers on the experience of men from minority ethnic groups, single men and gay men, highlighting a need for future research with these populations.
Conclusions
The review concludes that the most valued form of support men with prostate cancer experience is one‐to‐one peer support and support from partners. The review also shows that men perceive support groups to have two different roles, that of information giving (particularly when health professional led) and emotional sharing (peer led). Some men indicated the need following diagnosis to be referred by health professionals to one‐to‐one peer support, or to local support groups. This review also highlights the need for improved access to cancer specialist nurses throughout the care pathway, individually tailored supportive care and psychosexual support for treatment side effects.
Implications for Practice
There is a need for more timely and accurate information and resources to help manage daily living impacted by treatment side effects. For some men, this may translate into a need for access to psychosexual and specialist support.
Positive experiences with health professionals were considered to improve health outcomes. The practice implications of this study's findings are the need to improve access to cancer specialist nurses at key points in men's disease progression and care pathway.
Men in the included studies indicated a need for individually tailored care packages based on needs and changing needs.
There is also a need for healthcare professionals to acknowledge patients' uncertainty, and emotional responses in dealing with prostate cancer.
Health professionals also need to encourage self‐care of patients with prostate cancer and their partners, and to provide information and support to encourage this.
In view of the significant role played by partners, there is a need for health professionals to acknowledge the ‘care burden’ on partners/significant others and provide access to support.
Acknowledgements
The authors would like to acknowledge the role and work of the research advisory group (David Gillatt, John Graham, Alice Malpass and Bristol Prospect members: Malcolm Gamlin, Richard Firth, Geoff Perkins and Paul Williams). This study was supported by a NIHR RFPB grant (National Institute of Health Research, Research for Patient Benefit).
Biographies
Anna J.L. King is a research associate in the Centre of Academic Primary Care, School of Social and Community Medicine, University of Bristol. Her research interests lie in patient experience of health services, evaluation of health and social care, and involving patients in research.
Maggie Evans is a research fellow at the Centre of Academic Primary Care, School of Social and Community Medicine, University of Bristol. She specialises in qualitative work with a research focus on the supportive care needs of patients with cancer.
Theresa H.M. Moore is a research associate in the School of Social and Community Medicine, University of Bristol. Her experience lies in systematic reviews of interventions for treating or preventing disease.
Charlotte Paterson is an honorary senior research fellow, an experienced general practitioner and is currently training in acupuncture and Chinese medicine. Charlotte has a keen interest in methodology and experience of both qualitative and quantitative methods, including qualitative synthesis using meta‐ethnography.
Debbie Sharp is professor of Primary Health Care in the Centre of Academic Primary Care in the University of Bristol. She has had a long‐standing research interest in Complementary and Alternative Medicine, obtaining grant funding from a wide variety of sources and supervising higher degrees in this area.
Raj Persad is director of Oncology Studies at The Bristol Urological Institute and honorary professor at UWE. He is senior consultant urological surgeon in Bristol at North Bristol NHS Trust and a senior clinical lecturer at the University of Bristol. He is also honorary professor of Medicine at Pittsburgh University, USA, and member of the National Prostate Cancer Audit Clinical Reference Group.
Alyson Huntley is a research fellow in the Centre of Academic Primary care in the University of Bristol. She is an experienced systematic reviewer, and her research interests lie in the relationship of primary health care and the reduction of unscheduled secondary care, and supportive care interventions for patients with cancer.
Appendix 1 Medline Search Strategy run J uly 2013
Appendix 2 prisma flow chart of review.

Appendix 3 Critical Appraisal Skills Programme (CASP) evaluation of included studies
King A.J.L., Evans M., Moore T.H.M., Paterson C., Sharp D., Persad R. & Huntley A.L. (2015) European Journal of Cancer Care 24 , 618–634 Prostate cancer and supportive care: a systematic review and qualitative synthesis of men's experiences and unmet needs [ PMC free article ] [ PubMed ] [ Google Scholar ]
National Institute of Health Research grant, Research for Patient Benefit (RFPB code: PB‐PG ‐111‐26018)
- Arrington M. (2003) ‘I don't want to be an artificial man’: narrative reconstruction of sexuality among prostate cancer survivors . Sexuality and Culture 7 , 30–58. [ Google Scholar ]
- Bailey D.E., Wallace M. & Mishel M.H. (2007) Watching, waiting and uncertainty in prostate cancer . Journal of Clinical Nursing 16 , 734–741. [ PubMed ] [ Google Scholar ]
- Boehmer U. & Babayan R.K. (2005) A pilot study to determine support during the pre‐treatment phase of early prostate cancer . Psycho‐Oncology 14 , 442–449. [ PubMed ] [ Google Scholar ]
- Broom A. (2005) The eMale. Prostate cancer, masculinity and online support as a challenge to medical expertise . Journal of Sociology 41 , 87–104. [ Google Scholar ]
- Carter R., Bryant‐Lukosius D., DiCenso A., Blythe J. & Neville A.J. (2011) The supportive care needs of men with advanced prostate cancer . Oncology Nursing Forum 38 , 189–198. [ PubMed ] [ Google Scholar ]
- CASP (2014) Critical Appraisal Skills Programme . Available at: www.brookes.ac.uk/services/upgrade/study‐skills/critical‐appraisal.html . Accessed October 2014.
- Chambers S.K., Foley E., Galt E., Ferguson M. & Clutton S. (2012) Mindfulness groups for men with advanced prostate cancer: a pilot study to assess feasibility and effectiveness and the role of peer support . Supportive Care in Cancer 20 , 1183–1192. [ PubMed ] [ Google Scholar ]
- Cockle‐Hearne J. & Faithfull S. (2010) Self‐management for men surviving prostate cancer: a review of behavioural and psychosocial interventions to understand what strategies can work, for whom and in what circumstances . Psycho‐Oncology 19 , 909–922. [ PubMed ] [ Google Scholar ]
- Cockle‐Hearne J., Charnay‐Sonnek F., Denis L., Fairbanks H.E., Kelly D., Kav S., Leonard K., Muilekom E., van Fernandez‐Ortega P., Jensen B.T. & Faithfull S. (2013) The impact of supportive nursing care on the needs of men with prostate cancer: a study across seven European countries . British Journal of Cancer 109 , 2121–2130. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dixon‐Woods M., Sutton A., Shaw R., Miller T., Smith J., Young B. et al (2007) Appraising qualitative research for inclusion in systematic reviews: a quantitative and qualitative comparison of three methods . Journal of Health Services Research and Policy 12 , 42–47. [ PubMed ] [ Google Scholar ]
- Ervik B., Nordoy T. & Asplund K. (2010) Hit by waves – living with local advanced or localised prostate cancer treated with endocrine therapy or under active surveillance . Cancer Nursing 33 , 382–389. [ PubMed ] [ Google Scholar ]
- Ferlay J., Parkin D.M. & Steliarova‐Foucher E. (2008) Estimates of cancer incidence and mortality in Europe in 2008 . European Journal of Cancer 46 , 765–781. [ PubMed ] [ Google Scholar ]
- Galbraith M., Hays L. & Tanner T. (2012) What men say about surviving prostate cancer: complexities represented in a decade of comments . Clinical Journal of Oncology Nursing 16 , 65–72. [ PubMed ] [ Google Scholar ]
- Globocan . (2012) Globocan World Cancer Statistics . Available at: http://globocan.iarc.fr/Pages‐fact‐sheets‐cancer.aspx . Accessed October 2014.
- Gray R.E., Fitch M.I., Fergus K.D., Mykhalovskiy E. & Church K. (2002) Hegemonic masculinity and the experience of prostate cancer: a narrative approach . Journal of Aging and Identity 7 , 43–62. [ Google Scholar ]
- Gulavita S., Sinnott C., Setliff A.E. & Sellick S.M. (2000) Short report: what do men with prostate cancer want to know? Canadian Family Physician 46 , 1769–1771. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kohler N., Friedrich M., Gansera L., Holze S., Thiel R., Roth S., Rebmann U., Stolzenburg J.U., Truss M.C., Fahlenkamp D., Scholz H.‐J. & Brahler E. (2014) Psychological distress and adjustment to disease in patients before and after radical prostatectomy. Results of a prospective multi‐centre study . European Journal of Cancer Care , 23 , 795–802. doi: 10.1111/ecc.12186 . [ PubMed ] [ Google Scholar ]
- Lepore S.J. & Helgeson V.S. (1998) Social constraints, intrusive thoughts, and mental health after prostate cancer . Journal of Social and Clinical Psychology 17 , 89–106. [ Google Scholar ]
- Maliski S.L., Rivera S., Connor S., Lopez G. & Litwin M.S. (2008) Renegotiating masculine identity after prostate cancer treatment . Qualitative Health Research 18 , 1609–1620. [ PubMed ] [ Google Scholar ]
- Matsunaga D.S. & Gotay C.C. (2004) Characteristics contributing to an enduring prostate cancer support group in an Asian and Pacific islander community . Journal of Psychosocial Oncology 22 , 1–29. [ Google Scholar ]
- Milne J., Spiers J.A. & Moore K.N. (2008) Men's experiences following laparoscopic radical prostatectomy: a qualitative descriptive study . International Journal of Nursing Studies 45 , 765–774. [ PubMed ] [ Google Scholar ]
- Mishel M.H. (1990) Reconceptualization of the uncertainty in illness theory . Image–the Journal of Nursing Scholarship 22 , 256–262. [ PubMed ] [ Google Scholar ]
- Nanton V. & Dale J. (2011) It don't make sense to worry too much’: the experience of prostate cancer in African‐Caribbean men in the UK . European Journal of Cancer Care 20 , 62–71. [ PubMed ] [ Google Scholar ]
- Nanton V., Docherty A., Meystre C. & Dale J. (2009) Finding a pathway: information and uncertainty along the prostate cancer patient journey . British Journal of Health Psychology 14 , 437–458. [ PubMed ] [ Google Scholar ]
- NCSI (2013) Living with and Beyond Cancer: Taking Action to Improve Outcomes . NHS National Cancer Survivorship Initiative. Available at: http://www.ncsi.org.uk/wp‐content/uploads/Living‐with‐and‐beyond‐2013.pdf
- NICE (2008) Guidelines on Supportive and Palliative Care in Cancer Services . Available at: http://www.nice.org.uk/nicemedia/live/10893/28820/28820.pdf
- O'Brien R., Rose P., Campbell C., Weller D., Neal R.D., Wilkinson C., McIntosh H. & Watson E. (2010) Experiences of follow‐up after treatment in patients with prostate cancer: a qualitative study . BJU International 106 , 998–1003. [ PubMed ] [ Google Scholar ]
- O'Brien R., Rose P., Campbell C., Weller D. & Watson E. (2011) I wish I'd told them’: a qualitative study examining the unmet psychosexual needs of prostate cancer patients during follow‐up after treatment . Patient Education and Counselling 84 , 200–207. [ PubMed ] [ Google Scholar ]
- Oliffe J.L., Davison J., Pickles T. & Mroz L. (2009) The self‐management of uncertainty among men undertaking active surveillance for low‐risk prostate cancer . Qualitative Health Research 19 , 432–443. [ PubMed ] [ Google Scholar ]
- O'Shaughnessy P.K., Laws T.A. & Ester man A.J. (2013) The Prostate Cancer Journey. Results of an online survey of men and their partners . Cancer Nursing 1 , 1–12. [ PubMed ] [ Google Scholar ]
- Ream E., Quennell A., Fincham L., Faithfull S., Khoo V., Wilson‐Barnett J. & Richardson A. (2008) Supportive care needs of men living with prostate cancer in England: a survey . British Journal of Cancer 98 , 1903–1909. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ream E., Wilson‐Barnett J., Faithfull S., Fincham L., Khoo V. & Richardson A. (2009) Working patterns and perceived contribution of prostate cancer clinical nurse specialists: a mixed method investigation . International Journal of Nursing Studies 46 , 1345–1354. [ PubMed ] [ Google Scholar ]
- Rivers B., August E.M., Quin G.P., Gwede C.K., Pow‐Sang J.M., Green B.L. & Jacobsen P.B. (2012) Understanding the Psychosocial Issues of African American Couples Surviving Prostate Cancer . Journal of Cancer Education 27 , 546–558. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shaha M., Cox C., Talman K. & Kelly D. (2008) Uncertainty in breast, prostate and colorectal cancer: implications for supportive care . Journal of Nursing Scholarship 40 , 60–67. [ PubMed ] [ Google Scholar ]
- Sinfield P., Baker R., Camosso‐Stefinovic J., Colman A.M., Tarrant C., Mellon J.K., Steward W., Kockelbergh R. & Agarwal S. (2009) Men and carers’ experience of care for prostate cancer: a narrative literature review . Health Expectations: An International Journal of Public Participation in Health Care and Health Policy 12 , 301–312. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Steginga S.K., Occhipinti S., Dunn J., Gardiner R.A., Heathcote P. & Yaxley J. (2001) The supportive care needs of men with prostate cancer . Psycho‐Oncology 10 , 66–75. [ PubMed ] [ Google Scholar ]
- Tarrant C., Sinfield P., Agarwal S. & Baker R. (2008) Is seeing a specialist nurse associated with positive experiences of care? The role and value of specialist nurses in prostate cancer care . BMC Health Services Research 8 , 65. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Thomas C. (2013) The experiences of gay and bisexual men diagnosed with prostate cancer: results from an online focus group . European Journal of Cancer Care 22 , 522–529. [ PubMed ] [ Google Scholar ]
- Thomas J. & Harden A. (2008) Methods for the thematic synthesis of qualitative research in systematic reviews . BMC Medical Research Methodology 8 , 45 Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2478656/ [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wallace M. & Storms S. (2007) The needs of men with prostate cancer: results of a focus group study . Applied Nursing Research 20 , 181–187. [ PubMed ] [ Google Scholar ]
- Walsh E. & Hegarty J. (2010) Men's experiences of radical prostatectomy as treatment for prostate cancer . European Journal of Oncology Nursing 14 , 125–133. [ PubMed ] [ Google Scholar ]
A monthly newsletter from the National Institutes of Health, part of the U.S. Department of Health and Human Services
Search form
Print this issue
Health Capsule
Comparing Side Effects of Prostate Cancer Treatments

Prostate cancer is the most common cancer for men in the United States. Luckily, most men with prostate cancer will still be alive 15 years after diagnosis.
Men with prostate cancer that hasn’t spread outside the gland have several treatment choices. These include surgery, radiation therapy, and active surveillance, where treatment is delayed until a cancer starts to grow.
Men live a similar length of time regardless of the chosen treatment. But it’s been unclear if there were significant differences in the long-term side effects of these treatments. Side effects can include bladder and bowel problems, and difficulty with sexual functioning.
To learn more, researchers followed 2,500 men for 10 years after prostate cancer treatment. As expected, survival rates were similar. But the long-term side effects differed depending on the treatment.
Men who had surgery had a higher risk of leaking urine. But men who had radiation therapy had a higher risk of bowel problems. Certain men had a higher risk of sexual problems soon after surgery. But by 10 years, no significant differences were found between the treatment groups.
“Given the similar survival rates, the choice of treatment for patients may be influenced by the adverse effects of the treatments,” says Dr. Bashir Al Hussein Al Awamlh, of Vanderbilt University, who helped lead the study.
Related Stories

Testing an mRNA Vaccine to Treat Pancreatic Cancer

Stop Smoking Early To Improve Cancer Survival

Advances in Childhood Cancer

Are You Overdue for a Cervical Cancer Screening?
NIH Office of Communications and Public Liaison Building 31, Room 5B52 Bethesda, MD 20892-2094 [email protected] Tel: 301-451-8224
Editor: Harrison Wein, Ph.D. Managing Editor: Tianna Hicklin, Ph.D. Illustrator: Alan Defibaugh
Attention Editors: Reprint our articles and illustrations in your own publication. Our material is not copyrighted. Please acknowledge NIH News in Health as the source and send us a copy.
For more consumer health news and information, visit health.nih.gov .
For wellness toolkits, visit www.nih.gov/wellnesstoolkits .
My life was in danger when I was a federal agent working undercover to bust those who laundered millions of dollars for drug kingpins. My work made enemies who wanted me dead. So it was with some dread that I met last year with a highly reliable source, who confirmed I had once again become the target of one of the world’s deadliest killers. But this time, it wasn’t a Colombian drug lord. It was cancer.
The reliable source, my urologist, picked up on some red flags that are often ignored by other physicians. Thankfully, he identified this latest hit man at an early stage and in sufficient time for me to do as I’ve always done, conduct an intense study about the challenge confronting me and determine the best plan of action to attack it. I am sharing some general details about this journey in hopes that the research I conducted can be a resource for the nearly 1.5 million men per year, worldwide, diagnosed with prostate cancer. My goal is to be a tiny part of helping cancer victims from becoming a part of the unfortunate reality that roughly 375,000 men around the globe die from prostate cancer annually.
For those of you confronted with this challenge, please know that I’m happy to privately communicate directly with you in much greater detail about what I think I’ve learned about this killer. My many months of research opened my eyes to an array of tests that revealed important facts, helping me identify my best course of treatment. Additional fact-finding opened my eyes to the best qualifications of members on my treatment team, the significant number of different types of equipment used to deliver treatment to patients and the various protocols followed by radiation oncologists to treat this form of cancer. You may hear otherwise from some health care professionals, but my research and experience convinced me that treatment is definitely not one size fits all.
Initially, I read everything I could find about treatment options. Step 2 involved my reaching out to many friends and contacts who had been down this road before. Getting insight from them about their journey opened my eyes further to the vastly different methods of treating prostate cancer. Armed with the results of the first two steps, I identified the top three cancer centers I felt had the best reputation, personnel and equipment to lead me through this battle.
I visited each of those cancer centers and met with their prostate oncology teams, including the specific radiation oncologist at each center that, depending on my choice, would direct my treatment. I interviewed each team, learned the treatment protocols they felt were best for me and questioned them about why their protocols, in some instances, didn’t include certain methodologies I learned were employed at other radiation oncology centers that specialized in prostate cancer treatment.
My analysis led me to a specific course of treatment at the MD Anderson Cancer Center in Houston, where I just completed world-class care from an amazing team of radiation oncologists, radiation therapists, physicists and other health care professionals. Not everyone can get to Houston for treatments. Fortunately, there are cancer centers and oncology groups around the world that embrace the protocols I came to know are delivered at MD Anderson.
Spend your days with Hayes
Subscribe to our free Stephinitely newsletter
You’re all signed up!
Want more of our free, weekly newsletters in your inbox? Let’s get started.
With the help of the talented and caring radiation oncologist Dr. Quynh-Nhu Nguyen and her team, I learned details about their unique individualized approach to treatment. They recognize that many “patient unique” factors impact the formulation of the most effective treatment plan. Your age, general health, the stage of your cancer, the aggressiveness of your cancer cells, the condition of your prostate, the condition of your urinary tract, the state of organs and tissue in close proximity to your prostate, your prior medical history, family medical history and much more all play into determining optimal treatment protocol.
So, my friends, if you should find yourself in a battle with prostate cancer, please know that I’m here to share my research and thoughts with you. You’ll get wonderful advice from many different professional groups that deliver cancer treatment, but from a patient’s perspective, I’m ready to extend a helping hand of patient insight and support. I owe so much to so many people who have guided me through a course of treatment that is likely to enable me to achieve a cancer-free life. It would be a privilege to help you in your time of need.
Contact Robert Mazur at his website, RobertMazur.com . A federal agent for 27 years, Mazur is a court-certified expert in money laundering-related matters in both the U.S. and Canada. He is the New York Times bestselling author of “The Infiltrator,” a memoir about the first half of his life undercover as a money launderer within Pablo Escobar’s Medellin Cartel, and was an executive producer of the film by the same name. His latest book, “The Betrayal,” is a memoir about his final undercover assignment, a deep dive into Colombia’s Cali Cartel and Panama’s underworld that nearly cost him his life. He is president of KYC Solutions, a company that provides speaking, training, consulting and expert witness services globally.
MORE FOR YOU
- Advertisement
ONLY AVAILABLE FOR SUBSCRIBERS
The Tampa Bay Times e-Newspaper is a digital replica of the printed paper seven days a week that is available to read on desktop, mobile, and our app for subscribers only. To enjoy the e-Newspaper every day, please subscribe.
- Open access
- Published: 04 August 2022
Urinary symptoms and prostate cancer—the misconception that may be preventing earlier presentation and better survival outcomes
- Vincent J. Gnanapragasam 1 , 2 , 3 ,
- David Greenberg 4 &
- Neil Burnet 5
BMC Medicine volume 20 , Article number: 264 ( 2022 ) Cite this article
8951 Accesses
7 Citations
1365 Altmetric
Metrics details
Prostate cancer is an epidemic of the modern age, and despite efforts to improve awareness, it remains the case that mortality has hardly altered over the decades, driven largely by late presentation. There is a strong public perception that male urinary symptoms is one of the key indicators of prostate cancer, and this continues to be part of messaging from national guidelines and media health campaigns. This narrative, however, is not based on evidence and may be seriously hampering efforts to encourage early presentation.
Anatomically, prostate cancer most often arises in the peripheral zone, while urinary symptoms result from compression of the urethra by prostatic enlargement more centrally. Biopsy studies show that mean prostate volume is actually lower in men found to have (early) prostate cancer compared to those with benign biopsies. This inverse relationship between prostate size and the probability of cancer is so strong that PSA density (PSA corrected for prostate volume) is known to be significantly more accurate in predicting a positive biopsy than PSA alone. Thus, this disconnect between scientific evidence and the current perception is very striking. There is also evidence that using symptoms for investigating possible cancer may lead to higher proportions of men presenting with locally advanced or metastatic disease compared to PSA testing or screening programmes. Concerns about overwhelming health care services if men are encouraged to get tested without symptoms may also be overstated, with recent newer approaches to reduce over-investigation and treatment. In this article, we explore the link between urinary symptoms and prostate cancer and propose that public and professional messaging needs to change.
If rates of earlier diagnosis are to improve, we call for strong clear messaging that prostate cancer is a silent disease especially in the curable stages and men should come forward for testing regardless of whether or not they have symptoms. This should be done in parallel with other ongoing efforts to raise awareness including targeting men at highest risk due to racial ancestry or family history. While the current resurgence in interest and debate about prostate cancer screening is timely, change of this message by guideline bodies, charities and the media can be a first simple step to improving earlier presentation and hence cures rates.
Peer Review reports
Key message
Waiting for troublesome lower urinary tract symptoms as a trigger to see a GP about prostate cancer may potentially delay earlier diagnosis and management.
There is no evidence of a causal link between prostate cancer and either prostate size or troublesome male urinary symptoms. In fact, most evidence points to an inverse correlation.
Modern image-based diagnostics and risk-adapted management strategies have reduced the risks of over-investigation and over-treatment which previously deterred greater promotion of PSA testing in men with no symptoms.
It is now timely to re-brand early, curable prostate cancer as primarily an asymptomatic disease to encourage more men to come forward and get tested earlier.
There is a strong public perception that male urinary symptoms are a sign of prostate cancer. Yet, this notion is not borne out by the scientific evidence. Research over the last 30 years has consistently found no direct relationship between symptoms and prostate cancer. Despite this, the link between urinary symptoms and prostate cancer continues to be reinforced by national guidelines and media health promotion messaging. In this article, we review the scientific evidence base and how this perceived causative association may actually deter men from coming forward for early testing and detection of treatable cancer.
Prostate cancer—still a disease of late presentation and unchanged mortality rates
Prostate cancer is without a doubt a disease epidemic of the modern age. Although first described histologically only in 1853, as a single case report, today, it is actually the most common male cancer in the western world today and a major cause of morbidity and mortality [ 1 , 2 ]. The annual incidence is over 52,000 cases, and there are almost 12,000 deaths each year, 7% of all cancer deaths ( https://www.cancerresearchuk.org/about-cancer/prostate-cancer/symptoms ). Although considered typically a disease of older age, more than a quarter of cases occur before current retirement age. Despite significant recent advances in treatment, over the last decade, the proportion of men dying of prostate cancer has hardly altered in the UK and many countries, driven largely by late presentation of the disease. In England, for example, nearly half of all prostate cancers present as stage 3 or 4 ( https://www.npca.org.uk/content/uploads/2021/01/NPCA-Annual-Report-2020_-Infographic-140121.pdf/ ). On the face of it, it would seem that screening should also be introduced to reduce prostate cancer mortality, and this has been robustly debated over many years [ 3 ]. The converse argument is that this may result in many men being unnecessarily investigated and treated for likely indolent disease. As a result, outside of North America, few PSA-based testing programs have been introduced internationally. Recently, there has been a resurgence of interest in screening methods, particularly with the advent of prostate MRI which has shown high negative predictive values, thus reducing the numbers of men who proceed to biopsy [ 4 ]. Nevertheless, it remains to be seen if proposed new approaches (e.g. targeted genetic testing, MR imaging) will fulfil the Wilson and Jungner criteria for a screening programme [ 5 , 6 , 7 , 8 ]. In the meantime, it is important to consider how men currently seek advice about suspected prostate cancer, the recommendations in terms of testing and whether these remain fit for purpose.
Male urinary symptoms and prostate cancer—causality, association or no link at all?
For decades, the recommendation has been to use symptoms to look for possible cancer, in particular lower urinary tract symptoms (LUTS). Yet, the origins and evidence for this linkage are hard to uncover. ‘Urinary symptoms as a sign of prostate cancer’ is often part of the thrust of messages from the media and is included in information from national guidelines and charities as a means to encourage men to get tested ( https://www.nhs.uk/conditions/prostate-cancer/symptoms , https://www.cancercenter.com/cancer-types/prostate-cancer/symptoms , https://www.verywellhealth.com/symptoms-of-prostate-cancer-2782274 ). Although many information and official sites do mention that most prostate cancers may not cause symptoms, they do still very prominently list a number of urinary symptoms to look out ( https://www.nhs.uk/conditions/prostate-cancer/symptoms , https://www.cancercenter.com/cancer-types/prostate-cancer/symptoms , https://www.verywellhealth.com/symptoms-of-prostate-cancer-2782274 ). This is based on the notion that prostate cancer may manifest with symptoms such as slow urinary flow, frequency or nocturia which should trigger a visit to the GP for testing to exclude cancer. Indeed, the UK National Institute for Health and Care Excellence (NICE) makes a distinction between patients with and without symptoms in how to manage suspected prostate cancer, for example recently reviewing the evidence base for PSA thresholds, but only in the ‘symptomatic’ population [ 9 ]. Much of the basis for this distinction has come from studies in primary care-based referral practices of symptomatic men. The widely used QCancer® tool was developed using data from over 2 million men presenting to GPs. For prostate cancer, urinary retention, frequency, urgency and impotence were considered predictors of a diagnosis. However, PSA is not part of the model and there is no detail on the stage of cancers found through this route [ 10 ]. Staying with primary care, in an analysis piece from 2018, Just et al. debated the use of PSA in men presenting with urinary symptoms and pointed out the lack of evidence of its utility in cancer detection and that in fact current practice may lead to over-diagnosis of indolent cancers [ 11 ]. More recently. Koo et al. [ 12 ], as part of a wider study of primary care-detected malignancy, analysed a cohort of 1135 men who saw their GP for LUTS and were subsequently diagnosed with prostate cancer. In this sub-group, they reported that in diagnosed men nearly 20% already had stage IV, i.e. metastatic disease. This rate is much higher than in men investigated through a raised PSA route and also higher than the national overall rate of metastatic disease in men diagnosed through any route (Table 1 ) ( https://www.npca.org.uk/content/uploads/2021/01/NPCA-Annual-Report-2020_-Infographic-140121.pdf/ ). There are no direct comparison studies of detection rates and stage differences in PSA-detected versus symptom-detected cancers. So, is there evidence of a causal link between urinary symptoms and prostate cancer and to justify managing men differently?
Prostate cancer and gland size
Bladder outlet obstruction (most often due to benign prostate enlargement) and its symptomatic manifestations, difficulty with flow, hesitancy, nocturia and poor stream, are the most common symptoms taking a man to his GP and leading to a PSA test. The relationship between prostate size and cancer has been extensively explored since the earliest days of routine PSA and biopsies. Karakieweiz et al. were amongst the first to report that mean prostate volume was lower in men found to have prostate cancer compared to those with benign biopsies [ 15 ]. Since then, other studies have reported identical findings. In a meta-analysis compiled by Moolupuri et al., 28 out of 30 studies showed a clear inverse relationship between prostate size and the chance of finding prostate cancer at biopsy [ 16 ]. The remaining 2 studies were equivocal and none showed a positive correlation. This relationship is so strong that the PSA density (PSA corrected for prostate volume) is now well known to be significantly more accurate than PSA in predicting a positive biopsy and is used in everyday clinical practice [ 17 ]. In an elegant computer simulation, Lorenzo et al. postulated that an enlarged prostate could in fact cause mechanical suppression of tumour growth, which may explain the inverse size relationship with cancer detection [ 18 ]. One caveat is that many of these studies were done before pre-biopsy MRI imaging to target biopsies (as in modern pathways) and tumours may have been harder to find in larger prostates. However, a recent study from our own unit has identified that size-cancer relationship remained the same (inverse) in men investigated by MRI-guided biopsies [ 19 ].
Lower urinary tract symptoms (LUTS) and prostate cancer
Overall size alone of course does not explain all lower urinary tract symptoms. Anatomically, early stage cancer should not be expected to cause urinary symptoms. The most common site for malignancy (70%) is in the peripheral zone, while urinary symptoms as a result of (benign) prostatic enlargement occur because of growth of the transitional and central zones. The origins of a causal linkage between LUTS and cancer are hard to uncover but likely relate to the pre-PSA era before formal studies on this topic [ 20 ]. One of the only large epidemiological studies to report an association was the HUNT 2 study (conducted between 1995 and 2007 in Norway). But even this study found a paradoxical link with localised, but not advanced or fatal, prostate cancer [ 21 ]. The authors concluded that urinary symptoms were not caused by prostate cancer and that screening for early cancers on the basis of urinary symptoms was not justified. There is more recent level 1 data from randomised controlled screening trials about LUTS and prostate cancer. Nearly 10 years ago, the Gothenburg screening trial investigated the incidence of urinary symptoms and detection of cancer in men with a raised PSA (using a threshold of ≥ 3 ng/ml) [ 22 ]. Not only did they not find an association but they observed an inverse relationship between symptoms and the chance of a positive biopsy. More recently, the UK PROTECT trial also looked in detail at the LUTS scores that men reported: for every domain of urinary score there was either no association or a negative association with more severe symptoms and prostate cancer [ 23 ]. The authors concluded that a lack of urinary symptoms may in fact be an indicator of a higher likelihood of cancer. These and many other similar studies provide quite convincing evidence that LUTS and prostate cancer are not positively linked, may in fact be inversely associated, and when present are more likely to be (at most) co-incidental [ 24 , 25 ].
An urgent need to change the message
So where does this leave the notion of prostate cancer as a ‘symptomatic disease’? The idea that LUTS and cancer are causally associated is so strong that in a study looking at population-based awareness, 86% of the public associated prostate cancer with symptoms, but only 1% were aware that it could be asymptomatic [ 26 ]. Given the data above, this disconnect between scientific evidence and public perception is extremely striking. We believe that the time has come to urgently revaluate the messaging on urinary symptoms and recognise that the information currently being passed to the public is factually wrong. Any link between urinary symptoms and prostate cancer should be in our view removed as it risks men having a false sense of security if they do not have any urinary systems. Instead, there is a strong basis to emphasise that prostate cancer is silent or asymptomatic particularly in the curable stages. Waiting or looking out for urinary symptoms may potentially give a false sense of reassurance that all is well and delay presentation when the disease is treatable. Nevertheless, we are not advocating that patients with urinary symptoms be discouraged from presenting for investigation but rather that it should be recognised that male urinary symptoms cannot be used as a cardinal indicator of prostate cancer. Clearly, the downside of this change in message approach is that more men may approach GPs for a PSA test with the accompanying fears of over-investigation and treatment. However, there are a number of strategies that can already or will in future be able to reducing both concerns. At the primary care stage novel algorithms to risk assess patients for referral have been recently published using PSA combined with demographic and co-morbidity factors in a stepped approach to help decide who to refer [ 27 ]. With the use of MRI in diagnostic pathways to rule out indolent disease or negative findings, the risks of proceeding to an unnecessary biopsy after referral have also been largely mitigated (up to 40% reduction) [ 4 ]. The European Association of Urology for example has recently published recommendations for a risk-adapted early detection strategy using age-based PSA, testing schedules as well as MRI to rationalise who needs investigation (and who does not) [ 28 ]. In addition, after diagnosis, the rising use of active surveillance to manage early prostate cancer means that over-treatment is already much less of an issue. As an example, the National Prostate Cancer Audit in 2019 estimated that amongst men with favourable prognosis disease only 5% currently receive active treatment, a far cry from the days of previous screening studies ( https://www.npca.org.uk/content/uploads/2021/01/NPCA-Annual-Report-2020_-Infographic-140121.pdf/ ). Conversely, proponents of keeping the status quo may argue that that any testing is better than none and using LUTS to get men to a primary care doctor may be a ‘win’, regardless of whether or not there is an association. However, this could actually be considered to itself be a ‘screening strategy’ and one that has been shown to not be an effective way to detect cancer in the pre-PSA era [ 21 ]. As can be seen by the data in Table 1 , it is also the strategy which is most likely to result in a higher proportion of men detected with later stage disease. Prospective research is also needed to explore the current contrasting findings of PSA-detected versus symptom-detected cancers and its impact on stage at diagnosis and the longitudinal survival effect of waiting till symptoms lead to presentation.
We therefore call on guideline bodies, charities and the media to take urgent action to review the current public messaging and referral recommendations. Paramount is to abolish the public messaging suggesting that prostate cancer directly causes urinary symptoms. To maintain this fallacy is misleading. Efforts should instead be made to raise awareness that prostate cancer does not manifest with urinary symptoms. To be clear, we are not here advocating for an immediate screening programme nor are we asking to change already existing pathways (e.g. serendipitous investigation of men seeing primary care doctors for urinary symptoms). We recognise that the latter remains an important route for men to be detected and in particular for men who may not access health information resources or in hard to reach socio-demographics groups. For many of these men, the only reason to see a doctor is if they are having manifest bothersome symptoms. However, if men were aware that just because they had no symptoms did not mean they may not have cancer, more men might take up offers for tests. This could mean more tumours identified at an earlier stage and reduce the numbers of men experiencing late presentation with incurable disease. Eventually, we hope that an intelligent tiered screening programme will be possible, but until then, a simple change in message to correct years of misinformation would be a strong starting point.
Availability of data and materials
There is no new data or materials used in this article. Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Adams J. The case of scirrhous of the prostate gland with corresponding affliction of the lymphatic glands in the lumbar region and in the pelvis. Lancet. 1853;1:393–4.
Google Scholar
Taitt HE. Global trends and prostate cancer: a review of incidence, detection, and mortality as influenced by race, ethnicity, and geographic location. Am J Men Health. 2018;12:807–23.
Article Google Scholar
Ilic D, Djulbegovic M, Jung JH, et al. Prostate cancer screening with prostate-specific antigen (PSA) test: a systematic review and meta-analysis. BMJ. 2018;362:k3519.
Barrett T, Slough R, Sushentsev N, Shaida N, Koo BC, Caglic I, et al. Three-year experience of a dedicated prostate mpMRI pre-biopsy programme and effect on timed cancer diagnostic pathways. Clin Radiol. 2019;74(11):894.e1–9.
Article CAS Google Scholar
Wilson JMG, Jungner G. Principles and practice of screening for disease. Geneva: World Health Organization; 1968.
Vickers AJ, Russo G, Lilja H, Evans C, Schalken JA, Klein E, et al. How should molecular markers and magnetic resonance imaging be used in the early detection of prostate cancer? Eur Urol Oncol. 2022;5(2):135–7.
Papachristodoulou A, Abate-Shen C. Precision intervention for prostate cancer: re-evaluating who is at risk. Cancer Lett. 2022;10(538):215709.
Eklund M, Jäderling F, Discacciati A, Bergman M, Annerstedt M, Aly M, et al. STHLM3 consortium. MRI-targeted or standard biopsy in prostate cancer screening. N Engl J Med. 2021;385(10):908–20.
National Institute for Health and Care Excellence. Prostate cancer: diagnosis and management, NICE guideline [NG131]. 2021 update. Available from: https://www.nice.org.uk/guidance/ng131
Hippisley-Cox J, Coupland C. Symptoms and risk factors to identify men with suspected cancer in primary care: derivation and validation of an algorithm. Br J Gen Pract. 2013;63(606):e1–10.
Just J, Osgun F, Knight C. Lower urinary tract symptoms and prostate cancer: is PSA testing in men with symptoms wise? Br J Gen Pract. 2018;68(676):541–2.
Koo MM, Swann R, McPhail S, Abel GA, Elliss-Brookes L, Rubin GP, et al. Presenting symptoms of cancer and stage at diagnosis: evidence from a cross-sectional, population-based study. Lancet Oncol. 2020;21(1):73–9.
Hugosson J, Aus G, Lilja H, Lodding P, Pihl CG. Results of a randomized, population-based study of biennial screening using serum prostate-specific antigen measurement to detect prostate carcinoma. Cancer. 2004;100(7):1397–405.
Schröder FH, Hugosson J, Roobol MJ, Tammela TL, Ciatto S, Nelen V, et al. Screening and prostate-cancer mortality in a randomized European study. N Engl J Med. 2009;360(13):1320–8.
Karakiewicz PI, Bazinet M, Aprikian AG, Trudel C, Aronson S, Nachabé M, et al. Outcome of sextant biopsy according to gland volume. Urology. 1997;49(1):55–9.
Moolupuri A, Camacho J, de Riese WT. Association between prostate size and the incidence of prostate cancer: a meta-analysis and review for urologists and clinicians. Int Urol Nephrol. 2021;53(10):1955–61.
Boesen L, Nørgaard N, Løgager V, Balslev I, Bisbjerg R, Thestrup KC, et al. Prebiopsy biparametric magnetic resonance imaging combined with prostate-specific antigen density in detecting and ruling out Gleason 7-10 prostate cancer in biopsy-naïve men. Eur Urol Oncol. 2019;2(3):311–9.
Lorenzo G, Hughes TJR, Dominguez-Frojan P, Reali A, Gomez H. Computer simulations suggest that prostate enlargement due to benign prostatic hyperplasia mechanically impedes prostate cancer growth. Proc Natl Acad Sci U S A. 2019;116(4):1152–61.
Lophatananon A, Light A, Burns-Cox N, et al. Re-evaluating the diagnostic efficacy of PSA as a referral test to detect clinically significant prostate cancer in contemporary MRI-based image-guided biopsy pathways. J Clin Urol. December 2021. doi: https://doi.org/10.1177/20514158211059057 (In Press)
Rains AJH, Ritchie HD. Bailey & Love’s Short Textbook of Surgery. 19th ed. London: HK Lewis; 1984.
Martin RM, Vatten L, Gunnell D, Romundstad P, Nilsen TI. Lower urinary tract symptoms and risk of prostate cancer: the HUNT 2 Cohort, Norway. Int J Cancer. 2008;123(8):1924–8.
Frånlund M, Carlsson S, Stranne J, Aus G, Hugosson J. The absence of voiding symptoms in men with a prostate-specific antigen (PSA) concentration of ≥3.0 ng/mL is an independent risk factor for prostate cancer: results from the Gothenburg Randomized Screening Trial. BJU Int. 2012;110(5):638–43.
Collin SM, Metcalfe C, Donovan J, Lane JA, Davis M, Neal D, et al. Associations of lower urinary tract symptoms with prostate-specific antigen levels, and screen-detected localized and advanced prostate cancer: a case-control study nested within the UK population-based ProtecT (Prostate testing for cancer and Treatment) study. BJU Int. 2008;102(10):1400–6.
PubMed Google Scholar
Schenk JM, Kristal AR, Arnold KB, et al. Association of symptomatic benign prostatic hyperplasia and prostate cancer: results from the prostate cancer prevention trial. Am J Epidemiol. 2011;173:1419–28.
Chandra Engel J, Palsdottir T, Aly M, Egevad L, Grönberg H, Eklund M, et al. Lower urinary tract symptoms (LUTS) are not associated with an increased risk of prostate cancer in men 50-69 years with PSA ≥3 ng/ml. Scand J Urol. 2020;54(1):1–6.
Schulman CC, Kirby R, Fitzpatrick JM. Awareness of prostate cancer among the general public: findings of an independent international survey. Eur Urol. 2003;44(3):294–302.
Hippisley-Cox J, Coupland C. Predicting the risk of prostate cancer in asymptomatic men: a cohort study to develop and validate a novel algorithm. Br J Gen Pract. 2021;71(706):e364–71.
Van Poppel H, Roobol MJ, Chapple CR, Catto JWF, N'Dow J, Sønksen J, et al. Prostate-specific antigen testing as part of a risk-adapted early detection strategy for prostate cancer: European Association of Urology Position and Recommendations for 2021. Eur Urol. 2021;80(6):703–11.
Download references
Acknowledgements
Not applicable.
No funding was obtained for this study.
Author information
Authors and affiliations.
Department of Urology, Cambridge University Hospitals Trust, Cambridge, UK
Vincent J. Gnanapragasam
Division of Urology, Department of Surgery, University of Cambridge, Cambridge, CB2 0QQ, UK
Cambridge Urology Translational Research and Clinical Trials Office, Cambridge Biomedical Campus, Cambridge, UK
(Retired) Public Health England, Public Health England, National Cancer Registration and Analysis Service (Eastern Office), England, UK
David Greenberg
The Christie NHS Foundation Trust, Manchester, UK
Neil Burnet
You can also search for this author in PubMed Google Scholar
Contributions
VJG conceptualised the article and acts as guarantor. VJG and NGB researched content and source information for the article all of which are available as cited in the published medical literature. VG and NGB produced figures and drafted paper. DCG provided critical review and additional content and source material. All reviewed and approved the final manuscript.
Corresponding author
Correspondence to Vincent J. Gnanapragasam .
Ethics declarations
Ethics approval and consent to participate.
There were no ethical issues or need for consent to participate needed for this article.
Consent for publication
All authors give full consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gnanapragasam, V.J., Greenberg, D. & Burnet, N. Urinary symptoms and prostate cancer—the misconception that may be preventing earlier presentation and better survival outcomes. BMC Med 20 , 264 (2022). https://doi.org/10.1186/s12916-022-02453-7
Download citation
Received : 03 May 2022
Accepted : 28 June 2022
Published : 04 August 2022
DOI : https://doi.org/10.1186/s12916-022-02453-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Prostate cancer
- Lower urinary tract symptoms
- Early detection
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]

Ultrasound applied with MRI may be effective for treating prostate cancer
P recisely delivered ultrasound could be an effective treatment for prostate cancer , with high-frequency sound waves heating and killing off cancer cells, a new study says.
The treatment killed off all prostate cancer cells in 76% of men who underwent a follow-up biopsy one year later, researchers said.
It also cut down on unwanted side effects, such as incontinence and sexual dysfunction.
In the procedure, MRI scans are used to precisely apply ultrasound to a man's prostate cancer, through a small catheter-like device inserted through the urethra.
"This image-guided therapy maximizes our ability to kill cancer cells while minimizing collateral damage to the prostate to achieve the ultimate trifecta in prostate cancer treatment: full local cancer control while maintaining urinary continence and potency," lead researcher Dr. Steven Raman , a professor of radiology, urology and surgery at the David Geffen School of Medicine at UCLA, said in a news release.
For this study, 115 men with prostate cancer were recruited at 13 hospitals in five countries and given the ultrasound treatment, researchers said. The procedure can be performed in an outpatient facility in two or three hours, under general or spinal anesthesia.
Results show that the treatment reduced or eliminated cancer cells, and also shrank men's prostates and reduced their prostate-specific antigen (PSA) levels.
The men treated with ultrasound experienced a 92% decrease in average prostate size within a year, and a healthy decrease in PSA levels at five years. High PSA levels are a warning sign for prostate cancer.
The therapy also produced fewer side effects than other prostate cancer treatments.
After five years, 92% of the men had control over their bladder and 87% had good erectile function. Incontinence and erectile dysfunction are two common side effects of prostate cancer surgery.
Raman believes that ultrasound therapy "represents a revolution in whole-gland treatment for prostate cancer."
"Prostate cancer is the most common form of cancer in men, affecting one in eight men in their lifetime," he said. "We have more research to do, but if validated, (ultrasound) has the potential to change the standard of care for thousands of men."
Researchers are scheduled to present these findings in Salt Lake City at a meeting of the Society of Interventional Radiology, which begins Saturday.
Findings presented at medical meetings should be considered preliminary until published in a peer-reviewed journal.
More information
The California Institute of Technology has more about ultrasound treatment to kill cancer .
Copyright © 2024 HealthDay. All rights reserved.


- Weather
Search location by ZIP code
'it is that silent killer': doctors, survivors encourage men to get tested for prostate cancer.
- Copy Link Copy {copyShortcut} to copy Link copied!

GET LOCAL BREAKING NEWS ALERTS
The latest breaking updates, delivered straight to your email inbox.
Men’s health is back in the spotlight around the globe. King Charles III underwent an enlarged prostate procedure around the same time U.S. Secretary of Defense Lloyd Auston was given a prostate cancer diagnosis along with surgery.
Those who are both fighting and treating prostate issues are asking all men to step up and take the proper steps now for, hopefully, a better outcome later.
“I'm here 14 years later to let you know early detection saves lives,” Marcus Brooks said.
Brooks is a prostate cancer survivor and remembers when he got the news.
“Okay. So what's my next step? What do I need to do now to stay alive? I had no symptoms. I had no symptoms whatsoever,” he said.
Brooks was at a church event where PSA tests were being given out for free. He got the call a few days later that his numbers had a cause for concern. That PSA, or prostate specific antigen, test caught the cancer early. In his case, no invasive treatment was necessary.
He now gets annual checkups and advocates for men to take care of themselves.
“It's just a blood test. And that's what saved my life.”
The prostate gland primarily deals with urinary and sexual functions which can make it hard for men to talk about if they're having any issues. Often, the first thought of getting a prostate checked out is a rectal exam, but a PSA can come first before moving on to other forms of diagnosis and investigation.
“It's a difficult conversation. And men are, unfortunately, pretty shy about it. They don't go to their doctors. They don't want to talk about it. It's a very private issue,” Dr. Stephen Kappa, Vice President of The Urology Group, said.
Kappa says the stats tell the story.
About 250,000 men are diagnosed yearly with prostate cancer. Around 30,000 died.
One in eight men will get a confirmed diagnosis.
For Black men, it's one in six who are also twice as likely to die from it than their white counterparts.
“I start the conversation really saying, 'You're not alone,' and, 'Thank you for coming in and getting screened.' This is absolutely, critically important,” Kappa said.
Executive Director of the Cincinnati Cancer Foundation, Steve Abbott, fights the battle of cancer awareness, but also continues his own battle against metastatic prostate cancer. He has a family history of prostate cancer.
He got tested early, at age 44, and got good news. On August 2, 2013, everything changed.
“I turned 50. I went and got tested and my PSA had gone from 0.4 to 10.8, which was kind of a frightening trajectory in that amount of time because PSA tends to creep up. It doesn't tend to shoot up,” Abbott said.
After having his prostate removed, lingering cells in later tests showed the cancer, while minimal, was still present in Abbott’s body and had spread.
“We knew then we were able to conclusively know that it was going to be an incurable version of prostate cancer, incurable but treatable.”
With advancements in radiation treatment, and chemo and hormone therapy, the difficult diagnosis isn't letting the cancer stop him.
“I can either go into a hole and not talk about it and just kind of try to get through my life as best I can with it, or I can turn this into a cause and really get out there in front of people and talk about it,” Abbott said.
The message to men continues to be to put your pride aside and talk about your health.
“You can go get a blood test if nothing else. That simple, that will give you at least an indication of what your PSA is that might at least put you on notice that I need to get this checked into further,” Abbott said.
“I want to emphasize again to men, if we catch it early, if we spot it early, we can treat it successfully and get you back to a normal life,” Dr. Kappa said.
“It is that silent killer. Men get tested. It's only a blood test. And we go from there and I stand on and I advocate early detection saves lives,” Brooks said.
The first screening for all men should start at 50 to get a baseline PSA blood test. For black men, and anyone with a family history of prostate cancer, should start at 40.

IMAGES
VIDEO
COMMENTS
Show abstract. ... Prostate cancer is the most common cancer among men, and is the second-leading cause of cancer deaths in men in the United States [1]. Treatment methods include hormone therapy ...
Introduction. Prostate cancer is the second most common male cancer. 1 It is estimated that, by 2030, 1.7 million men will be living with prostate cancer. 2 Australia has the highest incidence of prostate cancer in the world, 1 attributed largely to a high rate of case-finding, in the form of measuring the concentration of prostate-specific antigen (PSA) in asymptomatic men.
diagnosed with early stage prostate cancer, increasing the risk of over treatment. There is a strong need for better prognostic markers of prostate cancer. Th e aim of this thesis was to evaluate an early prostate cancer screening study and to assess different possible prognostic factors of prostate cancer.
Prostate cancer diagnosis after prostate biopsies, and the subsequent treatment decision making, affect millions of men worldwide yearly [1, 2, 3]. ... This thesis is also emphasized by the fact that IHC was performed in a high proportion of patients (>47%) in order to rule out prostate cancer diagnoses (negative biopsy), which is also very ...
Abstract. The current diagnostic and stratification pathway for prostate cancer has led to over-diagnosis and over- treatment. This thesis aims to improve the prostate cancer diagnosis pathway by developing a minimally invasive blood test to inform diagnosis alongside mpMRI and to understand the true Gleason 4 burden which will help better stratify disease and guide clinicians in treatment ...
A thesis submitted to The University of Birmingham For the degree of DOCTOR OF PHILOSOPHY ... 8.4 Prostate cancer: current status and future research 136 8.4.1 Research on environmental exposures 136 8.4.2 Research on genetics 137 8.4.3 Future use of PSA in screening 140 ...
Prostate cancer is a leading cause of cancer death in men. Evaluating knowledge, practice and attitudes towards the condition is important to identify key areas where interventions can be instituted. This was a hospital-based descriptive cross-sectional study aimed at assessing knowledge, practice and attitude towards prostate cancer screening among male patients aged 40 years and above ...
With the burden of prostate cancer, it has become imperative to exploit cost-effective ways to tackle this menace. Women have demonstrated their ability to recognize early cancer signs, and it is, therefore, relevant to include women in strategies to improve the early detection of prostate cancer. This systematic review seeks to gather evidence from studies that investigated women's ...
Prostate cancer GEMM models driven by either PTEN-loss or hyperactivation of MYC exhibit significantly increased global protein synthesis by about 20%, an expected range for such potent drivers of prostate cancer development. 59 Unexpectedly however, significant suppression in global protein synthesis was observed in mice harboring both genetic ...
The thesis is based on data from two different overall projects: a survey sent to all members of the Swedish Prostate Cancer Federation (SPCF) and the PROstate Cancer-Experiences and Expectations During treatment (PROCEED) project. ... Results: Men with advanced prostate cancer experience an uncertain illness situation when living with a life ...
Prostate cancer has been a disease of older men but age at diagnosis is falling in Sweden. ... The overall purpose of this thesis was to identify and describe fatigue and its influence on men's lives when undergoing examinations for suspected prostate cancer and diagnosed with prostate cancer. Further, the purpose was to understand if ...
In paper II we examine if DHT promotes or protects from aggressive prostate cancer. Contrary to what one might assume, DHT protects from death in prostate cancer. The most common way to test for prostate cancer is by a PSA test. The PSA-test, if abnormal, could indicate prostate cancer.
Prostate cancer has emerged as the most frequently diagnosed cancer, except for non-melanoma skin cancer, among men in many Western countries in the last decade. ... This thesis begins with a descriptive epidemiological study using cancer registry incidence data from the West of Scotland from 1991 to 2007. The aim was to determine whether the ...
Screening for prostate cancer often includes a blood test for the prostate specific antigen (PSA) and/or a digital rectal exam (DRE; CDC 2010). Disagreement regarding guidelines for prostate cancer screening intensified recently (Bazell 2012). Issues of disagreement include the age at which men should begin screening for prostate cancer and the ...
The research presented in this thesis sought to investigate the prognostic and predictive significance of AR phosphorylation at serine 578 in hormone-naïve ... prostate cancer patients undergoing active surveillance, representing a cohort of patients with low-risk disease, as defined by current clinical markers such as PSA ...
Peter Kircher, a six-year prostate cancer fighter; Loch Anderson, a prostate cancer journeyman from Washington State; Steve Hentzen, the co-founder of the prostate network and a ten-plus year prostate cancer survivor; Marty Chakoian, an eighteen-year prostate cancer survivor and Seattle prostate cancer support group leader; A five-year
masks and lesion scores for 157 men with prostate cancer. The dataset is further explored in Chapter 3. The two main problems addressed in this thesis are the classification of lesions, including PIRADS and clinical significance, and the detection and segmentation of the prostate cancer lesions. For these problems different experiments were ...
Background Prostate cancer is the most commonly diagnosed non-skin cancer in men. Screening for prostate cancer is widely accepted; however concerns regarding the harms outweighing the benefits of screening exist. Although patient's play a pivotal role in the decision making process, men may not be aware of the controversies regarding prostate cancer screening.
Introduction. Prostate cancer is a prevalent malignant tumor in elderly men, ranking as the most common solid malignancy in men in western countries, with an increasing incidence year by year (Rebello et al., 2021).Current research indicates that the occurrence of prostate cancer is primarily associated with factors such as age, hormones, race, and genetics (Bergengren et al., 2023).
Prostate cancer overall has a strong five-year survival rate, thanks in part to these treatment methods. If the cancer hasn't spread to other parts of the body, the chance of recovery is about 99%.
The student is expected to complete the thesis Spring 2024 and start a Ph.D. program in mathematical biology in the Fall 2024 semester. Aims The data will be used for model validation particular to Chapter 5 from the book mentioned on "Prostate Cancer: PSA, AR, and ADT Dynamics".
Theses/Dissertations from 2022. Omics Analysis in Cancer and Development, Emalie J. Clement. Investigating the Role of Splenic Macrophages in Pancreatic Cancer, Daisy V. Gonzalez. Polymeric Chloroquine in Metastatic Pancreatic Cancer Therapy, Rubayat Islam Khan. Evaluating Targets and Therapeutics for the Treatment of Pancreatic Cancer, Shelby ...
The study followed nearly 2,500 American men 80 and younger who were diagnosed with prostate cancer of varying levels of severity from 2011 through early 2022. It built on prior observational ...
Prostate cancer is the second most common cancer in men worldwide, accounting for an estimated 1.1 million new cases diagnosed in 2012 (). Currently, there is a lack of specific guidance on supportive care for men with prostate cancer. This article describes ...
Prostate cancer is the most common cancer for men in the United States. Luckily, most men with prostate cancer will still be alive 15 years after diagnosis. Men with prostate cancer that hasn't spread outside the gland have several treatment choices. These include surgery, radiation therapy, and active surveillance, where treatment is delayed ...
Prostate cancer is the most common form of cancer that affects British men, with about 52,000 cases annually, according to Cancer Research UK senior science engagement manager Rupal Mistry.
Your age, general health, the stage of your cancer, the aggressiveness of your cancer cells, the condition of your prostate, the condition of your urinary tract, the state of organs and tissue in ...
Prostate cancer is an epidemic of the modern age, and despite efforts to improve awareness, it remains the case that mortality has hardly altered over the decades, driven largely by late presentation. There is a strong public perception that male urinary symptoms is one of the key indicators of prostate cancer, and this continues to be part of messaging from national guidelines and media ...
For this study, 115 men with prostate cancer were recruited at 13 hospitals in five countries and given the ultrasound treatment, researchers said. The procedure can be performed in an outpatient ...
on boeing planes as well from king charles the third's in large prostate procedure to u.s. secretary of defense lloyd austin getting a prostate cancer diagnosis and surgery, men's health has ...