An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.

- Needs assessment
Evidence review A
NICE Guideline, No. 216
- Copyright and Permissions
This evidence report contains information on 2 reviews relating to needs assessment, the first being an intervention effectiveness review and the second, a qualitative review.
- What is the effectiveness of social work approaches to assessing and reviewing complex care and support needs (including strengths-based approaches)?
- Based on the views and experiences of everyone involved, what works well and what could be improved about social work assessment and review of complex care and support needs?

Review question
Introduction.
A social work assessment is central to helping people understand their situation and needs and is the main means of access to social care, facilitating the provision of support to adults whose needs are complex. The Care Act sets out a number of requirements of a needs assessment, referring to the assessment and eligibility process as “…one of the most important elements of the care and support system”. The aim of this review was to explore the effectiveness of 3 main approaches to social work needs assessment, establishing the best way of identifying and assessing needs within this population. The review also aimed to find out the views and experiences of those involved in a social work needs assessment, to understand what works well and how the process could be improved.
Summary of the protocol
Please see Table 1 for a summary of the Population, Intervention, Comparison and Outcome (PICO) characteristics for the effectiveness review question.
Please see Table 2 for a summary of the Population and Phenomenon of interest for the qualitative review question.
Summary of the protocol (PICO table) – effectiveness question.
Summary of the protocol (population and phenomenon of interest) - qualitative question.
For further details, see the review protocols in Appendix A .
Methods and process
This was designed as a mixed-methods review using parallel synthesis of effectiveness and qualitative data. However no studies were identified which were applicable to the effectiveness review question so qualitative evidence alone is reported here.
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual . Methods specific to these review questions are described in the review protocol in appendix A and the methods document (supplementary document 1).
Declarations of interest were recorded according to NICE’s conflicts of interest policy .
Effectiveness evidence
Included studies.
A systematic review of the literature was conducted but no studies were identified which were applicable to this review question.
See the literature search strategy in appendix B and study selection flow chart in appendix C .
Excluded studies
Studies not included in this review are listed, and reasons for their exclusion are provided in appendix J .
Summary of included studies
No studies were identified which were applicable to this review question (and so there are no evidence tables in Appendix D ). No meta-analysis was conducted for this review (and so there are no forest plots in Appendix E ).
Qualitative evidence
A systematic review of the literature was conducted using a combined search for all qualitative questions. Six studies were included in this review ( Abendstern 2013 , Abendstern 2014 , Bolger 2014 , Darling 2012 , Symonds 2018 and Yeung 2016 ).
The data provided evidence on the views and experiences of a social work needs assessment. Data collection methods included interviews and focus groups (or a combination of both), and 1 ethnographic study.
Study population included people experiencing a social work needs assessment, their relatives or carers, as well as practitioners and care managers from adult social care departments.
The included studies are summarised in Table 3 .
Summaries of the studies that were included in this review are presented in Table 3 .
Summary of included studies.
See the full evidence tables in appendix D .
- Knowing what to expect from the assessment
- Support during the assessment
- Perceptions of how person-centred the assessment is
- Appropriateness of online assessment
- Balancing needs and wishes against available resources
- Meeting needs through self-assessment
- Person centred approach to self-assessment
- Social worker role in self-assessment
- Perceived ability to express preferences
- Satisfaction with social worker
- Assessing full range of strengths, needs and wishes
- Practitioners’ role as an advocate
The theme map illustrates these overarching themes and their related themes. Overarching themes are shown below in orange and central themes in blue.
Summary of the evidence
No studies were identified which were applicable to this review question (and so there are no evidence tables in Appendix D ). No meta-analysis was conducted for this review (and so there are no forest plots in appendix E ).
The synethesis of the evidence generated 7 main themes from evidence about the views of people involved in a social work needs assessment, namely adults with complex needs, carers and practitioners. One study provided evidence about problems accessing an assessment, in particular that it takes too long to get a response to a request for an assessment. Two studies provided evidence relating to whether the assessment met the person’s expectation. The evidence suggested that there was uncertainty about what to expect from the assessment. There was also evidence around support during the assessment with some people feeling satisfied with the support to complete assessments and others feeling they had very little support. One study provided evidence for carers’ satisfaction with the assessment process that suggested carers did not feel assessments were person-centred.
Four studies, provided evidence relating to the appropriateness of the conduct of assessments, including self-assessments. The evidence suggested that online self-assessment may not be appropriate for all groups of people. Evidence also showed there were mixed views among practitioners and people using services about how well self-assessment would meet the needs of people requiring high level support. Three studies provided evidence relating to the positive and negative aspects of the process of assessment and review. The evidence suggested that people were not able to express their preferences in an assessment, and were not able to view their completed review. The evidence also suggested that people were not able to express their preferences as language was shown to be a barrier during the assessment process. People were dissatisfied with the time taken for follow-up, and the time taken to complete a self-assessment. One study provided evidence on whether practitioners felt they had adequate time and resources to carry out an assessment. The evidence suggested that it could be difficult for practitioners to identify the full range of a person’s needs, and that the views of carers and family members were helpful. Three studies provided evidence relating to the practitioner’s role as gatekeeper. The evidence suggested that practitioners had to balance a person’s needs against available resources and budgets, and their role in the assessment process was that of an advocate.
See Appendix F for full GRADE-CERQual tables.
Economic evidence
A systematic review of the economic literature was conducted but no economic studies were identified which were applicable to this review question.
A single economic search was undertaken for all topics included in the scope of this guideline. See Supplement 2 for details.
A single economic search was undertaken for all topics included in the scope of this guideline. See supplement 2 for further information.
Summary of studies included in the economic evidence review
No economic studies were identified which were applicable to this review question.
Economic model
No economic modelling was undertaken for this review because the committee agreed that other topics were higher priorities for economic evaluation.
Addition of preparatory meeting before assessment
The committee considered making a recommendation which would allow for an additional preparatory meeting before any assessment where this was deemed of benefit to an individual in taking an active role in decision making about their care and where they explicitly requested it. Netten and Curtis 2020 estimated a mean caseload of 17.4 clients for social workers in children’s’ services at any one time. No equivalent estimate was given for social workers in adult care. It is difficult to estimate a client caseload per adult social worker given the number will depend on the complexity of the cases with more complex cases leading to a lower caseload. Such complexities are also likely to exist in children services. 17.4 clients was therefore deemed a reasonable estimate for caseload in adult care.
The average cost per person across all patients was estimated under a number of assumptions and for all 3 wage rates estimated from Netten and Curtis 2020 and discussed in detail in Review G, Appendix I . In summary 3 wage rates were estimated intended to give a best as well as a plausible lower and upper estimate of a social worker wage rate:
Wage A : All estimated costs of employment were included apart from those associated with gaining relevant qualifications. This estimate was thought most likely to reflect the true cost to the NHS & PSS from changes in the total number of hours worked.
Wage B : Only the annual wage plus employer on-costs (pension, national insurance etc.) were included. This represented a lower plausible estimate where there would be zero or minimal costs from needing to supply additional accommodation or administration for any additional employed social workers.
Wage C: Is as for Wage A but with qualification on-costs included. This was considered an upper estimate of the true cost of additional hours needed for these preparatory meetings.
Under all assumptions it was assumed that there was no cost of travel for the social worker to attend these meetings. This is unlikely to be a realistic assumption but travel costs are likely to vary significantly across England with travel costs (both social worker time and travel/motoring costs) likely to be lower in densely populated areas compared to those which are sparsely populated. It was also assumed in all scenarios that there would be no additional cost or time needed for arranging the meetings, preparing for them or completing any administration post meeting. Whilst these would take up social workers time to perform the total amount is unlikely to be different from if only one meeting had occurred. The estimates also do not attempt to account for any potential timesavings from the assessment meeting if certain information, such as processes, purposes and potential outcomes, discussed at the preparatory meeting do not have to be repeated at the assessment meeting.
Five assumptions were made which were used to estimate the entire range of plausible costs for preparatory meetings. Two assumptions assume full uptake for all assessments whilst two assume only partial uptake based on committee estimate. A final assumption has a mix of both in person and telephone/videoconference appointments. The uptake was assumed to be higher for telephone/videoconference meetings as opposed to face to face meetings. The 5 assumptions are:
Assumption 1: All people will receive a face to face personal preparatory meeting lasting 1 hour in total
Assumption 2: All people will receive a phone call or teleconference meeting lasting 20 minutes in total.
Assumption 3 : 10% of people will receive a in face to face personal preparatory meeting lasting 1 hour in total
Assumption 4: 25% of people will receive a phone call or teleconference meeting lasting 20 minutes in total.
Assumption 5: 10% of people will receive a in face to face and 25% will receive a phone call or videoconference meeting lasting their respective times as above.
It should be noted that assumptions around the length of time for a preparatory meeting are intended to be illustrative and there will be large variation in the complexity of cases and the time needed to effectively undertake them. These assumptions should not be seen as a target or an upper limit and longer meetings may often be necessary.
Estimated additional costs per person from preparatory meetings prior to assessment (with wage A being the best estimate and wage B the lower and Wage C the upper estimate – for details see above).
Such meetings are likely to add between £2.45 and £51.48 for every need assessment undertaken if they were all or a proportion were accompanied by a preparatory meeting. As discussed above some costs will be excluded from these. It is also likely that where only a proportion of people have a preparatory meeting these are the most complex cases and therefore may make up a higher proportion of the costs. For example the 10% of people who would have a face to face preparatory meeting may take up more than 10% of the time and consequently the costs than that of meetings for all. It also does not take account of whether additional social workers would need to be employed to cover such casework that otherwise would have been undertaken.
The committee’s discussion and interpretation of the evidence
The outcomes that matter most.
For the effectiveness review, satisfaction with the assessment and social care related quality of life were considered to be critical outcomes. Identification of strengths, timeliness of assessment and utility of assessment were considered to be important outcomes.
The outcomes selected as critical were chosen as they directly reflect whether a needs assessment has benefited the person being assessed. The outcomes identified as important were chosen because they reflect key aspects of the frameworks for assessment. These outcomes were also thought to be most likely to be reflected in contemporary research using quantitative methodologies.
To address the issue of what works well and what could be improved about a social work needs assessment, the second part of the review was designed to include qualitative data and as a result the committee could not specify in advance the data that would be located.
- Satisfaction with the process of accessing a social work assessment.
- Whether the assessment met the person’s expectations. Perceived appropriateness of the conduct of the assessment.
- Positive and negative aspects of the process of assessment and review.
- Perception about the impact of a social work assessment on meeting needs.
- Whether carers understand/ are made aware of their own right to assessment.
- Carers satisfaction with the assessment.
- Whether practitioners feel adequately trained and supervised.
- Whether practitioners feel they have adequate time and other resources to conduct assessments and reviews.
- Whether practitioners perceive their role as a ‘gate keeper’ to services or support.
These themes were chosen as they cover aspects of what works and does not work well from the perspective of everyone involved, and focus on the experiences, perceptions and attitudes of the person/s being assessed and social workers undertaking the assessment.
The quality of the evidence
There was no evidence identified for the effectiveness question.
The evidence was assessed using GRADE-CERQual methodology and the overall confidence in the findings ranged from low to high. The review findings were generally downgraded because of methodological limitations of the included studies, including, for example no information on data analysis and recruitment strategy. The findings were also downgraded for concerns over relevance because the study context in some instances was slightly different to the review protocol. Some findings were downgraded due to concerns around coherence because a few findings were underpinned by ambiguous or contradictory data that was not explained. Finally, some findings were downgraded for concerns over adequacy because together, the relevant studies did not offer rich data.
See appendix F for full GRADE-CERQual tables with quality ratings of all review findings.
Benefits and harms
Principles of social work for adults with complex needs – for social workers.
The committee used the evidence in this review to make a recommendation that ensures people are able to express their preferences, in particular regarding their communication needs and preferences throughout provision of support. They discussed evidence (A5.1.2 Language as a barrier; moderate quality) that showed language can present a communication barrier during assessments and agreed this could be addressed through a professional interpreting service (rather than a family member). Extrapolating from this and based on their experience, the committee discussed that throughout provision of support, including assessment, communication needs or preferences are not always met, and reasonable adjustments to address them are not always made. Therefore, the committee agreed it was important to address not only language but all communication needs and preferences, and ensure any information about the purpose and process of the assessment is communicated in an accessible way that meets the person’s needs. The committee were aware of recommendations in the NICE guidance on people’s experience in adult social care services , which address these issues and included a reference to this guidance in their recommendation. This would ensure that all adults with complex needs, regardless of their needs, receive the same access and support to care and ensures equality throughout. These can include different languages as provided by interpreters, sign language, Makaton, whether a communication partner needs to be present and any digital or manual devices that may aid communication. The need for augmentative and alternative communication methods or devices were also highlighted as important, and this can include talking mats, picture boards, or computer technologies that aid or replace speech. The committee also noted that certain statutory requirements, namely the Mental Capacity Act (s1, (3)) state that practical steps must be taken to ensure people are able to make decisions, so they also recommended that assessment documentation is provided in appropriate formats, such as braille, in different languages or audio recorded.
The committee, based on experience, also discussed the importance of identifying throughout their work with the person whether advocacy services could be needed and wanted, to support them and their families. They therefore added it to the recommendation. They also notes that there are sensory factors that may also affect a person’s abilitiy to participate in discussions (such as sounds or lights) and therefore added that sensory needs should also be considered.Following on from discussions around ensuring everyone receives the appropriate adjustments for their communication needs, the committee discussed that people’s life experiences including discrimination, marginalisation, and structural inequalities may have an influence in the assessment process. They acknowledged that people have varying levels of support needs, and different experiences with support agencies and processes, some negative and some positive, that could have an impact on the assessment process. They also discussed that culture and protected characteristics such as age may mean people are more reluctant to ask for help or discuss their needs. The committee felt it was important to address these to ensure equality during the assessment process, and made a recommendation to highlight these issues.
The committee recognised based on their experience that it is always useful to read the relevant NICE guideline that could affect the person that they are working with and gave some examples of guidance that may be relevant in the context of complex needs.
The committee discussed that as there was no effectiveness evidence related to different approaches to a social work needs assessment, they would use the qualitative evidence supported by their own experiential knowledge to make recommendations about the principles of arranging and conducting a social work needs assessment.
The committee discussed the importance of taking a tailored, individualised approach to a needs assessment, and used the evidence to make recommendations to support this.
Needs assessment – providing information
The committee discussed the evidence (A2.1 Knowing what to expect from the assessment; high quality) that showed people were not always aware of what to expect from assessments. They agreed on a recommendation to ensure that the process and purpose of an assessment are communicated beforehand. They discussed that adults with complex needs may be in contact with multiple services and other health professionals, and recognised the importance of clear communication to avoid confusion between services. The committee also highlighted that adults with complex needs may have multiple communication needs, and discussed that any information regarding the assessment process should be provided to a person in an accessible format and in line with their needs and preferences to ensure it is person centred. The committee discussed the evidence (A5.1 Perceived ability to express preferences; high quality) which suggested people did not get to see the forms before the assessment, or time to think about the questions and read through them once filled in. They used this evidence to expand on the recommendation and agreed that people should be given enough time to prepare and review documents. The committee agreed that this was important to highlight to ensure that people are given an opportunity to provide accurate and correct answers, which will contribute to the appropriate support given and their needs being addressed.
The committee used their expertise to expand on this evidence and made a recommendation for people to be signposted to information regarding their rights (such as the right for a carer’s assessment). This would help the person to understand what a social work needs assessment should involve, and their rights in relation to relevant issues such as information sharing, which are enshrined in the Care Act Code of Practice and the Mental Capacity Act.
Needs assessment - planning the assessment
Evidence (A2.1 Knowing what to expect from the assessment; high quality) that some people did not know what to expect from an assessment led the committee to discussions around the wellbeing of people being assessed and their carers. In their experience, there could be misperceptions about the aim of a social work assessment, for example that its aim is to facilitate admission to a care home, or to test for eligibility for services or as a means of reducing current support. They agreed that better understanding and knowledge about social work assessments, both in terms of what is involved and the likely outcome would reduce anxiety and stress. In particular, they highlighted the importance of ensuring that a flexible approach is taken during the assessment, as well as explaining complex concepts using simple, clear language. Based on informal consensus the committee agreed that social workers should conduct assessments in a way that minimises stress and that tailoring the assessment and using clear language would help to achieve this.
The committee discussed the review findings (A5.1 Perceived ability to express preferences; moderate to high quality), which suggested people were unable to express their preferences during assessments, either because they did not have enough time during the assessment, or there were issues around language being a barrier during the assessment. The committee suggested a preparatory meeting or initial contact before the assessment as a way of overcoming these issues. They also highlighted that this would be a way to facilitate the assessment to be individualised, by tailoring the assessment to any specific needs or preferences regarding communication. The committee agreed that this recommendation would also allow for the advanced planning of any interpreters required, and planning for information to be available in the appropriate formats discussed above. To ensure a person-centred approach, the committee agreed it was important to take into account individual preferences, with regard to the format of the preparatory initial contact or the fact that some individuals may not wish to have one. The committee discussed situations where a preparatory initial contact would not be possible or beneficial such as when there is an urgent need for an assessment. Therefore, they included this as a consideration in the recommendation. However, the committee discussed from their experiential knowledge that assessments can be overwhelming and may contribute to feelings of anxiety, potentially causing people to feel as though they are being monitored. They agreed that a preparatory initial contact would be an opportunity to explain the social work processes and potentially alleviate anxieties. The committee also discussed that such an initial contact may be useful when the person could have substantial difficulty in being involved in the assessment so that relevant adjustments can be planned in advance. They noted that this may then also be an opportunity to see whether an independent advocate should be provided to support the person to be able to actively participate in the assessment process.
The committee also recognised that it is not current practice to have a preparatory visit or make initial contact before an assessment, and highlighted the potential of a resource impact and difficulty in implementation due to staffing and workload issues. They therefore agreed that a preparatory initial contact should be available as an option the social worker could utilise, if they perceive this as the most useful approach. As the evidence did not support the specific process change of a preparatory visit or initial contact, they did not make this a strong recommendation.
The committee discussed other practical aspects that are needed to ensure an assessment is person-centred. The committee discussed the importance of considering where the assessment will take place. The committee discussed the evidence (A6.1 Assessing full range of strengths, needs and wishes; high quality), that suggested an assessment in the person’s home may help the assessor make a judgement on the broader, environmental aspects of a person’s need. However, they noted that the evidence did not come from the views of people using services and it was important to consider a person’s choice and preferences when deciding on the location since they will not necessarily want the assessment conducted at home. The committee therefore used the evidence and their experience of assessments to recommend that the location of the assessment be discussed with the person along with other practical aspects. From their experience the committee discussed that meetings could be remote (virtual or by phone) or in-person. They discussed the advantages and disadvantages of each of these options but did not reach consenus about recommending one over the other. They therefore highlighted that the person should be asked about their preferences in relation to this. However, they emphasised that where there are concern about potential safeguarding issues, an in-person assessment is likely to be needed to ensure the safety of the person.
While discussing the practicalities of assessment and the importance of making it as stress free as possible, the committee also agreed the social worker should ask the person what time of day they would prefer the assessment take place. The committee recognised that people having the assessment have important time commitments and that depending on their individual needs; there might also be times during the day where people feel more able to participate in the process. The committee also agreed that allowing for a preferred time may support a more collaborative approach to the assessment, particularly if the presence of other practitioners were required. They also discussed that accommodating time preferences would support family members or carers to take part when they are managing other commitments.
The committee discussed evidence (A6.1 Assessing full range of strengths, needs and wishes; high quality) which suggested that having a carer present during assessments might help the assessor identify needs, but raised the point that personal preferences about involving family members should be considered. They committee agreed that the choice to have a carer or family member present at the assessment is enshrined in the Care Act (part 1 s9 (5)) so they agreed that another practical consideration should be whether the person wishes that someone accompany them during the assessment. The committee also highlighted the relevance of the Mental Health Act Code of Practice (4.40 to 4.46) about involving carers, relatives, friends or advocates in Mental Health Act assessments. The committee acknowledged that a needs assessment may also provide the opportunity to tell carers that they also have a right to an assessment of their own needs, separate from the person being assessed. Aware of existing NICE guidance about Supporting Adult Carers, the committee signposted to that guideline.
The committee discussed the evidence around self-assessment. The evidence (A4.3 Meeting needs through self-assessment; moderate to high quality) showed that self-assessment may not be appropriate for all groups of people and may not be sufficient to address some complex needs. However, the evidence (A4.4 Person-centred approach to self-assessment; high quality) also suggested that self-assessment could be a way of ensuring a more person-centred approach to needs assessment. The committee agreed, based on the evidence and from experience, that for a person-centred approach to assessments, people could be offered a face-to-face assessment if a self-assessment was regarded to be insufficient to address a person’s needs. However, in line with a person-centred approach, they agreed to include in the recommendation that social workers should inform people who choose a self-assessment, of the advantages and disadvantages of self-assessment compared to a face-to-face assessment. They acknowledged that these would be different for people depending on their needs and their required support. The committee expanded on the evidence around the appropriateness of self-assessment in meeting peoples’ needs, and agreed there was a risk of inequity regarding information. They discussed that the advantage of an assessment with a social worker, over a self-assessment, was that the social worker could provide more information regarding, for example, eligibility for other assessments or legislative frameworks. The committee agreed it was important to ensure that if someone was conducting a self-assessment, then all the information provided during an assessment with a social worker is made available.
The committee discussed the importance of support for people who have chosen to have a self-assessment. They agreed that the evidence (A2.2 Support during the assessment process; moderate quality) supported a recommendation to offer support, and were also aware that supported self-assessment must be made available, according to section 6.45 of The Care and Support Statutory Guidance (2021). Acknowledging that people’s needs for support to complete a self-assessment will vary, they made a number of suggestions, for example the involvement of an advocate, or providing additional information.
Needs assessment - conducting the assessment
The committee discussed the importance of checking that any information provided by supported self-assessment is an accurate reflection of the person’s circumstances and made a recommendation to cross-reference with information from other sources and they noted that this would typically include involved family and carers or the multidisciplinary team. They agreed that this would lead to more appropriate and accurate assessments of need, and were aware that The Care and Support Statutory Guidance (2021) supported this recommendation.
The committee acknowledged that self-assessment can be a difficult process for people who do not have the appropriate support, and recognised the disadvantages of a recommendation that highlighted the self-assessment process. The committee discussed the perceived pressure or anxiety that can be placed around the conduct of assessment. The committee discussed that people may feel worried about the prospect of complicated form filling, and concerned that their needs cannot be fully expressed on a form. They also discussed that people may feel pressure from having to try and organise support from family and friends to assist them with the assessment. However, on balance the committee agreed that the reference to the requirements of The Care and Support Statutory Guidance (2021) for support during self-assessments, combined with their suggestions for the types of supports would alleviate these concerns.
The committee discussed the content of the assessment and the related eligibility criteria and the statutory guidance that supports the decision-making process during a needs assessment. They agreed that it was important to reference the eligibility criteria in a recommendation. They agreed that this would enable social workers to understand whether the needs assessment has correctly considered and identified all needs, regardless of the format taken. The committee were also aware of various guidance and information sources about the conduct of Care Act assessments, including material published by the Social Care Institute for Excellence. Although these are likely to benefit practitioners, they agreed to signpost to the Care Act itself and statutory guidance since it is not mandatory to follow other guides or advice.
Based on experience the committee discussed that some of the person’s needs may be outside of the expertise of the social worker, for example communication or mental health needs, and it is important that specialist input is sought to address these needs.
Needs assessment - recording and reviewing the assessment
The committee discussed the evidence (A5.1.1 Access to completed review; high quality) that showed some people were not given the opportunity to see draft copies of their assessment before they were finalised. As there was high confidence in this finding the committee agreed it was important to recommend that people see their assessment in draft form to correct any inaccuracies or differences of perspectives. The committee agreed that since this is also supported by the Care Act 2014 they could make a strong recommendation.
The committee used the evidence as well as experiential knowledge to make a recommendation for social workers to provide information regarding the complaints procedure. The committee discussed the various negative aspects of the needs assessment process which were identified by the evidence review (A5.1 Perceived ability to express preference; moderate to high quality). The recommendations already agreed by the committee were designed to target dissatisfaction regarding the inability to express preferences, not having access to a completed review and barriers such as language. However, from their experience the committee knew that the negative experiences identified by the evidence were a small selection of the problems that can occur in practice. They agreed that it was therefore important to ensure that adults with complex needs, people involved in a person’s care, and any other people important to them were aware of how to make complaints. This would ensure any issues and negative aspects not captured by the evidence are addressed and services are continuously improving.
The committee used their experience to discuss the importance of organisations providing people taking part in a self-assessment with any relevant and available information they may have about them. They agreed to make a recommendation supported by the Care and Support (Assessment) Regulations. The committee agreed that this would be in line with their discussions above regarding the importance of people being able to provide accurate information when completing assessments of need.
Risk assessment – recording and reviewing the assessment
Some of the evidence (A5.1 Perceived ability to express preferences; high quality; A5.1.1 Access to completed review; high quality) related to needs assessment was used to inform recommendations about risk assessment. The committee agreed that it was appropriate to use evidence related to a needs assessment, for recommendations for a risk assessment, as this echoed their experiences of risk assessment in practice. The committee used the evidence (A5.1 Perceived ability to express preferences; high quality; A5.1.1 Access to completed review; high quality) around people’s perceived ability to express preferences and frustrations about not seeing a copy of their completed review and they recommended that social workers should give people a copy of their risk assessment. This recommendation ensure a person-centred approach is taken to risk assessment and that information regarding risk is accurate and comprehensive.
The committee made a research recommendation to address the gaps in the evidence for a social work needs assessment. The committee initially wanted to find out about the best approach to a social work needs assessment but no effectiveness data were located. The qualitative data that were identified did not highlight a specific best approach to a social work needs assessment and the committee agreed to pursue this by recommending future research in this area. They were particularly interested in plugging the evidence gaps around strengths based needs assessment, which is growing in visibility in policy and practice terms but not thus far in research. Rights based approaches are also intrinsically linked with strengths based approaches so the committee agreed it would be beneficial for future NICE guidance to base recommendations on research findings about these approaches. They therefore also made a research recommendation to establish the acceptability of strengths and rights based approaches to social work assessment as well as the barriers and facilitators to delivering these. They agreed that a qualitative design would enable them to answer this question.
Cost effectiveness and resource use
The committee’s recommendation to consider arranging a preparatory meeting or initial contact before any needs assessment would add additional visits and increase contact time from social workers and an increase in resource use. The committee highlighted that this was unlikely to be standard practice but would be used by a social worker if it was needed to allow a person with complex needs to fully participate in their assessment and it was strongly indicated by the person that they would find it beneficial. Where appropriate this could be done via telephone or videoconferencing removing the time and cost of travelling to the appointment. Whilst this will lead to an increase in resource use it underpins the statutory guidance that an individual must be able to participate as fully as possible in decisions about them and be provided with the information and support necessary to enable this. The recommendation could improve future outcomes through enabling a person-centred approach potentially improving quality of life and preventing expensive interventions downstream such as hospitalisation.
All other recommendations should already be happening in most visits. A large number of the recommendations underpin actions that are mandated by other legislation. Those that are not are likely to require no or minimal additional resource to perform but will lead to a more person-centred assessment.
Other factors the committee took into account
The committee drew on NICE guideline on people’s experience in adult social care services : improving the experience of care and support for people using adult social care services and were aware that there is a NICE guideline on advocacy in progress ( advocacy services for adults with health and social care needs ) to which they cross-referred to signpost to recommendations regarding communication and the potential need for advocacy services. They recognised that it is important for social workers to have awareness of the guidelines that could affect the person that they are working with and how they work with them, to be able to give them the support they need and they gave some examples of guidelines that may be relevant in the context of complex needs. They also cross-referred to the NICE guidance for Supporting Adult Carers to highlight the carers’ rights to access to an assessment. The committee used the evidence as well as their own experiential knowledge to draw on three Acts of parliament, the Mental Health Act, the Mental Capacity Act 2005, Equality Act 2010 and the Care Act 2014 as well as the Care Act code of practice and The Care and Support (Assessment) Regulations 2014. They also drew on the professional standards from Social Work England , the Professional Capabilities Framework from the British Association for Social Workers and the Code of Ethics from the British Association for Social Workers .
Recommendations supported by this evidence review
This evidence review supports the following recommendations in the NICE guideline: 1.1.2 to 1.1.4, 1.1.6, 1.1.10, 1.2.1 to 1.2.15 and 1.2.38. It also supports research recommendation 1 on strengths and rights based approach to social work assessment.
References – included studies
Qualitative.
Abendstern 2013
Abenstern 2014
Bolger 2014
Darling 2012
Symonds 2018
- Caiels, J. Milne, A. Beadle-Brown, J. Taking a strenghs-based approach to social work and social care: A literature review. London, NIHR, 2021
- Gray, M. Back to basics: A critique of the strengths perspective in social work. Families in Society: the Journal of Contemporary Social Services, 92, 5–11, 2011
- Human Rights Watch, Unmet needs: Improper social care assessments for older people in England, https://www .hrw.org , 2020
- Prince, a.Ahuja, L. Bramwell, C. Briscoe S. Shaw, L. Nunns, M. O’Rourke,. G. Baron, S. Anderson, R. Research evidence on different strengths-based approaches within adult social work: a systematic review. Southampton: NIHR Health Services and Delivery Research Topic Report, 2020.
- Research in Practice, Human Rights principles in practice – a renewed focus on social justice at the heart of social care. https://www .researchinpractice .org.uk/adults /news-views/2020 /october/human-rights-principles-in-practice-a-renewed-focus-on-social-justice-at-the-heart-of-social-care/ , (2020)
- Slasberg, C., & Beresford, P. Strengths-based practice: Social care’s latest elixir or the next false dawn? Disability & Society, 32 (2), 269–273, 2017
- Social Care Institute for Excellence. Care act 2014: A strengths-based approach, 2015
Appendix A. Review protocols
Review protocol for review question: What is the effectiveness of social work approaches to assessing and reviewing complex care and support needs (including strengths-based approaches)? (PDF, 216K)
Review protocol for review question: Based on the views and experiences of everyone involved, what works well and what could be improved about social work assessment and review of complex care and support needs? (PDF, 229K)
Appendix B. Literature search strategies
Literature search strategies for review question: What is the effectiveness of social work approaches to assessing and reviewing complex care and support needs (including strengths-based approaches)? (PDF, 251K)
Literature search strategies for review question: Based on the views and experiences of everyone involved, what works well and what could be improved about social work assessment and review of complex care and support needs? (PDF, 319K)
Literature search strategies for economic studies (PDF, 388K)
Appendix C. Effectiveness and Qualitative evidence study selection
Study selection for: What is the effectiveness of social work approaches to assessing and reviewing complex care and support needs (including strengths-based approaches)? (PDF, 99K)
Study selection for: Based on the views and experiences of everyone involved, what works well and what could be improved about social work assessment and review of complex care and support needs? (PDF, 98K)
Appendix D. Evidence tables
Evidence tables for review question: what is the effectiveness of social work approaches to assessing and reviewing complex care and support needs (including strengths-based approaches).
No evidence was identified which was applicable to this review question.
Evidence tables for review question: Based on the views and experiences of everyone involved, what works well and what could be improved about social work assessment and review of complex care and support needs?
Download PDF (286K)
Appendix E. Forest plots
Forest plots for review questions: what is the effectiveness of social work approaches to assessing and reviewing complex care and support needs (including strengths-based approaches).
No meta-analysis was conducted for this review question and so there are no forest plots.
Appendix F. GRADE and GRADE-CERQual tables
Grade tables for review question: what is the effectiveness of social work approaches to assessing and reviewing complex care and support needs (including strengths-based approaches), grade cerqual tables for review question: based on the views and experiences of everyone involved, what works well and what could be improved about social work assessment and review of complex care and support needs.
Download PDF (249K)
Appendix G. Economic evidence study selection
Economic evidence study selection for review question: what is the effectiveness of social work approaches to assessing and reviewing complex care and support needs (including strengths-based approaches).
A single economic search was undertaken for all topics included in the scope of this guideline. See Supplement 2 for further information.
Appendix H. Economic evidence tables
Economic evidence tables for review question: what is the effectiveness of social work approaches to assessing and reviewing complex care and support needs (including strengths-based approaches), appendix i. economic model, economic model for review question: what is the effectiveness of social work approaches to assessing and reviewing complex care and support needs (including strengths-based approaches).
No economic analysis was conducted for this review question.
Appendix J. Excluded studies
Excluded studies for review question: what is the effectiveness of social work approaches to assessing and reviewing complex care and support needs (including strengths-based approaches), table 23 excluded studies and reasons for their exclusion.
View in own window
Excluded studies for review question: Based on the views and experiences of everyone involved, what works well and what could be improved about social work assessment and review of complex care and support needs?
Table 24 excluded studies and reasons for their exclusion, excluded economic studies.
No economic evidence was identified for this review. See supplement 2 for further information.
Appendix K. Research recommendations – full details
Research recommendation for review question A2: Based on the views and experiences of everyone involved, what works well and what could be improved about social work assessment and review of complex care and support needs? (PDF, 155K)
Evidence reviews underpinning recommendations 1.1.2 to 1.1.4, 1.1.6, 1.1.10, 1.2.1 to 1.2.15, 1.2.38 and research recommendation 1 in the NICE guideline
These evidence reviews were developed by the National Guideline Alliance
Disclaimer : The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government , Scottish Government , and Northern Ireland Executive . All NICE guidance is subject to regular review and may be updated or withdrawn.
- Cite this Page Needs assessment: Social work with adults experiencing complex needs: Evidence review A. London: National Institute for Health and Care Excellence (NICE); 2022 May. (NICE Guideline, No. 216.)
- PDF version of this title (1.8M)
In this Page
Other titles in this collection.
- NICE Evidence Reviews Collection
Related NICE guidance and evidence
- NICE Guideline 216: Social work with adults experiencing complex needs
Supplemental NICE documents
- Supplement 1: Methods (PDF)
- Supplement 2: Economic searches (PDF)
Related information
- PubMed Links to PubMed
Similar articles in PubMed
- A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. [JBI Libr Syst Rev. 2012] A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. Truglio-Londrigan M, Slyer JT, Singleton JK, Worral P. JBI Libr Syst Rev. 2012; 10(58):4633-4646.
- Promoting and supporting self-management for adults living in the community with physical chronic illness: A systematic review of the effectiveness and meaningfulness of the patient-practitioner encounter. [JBI Libr Syst Rev. 2009] Promoting and supporting self-management for adults living in the community with physical chronic illness: A systematic review of the effectiveness and meaningfulness of the patient-practitioner encounter. Rees S, Williams A. JBI Libr Syst Rev. 2009; 7(13):492-582.
- Palliative care experiences of adult cancer patients from ethnocultural groups: a qualitative systematic review protocol. [JBI Database System Rev Implem...] Palliative care experiences of adult cancer patients from ethnocultural groups: a qualitative systematic review protocol. Busolo D, Woodgate R. JBI Database System Rev Implement Rep. 2015 Jan; 13(1):99-111.
- Review Individual or family casework: Social work with adults experiencing complex needs: Evidence review F [ 2022] Review Individual or family casework: Social work with adults experiencing complex needs: Evidence review F . 2022 May
- Review Integrated health and social care in the community: A critical integrative review of the experiences and well-being needs of service users and their families. [Health Soc Care Community. 2021] Review Integrated health and social care in the community: A critical integrative review of the experiences and well-being needs of service users and their families. Henderson L, Bain H, Allan E, Kennedy C. Health Soc Care Community. 2021 Jul; 29(4):1145-1168. Epub 2020 Oct 15.
Recent Activity
- Needs assessment Needs assessment
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
A guiding framework for needs assessment evaluations to embed digital platforms in partnership with Indigenous communities
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – original draft
Affiliation School of Occupational and Public Health, Toronto Metropolitan University, Toronto, ON, Canada
Roles Data curation, Formal analysis, Investigation, Software, Visualization, Writing – original draft
Affiliation School of Public Health Sciences, University of Waterloo, Waterloo, ON, Canada
Roles Conceptualization, Investigation, Project administration, Resources, Supervision, Writing – review & editing
Affiliation Île-à-la-Crosse School Division, The Northern Village of Île-à-la-Crosse, Île-à-la-Crosse, SK, Canada
Roles Conceptualization, Investigation, Resources, Supervision
Roles Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing
* E-mail: [email protected]
Affiliations DEPtH Lab, Faculty of Health Sciences, Western University, London, ON, Canada, Department of Epidemiology and Biostatistics, Schulich School of Medicine and Dentistry, Western University, London, ON, Canada, Lawson Health Research Institute, London, Ontario, Canada
- Jasmin Bhawra,
- M. Claire Buchan,
- Brenda Green,
- Kelly Skinner,
- Tarun Reddy Katapally

- Published: December 22, 2022
- https://doi.org/10.1371/journal.pone.0279282
- Reader Comments
Introduction
In community-based research projects, needs assessments are one of the first steps to identify community priorities. Access-related issues often pose significant barriers to participation in research and evaluation for rural and remote communities, particularly Indigenous communities, which also have a complex relationship with academia due to a history of exploitation. To bridge this gap, work with Indigenous communities requires consistent and meaningful engagement. The prominence of digital devices (i.e., smartphones) offers an unparalleled opportunity for ethical and equitable engagement between researchers and communities across jurisdictions, particularly in remote communities.
This paper presents a framework to guide needs assessments which embed digital platforms in partnership with Indigenous communities. Guided by this framework, a qualitative needs assessment was conducted with a subarctic Métis community in Saskatchewan, Canada. This project is governed by an Advisory Council comprised of Knowledge Keepers, Elders, and youth in the community. An environmental scan of relevant programs, three key informant interviews, and two focus groups (n = 4 in each) were conducted to systematically identify community priorities.
Through discussions with the community, four priorities were identified: (1) the Coronavirus pandemic, (2) climate change impacts on the environment, (3) mental health and wellbeing, and (4) food security and sovereignty. Given the timing of the needs assessment, the community identified the Coronavirus pandemic as a key priority requiring digital initiatives.
Recommendations for community-based needs assessments to conceptualize and implement digital infrastructure are put forward, with an emphasis on self-governance and data sovereignty.
Citation: Bhawra J, Buchan MC, Green B, Skinner K, Katapally TR (2022) A guiding framework for needs assessment evaluations to embed digital platforms in partnership with Indigenous communities. PLoS ONE 17(12): e0279282. https://doi.org/10.1371/journal.pone.0279282
Editor: Stephane Shepherd, Swinburne University of Technology, AUSTRALIA
Received: June 1, 2022; Accepted: December 2, 2022; Published: December 22, 2022
Copyright: © 2022 Bhawra et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Data are co-owned by the community and all data requests should be approved by the Citizen Scientist Advisory Council and the University of Regina Research Office. Citizen Scientist Advisory Council Contact: Mr. Duane Favel, Mayor of Ile-a-lacrosse, email: [email protected] ; [email protected] University of Regina Research Office contact: Ara Steininger, Research Compliance Officer; E-mail: [email protected] . Those interested can access the data in the same manner as the authors.
Funding: TRK received funding from the Canadian Institutes of Health Research (CIHR) and the Canada Research Chairs Program to conduct this research. The funding organization had no role to play in any part of the study implementation of manuscript generation.
Competing interests: The authors have declared that no competing interests exist.
Community engagement has been the cornerstone of participatory action research in a range of disciplines. Every community has a unique culture and identity, hence community members are the experts regarding their diverse histories, priorities, and growth [ 1 – 3 ]. As a result, the successful uptake, implementation, and longevity of community-based research initiatives largely depends on meaningful community engagement [ 4 – 9 ]. There is a considerable body of evidence establishing the need for ethical community-research partnerships which empower citizens and ensure relevant and sustainable solutions [ 1 – 3 , 10 ]. For groups that have been marginalized or disadvantaged, community-engaged research that prioritizes citizens’ control in the research process can provide a platform to amplify citizens’ voices and ensure necessary representation in decision-making [ 11 ]. Such initiatives must be developed in alignment with a community’s cultural framework, expectations, and vision [ 12 ] to support continuous and meaningful engagement throughout the project. In particular, when partnering with Indigenous communities, a Two-Eyed Seeing approach can provide valuable perspective to combine the strengths of Indigenous and Western Knowledges, including culturally relevant methods, technologies, and tools [ 13 – 15 ].
Many communities have a complicated relationship with research as a result of colonialism, and the trauma of exploitation and discrimination has continued to limit the participation of some communities in academic partnerships [ 16 ]. Indigenous Peoples in Canada experience a disproportionate number of health, economic, and social inequalities compared to non-Indigenous Canadians [ 17 ]. Many of these health (e.g., elevated risk of chronic and communicable diseases) [ 18 – 21 ]), socioeconomic (e.g., elevated levels of unemployment and poverty) [ 19 , 22 – 24 ], and social (e.g., racism and discrimination) [ 19 , 22 – 24 ]) inequities can be traced back to the long-term impacts of assimilation, colonization, residential schools, and a lack of access to healthcare [ 19 , 20 , 22 – 24 ]. To bridge this gap, and more importantly, to work towards Truth and Reconciliation [ 25 ], work with Indigenous Peoples must be community-driven, and community-academia relationship building is essential before exploring co-conceptualization of initiatives [ 26 ].
One of the first steps in building a relationship is to learn more about community priorities by conducting a needs assessment [ 27 , 28 ]. A needs assessment is a research and evaluation method for identifying areas for improvement or gaps in current policies, programs, and services [ 29 ]. When conducted in partnership with a specific community, needs assessments can identify priorities and be used to develop innovative solutions, while leveraging the existing knowledge and systems that communities have in place [ 30 ]. Needs assessments pave the path for understanding the value and applicability of research for community members, incorporating key perspectives, and building authentic partnerships with communities to support effective translation of research into practice.
For rural, remote, and northern communities within Canada, issues related to access (e.g., geographic location, transportation, methods of communication, etc.) pose significant barriers to participation in research and related initiatives [ 31 ]. Digital devices, and in particular, the extensive usage of smartphones [ 32 ] offers a new opportunity to ethically and equitably engage citizens [ 33 ]. Digital platforms (also referred to as digital tools) are applications and software programs accessible through digital devices. Digital platforms can be used for a variety of purposes, ranging from project management, to healthcare delivery or mass communication [ 34 ]. Digital infrastructure–the larger systems which support access and use of these digital platforms, including internet, satellites, cellular networks, and data storage centres [ 34 ]. The Coronavirus (COVID-19) pandemic has catalyzed the expansion of digital technology, infrastructure and the use of digital devices in delivering essential services (e.g., healthcare) and programs to communities [ 35 , 36 ].
While digital platforms have been used in Indigenous communities for numerous initiatives, including environmental mapping initiatives (e.g., research and monitoring, land use planning, and wildlife and harvest studies) [ 37 , 38 ] and telehealth [ 39 ], there has largely been isolated app development without a corresponding investment in digital infrastructure. This approach limits the sustainability of digital initiatives, and importantly does not acknowledge an Indigenous world view of holistic solutions [ 39 ].
Thus given the increasing prominence of digital devices [ 39 , 40 ], it is critical to evaluate the conceptualization, implementation, and knowledge dissemination of digital platforms. To date, there is little guidance on how to evaluate digital platforms, particularly in partnership with rural and remote communities [ 41 ]. A review of recent literature on community-based needs assessments uncovered numerous resources for conducting evaluations of digital platforms, however, a key gap is the lack of practical guidance for conducting needs assessments in close collaboration with communities in ways that acknowledge existing needs, resources, supports and infrastructure that also incorporates the potential role of digital platforms in addressing community priorities.
This paper aims to provide researchers and evaluators with a framework (step-by-step guide) to conduct needs assessments for digital platforms in collaboration with Indigenous communities. To achieve this goal, a novel needs assessment framework was developed using a Two-Eyed Seeing approach [ 13 – 15 ] to enable the identification of community priorities, barriers and supports, as well as existing digital infrastructure to successfully implement digital solutions. To demonstrate the application of this framework, a community-engaged needs assessment conducted with a subarctic Indigenous community in Canada is described and discussed in detail.
Framework design and development
This project commenced with the design and development of a new framework to guide community-based needs assessments in the digital age.
Needs assessments
Needs assessments are a type of formative evaluation and are often considered a form of strategic or program planning, even more than they are considered a type of evaluation. Needs assessments can occur both before and during an evaluation or program implementation; however, needs assessments are most effective when they are conducted before a new initiative begins or before a decision is made about what to do (e.g., how to make program changes) [ 29 ]. Typically, a needs assessment includes: 1) collecting information about a community; 2) determining what needs are already being met; and 3) determining what needs are not being met and what resources are available to meet those needs [ 42 ].
Framework development
Based on existing literature, community consultation, and drawing expertise from our team of evaluation experts who have over a decade of experience working with Indigenous communities on a range of research and evaluation projects, a novel framework was developed to guide community-based needs assessments focused on the application of digital platforms.
This framework (see Fig 1 ) is driven by core questions necessary to identify community priorities that can be addressed by developing and implementing digital platforms. Through team discussion and community consultation, five key topic areas for the assessment of community needs were identified: i) current supports; ii) desired supports; iii) barriers; iv) community engagement; and v) digital access and connectivity. A series of general questions across the five needs assessment topic areas were developed. Thereafter, a set of sub-questions were embedded in each key topic area.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0279282.g001
The Guiding Framework outlines an approach for conducting community needs assessments which can be adapted across communities and jurisdictions. This framework offers a flexible template that can be used iteratively and applied to various community-engaged needs assessments in a range of areas, including but not limited to community health and wellness projects. The questions assigned to each topic area can be used to guide needs assessments of any priority identified by community stakeholders as suitable for addressing with digital platforms.
Needs assessment methods
The Guiding Framework was implemented in collaboration with a subarctic Indigenous community in Canada, and was used to identify key community priorities, barriers, supports, and existing digital infrastructure which could inform the design and implementation of tailored digital platforms.
Using an environmental scan of relevant documents and qualitative focus groups and interviews, a needs assessment was conducted with the Northern Village of Île-à-la-Crosse, Saskatchewan, Canada between February and May 2020.
This project is governed by a Citizen Scientist Advisory Council which included researchers, Knowledge Keepers, Elders, and youth from Île-à-la-Crosse. The study PI (TRK) and Co-Investigator (JB) developed a relationship with key decision-makers in Île-à-la-Crosse in 2020. Through their guidance and several community visits, the decision-makers introduced the research team to Elders, youth, and other community members to gain a better understanding of current priorities and needs in Île-à-la-Crosse. The research team developed relationships with these community members and invited them to join the Council to formally capture feedback and plan ongoing projects to promote health and wellbeing in the community. The Council represents the needs and interests of the community, and guides the project development, implementation, and evaluation. Council members were provided with Can $150 (US $119.30) as honoraria for each meeting to respect their time, knowledge, and contributions.
Written consent was obtained from all focus group participants and verbal consent was obtained from all key informants participating in interviews. This study received ethics clearance from the research ethics boards of the University of Regina and the University of Saskatchewan through a synchronized review protocol (REB# 2017–29).
Established in 1776, Île-à-la-Crosse is a northern subarctic community with road access in northwest Saskatchewan. Sakitawak, the Cree name for Île-à-la-Crosse, means “where the rivers meet,” hence the community was an historically important meeting point for the fur trade in the 1800s [ 43 , 44 ] The community lies on a peninsula on the Churchill River, near the intersections with the Beaver River and Canoe River systems. Île-à-la-Crosse has a rich history dating back to the fur trade. Due to its strategic location, Montreal-based fur traders established the first trading point in Île-à-la-Crosse in 1776, making the community Saskatchewan’s oldest continually inhabited community next to Cumberland House [ 45 ]. In 1821, Île-à-la-Crosse became the headquarters for the Hudson’s Bay Company’s operations in the territory. In 1860, the first convent was established bringing Western culture, medical services, and education to the community.
Île-à-la-Crosse has a population of roughly 1,300 people [ 19 ]. Consistent with Indigenous populations across Canada, the average age of the community is 32.7 years, roughly 10 years younger than the Canadian non-Indigenous average [ 19 ]. Census data report that just under half (44%) of the community’s population is under the age of 25, 46.3% are aged 25–64, and 9.3% aged 65 and over [ 19 ]. Members of the community predominantly identify as Métis (77%), with some identifying as First Nations (18%), multiple Indigenous responses (1.2%), and non-Indigenous (2.7%) [ 19 ]. Many community members are employed in a traditional manner utilizing resources of the land (e.g., hunting, fishing, trapping), others in a less traditional manner (e.g., lumbering, tourism, wild rice harvesting), and some are employed through the hospital and schools. The community currently has one elementary school with approximately 200 students from preschool to Grade 6, and one high school serving Grades 7–12 with adult educational programming. Île-à-la-Crosse has a regional hospital with Emergency Services, which includes a health services centre with a total of 29 beds. Other infrastructure of the community includes a Royal Canadian Mounted Police (RCMP) station, a village office, volunteer fire brigade, and a catholic church [ 46 ].
Needs assessment approach
Île-à-la-Crosse shared their vision of integrating digital technology and infrastructure as part of its growth, thus the needs assessment was identified as an appropriate method to provide the formative information necessary to understand what the needs are, including who (i.e., players, partners), and what (i.e., information sources) would need to be involved, what opportunities exist to address the needs, and setting priorities for action with key community stakeholders [ 47 ]. As a starting point and rationale for this needs assessment, the community of Île-à-la-Crosse values the potential of technology for improving health communication, information reach, access to resources, and care, and was interested in identifying priorities to begin building digital infrastructure. Given the timing of the COVID-19 pandemic, being responsive to community health needs were key priorities that they wanted to start addressing using a digital platform. This needs assessment facilitated and enabled new conversations around key priorities and next steps.
The evaluation approach was culturally-responsive and included empowerment principles [ 48 – 50 ]. Empowerment evaluation intends to foster self-determination. The empowerment approach [ 50 ] involved community members–represented through the Citizen Scientist Advisory Council–engaging in co-production of the evaluation design and implementation by establishing key objectives for the evaluation, informing evaluation questions, building relevant and culturally responsive indicators, developing focus group guides, leading recruitment and data collection, and interpreting results [ 51 ]. In this way, the approach incorporated local community and Indigenous Knowledges as well as Western knowledge, in a similar approach to Two-Eyed Seeing [ 13 – 15 ]. Using these needs assessment evaluation results, the community will identify emerging needs and potential application issues, and work with the researchers to continue shaping project development and implementation.
Two-Eyed Seeing to embed digital platforms
Two-Eyed Seeing as described by Elder Albert Marshall [ 13 , 14 ], refers to learning to see with the strengths of Indigenous and Western Knowledges. Our engagement and overall approach to working with the community of Île-à-la-Crosse takes a Two-Eyed Seeing lens, from co-conceptualization of solutions, which starts with understanding the needs of the community. All needs are a result of direct Indigenous Knowledge that was provided by the Advisory Council. Indigenous Knowledge is not limited to the knowledge of Elders and Traditional Knowledge Keepers; however, they play a critical role in guiding that knowledge through by providing historical, geographic, and cultural context. Moreover, the Knowledge Keepers can be key decision-makers in the community, and in our case, they were key informants who participated in this needs assessment. Every aspect of needs assessment was dependent on the Advisory Council and Key informants providing the Indigenous Knowledge that the research team needed to tailor digital solutions. As a result, Two-Eyed Seeing approach informed all aspects of the research process.
As we are working to develop, and bring digital platforms and technologies (i.e., Western methods) to address key community priorities, Indigenous Knowledge is central to the overall project. Indigenous Elders, decision-makers, and Advisory Council members are bringing both their historical and lived experience to inform project goals, key priority areas, target groups, and methods. Île-à-la-Crosse is a predominantly Metis community, which differs in culture from other Indigenous communities in Canada—First Nations and Inuit communities. Ceremony is not a key part of community functioning; thus, specific cultural ceremonies were not conducted upon advice of the Advisory Council. Instead, the knowledge of historical issues, challenges, and success stories in the community is considered Indigenous Knowledge for this needs assessment, and more importantly, this Indigenous Knowledge informed the focus areas and next steps for this project. Overall, the spirit of collaboration and co-creation which combined Western research methods/technology with Indigenous Knowledge and expertise is considered Two-Eyed Seeing in this project. This lens was taken at all phases, from the engagement stage to Advisory Council meetings, to planning and executing the needs assessment and next steps.
Data collection
In order to obtain an in-depth understanding of the key priorities and supports within the community of Île-à-la-Crosse, this needs assessment used a qualitative approach. An environmental scan was conducted in February 2020 of current school and community policies and programs. Published reports, meeting memos, community social media accounts, and the Île-à-la-Crosse website were reviewed for existing policies and programs. The Citizen Scientist Advisory Council identified appropriate data sources for the document review and corroborated which programs and initiatives were currently active in the community.
Qualitative data were collected from key decision-makers and other members within the community. A purposeful convenience sampling approach was employed to identify members of the community who could serve on the Council and participate in focus group discussions. Key decision makers and existing Council members recommended other community members who could join the focus group discussions to provide detailed and relevant information on community priorities, digital infrastructure, supports, and challenges. Two focus groups were conducted by members of the research team in Île-à-la-Crosse with the Council in May 2020. Focus group participants were asked to describe community priorities, supports, and barriers, as well as experience and comfort with digital platforms. Each focus group had four participants, were two-hours in length, and followed an unstructured approach. Three key informant interviews were conducted in Île-à-la-Crosse between February and April 2020. One-hour interviews were conducted one-on-one and followed a semi-structured interview format. The focus groups and key informant interviews were led by the study PI, TRK, and Co-Investigator, JB, who have extensive training and experience with qualitative research methods, particularly in partnership with Indigenous communities. Focus groups and key informant interviews were conducted virtually using Zoom [ 52 ]. The key informant interviews and focus groups were audio-recorded and transcribed. All data were aggregated, anonymized, and securely stored in a cloud server. Data are owned by the community. Both the Council and the research team have equal access to the data.
Data analysis
All documents identified through the environmental scan were reviewed for key themes. A list of existing school and community programs was compiled and organized by theme (i.e., education-focused, nutrition-focused, health-focused, etc.). Follow-up conversations with key informants verified the continued planning and provision of these programs.
Following the 6-step method by Braun and Clarke (2006), a thematic analysis was conducted to systematically identify key topic areas and patterns across discussions [ 53 ]. A shortlist of themes was created for the key informant interviews and focus groups, respectively. A manual open coding process was conducted by two reviewers who reached consensus on the final coding manual and themes. Separate analyses were conducted for key informant interviews and focus group discussions; however, findings were synthesized to identify key themes and sub-themes in key priorities for the community, community supports and barriers, as well as digital connectivity and infrastructure needs.
Needs assessment findings
The needs assessment guiding framework informed specific discussions of key issues in the community of Île-à-la-Crosse. Key informant interviews and focus group discussions commenced by asking about priorities–“what are the key areas of focus for the community?” In all conversations–including a document review of initiatives in Île-à-la-Crosse–health was highlighted as a current priority; hence, questions in the guiding framework were tailored to fit a needs assessment focused on community health. The following five overarching evaluation questions were used to guide the evaluation: i) What are the prominent health issues facing residents of Île-à-la-Crosse?; ii) What supports are currently available to help residents address prominent health issues in the community?; iii) What types of barriers do community members face to accessing services to manage their health?; iv) How is health-related information currently shared in the community?; and v) To what extent are health services and information currently managed digitally/electronically? The evaluation questions were kept broad to capture a range of perspectives. An evaluation matrix linking the proposed evaluation questions to their respective sub-questions, indicators, and data collection tools is outlined in Table 1 .
https://doi.org/10.1371/journal.pone.0279282.t001
Feedback on each needs assessment topic area is summarized in the sections below. Sample quotes supporting each of the key topic areas is provided in Table 2 .
https://doi.org/10.1371/journal.pone.0279282.t002
Key priorities
Four priorities were identified through the focus groups, key informant interviews, and document review ( Fig 2 ). Given the timing of the discussion, the primary issue of concern was the COVID-19 pandemic. Many community members were worried about contracting the virus, and the risk it posed to Elders in the community. Of greater concern, however, was how COVID-19 exacerbated many existing health concerns including diabetes and hypertension in the community. For example, routine procedures were postponed and community members with other health conditions were not receiving routine healthcare during the height of the pandemic. The St. Joseph’s Hospital and Health Centre services Île-à-la-Crosse and bordering communities, hence maintaining capacity for COVID-19 patients was a priority. COVID-19 exposed existing barriers in the healthcare system which are described in greater detail in the barriers to community health section.
https://doi.org/10.1371/journal.pone.0279282.g002
Another priority discussed by many community members was climate change and the environment. Community members noted that changes in wildlife patterns, land use, and early winter ice road thaw were areas of concern, particularly due to the impact these factors have on traditional food acquisition practices (i.e., hunting) and food access. For instance, the geographic location of Île-à-la-Crosse is surrounded by a lake, and the main highway which connects the community to the land has experienced increased flooding in the past few years.
In addition to posing immediate danger to community members, food security and sovereignty are also closely linked to road access. While the community produces some of its own food through the local fishery and greenhouses, Île-à-la-Crosse is still dependent on a food supply from the south (i.e., Saskatoon). During COVID-19, food access was further restricted due to limited transport and delivery of food products, which increased the risk of food insecurity for community members. Food insecurity was believed to be of bigger concern for Elders in the community compared to younger members. Younger community members expressed having the ability to source their own food in a variety of capacities (e.g., fishing in the lake), whereas Elders rely more heavily on community resources and support (e.g., grocery stores, friends, and family).
Community members also discussed issues surrounding mental health and wellbeing. This topic was of particular concern for youth and Elders in the community. Community members discussed the importance of identifying covert racism (vs. discrimination) that exists within health services that exacerbated mental health issues and care, as well as developing coping strategies, resilience, and supports to prevent mental health crises. Key informants emphasized the need to minimize the stigma around mental health and focus on holistic wellbeing as they work to develop strategies to improve community wellness.
Community health supports
Île-à-la-Crosse has been working on developing supports to improve community health through various initiatives. A document review identified a community-specific wellness model which has informed program development and planning over the past few years. The key components of the Île-à-la-Crosse wellness model are: i) healthy parenting; ii) healthy youth; iii) healthy communities; iv) Elders; v) healing towards wellness; and vi) food sovereignty. The Elders Lodge in the community provides support for holistic wellbeing by promoting intergenerational knowledge transmission, guidance to youth and community members, as well as land-based activities which improve bonding, cultural awareness, and mental and spiritual well-being among community members. The Elders Lodge hosts both drop-in and organized events.
Several initiatives have been developed to support food sovereignty in the community, including a greenhouse program where fruits and vegetables are grown and shared locally. This program is run in partnership with the school to increase food knowledge and skills among youth. In addition, after-school programs including traditional food education (i.e., cooking classes) and land-based activities (i.e., berry picking) led by Elders support the goals of the wellness model. The community is currently working on developing additional programs dedicated to improving mental wellness among adults, youth, and Elders.
Barriers to community health
When key informants were asked to identify barriers to community health, they described delays in access to timely health information. For example, daily COVID-19 tests conducted at the regional health centre in Île-à-la-Crosse were relayed to the provincial health authority; however, information about the total number of COVID-19 cases could take up to one week to be sent back to the community. This time lag restricted community decision-makers’ ability to enact timely policy (i.e., contact tracing) and rapidly respond to managing cases.
A second barrier that was raised by community members was a delay in access to timely healthcare. The Île-à-la-Crosse hospital is a regional health service centre serving the community as well as surrounding areas. Community members noted that the load often exceeded the capacity of the single hospital, and some patients and procedures were relocated to hospitals and clinics in the larger city of Saskatoon, Saskatchewan. This was reported to be challenging for many community members as it was associated with longer wait times, long commutes, and sometimes required time off work. Many of these challenges were exacerbated during the COVID-19 pandemic. As a result of the pandemic, many medical centres and hospitals postponed routine and elective medical procedures in an attempt to accommodate the overwhelming influx of patients who contracted COVID-19. In addition, community members were advised to avoid spending time in health centres to limit risk of exposure to the virus. These COVID-related changes further delayed access to timely healthcare for many community members of Île-à-la-Crosse.
Several community members reported experiencing institutional racism in healthcare and social service settings outside of Île-à-la-Crosse. This was particularly exacerbated during the COVID-19 movement restrictions, where community members faced significant difficulties in accessing services and care in larger urban centres, and experienced further discrimination due to the stigma of COVID-19-related rumours about communities in the north.
Lastly, community members discussed a lack of awareness about some health topics, including where and how to access reliable health information. Some community members attributed this lack of awareness to a general distrust in government health information due to a history of colonialism and exploitation in Canada, which likely contributed to increased misinformation about COVID-19 risk and spread.
Health communication
The primary modes of communication within Île-à-la-Crosse are radio and social media. These platforms were used throughout the pandemic to communicate health information about COVID-19 case counts and trends. Community members also reported obtaining health information from healthcare practitioners (i.e., for those already visiting a healthcare provider), Elders, and the internet. Key informants indicated an interest in improving digital infrastructure to enable sharing of timely and accurate health information with community members and minimize misinformation. Key informants also reported room for improvement in the community’s digital health infrastructure, particularly in improving timely communication with community members, and to inform decision-making in crisis situations.
Digital infrastructure and connectivity
Île-à-la-Crosse has its own cell tower which offers reliable access to cellular data. The community also has access to internet via the provincial internet provider–SaskTel, as well as a local internet provider—Île-à-la-Crosse Communications Society Inc. Key informants and community members confirmed that most individuals above 13 years of age have access to smartphones, and that these mobile devices are the primary mode of internet access. However, it was unclear whether everyone who owns smartphones also has consistent data plans or home internet connections. Key informants described the great potential of digital devices like smartphones to increase the speed and accuracy of information sharing. Discussions with both key informants and community members suggested the need for a community-specific app or platform which could provide timely health information that was tailored to the community’s needs.
Community members noted that expanding digital infrastructure had to be paired with efforts to improve digital literacy–particularly as it relates to data security, privacy, and online misinformation. A separate initiative was discussed which could work to improve digital literacy among youth and Elders, as this would improve both the uptake of digital health platforms, as well as their usefulness and application. Key informants discussed the importance of building digital infrastructure that would enable data sovereignty, self-governance, and determination. The key informants, who are also primary decision-makers in the community, described opportunities for ethical development of digital platforms that would ensure that data is owned by the community.
Needs assessments are commonly the first step in understanding specific community needs, [ 27 , 28 ]; however, few evaluation frameworks provide practical guidance on how to engage communities in needs assessments [ 41 ]. This paper provides a step-by-step guide for conducting needs assessments in collaboration with communities in the digital age. Using the series of questions outlined in the Guiding Framework, researchers and evaluators can gain an in-depth understanding of a community’s priorities, needs, existing capacity, and relevant solutions.
The Guiding Framework was critical to establishing a partnership with the community of Île-à-la-Crosse, as it enabled the research team to obtain detailed insight into their priorities–in this case, community health–as well as community capacity. Taking a Two-Eyed Seeing approach [ 15 ], conversations with the community highlighted strengths of Western digital technology and the diversity of Indigenous Knowledges for addressing priorities [ 13 ]. This approach was also important to establishing trust and respect for the variety of perspectives that could be used to address community priorities. The resulting partnership also enabled the conceptualization of tangible action items that were aligned with current and future priorities–a key factor in the sustainability and feasibility of community-based initiatives [ 4 – 8 , 54 ].
Challenges and opportunities for using digital platforms for priorities identified by needs assessment
Many rural and remote communities face similar challenges and share common priorities with Île-à-la-Crosse. For example, resource and service access, including food and other essential supplies, healthcare, and internet connectivity are issues faced by many rural and remote communities across Canada [ 55 – 60 ]. Key informants and community members from our partner community corroborated these access issues, particularly in relation to public health. Given the potential for digital technology to bridge access gaps, it has become pertinent to invest in digital infrastructure and platform development.
Research has shown that in many rural and remote communities, smartphone ownership is not the limiting factor–it is internet inequity, which is defined as differential internet access based on wealth, location (urban, rural, or remote), gender, age, or ethnicity [ 61 ]. The United Nations has declared internet access a human right [ 10 ], which makes it imperative to develop digital infrastructure such as internet connectivity to improve digital accessibility. Île-à-la-Crosse has its own cell tower which offers reliable access to cellular data. The community of Île-à-la-Crosse also has access to consistent and dedicated internet service through a provincial internet provider and local internet provider. The needs assessment showed that the universality of smartphone ownership combined with good internet connectivity lays the foundation for the development of tailored, culturally appropriate digital health platforms in communities like Île-à-la-Crosse.
In particular, the needs assessment revealed that smartphone apps, which most citizens are well-versed with, can be used to provide local services and access to resources. For example, a locally developed app can connect the Mayor’s office with community members in real-time to provide updates on COVID-19 outbreaks. Apps also have the potential to connect communities to resources within and outside of the community [ 35 , 57 ]. For example, advanced artificial intelligence algorithms can be used to anticipate community needs prior to urgent crises like COVID-19, environmental disasters, or food crises [ 35 , 62 – 65 ]. To date, the issue has not been the lack of technology or ability to bridge this gap for rural and remote communities. Instead, larger systemic inequities have limited our ability to co-create local solutions for global problems by decentralizing technology that is widely available [ 35 , 66 ], which highlights upstream inequities in developing digital platforms.
Recommendations for inclusive digital needs assessments
Given the widespread adoption of digital technology, digital platforms can provide rich data to identify and address community crises [ 2 , 3 , 35 ]. Importantly, co-created digital platforms can be used to share knowledge in real-time with community members and other stakeholders to enable remote engagement, which is especially important during crisis situations such as a pandemic [ 2 , 3 , 35 ]. As we implement creative digital platforms in varied programs or research projects, we must also integrate this digital perspective into the evaluation process. Research and evaluation literature has well established approaches to needs assessment evaluations [ 29 , 42 , 67 ]; however, in the 21st century, we need to account for the use and application of digital platforms in community-focused initiatives. To identify how and where digital platforms can play a role in addressing community priorities, we propose several recommendations for inclusive community-based needs assessments.
First, at the crux of all community-based needs assessments is relationships. A relationship built on respect, reciprocity, mutual understanding, and prioritizing the needs and vision of communities is essential for sustainable impact. The First Nations OCAP® principles [ 68 ] informed conversations between the research team and community about data ownership and control. These principles include ownership of knowledge and data, control over all aspects of research, access to information about one’s own community, and possession or control of data [ 68 ]. The OCAP® principles ensure First Nations and other Indigenous Peoples the right to their own information, and also reflect commitments to use and share information in a way that maximizes the benefit to a community, while minimizing harm. Some communities may choose to lead a project, or work closely in collaboration with experts for specific projects. Irrespective of the project dynamics, needs assessments rely on detailed information and context about a community for a project to succeed.
Second, it is important for researchers and evaluators to gain an understanding of the current digital infrastructure and connectivity in the community. The needs assessment framework ( Fig 1 ) includes relevant questions for identifying data and WIFI access in a community, penetration of digital devices, and existing digital infrastructure. Even for community-based initiatives that are not focused on a digital platforms, digital technologies will inevitably be a part of the solution, a barrier, or both. Hence the digital landscape has become part of the context that we must capture and understand in a needs assessment to better design and develop programming, policies, and other initiatives.
Third, it is important to ask the question of where and how a digital tool or platform could help. Are there gaps that digital platforms can help address or fill? In rural and remote communities, in particular, digital platforms can provide access to real-time information and services not otherwise available. For example, Telehealth [ 69 , 70 ] in the Canadian north offers citizens access to essential healthcare services, including video appointments with medical specialists. Prior to Telehealth, many residents would need to fly into bigger cities in the nearest province to access health care [ 55 ].
Lastly, an understanding of the broader context which affects a community’s ability to adopt digital platforms is critical to the success of digital initiatives. This includes, but is not limited to, capturing data on socioeconomic status and the accessibility of internet-connected digital devices. Digital platforms should help to bridge the divide in resource, service, and information access–not widen the gap. For some communities, this may require working on building digital infrastructure and obtaining dedicated funds to expand access prior to implementing digital initiatives. In addition, digital literacy cannot be taken for granted. Digital literacy refers to individuals’ ability to not only use digital devices, but according to Eshet-Alkalai [ 71 ], “includes a large variety of complex cognitive, motor, sociological, and emotional skills, which users need in order to function effectively in digital environments.” In its simplest form, digital literacy may include the ability to navigate digital platforms, download apps, and communicate electronically. Other more specific skills include ability to read and understand instructions, terms and services, as well as data privacy and security statements [ 72 – 74 ] As part of a needs assessment, identifying digital literacy within a community is an important step to safe, ethical, and relevant digital tool development.
Considering the challenges, immense potential, and learnings from applying the Guiding Framework, a tailored digital platform was conceptualized called Sakitawak Health.
Development of Sakitawak Health
Sakitawak Health is a culturally-responsive digital epidemiological platform to monitor, mitigate, and manage COVID-19 outbreaks. The needs assessment concluded that digital platforms can be used for emerging or other existing population health crises within Île-à-la-Crosse and potentially other Indigenous communities. Moreover, to co-create digital platforms, the Île-à-la-Crosse Citizen Scientist Advisory Council identified key features to embed in CO-Away, including free virtual care for citizens via a smartphone app at the frontend, and access to anonymized community data on the backend for decision-makers.
The app will provide three key precision medicine services that are specific to each citizen: 1) continuous risk assessment of COVID-19 infection; 2) evidence-based public health communication; and 3) citizen reporting of food availability, access to public services, and COVID-19 symptoms and test results. These culturally-responsive features have been co-created with Métis decision-makers in Île-à-la-Crosse based on imminent community needs and preferences. CO-Away will enable real-time data collection through continuous citizen engagement to inform municipal jurisdictional policies.
There are three guiding principles for developing Sakitawak Health: I) Citizen empowerment and data ownership: Active engagement is enabled through app features such as visualizing community risk. More importantly, the community owns the data to ensure data sovereignty; II) Privacy: Utilizing a cutting-edge methodology called federated machine learning, we will develop artificial intelligence algorithms that stores sensitive data such as participant location on mobile devices itself (i.e., sensitive data are not stored in external servers); III) Security and scalability: The backend server will be located in Cloud in Canada, which allows for horizontal and vertical scalability (i.e., the potential for developing multiple frontend apps and decision-making dashboards).
Recognizing the importance of data sovereignty and Indigenous self-governance
Data sovereignty and social justice are important aspects of community-based work, particularly for communities that have experienced discrimination or systemic inequities [ 2 , 75 ]. Data sovereignty refers to meaningful control and ownership of one’s data [ 76 ]. For Indigenous communities in Canada, self-determination and self-governance are of paramount importance given the colonial history of oppression, trauma, and disenfranchisement [ 77 ], and data sovereignty and ownership of digital platforms can promote that independence. In conducting digital community-based needs assessments, the application of a Two-Eyed Seeing lens enables us to leverage strengths of both Indigenous and Western Ways of Knowing to help focus on key priorities and develop solutions.
The engagement and overall approach to working with the community of Île-à-la-Crosse applied a Two-Eyed Seeing lens. In the needs assessment with Île-à-la-Crosse, Two-Eyed Seeing involved incorporation of Métis Knowledge during team engagements, which ensured that any digital platforms developed would incorporate Indigenous Knowledge to promote data sovereignty. All priorities identified within this manuscript are a result of direct Indigenous Knowledge that was provided by the Council. Indigenous Knowledge is not limited to the knowledge of Elders and Traditional Knowledge Keepers; however, they play a critical role in guiding that knowledge through by providing historical, geographic, and cultural context. Discussions with Île-à-la-Crosse about data sovereignty centered around citizen ownership of data, community access, and ensuring data privacy and security. The ultimate goal of this approach to data sovereignty is to facilitate decreased dependence on external systems and use digital solutions for Indigenous self-determination and self-governance.
The needs assessment represents the first phase of a larger evaluation strategy to develop and implement culturally appropriate digital platforms for community health. Phase 1 involved identifying core health priorities and desired supports in the community of Île-à-la-Crosse. Based on the needs assessment findings, Phase 2 of this project will involve the development of tailored digital health platforms and programming to support digital literacy. As part of Phase 2, digital literacy programs and tailored digital health platforms will be pilot tested and adapted prior to their implementation. In Phase 3, a process evaluation will be conducted to assess the reach, uptake, and use of digital health platforms and digital literacy programming. Integrated knowledge translation will be conducted during all phases to ensure continuous feedback, communication, and knowledge sharing with all relevant stakeholder groups.
Conclusions
Needs assessments can facilitate important conversations in community-based research and evaluation to learn about key priorities, challenges, and opportunities for growth. The Guiding Framework for Community-Based Needs Assessments to Embed Digital Platforms details a step-by-step approach to begin a conversation with communities to better understand their needs, and to tailor research and evaluation projects focused on embedding digital platforms. In Île-à-la-Crosse, the needs assessment framework has propelled the launch of a timely, community-engaged digital initiative to address key priorities, starting with COVID-19. Overall, tailored platforms can help bridge existing gaps in resource, program, and service access in Indigenous communities, irrespective of their location across the world.
Supporting information
https://doi.org/10.1371/journal.pone.0279282.s001
Acknowledgments
The authors would like to acknowledge the contributions of community members of Île-à-la-Crosse. The Elders, youth, and key decision-makers who are part of the Île-à-la-Crosse Citizen Scientist Advisory Council have been invaluable in providing support, guidance, and cultural training to the research team. The authors also acknowledge the support of the Canadian Internet Registration Authority in advancing the uptake of digital health applications.
- View Article
- Google Scholar
- 2. Smith LT. Decolonizing Methodologies: Research and Indigenous Peoples. London; New York; Dunedin: Zed Books Ltd; University of Otago Press; Distributed in the USA exclusively by St Martin’s Press; 2021. https://doi.org/10.4324/9781315597843-10 .
- 7. Narayan D. Empowerment and Poverty Reduction: A Sourcebook. Washington, D.C.; The World Bank; 2002.
- 8. Cairncross L, Morrell C, Drake J, Brownhill S. Tenants Managing: An Evaluation of Tenant Management Organisations in England. London: Office of the Deputy Prime Minister; 2002.
- 9. Pratchett L, Durose C, Lowndes V, Smith G, Stoker G, Wales C. Empowering communities to influence local decision making: systematic review of the evidence. London: 2009.
- 10. La Rue F. Report of the Special Rapporteur on the Promotion and Protection of the Right to Freedom of Opinion and Expression, Frank La Rue: addendum. 2011.
- PubMed/NCBI
- 19. Statistics Canada. Île-à-la-Crosse, NV [Census subdivision], Saskatchewan and Saskatchewan [Province] (table). Ottawa: 2017. https://doi.org/Statistics Canada Catalogue no. 98-316-X2016001.
- 20. Waldram JB, Herring A, Young TK. Aboriginal Health in Canada: Historical, Cultural, and Epidemiological Perspectives. 2nd editio. Toronto: University of Toronto Press; n.d.
- 22. Central Urban Métis Federation Inc., Kinistin Saulteaux Nation, Saskatoon Health Region. Strengthening the Circle: Partnering for Improved Health for Aboriginal People. Saskatoon, SK: 2010.
- 28. Pavlish CP, Pharris MD. Community-based collaborative action research : a nursing approach. Sudbury, MA: Jones & Bartlett Learning; 2012.
- 42. Stufflebeam DL, Shinkfield AJ. Evaluation theory, models, and applications. 1st ed. San Francisco, CA: Jossey-Bass; 2007.
- 43. McLennan D. Sakitawak Development’s Facebook Page n.d.
- 44. Cameco Corp. Patuanak—English River First Nation—Community Profiles—Community. Cameco North Saskatchewan 2020.
- 45. McLennan D. The Encyclopedia of Saskatchewan: Île-à-la-Crosse n.d. https://esask.uregina.ca/entry/ile-a-la-crosse.jsp .
- 52. Zoom Video Communications Inc. Security guide 2016.
- 68. The First Nations Information Governance Centre. The First Nations Principles of OCAP TM Training Course 2021:1–6. https://fnigc.ca/ocap-training .
- 69. Telehealth 2021. North Heal 2021. https://www.northernhealth.ca/services/digital-health/telehealth .
- 75. Kukutai T, Taylor J, editors. Indigenous Data Sovereignty: Toward an Agenda. The Australian National University Press; 2016. https://doi.org/10.1109/IPDPSW.2014.214 .
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Approaches to community needs assessment: a literature review

1995, Journal of Advanced Nursing
Related Papers
Journal of Advanced Nursing
Sarah A Cowley
Journal of Nursing Management
Sarah A Cowley , Sinéad Hanafin
Journal of advanced …
Ronnie Moore
International Journal of Nursing Studies
Journal of Clinical Nursing
Vari M Drennan
RELATED PAPERS
Journal of Public Health
Richard Reading
Journal of Public Health Medicine
mouhamed idhrees
Primary Health Care Research & Development
Sandra Dowling , Sarah A Cowley
Revista da Escola de Enfermagem da USP
Diane Stockton
Community practitioner : the journal of the Community Practitioners' & Health Visitors' Association
Wendy Bateman
Karen Whittaker
Nurse Education Today
Sarah J Neill
Brenda Roche
Flora Cornish
British Journal of Community Nursing
Dean Whitehead
Public Health Nursing
Peter Griffiths
Social Science & Medicine
Astier M. Almedom
Gillian Dalley
Public Health
Health & Social Care in The Community
Siobhan Reilly
African health sciences
dorcas nyanyiwa
Alison While
Clinical Effectiveness in Nursing
Patrick A Crookes
Kate Gerrish
G. Spiers , Suzanne Mukherjee , K. Gridley
Journal of Pediatric Nursing
Rosario Baxter
Kerry Mummery
Archives of Disease in Childhood
Krystyna Makowiecka
Gender Work and Organization
Jane Sandall

RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- Open access
- Published: 17 January 2023
A scoping review of community health needs and assets assessment: concepts, rationale, tools and uses
- Hamid Ravaghi 1 ,
- Ann-Lise Guisset 2 ,
- Samar Elfeky 3 ,
- Naima Nasir 4 ,
- Sedigheh Khani 5 ,
- Elham Ahmadnezhad 6 &
- Zhaleh Abdi 7
BMC Health Services Research volume 23 , Article number: 44 ( 2023 ) Cite this article
25k Accesses
16 Citations
2 Altmetric
Metrics details
Community health needs and assets assessment is a means of identifying and describing community health needs and resources, serving as a mechanism to gain the necessary information to make informed choices about community health. The current review of the literature was performed in order to shed more light on concepts, rationale, tools and uses of community health needs and assets assessment.
We conducted a scoping review of the literature published in English using PubMed, Embase, Scopus, Web of Science, PDQ evidence, NIH database, Cochrane library, CDC library, Trip, and Global Health Library databases until March 2021.
A total of 169 articles including both empirical papers and theoretical and conceptual work were ultimately retained for analysis. Relevant concepts were examined guided by a conceptual framework. The empirical papers were dominantly conducted in the United States. Qualitative, quantitative and mixed-method approaches were used to collect data on community health needs and assets, with an increasing trend of using mixed-method approaches. Almost half of the included empirical studies used participatory approaches to incorporate community inputs into the process.
Our findings highlight the need for having holistic approaches to assess community’s health needs focusing on physical, mental and social wellbeing, along with considering the broader systems factors and structural challenges to individual and population health. Furthermore, the findings emphasize assessing community health assets as an integral component of the process, beginning foremost with community capabilities and knowledge. There has been a trend toward using mixed-methods approaches to conduct the assessment in recent years that led to the inclusion of the voices of all community members, particularly vulnerable and disadvantaged groups. A notable gap in the existing literature is the lack of long-term or longitudinal–assessment of the community health needs assessment impacts.
Peer Review reports
The population-based health approach aims to improve the population’s health, promote community resilience and reduce health inequities across the socioeconomic gradient via inter-sectoral partnerships among community groups, government, healthcare systems, and other stakeholders [ 1 ]. One key feature for adopting a population-based health approach is to ensure that it is grounded on a solid understanding of community health needs and assets by triangulating evidence from service providers and community members on services availability, accessibility, utilization and experience [ 2 , 3 ]. The process of identification of unmet health needs in a population is crucial for local authorities seeking to plan appropriate and effective programmes to meet these needs [ 3 , 4 ]. If these needs are ignored, then there is a risk of a top-down approach for providing health services, reflecting what a few people perceive to be the needs of the population rather than what they actually are [ 4 , 5 ].
In this context, community health needs assessment is a means of developing a comprehensive understanding of a community’s health and health needs as well as designing interventions to improve community health [ 6 ]. Though the process of community health needs assessment can be conducted in several ways, the primary purpose is to provide community leaders or healthcare providers with an overview of local policy, systems, and environmental change strategies currently in place and help to identify areas for improvement [ 7 ]. Community health needs assessment can provide them with a more nuanced understanding of the communities they serve, making them aware of pressing issues that require system-level changes and support their efforts for resource mobilization to initiate innovative programmes [ 8 , 9 ]. The process to gather evidence on community health needs can also serve as a springboard to strengthen community engagement [ 10 ].
In general, needs assessments are usually designed to evaluate gaps between current situations and desired outcomes, along with possible solutions to address the gaps. Recently, there has been a trend to move away from framing a community with a deficit perspective (need-based approach) to focus on community assets and resources, called community health needs and assets assessment [ 11 , 12 ]. In contrast to a need-based perspective which focuses on local deficits and resources outside the community, an asset-based perspective focuses on honing and leveraging existing strengths within the community to address community needs [ 12 , 13 , 14 ].
Studies have shown that community health needs assessment is used widely by different users and across different settings [ 15 , 16 ]. However, these studies varied widely in terms of purpose, process and methods of conducting community health needs assessment. Furthermore, the extent to which an asset-based approach is used is unclear, beyond the inclusion in guidance and recommendations. Thus, to support national or local decision-makers to make informed choices about the scope, tools, methods and use of community health needs and assets assessment, this scoping review of the literature aimed at: 1) Providing conceptual clarity on community health needs and assets assessment, 2) Determining for what purpose and with what methods community health needs and assets assessment are used globally, 3) Drawing the lessons learnt from previous experience with community health needs and assets assessment: what works in what context and under what conditions, 4) Documenting evidence of impact of community health needs and assets assessment, 5) Consolidating tools and methods used to collect evidence/data underpinning community health needs and assets assessment processes.
Search strategy
Ten databases, including PubMed, Embase, Scopus, Web of Science, PDQ evidence, NIH database, Cochrane library, CDC library, Trip, and Global Health Library were searched in February and March 2021. The search strategy was developed through discussion with experts in the field of population health, a research librarian, and a narrative review of the literature. Preliminary search terms were developed by the research team to reflect a number of core concepts including needs, population, needs assessment, assets assessment and participation. The search process was performed by a librarian with expertise in the use of literature databases (SK). The search terms were pilot-tested and agreed upon within the research team. The PubMed database search strategy presented in Additional file 1 .
Inclusion and exclusion criteria
Studies that focus on community health needs and assets assessment in terms of concepts, rationale, uses and tools were considered in both high-income countries (HICs) and low-and middle-income counties (LIMCs). We included studies in the review if they met the following criteria: 1) Papers providing conceptual clarity and explaining rationale for community health needs and (assets) assessment (This can be articles describing community health needs assessment or community assets assessment or community health needs and assets assessments at the same time or separately). The terms capabilities/ strengths/ resources can be used in place of assets and were considered.); 2) Papers describing or evaluating experiences implementing community health needs (and assets) assessment in a single site or multiple sites; 3) Methodological papers describing tools/approaches for community health needs (and assets) assessment; 4) Review of the literature on community health needs (and assets) assessment.
Types of papers not include in the review were: 1) Studies without a clear description of the community health needs and (assets) assessment methods, 2) Studies assessed a single dimension (i.e. health outcomes only, or healthcare providers’ capabilities only such as patient surveys, health outcomes dashboard, health facility assessment), 3) Studies related to a single disease or programme, 4) Studies focused only on engaging individual patient in their own care, and 5) Studies were not in English.
Three reviewers participated in the selection of the relevant studies (HR, ZA, NN). The eligibility and relevance of the articles were determined by two reviewers independently using the above predefined criteria. In the event of disagreement, a consensus was found between all the reviewers about the status of the article.
Data extraction
Separate data extraction forms were developed for the extraction of the three main categories of papers: conceptual, empirical and review papers. Totally, 121 empirical papers (including 6 review papers) and 48 conceptual and methodological papers were reviewed. Following topics were extracted for empirical papers: 1) General characteristics including author(s), year of publication, country of implementation, study objective(s) and study method; 2) Community health needs and (assets) assessment framing including rational, definitions of community health needs and (assets) assessment/ needs/ assets/ community, initiator(s) or user(s) of the process; 3) Key steps of the process, collected data, data collection tools; 4) Community engagement and the level of engagement; 5) Use of community health needs and (assets) assessment findings, impact of community health needs and (assets) assessment; 6) Facilitators and barriers. Data extraction forms are presented in Additional file 2 .
Data extraction forms were pilot-tested prior to the implementation. Two authors (ZA, HR) independently performed a pilot data extraction of a random sample of ten original articles. After piloting, the authors assessed the extracted data in relation to the scoping review questions and revised them accordingly. The content of the form was finalized by discussion within the team. Regarding conceptual papers, two authors (NN and ZA) initially extracted data from three randomly selected papers and subsequently refined and amended the form having research team inputs.
Four reviewers extracted included studies independently. The data extracted were cross-checked by one of the authors and mutual consensus resolved discrepancies. Individual data extraction forms of empirical papers were then merged into a single, unifying document used for the interpretation and presentation of the results. Following typical scoping review methods, the methodological quality of the included articles was not assessed systematically, however, only peer-reviewed articles were included in our review process [ 17 ].
Synthesis of results
Following reading and extracting conceptual papers, a preliminary conceptual framework (Fig. 1 ) was developed and discussed and agreed upon by team members. The integrative synthesis of the evidence was employed. Specifically, it involved the narrative description of concepts and definitions, key steps of the community health needs assessment and barriers and facilitators of the implementing community health needs assessment.
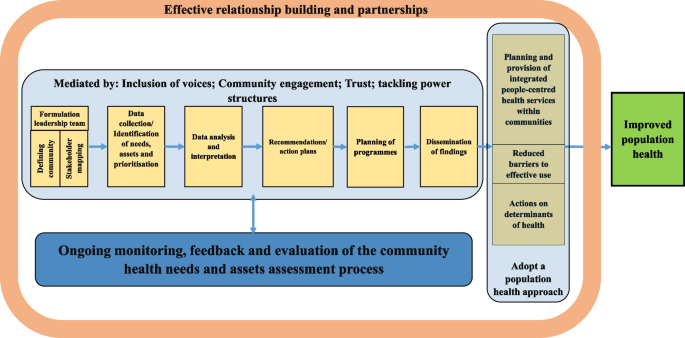
Conceptual framework of the review
The study selection process is summarized in Fig. 2 . Just over 12,000 records were obtained from the ten databases searched. Articles with obviously irrelevant titles were excluded, as were news items, letters, editorials, book reviews, and articles appearing in newsletters or magazines rather than peer review journals. The remaining abstracts were retrieved, read and assessed. A total of 169 articles including both empirical papers and theoretical and conceptual work were ultimately retained for analysis. A list of all studies with a short description, including the year of publication, key focus, study period, and methods, is presented in Additional files 3 and 4 . The first part of the results section focuses on definitions and concepts of community health needs assessment using both conceptual and empirical papers. In the second part of the results section, we describe key steps of the community health needs assessment and tools and methods used to collect data through content analysis of 121 included empirical papers. We also report some important challenges and facilitators faced by included studies while performing community health needs assessment. Role of community participation in the process and the spectrum and types of the participation is discussed in the last part.
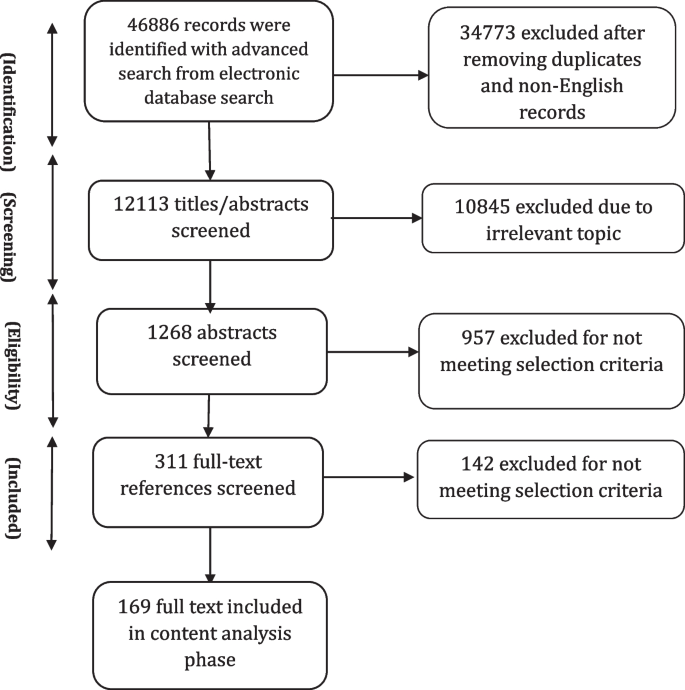
Information flow in scoping review
General characteristics of the included studies
The review showed that community health needs assessment is used widely by different users and across different settings in both HICs and LMICs. Among included empirical studies, 81 (out of 121) were conducted in the United States (US). There were papers from Australia ( n = 4), South Africa ( n = 3), Kenya ( n = 3), Uinted Kingdom (UK) ( n = 2), Canada ( n = 2), China ( n = 2), Dominican Republic ( n = 2), Republic of Ireland ( n = 2), Iran ( n = 2), India (2), Honduras ( n = 1), Netherland ( n = 1), Vietnam ( n = 1), Sudan ( n = 1), New Zealand ( n = 1), Madagascar ( n = 1), Malaysia ( n = 1), Ecuador ( n = 1), Indonesia ( n = 1), Uganda ( n = 1), Taiwan ( n = 1), Kyrgyzstan ( n = 1), Saudi Arabia ( n = 1), Haiti ( n = 1), Honduras ( n = 1) and Korea ( n = 1).
Definition of needs
The review showed “need” was a multi-faceted concept with no universal definition. There was a differentiation between “health need” and “healthcare need” in the reviewed literature. Healthcare needs can benefit from health care (health education, disease prevention, diagnosis, treatment, rehabilitation and terminal care). Healthcare providers usually consider needs in terms of healthcare services that they can supply. However, health needs incorporate the wider social and environmental determinants of health, such as deprivation, housing, diet, education and employment. This broader definition allows looking beyond the confines of the medical model based on health services, to the wider influences on health [ 3 ].
In this review, relatively few empirical studies focus narrowly on healthcare needs, without attention to other determinants of health that can affect health [ 18 , 19 , 20 , 21 , 22 , 23 ]. Most of the included empirical studies looked beyond “physical health needs” to consider wider “social determinants of health” or non-medical factors that can affect a person’s overall health and health outcomes as the conditions—shaped by political, social, and economic forces—in which people are born, grow, live, work, and age [ 24 ]. Notably, the need was recognised as a “dynamic concept” whose definition will vary with time according to context and resources available to address these needs [ 16 ].
Definition of community
In general, “community” has been defined as “people with a basis of common interests and network of personal interactions grouped either based on locality or on a specific shared concerns or both” [ 25 ]. Shared common interests are particularly important as they can be assessed and, hopefully, met at a community level [ 26 ]. Importantly, community is a dynamic concept as individuals can belong to several communities at various times. In our review, community was defined by included studies, particularly those initiated by local authorities or healthcare providers (e.g., hospitals), based on geographical indicators such as county designations or based on the location of the hospital’s/facility’s/authority’s existing or potential service users. Some included empirical studies considered community based on shared interests or characteristics such as race/ethnicity, sexual orientation, or occupation. Medically underserved populations including rural areas [ 27 , 28 , 29 , 30 ], impoverished urban sectors [ 31 ], the homeless [ 32 , 33 , 34 , 35 ], persons in poverty or of low socioeconomic status, vulnerable children and families [ 18 , 28 , 36 , 37 , 38 ], the elderly [ 8 , 39 , 40 , 41 , 42 ], women and girls [ 43 , 44 , 45 , 46 , 47 ], LGBT (Lesbian, gay, bisexual, and transgender) individuals [ 48 , 49 , 50 , 51 ], displaced populations, immigrants and racial, ethnic and religious minority groups [ 12 , 19 , 36 , 42 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 ] and persons with severe and chronic health problems [ 79 ] were considered as a “community” by a number of included studies.
While defining community, a number of its characteristics were determined by included studies including: history, existing groups, physical aspects (i.e. geographic location, community size, its topography and etc.), infrastructure (i.e. health and social care facilities, public transportation, roads, bridges, electricity, mobile telephone services and etc.), demographics (i.e. age, gender, race and ethnicity, marital status, education, number of people in household, first language and etc.), economic conditions, deprivation and/or inequalities, government/politics, community leaders (formal and informal), community culture (formal and informal), existing institutions, crime and community safety, lifestyle and leisure, general health problems and epidemiology.
In our review, community health needs and assets assessment were performed by different organizations as the first step in community health promotion planning, including local health authorities (district/local), community entities [i.e. non-governmental organizations (NGOs), civil society organizations (CSOs), faith-based organizations (FBOs), community-based organizations (CBOs)] and hospitals (public/private). Included studies mostly conducted health needs assessment at the local level (e.g. cities, counties, or other municipalities). The broader understanding of health and its determinants suggests that many public and private entities have a stake in or can affect the community’s health. To engage stakeholders in the process, a number of included empirical studies ( n = 56, 49%) sought representatives from the community that were best positioned to speak about community health based on their specific knowledge or line of work. These stakeholders were individuals from community and entities who may explicitly be concerned with health or not, which varied by the community context and culture. To have a comprehensive overview of a community needs, it was asserted that defining communities needs to be dynamic and socially constructed to take into account all voices and members, especially those not ordinarily included [ 80 ]. Community should be defined in a manner that does not exclude medically underserved, low-income, or minority populations. Integrating community voices is especially important in designing plans and programmes aimed at reducing health disparities in the community [ 58 , 81 , 82 ].
Definition of assets
Overall, there were limited definitions for “community assets” in the reviewed literature. Assets were described as resources, places, businesses, organizations, and people that can be mobilized to improve the community [ 11 , 83 ]. This includes members of the community themselves and their capabilities. Assets can therefore be described as the collective resources which individuals and communities have at their disposal, which protect against adverse health outcomes and promote health status [ 83 , 84 ].
Of 115 included empirical studies, 30 studies addressed community assets while performing community health needs assessment. A wide range of assets, from tangible resources to intangible ones, were considered that can be classified into seven broad categories as follows:
Community demographic characteristics: Literacy rates [ 13 ], youth population [ 58 , 68 ], and elderly population [ 68 ];
Natural capitals: Geographical location and natural resources [ 21 , 81 , 85 ];
Economic and financial capitals: Community business [ 12 , 81 ] community members’ income [ 21 ], and housing land ownership [ 13 ];
Community infrastructure: Level of technology/mobile phone coverage [ 13 , 21 ], transportation [ 86 ], parks and sidewalks [ 12 ], sport and recreational facilities [ 31 , 87 , 88 ], public libraries and community centres [ 88 ];
Community social and educational facilities: Non-profit and non-governmental organizations [ 59 , 87 ], media [ 89 ], educational institutions [ 12 , 31 , 81 , 90 ], faith communities [ 58 , 81 , 90 ], and community associations [ 31 ];
Community health and social facilities: Health and social facilities and providers [ 72 , 81 , 85 , 86 , 89 ], traditional medicine providers [ 72 ], and ongoing health programmes [ 13 , 87 ];
Community’s social and cultural values and resources: Tribal and community culture [ 58 , 68 , 74 , 91 ], cultural diversity [ 81 ], spirituality and religion [ 58 , 74 ], strong family bonds and values [ 59 , 74 ], strong community connections, teamwork and willingness to volunteer [ 21 , 81 , 86 , 91 ], mutual support, social support and networks [ 45 , 58 , 81 , 85 ], unity, community cohesion and collectivity [ 21 , 59 , 74 ], community capacity [ 58 ], community-led activities [ 86 , 91 ], and community values and traditions [ 68 , 74 , 86 ], resiliency [ 58 ], unifying power of communities [ 13 ], community administration units e.g. women’s committees [ 13 ], an existing group of dedicated healthcare providers [ 39 ], a group of concerned citizens [ 39 ], community safety [ 12 ], the knowledge base of the community members themselves [ 39 ] and members’ desire to be healthy [ 58 ].
Various qualitative methods such as individual interviews (one-on-one structured conversations) or focus groups (guided, structured, small group discussions) with community members, or key informants’ interviews (formal and informal conversations with leaders and stakeholder groups) or a combination of these methods were reported as the main methods to collect information on community’s assets among reviewed studies. Of these, focus group was the widely used method in community assets assessment [ 8 , 21 , 31 , 45 , 58 , 59 , 67 , 81 , 82 , 85 , 87 , 90 , 92 , 93 ].
Definition of community health needs (and assets) assessment
The terms “Community Needs Assessment (CNA)”, “Community Health Needs Assessment (CHNA)”, and “Community Health Needs and Assets Assessment (CHNAA)” were used interchangeably in the literature referring to the process of identifying health needs (and assets) of a given community. Since this review focuses on both community needs and assets, we will use the CHNAA term for the description of the process in this paper.
None of the papers reviewed provided a specific definition for CHNAA. In general, reviewed papers defined CHNAA as: A collaborative, community-engaged, systematic, ongoing, continuous, proactive, comprehensive, cyclical, regular, modifying method or process [ 28 , 33 , 69 , 92 , 94 , 95 , 96 , 97 , 98 ]; For the identification, collection, assembly, analysis, distribution, and dissemination of information on key health needs, social needs, concerns, problems, gaps, issues, factors, capabilities, strengths, assets, resources; About communities (or individuals) [ 21 , 23 , 28 , 31 , 33 , 37 , 41 , 45 , 54 , 79 , 89 , 94 , 95 , 96 , 97 , 99 , 100 , 101 , 102 ]; To achieve agreed priorities, create a shared vision, plan actions, garner resources, engage stakeholders, work collaboratively, establish relationships, implement culturally appropriate, multi-sectoral/multilevel intervention strategies, empower residents and enhance community capacity and participation in decision-making process [ 12 , 13 , 20 , 27 , 28 , 37 , 45 , 70 , 79 , 89 , 91 , 92 , 94 , 95 , 97 , 98 , 99 , 101 , 102 , 103 , 104 ]; Towards improving health and wellbeing, building and transforming health of the communities, increasing community benefits, reducing inequalities; Through which primary/secondary healthcare can respond to local and national priorities [ 20 , 23 , 28 , 40 , 51 , 59 , 69 , 97 , 103 , 105 , 106 ].
The included studies listed a number of reasons as the rationale for conducting CHNAA. Legislative requirements were most cited as the main rational for conducting CHNAA, particularly among studies conducted in the UK and US. Since the late 1980s, the concept of health needs assessment has gained increasing prominence within the National Health Service (NHS) in the UK. This has been prompted by a series of policy initiatives requiring health facilities to assess needs of their populations and to use these assessments to set priorities to improve the health of their local population [ 107 , 108 ]. In the US, several national, federal, state, and local funding sources require entities to conduct CHNAA to demonstrate a significant need for their services and programmes to be funded. The most important one is Patient Protection and Affordable Care Act (ACA-2010), requiring non-profit hospitals as tax-exempt entities to perform CHNAAs to maintain non-profit status regularly [ 92 ]. Other reasons were mentioned by included studies as the rationales for conducting CHNAA were: lack of information of health needs of a specific community, to facilitate health research and related interventions in a community, to inform the design of contextually relevant programmes and policies, to develop community health improvement plans or health promotion interventions, to develop or update strategic plans, and to receive resources and funds.
Key steps to conduct CHNAA
The number and nature of CHNAA process steps varied among reviewed studies. However, broadly CHNAAs involved six main steps as follow:
Formulation of a leadership team
Forming a leadership team, which was called by different names such as the steering committee/ the research advisory committee (RAC)/ the collaborative task force/ or the community advisory board (CAB), was known as the preliminary step of a CHNAA process. The steering committee was usually composed of local representatives from local agencies and organizations (e.g. non-profit organizations, community service agencies, media outlets, county and municipal governments, colleges and universities, faith-based organizations, and healthcare providers), community members, community stakeholders and leaders, academic partners, health and social officials, and representatives from the investigator body to help guide the development of the CHNAA project.
Leadership team responsibilities were reported as providing inputs on the research purpose, selecting and verifying study methodology and design, providing inputs and feedback on initial survey/topic content and selecting final survey/ topic guide questions, reviewing survey/topic guide length, and ensuring culturally relevant and resonant wording, comprehension and face validity, and monitoring the progress of the data collection. Feedback and recommendations from the steering committee were incorporated throughout the CHNAA process as well. Steering committees usually met on a regular basis.
Identification of needs, assets and prioritisation
To collect information on community health, needs and assets, both primary and secondary data were utilized by included studies. Secondary data included information on community socio-demographic and indicators on health status, access, utilization and satisfaction with health and social services at different levels (e.g. community, sub-national and national) to develop a picture of the overall community health. Primary data were collected through quantitative and qualitative methods and mixed-methods approaches.
Quantitative studies
Some empirical studies used individual/household surveys as the only source to identify community needs and concerns ( n = 28, 24.%). Surveys were a popular method of gathering opinions, preferences and perceptions of needs. Needs assessment surveys typically have written, closed-ended questions filled through the interview (face to face/telephone) or self-completion (paper or online) by community members. Generally, two main kinds of surveys were used by included studies: a) community health assessment survey, and b) community concerns survey. A number of included studies used health assessment surveys as the key data sources of the CHNAA process ( n = 22, 19%) or along with other types of data, mainly qualitative data ( n = 21, 18.%). Health assessment surveys typically collected information on demographics, socio-economic variables, respondents’ health status, choice of healthcare providers, and healthcare access issues among community members. Survey questionnaires were mostly developed with inputs from the literature review (similar health assessment surveys conducted at the local or national level), community members and project team discussions. Additional file 5 shows the most important data and indicators collected by included studies through conducting community health assessment surveys.
Another form of surveys, used alone or in combination with qualitative methods ( n = 15, 13.5%), was the community concerns survey in which people (community members and/or key informants) are asked to help identify what they see as the most important issues facing their community leading to an inventory of their health priorities [ 12 , 20 , 23 , 27 , 29 , 55 , 69 , 74 , 101 , 103 , 109 , 110 , 111 , 112 , 113 ]. A straightforward way to estimate the needs of a community was to simply ask residents their opinion on what particular services are most needed in the community. The focus of this methodology was to create an agenda based on the perceived needs and concerns of community residents. The concerns surveys were based on either focus group discussion with community members and experts or literature review by the researchers or both. Generally, while filling community concerns survey, individuals were asked to rate the importance of each issue in their community on a scale (e.g. 0 = not important, 5 = extremely important) [ 23 , 27 , 29 , 55 , 74 , 110 ]. Participants could also add and rate concerns or service needs that were not listed. Finally, each health problem identified by the community was weighted based on the frequency it was selected on the survey.
General coverage of the surveys was the population aged 18 or over currently residing in the community for a minimum period of time (at least a few months) and able to provide consent for participation. Most surveys were written, closed-ended questions filled through face to face or telephone interviews or self-completion by community members. In addition to the paper-form survey, some studies used email and social media platforms to allow residents to anonymously complete online surveys [ 29 , 51 , 57 , 96 , 103 , 110 , 114 ]. A few studies reported that residents received monetary or nonmonetary incentives for their participation upon survey completion [ 19 , 71 , 74 , 77 , 110 ]. Sampling techniques commonly used are those that promote participation in CHNAAs such as convenience sampling [ 20 , 35 , 40 , 51 , 52 , 57 , 64 , 65 , 71 , 74 , 75 , 77 , 86 , 96 , 101 , 103 , 104 , 110 , 114 , 115 ]. Only a few studies used random sampling or demonstrated the representativeness of their samples. Their response rates varied between 8 to 95.5%. Most surveys recruited local surveyors and provided them with research training to ensure consistent survey administration to attract community participation. Some studies that assessed health needs among immigrant communities or minority groups recruited bilingual surveyors or/and provided participants with two versions of the instruments, one in the native language to maximize community engagement [ 12 , 27 , 52 , 65 , 71 , 86 , 103 ]. Surveys that took a participatory approach to the design, content, terminology, and language level, were reported more understandable and culturally relevant to the community members [ 52 , 65 , 75 ].
Health needs assessment surveys (both concerns surveys and health assessment surveys) reported limitations to data collection based on the assessment timing, data availability, and sample response. As said earlier, using a convenience sampling and non-representative samples, small sample size and inter-rater reliability between surveyors were among some important methodological limitations reported by these studies, which limited the generalisability of the study findings to the entire community population [ 35 , 57 , 65 , 71 , 74 , 75 , 77 , 96 , 106 , 116 ]. Convenience sampling method and using community events as sampling sites led to sampling bias in some studies (e.g., an over-representation of some specific groups of the population such as women and low –income or high-income groups) [ 57 , 63 , 65 , 66 , 71 , 74 , 75 , 78 , 103 , 114 , 115 ].
Qualitative studies
Among included studies, about 34% ( n = 39) used qualitative methods as the main source of data collection on community needs and assets. Some of these studies justified the use of qualitative approach by explaining how the overreliance on quantitative, population-level data resulted in CHNAAs failing to identify health needs and interests of all community members, particularly those of vulnerable population and underrepresented marginalized segments of the community. In addition, these studies concluded that integrating qualitative methods into the CHNAA process has the potential to involve community members in a more participatory fashion, perhaps improving future collaborations between communities and service providers. Such collaborations can help to design focused initiatives, making them more meaningful and culturally appropriate [ 12 , 59 , 91 , 102 ].
Key informant interviews, individual interviews with community members, focus groups with community members and community forums were among the qualitative data collection techniques used individually or in combination with each other by these studies to collect data on community needs and assets. They asserted that qualitative techniques specifically targeted to underrepresented segments of the population proved to be effective mechanisms to explore the participants’ perceptions on issues surrounding community health needs and assets. The most used technique to elicit community members’ opinions were focus group discussions and key informant interviews.
Small sample size and single-site setting were mentioned as the most cited limitations of the qualitative CHNAAs that limit these studies generalisability. Because the studied communities were unique communities with unique assets, constraints, and health needs, the CHNAA findings cannot be generalised to other communities [ 32 , 39 , 62 , 70 , 72 , 73 , 91 , 117 , 118 ]. Another limitation mentioned by some studies was that the demographic composition of the focus group participants, specifically with regards to race, gender, socio-economic status and age group, did not fully reflect the population of studied community as a whole [ 13 , 61 , 62 , 72 , 97 , 119 ]. Some studies reported that they could not include all influencing key informants in the community to facilitate broader understandings of health needs [ 13 , 120 ].
Mixed- methods studies
A variety of data collection methods were used in a number of included studies to ensure that a comprehensive picture of community health needs and resources was obtained ( n = 48, 42%). Some of these studies were two-phase explanatory mixed-methods studies, with the quantitative phase preceding the qualitative phase ( n = 14, 12%). They conducted targeted focus groups or community listening sessions or interview with community members/key informants following needs assessment survey to supplement the findings from the survey and provide further information about health status, needs of daily living, barrier to health and access to community resources [ 8 , 21 , 41 , 53 , 55 , 66 , 67 , 93 , 94 , 95 , 99 , 113 , 114 , 121 ]. In addition to these studies, some studies used triangulation mixed-method design to obtain complementary qualitative and quantitative data on community health needs and issues ( n = 13, 11%). These studies confirmed that using multiple data sources ensured researchers obtain a complete picture of the community health needs. Applying qualitative methods in the form of focus groups and semi-structured interviews enabled exploration of problems and needs within their social context and provided a wider perspective on issues raised. However, to conduct such studies CHNAA teams had to have members who have qualitative and quantitative expertise. There were some limitations specific to the mixed-method studies, including lack of rigor in integrating qualitative and quantitative findings, relying heavily on quantitative data for health need determination, and absence of the voices of the communities most in need [ 69 , 91 ].
Data analysis and interpretation
Qualitative data from focus group discussions and key informant interviews were mainly audio-recorded and transcribed verbatim by the research team and all identifying information was removed. Different analytical approaches, mostly content analysis and thematic analysis, were used to identify main themes related to assets, needs and gaps in the service system and priority populations.
Quantitative data from surveys were analysed using statistical software. Descriptive statistics were used to describe the sample in terms of socioeconomic background and present the prevalence of chronic diseases, risk factors, and health behaviours. Statistical analytical tests were also used to compare results between different groups of community members. Results also were compared by those at the state/ national level or from a similar community. Those diseases or risk factors that had a high prevalence among community members are regarded as priorities that to be addressed further.
Formulation of recommendations across various levels (individual, institution, community, policy levels)
Following analysis of the quantitative and qualitative data, the studies included in the review provided a thorough list of health needs and assets of the community. Included studies mainly used CHNAA outputs: 1) as a resource to provide baseline data of community’s health; 2) as a resource to prioritize and plan services; 3) as a resource for writing grant applications; 4) as a resource to guide a comprehensive health promotion strategy.
Not all included CHNAAs proposed interventions to address identified needs and issues. Some of the included studies ( n = 45, 39%) just provided a snapshot of the most important issues faced by the studied community. They demonstrated several areas where CHNAAs provide more information to researchers, community organizations, and policy-makers. On the other hand, not all identified issues and needs were addressed by those studies performed CHNAA in order to implement interventions or strategies. In practice, specific populations or a number of specific health conditions or health risks, or overarching issues such as health inequality and disparities were prioritized by these studies.
In most cases, decisions on implementation were carried out by the CHNAA steering committees or the research teams. Only a number of studies used a clear and explicit set of criteria for deciding the importance of each issue [ 22 , 27 , 43 , 67 , 94 , 118 , 122 ]. A wide range of criteria were used by included studies such as: impact, urgency, community concern, achievability within the set time [ 94 ], seriousness, urgency, solvability, and financial burden of the problems [ 27 ], perception of survey participants on importance of the identified issues and feasibility of intervention, prevalence, fatality, social and cultural stigma [ 22 ], possible interventions, organizational capacity, and community assets and resources [ 13 ], importance and possibility of the effecting change [ 43 ], prevalence, impact on the duration of sickness, impact on mortality, and the availability of treatment [ 122 ], impact of the problem on the overall wellness, quality of life, and resources of their community [ 118 ], factors of health issue, size, seriousness, and effectiveness of available interventions [ 101 ], importance and feasibility [ 67 ].
Different techniques for ranking priorities were applied by included studies such as: 1) Multi-voting technique (decide on priorities by agreeing or disagreeing in group discussions and continuing process/rounds until a final list is developed), 2) Strategy lists (determine if the health needs are of “high or low importance” by placing emphasis on problems whose solutions have maximum impact, with the possibility of limited resource), 3) Nominal group technique (rate health problems from 1 to 10 through group discussion), and 4) Prioritization matrix (weigh and rank multiple criteria for prioritization with numeric values to determine health needs with high importance).
Overall, health priority types were categorized into four main categories by included studies:
Medical conditions (e.g. obesity, diabetes, heart diseases, asthma, mental health disorders, substance abuse, vision/ dental problems, HIV/AIDS and sexually transmitted diseases, injuries and health consultations).
Health behaviours (e.g. physical activity, eating habits/ nutrition, tobacco consumption, teen pregnancy and violence/gangs).
Community conditions (e.g. poverty and unemployment, environmental and infrastructural conditions, such as air quality/pollution, transportation, access to clean water and sanitation, community collaboration, and access to healthy food, exercise facilities and occupational concerns).
Health systems priorities (e.g. access to care, including primary care and higher levels of care, specialty care, mental/ behavioural health care and dental care, quality and acceptability of health services, lack of cultural competence in health systems, flexible hours and waiting time).
However, guided by a community-based participatory research (CBPR) approach, a number of studies involved community members and stakeholders in priority identification or ranking [ 12 , 21 , 22 , 23 , 27 , 29 , 31 , 36 , 41 , 43 , 49 , 53 , 55 , 56 , 58 , 59 , 60 , 62 , 63 , 68 , 70 , 74 , 86 , 87 , 88 , 90 , 92 , 99 , 100 , 103 , 104 , 110 , 114 , 117 , 118 , 119 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 ], in potential strategy selection [ 13 , 19 , 67 , 82 , 89 , 130 ], and in carrying out strategies [ 8 , 37 , 69 , 81 , 93 , 105 , 113 ]. They asserted that by involving the perspectives of the relevant stakeholders, a comprehensive overview of the issues and possible effective solutions was created.
Planning of programmes and interventions, implementation and evaluation
The results of CHNAA were used in various ways by included studies. In some studies, particularly researcher-led studies with limited support or involvement of the local authorities, CHNAA just led to the identification of new, locally relevant issues and priorities without any further actions ( n = 45, 39%). The results of these CHNAAs provided more information to researchers, community organizations, and local policy-makers. Their results also may guide further research agenda in the community [ 18 , 21 , 23 , 29 , 35 , 39 , 40 , 42 , 44 , 48 , 49 , 50 , 52 , 54 , 55 , 62 , 64 , 65 , 66 , 69 , 70 , 71 , 72 , 73 , 76 , 77 , 78 , 85 , 96 , 106 , 122 , 123 , 131 , 132 , 133 , 134 , 135 ]. Some of these studies tried to present their results to the local authorities through various channels in the hope that it would modify existing programmes or implement new ones to meet the needs of the community residents. In addition to identification of relevant issues and priorities, included studies listed at least one outcome associated with the reported CHNAA activity as follows:
Development or modification of health and social policy and programmes: The knowledge provided by CHNAAs helped develop better tailored, and thereby potentially more effective interventions by a number of studies. Further, the information gathered from the CHNAA process was used as the baseline against which to measure future targets for assessment efforts and progress in areas were targeted ( n = 36).
Formation of new partnership: In some cases, a new partnership among entities involved in CHNAA was formed to address health issues. One of the partnerships reported successful was the community–academic partnership in which communities used the research capacity of academic institutions to conduct the CHNAAs ( n = 20). Another type of the partnership reported by some studies was the collaboration among healthcare organizations serving the same geographic area to conduct CHNAA jointly. Conducting a joint CHNAA may avoid duplication of planning efforts and obviate the creation of multiple community health needs assessments for the same population ( n = 5).
Development of new recommendations: Several suggestions were proposed to be considered while designing health improvement interventions in the future by some of the included studies ( n = 18).
Setting or altering strategic direction: Strategic agency direction was established or altered in some cases, which might indicate that the CHNAA was used to redirect resources better to meet the needs of the community ( n = 4).
Raising awareness about health issues: One of the most important insights brought by CHNAA findings was the recognition of the health priorities and contributing factors by the community members, leaders and researchers, leading to an increased awareness of community issues among them ( n = 8).
Engaging and motivating policy-makers and stakeholders: A few studies reported that CHNAAs provided health organizations with the opportunity to identify and interact with key policy-makers, community leaders, and key stakeholders about health priorities and concerns, which might foster a sense of collective ownership and trust in the results and increase the likelihood that the CHNAA will be used ( n = 5).
Having an impact on obtaining resources and resource allocation: The CHNAAs provided the community partners with locally relevant information regarding the current status of health and perceived community needs to inform resource allocation and applications for new grants for the initiation of new programmes ( n = 14)
Contribution to the development of CHNAA process: Some studies reported that the specific methods used in their CHNAA processes could contribute to more relevant and effective community health need assessment process ( n = 10).
Dissemination of findings
Disseminating of the findings and knowledge gained to all partners involved was a foremost step of CHNAAs. The most cited product of the CHNAA process in the included studies was the community needs assessment report. This report includes information about the health of the community as well as the community’s capacity to improve the lives of residents. The report provides the basis for discussion and future actions. In addition to the final report, other channels to disseminate CHNAAs findings were reported as: publishing CHNAA main results in local newspapers, communicating research results with community members and stakeholders in public forums or meetings, presentation results to the steering committee and various stakeholders, posting the report on the local authorities websites, individual meetings with community leaders and stakeholders, posters, and presentation of findings in academic conferences.
Community participation
Among included studies, around 50 studies (44%) reported using participatory approaches and techniques to encourage community members' participation in CHNAA process. Unlike traditional approaches to health needs assessment, participatory approaches aimed to incorporate community inputs at all stages of the research process to enhance capacity building and overcome barriers to research raised by matters of trust, communication, cultural differences, power and representation. A variety of participatory approaches (e.g. community based participatory research (CBPR), participatory rural appraisal, participatory action research (PAR), rapid participatory appraisal (RPA), tribal participatory research, community-based collaborative action research (CBCAR), precede-proceed model, concept mapping and photovoice) were used by these studies to ensure that communities participate in CHNAA, from defining the community to identifying needs and assets and developing new interventions.
Pennel and colleagues classified the depth of the community participation in CHNAA activities into four main categories [ 136 ]. In this classification, depth of the community participation was assessed by the types of activities in which participants were involved throughout the assessment and planning process as follows:
No participation: No attempt to engage community stakeholders or members;
Consultation-only: Engagement of health-related stakeholders, broader community stakeholders, and/or community members to identify health needs through surveys, interviews, and/or focus groups; verified or validated health needs/priorities with local experts;
Moderate participation: Involvement of community stakeholders/ or community members in priority identification; involvement of community stakeholders in strategy selection;
Extensive participation: Involvement of community stakeholders/or community members to develop and carry out strategies.
The above classification was used to assess the depth of the community participation by included studies. Based on the content analysis, community participation in CHNAA process varied considerably across the included empirical studies, from minimal to in-depth participation (Table 1 ). Around 65% of the included studies were involved in consultation-only to identify health needs through one-way communication using tools such as surveys, interviews, and focus group to identify community needs and resources. Around 22% of the included studies solicited moderate participation from the community by involving community in verifying needs and final priority selection and only about 10% of the included studies reported a broad and deep community participation including community involvement in designing and implementing strategies to improve community health.
Three categories of challenges were cited by the reviewed studies while performing CHNAA projects.
Methodological challenges: These are mainly associated with quantitative and qualitative data collection methods, which were discussed earlier. Other methodological challenges cited were: difficulties in aggregating and making sense of data collected from various sources (triangulation), non-generalisability of site-specific data and limitations of the use of existing epidemiological data alone, which does not provide a comprehensive view of health needs, yet is often the most available source of information. Traditional approaches to data collection were challenging where language and literacy barriers existed [ 12 , 52 , 65 , 71 ]. Another major challenge reported by studies used community-based participatory research approaches was the challenge of involving the community in decisions related to research design and data collection methods while maintaining an appropriate level of methodological validity and reliability [ 56 , 81 , 121 ]. In addition, participation was not without challenges. Including the perspectives of stakeholders and residents can lead to differing accounts of what services are seen as essential, and each party may push their own agenda based on their personal or professional interests. Further, linguistic and cultural barriers may be a major factor among minority groups hindering participation in such endeavors [ 81 , 137 ].
Logistical challenges: The major logistical challenges reported were the need for a considerable amount of time (often inadequate), and resources required to conduct a comprehensive assessment [ 80 , 138 ]. Good quality local data on the needs and utilization of health services are usually difficult to obtain [ 9 ]. Financial costs are considerable and the depth of information obtained will ultimately depend upon the methods employed [ 139 , 140 ]. In addition, health professionals, managers and others involved in health services planning and delivery may not have the requisite skills to conduct CHNAAs. This goes beyond technical skills and places an emphasis on soft skills and flexibility including good listening skills, the ability to establish trusting relationships, empathy, working with diverse groups and reflexivity [ 140 , 141 ]. Moreover, limited health information infrastructure and systems in developing countries settings may have hindered the availability of good quality information to conduct CHNAAs [ 13 , 28 , 30 , 142 ].
Ethical challenges: Concerns were raised about the ethical issues associated with community consultation about felt needs followed by priority setting process that leaves many needs unaddressed and the bulk of expectations dashed. Labelling, stigma and stereo- typing are other problems raised by needs assessment [ 143 ]. Needs assessment results may not be utilised, leaving unmet expectations and may require extensive financial and political support to lead to changes in health service planning and delivery [ 9 ]. Comprehensive health needs assessment is likely to produce different, potentially conflicting needs, exposing hidden conflicts and tensions in communities without any mechanisms to address these issues [ 5 ]. Further, local participation may only allow those who are able to voice their needs to do so, leaving behind the silent or hidden voices [ 81 ]. Involvement of the community in the needs assessment process also impacts upon possible outcomes of the project especially since it is likely that expectations of changes to programmes and service delivery may have arisen from local participation [ 144 ].
Facilitators and enablers
CHNAA projects need to be organized in such a way that they have clear objectives, and are adequately resourced by experienced staff. In addition, factors such as clear objectives, decisive leadership, teamwork, communication, sound study design, adequate resourcing, skilled staff, sufficient time and ownership by stakeholders are among those factors that contribute to the successful implementation of CHNAAs [ 15 , 145 ]. Most studies cited community participation as a major facilitator of the CHNAA process and outcomes. Participation was shown to foster bidirectional learning and communications, where both health authorities and the community learnt about needs and priorities. Different benefits for community engagement were mentioned by reviewed literature including, improved participants’ recruitment, enhanced capacity among stakeholders, productive conflict resolution, increased quality of outputs and outcomes, increased sustainability of project goals beyond funding and timelines and development of linguistically and culturally appropriate measures. In addition, incorporating community voices has the potential to inform the development of sound measures to tackle health disparities in the basis of race, social class and ethnicity [ 12 , 27 , 30 , 91 , 103 , 110 , 126 , 146 ].
The main objective of our scoping review was to provide an overview of why and how community health needs and assets assessments (CHNAAs) have been used globally. Substantial variation was found among the studies reviewed concerning definitions, process, participants, methods, goals, and products, yet there were many common characteristics.
Some CHNAAs focused narrowly on health care in assessing needs, with scant attention to other community issues that can affect health. However, most of the included studies looked beyond health needs and considered social and environmental conditions influencing community health. We argue all CHNAAs should approach community health needs assessment holistically, focusing on both individual physical and mental wellbeing as well as casting a social determinants of health lens on the population health.
The review showed that community health needs assessment is used widely by different users and across different settings in both HICs and LMICs. However, in countries such as the US it has become institutionalized and has accordingly been developed, as service providers, particularly hospitals, are mandated to perform CHNAA to compliance with legislative mandates. However, though federal and state laws impose requirements on hospitals to conduct CHNAAs, the methods for needs assessments are generally left to the discretion of each hospital [ 147 ]. As a result, assessment methods vary widely. US-based CHNAAs either develop their own CHNAA processes or utilize a process developed at the state or national level to guide their efforts. A number of toolkits have been provided by different organizations across US to help healthcare providers to conduct CHNAA projects [ 6 , 148 , 149 ]. This highlights the need for consensus guidance across many countries and settings while maintaining the responsiveness to contextual needs, assets and priorities.
Both qualitative and quantitative approaches were employed to collect data on community health needs and assets. Overall, there has been a growing use of mixed-methods approaches to conduct CHNAA in recent years, owing to the recognition in the literature that using qualitative and quantitative approaches simultaneously can provide complementary insights determining community health needs and assets [ 69 , 91 , 104 ]. Although quantitative approaches yield concrete evidence of community needs and assets, qualitative approaches provide a context for how these issues can be addressed using available resources [ 91 , 102 ]. Using qualitative methods in conjunction with more traditional quantitative approaches is especially appropriate for studying complex public health issues and promotes the alignment of implementation plans with the local needs of community members [ 59 , 69 , 91 ]. The growing use of mixed-methods approaches has practical implications for research training and capacity building within entities performing CHNAAs. Organizations who wish to conduct CHNAAs will need to ensure that the competencies and expertise required for mixed-methods studies are available.
Although only a small number of studies provided definitions of assets, there is a growing interest in the literature in asset-based assessment, which examines and mobilizes community assets, instead of focusing on only the needs of communities [ 11 , 84 ]. Unlike need-based or deficit approaches, asset-based approaches document resources and focus on strengths to enhance and preserve rather than deficits to be remedied. Related to principles of empowerment, it postulates that solutions to community problems already exist within a community’s assets. By recognizing existing capacity, communities can become empowered to take ownership of their health and improve as a population [ 11 , 31 , 125 ]. An asset-based approach was recognized as essential for enhancing trust and community coalitions [ 83 ]. Further, it is more participatory in nature through involving community stakeholders throughout the needs assessment process [ 82 , 83 ]. In particular, it highlights community resilience, resources, and opportunities for positive growth rather than focusing solely on health problems or other concerns [ 14 , 84 , 88 ]. In developing countries, assets identified from within the community are crucial for later use in the implementation of health programmes. The shift from a traditional needs-based perspective to an asset-based perspective to health needs assessment can help to address resource constraints in these countries [ 13 , 30 , 150 ].
There was a growing interest in the use of participatory approaches and in their value in identifying and addressing community health needs over recent years among included studies. About half of the reviewed studies applied CBPR or other community-engaged approaches to perform CHNAA. There are several opportunities to fully engage patients, families, and communities in healthcare delivery redesign to ensure that they are provided in a way that address the community members’ needs and preferences. The CHNAA process is one mechanism for this engagement—and a good precursor to deeper engagement and collaboration [ 91 , 97 , 123 ]. Integrating community voices into CHNAA process may be crucially important for confronting health disparities at the community level, which stemming from socio-historical processes, including racial and ethnic discrimination and economic inequality [ 33 , 74 , 86 , 91 ]. To eliminate health disparities, it is critical first to understand social, cultural, and economic determinants of health. CHNAAs, particularly when they include the voices of community residents, can provide an opportunity to understand local processes contributing to health disparities. This knowledge can then be used to inform health and equity initiatives [ 91 , 110 , 126 ]. The development process and implementation of a CHNAA project is an important example of evidence-based public health practice. It is a way to address health and health care disparities experienced by medically underserved populations [ 86 , 92 , 126 ]. Those studies used a participatory approach reported that by having community participation, concerns and issues of the most marginalized and vulnerable populations were voiced. The inclusion of these voices allowed for a broader and deeper understanding of the concerns of those who are typically marginalized and that may be missed in traditional health needs assessment methodologies [ 33 , 56 , 58 , 74 , 86 , 110 , 137 , 146 ]. Hence, defining communities while performing CHNAA needs to be dynamic and socially constructed to take into account all voices and members especially those not ordinarily included. This deeper understanding is critical to move public health practice and research upstream to address structural and social determinants of health necessary for population-level reductions in health inequities [ 80 , 91 ].
Although there is widespread theoretical recognition of the importance of in-depth community participation in CHNAA, this has not been fully embraced in practice based on our review. Included studies reported community involvement in various stages of CHNAA with varying depth reflecting a continuum from no participation to extensive participation, in which most studies were located at the middle of the participation continuum. The literature review suggests while certain community stakeholders were engaged in the CHNAA process, most studies did not involve a broad range of stakeholders through adopting a full participation approach. One reason for this could be that for most studies conducted in the US, CHNAA was performed to comply with ACA requirements, which requires hospitals to incorporate inputs of the population served as part of the CHNAA process. Since community inputs as well as the process as a whole is not well-defined by these regulations [ 20 ], it seems that the majority of included US-based studies tried to meet legislative requirements by incorporating a minimum level of community and stakeholders’ participation in CHNAA process. In addition, the concept of community engagement in health services planning and implementation has evolved over recent years, from one-way consultative processes to bi-directional collaboration and shared leadership. Although undertaking an in-depth participatory approach through extensive participation of community stakeholders in CHNAAs may pose certain challenges for healthcare providers including requiring additional time and other resources to collaborate with community residents, we argue the benefits to this approach are important to improve health, as reported by some included studies [ 80 , 118 , 151 ].
A notable gap in the existing literature is the lack of long-term or longitudinal–assessment of CHNAA. The review showed that additional research into CHNAA implementation and outcomes is needed. Currently, there are limited data describing the impact of CHNAAs on health outcomes. However, there is ample evidence on different short-term impacts associated with CHNAA implementation, including, the development of health and social interventions, forming the new partnership, raising awareness on health issues, engaging policy-makers, and facilitating obtaining resources. In other words, it is unclear how CHNAA projects are linked directly to health outcomes. Furthermore, the mechanisms between the conduct and use of CHNAA remain largely unknown in the literature [ 152 , 153 ]. Clearly, not all CHNAA projects result in changes to policies or programmes, and conversely, many programme and policy decisions are made in the absence of CHNAA data [ 154 , 155 ]. Still, further research to understand these mechanisms and the long term impact of CHNAA is needed to support evidence of its use and value in addressing individual and population health needs.
This scoping review aimed to provide clarity and supplement the evidence on the key concepts, rationale, methods, tools and outcomes of community health needs and assets assessments (CHNAAs). Importantly, it highlights the need for holistic approaches to needs assessments to focus on physical, mental and social wellbeing, along with considering wider systems factors and structural challenges to individual and population health. Furthermore, the findings emphasize the inclusion of community assets in community health assessments, beginning foremost with community capabilities and knowledge. It is encouraging to see the use of pragmatic approaches including both qualitative and quantitative methods in CHNAA process in the literature. This will help to ensure that a robust and in-depth exploration of needs and assets is available to guide decision making. Although we recognize the challenges with providing consensus on definitions, processes and tools for CHNAA, we argue that more clarity is needed on the key considerations, steps and outcomes for this process across various settings. This study attempts to provide some theoretical insights and empirical information concerning the process, which hopefully will provide useful guidance to community organizations, policy- makers, health service providers and researchers seeking to develop and implement community health needs and assets assessment.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Institute of Medicne. The future of the public’s health in the 21st century: National Academy Press; 2003.
Google Scholar
Fuller J, Bentley M, Shotton D. Use of community health needs assessment for regional planning in country South Australia. Aust J Rural Health. 2001;9(1):12–7. https://doi.org/10.1046/j.1440-1584.2001.00353.x .
Article CAS Google Scholar
Wright J, Williams R, Wilkinson JR. Development and importance of health needs assessment. BMJ. 1998;316(7140):1310–3. https://doi.org/10.1136/bmj.316.7140.1310 .
Wright J, Walley J. Assessing health needs in developing countries. BMJ. 1998;316(7147):1819–23. https://doi.org/10.1136/bmj.316.7147.1819 .
Jordan J, Dowswell T, Harrison S, Lilford RJ, Mort M. Health needs assessment: Whose priorities? Listening to users and the public. BMJ. 1998;316(7145):1668–70. https://doi.org/10.1136/bmj.316.7145.1668 .
Myers S, Stoto MA: Criteria for assessing the usefulness of community health assessments; a literature review. 2006. https://www.rand.org/pubs/technical_reports/TR314.html . Accessed 18 Nov 2020.
Centers for Disease Control and Prevention (CDC). Community needs assessment. Atlanta: GA.
Finifter DH, Jensen CJ, Wilson CE, Koenig BL. A comprehensive, multitiered, targeted community needs assessment model: methodology, dissemination, and implementation. Fam Community Health. 2005:293–306. https://doi.org/10.1097/00003727-200510000-00003 .
Stevens A, Gillam S. Needs assessment: from theory to practice. BMJ. 1998;316(7142):1448–52. https://doi.org/10.1136/bmj.316.7142.1448 .
Friedman DJ, Parrish RG. Is community health assessment worthwhile? J Public Health Manag Pract. 2009;15(1):3–9. https://doi.org/10.1097/01.PHH.0000342943.41080.ef .
Article Google Scholar
Altschuld JW, Hung HL, Lee YF. Needs assessment and asset/capacity building: A promising development in practice. New Dir Eval. 2014;2014(144):89–103. https://doi.org/10.1002/ev.20105 .
Jackson KM, Pukys S, Castro A, Hermosura L, Mendez J, Vohra-Gupta S, et al. Using the transformative paradigm to conduct a mixed methods needs assessment of a marginalized community: Methodological lessons and implications. Eval Program Plann. 2018;66:111–9. https://doi.org/10.1016/j.evalprogplan.2017.09.010 .
Mathias KR, Mathias JM, Hill PC. An asset-focused health needs assessment in a rural community in North India. Asia Pac J Public Health. 2015;27(2):NP2623–34. https://doi.org/10.1177/1010539511421193 .
Kirk CM, Johnson-Hakim S, Anglin A, Connelly C. Putting the community back into community health needs assessments: Maximizing partnerships via community-based participatory research. Prog Community Health Partnersh. 2017;11(2):167–73. https://doi.org/10.1353/cpr.2017.0021 .
Coster G, Mays N, Scott C, Cumming J. The impact of health needs assessment and prioritisation on District Health Board planning in New Zealand. Int J Health Plann Manag. 2009;24(4):276–89. https://doi.org/10.1002/hpm.1011 .
Parry-Jones B, Soulsby J. Needs-led assessment: the challenges and the reality. Health Soc Care Community. 2001;9(6):414–28. https://doi.org/10.1046/j.0966-0410.2001.00316.x .
Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. JBI Evidence Implementation. 2015;13(3):141–6. https://doi.org/10.1097/XEB.0000000000000050 .
Anselma M, Chinapaw MJM, Altenburg TM. Determinants of child health behaviors in a disadvantaged area from a community perspective: A participatory needs assessment. Int J Environ Res Public Health. 2018;15(4):644. https://doi.org/10.3390/ijerph15040644 .
Berkley-Patton J, Thompson CB, Bradley-Ewing A, Marcie B, Booker A, Catley D, et al. Identifying health conditions, priorities, and relevant multilevel health promotion intervention strategies in African American churches: A faith community health needs assessment. Eval Program Plann. 2018;67:19. https://doi.org/10.1016/j.evalprogplan.2017.10.012 .
Bias TK, Abildso CG, Vasile E, Coffman J. The impact of community input in community health needs assessments. J Public Health Manag Pract. 2017;23:S29–33. https://doi.org/10.1097/PHH.0000000000000586 .
Cho S, Lee H, Yoon S, Kim Y, Levin P, Kim E. Community health needs assessment: a nurses’ global health project in Vietnam. Int Nurs Rev. 2018;65(4):505–14. https://doi.org/10.1111/inr.12443 .
Kapiriri L, Frithjof NorheimMD PDO. Whose priorities count? Comparison of community-identified health problems and Burden-of-Disease-assessed health priorities in a district in Uganda. Health Expect. 2002;5(1):55–62. https://doi.org/10.1046/j.1369-6513.2002.00161.x .
Li Y, Cao J, Lin H, Li D, Wang Y, He J. Community health needs assessment with precede-proceed model: a mixed methods study. BMC Health Serv Res. 2009;9(1):1–14. https://doi.org/10.1186/1472-6963-9-181 .
World Health Organization. Social Determinants of Health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1 . Acessed 10 Oct 2022.
Smithies J, Adams L, Webster G, Beattie A. Community participation in health promotion: Health Education Authority London; 1990.
Jack K, Holt M. Community profiling as part of a health needs assessment. Nurs Stand. 2008;22(18):51–8. https://doi.org/10.7748/ns2008.01.22.18.51.c6311 .
Ahari SS, Habibzadeh S, Yousefi M, Amani F, Abdi R. Community based needs assessment in an urban area; A participatory action research project. BMC Public Health. 2012;12(1):1–8. https://doi.org/10.1186/1471-2458-12-161 .
Shin H, Lee SJ, Lee Y-n, Shon S. Community health needs assessment for a child health promotion program in Kyrgyzstan. Eval Program Plann. 2019;74:1–9. https://doi.org/10.1016/j.evalprogplan.2019.02.005 .
Birdwell SW, Calesaric H. Identifying Health Care Needs of Rural Ohio Citizens: An Evaluation of a Two-stage Methodology. J Rural Health. 1996;12(2):130–6. https://doi.org/10.1111/j.1748-0361.1996.tb00784.x .
Pepall E, Earnest J, James R. Understanding community perceptions of health and social needs in a rural Balinese village: results of a rapid participatory appraisal. Health Promot Int. 2007;22(1):44–52. https://doi.org/10.1093/heapro/dal042 .
Moore de Peralta A, Davis L, Brown K, Fuentes M, Falconer NS, Charles J, et al. Using Community-Engaged Research to Explore Social Determinants of Health in a Low-Resource Community in the Dominican Republic: A Community Health Assessment. Hisp Health Care Int. 2020;18(3):127–37. https://doi.org/10.1177/1540415319874812 .
Ake T, Diehr S, Ruffalo L, Farias E, Fitzgerald A, Good SD, et al. Needs assessment for creating a patient-centered, community-engaged health program for homeless pregnant women. J Patient Cent Res Rev. 2018;5(1):36. https://doi.org/10.17294/2330-0698.1591 .
Kiser T, Hulton L. Addressing health care needs in the homeless population: a new approach using participatory action research. SAGE Open. 2018;8(3):2158244018789750. https://doi.org/10.1177/2158244018789750 .
Schaffer MA, Mather S, Gustafson V. Service learning: A strategy for conducting a health needs assessment of the homeless. Health Care Poor Underserved. 2000;11(4):385–99. https://doi.org/10.1353/hpu.2010.0746 .
Kehn M, Ho P, Kroll T. Identifying the health service needs of homeless adults with physical disabilities. Public Health. 2013;127(8):785–7. https://doi.org/10.1016/j.puhe.2013.01.011 .
Sangalang CC, Ngouy S, Lau AS. Using community-based participatory research to identify health issues for Cambodian American youth. Fam Community Health. 2015;38(1):55. https://doi.org/10.1097/FCH.0000000000000056 .
Jeffery V, Ervin K. Responding to rural health needs through community participation: addressing the concerns of children and young adults. Aust Prim Health. 2011;17(2):125–30. https://doi.org/10.1071/PY10050 .
Harrison L, Scarinci I. Child health needs of rural Alabama Latino families. J Community Health Nurs. 2007;24(1):31–47. https://doi.org/10.1080/07370010709336584 .
Averill J. Keys to the puzzle: Recognizing strengths in a rural community. Public Health Nurs. 2003;20(6):449–55. https://doi.org/10.1046/j.1525-1446.2003.20605.x .
Din NC, Ghazali SE, Ibrahim N, Ahmad M, Said Z, Ghazali AR, et al. Health needs assessment of older people in an agricultural plantation. Int J Gerontol. 2014;8(3):120–6. https://doi.org/10.1016/j.ijge.2013.12.003 .
Nolin J, Wilburn ST, Wilburn KT, Weaver D. Health and social service needs of older adults: Implementing a community-based needs assessment. Eval Program Plann. 2006;29(3):217–26. https://doi.org/10.1016/j.evalprogplan.2006.06.003 .
Lee LL, Lin SH, Philp I. Health needs of older Aboriginal people in Taiwan: a community-based assessment using a multidimensional instrument. J Clin Nurs. 2015;24(17–18):2514–21. https://doi.org/10.1111/jocn.12842 .
Núñez AE, Robertson-James C, Reels S, Weingartner RM, Bungy BL. Conducting a needs assessment for women and girls using a gender analysis framework: The Philadelphia Ujima coalition for a healthier community experience. Womens Health Issues. 2012;22(6):e527–34. https://doi.org/10.1016/j.whi.2012.08.002 .
Urrutia RP, Merisier D, Small M, Urrutia E, Tinfo N, Walmer DK. Unmet health needs identified by Haitian women as priorities for attention: a qualitative study. Reprod Health Matters. 2012;20(39):93–103. https://doi.org/10.1016/s0968-8080(12)39602-x .
Zimmermann K, Khare MM, Wright C, Hasler A, Kerch S, Moehring P, et al. Application of a gender-based approach to conducting a community health assessment for rural women in Southern Illinois. Eval Program Plann. 2015;51:27–34. https://doi.org/10.1016/j.evalprogplan.2014.12.004 .
Dell EM, Erikson SL, Andrianirina E, Smith G. Women’s knowledge in Madagascar: A health needs assessment study. Global public health. 2012;7(1):29–41. https://doi.org/10.1080/17441692.2011.557083 .
Chhabra R, Teitelman N, Silver EJ, Raufman J, Bauman LJ. Vulnerability Multiplied: Health Needs Assessment of 13–18-Year-Old Female Orphan and Vulnerable Children in Kenya. World Med Health Policy. 2018;10(2):129–45. https://doi.org/10.1002/wmh3.267 .
Stepleman LM, Yohannan J, Scott SM, Titus LL, Walker J, Lopez EJ, et al. Health needs and experiences of a LGBT population in Georgia and South Carolina. Homosex. 2019;66(7):989–1013. https://doi.org/10.1080/00918369.2018.1490573 .
Wilson BD, Neubauer LC, Park A, Abuor P, Harper GW. The sexual health needs of sexual minority women in Western Kenya: An exploratory community assessment and public policy analysis. Glob Public Health. 2019;14(10):1495–508. https://doi.org/10.1080/17441692.2019.1611895 .
Zajac C, Godshall KC. Empowerment through accessibility: Community needs assessment data for LGBTQ communities. Soc Work Public Health. 2020;35(6):483–93. https://doi.org/10.1080/19371918.2020.1798322 .
Coleman JD, Irwin JA, Wilson RC, Miller HC. The South Carolina LGBT needs assessment: A descriptive overview. Homosex. 2014;61(8):1152–71. https://doi.org/10.1080/00918369.2014.872515 .
Bhimla A, Yap L, Lee M, Seals B, Aczon H, Ma GX. Addressing the health needs of high-risk Filipino Americans in the greater Philadelphia region. J Community Health. 2017;42(2):269–77. https://doi.org/10.1007/s10900-016-0252-0 .
Bopp M, Fallon EA, Bolton DJ, Kaczynski AT, Lukwago S, Brooks A. Conducting a Hispanic Health Needs Assessment in rural Kansas: Building the foundation for community action. Eval Program Plann. 2012;35(4):453–60. https://doi.org/10.1016/j.evalprogplan.2012.02.002 .
Burns JC, Teadt S, Bradley WW Sr, Shade GH Jr. Enhancing Adolescent and Young Adult Health Services! A Review of the Community Needs Assessment Process in an Urban Federally Qualified Health Center. Health Equity. 2020;4(1):218–24. https://doi.org/10.1089/heq.2019.0108 .
Corona R, Gonzalez T, Cohen R, Edwards C, Edmonds T. Richmond Latino needs assessment: A community-university partnership to identify health concerns and service needs for Latino youth. J Community Health. 2009;34(3):195–201. https://doi.org/10.1007/s10900-008-9140-6 .
Doyle E, Rager R, Bates D, Cooper C. Using community-based participatory research to assess health needs among migrant and seasonal farmworkers. Am J Health Educ. 2006;37(5):279–88. https://doi.org/10.1080/19325037.2006.10598916 .
Ghimire S, Cheong P, Sagadraca L, Chien L-C, Sy FS. A health needs assessment of the Filipino American community in the greater Las Vegas area. Health Equity. 2018;2(1):334–48. https://doi.org/10.1089/heq.2018.0042 .
Hebert-Beirne J, Felner JK, Castañeda Y, Cohen S. Enhancing themes and strengths assessment: leveraging academic-led qualitative inquiry in community health assessment to uncover roots of community health inequities. J Public Health Manag Pract. 2017;23(4):370–9. https://doi.org/10.1097/phh.0000000000000478 .
Hebert-Beirne J, Hernandez SG, Felner J, Schwiesow J, Mayer A, Rak K, et al. Using community-driven, participatory qualitative inquiry to discern nuanced community health needs and assets of Chicago’s La Villita, a Mexican immigrant neighborhood. J Community Health. 2018;43(4):775–86. https://doi.org/10.1007/s10900-018-0484-2 .
Hernandez SG, Genkova A, Castañeda Y, Alexander S, Hebert-Beirne J. Oral histories as critical qualitative inquiry in community health assessment. Health Educ Behav. 2017;44(5):705–15. https://doi.org/10.1177/1090198117728546 .
Lee S, Ma GX, Juon H-S, Martinez G, Hsu CE, Bawa J. Assessing the needs and guiding the future: findings from the health needs assessment in 13 Asian American communities of Maryland in the United States. J Immigr Minor Health. 2011;13(2):395–401. https://doi.org/10.1007/s10903-009-9310-3 .
Martinez IL, Carter-Pokras O. Assessing health concerns and barriers in a heterogeneous Latino community. J Health Care Poor Underserved. 2006;17(4):899–909. https://doi.org/10.1353/hpu.2006.0129 .
Mannix TR, Austin SD, Baayd JL, Simonsen SE. A community needs assessment of urban Utah American Indians and Alaska natives. J Community Health. 2018;43(6):1217–27. https://doi.org/10.1007/s10900-018-0542-9 .
Montano JJ, Acosta-Deprez V, Sinay T. Assessing the health care needs of Filipino Americans in greater Long Beach. Public Admin Manag. 2009;14(1):156.
Patel VV, Rajpathak S, Karasz A. Bangladeshi immigrants in New York City: a community based health needs assessment of a hard to reach population. J Immigr Minor Health. 2012;14(5):767–73. https://doi.org/10.1007/s10903-011-9555-5 .
Su D, Garg A, Wiens J, Meyer E, Cai G. Assessing health needs in African American churches: a mixed-methods study. J Relig Health. 2021;60(2):1179–97. https://doi.org/10.1007/s10943-019-00924-5 .
Suiter SV. Community health needs assessment and action planning in seven Dominican bateyes. Eval Program Plann. 2017;60:103–11. https://doi.org/10.1016/j.evalprogplan.2016.10.011 .
Thomas LR, Donovan DM, Sigo RL. Identifying community needs and resources in a Native community: A research partnership in the Pacific Northwest. Int J Ment Health Addict. 2010;8(2):362–73. https://doi.org/10.1007/s11469-009-9233-1 .
Weathers B, Barg FK, Bowman M, Briggs V, Delmoor E, Kumanyika S, et al. Using a mixed-methods approach to identify health concerns in an African American community. Am J Public Health. 2011;101(11):2087–92. https://doi.org/10.2105/AJPH.2010.191775 .
Dong X, Chang E, Wong E, Wong B, Skarupski KA, Simon MA. Assessing the health needs of Chinese older adults: Findings from a community-based participatory research study in Chicago's Chinatown. J Aging Res. 2010. https://doi.org/10.4061/2010/124246 .
Sarsour L, Tong VS, Jaber O, Talbi M, Julliard K. Health assessment of the Arab American community in southwest Brooklyn. J Community Health. 2010;35(6):653–9. https://doi.org/10.1007/s10900-010-9260-7 .
Thein K, Zaw KT, Teng R-E, Liang C, Julliard K. Health Needs in Brooklyn's Chinatown: A Pilot Assessment Using Rapid Participatory Appraisal. J Health Care Poor Underserved. 2009;20(2):378–94. https://doi.org/10.1353/hpu.0.0140 .
Careyva BA, Hamadani R, Friel T, Coyne CA. A social needs assessment tool for an urban Latino population. J Community Health. 2018;43(1):137–45. https://doi.org/10.1007/s10900-017-0396-6 .
Johnson CV, Bartgis J, Worley JA, Hellman CM, Burkhart R. Urban Indian voices: a community-based participatory research health and needs assessment. Am Indian Alsk Native Mentl Health Res. 2010;17(1):49–70. https://doi.org/10.5820/aian.1701.2010.49 .
Puertas B, Schlesser M. Assessing community health among indigenous populations in Ecuador with a participatory approach: implications for health reform. J Community Health. 2001;26(2):133–47. https://doi.org/10.1023/a:1005281314274 .
Miller K, Yost B, Abbott C, Thompson Buckland S, Dlugi E, Adams Z, et al. Health needs assessment of five Pennsylvania Plain populations. Int J Environ Res Public Health. 2019;16(13):2378. https://doi.org/10.3390/ijerph16132378 .
Tendulkar SA, Hamilton RC, Chu C, Arsenault L, Duffy K, Huynh V, et al. Investigating the myth of the “model minority”: a participatory community health assessment of Chinese and Vietnamese adults. J Immigr Minor Health. 2012;14(5):850–7. https://doi.org/10.1007/s10903-011-9517-y .
Peak T, Gast J, Ahlstrom D. A needs assessment of Latino men’s health concerns. Am J Mens Health. 2010;4(1):22–32. https://doi.org/10.1177/1557988308327051 .
Brock KE, Allen KE, Barton C, Shapiro R, Weintraub B, Wasilewski-Masker K, et al. A Methodologic Approach to Conducting a Statewide Community Needs Assessment of Pediatric Palliative Care and Hospice Resources. J Pain Symptom Manag. 2020;60(3):531–8. e538. https://doi.org/10.1016/j.jpainsymman.2020.04.004 .
Franz BA, Skinner D, Murphy JW. Defining “Community” in community health evaluation: perspectives from a sample of nonprofit Appalachian hospitals. Am J Eval. 2018;39(2):237–56. https://doi.org/10.1177/1098214017722857 .
Clark MJ, Cary S, Diemert G, Ceballos R, Sifuentes M, Atteberry I, et al. Involving communities in community assessment. Public Health Nurs. 2003;20(6):456–63. https://doi.org/10.1046/j.1525-1446.2003.20606.x .
Van Gelderen SA, Krumwiede KA, Krumwiede NK, Fenske C. Trialing the community-based collaborative action research framework: supporting rural health through a community health needs assessment. Health Promot Pract. 2018;19(5):673–83. https://doi.org/10.1177/1524839917754043 .
Goldman KD, Schmalz KJ. “Accentuate the positive!” using an asset-mapping tool as part of a community-health needs assessment. Health Promot Pract. 2005;6(2):125–8. https://doi.org/10.1177/1524839904273344 .
Sharpe PA, Greaney ML, Lee PR, Royce SW. Assets-oriented community assessment. Public Health Rep. 2000;115(2–3):205. https://doi.org/10.1093/phr/115.2.205 .
Mathias K, Rawat M, Thompson A, Gaitonde R, Jain S. Exploring community mental health systems–A participatory health needs and assets assessment in the Yamuna valley, North India. Int J Health Policy Manag. 2020. https://doi.org/10.34172/ijhpm.2020.222 .
deValpine MG, Trull LH. Health Equity in Community Assessments: A Participatory Approach in Rural Virginia. SAGE Open. 2019;9(1):2158244019838925. https://doi.org/10.1177/2158244019838925 .
Lewis H, Rudolph M, White L. Rapid appraisal of the health promotion needs of the Hillbrow Community, South Africa. Int J Healthc Technol Manag. 2003;5(1–2):20–33. https://doi.org/10.1504/IJHTM.2003.003338 .
Talmage C, Mercado M, Yoder G, Hamm K, Wolfersteig W. Critiquing Indicators of Community Strengths in Community Health Needs Assessments. Int J Community Well-Being. 2021:1–22. https://doi.org/10.1007/s42413-020-00106-2 .
Idali Torres M. Assessing health in an urban neighborhood: community process, data results and implications for practice. J Community Health. 1998;23(3):211–26. https://doi.org/10.1023/a:1018720515644 .
Garrettson M, Walline V, Heisler J, Townsend J. New medical school engages rural communities to conduct regional health assessment. Fam Med. 2010;42(10):693.
Cain CL, Orionzi D, O’Brien M, Trahan L. The power of community voices for enhancing community health needs assessments. Health Promot Pract. 2017;18(3):437–43. https://doi.org/10.1177/1524839916634404 .
Grant CG, Ramos R, Davis JL, Green BL. Community health needs assessment: a pathway to the future and a vision for leaders. Health Care Manag (Frederick). 2015;34(2):147–56. https://doi.org/10.1097/hcm.0000000000000057 .
Robinson A, Cherry TS, Elliott M, Davis M, Bagwell G. Leveraging university-community partnerships in rural Georgia: A community health needs assessment template for hospitals. J Ga Public Health Assoc. 2016:365–72. https://doi.org/10.21633/JGPHA.5.409 .
Alfano-Sobsey E, Ledford SL, Decosimo K, Horney JA. Community health needs assessment in Wake County, North Carolina: partnership of public health, hospitals, academia, and other stakeholders. N C Med J. 2014;75(6):376–83. https://doi.org/10.18043/ncm.75.6.376 .
Waling A, Fildes D. ‘Don't fix what ain’t broke’: evaluating the effectiveness of a Men's Shed in inner-regional A ustralia. Health Soc Care Community. 2017;25(2):758–68. https://doi.org/10.1111/hsc.12365 .
Witten NA, Orr MP, Maskarinec GG. Medical School Hotline: An Online, Quantitative Community Health Needs Assessment of Hale ‘iwa and Waialua, O ‘ahu, Hawai ‘i. H Hawaii J Health Soc Welf. 2020;79(10):306.
Woodyard CD, Przybyla S, Hallam JS. A community health needs assessment using principles of community-based participatory research in a Mississippi Delta community: a novel methodological approach. Community Dev. 2015;46(2):84–99. https://doi.org/10.1080/15575330.2015.1006240 .
O’Kelly C, Cullen W, O’Kelly S, O’Kelly F, Bury G. A primary care-based health needs assessment in inner city Dublin. Ir J Med Sci. 2010;179(3):399–403. https://doi.org/10.1007/s11845-010-0483-5 .
Knox S, Chapman P, Your health—your say. A case study of community involvement in a community health needs assessment project in a regional city of Australia. Cities. 1995;12(2):111–4. https://doi.org/10.1016/0264-2751(95)00011-a .
Murray SA, Tapson J, Turnbull L, McCallum J, Little A. Listening to local voices: adapting rapid appraisal to assess health and social needs in general practice. BMJ. 1994;308(6930):698–700. https://doi.org/10.1136/bmj.308.6930.698 .
Stanley SA, Stein DS. Health Watch 2000: community health assessment in south central Ohio. J Community Health Nurs. 1998;15(4):225–36. https://doi.org/10.1207/s15327655jchn1504_4 .
Ying L, Daikun L, Jia H, Kai S, HongHong L, Hu Z. Assessment of community health needs of Chongqing residents. a qualitative study. Mil Med Res. 2008;23(5):289–99. https://doi.org/10.1016/S1000-1948(08)60056-8 .
Kwan K, Do-Reynoso V, Zarate-Gonzalez G, Goldman-Mellor S. Development and implementation of a community health survey for public health accreditation: Case study from a rural county in California. Eval Program Plann. 2018;67:47–52. https://doi.org/10.1016/j.evalprogplan.2017.11.004 .
Green S, Parkinson L, Bonevski B, Considine R. Community health needs assessment for health service planning: realising consumer participation in the health service setting. Health Promot J Austr. 2004;15(2):142–9. https://doi.org/10.1071/HE04142 .
Horne M, Costello J. A public health approach to health needs assessment at the interface of primary care and community development: findings from an action research study. Prim Health Care Res Dev. 2003;4(4):340–52. https://doi.org/10.1191/1463423603pc173oa .
Lundeen SP. Health needs of a suburban community: a nursing assessment approach. J Community Health Nurs. 1992;9(4):235–44. https://doi.org/10.1207/s15327655jchn0904_5 .
Jordan J, Wright J. Making sense of health needs assessment. Br Gen Pract. 1997;47(424):695.
CAS Google Scholar
Hensher M, Fulop N. The influence of health needs assessment on health care decision-making in London health authorities. J Health Serv Policy. 1999;4(2):90–5. https://doi.org/10.1177/135581969900400206 .
Asadi-Lari M, Farshad A, Assaei S, Mahdavi MV, Akbari M, Ameri A, et al. Applying a basic development needs approach for sustainable and integrated community development in less-developed areas: report of ongoing Iranian experience. Public Health. 2005;119(6):474–82. https://doi.org/10.1016/j.puhe.2004.08.014 .
Akintobi TH, Lockamy E, Goodin L, Hernandez ND, Slocumb T, Blumenthal D, et al. Processes and outcomes of a community-based participatory research-driven health needs assessment: a tool for moving health disparity reporting to evidence-based action. Prog Community Health Partnersh. 2018;12(1 Suppl):139. https://doi.org/10.1353/cpr.2018.0029 .
Yoo IY, Cho WJ, Chae SM, Kim MJ. Community health service needs assessment in Korea using OMAHA Classification System. Int J Nurs Stud. 2004;41(6):697–702. https://doi.org/10.1016/j.ijnurstu.2004.02.007 .
Louw J, Carolissen R. Community health needs, community participation, and evaluation research. Eval Program Plann. 1995;18(4):365–9.
Plescia M, Koontz S, Laurent S. Community assessment in a vertically integrated health care system. Am J Public Health. 2001;91(5):811. https://doi.org/10.2105/AJPH.91.5.811 .
Sampson G, Gearin KJM, Boe M. A rural local health department–hospital collaborative for a countywide community health assessment. J Public Health Manag Pract. 2015;21(1):23–30. https://doi.org/10.1097/phh.0000000000000088 .
Vyas AN, Chaudhary N, Ramiah K, Landry M. Addressing a Growing Community’s Health Needs: Project SAHNA (South Asian Health Needs Assessment). J Immigr Minor Health. 2013;15(3):577–83. https://doi.org/10.1007/s10903-012-9655-x .
Van Rie A, West N, Schwartz S, Mutunga L, Hanrahan C, Ncayiyana J, et al. The unmet needs and health priorities of the urban poor: Generating the evidence base for urban community health worker programmes in South Afric. S Afr Med J. 2018;108(9). https://doi.org/10.7196/SAMJ.2018.v108i9.13054 .
Dennis MK, Momper SL. An urban American Indian health clinic's response to a community needs assessment. Am Indian Alsk Native Ment Health Res. 2016;23(5). https://doi.org/10.5820/aian.2305.2016.15 .
Schutte DL, Goris ED, Rivard JL, Schutte BC, Committee CCRA. Community Health Needs Assessment in a Rural Setting. Foundation for a Community–Academic Partnership. J High Educ Outreach Engagem. 2016;20(2):85–108.
Velonis AJ, Molnar A, Lee-Foon N, Rahim A, Boushel M, O’Campo P. “One program that could improve health in this neighbourhood is _?” using concept mapping to engage communities as part of a health and human services needs assessment. BMC Health Serv Res. 2018;18(1):1–12. https://doi.org/10.1186/s12913-018-2936-x .
Torres Stone RA, Cardemil EV, Keefe K, Bik P, Dyer Z, Clark KE. A community mental health needs assessment of a racially and ethnically diverse population in New England: Narratives from community stakeholders. Community Ment Health J. 2020;56(5):947–58. https://doi.org/10.1007/s10597-020-00562-2 .
Agrusti T, Bohn J, Dunn E, Bell C, Ziegler A. The story so far: a mixed-methods evaluation of county-level behavioral health needs, policies, and programs. Soc Work Ment Health. 2020;18(3):257–73. https://doi.org/10.1080/15332985.2020.1720889 .
Palmer CA. Rapid appraisal of needs in reproductive health care in southern Sudan: qualitative study. BMJ. 1999;319(7212):743–8. https://doi.org/10.1136/bmj.319.7212.743 .
Lazenbatt A, Lynch U, O'Neill E. Revealing the hidden ‘troubles’ in Northern Ireland: the role of participatory rapid appraisal. Health Educ Res. 2001;16(5):567–78. https://doi.org/10.1093/her/16.5.567 .
Kingery FP, Naanyu V, Allen W, Patel P. Photovoice in Kenya: Using a community-based participatory research method to identify health needs. Qual Health Res. 2016;26(1):92–104. https://doi.org/10.1177/1049732315617738 .
Sabin AV, Levin PF. The Journey to Meet Emerging Community Benefit Requirements in a Rural Hospital: A Case Study. Online J Issues Nurs. 2016;21(1). https://doi.org/10.3912/OJIN.Vol21No01PPT01 .
Lightfoot AF, De Marco MM, Dendas RC, Jackson MR, Meehan EF. Engaging underserved populations in Affordable Care Act-required needs assessments. J Health Care Poor Underserved. 2014;25(1):11–8. https://doi.org/10.1353/hpu.2014.0060 .
Amendola MG, Nazario N, Sanchez V. Using CBPR to assess client needs at a social service agency. Public Health Nurs. 2016;33(2):167–75. https://doi.org/10.1111/phn.12204 .
Harmon BE, Pichon LC, Powell TW, Rugless F, McCann L, Minor LL, et al. Developing a Congregational Health Needs Assessment: Lessons Learned from Using a Participatory Research Approach. Prog Community Health Partnersh. 2021;15(1):47–58. https://doi.org/10.1353/cpr.2021.0004 .
Mulvihill BA, Pass MA, Miller TM, Mulvihill FX, Klerman LV. Collaborative needs assessment and systems development in Alabama: Process and products. Am J Prev Med. 1996;12(4):14–9.
Santilli A, Carroll-Scott A, Ickovics JR. Applying community organizing principles to assess health needs in New Haven, Connecticut. Am J Public Health. 2016;106(5):841–7. https://doi.org/10.2105/ajph.2016.303050 .
Milaat W, Bani I, Aqeely H, Makeen A, Salih A, Alnagaar M. Jazan Health needs assessment: a key informant approach. J Public Health Med. 2007;6:105–10.
Kulig JC, Wilde I. Collaboration between communities and universities: Completion of a community needs assessment. Public Health Nurs. 1996;13(2):112–9. https://doi.org/10.1111/j.1525-1446.1996.tb00228.x .
Running A, Martin K, Tolle LW. An innovative model for conducting a participatory community health assessment. J Community Health Nurs. 2007;24(4):203–13. https://doi.org/10.1080/07370010701645869 .
Smith SM, Long J, Deady J, O'Keeffe F, Handy D, O'Dowd T. Adapting developing country epidemiological assessment techniques to improve the quality of health needs assessments in developed countries. BMC Health Serv Res. 2005;5(1):1–7. https://doi.org/10.1186/1472-6963-5-32 .
Wood EA, Chapman KS, Beau de Rochars VM, Mckune SL. Community-based health needs assessment in Léogâne and Gressier, Haiti: six years post-earthquake. J Int Humanit Action. 2017;2(1):1–8. https://doi.org/10.1186/s41018-017-0026-z .
Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D, Wang J. A mixed-methods approach to understanding community participation in community health needs assessments. J Public Health Manag Pract. 2017;23(2):112–21. https://doi.org/10.1097/PHH.0000000000000362 .
Lillie-Blanton M, Hoffman SC. Conducting an assessment of health needs and resources in a racial/ethnic minority community. Health Serv Res. 1995;30(1 Pt 2):225.
Irani P, Bohn C, Halasan C, Landen M, McCusker D. Community health assessment: driving the need for current, easily accessible population health data. J Public Health Manag Pract. 2006;12(2):113–8. https://doi.org/10.1097/00124784-200603000-00002 .
Alberti P. Community health needs assessments: filling data gaps for population health research and management. EGEMS. 2014;2(4). https://doi.org/10.13063/2327-9214.1174 .
Skinner D, Franz B, Kelleher K. What challenges do nonprofit hospitals face in taking on community health needs assessments? A qualitative study from Appalachian Ohio. J Rural Health. 2018;34(2):182–92. https://doi.org/10.1111/jrh.12246 .
Stoto MA, Davis MV, Atkins A. Making better use of population health data for community health needs assessments. EGEMs. 2019;7(1). https://doi.org/10.5334/egems.305 .
Smith LU, Burdine JN. Community health assessment opportunities and challenges in the 21st century: Implications for professional development. J Public Health Manag Pract. 2017;23:S63–4. https://doi.org/10.1097/PHH.0000000000000601 .
Hawe P. Needs assessment must become more change-focused. Aust N Z J Public Health. 1996;20(5):473–8. https://doi.org/10.1111/j.1467-842x.1996.tb01624.x .
Jordan J, Wright J, Wilkinson J, Williams R. Assessing local health needs in primary care: understanding and experience in three English districts. Qual Health Care. 1998;7(2):83–9. https://doi.org/10.1136/qshc.7.2.83 .
Curtis DC. Evaluation of community health assessment in Kansas. J Public Health Manag Pract. 2002:20–5. https://doi.org/10.1097/00124784-200207000-00005 .
Kim S, Flaskerud JH, Koniak-Griffin D, Dixon EL. Using community-partnered participatory research to address health disparities in a Latino community. J Prof Nurs. 2005;21(4):199–209. https://doi.org/10.1016/j.profnurs.2005.05.005 .
Crossley M. Tax-exempt hospitals, community health needs and addressing disparities. Howard Law J. 2011;55:687.
Schifferdecker KE, Bazos DA, Sutherland KA, LaFave LRA, Fedrizzi R, Hoebeke J. A review of tools to assist hospitals in meeting community health assessment and implementation strategy requirements. J Healthc Manag. 2016;61(1):44.
Becker KL. Conducting community health needs assessments in rural communities: Lessons learned. Health Promot Pract. 2015;16(1):15–9. https://doi.org/10.1177/1524839914555887 .
Pepall E, James R, Earnest J. Guidelines for conducting rapid participatory appraisals of community health needs in developing countries: experience from Tulikup, Bali. Asia Pac J Public Health. 2006;18(3):42–8. https://doi.org/10.1177/10105395060180030801 .
Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D, Wang J. Community health needs assessment: potential for population health improvement. Popul Health Manag. 2016;19(3):178–86. https://doi.org/10.1089/pop.2015.0075 .
Solet D, Ciske S, Gaonkar R, Horsley K, McNees M, Nandi P, et al. Effective community health assessments in King County, Washington. J Public Health Manag Pract. 2009;15(1):33–40. https://doi.org/10.1097/PHH.0b013e3181903c11 .
Spice C, Snyder K. Reviewing self-reported impacts of community health assessment in local health jurisdictions. J Public Health Manag Pract. 2009;15(1):18–23. https://doi.org/10.1097/PHH.0b013e3181903c57 .
Diaz HJ-M, Ainsworth D, Schmidtlein MC. Funding priorities: data-driven approach for prioritizing community health needs in vulnerable communities. Health Promot Pract. 2019;20(4):616–23. https://doi.org/10.1177/1524839918771977 .
Franz B, Cronin CE, Singh S. Are nonprofit hospitals addressing the most critical community health needs that they identify in their community health needs assessments? J Public Health Manag Pract. 2021;27(1):80–7. https://doi.org/10.1097/phh.0000000000001034 .
Cramer GR, Singh SR, Flaherty S, Young GJ. The progress of US hospitals in addressing community health needs. Am J Public Health. 2017;107(2):255–61. https://doi.org/10.2105/AJPH.2016.303570 .
Kazda MJ, Beel ER, Villegas D, Martinez JG, Patel N, Migala W. Methodological complexities and the use of GIS in conducting a community needs assessment of a large US municipality. J Community Health. 2009;34(3):210–5. https://doi.org/10.1007/s10900-008-9143-3 .
Pennel CL, McLeroy KR, Burdine JN, Matarrita-Cascante D. Nonprofit hospitals’ approach to community health needs assessment. Am J Public Health. 2015;105(3):e103–13. https://doi.org/10.2105/ajph.2014.302286 .
Vance RA, Basta TB, Bute JJ, Denham SA. Identifying the health needs in rural Appalachian Ohio: Outcomes of a rural community-academic partnership. Am J Health Sci. 2012;3(2):115–24. https://doi.org/10.19030/ajhs.v3i2.6942 .
Bias T, Abildso C, Sarkees E. The Importance of Individual-Site and System-Wide Community Health Needs Assessments. Front Public Health. 2020;20. https://doi.org/10.3389/fpubh.2020.00020 .
Billings JR, Cowley S. Approaches to community needs assessment: a literature review. J Adv Nurs. 1995;22(4):721–30. https://doi.org/10.1046/j.1365-2648.1995.22040721.x .
Brazil K, Anderson M. Assessing health service needs: Tools for health planning. HealthC Manage Forum. 1996:22–7. https://doi.org/10.1016/S0840-4704(10)60940-4 .
Campbell S. Assessing community healthcare needs: lessons from Africa. Nurs Stand. 2001;15(47):41. https://doi.org/10.7748/ns2001.08.15.47.41.c3070 .
Carlton EL, Singh SR. Joint community health needs assessments as a path for coordinating community-wide health improvement efforts between hospitals and local health departments. Am J Public Health. 2018;108(5):676–82. https://doi.org/10.2105/ajph.2018.304339 .
Declercq ER, Bichell TJV, Center JK. Population-based needs assessment: bringing public health to midwifery practice. J Nurse Midwifery. 1997;42(6):478–88. https://doi.org/10.1016/s0091-2182(97)00081-5 .
Evans-Agnew R, Reyes D, Primomo J, Meyer K, Matlock-Hightower C. Community health needs assessments: Expanding the boundaries of nursing education in population health. Public Health Nurs. 2017;34(1):69–77. https://doi.org/10.1111/phn.12298 .
Guareschi PA, Jovchelovitch S. Participation, health and the development of community resources in Southern Brazil. J Health Psychol. 2004;9(2):311–22. https://doi.org/10.1177/1359105304040896 .
Holakouie NK, Ahmadvand A, Ahmadnezhad E, Alami A. A community assessment model appropriate for the Iranian community. Iran J Public Health. 2014;43(3):323.
Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19(1):173–202. https://doi.org/10.1146/annurev.publhealth.19.1.173 .
King CJ, Roach JL. Community health needs assessments: a framework for America’s hospitals. Popul Health Manag. 2016;19(2):78–80. https://doi.org/10.1089/pop.2015.0053 .
Misra R, Ballard D. Community needs and strengths assessments as an active learning project. J Sch Health. 2003;73(7):269–71. https://doi.org/10.1111/j.1746-1561.2003.tb06577.x .
Powell RE, Doty AM, Rising KL, Karp DN, Baehr A, Carr BG. A content analysis of nonprofit hospital community health needs assessments and community benefit implementation strategies in Philadelphia. J Public Health Manag Pract. 2018;24(4):326–34. https://doi.org/10.1097/phh.0000000000000621 .
Reece SM. Community analysis for health planning: strategies for primary care practitioners. The. Nurse Pract. 1998;23(10):46 49, 53-46 passim.
Stoto MA, Straus SG, Bohn C, Irani P. A web-based tool for assessing and improving the usefulness of community health assessments. J Public Health Manag Pract. 2009;15(1):10–7. https://doi.org/10.1097/01.PHH.0000342944.48703.21 .
Wetta RE, Pezzino G, LaClair B, Orr S, Brown MB. Voices across Kansas: community health assessment and improvement efforts among local health departments. J Public Health Manag Pract. 2014;20(1):39–42. https://doi.org/10.1097/phh.0b013e3182a9572a .
Download references
Acknowledgements
We acknowledge contribution of the research assistants helped with data extraction.
This work was funded by department of UHC Life course/Integrated Health Services (IHS), World Health Organization (WHO) headquarter (HQ). ZA received the research grant. The authors HR, AS, and SE from WHO commissioned the study, contributed to the direction of the work, and commented on the drafts.
Author information
Authors and affiliations.
Department of Universal Health Coverage/Health Systems (UHS), World Health Organization, Regional Office for the Eastern Mediterranean, Cairo, Egypt
Hamid Ravaghi
Department of Integrated Health Services (IHS), World Health Organization, Headquarters, Geneva, Switzerland
Ann-Lise Guisset
Department of Healthier Populations (DHP), World Health Organization, Regional Office of Eastern Mediterranean Region, Cairo, Egypt
Samar Elfeky
Center for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, UK
Naima Nasir
National library and Archives of Iran, Tehran, Iran
Sedigheh Khani
National Institute of Health Research (NIHR), Tehran University of Medical Sciences, Tehran (TUMS), Tehran, Iran
Elham Ahmadnezhad
Zhaleh Abdi
You can also search for this author in PubMed Google Scholar
Contributions
AG, HR and SE conceived the study and participated in its design. SK conducted the literature search and prepared the search results for analysis. NN developed the study framework, the data abstraction forms and the manuscript outline. The literature was analysed by ZA, EA and NN under the supervision of HR and AG. ZA drafted the final version of the manuscript and HR, NN, AG and SE reviewed it. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Zhaleh Abdi .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors have no competing interests. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the World Health Organization (WHO).
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
PubMed database search strategy.
Additional file 2.
Content of the extraction forms.
Additional file 3.
List of included empirical papers [ 156 – 159 ].
Additional file 4.
List of included non-empirical papers [ 160 -– 175 ] .
Additional file 5.
Health indicators collected by community health assessment surveys.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ravaghi, H., Guisset, AL., Elfeky, S. et al. A scoping review of community health needs and assets assessment: concepts, rationale, tools and uses. BMC Health Serv Res 23 , 44 (2023). https://doi.org/10.1186/s12913-022-08983-3
Download citation
Received : 20 May 2022
Accepted : 19 December 2022
Published : 17 January 2023
DOI : https://doi.org/10.1186/s12913-022-08983-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health Needs Assessment
- Needs Assessment
- Assets Assessment
- Population Health
- Scoping Review
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Joyner Library
- Laupus Health Sciences Library
- Music Library
- Digital Collections
- Special Collections
- North Carolina Collection
- Teaching Resources
- The ScholarShip Institutional Repository
- Country Doctor Museum
HLTH 4609: Needs Assessment and Program Planning: Literature Review
- Health Statistics Sources
- Literature Review
- Evaluate Webpages
- APA Citation
Choosing a Topic
Choosing your topic is one of the most important steps for a graduate student, and should be done in consultation with your faculty advisor. Some of the tips presented in the video below can help you get started.
The Literature Review
This tutorial from NCSU gives a good overview of the process of the literature review.
Types of Literature Reviews
Completing Literature Reviews
Links to Further Help You...
- UNC Writing Center Handout for Writing a Lit Review
- Purdue Online Writing Lab Social Work Literature Review Guidelines (Not only for Social Work!)
- UW-Madison Writing Center Learn How to Write a Review of Literature
- University of Toronto The Literature Review: A Few Tips on Conducting It
- Mindmap The Literature Review in Under 5 Minutes
- << Previous: Health Statistics Sources
- Next: Evaluate Webpages >>
- Last Updated: Dec 21, 2022 1:54 PM
- URL: https://libguides.ecu.edu/HLTH4609
Harvey Cushing/John Hay Whitney Medical Library
- Collections
- Research Help
YSN Doctoral Programs: Steps in Conducting a Literature Review
- Biomedical Databases
- Global (Public Health) Databases
- Soc. Sci., History, and Law Databases
- Grey Literature
- Trials Registers
- Data and Statistics
- Public Policy
- Google Tips
- Recommended Books
- Steps in Conducting a Literature Review
What is a literature review?
A literature review is an integrated analysis -- not just a summary-- of scholarly writings and other relevant evidence related directly to your research question. That is, it represents a synthesis of the evidence that provides background information on your topic and shows a association between the evidence and your research question.
A literature review may be a stand alone work or the introduction to a larger research paper, depending on the assignment. Rely heavily on the guidelines your instructor has given you.
Why is it important?
A literature review is important because it:
- Explains the background of research on a topic.
- Demonstrates why a topic is significant to a subject area.
- Discovers relationships between research studies/ideas.
- Identifies major themes, concepts, and researchers on a topic.
- Identifies critical gaps and points of disagreement.
- Discusses further research questions that logically come out of the previous studies.
APA7 Style resources
APA Style Blog - for those harder to find answers
1. Choose a topic. Define your research question.
Your literature review should be guided by your central research question. The literature represents background and research developments related to a specific research question, interpreted and analyzed by you in a synthesized way.
- Make sure your research question is not too broad or too narrow. Is it manageable?
- Begin writing down terms that are related to your question. These will be useful for searches later.
- If you have the opportunity, discuss your topic with your professor and your class mates.
2. Decide on the scope of your review
How many studies do you need to look at? How comprehensive should it be? How many years should it cover?
- This may depend on your assignment. How many sources does the assignment require?
3. Select the databases you will use to conduct your searches.
Make a list of the databases you will search.
Where to find databases:
- use the tabs on this guide
- Find other databases in the Nursing Information Resources web page
- More on the Medical Library web page
- ... and more on the Yale University Library web page
4. Conduct your searches to find the evidence. Keep track of your searches.
- Use the key words in your question, as well as synonyms for those words, as terms in your search. Use the database tutorials for help.
- Save the searches in the databases. This saves time when you want to redo, or modify, the searches. It is also helpful to use as a guide is the searches are not finding any useful results.
- Review the abstracts of research studies carefully. This will save you time.
- Use the bibliographies and references of research studies you find to locate others.
- Check with your professor, or a subject expert in the field, if you are missing any key works in the field.
- Ask your librarian for help at any time.
- Use a citation manager, such as EndNote as the repository for your citations. See the EndNote tutorials for help.
Review the literature
Some questions to help you analyze the research:
- What was the research question of the study you are reviewing? What were the authors trying to discover?
- Was the research funded by a source that could influence the findings?
- What were the research methodologies? Analyze its literature review, the samples and variables used, the results, and the conclusions.
- Does the research seem to be complete? Could it have been conducted more soundly? What further questions does it raise?
- If there are conflicting studies, why do you think that is?
- How are the authors viewed in the field? Has this study been cited? If so, how has it been analyzed?
Tips:
- Review the abstracts carefully.
- Keep careful notes so that you may track your thought processes during the research process.
- Create a matrix of the studies for easy analysis, and synthesis, across all of the studies.
- << Previous: Recommended Books
- Last Updated: Jan 4, 2024 10:52 AM
- URL: https://guides.library.yale.edu/YSNDoctoral
Literature reviews
A literature review is a research task that finds, evaluates and discusses information on a particular topic. You need to analyse multiple texts, and discuss key ideas that you find in the reading.
A literature review may also identify gaps for further research. It is not a process of summarising texts separately – that is done in an annotated bibliography .
A good literature review should:
- be well researched, planned and structured
- discuss a relevant issue, problem or practice that relates to your subject
- explain why your chosen topic is important
- identify key ideas or themes in the literature
- synthesise these findings into thematic paragraphs, using sufficient citations and correct referencing
- demonstrate your understanding of the topic and develop your knowledge and evidence-based practice.
Literature reviews differ across disciplines, so use your assessment instructions and marking criteria as your ultimate guide.
7 steps for writing a literature review
1. analyse the task.
Read the assessment instructions and marking rubric carefully. Note how many sources you need to include in your literature review and any guidelines on selecting the literature.
Choose a topic that interests you. A topic that is important to you will help you stay focused.
2. Establish a clear research question
A good research question will help you narrow down your topic so that it is manageable. If your question is too broad, you may be overwhelmed by the reading. If it is too narrow, you won’t find enough literature.
3. Search for relevant literature
Use keywords from your research question to begin searching .
In the research question "What factors impact student learning when on nursing placement?", the keywords are: student, learning, nursing and placement.
4. Read and review the literature, and take notes
When reading the literature, consider the following:
- Is the article relevant to your topic? For journal articles, read the abstract. For other sources, scan quickly and discard if you can’t see anything useful.
- Who is the author/s and what is their expertise?
- Is the source credible and scholarly ? Use any evaluation tools provided by your subject.
- What is the main topic and what themes are discussed?
Pay attention to important information, such as the abstract, introduction, headings/subheadings, graphs/tables and conclusion.
Take notes using the Cornell method or a note-taking grid. Keeping notes that help you remember the content and relevance of each source is vital for writing a literature review.
- Example note-taking grid for a literature review [Word - 14KB]
5. Identify common themes or areas for further research
It's important to understand the relationships between the sources you've read. Look out for:
- themes: what questions, ideas or topics recur across the literature? Where do authors agree or disagree?
- areas for further research: what is missing from the literature? Are there any weaknesses?
6. Plan the structure of the literature review
Before you start writing, plan how your literature review will be organised.
Literature reviews are usually organised thematically, meaning they discuss one theme after another. You can also organise your ideas chronologically (from past to present) or by methodology (e.g. comparing findings from qualitative and quantitative research).
7. Write, edit, proofread, submit
It's easy to get lost in the reading and not leave enough time for polishing your writing. Use the Assessment Planner to make a clear study plan that includes time for writing, editing and proofreading.
Structure of a literature review
Introduction.
The introduction should include:
- context or background : give a brief summary of the context for your research question and explain why it is important
- purpose (thesis statement): state the purpose of the literature review. This is a statement generated from the research question
- scope (roadmap): outline the specific themes the literature review will focus on and give the reader a sense of how your writing is organised.
Each body paragraph focuses on a specific theme and draws on several pieces of literature.
Paragraphs should include:
- topic sentence: start with the theme of the paragraph
- synthesis of evidence: make connections between multiple sources by comparing and contrasting their views. Use summaries, paraphrases and quotes , and don't forget to properly reference your sources
- analysis or evaluation: add your own interpretation of the findings and comment on any strengths, weaknesses, gaps or areas for further research in the literature
- link: end the paragraph by either linking back to your main topic or to the following paragraph.
Conclusions should include:
- restate the purpose of the review
- summary of the main findings : remind your reader of the main points. Make sure you paraphrase your ideas, so you don’t use the same wording as elsewhere in the literature review
- implications of the findings: suggest how the findings might be important for practice in your field
- areas for further research : provide suggestions for future research to address the problem, issue or question.
The conclusion is followed by a Reference list or Bibliography. Consult the Style notes page of the Academic Referencing Tool for examples.
For complete sample literature reviews with further annotations, see the Word and PDF documents below.
- Example Literature Review - Allied Health [PDF 245KB]
- Example Literature Review - Allied Health [Word 69KB]
- Example Literature Review - Education [PDF 283KB]
- Example Literature Review - Education [Word 104KB]
Further resources
- Using a reading to choose a research topic worksheet
- Manchester Academic Phrasebank - Phrases for academic writing and reporting on research
- Turn a stack of papers into a literature review: Useful tool for beginners (Journal article)
Pathfinder link
Still have questions? Do you want to talk to an expert? Peer Learning Advisors or Academic Skills and Language Advisors are available.
Cant R., Ryan, C., Hughes, L., Luders, E., & Cooper, S. (2021). What helps, what hinders? Undergraduate nursing students’ perceptions of clinical placements based on a thematic synthesis of literature. SAGE Open Nursing, 7, 1-20. https://doi.org/10.1177/23779608211035845 Adapted and used under CC BY-NC 4.0 license
- << Previous: Annotated bibliographies
- Next: Presentations >>

Literature Review: Assess your Literature Review
- Video Tutorial
- Research Question
- Select Resources
- Search Strategy
Assess your Literature Review
- Sample Literature Reviews
- Resource List
- Quick Links
- Avoid Plagiarism
- Use the rubric below to evaluate the quality of your literature review. If your instructor has provided you with a rubric, you should use the criteria listed in that course or assignment rubric to ensure that your paper will meet the expectations for the course. ( Download a copy of the rubric.)
Adapted from Education 690: Assessment Rubric/Criteria for Literature Review, retrieved September 29,2010 from http://edweb.sdsu.edu/courses/ed690dr/grading/literaturereviewrubrique.html and Boote, D.N. & Biele, P. (2005). Scholars before researchers: On the centrality of the dissertation literature review in research preparation. Educational Researcher. 34(6) p. 8.
- << Previous: PLAGIARISM
- Next: Sample Literature Reviews >>
- Last Updated: Apr 24, 2024 3:03 PM
- URL: https://research.auctr.edu/literaturereview

IMAGES
VIDEO
COMMENTS
Included studies. A systematic review of the literature was conducted using a combined search for all qualitative questions. Six studies were included in this review (Abendstern 2013, Abendstern 2014, Bolger 2014, Darling 2012, Symonds 2018 and Yeung 2016).The data provided evidence on the views and experiences of a social work needs assessment.
A review of recent literature on community-based needs assessments uncovered numerous resources for conducting evaluations of digital platforms, however, a key gap is the lack of practical guidance for conducting needs assessments in close collaboration with communities in ways that acknowledge existing needs, resources, supports and ...
The stand-alone literature review can be categorized by the purpose for the review, which needs to be determined before any work is done. Building from Paré et al. (2015) and Templier and Paré (2015), we group literature reviews into four categories based on the review's purpose: describe, test, extend, and critique. This section provides a ...
Entering the term "needs assessment" into PubMed, with a limit on the term only appearing in the title and abstract, no limits on language and articles published in the past 20 years yields 2,418 results. ... This review of the literature was by no means systematic but had as its aim to highlight the gap between tools used to assess health ...
Writing a literature review requires a range of skills to gather, sort, evaluate and summarise peer-reviewed published data into a relevant and informative unbiased narrative. Digital access to research papers, academic texts, review articles, reference databases and public data sets are all sources of information that are available to enrich ...
See Full PDFDownload PDF. Journal of Advanced Nursing, 1995, 22, 721-730 Approaches to community needs assessment: a literature review Jennifer Ruth Billings BSc (Hons) RGN RHV DPNS Research Assistant and Sarah Cowley BA Phi3 PGDE RGN RCNT RHV FWT HVT Lecturer, Department of Nursing Studies, Kings CollegeLondon, London, England ...
This literature review sets out to explore, delineate and critically analyse the various approaches to community needs assessment, to facilitate a greater understanding of their strengths and weaknesses. In the light of the growing awareness of professionals in the community of the need to undertake health needs assessments of the population, this literature review sets out to explore ...
Examples of literature reviews. Step 1 - Search for relevant literature. Step 2 - Evaluate and select sources. Step 3 - Identify themes, debates, and gaps. Step 4 - Outline your literature review's structure. Step 5 - Write your literature review.
Community health needs and assets assessment is a means of identifying and describing community health needs and resources, serving as a mechanism to gain the necessary information to make informed choices about community health. The current review of the literature was performed in order to shed more light on concepts, rationale, tools and uses of community health needs and assets assessment.
Social Work Literature Review Guidelines (Not only for Social Work!) UW-Madison Writing Center. Learn How to Write a Review of Literature. University of Toronto. ... Tags: health, Health needs assessment, Health program, Health program planning, HLTH 4609. East Carolina University.
Systematic identification of a population's needs or the assessment of individuals to determine the proper level of services needed. | Explore the latest full-text research PDFs, articles ...
Chapter II: Literature Review Needs Assessment and Analysis Needs assessment is the process of identifying performance n~eds and then prioritizing those needs (Kaufman, 1986, 1994; Rothwell & Kazanas, 2004). Stated another way, a performance need is the difference between current and desired
literature review on Protective Factors). Some risk/needs assessment tools take a more strengths-based approach by considering the presence of protective factors when estimating a youth's level of risk (Vincent, Guy, and Grisso 2012). Responsivity factors. may also be considered in risk/needs assessments. They are noncriminogenic factors that ...
A literature review is an integrated analysis-- not just a summary-- of scholarly writings and other relevant evidence related directly to your research question.That is, it represents a synthesis of the evidence that provides background information on your topic and shows a association between the evidence and your research question.
7 steps for writing a literature review. 1. Analyse the task. Read the assessment instructions and marking rubric carefully. Note how many sources you need to include in your literature review and any guidelines on selecting the literature. Choose a topic that interests you.
In addition, they state that a quality literature review needs to be replicable, that is, the method must be described such that an external reader could replicate the study and reach similar findings. Lastly, they state that a literature review must be useful for scholars and practitioners. However, evaluating different types of literature ...
Assessment; Avoid Plagiarism; Assess your Literature Review. Use the rubric below to evaluate the quality of your literature review. If your instructor has provided you with a rubric, you should use the criteria listed in that course or assignment rubric to ensure that your paper will meet the expectations for the course.
Background. A rigorous learning needs assessment (LNA) is a crucial initial step in the Continuing Professional Development (CPD) process. This scoping review aimed to collate, summarize, and categorize the reported LNA approaches adopted to inform healthcare professional CPD and highlight the gaps for further research.
Conclusion. Considering a proposal for a 'harmonised assessment approach' in a heterogeneous multi-country context of 31 EU/EEA countries, the literature review confirms that, for the purpose of the planned EU/EEA-wide training needs assessment, the most optimal way is to administer an online survey.
Assessment is frequently described as a four-step process.1,7 Learning outcomes or objectives are developed first. Second, assessment tools are created to measure how well the student has learned. The third step is the actual teaching and learning process, during and after which assess-ment tools can be administered.
The Centers for Medicare & Medicaid Services have mandated that hospitals implement measures to screen social determinants of health (SDoH). We sought to report on available SDoH screening tools. PubMed, Scopus, Web of Science, as well as the grey literature were searched (1980 to November 2023). The included studies were US-based, written in English, and examined a screening tool to assess SDoH.