Endocrine Abstracts
- Issues/Conferences
- Our Services
ICEECE2012 Poster Presentations Clinical case reports - Pituitary/Adrenal (58 abstracts)

Central diabetes insipidus: about two clinical cases
C. nogueira 1, , m. matos 1, , c. esteves 1, , g. jorge 1 , j. couto 2 , c. neves 1, , j. queirós 1 , e. vinha 1 , i. bernardes 1 & d. carvalho 1,.
1 Centro Hospitalar São João, Porto, Portugal; 2 Instituto Português de Oncologia, Porto, Portugal; 3 University of Porto, Porto, Portugal.
Introduction: Central diabetes insipidus (CDI) is produced by the destruction of the magnocellular neurons of the hypothalamic supraoptic and paraventricular nuclei which results in decreased arginine vasopressin (AVP) synthesis and secretion.
Case report 1: Forty-five year old female, previously healthy, was observed in April 2011 complaining of polydipsia, polyuria, nocturia and weight loss since January. Diabetes mellitus (DM) was excluded and she was admitted for study of possible diabetes insipidus. Water deprivation test was suggestive of CDI. Magnetic resonance imaging (MRI) showed infundibular hypophysitis and no hyperintense signal in the neurohypophysis. Autoimmune diseases, infections and infiltrative diseases were excluded. Imaging (chest x-ray, abdominal ultrasound, mammography, breast ultrasound and thoracoabdominal CT) was normal. No other pituitary deficits were shown. She started therapy with oral desmopressin with clinical improvement.
Case report 2: Fourty-three year old man, previously healthy, was seen in August 2011 complaining of polydipsia, polyuria and nocturia during the previous 3 months. DM was excluded. Water deprivation test was positive for CDI. Pituitary MRI was normal, with normal signal of high intensity in the neutohypophysis. He had no other hormonal deficits. Autoimmune and infectous diseases were excluded. After initiation of oral desmopressin the symptoms disappeared.
Discussion: In both cases it was not determined the etiology of CDI, as it may occur in 20–50% of CDI cases. In our institution is not possible to determine antibodies towards vasopressin secretory cells, which does not allow the diagnosis of this autoimmune form of CDI. The infundibular hypophysitis, observed in the first case, can occur in about 50% of idiopathic cases and more frequently in women. The lymphocytic hypophysitis can be diagnosed by pituitary biopsy, but it’s a very aggressive procedure and almost never performed. These cases highlight the difficulty of the etiologic diagnosis of CDI. However, proper treatment allows the symptoms control.
Declaration of interest: The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research project.
Funding: This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
15th International & 14th European Congress of Endocrinology
Browse other volumes
Article tools
My recent searches, my recently viewed abstracts, nogueira c., bernardes i., carvalho d..

Endocrine Abstracts ISSN 1470-3947 (print) | ISSN 1479-6848 (online) © Bioscientifica 2024 | Privacy policy | Cookie settings
BiosciAbstracts
Bioscientifica Abstracts is the gateway to a series of products that provide a permanent, citable record of abstracts for biomedical and life science conferences.
Diabetes Insipidus Case Study (60 min)
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
You just started your shift, what nursing assessments will be your priority at this point?
- Assess ventilator and respiratory status, lung sounds, SpO2
- Assess EVD system for integrity and that it is draining appropriately
- Complete neuro exam including pupils, GCS, reflexes, and LOC.
- Full set of vitals plus assessing IV sites for signs of infiltration or infection
- Assessing foley site and urine output
- Turning and assessing skin top to tail
Mrs. Ford’s vital signs are as follows: BP 124/68 MAP 86
HR 84 Temp 98.9 RR 16 (ventilated) ICP 12
She is not on any sedation. You determine her GCS is 6, she withdraws to pain, but does not open her eyes. Her pupils are equal and reactive bilaterally, 4mm. For this hour she has put out 120 ml of urine that is clear and yellow. She is receiving normal saline at 75 mL/hour as well as tube feeds at 40 mL/hour. Her EVD is open at 15 cmH 2 O and draining a clear pink fluid, 6 ml this hour.
faq lesson=”true” blooms=”Application” question=”Calculate her cerebral perfusion pressure.”]
- CPP = MAP – ICP
- 86 – 12 = 74 mmHg [/faq]
Given the assessment information that you have, what are you most concerned for with this patient?
- Immobility – skin and muscle breakdown
- Increased ICP → herniation → death
- Damage to Pituitary and/or Hypothalamus glands → can cause SIADH, DI, temperature regulation issues, as well as issues with CNS functions like breathing
- This patient clearly has a significant brain injury. I would be concerned for and monitoring for the following complications:
Hourly urine output for Mrs. Ford For the last 3 hours were 180 mL, 240 mL, and 440 mL. The urine is clear and barely pale yellow. Her blood pressure is 108/56, HR is 104. Her ICP is 15.
What could be going on physiologically with Mrs. Ford?
- This is likely Diabetes Insipidus due to the known neurological issue and the excessive output of clear, barely pale yellow urine.
- Neurological damage can cause damage to the pituitary gland – causing a LACK of secretion of ADH (Antidiuretic Hormone). This means the patient can no longer retain water and therefore begins to dump water excessively – this is why the urine looks almost like water.
- This will cause the blood to be super concentrated and could cause a lot of other issues because of it.
What further diagnostic testing do you expect the provider to order?
- Note: Polyuria WITHOUT hyperosmolality may indicate Primary Polydipsia – a condition in which patients literally drink water excessively and send themselves into a water intoxication/hypernatremic state.
- Check a CMP with serum osmolality to see if she is hyperosmolar or hypernatremic
- Check urine specific gravity and urine osmolarity – again this can tell us if she’s dumping lots of urine or if she’s just dumping a ton of water. Low specific gravity indiacates DI.
Lab Values: Na + 155 mg/dL Serum osmo 310 mOsm/kg Urine SG 1.005
Explain the significance of these lab values considering the patient's diagnosis.
- The patient is dumping excessive amounts of water in the urine, that is why her urine specific gravity is so low
- Because of the loss of water, the blood is now super concentrated, creating hypernatremia and a high serum osmolality.
What medications and or treatment changes do you expect the provider to order?
- The IV fluids need to be changed to D5W or D10W
- Free water via the OG tube will also help with the sodium levels
- DDAVP (Desmopressin) or Vasopressin should be ordered to replace the ADH that isn’t working
The provider orders the following:
Free water flush via OG Tube – 200 mL q4h
Change IVF to D5W at 125 mL/hr
Desmopressin (DDAVP) 2 mcg IV push q 12h
Daily weight
q4h Sodium and Serum Osmolality levels
You set the tube feeding pump to administer the free water and change the IV fluids while waiting for the DDAVP from the pharmacy
What regular monitoring will need to be done for Mrs. Ford during this treatment?
- Hourly urine output + urine specific gravity
- Continue frequent monitoring of vital signs and ICP/CPP
- Re-draw labs as ordered to ensure sodium is not being corrected too quickly
After 2 days of treatment, misses Fords urine output and urine specific gravity return to Baseline. However, she continues to have a GCS between 4 + 6, and now her left pupil is 8mm and fixed. The nurse notes her respiratory rate is erratic, her ICP is 18, and her heart rate is dropping.
What do you believe could be happening to Mrs. Ford at this time?
- Mrs. Ford may be experiencing brain herniation due to the bleeding and swelling in and around her brain
- Unfortunately, many times these patients cannot be returned to their normal baseline due to the extent of the damage.
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
- Publications
- Conferences & Events
- Professional Learning
- Science Standards
- Awards & Competitions
- Daily Do Lesson Plans
- Free Resources
- American Rescue Plan
- For Preservice Teachers
- NCCSTS Case Collection
- Partner Jobs in Education
- Interactive eBooks+
- Digital Catalog
- Regional Product Representatives
- e-Newsletters
- Bestselling Books
- Latest Books
- Popular Book Series
- Prospective Authors
- Web Seminars
- Exhibits & Sponsorship
- Conference Reviewers
- National Conference • Denver 24
- Leaders Institute 2024
- National Conference • New Orleans 24
- Submit a Proposal
- Latest Resources
- Professional Learning Units & Courses
- For Districts
- Online Course Providers
- Schools & Districts
- College Professors & Students
- The Standards
- Teachers and Admin
- eCYBERMISSION
- Toshiba/NSTA ExploraVision
- Junior Science & Humanities Symposium
- Teaching Awards
- Climate Change
- Earth & Space Science
- New Science Teachers
- Early Childhood
- Middle School
- High School
- Postsecondary
- Informal Education
- Journal Articles
- Lesson Plans
- e-newsletters
- Science & Children
- Science Scope
- The Science Teacher
- Journal of College Sci. Teaching
- Connected Science Learning
- NSTA Reports
- Next-Gen Navigator
- Science Update
- Teacher Tip Tuesday
- Trans. Sci. Learning
MyNSTA Community
- My Collections
A Case of Diabetes Insipidus
By David F. Dean (rr)
Share Start a Discussion
“Amanda Richards,” a 20-year-old junior in college, is majoring in biology and hopes to be a pediatrician one day. For about a month, she has been waking up frequently at night to go to the bathroom. Most recently, she has noticed that she needs to go to the bathroom during the day more often, almost hourly. Students read about these symptoms and then answer a set of directed questions designed to teach facts and principles of physiology using reference books, textbooks, the Internet, and each other as sources of information. The case has been used in a sophomore-level course in human anatomy and physiology as well as in senior-level course in general physiology.
Download Case
Date Posted
- Learn about the similarities and dissimilarities between diabetes insipidus and diabetes mellitus.
- Understand the basic differences between the four types of diabetes insipidus.
- Be able to define and describe excessive thirst and urination in adults.
- Understand the methods by which diabetes insipidus is diagnosed and treated.
- Learn about other conditions which produce symptoms similar to those produced by diabetes insipidus.
- Be able to describe the physiological effects of antidiuretic hormone other than the maintenance of body water balance.
Pituitary diabetes insipidus; diabetic; antidiuretic hormone; ADH; vasopressin; osmoreceptors; osmolarity; polyuria; polydipsia; supraoptic nuclei; kidney function
Subject Headings
EDUCATIONAL LEVEL
Undergraduate lower division, Undergraduate upper division
TOPICAL AREAS
TYPE/METHODS
Teaching Notes & Answer Key
Teaching notes.
Case teaching notes are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Teaching notes are intended to help teachers select and adopt a case. They typically include a summary of the case, teaching objectives, information about the intended audience, details about how the case may be taught, and a list of references and resources.
Download Notes
Answer Keys are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Download Answer Key
Materials & Media
Supplemental materials, you may also like.
Web Seminar
Join us on Thursday, June 13, 2024, from 7:00 PM to 8:00 PM ET, to learn about the science and technology of firefighting. Wildfires have become an e...
Join us on Thursday, October 10, 2024, from 7:00 to 8:00 PM ET, for a Science Update web seminar presented by NOAA about climate science and marine sa...
- Patient Care & Health Information
- Diseases & Conditions
- Diabetes insipidus
Diabetes insipidus (die-uh-BEE-teze in-SIP-uh-dus) is an uncommon problem that causes the fluids in the body to become out of balance. That prompts the body to make large amounts of urine. It also causes a feeling of being very thirsty even after having something to drink. Diabetes insipidus also is called arginine vasopressin deficiency and arginine vasopressin resistance.
While the terms "diabetes insipidus" and "diabetes mellitus" sound alike, the two conditions are not connected. Diabetes mellitus involves high blood sugar levels. It's a common condition, and it's often called simply diabetes.
There's no cure for diabetes insipidus. But treatment is available that can ease its symptoms. That includes relieving thirst, lowering the amount of urine the body makes and preventing dehydration.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms of diabetes insipidus in adults include:
- Being very thirsty, often with a preference for cold water.
- Making large amounts of pale urine.
- Getting up to urinate and drink water often during the night.
Adults typically urinate an average of 1 to 3 quarts (about 1 to 3 liters) a day. People who have diabetes insipidus and who drink a lot of fluids may make as much as 20 quarts (about 19 liters) of urine a day.
A baby or young child who has diabetes insipidus may have these symptoms:
- Large amounts of pale urine that result in heavy, wet diapers.
- Bed-wetting.
- Being very thirsty, with a preference for drinking water and cold liquids.
- Weight loss.
- Poor growth.
- Irritability.
- Constipation.
- Problems sleeping.
- Vision problems.
When to see a doctor
See your health care provider right away if you notice that you're urinating much more than usual and you're very thirsty on a regular basis.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
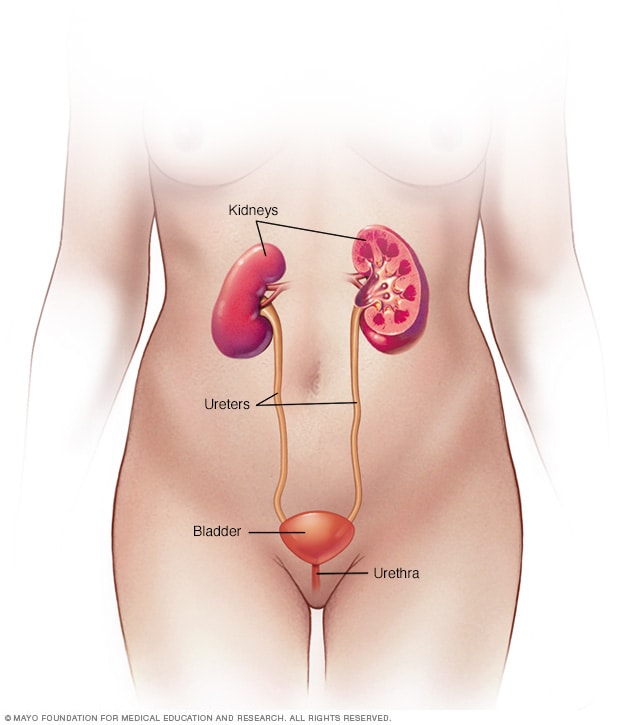
Female urinary system
Your urinary system includes the kidneys, ureters, bladder and urethra. The urinary system removes waste from the body through urine. The kidneys are located toward the back of the upper abdomen. They filter waste and fluid from the blood and produce urine. Urine moves from the kidneys through narrow tubes to the bladder. These tubes are called the ureters. The bladder stores urine until it's time to urinate. Urine leaves the body through another small tube called the urethra.
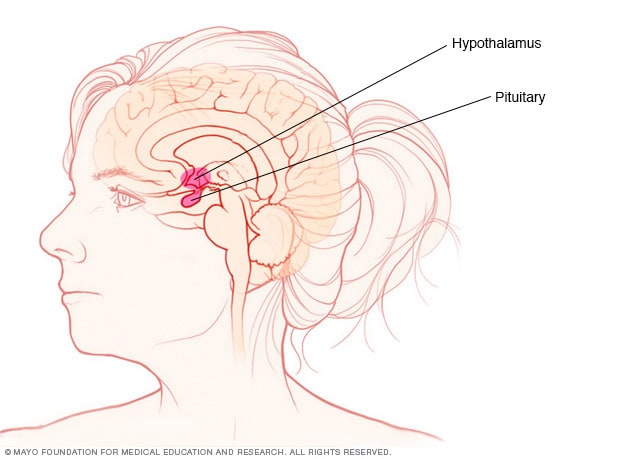

Pituitary gland and hypothalamus
The pituitary gland and the hypothalamus are in the brain. They control hormone production.
Diabetes insipidus happens when the body can't balance its fluid levels in a healthy way.
Fluid in the blood is filtered through the kidneys to remove waste. Afterward, most of that fluid is returned to the bloodstream. The waste and a small amount of fluid leave the kidneys as urine. Urine leaves the body after it's temporarily stored in the bladder.
A hormone known as antidiuretic hormone (ADH) — also called vasopressin — is needed to get the fluid that's filtered by the kidneys back into the bloodstream. ADH is made in a part of the brain called the hypothalamus. It's then stored in the pituitary gland, a small gland found at the base of the brain. Conditions that cause the brain to make too little ADH or disorders that block the effect of ADH cause the body to make too much urine.
In diabetes insipidus, the body can't properly balance fluid levels. The cause of the fluid imbalance depends on the type of diabetes insipidus.
- Central diabetes insipidus. Damage to the pituitary gland or hypothalamus from surgery, a tumor, a head injury or an illness can cause central diabetes insipidus. That damage affects the production, storage and release of ADH . An inherited disorder may cause this condition too. It also can be the result of an autoimmune reaction that causes the body's immune system to damage the cells that make ADH .
- An inherited disorder.
- Certain medicines, including lithium and antiviral medicines such as foscarnet (Foscavir).
- Low levels of potassium in the blood.
- High levels of calcium in the blood.
- A blocked urinary tract or a urinary tract infection.
- A chronic kidney condition.
- Gestational diabetes insipidus. This rare form of diabetes insipidus only happens during pregnancy. It develops when an enzyme made by the placenta destroys ADH in a pregnant person.
- Primary polydipsia. This condition also is called dipsogenic diabetes insipidus. People who have this disorder constantly feel thirsty and drink lots of fluids. It can be caused by damage to the thirst-regulating mechanism in the hypothalamus. It also has been linked to mental illness, such as schizophrenia.
Sometimes no clear cause of diabetes insipidus can be found. In that case, repeat testing over time often is useful. Testing may be able to identify an underlying cause eventually.
Risk factors
Anyone can get diabetes insipidus. But those at higher risk include people who:
- Have a family history of the disorder.
- Take certain medicines, such as diuretics, that could lead to kidney problems.
- Have high levels of calcium or low levels of potassium in their blood.
- Have had a serious head injury or brain surgery.
Complications
Dehydration.
Diabetes insipidus may lead to dehydration. That happens when the body loses too much fluid. Dehydration can cause:
- Extreme tiredness.
- Lightheadedness.
Electrolyte imbalance
Diabetes insipidus can change the levels of minerals in the blood that maintain the body's balance of fluids. Those minerals, called electrolytes, include sodium and potassium. Symptoms of an electrolyte imbalance may include:
- Loss of appetite.
- Ferri FF. Diabetes insipidus. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed Jan. 10, 2023.
- Diabetes insipidus. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/kidney-disease/diabetes-insipidus. Accessed Jan. 15, 2021.
- Bichet DG. Clinical manifestations and causes of central diabetes insipidus. https://www.uptodate.com/contents/search. Accessed Jan. 10, 2023.
- Bichet DG. Treatment of central diabetes insipidus (vasopressin deficiency). https://www.uptodate.com/contents/search. Accessed Jan. 10, 2023.
- AskMayoExpert. Diabetes insipidus and polyuria (child). Mayo Clinic; 2022.
- Melmed S, et al. Posterior pituitary. In: Williams Textbook of Endocrinology. 14th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Jan. 11, 2023.
- Walls RM, et al., eds. Electrolyte disorders. In: Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Elsevier; 2023. https://www.clinicalkey.com. Accessed Jan. 11, 2023.
- Arima H, et al. Changing the name of diabetes insipidus: A position statement of the working group for renaming diabetes insipidus. Journal of Clinical Endocrinology & Metabolism. 2022; doi:10.1210/clinem/dgac547.
Associated Procedures
- Genetic testing
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Clin Endocrinol Metab

Clinical Case Seminar
Central diabetes insipidus: a previously unreported side effect of temozolomide.
Temozolomide (TMZ) is an alkylating agent primarily used to treat tumors of the central nervous system. We describe 2 patients with apparent TMZ-induced central diabetes insipidus. Using our institution's Research Patient Database Registry, we identified 3 additional potential cases of TMZ-induced diabetes insipidus among a group of 1545 patients treated with TMZ.
Case Presentations:
A 53-year-old male with an oligoastrocytoma and a 38-year-old male with an oligodendroglioma each developed symptoms of polydipsia and polyuria approximately 2 months after the initiation of TMZ. Laboratory analyses demonstrated hypernatremia and urinary concentrating defects, consistent with the presence of diabetes insipidus, and the patients were successfully treated with desmopressin acetate. Desmopressin acetate was withdrawn after the discontinuation of TMZ, and diabetes insipidus did not recur. Magnetic resonance imaging of the pituitary and hypothalamus was unremarkable apart from the absence of a posterior pituitary bright spot in both of the cases. Anterior pituitary function tests were normal in both cases. Using the Research Patient Database Registry database, we identified the 2 index cases and 3 additional potential cases of diabetes insipidus for an estimated prevalence of 0.3% (5 cases of diabetes insipidus per 1545 patients prescribed TMZ).
Conclusions:
Central diabetes insipidus is a rare but reversible side effect of treatment with TMZ.
Temozolomide (TMZ) is an oral alkylating agent and an imidazotetrazine derivative of dacarbazine ( 1 ). TMZ is currently approved in the United States for treatment of glioblastoma multiforme and recurrent anaplastic astrocytoma. Off-label uses include the treatment of other tumors such as oligodendrogliomas, metastatic melanoma, nonpituitary neuroendocrine tumors, and aggressive pituitary neoplasms that are resistant to standard therapies ( 2 ). Treatment with TMZ is generally well tolerated. Common side effects include nausea/vomiting, headache, fatigue, and myelosuppression ( 3 , 4 ). In this paper we describe 2 cases of central diabetes insipidus that developed after TMZ initiation and resolved after discontinuation of TMZ. To search for other cases, we used our institution's Research Patient Database Registry (RPDR) to examine the records of patients treated with TMZ in several affiliated medical centers. In addition to the 2 index cases, 3 additional potential cases of TMZ-induced diabetes insipidus were identified. No prior report describes an association between diabetes insipidus with TMZ therapy.
A 53-year-old male initially presented with left-hand weakness and was found to have a 4.5-cm right posterior parietal lobe mass. He underwent a right parietal craniotomy and was diagnosed with a World Health Organization (WHO) grade II oligoastrocytoma. Surgery was followed by treatment with TMZ (150 mg daily). The patient developed new symptoms of polydipsia (approximately 5.5 L daily fluid intake) and polyuria/nocturia (urination of large volumes on an hourly basis during the day and nighttime) approximately 2 months after the initiation of TMZ. Laboratory tests obtained concurrently demonstrated hypernatremia and the presence of a urinary concentrating defect: serum sodium 151 mmol/L (normal 135–145 mmol/L), serum osmolality 319 mOsm/kg (normal: 280–296 mOsm/kg), and urine specific gravity 1.005. A modified overnight water deprivation test was also attempted, but it could not be completed. (The patient was instructed to avoid fluid intake overnight and have serum and urine laboratory tests performed in the morning. However, the patient consumed 1 L of fluid prior to the morning sample collection due to intense thirst.) Nonetheless, morning laboratory tests showed a serum sodium concentration of 149 mmol/L and a urine osmolality of 222 mOsm/kg.
Anterior pituitary function was assessed at the time of diagnosis and was normal ( Table 1 ). Treatment with twice-daily oral 1-desamino-8- D -arginine vasopressin acetate (DDAVP) (300 μg every morning and 400 μg every night) alleviated the patient's symptoms. Subsequent laboratory measures showed a serum sodium concentration of 145 mmol/L, serum osmolality 295 mOsm/kg, and urine osmolality of 508 mOsm/kg. TMZ was discontinued after 20 months of treatment due to durable tumor response/resolution, and additional antineoplastic treatment was not required. DDAVP was tapered off several months later, and polydipsia and polyuria did not recur. A modified overnight water deprivation test was repeated 4 weeks after DDAVP had been withdrawn. Laboratory tests on the following morning showed a serum sodium concentration of 140 mmol/L and a urine osmolality of 667 mOsm/kg. Whole-brain magnetic resonance imaging (MRI) scans performed before, during, and after TMZ treatment did not show any evidence of a mass lesion or infiltrative process in the pituitary or hypothalamus. The posterior pituitary bright spot was not visible before, during, or after development of diabetes insipidus. The patient did not receive any radiation therapy or additional chemotherapy for his malignancy before, during, or immediately after treatment with TMZ. Figure 1 illustrates a time line of the patient's biochemical test results. He has not experienced a recurrence of diabetes insipidus since discontinuation of TMZ. He has been followed by serial radiological imaging for approximately 6 years since completion of TMZ.
Anterior Pituitary Function Tests, Cases 1 and 2
Assay normal ranges are as follows: free T 4 (0.9–1.8 ng/mL); IGF-I (114–492 ng/mL); total T (270–1070 ng/dL); and prolactin (0–15 ng/mL).

The development and resolution of diabetes insipidus in case 1. ♦ and □ denote serum sodium concentration and urine osmolality, respectively.
A 38-year-old male was treated with TMZ for a WHO grade II oligodendroglioma located in the left frontal lobe. The patient underwent 2 craniotomies 4 years and 2 months prior to treatment with TMZ, respectively. Two months after starting TMZ (140 mg daily), the patient began to note an increased sense of thirst and frequency of urination. He voided large volumes of urine on an hourly basis during the daytime and woke approximately 10 times per night to urinate and to drink liquids. He developed mild hypernatremia (serum sodium concentration 146 mmol/L).
Concurrent serum and urine laboratory measurements showed a serum sodium concentration of 143 mmol/L, serum osmolality of 302 mOsm/kg, and urine specific gravity of 1.006. An additional set of laboratory tests demonstrated a serum osmolality of 296 mOsm/kg with a concurrent urine osmolality of 196 mOsm/kg. Anterior pituitary function tests assessed at the time of diagnosis were normal ( Table 1 ). Intranasal DDAVP (10 μg once to twice daily) relieved the patient's symptoms. TMZ was stopped 6 months after DDAVP was started due to tumor regression/resolution. The total duration of treatment with TMZ was 9 months. DDAVP was withdrawn 2 months after TMZ was discontinued, and the patient did not experience recurrent polydipsia or polyuria. Laboratory studies obtained 2 weeks after cessation of DDAVP showed a serum sodium concentration of 139 mmol/L, and concurrent urine-specific gravity of 1.019. Whole-brain MRIs performed before and after TMZ treatment and a dedicated pituitary MRI during active diabetes insipidus did not show any evidence of a mass lesion or infiltrative process in the pituitary or hypothalamus ( Figure 2 ). The posterior pituitary bright spot was not visible before, during, or after development of diabetes insipidus. The patient has not had any tumor recurrence since the completion of TMZ treatment and has not required any additional antineoplastic therapy. He has been followed by serial radiologic imaging for approximately eight years since completion of TMZ. He has not experienced a recurrence of diabetes insipidus since discontinuation of TMZ.

Postcontrast T1-weighted MRI sagittal images obtained from case 2 (A) prior to TMZ treatment and the development of diabetes insipidus, during TMZ treatment and active diabetes insipidus (B), and after TMZ was discontinued and diabetes insipidus had resolved (C).
Additional cases
The RPDR is an electronic data repository that compiles clinical and demographic data from patients in the Partners Healthcare system dating back to the early 1990s. The database contains records from more than 4.6 million patients and includes more than 1.2 billion clinical and demographic data entries. The registry may be searched using coded fields for medication prescriptions, medical diagnoses, laboratory parameters, radiological studies, interventional procedures, demographic details, vital signs, and certain examination findings. We queried patient records from the Massachusetts General Hospital, Brigham and Women's Hospital, and the Dana Farber Cancer Institute and identified 1545 patients (878 males and 667 females) treated with temozolomide.
We then performed a secondary query of these patients to identify individuals whose clinical records included a coded diagnosis of hypernatremia or diabetes insipidus or had received a prescription for desmopressin acetate or DDAVP. Forty-four of 1545 patients met these search criteria. The medical records of these 44 patients were thoroughly examined. Clinical histories and/or laboratory records were suggestive of possible TMZ-induced diabetes insipidus in 5 of these patients. Two of the 5 patients were the index cases 1 and 2 described above, and 3 additional potential cases were also identified. In most of the 39 excluded patients, individuals were diagnosed with hypernatremia in the days or weeks preceding their deaths, often in the context of alterations in mental status. Laboratory records indicate that these patients did not have urinary concentrating defects. A minority of the 39 patients were diagnosed with diabetes insipidus prior to treatment with TMZ (in the context of metastatic disease involving the pituitary and/or hypothalamus) or experienced transient diabetes insipidus after transsphenoidal surgery or a craniotomy.
A 45-year-old male received TMZ (140 mg daily) for treatment of a right frontal oligodendroglioma. Three months after the initiation of TMZ, he abruptly developed polydipsia and polyuria that was independent of fluid intake. Approximately 4 weeks later, TMZ was discontinued, and the patient began treatment with DDAVP by rhinal tube. DDAVP (10 μg once daily) successfully relieved his symptoms of polyuria and polydipsia. Shortly thereafter, the patient departed on a trip, but he did not remember to bring any DDAVP. He did not develop polydipsia and polyuria during his trip, and he had no further recurrence of these symptoms after his travels despite remaining off DDAVP. Serum and urine laboratory tests were not obtained prior to the initiation of DDAVP. Laboratory tests measured 3 months after discontinuation of DDAVP showed a serum sodium concentration of 144 mmol/L, serum osmolality 294 mOsm/kg, and a concurrent urine osmolality of 496 mOsm/kg. Whole-brain MRIs performed prior to TMZ therapy and 3 months after its conclusion did not show any evidence of a mass lesion or infiltrative process in the pituitary or hypothalamus. The patient did not receive any radiation therapy or additional chemotherapy before, during, or immediately after TMZ.
A 49-year-old male was treated with TMZ (280 mg daily for 7 days on alternate weeks separated by 7 days off treatment) for a clinically nonfunctioning pancreatic neuroendocrine tumor that had metastasized to the liver. Approximately 2 months after starting TMZ, the patient developed polydipsia and polyuria. He experienced persistent hypernatremia for approximately 1 month (serum sodium concentrations of 143–146 mmol/L, normal range of 136–142 mmol/L). Concurrent measurements of urine-specific gravity ranged from 1.003 to 1.006. (Serum osmolality and urine osmolality were not assessed.) The patient's serum creatinine rose from 1.2 to 1.6 mg/dL, and a fractional excretion of sodium was calculated to be 0.7%. The patient's polydipsia and polyuria spontaneously resolved after 2 months. TMZ was continued throughout this period of time and was terminated 13 months later. Prophylactic antibiotic therapy with trimethoprim/sulfamethoxazole was started approximately 2 weeks before the patient developed polyuria and polydipsia and acute renal insufficiency. The patient was given a presumptive diagnosis of acute interstitial nephritis. Laboratory evaluation did not show the presence of peripheral eosinophilia or urine eosinophils. The patient did not have any intracranial metastases or receive additional chemotherapy before or during treatment with TMZ. Whole-brain MRIs performed 1 year prior to TMZ treatment and 10 months after the resolution of polyuria and polydipsia did not reveal any mass lesion of infiltrative process involving the pituitary or hypothalamus.
A 44-year-old male received TMZ (150 mg daily) plus bevacizumab (10 mg/kg every 2 weeks) for treatment of an astrocytoma with gliomatosis cerebri. Serum sodium values and urinalyses were obtained on a biweekly basis during TMZ therapy. Three months after initiation of TMZ, laboratory measures demonstrated an increase in baseline serum sodium values from a range of 138–140 mmol/L to 142–145 mmol/L, and concurrent values of urine-specific gravity had decreased from 1.010–1.020 to less than 1.006–1.010. This probable urinary-concentrating defect reversed after approximately 6 weeks. Available records did not indicate whether the patient experienced symptoms of polydipsia or polyuria, but clinical notes did describe that he experienced new sleep difficulties during this period of time. Whole-brain MRI studies obtained before the initiation of TMZ, while the urinary concentrating defect was present, and 2 months after its resolution did not indicate the presence of a mass lesion or infiltrative process in the pituitary or hypothalamus. The patient did receive fractionated whole-brain irradiation (50.4 Gy, divided over 28 fractions) 6 months before starting TMZ.
We demonstrate for the first time that treatment with TMZ may be associated with the development of new central diabetes insipidus. In these cases, diabetes insipidus developed within 2–3 months after starting TMZ. Patients' symptoms and laboratory abnormalities corrected after treatment with DDAVP. Urinary concentrating defects eventually resolved in each of the cases. Reversal was documented within several months of TMZ cessation in 3 cases. In 2 potential cases of diabetes insipidus, spontaneous resolution occurred despite continuation of treatment with TMZ.
The precise mechanism for TMZ-induced diabetes insipidus is unclear. Posterior pituitary bright spots on MRI indicate the presence of antidiuretic hormone (ADH)-containing granules ( 5 , 6 ). This area of hyperintensity on T1-weighted images is absent in some normal individuals ( 7 ) and most patients with central diabetes insipidus ( 8 – 10 ). Posterior pituitary bright spots were not visible on precontrast T1-weighted images in cases 1 or 2 prior to treatment with TMZ, during active diabetes insipidus, or after TMZ had been discontinued (posterior pituitary bright spots also were not visible in the MRIs of cases 3, 4, and 5). TMZ may affect ADH production. Alternatively, TMZ might interfere with ADH storage and/or secretion from the neurohypophysis. An in vitro study demonstrated that treatment with TMZ causes actin depolymerization in human glioma cells ( 11 ). Filamentous actin regulates exocytosis in the neurons of the posterior pituitary, and disruption of the cytoskeleton may potentially impair intracellular transport of ADH to the axon terminal and hormone release ( 12 ). TMZ forms methyl adducts with purine bases ( 1 ). Potential modification of purinergic receptor signaling by TMZ and inhibition of protein kinase C activity may also affect ADH release ( 13 , 14 ).
Although standard TMZ dosing regimens typically consist of 5 days of treatment in every 28-day cycle, more intensive dosing strategies have also been studied ( 15 ). Four of the 5 patients described in this series received daily TMZ. One patient (case 4) was treated with daily TMZ on alternate weeks. It is unclear whether TMZ-induced diabetes insipidus occurs in patients receiving standard dosing regimens. Although approximately 43% of the 1545 patients treated with TMZ were female, all 5 cases of apparent TMZ-induced diabetes insipidus occurred in males. Due to the limited number of cases, however, we are unable to determine whether diabetes insipidus represents a gender-specific effect of TMZ.
Clinically significant diabetes insipidus appears to be a rare side effect of treatment with TMZ. If all 5 of the reported cases are included, the prevalence of diabetes insipidus was 0.3% in our survey of 1545 patients treated with TMZ. We postulate, however, that this figure likely underestimates the true prevalence of TMZ-induced diabetes insipidus in this population. Urinary incontinence and increased urinary frequency were reported in 8% and 6%, respectively, of patients with anaplastic astrocytoma treated with TMZ ( 16 ). It is possible that a portion of these adverse events represented undiagnosed cases of diabetes insipidus. We performed an additional query of the 1545 patients treated with TMZ using the following coded diagnoses: incontinence of urine, urinary frequency, polyuria, or polydipsia. Two hundred eight patients met these search criteria. One hundred sixty-four of these patients (approximately 11% of the original cohort of 1545 patients) did not receive a prescription for desmopressin acetate or DDAVP or have clinical records that included a coded diagnosis of hypernatremia or diabetes insipidus. Although we can not confirm the presence of a urinary concentrating defect in these individuals, it is possible that a portion of these cases represent undiagnosed or mild diabetes insipidus.
We were able to successfully identify several possible cases of diabetes insipidus by searching an electronic database registry. Nonetheless, patient record analyses in the RPDR are retrospective and are limited by factors that affect data entry, such as variability in diagnostic coding or the choice of clinical descriptors by medical providers. The RPDR is also unable to conduct medication dose search queries, and therefore, the proportion of patients receiving dose-dense TMZ regimens is unclear. As such, it is difficult to quantify the true prevalence of this side effect and its relationship to the dose schedule of TMZ. MRI protocol selection represents an additional limitation in our case series. With the exception of the MRI performed during the period of active diabetes insipidus in case 2, previously described brain MRIs were not dedicated pituitary studies. It is possible that posterior pituitary bright spots would have been visible in some patients if a greater number of image slices were obtained from the sella.
To our knowledge, this case series represents the first report of central diabetes insipidus occurring in association with TMZ or any other alkylating chemotherapeutic agent. Diabetes insipidus in these patients is reversible and responds readily to vasopressin analog replacement therapy. The prevalence of TMZ-induced diabetes insipidus appears to be rare, but it may be underdiagnosed in this patient population. The recognition and treatment of diabetes insipidus in these patients can potentially improve quality of life and functional capacity.
Acknowledgments
We thank the Partners Health Care Research Patient Data Registry group for facilitating the use of their database.
This work was supported by the National Institutes of Health Grant K23DK087857 (to H.M.).
Disclosure Summary: H.M. has received investigator-initiated research support from Pfizer, Inc unrelated to the manuscript. The other authors have nothing to declare.
Abbreviations:

Provide details on what you need help with along with a budget and time limit. Questions are posted anonymously and can be made 100% private.

Studypool matches you to the best tutor to help you with your question. Our tutors are highly qualified and vetted.

Your matched tutor provides personalized help according to your question details. Payment is made only after you have completed your 1-on-1 session and are satisfied with your session.

- Homework Q&A
- Become a Tutor
All Subjects
Mathematics
Programming
Health & Medical
Engineering
Computer Science
Foreign Languages
Access over 20 million homework & study documents
Diabetes insipidus pathophysiology case study presentation.

Sign up to view the full document!

24/7 Homework Help
Stuck on a homework question? Our verified tutors can answer all questions, from basic math to advanced rocket science !

Similar Documents
working on a homework question?
Studypool is powered by Microtutoring TM
Copyright © 2024. Studypool Inc.
Studypool is not sponsored or endorsed by any college or university.
Ongoing Conversations

Access over 20 million homework documents through the notebank
Get on-demand Q&A homework help from verified tutors
Read 1000s of rich book guides covering popular titles

Sign up with Google
Sign up with Facebook
Already have an account? Login
Login with Google
Login with Facebook
Don't have an account? Sign Up
Diabetes insipidus
Jul 21, 2014
1.18k likes | 3.66k Views
Diabetes insipidus. By Bruna Corrales. Definitons. Diabetes Insipidus ≠ Diabetes M ellitus From the Greek: Diabainein -"to pass through“ From Latin: Insipidus - "having no flavor". Normal Production of ADH.
Share Presentation
- pituitary gland
- fluid intake
- cardiovascular collapse
- normal person
- medical alert card

Presentation Transcript
Diabetes insipidus By Bruna Corrales
Definitons • Diabetes Insipidus ≠ Diabetes Mellitus • From the Greek: Diabainein -"to pass through“ • From Latin: Insipidus - "having no flavor"
Normal Productionof ADH Diabetes Insipidus occurs when this precise system for regulating the kidneys' handling of fluids is disrupted.
Four typesof Diabetes Insipidus Central DI, Nephrogenic DI, Dipsogenic DI and Gestational DI.
Central DI • Most common and serious type of DI. • Results from damage to the pituitary gland. • Disrupts the normal storage and release of ADH. • Causes : different diseases as well as by head injuries, neurosurgery, or genetic disorders. • Tratment: Demopressin (synthetic antidiuretic ). • Prevented : Helmets, sit belts and other protective equipaments.
Nephrogenic DI • Results when the kidneys are unable to respond to ADH. • Cause :drugs (such as lithium) , chronic and inherited genetic disorders. • Sometimes the cause of Nephrogenic DI is never discovered. • Treatment : low-salt diet to reduce the amount of urine produced by the kidneys and diuretic called Hydrochlorothiazide (HCTZ). • Prevention: Any known way.
Dipsogenic DI • Uncommon type of DI • Results in an abnormal increase in thirst and fluid intake that suppresses ADH secretion and increases urine output. • Cause: defect in or damage to the thirst mechanism, which is located in the hypothalamus. • Treatment: no known long-term treatment. • Can’t use drugs prescribed to the other types of DI because they may decrease urine output but not the patient's thirst and fluid intake. At water intoxication can happen, reducing the concentration of sodium in the blood. It can seriously damage the patient's. • Prevention: Any known way
Gestational DI • Occurs only during pregnancy • Results when an enzyme made by the placenta destroys ADH in the mother. • Treatment: Demopressin. • Prevention: Anyknownway.
SymptomsandSigns Extreme thirst Excretion of an excessive amount of diluted urine Normal person - 2.6 quarts (about 2.5 liters) of urine Diabetes insipidus - 16 quarts (about 15 liters) of urine
Diagnoses ( testsandexams) • Laboratory examination urine. • Laboratory blood examination. • Miller-Moses, the water deprivation test. • magnetic resonance imaging (MRI) .
Prognosis Health adults : • Low rates of death • Patients usually have normal lives, as long there is water available People with other illnesses, children and the elderly : • Dehydration • High levels of sodium in the blood • Fever • Cardiovascular collapse • Eventual death Pregnant woman : • Risk of preeclampsia and other complications of pregnancy. • Should follow carefully the doctor’s recommendation.
Prognosis • Be mindful of the importance of balancing salt and water intake. • Extra precautions against dehydration in hot weather . • Treat vomiting or diarrhea promptly when traveling. • Carry a medical alert card or wear a medical alert bracelet.
- More by User
Diabetes Insipidus & ADH hypersecretion
Diabetes Insipidus & ADH hypersecretion. Dr. Abdulmoein Eid Al-Agha Assistant Professor & Consultant Pediatric Endocrinologist, King AbdulAziz University & Dr. Erfan Hospital - Jeddah. The Pituitary Gland. The pituitary composed of 2 lobes: anterior lobe “ adenohypophysis”
878 views • 27 slides
DIABETES INSIPIDUS
Dr. Abdelaziz Elamin MD, PhD, FRCPCH Professor of Child Health consultant pediatric endocrinologist Sultan Qaboos University Muscat, Oman. [email protected]. DIABETES INSIPIDUS. DIABETES INSIPIDUS.
1.06k views • 28 slides
A case of DIABETES MELLITUS WITH CENTRAL DIABETES INSIPIDUS
A case of DIABETES MELLITUS WITH CENTRAL DIABETES INSIPIDUS. Prof. DR. M.NATARAJAN MD DR.SYED BAHAVUDEEN HUSSAINI MD DNB DR. VALLI DEVI MD Presentor ; P. Muthukrishnan. 63 years male known case of type 2 diabetes presented complaints of polyuria polydipsia 7 days.
1.39k views • 31 slides
Postpartum Hypopituitarism Overt Diabetes Insipidus after Massive Postpartum Hemorrhage
. A 39-year-old lady delivered a normal term male infant weighting 3500g, about 3 hours ago without any instrument and uterine pressure. However, massive vaginal bleeding occurred one hour after this delivery. Oxytocin and methylergonovin were prescribed, but in vain. . . Massive
477 views • 36 slides
Proximal Nephron Na coupled transport systems Diabetes Mellitus, Nephrogenic glucosuria Diabetes Insipidus
What effect does the disorder have on renal glucose excretion?. Group 1: Diabetes MellitusGroup 2: Nephrogenic Glucosuria Group 3: Diabetes InsipidusWhat effect does the disorder have on renal glucose excretion? What is the underlying cause?Are there any changes in NaCl, K or water excretio
506 views • 27 slides
MEDICAL GRANDROUNDS ON DIABETES INSIPIDUS
MEDICAL GRANDROUNDS ON DIABETES INSIPIDUS. Desiree B. Yano-Simbulan, M.D. Maricel B. Peniero, M.D. November 8, 2007. LEARNING OBJECTIVES. To present a case of a 50 year old female with diabetes insipidus To provide an overview in the diagnostic approach to polyuria and diabetes insipidus
1.79k views • 59 slides
DIABETES INSIPIDUS AND ADIPSIA
DIABETES INSIPIDUS AND ADIPSIA. JONATHAN D. LEFFERT, MD SEPTEMBER 22, 2004. CASE PRESENTATION.
555 views • 20 slides
Diabetes Insipidus
Diabetes Insipidus. Ovidiu Galescu MD. Definition.
448 views • 11 slides
A novel mutation in the AVPR2 gene in a Palestinian family with nephrogenic diabetes insipidus
A novel mutation in the AVPR2 gene in a Palestinian family with nephrogenic diabetes insipidus. Abdulsalam Abu Libdeh, MD Pediatric Endocrinologist Makassed Islamic Hospital. Case presentation.
439 views • 32 slides
Chap44 Diabetes insipidus and aquaporin (ADH, aldosterone and ACTH)
Chap44 Diabetes insipidus and aquaporin (ADH, aldosterone and ACTH). B9902036 洪健睿 B9902045 許仲皓. Diabetes insipidus (DI). Frequency : uncommon, with a prevalence of 1 case per 25,000 population (as in the United States). Signs and symptoms :
602 views • 11 slides
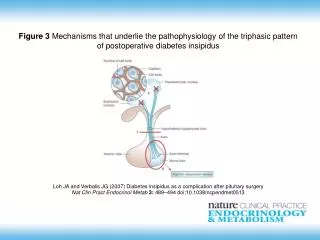
Loh JA and Verbalis JG (2007) Diabetes insipidus as a complication after pituitary surgery
Figure 3 Mechanisms that underlie the pathophysiology of the triphasic pattern of postoperative diabetes insipidus. Loh JA and Verbalis JG (2007) Diabetes insipidus as a complication after pituitary surgery Nat Clin Pract Endocrinol Metab 3: 489 – 494 doi:10.1038/ ncpendmet0513.
279 views • 1 slides
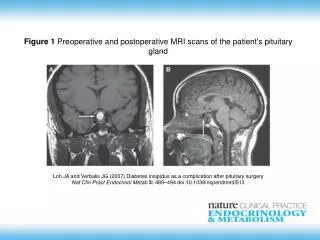
Figure 1 Preoperative and postoperative MRI scans of the patient's pituitary gland. Loh JA and Verbalis JG (2007) Diabetes insipidus as a complication after pituitary surgery Nat Clin Pract Endocrinol Metab 3: 489 – 494 doi:10.1038/ ncpendmet0513.
182 views • 1 slides
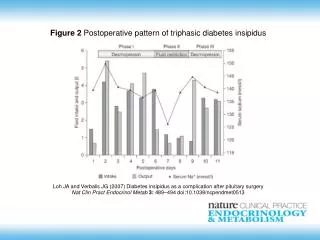
Figure 2 Postoperative pattern of triphasic diabetes insipidus. Loh JA and Verbalis JG (2007) Diabetes insipidus as a complication after pituitary surgery Nat Clin Pract Endocrinol Metab 3: 489 – 494 doi:10.1038/ ncpendmet0513.
247 views • 1 slides
Diabetes Insipidus. Endocrinology Rounds November 4, 2009 Selina Liu PGY4 Endocrinology. Objectives. To understand and describe the pathophysiology of diabetes insipidus To be able to diagnose and treat diabetes insipidus. Objectives. To name this statue, and its location
5.9k views • 56 slides
1 . 26 y/o female S/S: polyuria and diabetes insipidus for 2 years , weight loss (+)
1 . 26 y/o female S/S: polyuria and diabetes insipidus for 2 years , weight loss (+). Dx : germinoma. 2 . A 72-year-old female with a systemic disorder undergoes a staging brain MRI. (Breast) Metastasis to the Pineal Gland.
364 views • 22 slides
Diabetes Insipidus in Canines
Diabetes Insipidus in Canines. Lauren Liba Eric Malarney. What is Diabetes Insipidus???. A disorder of water imbalance This disorder is a completely different disease from diabetes mellitus, which is a disorder of glucose metabolism involving the hormone insulin.
797 views • 52 slides
Causes Of Nephrogenic Diabetes Insipidus (NDI)
This power point presentation describes about Causes Of Nephrogenic Diabetes Insipidus (NDI)
282 views • 12 slides

Natural Ways to Treat Diabetes Insipidus and Mellitus at Home
This power point presentation describes about natural ways to treat diabetes insipidus and mellitus at home.
190 views • 12 slides
379 views • 32 slides

IMAGES
VIDEO
COMMENTS
Causes A) Central diabetes. B) Nephrogenic. Pathophysiology A) Central diabetes. B) Nephrogenic diabetes. Signs and symptoms . Diagnostic test results . Goals of management . Treatments Replacement vasopressin. Treatment A thiazide.
CLINICAL VIGNETTE. A Spontaneous Case of Central Diabetes Insipidus. Anh Kieu, MD and Serena Wang, MD (co-first authors) Case Presentation. A 57-year-old woman presented with 2-months of dry mouth and polyuria. Symptoms developed acutely and also included dry eyes and fatigue. She had increased her water intake to 40 cups per day and noted ...
Introduction and background. Diabetes insipidus (DI) is a rare disorder, affecting roughly 1 in 25,000 people or about 0.004% of the global population [].Due to the rare occurrence in the population, the various forms of DI can be relatively neglected in medical education as well as in a research setting for improving clinical management []. ...
Case report 1: Forty-five year old female, previously healthy, was observed in April 2011 complaining of polydipsia, polyuria, nocturia and weight loss since January. Diabetes mellitus (DM) was excluded and she was admitted for study of possible diabetes insipidus. Water deprivation test was suggestive of CDI. Magnetic resonance imaging (MRI ...
View Answer. The provider orders the following: Free water flush via OG Tube - 200 mL q4h. Change IVF to D5W at 125 mL/hr. Desmopressin (DDAVP) 2 mcg IV push q 12h. Daily weight. q4h Sodium and Serum Osmolality levels. You set the tube feeding pump to administer the free water and change the IV fluids while waiting for the DDAVP from the ...
A Case of Diabetes Insipidus. by. David F. Dean. Department of Biology Spring Hill College. Case Presentation. Amanda Richards is a -year-old junior in college. She is majoring in biology and hopes someday to be a pediatrician. Beginning about a month ago, Amanda noticed that she was waking up once, sometimes twice a night, by the need to go to ...
Arginine vasopressin disorder is a clinical syndrome characterized by the passage of abnormally large volumes of urine (diabetes) that is dilute (hypotonic) and devoid of dissolved solutes (ie, insipid). They belong to a group of inherited or acquired disorders of polyuria and polydipsia. This is associated with insufficient arginine vasopressin (AVP), antidiuretic hormone (ADH) secretion, or ...
Results from a retrospective study in 137 patients with central diabetes insipidus showed a 27% prevalence of mild and a 15% prevalence of profound hyponatraemia. ... health-care professionals have a poor awareness of central diabetes insipidus and occasionally published case reports highlight the tragic and fatal consequences of treatment ...
Next: Physical Examination. Diabetes insipidus (DI) is defined as the passage of large volumes (>3 L/24 hr) of dilute urine (< 300 mOsm/kg). It has the following 2 major forms: Central (neurogenic, pituitary, or neurohypophyseal) DI, characterized by decreased secretion of antidiuretic hormone (ADH; also referred to as arginine vasopressin [AVP ...
Diabetes insipidus (DI) is a rare disease that causes frequent urination. The large volume of urine is diluted, mostly water. To make up for lost water, a person with DI may feel the need to drink large amounts and is likely to urinate frequently, even at night, which can disrupt sleep and, on occa sion, cause bedwetting.
Objectives. Learn about the similarities and dissimilarities between diabetes insipidus and diabetes mellitus. Understand the basic differences between the four types of diabetes insipidus. Be able to define and describe excessive thirst and urination in adults. Understand the methods by which diabetes insipidus is diagnosed and treated.
Central diabetes insipidus can be caused by the destruction or degeneration of neurons that originate in the supraoptic and paraventricular nuclei of the hypothalamus. Known causes of these lesions include tumors, local inflammatory, autoimmune or vascular diseases, trauma, and surgery, but many CDI cases are of unknown cause 1 .
We report a case of a patient with mild traumatic brain injury (TBI) who was diagnosed with permanent central diabetes insipidus (DI). A 21-year-old man was admitted to our outpatient clinic with polyuria and polydipsia 1 week after a mild head injury. He was well, except for these complaints. The initial laboratory workup was consistent with ...
Case Discussion on Central Diabetes Insipidus. A 12 year old female patient came to OPD with the chief complaints of increased thirst and increased frequency of urination for last 1 year. She drank about 10-11 liters of water everyday and passed similar amount of urine with a frequency of 10-12 episodes on daytime and 3-4 episode on night time.
Feb 17, 2018 • Download as PPTX, PDF •. 60 likes • 51,226 views. R. Ratheesh R. Diabetes Insipidus. Health & Medicine. 1 of 16. Download now. Diabetes Insipidus - Download as a PDF or view online for free.
Symptoms. Symptoms of diabetes insipidus in adults include: Being very thirsty, often with a preference for cold water. Making large amounts of pale urine. Getting up to urinate and drink water often during the night. Adults typically urinate an average of 1 to 3 quarts (about 1 to 3 liters) a day.
BACKGROUND:Diabetes insipidus (DI) is a clinical syndrome characterized by polyuria and polydipsia that result from a deficiency of antidiuretic hormone (ADH), central DI, or resistance to ADH, nephrogenic DI. In otherwise healthy patients with DI, normal thirst mechanism, and free access to water, the thirst system can maintain plasma osmolality in the near-normal range.
An in vitro study demonstrated that treatment with TMZ causes actin depolymerization in human glioma cells . Filamentous actin regulates exocytosis in the neurons of the posterior pituitary, ... With the exception of the MRI performed during the period of active diabetes insipidus in case 2, previously described brain MRIs were not dedicated ...
Unformatted Attachment Preview. Diabetes Insipidus By: Case Study James is a 21 year old male who attends college. He often binge drinks alcohol. Lately he has been feeling very thirsty and has frequent urination episodes. At first he thought it was due to his drinking habit, so he stopped drinking but the symptoms continued.
Presentation Transcript. Normal Productionof ADH Diabetes Insipidus occurs when this precise system for regulating the kidneys' handling of fluids is disrupted. Four typesof Diabetes Insipidus Central DI, Nephrogenic DI, Dipsogenic DI and Gestational DI. Central DI • Most common and serious type of DI. • Results from damage to the pituitary ...
Case study of Diabetes Insipidus Case Presentation Amanda Richards is a 20-year-old junior in college. She is majoring in biology and hopes someday to be a pediatrician. Beginning about a month ago, Amanda noticed that she was waking up once, sometimes twice a night, by the need to go to the bathroom. More recently, she has noticed that she needs to go to the bathroom during her school day ...
9. The differences between this two is that Diabetes insipidus causes kidney failure while diabetes mellitus results from insulin deficiency or resistance leading to high blood glucose. Diabetes insipidus and diabetes mellitus are unrelated, although they can have similar signs and symptoms, like excessive thirst and excessive urination ...
the present paper is to make a contribution to the scientific literature on ECD by reporting our experience with a complex clinical case report, along with a concise review of the literature. We discussed the unusual clinical presentation, the complex diagnostic process and the comparison with other published cases. Patient concerns: A 70-year-old man presented with arthralgia due to multiple ...