
- Latest news
- UCL in the media
- Services for media
- Student news
- Tell us your story


Significant rise in ADHD diagnoses in the UK
17 July 2023
Both ADHD diagnoses and prescriptions for ADHD medication have increased significantly over the past two decades, except in children under five, finds a new study by UCL researchers.

The research, published in BJPsych Open, reviewed data from 7 million individuals aged three to 99, from IQVIA Medical Research Data, a UK primary care database, between 2000 and 2018.
Of these individuals, 35,877 had an ADHD diagnosis and 18,518 received prescriptions for ADHD medication from their GP.
Although the number of individuals receiving medication for ADHD is still relatively low, the researchers found that ADHD was more commonly diagnosed in children than in adults, and was more common in boys and men than girls and women.
The findings showed that, in absolute terms, the increase was highest in children: amongst boys aged 10-16 years, 1.4% had an ADHD diagnosis and 0.6% had been prescribed ADHD medication in 2000, rising to 3.5% and 2.4% respectively in 2018.
But the relative increase was largest among adults. For example, over that time, there was approximately a twenty-fold increase in ADHD diagnoses and nearly fifty-fold in ADHD prescriptions in men between the ages of 18-29 (from 0.01% to 0.56%) .
However, there was no significant increase in children under five.
Lead author, Dr Doug McKechnie (UCL Institute of Epidemiology & Health Care), said: “ADHD diagnoses and prescriptions for ADHD medication by a GP have become more common over time.
“Whilst ADHD is most likely to be diagnosed in childhood, an increasing number of people are diagnosed for the first time in adulthood. We do not know exactly why this is happening, but it may be that ADHD has become better recognised and diagnosed.
“Over the last few years, there have been many reports of long waiting lists for ADHD assessments on the NHS, especially in adults. It’s likely that more and more people will be diagnosed with, and treated for, ADHD, so specialist services need to be made available to handle this.”
Symptoms of ADHD include impulsiveness, disorganisation, poor time management skills, difficulty focusing and restlessness. ADHD symptoms start in childhood, but are increasingly recognised to persist in adults.
The number of ADHD diagnoses were about two times higher in the most deprived areas amongst both children and adults, when compared to the least deprived areas.
Dr McKechnie added: “Many people are accessing private care for ADHD. This may create healthcare inequalities given that ADHD is more common in deprived areas. People living in deprived areas may not be able to afford private healthcare, and may suffer with undiagnosed and untreated symptoms of ADHD for longer. If people in deprived areas are struggling to get diagnosed with ADHD, our results may actually under-estimate how many people there have it, as we only counted diagnosed ADHD.”
The research also highlights how ADHD medication is now being more frequently prescribed.
In the NHS, such prescriptions start with a referral from a specialist before being handed over to GPs.
The researchers are calling for GPs to have better support in prescribing and monitoring these medications.
Dr McKechnie said: “There are already many demands on GPs’ time. We need to ensure we have the right frameworks in place to support them as rates and awareness of ADHD increase - allowing patients to receive prompt, safe and effective care.”
Dr Peter Carpenter, Chair of the Royal College of Psychiatrists’ Neurodevelopmental Special Interest Group , said: “People with ADHD can struggle with significant disruption to their personal and professional lives if the condition is left untreated. It’s good to see public awareness of the disorder has grown and that more people are coming forward for a diagnostic assessment and treatment.
“ Once someone has a diagnosis, they usually benefit from adjustments at work or in other areas of their daily lives. Medication can help treat symptoms of inattention, hyperactivity and impulsivity, particularly in those who have a moderate to severe expression of ADHD. Talking therapies and peer support groups can also be beneficial.
“NHS mental health and primary care services must be provided with the necessary resources to meet this unprecedented rise in demand for support. Only with proper funding will they be able to effectively manage growing waiting lists for assessments and provide timely and high-quality post-diagnostic care to those who need it.”
Dr McKechnie is supported by funding from the National Institute of Health and Care Research (NIHR).
Study limitations
The study only captured ADHD medication prescriptions in NHS primary care and not secondary care, which will under-estimate the overall incidence and prevalence of medication usage.
The study period finished in 2018 and since then, various events, including the Covid-19 pandemic, have had a substantial impact upon mental health services. It is therefore likely that the incidence and prevalence of ADHD in the UK has continued to change between the end of the study and the present date.
- Research in BJPsych Open
- Dr Doug McKechnie's academic profile
- UCL Institute of Epidemiology & Health
- UCL Population Health Sciences
- Credit: David Benedict on iStock
Media contact
Poppy danby .
E: p.danby [at] ucl.ac.uk
Internet Explorer is no longer supported by Microsoft. To browse the NIHR site please use a modern, secure browser like Google Chrome, Mozilla Firefox, or Microsoft Edge.

Significant rise in ADHD diagnoses in the UK

Published: 18 July 2023
The diagnoses and prescriptions for attention deficit hyperactivity disorder (ADHD) medication have increased significantly, according to a new study funded by NIHR.
The research reviewed 7 million individuals aged three to 99 between 2000 and 2018. It used data from the IQVIA Medical Research Data, a UK primary care database.
Researchers from University College London (UCL) found:
- 35,877 had an ADHD diagnosis
- 18,518 received prescriptions for ADHD medication
- a 20-fold increase in ADHD diagnoses
- a 50-fold increase in ADHD prescriptions in men aged 18-29 (from 0.01% to 0.56%)
- ADHD diagnoses were about two times higher in the most deprived areas
Findings revealed that ADHD was more commonly diagnosed in children, boys and men. However, the relative increase was largest among adults.
Amongst boys aged 10-16, 1.4% had an ADHD diagnosis and 0.6% had been prescribed ADHD medication in 2000. This had risen to 3.5% and 2.4% respectively in 2018. There was no significant increase in children under five.
Adults diagnosed with ADHD increasing
ADHD symptoms start in childhood, but are increasingly recognised in adults. Symptoms of ADHD include:
- impulsiveness
- disorganisation
- poor time management skills
- difficulty focusing
- restlessness
Lead author, Dr Doug McKechnie, UCL Institute of Epidemiology and Health Care, who is funded by an NIHR In-Practice Fellowship , said: “ADHD diagnoses and prescriptions for ADHD medication by a GP have become more common over time.
“Whilst ADHD is most likely to be diagnosed in childhood, an increasing number of people are diagnosed for the first time in adulthood. We do not know exactly why this is happening, but it may be that ADHD has become better recognised and diagnosed.”
The research highlighted how ADHD medication is more frequently prescribed. In the NHS, prescriptions start with a referral from a specialist before being handed over to GPs.
Researchers say GPs need to have better support in prescribing and monitoring these medications.
Study limitations
The study only captured ADHD medication prescriptions in NHS primary care and not secondary care. Researchers say this will under-estimate the overall incidence and prevalence of medication usage.
The study period also finished in 2018. Since then, various events, including the Covid-19 pandemic, have had a substantial impact upon mental health services. It is therefore likely that the incidence and prevalence of ADHD in the UK has continued to change between the end of the study and the present date.
Find out more about this research.
Latest news
Scientists close in on blood test to stop spread of tuberculosis
£17.9m for Advanced Therapy Treatment Centre network to bolster clinical trial infrastructure in the UK
NIHR ARCs and HINs: Collaborating to support post-pandemic NHS priorities
43 research leaders awarded prestigious NIHR Senior Investigator award
New mpox vaccine being tested in the UK
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Topic collections
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 21, Issue 4
- Twenty years of research on attention-deficit/hyperactivity disorder (ADHD): looking back, looking forward
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Samuele Cortese 1 , 2 , 3 , 4 , 5 ,
- David Coghill 6 , 7 , 8
- 1 Academic Unit of Psychology, Center for Innovation in Mental Health , University of Southampton , Southampton , UK
- 2 Clinical and Experimental Sciences (CNS and Psychiatry), Faculty of Medicine , University of Southampton , Southampton , UK
- 3 Solent NHS Trust , Southampton , UK
- 4 New York University Child Study Center , New York City , New York , USA
- 5 Division of Psychiatry and Applied Psychology, School of Medicine , University of Nottingham , Nottingham , UK
- 6 Departments of Paediatrics and Psychiatry, Faculty of Medicine, Dentistry and Health Sciences , University of Melbourne , Melbourne , Victoria , Australia
- 7 Murdoch Children’s Research Institute , Melbourne , Victoria , Australia
- 8 Royal Children’s Hospital , Melbourne , Victoria , Australia
- Correspondence to Dr Samuele Cortese, Academic Unit of Psychology and Clinical and Experimental Sciences (CNS and Psychiatry), University of Southampton, Southampton SO17 1BJ, UK; samuele.cortese{at}gmail.com
In this clinical review we summarise what in our view have been some the most important advances in the past two decades, in terms of diagnostic definition, epidemiology, genetics and environmental causes, neuroimaging/cognition and treatment of attention-deficit/hyperactivity disorder (ADHD), including: (1) the most recent changes to the diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders and International Classification of Diseases; (2) meta-analytic evidence showing that, after accounting for diagnostic methods, the rates of ADHD are fairly consistent across Western countries; (3) the recent finding of the first genome-wide significant risk loci for ADHD; (4) the paradigm shift in the pathophysiological conceptualisation of ADHD from alterations in individual brain regions to a complex dysfunction in brain networks; (5) evidence supporting the short-term efficacy of ADHD pharmacological treatments, with a different profile of efficacy and tolerability in children/adolescents versus adults; (6) a series of meta-analyses showing that, while non-pharmacological treatment may not be effective to target ADHD core symptoms, some of them effectively address ADHD-related impairments (such as oppositional behaviours for parent training and working memory deficits for cognitive training). We also discuss key priorities for future research in each of these areas of investigation. Overall, while many research questions have been answered, many others need to be addressed. Strengthening multidisciplinary collaborations, relying on large data sets in the spirit of Open Science and supporting research in less advantaged countries will be key to face the challenges ahead.
https://doi.org/10.1136/ebmental-2018-300050
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is the most common neurodevelopmental disorder in children, with an estimated worldwide prevalence around 5%. 1 Although it has for a long time been considered a childhood disorder, it is now established that impairing ADHD symptoms persist in adulthood in a sizeable portion of cases (around 65%), 2 although there is variability in the estimate due to methodological heterogeneity across studies. 3
As for other mental health conditions there has, over the past two decades, been an increasing body of research on ADHD. Reasons for this increase include: increased recognition of the impact of ADHD on functioning; advances in research methodology and technology; and interest from pharmaceutical companies.
Here, we provide an overview of what we deem have been some the most important advances, in the past two decades, in ADHD research. We also discuss key areas for future research.
Given the large body of literature and space constraints, this review is selective rather than systematic and comprehensive. We relied mostly on meta-analyses, retrieved with a search in PubMed using the following syntax/terms (update: 8 August 2018): (ADHD OR Attention Deficit OR Hyperkinetic Disorder) AND (meta-analy* OR metaanaly).
Presentation
Diagnostic definition.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), 4 published in 2013, introduced several significant changes in relation to the DSM Fourth Edition Text Revision (DSM-IV-TR) 5 criteria. First, the threshold in the number of symptoms (criterion A) necessary for the diagnosis in older adolescents and adults was reduced from 6 to 5. This change is in keeping with the notion that, despite a reduction in the number of symptoms over development, adults with ADHD in childhood can still present with impairment. 2 The required age of onset was increased from ‘prior to 7’ to ‘prior to 12’. The purpose of these changes was well intended and designed to facilitate the diagnostic process in adults, who often have trouble pinpointing the exact age of onset, especially if early in the development. Unfortunately, neither change was based on empirical evidence, and methods used for diagnostic ascertainment in adults are still under debate. 3 Another pivotal change in DSM-5 is the removal of the veto around the dual diagnosis of ADHD and autism spectrum disorders (ASD) that was present in previous editions of the DSM. Unlike the age of onset and symptom number changes this change is supported by a significant body of research (see ref 6 ). Finally, the (sub)types of ADHD defined in the DSM-IV-(TR) were replaced by the notion of different presentations. This acknowledges the instability in the phenotypic manifestation of inattention or hyperactive/impulsive symptoms over time, 7 in contrast to the more static notion of a subtype.
With regard to the International Classification of Diseases (ICD), it appears that the veto to diagnose ASD in the presence of ADHD will be retained in the upcoming ICD 11th Revision ( https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f821852937 ).
Overall, while these changes to a degree reflect recent empirical evidence and/or practical needs in the diagnostic process, there are still issues that need to be addressed. First, current criteria still focus on the number of symptoms rather than on a more precise definition of functional impairment. This should be a priority for the field and efforts, such as the development of the International Classification of Functioning, Disability and Health: Child and Youth version, are already ongoing. 8 Second, while currently each of the symptoms listed in the DSM criterion A carries the same weight, it has been argued that inattention should be more heavily weighted than hyperactivity/impulsivity. 9 Supporting evidence, which comes from clinical samples, needs to be replicated in population-based studies. Third, from a practical standpoint, it is unclear on how to best integrate different information sources (eg, parents, teachers, etc). Addressing this challenge is pivotal. Fourth, although proposed as a separate type of ADHD or even a separate diagnostic entity, the extent to which the construct of sluggish cognitive tempo (impairment of attention in hypoactive-appearing individuals) overlaps with ADHD inattentive presentation remains still unclear. 10 11 Finally, one of the most controversial topics in the entire field of ADHD research is currently around the possibility that ADHD can emerge de novo in adulthood, in contrast to its conceptualisation as a neurodevelopmental disorder. Despite an increasing number of important studies, the controversy is far from being solved 12 and we expect it will be a major focus of research in the field in coming years.
We also expect that proposed radical, although controversial, changes in the nosographic approach to mental health conditions, such as the Research Domain Criteria will significantly influence future research on ADHD. 13
Epidemiology
One of the most controversial questions in relation to the epidemiology of ADHD has been around possible differences in the prevalence of the disorder in different countries. In particular, the differential rates of clinical diagnosis in North America and Europe are cited by detractors of ADHD, as supporting the notion that ADHD is not a ‘real’ disorder but rather a social construct. 14 However, a meta-analysis published in 2007 1 found that diagnostic criteria, source of information, requirement of impairment for diagnosis and geographic origin of the studies significantly impacted on the estimated pooled rate of ADHD (5.29%). A significant difference in prevalence emerged only between North America and both Africa and the Middle East, although evidence from non-Western countries was limited. However, as there were only a limited number of studies available for Africa and Middle East, these findings should be considered with caution. By contrast, no significant differences emerged between Europe and North America, suggesting that when using the same diagnostic approach the rates of the disorder are fairly consistent in Western countries, with variability in the prevalence accounted for primarily by methods used to diagnose ADHD. Another more recent meta-analysis 15 found no evidence to support an increase in the epidemiological prevalence of ADHD over the past three decades when standardised diagnostic procedures are followed. This implies that the trend for increased rates of diagnosis 16 are not accounted for by actual increases in prevalence. Rather, the mismatch between administrative and epidemiological rates of the disorder, which varies between the USA and Europe, is likely accounted for by cultural and social factors. 16
As the bulk of the available epidemiological studies focus on school-age children from North America and Europe, further population-based studies from other continents as well as in preschoolers and adults should be encouraged. Additionally, longitudinal epidemiological studies aimed at better understanding the developmental trajectories and predictors of remission/persistence of ADHD in adulthood will be instrumental, alongside other clinical, neuropsychological, genetic and neuroimaging studies, to inform prevention programmes. Development of a standardised definition of caseness and remission will be pivotal for this body of research to be fruitful.
Genetics and environmental causes of ADHD
Studies of twins and adopted children indicate a high heritability for ADHD (60%–90%). 17 Efforts to find the genes underpinning this heritability have been more challenging than initially anticipated. As for other mental health conditions, it became clear that ADHD aetiology is accounted for by a complex interaction of many genes each with a relatively small effect and by gene × environment interactions. 18
The first approach to finding the genes involved in ADHD was the ‘candidate gene’ approach. This approach focuses on identifying the variants in genes coding for proteins hypothesised, a priori, to be involved in the pathophysiology of ADHD. These studies identified only about 10 genes as having significant support, 19 which together accounted for only a small fraction of the total ADHD heritability. The next major approach, ‘genome-wide association studies’ (GWAS), which allows the analysis of a large number of common (ie, present at greater than 5% frequency in the population) single-nucleotide polymorphisms across the entire genome, was initially unsuccessful in ADHD, as the available sample was too small to show a meaningful effect. However, in a major breakthrough, the first 12 independent loci have been recently identified through GWAS. 20 Associations were enriched in loss-of-function intolerant genes and brain-expressed regulatory marks, paving the way for a number of novel lines of investigation on the neurobiology of ADHD.
A further recently developed approach focuses on rare (ie, a frequency in the general population below 1%) ‘copy number variants’ (CNV). These are defined as replications or deletions of the DNA with a length of at least 1 kb. CNVs over-represented in ADHD have been detected, but their contribution can so far only explain 0.2% of ADHD heritability. 21
As for environmental aetiological factors, there have been, over the past years, considerable data suggesting that prenatal and postnatal factors, such as maternal smoking and alcohol use, low birth weight, premature birth and exposure to environmental toxins, such as organophosphate pesticides, polychlorinated biphenyls and zinc, are associated with increased risk for ADHD. 17 22 However, except for preterm birth, genetics studies have implicated unmeasured familial confounding factors, which are not in line with a causal role of environmental factors. 23
Severe maternal deprivation has also been related to the development of ADHD-like symptoms. 24
The study of the causes of ADHD still has many unanswered questions. We need a better understanding of how genes interact with each other, and of the interplay between environmental factors and genes. Genetics has the potential to offer many other exciting future avenues of research in ADHD. We will only mention briefly here: (1) the use of induced pluripotent stem cell derived from peripheral tissue of patients with ADHD and used to generate brain cells with the aim to model brain circuits and responses to medications or other stressors; (2) the use of zebrafish and fruit fly models to augment currently available animal models of ADHD.
Neuroimaging and neurocognition
Initial pathophysiological models of ADHD published 20 years ago 25 were based on dysfunctions in a limited number of brain areas, namely the frontal cortex and the basal ganglia. Over the past two decades, and similar to other mental health conditions, a major paradigm shift from alterations in individual brain regions to dysfunction in brain networks has begun to reshape our understanding of the pathophysiology of ADHD. Structurally, meta-analyses and mega-analyses of the structural MRI studies conducted over the past two decades pointed to consistently replicated alterations in the basal ganglia, 26 and in a number of other subcortical areas. 27 Functionally, a comprehensive meta-analysis 28 found that the majority of the ADHD-related hypoactivated areas were related to the ventral attention and the frontoparietal networks. By contrast, the majority of ADHD-related hyperactivated areas fell within the default mode network and other hyperactivated areas were within the visual network. This is in line with the hypothesis that the attentional lapses that characterise ADHD result from an inappropriate intrusion of the default network in the activity of task-positive networks frontoparietal, ventral or dorsal attention networks, 28 according to the default network hypothesis of ADHD , 29 which has been arguably one of the most inspiring proposals in the neuroscience of ADHD over the past two decades.
While we have gained insight into the brain networks that are dysfunctional in ADHD and in the delay in cortical maturation, 30 we look forward to the next generation of neuroimaging studies which we hope will start to translate these findings into the clinical practice. The introduction of machine learning approaches, such as support vector machine, has been welcomed in the field of clinical neuroscience as a way to translate neuroscientific findings at the individual patient level, thus overcoming the main limitation of current studies that can only provide results valid at the group, rather than individual, level. 31 An increasing number of studies have used machine learning based on MRI data to validate the diagnosis of ADHD with varying degrees of success. 32 33
Neurocognitive studies have made a considerable contribution to our understanding of ADHD. In recent years, the field has moved away from linear single-cause models of ADHD towards multipathway models that emphasise the heterogeneity inherent to ADHD and provide a link between individual differences at the brain level and clinical presentation. 34 35
We believe that an interesting line of research for the future will be to combine genetics, clinical, neurocognitive and neuroimaging data to define, via machine learning approaches, response to treatment, tolerability profiles and functional trajectory of the disorder over time. This will be a crucial step towards personalised and precision approaches to treatment.
Over the past two decades, there has been a marked increase in the number of randomised controlled trials (RCT) aimed at testing the short-term efficacy and tolerability of pharmacological treatments for ADHD (both stimulant and non-stimulant medications). Most have been sponsored by Big Pharma and were designed to support the licence of the medication. In parallel, due to concerns around possible side effects of medications and lack of clarity around their long-term effects, several lines of research on non-pharmacological interventions have been developed. Recent important methodologically sound meta-analyses allow us to summarise and critically discuss this large body of evidence.
For the pharmacological interventions, a comprehensive network meta-analysis 36 of 133 double-blind RCTs demonstrated high to moderate effect sizes (in terms of efficacy) for the different medications versus placebo. Standardised mean differences (SMD) ranged from −1.02 (95% CI −1.19 to −0.85) for amphetamines to −0.56 (95% CI −0.66 to −0.45) for atomoxetine (methylphenidate: −0.78, 95% CI −0.93 to −0.62). In children/adolescents, methylphenidate was the only drug with better acceptability than placebo; in adults this was the case only for amphetamines (with no difference between placebo and other active drugs). Taking into account both efficacy and safety, evidence from this meta-analysis supported methylphenidate as preferred first-choice medication for the short-term treatment of ADHD in children/adolescents and amphetamines for adults.
As for non-pharmacological options, a comprehensive synthesis on non-pharmacological treatments for children and adolescents with ADHD has been provided in a series of meta-analyses by the European ADHD Guidelines Group (EAGG). In 2013, they published a first systematic review/meta-analysis 37 addressing the efficacy of behavioural interventions, diet interventions (restricted elimination diets, artificial food colour exclusions and free fatty acid supplementation), cognitive training and neurofeedback on ADHD core symptoms (ie, inattention, hyperactivity and impulsivity). The systematic review included only RCTs and considered two contrasting outcomes: those rated by individuals not blinded to the treatment condition (active vs control) and those rated by individuals who were probably blinded to treatment (eg, teachers in trials assessing a behavioural intervention implemented with parents). The results were strikingly different depending on the type rater. When considering not blinded ratings, all interventions resulted significantly more efficacious than the control condition in terms of reduction of ADHD core symptoms. However, when considering the more rigorous probably blinded ratings, only free fatty acid supplementation and artificial food colour exclusion remained significantly more efficacious than the control conditions, with small effect sizes (SMD=0.16 and 0.42, respectively), indicating that the clinical impact of these treatments on ADHD core symptoms is, at the group level, modest.
Subsequent EAGG meta-analyses focused on ADHD core symptoms and on ADHD-related problems. A meta-analysis 38 specifically focusing on behavioural interventions showed that, even when considering probably blinded ratings, the behavioural interventions were efficacious at improving important aspects related to ADHD, namely parenting (SMD for positive parenting 0.63; SMD for negative parenting 0.43) and conduct problems (SMD 0.31). Another updated meta-analysis 39 on cognitive training, which was found efficacious in improving verbal and visual working memory, which are impaired in a sizeable portion of children with ADHD and have been demonstrated to dissociate from ADHD symptoms. 40 These meta-analyses also suggest that training which targets several neuropsychological aspects may be more efficacious at improving ADHD symptoms, than training targeting only one aspect of cognitive functioning. The most recent meta-analysis 41 by the EAGG on neurofeedback did not provide support for the efficacy of neurofeedback on any of the neuropsychological and academic outcomes. Overall, this body of research does not provide solid evidence to routinely recommend non-pharmacological interventions as highly effective treatments for ADHD core symptoms, although some of them (eg, behavioural interventions or cognitive training) may be effective for important associated impairments (oppositional behaviours and working memory deficits, respectively). The role of fatty acid supplementation and artificial food colours exclusion as possible treatment strategies should be considered cautiously given the small effect size, with CIs close to non-significance.
Probably, the most crucial area of future treatment research in ADHD will be to gain insight into the long-term positive and negative effects of treatments, using randomised trials with withdrawn designs, as well as additional population-based studies with self-controlled methodologies and longitudinal follow-up studies. These should clarify the conclusions from the various follow-up waves of the Multimodal Treatment of ADHD (MTA) study, showing that neither the type and intensity of treatment received during the initial 15-month randomised phase of the study (treatment as usual medication (MED), behavioural therapy (BEH), medication plus behavioural therapy (COMB)) nor exposure to medication over the subsequent observational periods predicted the functional outcome at follow-up which has now extended to 16 years. Of note, in the MTA, the treatments received in the three experimental arms (MED, BEH, COMB) during initial 15-month randomised phase were carefully crafted in an attempt to achieve optimal outcomes. After this initial phase all participants were free to choose the type of treatment they received from their regular provider. As it is likely that these treatments were not as carefully optimised and monitored as the three experimental groups during the randomised phase, these longer term findings of the MTA are not easily interpretable and might be, to some extent, misleading.
Conclusions
Many questions have been successfully answered in the field of ADHD. Many others remain to be addressed. Additional multidisciplinary collaborations, use of large data sets in the spirit of Open Science and support of research activities in less advantaged countries are key to address the challenge.
- Polanczyk G ,
- de Lima MS ,
- Horta BL , et al
- Faraone SV ,
- Biederman J ,
- Sibley MH ,
- Mitchell JT ,
- 4. ↵ American Psychiatric Association . Diagnostic and statistical manual of mental disorders, DSM-5 . Fifth edn . American Psychiatric Publishing , 2013 .
- 5. ↵ American Psychiatric Association . Diagnostic and statistical manual of mental disorders . Fourth edn : American Psychiatric Publishing , 2000 .
- Visser JC ,
- Rommelse NN ,
- Greven CU , et al
- Willcutt EG ,
- Pennington BF , et al
- Coghill D , et al
- Sokolova E ,
- Claassen T , et al
- Becker SP ,
- Leopold DR ,
- Burns GL , et al
- Agnew-Blais J ,
- Arseneault L
- Peterson BS
- Sergeant J ,
- Gillberg C , et al
- Polanczyk GV ,
- Salum GA , et al
- Daley D , et al
- Asherson P ,
- Banaschewski T , et al
- Cummins TD ,
- Tong J , et al
- 20. ↵ Discovery Of The First Genome-Wide Significant Risk Loci For ADHD . https://www.biorxiv.org/content/early/2017/06/03/145581
- Hohmann S ,
- Lahey BB , et al
- Sciberras E ,
- Mulraney M ,
- Silva D , et al
- Stevens SE ,
- Sonuga-Barke EJ ,
- Kreppner JM , et al
- Castellanos FX
- Rubia K , et al
- Hoogman M ,
- Bralten J ,
- Hibar DP , et al
- Cortese S ,
- Chabernaud C , et al
- Eckstrand K ,
- Sharp W , et al
- Pettersson-Yeo W ,
- Marquand AF , et al
- Johnston BA ,
- Matthews K , et al
- Coghill DR ,
- Del Giovane C , et al
- Brandeis D ,
- Cortese S , et al
- van der Oord S ,
- Ferrin M , et al
- Brandeis D , et al
- Rhodes SM ,
Contributors SC drafted the paper. DC revised the first draft.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests SC declares reimbursement for travel and accommodation expenses from the Association for Child and Adolescent Central Health (ACAMH) in relation to lectures delivered for ACAMH, and from Healthcare Convention for educational activity on ADHD. DC declares grants and personal fees from Shire and Servier; personal fees from Eli Lilly, Novartis and Oxford University Press; and grants from Vifor.
Patient consent Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
- Open access
- Published: 22 April 2022
University students with attention deficit hyperactivity disorder (ADHD): a consensus statement from the UK Adult ADHD Network (UKAAN)
- Jane A. Sedgwick-Müller 1 ,
- Ulrich Müller-Sedgwick 2 ,
- Marios Adamou 3 ,
- Marco Catani 4 ,
- Rebecca Champ 3 ,
- Gísli Gudjónsson 5 ,
- Dietmar Hank 6 ,
- Mark Pitts 7 ,
- Susan Young 8 &
- Philip Asherson 9
BMC Psychiatry volume 22 , Article number: 292 ( 2022 ) Cite this article
40k Accesses
10 Citations
65 Altmetric
Metrics details
Attention deficit hyperactivity disorder (ADHD) is associated with poor educational outcomes that can have long-term negative effects on the mental health, wellbeing, and socio-economic outcomes of university students. Mental health provision for university students with ADHD is often inadequate due to long waiting times for access to diagnosis and treatment in specialist National Health Service (NHS) clinics. ADHD is a hidden and marginalised disability, and within higher education in the UK, the categorisation of ADHD as a specific learning difference (or difficulty) may be contributing to this.
This consensus aims to provide an informed understanding of the impact of ADHD on the educational (or academic) outcomes of university students and highlight an urgent need for timely access to treatment and management.
The UK Adult ADHD Network (UKAAN) convened a meeting of practitioners and experts from England, Wales, and Scotland, to discuss issues that university students with ADHD can experience or present with during their programme of studies and how best to address them. A report on the collective analysis, evaluation, and opinions of the expert panel and published literature about the impact of ADHD on the educational outcomes of university students is presented.
A consensus was reached that offers expert advice, practical guidance, and recommendations to support the medical, education, and disability practitioners working with university students with ADHD.
Conclusions
Practical advice, guidance, and recommendations based on expert consensus can inform the identification of ADHD in university students, personalised interventions, and educational support, as well as contribute to existing research in this topic area. There is a need to move away from prevailing notions within higher education about ADHD being a specific learning difference (or difficulty) and attend to the urgent need for university students with ADHD to have timely access to treatment and support. A multimodal approach can be adapted to support university students with ADHD. This approach would view timely access to treatment, including reasonable adjustments and educational support, as having a positive impact on the academic performance and achievement of university students with ADHD.
Peer Review reports
Going to university can be an exciting experience, but it is also a daunting and stressful experience for new and returning students. The pressure to do well academically and cope with an array of lifestyle changes, can impact on the mental health and wellbeing of university students, especially students with ADHD who are transitioning from adolescence into adulthood [ 1 ]. This transitional phase defines a critical developmental stage in life termed “emerging adulthood” [ 2 ]. Institutions of higher education (HEIs or universities) are arguably designed for the kind of identity exploration that defines emerging adulthood. This includes leaving home to go to university, and perhaps for the first time, being independent and responsible for managing one’s own finances and dietary needs, whilst at the same time being exposed to a multitude of different worldviews and new opportunities for friendships, romances, partying and work [ 3 ]. Emerging adulthood is also recognised as a peak period for experimentation with substance use or high-risk sexual and other behaviours, and for the onset or exacerbation of mental health problems including self-harm and suicide [ 4 ]. The mental health and wellbeing of university students is a cause for concern [ 1 , 5 ], and the experience of the expert group is that emerging adults with ADHD may be particularly vulnerable during and after transitioning to university.
ADHD is a neurodevelopmental disorder that begins in childhood and frequently persists into adulthood. ADHD is clinically defined by persisting symptoms of inattention, hyperactivity and impulsivity that can cause functional impairments in multiple domains of daily life. In the Diagnostic and Statistical Manual version 5 (DSM-5) [ 6 ], and the International Classification of Diseases version 11 (ICD-11) [ 7 ], diagnostic requirements for ADHD are broadly similar. For this reason, and since the ICD-11 officially comes into effect in January 2022, in this report, reference is made to DSM-5 diagnostic requirements for ADHD in adults. Table 1 lists some typical characteristics and behaviours seen in adults with ADHD, including university students. It is also not uncommon for university students with ADHD to present with co-occurring specific learning differences (or difficulties) (SpLDs), developmental co-ordination disorder (DCD) or dyspraxia as the former term, autism spectrum disorder (ASD), anxiety, depression, personality, eating, and substance use disorders [ 8 , 9 , 10 , 11 , 12 , 13 , 14 ]. A significant majority of university students with ADHD will experience academic difficulties to varying degrees of severity [ 15 , 16 ]. Previous studies refer to “educational or academic outcomes” in terms of academic achievement ( attainment of information and skills learnt, grades obtained on continuous assessments such as standardised examinations or coursework ) and academic performance ( completed years of schooling, enrolment into university, final grades awarded, retention, and progression ) [ 17 ]. Evidence suggests ADHD will impact on these different academic domains in a negative way [ 18 ].
Historical context
The historical context matters a lot for understanding the ways in which ADHD exists in society, including how it is perceived, experienced, and managed. Within UK HEIs, ADHD is perceived and/or conceptualised as a SpLD [ 22 ]. In the special educational needs and disability (SEND) code of practice (0 to 25 years), ADHD is conceptualised as a social, emotional, and mental health difficulty [ 23 ], and in the DSM-5 and ICD-11, ADHD is defined as “ the most common mental health disorder in childhood that often persists in adulthood ” [ 6 , 7 ]. These conceptual differences reflect how the nomenclature, understanding of functional impairments, and clinical characteristics of ADHD within different professional contexts have evolved over time. However for some authors, it was the inception of compulsory education in the late nineteenth century, rather than advances in the medical sciences, that transformed ADHD into a salient societal concern [ 24 ]. In the UK, when compulsory education was first instituted, government funding to schools including salaries for teachers, was based on the numbers of students that attended school for at least 100 days per academic year and passed standardised examinations in the 3Rs (reading, writing, arithmetic) [ 25 ]. This system, known at the time as “payment by results” [ 26 ], is said to have also motivated teachers to raise concerns about students who struggled to pass the 3Rs examinations, and eventually these students were deemed uneducable in mainstream schools [ 27 , 28 ]. Some of these students were described as “… hyperactive, distractible, unruly and unmanageable in school … frequently disturbing the whole class … quarrelsome and impulsive … often leaving the school building during class time without permission ” [ 29 ], p.15).
The Egerton Royal Commission [ 30 ], was first to examine the problem of uneducable students in mainstream schools. In its final report the umbrella term “feeble-minded”, although pejorative today, was introduced to categorise students assessed and certified as needing special education. Arguably, feeble-mindedness is the antecedent for a variety of social, emotional, mental and physical health difficulties that can cause learning problems for a sub-set of students. The early use of the term in education also marked the medicalisation of poor scholastic performance and failure [ 31 ]. Although Still’s observation of a “ moral defect without intellectual impairment ” in school children [ 32 ], was heralded as an early descriptor of the contemporary medical concept of ADHD [ 33 ], the term feeble-minded categorised all “ children who could not be properly taught in ordinary elementary schools by ordinary methods, ” and this included the children who Still had described [ 34 ]. In the early twentieth century, new research on the heritability of intelligence roused a relentless eugenic enterprise to eradicate feeble-mindedness by preventing its procreation [ 35 ]. These events coincided with the development of psychometric tests of intelligence [ 36 , 37 , 38 ], and their use within education became the means by which students were differentiated as either feeble-minded or “simply dull/backward”. The former group of students were sent to newly established residential colonies for care and management under the Mental Deficiency Act 1913, whilst the dull/backward students continued to be educated within mainstream schools [ 39 ].
In 1913, Cyril Burt (1883–1971), the father of educational psychology in the UK, was the first psychologist to be appointed by the London County Council (LCC) to assess students referred under the Mental Deficiency Act. Burt administered psychometric tests with these students, conducted extensive ground-breaking research into educational backwardness, developed standardised tests for use in schools and provided teachers with psychological advice on how best to manage emotional and behavioural disorders in students [ 40 ]. Through his work, Burt argued that intellectual ability was on a continuum, intelligence between boys and girls was the same, academic performance and achievement was variable, and that learning differences (or difficulties) observed in students considered dull, backward, feeble-minded or maladjusted, constituted a single problem [ 41 , 42 , 43 , 44 ]. Burt’s seminal work on educational backwardness was insightful, in the sense that it not only associated causes of backwardness in students with low scores on a psychometric test or other environmental factors, but also with disorders of temperament and conduct. One category within these disorders was the “excitable and unrepressed child” [ 44 ], and descriptors of this disorder are clearly akin to the characteristics of ADHD known today. Interestingly, Burt published his work on the “backward child” in 1937, the same year that Charles Bradley in the USA reported on the positive effects of psychostimulant medication in students who exhibited various behaviour disorders [ 45 ].
The influence of Burt’s work on educational policy and provisions for students with special educational needs was profound [ 46 ]. It was reflected in the landmark Warnock Report on special education [ 47 ]. The recommendations of Warnock Report compelled legislators to enshrine the policy of inclusion within the Education Act 1981, and to introduce the broad concept of “special educational needs” (SEN) to categorise students with a range of learning difficulties and/or disabilities. Descriptors of SEN have since transformed into those listed in the current SEND code of practice (0 to 25 years) [ 23 ]. But despite all this early work, ADHD has continued to be a contentious and controversial medical diagnosis in UK, with one study reporting that only “ 73 hyperactive children were seen at the Maudsley and Bethlem Royal Hospital in London between 1968 and 1980 ” [ 48 ], p.16–17). Following the publication of a protocol for the treatment of ADHD based on DSM-IV criteria [ 49 ], diagnostic rates of ADHD increased in the UK and continued to do so with subsequent publications of clinical guidance for the diagnosis and management of ADHD in children, young people, and adults [ 50 ]. There are still many challenges with regards to timely access to diagnosis and treatment for university students with ADHD, and support for practitioners and educators who have reported ADHD as one of the most challenging disorders to deal with in university students [ 51 ]. These views echoed in the Institute for Employment Studies (IES) report on support for disabled students in higher education in England for the Office for Students (OfS) [ 52 ]. This IES report noted that “… providers [university disability services] were facing a number of, often shared, challenges ...” (p.132), which included dealing with a rising numbers of university students with ADHD and complex mental health needs. One provider quoted by the IES said that:
“… the support provisions for disabled students is understandably being affected by external factors. How to manage that impact is a focus for the disability and dyslexia team… this includes… the number of students with ADHD which has grown dramatically in recent years. This group of students are very challenging to support for both the service and for academic staff. The disability and dyslexia service need training and development to enable them to both support these students and the academic staff working with them ... ” [ 52 ] p.134).
Effects of ADHD within higher education
In the UK, across Europe and worldwide, there is a paucity of research about university students with ADHD. Previous studies mostly seem to originate from North America, where research activity in this topic area has been ongoing since the 1990s, and the impact of ADHD on the educational outcomes of college (or university) students is more widely understood. A comprehensive review of these studies was conducted by Sedgwick [ 21 ], and a summary of the main findings are presented in Table 2 .
ADHD and intellectual giftedness
The relevance of intellectual giftedness to university students with ADHD was considered by the expert group. Intellectual giftedness is another contested concept variously defined as exceptional intellectual ability, academic talent, or high-potential learners, with concurrent traits of creativity, curiosity, effort, and self-motivation [ 53 , 54 , 55 , 56 ]. Intellectual giftedness is referenced in the Canadian ADHD Practice Guidelines [ 57 ], but not in the DSM-5 or ICD-11 [ 6 , 7 ], or other clinical guidelines [ 50 ]. Research suggests that intellectual giftedness can either over-shadow or compensate for attention difficulties, or the behaviours associated with ADHD can over-shadow traits of intellectual giftedness, and that students with both ADHD and intellectual giftedness can be difficult to identify or assess using standardised measures and observational checklists [ 58 , 59 , 60 , 61 , 62 ]. The co-existence of ADHD in intellectually gifted individuals, including university students, is controversial. The theories of positive disintegration [ 63 ], and asynchronous development [ 64 ], have both been used to understand various aspects of intellectual giftedness in students with ADHD. Important areas of current research include the potential misdiagnosis of intellectual giftedness as ADHD, and the occurrence of ADHD and intellectual giftedness as a dual diagnosis [ 65 ].
Intellectual giftedness in students with ADHD is thought to be under-identified by parents, educators, psychologists, and physicians. Brown et al., for instance, reported that “ adults with IQ scores in and above superior range have often sought evaluation and treatment for chronic difficulties with organizing their work, excessive procrastination, inconsistent effort, excessive forgetfulness, and lack of adequate focus for school and/or employment. They question whether they might have an attention deficit disorder, but often they have been told by educators and clinicians that their superior intelligence precludes having ADHD ” [ 66 ], p.161).
Intellectual giftedness does not preclude having ADHD, and in some university students with ADHD it could mitigate some deficits in executive function and allow them to flourish academically or to go on and have successful careers [ 67 , 68 , 69 ]. Some authors proposed that a degree of autism (or savantism) could foster a special talent in gifted individuals [ 70 ], including individuals with ADHD [ 71 , 72 ]. Other authors warn that intellectual giftedness may only be a protective factor for students with ADHD during their pre-18 school years [ 59 , 73 ]. This may change when they transition into higher education where self-directed learning becomes an essential academic skill and when challenges such as living away from a structured home environment, or needing to be more organised, can precipitate a worsening of ADHD symptoms and significant levels of impairment start to emerge [ 74 , 75 ]. These issues may become more apparent in post-graduate students, who are selected based on their undergraduate academic achievements [ 56 , 76 , 77 ]. Empirical studies between 2000 and 2014 about the identification, misdiagnosis and dual diagnosis of intellectual giftedness and ADHD were reviewed by Mullet and Rinn, [ 65 ]. From this review, traits of intellectual giftedness versus ADHD have been compiled for the purposes of clarity. These are listed in Table 3 below.
In sum, this report presents a selective review of previously published literature on ADHD in university students and consensus based on expert opinions. It aims to critically examine and discuss the impact of ADHD on educational outcomes of university students and provide evidence-based, practical advice and guidance on how best to support these students during their programme of studies. Expert consensual advice and guidance in relation to screening and diagnostic assessments for ADHD in adults, specific interventions for university students with ADHD, a potential model for service provision, staff training and development, will contribute to existing research in this topic area.
The purpose of the expert consensus meeting was to formulate practical advice, guidance, and recommendations for supporting medical, mental health, educational and disability practitioners who work with university students with ADHD. This report is based on previously published literature that was identified, selected, collated, and critically reviewed using a framework for scoping studies [ 78 ], as well as the professional experience of the expert group. The consensus meeting was convened by the UK Adult ADHD Network ( www.UKAAN.org ) in July 2017. UKAAN is an organisation founded in 2009 by a group of mental health specialists, responding to NICE guidelines [ 50 ], and recommendations from the British Association for Psychopharmacology (BAP) [ 79 , 80 ], for the purpose of providing support, research, education, and training to professionals working with adults with ADHD. The aims of the consensus meeting were to address the following questions:
Is ADHD a hidden disability within higher education institutions (HEIs)?
Is ADHD a specific learning (difficulty) or difference?
What are the similarities and differences between ADHD, specific learning (difficulties) or differences & other mental health conditions?
What is the impact of stigma?
What constitutes best practice for supporting university students with ADHD?
Service provision
Screening & diagnostic testing
Pharmacological & non-pharmacological interventions
Staff training and development
Meeting attendees included the authors and 48 other mental health, neurodiversity, and disability practitioners, learning assessors and 2 university students with ADHD from England, Wales, and Scotland. The authors who attended the meeting represented a multidisciplinary group of prescribing and non-prescribing clinicians, practitioners, and academics, with extensive experience and expertise in working with adults with ADHD, including university students. Attendees engaged in conversations throughout the day with the aim of achieving consensus. The meeting was structured around presentations on relevant topics that are listed below, and the personal accounts from the 2 university students with ADHD, followed by questions, and answers (Q&As).
The first author facilitated discussions among the attendees to elicit verbal accounts of experience and to reach a consensus position on the topic being discussed. At the end of the meeting, the first author presented a summary of the main points previously agreed (which are listed in Table 4 ), and then asked the attendees to raise a hand to indicate whether they agreed with each point being raised. This is line with the phenomenological methodological framework that was used to gain an emic or “insiders” perspective of the attendee’s experiences, knowledge, and expertise of working with university students with ADHD [ 81 , 82 ]. The consensus meeting started with an overview of the neurobiology of ADHD to set the scene, then invited speakers presented on the following topics:
The effectiveness of stimulant medication in treating ADHD.
Academic coaching for university students with ADHD.
The SpLD Assessment Standards Committee (SASC) guidelines for the assessment of ADHD in university students.
Tele-psychiatry: Internet based treatment services for university student with ADHD.
The student experience: What is it like to be a university student with ADHD?
The attendees and speakers consented to the presentations and discussions being audio recorded. After the meeting, the recording was transcribed verbatim with care taken to remove all identifiable information. Authorship of the manuscript was based on involvement during the meeting, a willingness to work on the manuscript after the meeting, clinical and professional expertise in the assessment and treatment of ADHD in university students. The first author (JSM) consolidated the presentations, data from the transcripts and notes relevant to the main points agreed in the meeting, into a manuscript that was circulated amongst the authors for review, revision, final agreement, and approval. This manuscript reflects the clinical experience and expertise of the authors and is supported by published literature.
Results and consensus outcome
The series of questions and summary of main points addressed during the meeting were collated and are discussed below. A summary of the main recommendations is listed in Table 10 .
Only one study was found that reported on the prevalence of ADHD in UK university students. In this study Pope et al. [ 83 ] used the Conners’ Adult ADHD Self-Rating Scale to assess for symptoms of ADHD in 1185 undergraduate psychology students from four UK universities. The findings revealed that about 7% of these students self-reported above-threshold symptoms of ADHD. In a study from the USA, DuPaul et al. [ 84 ] reported that at least 25% of college students with disabilities were diagnosed with ADHD. Among university students in China ( n = 343), and in the USA ( n = 283), ADHD was reported to be around 5% in the USA cohort and 8% in the Chinese cohort [ 85 ]. These data clearly depict variability, with some reported rates suggesting a higher prevalence of ADHD among university students, when compared to the reported worldwide prevalence estimate of 2–3% for ADHD in adults [ 10 ]. However the studies that reported higher prevalence estimates (e.g., Norvilitis et al. [ 85 ] did seem to have determined the presence of ADHD based on a count of symptoms alone, and did not assess functional impairments to meet full diagnostic requirements for ADHD. Perhaps if functional impairments had also been considered, prevalence rates of ADHD in university students may have been similar to the prevalence rates reported for adults [ 86 ].
University students with ADHD are part of a much bigger group of disabled students that are represented within the widening participation (WP) strategy that forms a major component of higher education policy in the UK [ 87 ]. The WP strategy requires HEIs in the UK to collect, analyse, and respond to data on disabled students. To do so, HEIs utilise UCAS (Universities and Colleges Admissions Service), codes and categories of disability listed in Table 5 . As shown, ADHD is listed “ G – Specific Learning Difference e.g., dyslexia, dyspraxia, or ADHD .” The Higher Education Statistical Agency (HESA, https://www.hesa.ac.uk ) also collect, process, and publish data about disabled students within higher education in the UK. Figure 1 depicts percentages of the HESA Data for “ UK domiciled students’ enrolments by disability and sex” based on a total number of 307,975 for the academic years 2014/15–2018/19 [ 22 ]. From this data it is also not possible to ascertain a prevalence estimate for ADHD among university students or even to identify if ADHD exists within higher education.
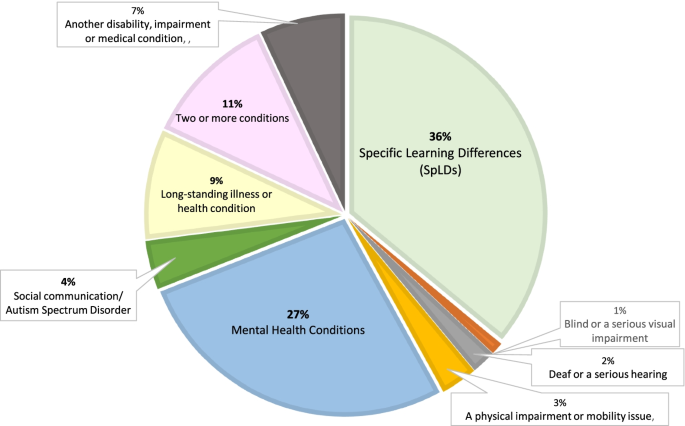
Disabled university students in the UK. Source: Table 15: UK-domiciled student enrolments by disability and sex , for the academic year 2018-19, (total number of disabled students 316,380) [ 22 ]. NB: There are high rates of overlap between ADHD and both SpLDs and mental health conditions, but the prevalence of ADHD is unknown, because there is no separate category for it
Figure 2 depicts in percentages published data from 25 HEIs in Ireland, based on a total number of 12,630 university students who declared a disability for the academic year 2016/17 [ 88 ]. There are clear similarities between this data and the HESA data depicted in Fig. 1 . But there are also differences in the numbers of university students who declared a mental health condition (27% in the UK vs. 13.9% in Ireland), a specific learning difference (UK 36% vs. Ireland 41.4%) and autism spectrum disorder/ASD (UK 4% vs. Ireland 5.4%). In Ireland, data is also collected on university students who declare a developmental co-ordination disorder (DCD, or dyspraxia, 6.1%) and ADHD (5.2%), but similar data is not collected in the UK. During the consensus meeting there was unanimous agreement that ADHD should no longer be subsumed under the category of a SpLD. The obvious consequence of continuing to do so is that a prevalence estimate for ADHD in UK university students will always be hard to ascertain.
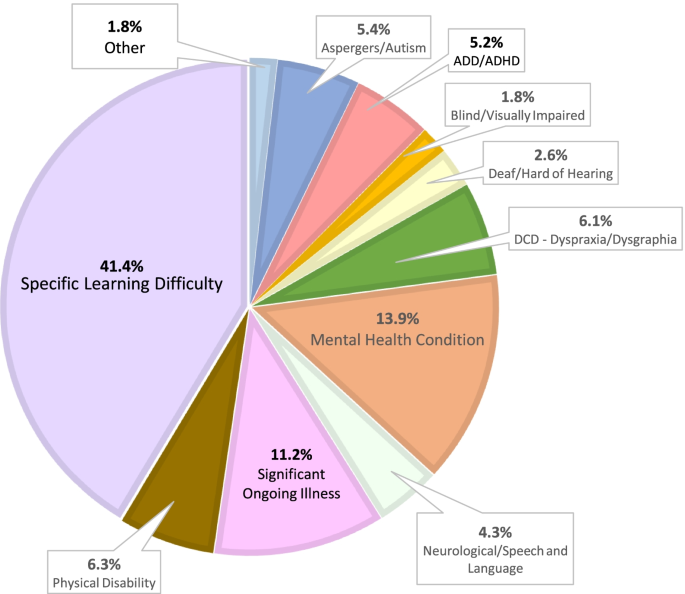
Disabled university students in Ireland. Source: Fig. 3 Breakdown of students by Category of Disability 2016/17 (total number of disabled students 12,630) [ 88 ]
Recommendation 1. The categorisation of ADHD
The expert group recommends that ADHD should no longer be subsumed under the category of a SpLD in HESA data return categories or by university services and should be coded or categorised separately. If ADHD continues to be coded or categorised as an SpLD then no specific data about the numbers of university students who declare ADHD as a disability within UK HEIs will be collected. ADHD is a mental health condition and not a SpLD. ADHD has specific diagnostic criteria within the DSM-5 [ 6 ], and ICD-11 [ 7 ], as well as efficacious treatments (medication and psychosocial interventions) [ 89 , 90 ]. A separate code to categorise ADHD within UK HEIs could result in greater recognition of the disorder and increase understanding about how it impacts on academic performance and achievement.
What are the differences between ADHD and SpLDs?
Dyslexia, dyscalculia, dysgraphia, and dyspraxia (or DCD) and ADHD are all categorised as SpLDs within UK HEIs. However, in the DSM-5, dyslexia, dyscalculia, and dysgraphia are grouped together under a single diagnostic category of “specific learning disorder” (SLD, or learning disorder), whilst DCD is classified separately as a motor disorder and ADHD as a neurodevelopmental disorder [ 6 ]. SpLDs are not synonymous with SLD, but a university student who has been diagnosed with a SLD can also expect to meet criteria for a SpLD, be registered as disabled and qualify for reasonable adjustments under the Equality Act 2010. Specifiers and characteristics of SLD and typical SpLD terms used in higher education are listed in Table 6 . Unlike ADHD, there are no known medical treatments for SLD (or SpLDs), therefore reasonable adjustments (or accommodations) are required to limit their impact within educational settings. Reading disorder (RD, e.g., dyslexia) is the most prevalent SpLD reported to account for up to 80% of all SpLDs [ 91 ]. Bidirectional comorbidity between RD and ADHD which is estimated at 25–40%, is likely due to shared genetic risk factors [ 92 ]. This may also explain why deficits in executive function are seen in both ADHD and RD [ 93 , 94 ]. Executive functions (EF) are described as a set of top-down mental skills essential for academic performance. In Table 7 , EFs are conceptualised in terms of their organisational and regulatory functions. The three commonly described EFs are inhibitory control, working memory and cognitive flexibility [ 95 , 96 ]. Although research suggests that deficits in EF can adversely impact academic functioning due to the problems they can cause with sustaining attention, forgetfulness, procrastination, organisation skills, prioritising, regulating alertness, emotional and behavioural self-control, psychometric tests of EF are still not sensitive enough to assess for the core deficits of ADHD [ 97 , 98 , 99 , 100 , 101 , 102 , 103 ].
The Baddeley and Hitch [ 107 ] conceptual model of working memory (WM) in Fig. 3 , proposes that WM is a core EF for storing and manipulating information, and with a central role in attention, allocating data to its slave systems (phonological loop and visuo-spatial sketchpad), performing task switching, mental arithmetic, problem solving and interfacing with long-term memory through the episodic buffer. The episodic buffer acts as a temporary store for the phonological loop, which processes spoken and written information, whilst the visuo-spatial sketchpad processes visual imagery. Although this model can be used to understand the importance of WM in academic tasks such as reading, comprehension, verbal reasoning (phonological loop), navigation (visuo-spatial processing) and problem-solving (central executive) [ 107 , 108 , 109 , 110 , 111 ], the model can also be used to understand how deficits in WM might occur in both ADHD and reading disorder [ 93 ]. Reading disorder (e.g., dyslexia) is defined by deficits in decoding the speech sounds of words and structure of language (phonological weakness), fluency (an inability to ready quickly with appropriate expression) and processing speed [ 11 , 91 , 93 , 102 ].
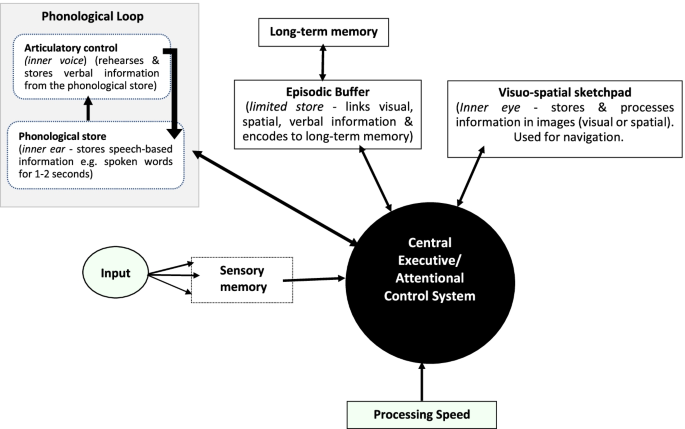
Model of Working Memory (Adapted from Baddeley [ 111 ]
Processing speed (PS) is not an EF per se, rather it is said to be a cognitive ability that describes the amount of time it takes to identify, understand, react, or respond to information received, whether it be visual (letters and numbers), auditory (language) or movement [ 112 ]. Since PS is surmised to impact on WM, phonological loop and visuo-spatial sketchpad processes, and the fine motor co-ordination associated with DCD, it’s impact on academic performance is also said to be direct [ 113 ]. PS is an index score on the WAIS (Wechsler Adult Intelligence Scale), measured by rapid automatized naming of pictured objects, letters, numbers, and colours [ 112 ]. Slow PS or PS deficits, often identified by a low PS score on the WAIS, has been associated with reading disorder [ 102 ], ASD and ADHD [ 114 ]. This also means when a student is identified with PS deficits on the WAIS for instance, certain academic tasks, such as an examination which requires “ an ability to quickly come up with an answer and retrieve information from memory ”, may take longer to complete, hence these students tend to be awarded extra writing time for examinations as a reasonable adjustment [ 115 ], p4). PS deficits are also implicated in the comorbidity between ADHD and reading disorder [ 116 ], the combined effect of which may produce more severe learning problems than when each of these disorders occurs on its own [ 11 , 117 , 118 ]. High rates of comorbidity are also reported between ADHD and other SpLDs (e.g., dyscalculia and dysgraphia), and other disorders such as DCD and ASD, with similar combined effects as those surmised between ADHD and RD, but a paucity of research limits understanding of the severity of cognitive deficits in these comorbidities and their impact on academic functioning [ 8 , 14 , 70 , 119 , 120 , 121 ].
Recommendation 2. ADHD and SpLDs
Comorbidity between ADHD and other neurodevelopment disorders, which include SpLDs, adversely impacts on academic functioning. The expert group therefore recommends screening for ADHD as part of routine practice for university students who report learning difficulties that seem to be associated with dyslexia, dyscalculia, dysgraphia, dyspraxia and/or ASD, not only because these conditions are highly likely to co-occur [ 8 , 11 , 14 ], but ADHD can be missed if a student is only screened for SpLDs and/or ASD. For students that screen positive for ADHD, a referral for treatment and management by a suitably qualified mental health professional (e.g., student health GP, psychiatrist, or mental health nurse/practitioner) is important. Although ADHD on its own can provide an explanation for learning problems within higher education, it can also add complexity to the learning problems associated with SpLDs, DCD or ASD. These complexities need to be considered when assessing for, and/or awarding reasonable adjustments. Screening tools that are used in routine practice are listed in Table 8 .
What are the differences between ADHD and other mental health conditions?
It is equally important to differentiate ADHD from other mental health conditions and to consider the impact of these conditions on university students with ADHD when they do co-occur. Year-on-year increases in the number of students declaring a mental health condition at university have been observed, with current prevalence estimates of 27% amongst university students who declare a mental health disability before or during their programme of studies (see Fig. 1 ). A study by Anastopoulos et al. [ 16 ] examined rates and patterns of co-occurring disorders in 443 university students with ADHD. The findings of this study revealed that 55% of these students had at least one comorbidity whilst 32% had two or more, and that commonly reported comorbidities with ADHD were depressive and anxiety disorders. These elevated rates differ from rates reported in an epidemiological study conducted in 20 high, medium, and low-income countries involving 26,774 adults with ADHD. This study found that 23% of these adults with ADHD had at least one mental health comorbidity, while 14% had two or three comorbidities, and that commonly reported comorbidities with ADHD were also anxiety disorders (34%), mood disorders (22%), as well as behavioural disorders (15%) and substance use disorders (11%) [ 10 ]. Similar findings were reported in qualitative studies, although the participants in these studies, also reported positive aspects of ADHD such as high levels of energy and drive, creativity, hyper-focus, agreeableness, empathy, self-acceptance, and a willingness to assist others [ 132 , 133 ].
During the consensus meeting the discussion mostly focused on university students who frequently reported anxiety and depression. Different types of anxiety (e.g., generalised anxiety disorder, social anxiety, specific phobias, agoraphobia, panic disorder, substance/medication induced anxiety ), or depressive disorders (e.g., mood dysregulation disorder, major depressive disorder, dysthymia, premenstrual dysphoria, substance/medication induced depression ), were discussed in relation to ADHD. Major depressive disorder (MDD) does show some overlap with ADHD symptoms such as poor concentration and working memory performance, but in MDD these characteristics are episodic and only arise during periods of low mood, anhedonia (loss of interest/enjoyment in ordinary experiences), or when there are ruminations dominated by negative content, and appetite disturbances, which are not characteristic of ADHD [ 134 ]. In contrast, people with ADHD usually present with attention regulation problems. This means they may be able to focus during highly stimulating or interesting tasks and activities, but problems with concentration will remain regardless of mood state [ 19 ]. Poor concentration and restlessness are also symptoms that are shared between anxiety disorders and ADHD. Anxiety disorders are characterised by fluctuations in pathologic worry, fear, and somatic symptoms, which drive concentration problems, whereas in ADHD, problems with attention and restlessness, drive concentration problems and reflect persistent traits that are independent of anxiety [ 134 ].
University students with ADHD can present to medical, counselling, and disability services with problems related to anxiety and/or depression, because challenges of university life can also play an important role in affected mental health. Both anxiety and depression are frequently co-occurring conditions in adults with ADHD [ 10 ], as well as in university students with ADHD [ 16 ]. However, it is still important to be aware that symptoms of ADHD can mimic both anxiety and depression [ 19 ], and that anxiety and depression can in turn affect attention, concentration, processing speed, and motivation, giving rise to poor performance on reading, writing, attending classes and group work [ 135 ]. University students with ADHD can also be prone to “test anxiety” and experience disabling levels of worry, emotional and somatic symptoms, that exacerbates their ability to focus and perform during evaluative assessments such as examinations. This may further increase the risk that they achieve poor grades, or delay completing their programme of studies [ 136 , 137 ]. More generally, symptoms of ADHD can be misdiagnosed for anxiety, mood, or personality disorders. This may be an issue for females with ADHD whose symptoms are more likely to reflect internalising symptoms and emotional dysregulation [ 138 ].
Emotional dysregulation is a prominent feature in ADHD and is listed in the DSM-5 as a characteristic that supports the diagnosis of ADHD [ 6 ]. Research suggests that up to 80% or more adults with ADHD report significant levels of emotional dysregulation/lability marked by irritability, volatility, a hot temper, low frustration tolerance and sensitivity to criticism [ 139 , 140 , 141 ]. These attributes do reflect a part of the normal range of mood symptoms for people with ADHD, but if severe, then they can also be misconstrued for MDD, bipolar disorder or a personality disorder. Emotional lability (EL) in adults with ADHD tends to manifest as short-lived emotional outbursts, or feelings of irritability, frustration, or anger that is often (but not always) in response to daily events [ 140 ]. Studies on EL in adults with ADHD also suggest that it is more closely linked to the development of low self-esteem and poor self-concept, when compared to the other core features of ADHD [ 140 , 142 ]. University students with ADHD who have problems with EL are more likely to encounter additional challenges with making and maintaining academic and social relationships [ 143 ], or with participating in group work, team sports, societies, or other activities at university, especially if they frequently express anger, sadness, or anxiety when with others [ 144 ].
University students with ADHD who do not cope well with anger or sadness may also use tobacco, alcohol, cannabis, or other drugs; sex, gambling, or gaming as coping strategies [ 145 , 146 , 147 ]. Some students with ADHD may not be able to control their alcohol intake for instance, and binge drink often or report more drinking-induced blackouts, loss of friends or romantic partners as a result of their drinking habits [ 147 ]. In the study by Rooney et al., [ 148 ], although students with ADHD did not report higher levels of alcohol use, they did report more dangerous/hazardous use. In another study when university students with ADHD escalated their substance use, they increasingly skipped classes and reductions in their academic grades were observed [ 149 ]. Although similar problems are seen in clinical practice with other drugs of abuse such as cocaine [ 150 ], some drugs are used to control symptoms of ADHD. For example, cannabis may help reduce some ADHD related problems such as restlessness, EL and problems getting to sleep [ 151 ]. In contrast to poor mental health, emotional wellbeing is increasingly being viewed as important for enhancing a student’s motivation to learn, academic performance and interpersonal skills. Studies have shown that reducing stress, and increasing enthusiasm, contentment, joy, hope, pride, exuberance, and elatedness are linked to improvements in academic self-efficacy, interest, effort, engagement, performance, and achievement [ 152 , 153 , 154 , 155 , 156 ]. There are also positive aspects of ADHD that can be useful at university [ 133 ].
Recommendation 3. ADHD and mental health conditions
The expert group recommends that university students who present with enduring anxiety and depression, and report persistent problems with learning or studying, should be screened for ADHD. ADHD can mimic these conditions, and likewise, anxiety and depression can mimic ADHD. Anxiety and depression may also reflect a normal stress response to the educational and psychosocial impairments of ADHD. Screening for ADHD should therefore be conducted in all students diagnosed with, or frequently complaining about, anxiety or depression (or other chronic mental health problems), particularly when they are taking medication and there is no or only limited improvements in their mental state. For students that screen positive for ADHD, a referral for treatment and management by a suitably qualified mental health professional (e.g., student health GP, psychiatrist, or mental health nurse/practitioner), is important.
What is the impact of stigma on university students with ADHD?
Stigmata are the beliefs, attitudes and structures that interact at an individual, group, or institutional level, to discriminate against a person based on a perceivable social characteristic that sets them aside from others [ 157 ]. ADHD, a diagnostic label, is a perceivable social characteristic that can be stigmatised as laziness, bad behaviour, or as having “special needs” [ 158 , 159 ]. There are lingering myths, misconceptions, negative stereotypes, and labels associated with ADHD [ 160 ]. Some medical professionals in the UK, Europe, and Australia, have expressed doubts about whether ADHD is real, over-emphasising the aetiological role of parenting, or questioning the role of stimulant medication in its treatment [ 161 ]. In one study a group of university students were asked to rate the likelihood of interacting with, collaborating on a group project with, getting to know, becoming friends with, living with, working with, or dating a peer with either ADHD, a general medical condition, or an ambiguous flaw such as perfectionism. Peers with ADHD were rated as less socially desirable than peers in the other two groups [ 162 ]. In young people with ADHD, although self-stigma can present as a sense of feeling different from same age peers or by negative self-evaluations, some young people have also challenged ADHD related stigma by openly disclosing and talking about their diagnosis [ 163 ].
Some professionals may fear treating a “fake disease” or causing a drug dependency by prescribing stimulant medication, even though there is no empirical evidence to support these views [ 50 , 158 , 164 ]. Missing or failing to identify ADHD is more likely to happen in university students who are intellectually gifted, getting good grades, or in those, particularly females, who may be misdiagnosed with anxiety, depression, eating or personality disorders [ 50 , 138 , 158 ]. Some studies from the USA suggest that university students without ADHD can malinger for the purposes of obtaining a prescription for stimulant medication for use as “study drugs” [ 165 , 166 ]. Malingering with ADHD for this purpose may be a phenomenon more often observed in the USA, where ADHD is more commonly diagnosed and treated in primary care. This is not the same as in the UK and Europe more generally, where ADHD in adults is an under-diagnosed and under-treated condition and suitably qualified and trained medical or non-medical prescribers (e.g. mental health nurses or pharmacists) treat ADHD [ 19 ]. From the perspective of the expert group, concerns about malingering can further stigmatise university students with ADHD in the UK, as well as discourage disclosure, bias the way a screening or diagnostic assessment is conducted and result in a failure to recognise a legitimate disorder with an effective treatment. The experience of the expert group is that malingering with ADHD is not common (even unusual) for university students in the UK. Instead, they tend to work exceptionally hard to overcome their deficits associated with ADHD and still experience academic outcomes that fall below that expected from their general intellectual ability. The need to tackle the stigma associated with ADHD was discussed during the consensus meeting, in terms of how it deterred disclosure, seeking a formal diagnosis, taking medication, or seeking additional support. Concerns about disclosing ADHD (or other mental health conditions) were also noted in the Institute for Employment Studies report to the Office for Students [ 52 ].
Recommendation 4. ADHD and stigma
The expert group recommends that targeted programmes of training for university student support staff should include psychoeducation, how to screen for ADHD and use recommended strategies for supporting university students with ADHD. This training can also be used to raise awareness about the potential stigma associated with ADHD, its consequences and potential impact on the screening and diagnostic process, willingness to disclose ADHD at university and accept treatment.
What is best practice for supporting university students with ADHD?
In the UK, clinical guidance recommends that the medical diagnosis of ADHD must be done by a suitably qualified practitioner, and with primary care staff providing support through shared care protocols [ 50 ]. The expert group is aware that at present, waiting times for access to treatment via specialist NHS adult ADHD clinics can be anything of up to two years or longer in some areas of the country. Given the high cost of tuition fees for university and living expenses, plus added pressures to complete a university degree on time, students with ADHD simply cannot afford to wait two or more years to access treatment in specialist NHS services, without risking poor academic performance, failure, drop-out or increased burden of illness. For some of these students the misuse of caffeine products, cannabis, alcohol, or stimulants (licit or illicit) may seem like attractive options for self-medication. Seeking an educational diagnosis of a SpLD, funded through the university disability service, maybe an attractive option that can enable access to educational support. But if the core symptoms of ADHD remain untreated, students with ADHD can continue to experience learning (and possibly other) problems during their time at university.
In one systematic review of 176 studies about the long-term educational outcomes of untreated versus treated ADHD, academic outcomes were found to be worse in students with untreated ADHD when compared to their non-ADHD peers, after controlling for IQ [ 18 ]. Another finding was that academic outcomes improved significantly when multimodal treatment was used, in comparison to when pharmacological or non-pharmacological treatments were used alone [ 18 ]. The provision of rapid access to treatment for university students with ADHD maybe challenging for clinicians working in specialist NHS services. But the expert group has found that some HEIs are using funds from their disability services budget to fund private diagnostic assessments for their students, and are commissioning medical treatment (e.g., bespoke services through the NHS or privately). These HEIs in turn note these initiatives in their “access and participation plans” (APPs) for the OfS, to demonstrate how they are improving equality of opportunity for students with ADHD, who traditionally experience poor educational access, achievement, and attainment [ 21 ].
Recommendation 5. Service provision
The expert group recommends that a rapid access pathway of care for university students with ADHD be developed collaboratively between university central support services, and NHS primary and secondary care, or private providers. University disability services currently fund diagnostic assessments for SpLDs. This budget could also be made available to university students with ADHD to enable them to at least obtain a diagnostic assessment and reasonable adjustments. The expert group provides an example of a potential support pathway for university students with ADHD, which is presented in Fig. 4 .
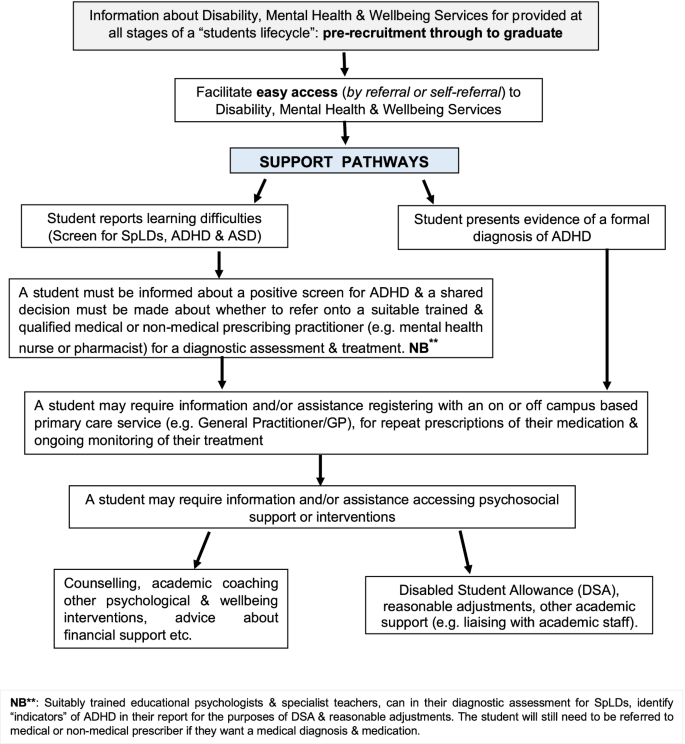
Potential Support pathway for university students with ADHD
Which screening tools and diagnostic assessments are useful?
Screening tools are used to indicate if symptoms of ADHD and/or any other co-occurring conditions that are likely to complicate the learning problems that university students with ADHD are present or not. Screening for ADHD and other potential comorbidities is done routinely in clinical practice, because it’s important to differentiate the conditions underlying the student’s presenting symptoms and consider whether they may or may not require additional reasonable adjustments or support from other services (e.g., GP, mental health, or counselling). A widely used screening tool for ADHD based on DSM-5 diagnostic criteria, is the World Health Organisation Adult ADHD Self-Report Scale (ASRSv1.1) [ 122 ], now updated to an online DSM-5 version (see Table 8 for further details and weblinks). The 18-item ASRS consists of all the diagnostic symptoms of ADHD and is useful as a screener for gathering information about ADHD symptoms that can be examined more in-depth during a diagnostic assessment. If the ASRS screener is positive for ADHD, and there are indications of sustained difficulties with attention, motor restlessness/overactivity or impulsive behaviour, then it must trigger a full diagnostic assessment by a suitably qualified practitioner.
The SpLD Assessment and Standards Committee (SASC) guidance for the assessment of ADHD, also states that “ practitioner psychologists and specialist teacher assessors who have relevant training can identify specific learning difficulties and patterns of behaviour that together would strongly suggest a student has ADHD; and in this situation they can make relevant recommendations for support at Further and or Higher Education institutions. Such diagnostic assessments should be accepted by SFE in support of an application for Disabled Students’ Allowance ” [ 167 ], p.2). This means university students can have indicators of ADHD identified as part of a SpLD diagnostic assessment and then use their diagnostic report to apply for reasonable adjustments and DSA (Disabled Student Allowance). However, even with additional educational support in place (e.g., DSA, reasonable adjustments, or sessions of study skills), ADHD can continue to impair academic functioning if it remains untreated [ 18 ]. In a few cases it can be hard to tell if ADHD with or without co-occurring learning disorders or mental health symptoms, including intellectual giftedness, are different facets of the same condition or reflect separate disorders [ 168 ]. For instance, a student with undiagnosed ADHD who keeps performing badly academically, despite studying extra hard, may start to worry excessively or feel like a failure and then become depressed. This student may seek help because they are feeling anxious or depressed, but in fact the underlying condition is ADHD.
There are effective screening tools for anxiety, depression and substance misuse that can be used with university students with ADHD. The 10-item Kessler Psychological Distress Scale (K10) can be used to screen for anxiety and depression [ 125 ], or the 16-item Penn State Worry Questionnaire (PSWQ) can be used to screen for pathological worry, which is a dominant feature in generalised anxiety disorder [ 126 ]. There are useful screening tools in the appendices of the Improving Access to Psychological Therapies (IAPT) manual, including the Generalised Anxiety Disorder scale (GAD-2, GAD-7), Panic Disorders Severity Scale (PDSS), and the Patient Health Questionnaire (PHQ-9, for depression) [ 128 ]. The Simple Screening Instrument for Substance Abuse (SSI-SA) (Center for Substance Abuse Treatment, 1994) is widely used as a brief screen by practitioners and assessors with little experience of substance misuse [ 127 ]. NICE clinical guidance [CG123] also offers very clear advice and guidance for screening common mental health disorders, and recommends that if a practitioner conducting the screen identifies a possible anxiety disorder or depression, and they are not competent to perform a full mental health assessment, then they must refer the student to an appropriate healthcare professional [ 169 ].
Some students may have additional problems related to a SpLD (e.g., dyslexia) or ASD. Useful screeners for these conditions are the Adult Dyslexia Checklist which is available for free from the British Dyslexia Association website [ 124 ], and the Autism-Spectrum Quotient (AQ-10), is also available for free download [ 123 ]. If a student with ADHD screens positive for a SpLD or ASD, then a shared decision with the student can be made about the usefulness or value of a referral for a diagnostic assessment of these comorbid conditions. It might be for example, that a positive screen of either condition and careful questioning about functional impairments, will be enough to assess their impact on studying and how best to mitigate them with additional support (e.g., counselling, specialist mentoring, academic coaching, extra writing time for examinations). There is also evidence which suggests that once the core symptoms of ADHD are treated, problems related to co-occurring SpLDs, ASD traits, anxiety or depression may in turn improve [ 9 , 158 , 170 ]. During the shared decision-making process, an agreement with the student can be also reached about whether to include results of a positive screen for a SpLD and/or ASD in their diagnostic report, which can include a write-up about the potential complexities these conditions might add to a student’s ability to study effectively. Further details and weblinks for the screening tools are provided in Table 8 .
At present there are no neuroimaging, genetic, neurochemical, or neuropsychological diagnostic tests for ADHD that are sufficiently sensitive or specific. Neuropsychological tests such as Stop Signal Reaction Time, IQ, or various computerised tests of executive functions (e.g., CANTAB) or QB-Test, can however, complement a diagnostic assessment for ADHD and provide additional information about cognitive performance [ 171 ]. Some authors (e.g., Brown [ 98 ], conceptualise ADHD as a disorder of executive function (EF), and many learning problems that university students with ADHD experience may be due to deficits in EF (e.g., poor organisation, planning and time management skills, inattention, or emotional lability) [ 172 ]. Although these EF deficits are not well reflected in cognitive performance tests [ 173 ], an assessment of EF behaviours such as those captured by the BRIEF questionnaire are strongly related to ADHD and associated functional impairments [ 174 ]. The recommendation of the expert group (and all national/international guidelines) is that a diagnostic assessment for adults with ADHD should be based on self-reported symptoms, which are best obtained by using a semi-structured in-depth diagnostic interview. An example of such a tool is the “Diagnostic Interview for Adult ADHD” (DIVA-5), which is based on the symptom and impairment criteria of the DSM-5 [ 129 ]. The ACE+ is another diagnostic tool that can be useful, and it has the option to use either DSM-5 or ICD-11 diagnostic criteria [ 130 ]. The DIVA-5 is available for a one-off fee of 10 Euro whereas the ACE+ is free to download, with digital versions in English and other languages (see Table 8 for further details and weblinks). Collateral information can also be obtained from informants such as close friends or relatives, and school records, especially for the evaluation of age of onset.
ADHD in adults is diagnosed when 5 or more symptoms of inattention and/or hyperactivity-impulsivity are present, and with several of them being present before 12 years old. These core symptoms must have persisted for at least 6 months, and in clinical practice the expectation is of a chronic trait-like course from the age of onset during childhood or early adolescence. The symptoms of ADHD should be to a degree that is inconsistent with the developmental level for that individual and must cause functional impairments in 2 or more settings (e.g., at home, university, work, with friends or relative, or in other activities) [ 6 ]. During the diagnostic process conducting a detailed evaluation of how the student’s presenting symptoms impact on their academic productivity is essential. Potential education-related impairments due to ADHD are listed in Table 9 . Individually assessing and writing about education-related problems in the student’s diagnostic report will help practitioners working in student disability services to devise personalised support, as well as allow for the effectiveness of this support to be evaluated. The Weiss Functional Impairment Rating Scale – Self Report (WFRIS-S), is a useful tool for assessing and monitoring changes in functional impairments associated with ADHD in different domains [ 131 ].
Practitioners and assessors need to be aware that ADHD symptoms and functional impairments present differently in each student and their impact can also change over the course of their programme of studies [ 19 ]. The experience of the expert group is that some students meeting diagnostic criteria for ADHD may not want to take prescribed medication in the first instance. But as their programme of studies progresses this may change, and the student may want and require medication to reduce core symptoms of the disorder. While psychoeducation, and environmental modifications (including reasonable adjustments) can help support university students with ADHD (and may be sufficient in some cases), only medication has been found to reduce core symptoms [ 89 ]. It is the experience of the expert group that university students with ADHD often have well developed compensatory strategies such as being overly organised, almost in an obsessive manner, or studying extra hard for long periods of time to ensure adequate performance. They may also have lost the usual structured support of parents and school when they were younger, so that impairments can increasingly accrue as their course develops. During diagnostic assessments, some students can find it hard to remember what their ADHD symptoms and impairments may have been like during childhood. When this happens, it is best to focus on their presenting symptoms and establish whether at least 5 or more of them are currently present and cause impairment, then track back in time to establish as far as possible an age at which current symptoms started.
In most cases of ADHD an individual is unable to identify a clear age of onset and they have the perception that the symptoms were always present. A typical response is that the symptoms have been present for as long as they can recall. Remembering symptomatic behaviours in childhood is especially hard when the student’s parents or other care givers have given them a lot of support during their academic career, or provided them with structure and routine, or when the student, had predominantly inattentive symptoms in childhood, that were not noticed either by their parents or teachers. This is more likely in females (and some men) with ADHD, who tend to present with predominantly inattentive symptoms and few hyperactive-impulsive symptoms or less disruptive behaviour [ 50 , 138 , 175 ]. The gender bias in ADHD seems to become less skewed in adulthood when women with ADHD may be diagnosed, often for the first time [ 138 ]. Practitioners and assessors conducting a diagnostic assessment need to be aware that female students can present with study related problems due to ADHD for the first time whilst at university. These students may or may not have a previous diagnosis of another mental health condition, which will need to be reviewed if they are diagnosed with ADHD [ 138 ].
During face-to-face diagnostic assessments, compensatory strategies can be minimised. For instance, the student may not recognise that sustaining attention or organisation is problematic for them, when a more objective appraisal suggests that this is a persistence problem. This can occur because symptoms of ADHD reflect lifelong traits, or because the student has well developed compensatory strategies. When this happens, it’s best to assess the degree of effort that the student needs to put into maintaining a compensatory strategy (for example, if the student did not put in extra effort to be organised then what would happen ?). Students with severe ADHD may be easier to screen and diagnostically assess, but if these students have developed good compensatory strategies (as discussed in the section on intellectual giftedness), it can be hard to determine how severe and impairing their ADHD symptoms are in other functional domains (e.g., social relationships). It may also be at a time when compensatory strategies are sufficient to mitigate ADHD related impairments, but this may not always be the case as their programme of studies progresses. Some students may present with “subthreshold symptoms” of ADHD (i.e., symptoms just below the threshold for a diagnosis of ADHD to be made), yet they appear to be significantly impaired by these symptoms and therefore need additional support, and perhaps treatment. The experience of the expert group is that impairments are also informed by co-morbidities and that several sub-threshold comorbidities (particularly of neurodevelopmental disorders) can be more impactful than a single disorder above the diagnostic threshold [ 176 ].
Recommendation 6. Screening tools and diagnostic assessments
The expert group recommends that practitioners and assessors be given training in how to screen for and diagnostically assess ADHD using robust and evidence-based rating scales, screening tools, and standardised clinical interviews. This training should include how to conduct a detailed evaluation of education related functional impairments, write up a diagnostic report with recommendations for reasonable adjustments and make a direct referral for medical treatment if requested, to a suitably qualified practitioner with expertise in the management and treatment of ADHD in adults (e.g., a psychiatrist or mental health nurse/pharmacist non-medical prescriber). A list of standardised screening and diagnostic tools are presented in Table 8 below.
What pharmacological and non-pharmacological interventions are useful?
Following initial psychoeducation about ADHD and its impact, NICE guidance [ 50 ] recommends making “environmental modifications”. In the context of university students with ADHD environmental modifications can take the form of “reasonable adjustments” to programmes of study under the Equality Act 2010. Potential learning problems associated with ADHD and potential reasonable adjustments are listed in Table 9 . Adjustments can also be made to study environments (e.g., making available a quiet study room in the library, recommend taking frequent breaks when studying, breaking down daily targets, using digital diaries and reminders, regular forms of exercise) [ 172 ]. If these adjustments/ modifications have been applied and functional impairments continue in at least one domain (e.g. academic performance, or studying/learning difficulties), then medication should be considered.
NICE guidance [ 50 ] recommends psychostimulant medication (i.e., methylphenidate or lisdexamphetamine) as first-line medical treatment for ADHD in adults. Psychostimulant medications are among the most effective medications in use within adult mental health [ 89 ], and among the most efficacious of all common medical drugs [ 177 ]. Stimulant medications often produce a substantial reduction in ADHD symptoms and associated impairments. However, stimulant medications can also have adverse effects, which in most cases are either dose-related, mild, or transient such as headache, reduced appetite, nausea, palpitations, difficulty falling asleep and dry mouth [ 89 ]. In a few cases, these adverse effects may be undesirable, and an individual may decide to stop using stimulant medication. Stimulant medications can also increase blood pressure and heart rate, therefore people who take these medications are assessed at baseline and monitored during their treatment [ 50 ]. Empirical research about the efficacy of treating university students with ADHD is rare and the extent to which prescribers consider the unique demands of university life when prescribing medication to students is unknown [ 178 ].
The first randomised controlled trial of lisdexamphetamine with a sample of 24 university students diagnosed with ADHD was conducted by DuPaul et al., [ 179 ]. In this study, lisdexamphetamine was administered over a 5-week period and large reductions in the students ADHD symptoms were observed, alongside improvements in their task management, planning, organisation, use of study skills and working memory. Although the short duration of this study precluded an assessment of academic functioning over the long-term, in other studies, university students with ADHD who took medication did report improvements in their note taking, scores on tests, writing output and completion of course work [ 180 ]. In a pharmaco-epidemiological study from Sweden young people with ADHD taking medication were also found to have better scores in standardised university entrance examinations when compared to peers with ADHD not taking medication [ 181 ]. It is noted, however, that a substantial number of university students with ADHD do not take their medication as prescribed [ 182 ]. Some university students with ADHD may use their medication flexibly, with optimum dosing during times of writing assignments or studying for examinations and then no medication on days without academic work, e.g., at weekends or during holidays [ 183 ]. When treating university students with ADHD, prescribing practitioners therefore need to be open to discussing the benefits and drawbacks of flexible dosing with students and be willing to offer appropriate guidance and advice [ 184 , 185 ].
Non-pharmacological interventions
The view of the expert group is that non-pharmacological interventions are particularly important for university students who want or need to learn how to best manage their ADHD and overcome the learning difficulties that they experience. Medication alone maybe sufficient for a subgroup of university students, but persistent difficulties are more often seen, and additional support maybe required. Non-pharmacological interventions begin with psychoeducation. The experience of the expert group is that newly diagnosed students are keen to have a conversation about their diagnosis, including whether or not to disclose it to academic staff or future employers, the benefits, and drawbacks of taking medication, including flexible dosing, “drug holidays”, effects of medication on alcohol or other drugs, the positive attributes of ADHD (e.g., creativity), psychological interventions and reasonable adjustments. Research about the effectiveness of non-pharmacological interventions for adults with ADHD is mixed and inconclusive, but positive effects have been reported for mindfulness on core symptoms of ADHD including mind wandering [ 186 ], dialectical behaviour therapy (DBT) and cognitive behavioural therapy (CBT) [ 187 , 188 , 189 ].
Although research about non-pharmacological interventions for university students with ADHD is limited, new studies have been published. For instance, Anastopoulos et al. [ 190 ] and Eddy et al. [ 191 ] reported on the findings of a randomised controlled trial (RCT) that examined the efficacy of a CBT based program called ACCESS (Accessing Campus Connections and Empowering Student Success) for university students with ADHD. During the ACCESS program - psychoeducation, cognitive and behavioural strategies targeting executive function (EF) and patterns of maladaptive thinking, were delivered. Participants, who met DSM-5 diagnostic criteria for ADHD and were taking medication, were recruited from two large public universities in the USA and randomly assigned to either the ACCESS program group ( n = 119) or a Delayed Treatment Control (DTC) group ( n = 131). The findings revealed that the ACCESS program group participants self-reported significant improvements in their knowledge of ADHD, symptoms of inattention, EF, utilisation of disability accommodations (or reasonable adjustments), as well as a moderate decline in maladaptive thinking, when compared to DTC group participants. However, neither ACCESS program and DTC group participants reported significant improvements in their interpersonal functioning and educational outcomes (grade point average/GPA and course grade completion). The authors concluded that the ACCESS program made a large difference to the participants core symptoms of ADHD and EF.
Indeed, as noted previously, EF deficits have been shown to mediate the association between ADHD and impairments in academic functioning [ 100 ]. The finding that the ACCESS program positively impacted on the participants EF is therefore encouraging. It also supports the findings of an earlier pilot study about a CBT based group intervention to enhance EF functioning in university students with ADHD [ 172 ], and strengthens a more recent finding about how steep temporal discounting may play a key role in the daily life challenges that university students with ADHD encounter. Temporal discounting (TD) describes how the subjective value of a reward significantly declines when the said reward is delayed [ 192 ]. In a pilot study by Scheres and Solanto [ 193 ], steep TD was not only associated with combined type ADHD, specifically the hyperactivity-impulsivity symptom domain, but also with poor utilisation of learning and/or study skills. TD was therefore postulated to be an important target for EF interventions for university students with or without ADHD [ 193 ], more so for interventions that were designed to activate and sustain motivation to pursue a long-term goal for a reward, such as pursuing and completing a university degree [ 194 ]. Findings like this could be useful for enhancing the effectiveness of CBT based interventions for university students with ADHD like the ACCESS program, by for example, tailoring EF interventions to also target TD. Maybe this could improve educational outcomes and perhaps interpersonal functioning of university students with ADHD, which in the study reported by Anastopoulos et al. [ 190 ] showed no significant improvements.
The report that the ACCESS program made a large difference to the students’ core symptoms of ADHD, seems to contradict what the World Federation of ADHD international consensus statement acknowledged about good treatments for ADHD being available, but even the best treatments are only partially effective [ 164 ]. Overall, there is only low-quality evidence that CBT interventions might be beneficial for treating core symptoms of ADHD in adults, in the short-term, or for improving co-occurring symptoms of anxiety and depression [ 164 , 195 ]. It was noted by Anastopoulos et al., [ 190 ], that participants in both study groups increased their use of ADHD medications over the course of the study. Perhaps this was the real reason that the participants core symptoms of ADHD improved. After all, this is what ADHD medications are designed to do and treatments for ADHD usually become more effective when medication is combined with a CBT intervention [ 195 ], or when multimodal interventions are used [ 196 ].
Hence academic coaching, which tends to be a derivative of CBT, could be another useful intervention for optimising coping strategies in university students with ADHD. For instance, coaching has been used to help identify study goals, develop study plans and strategies for achieving these plans, monitoring their progress towards attaining them and to foster self-determination [ 197 ]. In one study, academic coaches helped university students with ADHD to develop better time management, organisational skills, pay more attention in classes and to take good notes, and improvements in these skills were observed after 8 weeks [ 198 ]. In another study, university students with ADHD reported that academic coaching had helped to enhance their self-discipline, self-efficacy, study skills, ability to formulate realistic goals and to think more about long-term goals and maintain motivation to achieve them [ 199 ]. Additional benefits of coaching can be in helping university students with ADHD feel more in control of their emotions and behaviours in the face of external demands [ 200 ]. Academic coaching (or specialist mentoring, or specialist one-to-one study skills support), can also be funded via DSA as specialist access and learning facilitators (Band 4). Academic coaching, supportive counselling and/or CBT, whether delivered face-to-face or online can be effective non-pharmacological interventions for university students with ADHD [ 188 , 189 , 201 ], and the potential of these interventions to improve academic performance is evident in the promising results of recent studies e.g. [ 172 , 190 ].
Recommendation 7. Multimodal interventions
The expert group recommends multimodal interventions for university students with ADHD, that comprise a variety of interventions including environmental modifications, psychoeducation, medication, academic coaching, DBT, CBT, counselling and/or mindfulness-based interventions. University counselling and disability services do tend to offer a range of psychosocial interventions for students, whether delivered online, face-to-face or in a group.
What are the staff training and developmental needs?
In the Institute for Employment Studies report to the Office for Students, practitioners working in university disability services identified a need for training and development to enable them to both support university students with ADHD and the academic staff working with them [ 52 ]. The SpLD Assessments and Standards Committee (SASC) [ 167 ], also recommended that practitioner psychologists and specialist teacher assessors require appropriate training to identify “ specific learning difficulties and patterns of behaviour that together would strongly suggest that a student has ADHD ” (p.11). The need for staff training and development was discussed during the consensus meeting, and it included training in how to liaise with and refer university students with ADHD to a suitably qualified practitioner for a diagnostic assessment (e.g., a psychiatrist, mental health nurse/ pharmacist non-medical prescriber). Practitioners and assessors seemed keen to receive “certified training” as a way to achieve the SASC recommendations for “appropriate training”. A certified educational programme about ADHD at university level 6 or 7, could be developed and delivered for example online, as a post-qualification professional training or continuous professional development (CPD). But at present, no such course/programme exists in the UK. UKAAN offers training for healthcare professionals and can deliver bespoke training to practitioners and assessors who work with university students, and some disability services have already done so. During the consensus meeting some practitioners and assessors said they often gained relevant experience by having previously worked, or currently working, with university students with ADHD or through their own personal lived experiences, and that they made use of these experiences in their role.
Recommendation 8. Training and development
The expert group recommends that staff training, and development be prioritised under the inclusive practice agenda in higher education. This training should include psychoeducation, procedures for screening and assessing for ADHD, and useful strategies for supporting university students with ADHD. This will enhance the knowledge and skills of practitioners and assessors who work with and/or support university students with ADHD.
Discussion & conclusion
This was a report of the UKAAN expert consensus meeting about university students with ADHD, which was held before the COVID-19 pandemic. Since then, the pandemic has altered higher education in a monumental way. When lockdown was first imposed in the UK, university campuses were suddenly closed. Students and staff had to quickly adapt to online delivery of lectures and classes, and there was uncertainty about being able to access digital technologies and quite places to study or work at home. There was also confusion among students about study expectations, assessments, workloads, retention, and completion [ 202 , 203 , 204 ]. Undoubtedly the pandemic has caused much suffering, frustration, fear, loss and other negative thoughts, emotions, and experiences for many people, including university students with ADHD [ 205 ]. However, findings about the impact of the pandemic on university students has been mixed. Frampton and Smithies [ 206 ], reported on a Students Minds survey about life during the pandemic involving 1100 university students. The findings of this survey revealed that 74% of respondents reported that the pandemic had a negative impact on their mental health and wellbeing, whilst only 10% of respondents reported positive effects. In this survey, disabled and non-disabled students were also asked whether they agreed or disagreed with the statement “ online learning has allowed me to engage with my course more positively ”, and the findings revealed that 59% of disabled students compared with 55% of non-disabled students disagreed with the statement. This also suggests that just under-half of these students agreed with the statement. In another study, 79 university students in one Faculty of Life Sciences were surveyed and participated in focus groups about how they experienced the sudden shift to online learning during the lockdown [ 207 ]. This study found that 75% of the students who participated in the study, reported that their life had become more difficult and 50% reported that learning outcomes would be hard to achieve, but after 12 weeks into the lockdown, corresponding rates changed to 57 and 71% respectively [ 207 ].
The findings of existing studies do suggest that during the COVID-19 lockdown, virtual learning for some university students may have had benefits such as enabling greater attendance, engagement, and participation in teaching sessions, especially for students who previously felt anxious about asking questions in front of others or some disabled students [ 202 ]. Students who were used to spending time online – on the Internet including social media platforms for example, seemed to exhibit strong motivation for eLearning, and reported lower levels of distress during the pandemic [ 208 ]. However, there are also concerning reports about ADHD being a risk factor for COVID-19 infection [ 209 , 210 ]. These reports are perhaps pertinent for university students with ADHD who may have participated in demonstrations during the pandemic such as Black Lives Matter (BLM), living arrangements in student halls of residence, sexual harassment, assault and “rape culture” in UK universities [ 206 , 211 ], or illegal COVID raves [ 212 ], or the COVID anti-vaccine and lockdown protests [ 213 ]. It can be argued that the pandemic may have longer-term negative consequences on current and future career prospects for university students with ADHD, but outside of this, no firm conclusions from the existing research can be drawn.
Evidence is stronger for poor education (or academic) performance and achievement having a long-term negative impact on mental health, wellbeing, and socio-economic outcomes [ 214 ]. Even though there is a paucity of research about university students with ADHD in the UK and rest of Europe, the importance of attending to the mental health of university students in the UK has been recognised. The Royal College of Psychiatrists recently published a college report on the mental health of higher education students, and Sedgwick-Müller et al., contributed a section on ADHD in this report [ 1 ]. The expert group is also aware that ADHD is a hidden disability within UK HEIs and its categorisation as a SpLD may be contributing to this, therefore university students with ADHD continue to be at risk of marginalisation and disadvantage. The expert group recommends that ADHD should be catered for under a separate category within UK HEIs, as this may enable greater recognition of ADHD and for its impact on learning within higher education to be adequately assessed and mitigated. With aspirations towards widening participation and inclusive practices in higher education [ 52 ], understanding exactly “what works” best for university students with ADHD is imperative. The four key stages in a student’s lifecycle are access to higher education (the extent to which students can gain entrance to different types of HEIs), retention (the likelihood of continuing or withdrawing from a programme of studies), attainment (the extent to which university students are enabled to achieve their full academic potential) , and progression (successful transitions within a programme of studies and afterwards into employment or further study )” [ 215 ], p.5). Each of these 4 key stages in a student’s lifecycle can be adversely affected by either having and/or not recognising ADHD, and by delaying access to a screening, diagnostic assessment, treatment, and educational support. Interventions in a student’s first year at university, according to Clery and Topper, should focus on enhancing their academic achievement because retention, attainment, and progression tends to be more favourable for university students who perform well academically in their first year [ 216 ].
In summary, UKAAN convened an expert consensus meeting to provide an informed understanding about the impact of ADHD on the educational (or academic) outcomes of university students and to highlight an urgent need for timely access to treatment and management. An overview of key issues, as well as expert advice and guidance has been offered. In Table 10 below, the main recommendations of the expert group are summarised. There is little doubt that university students with ADHD are struggling with long delays in accessing a diagnostic assessment, treatment, and personalised educational support. The provision of rapid access treatment and care pathways can be challenging for clinicians working in specialist NHS ADHD clinics, but examples of good practice are also beginning to emerge, with some university disability services drawing on their own budgets to support their students. Further work is needed to develop and evaluate efficient and cost-effective treatment and care pathways for university students with ADHD (for example see Fig. 4 ), and to adopt models of best practice across the sector. University students, including those with ADHD, are at a crucial transitioning stage in life and their success at university is likely to determine their success in highly competitive employment markets. This strengthens the argument to support all university students in an inclusive manner. Methods for inclusive teaching and learning are also likely to cater to disabled students, including university students with ADHD.
Availability of data and materials
Data sharing is not applicable to this article as no data sets were generated or analysed during the study.
Abbreviations
ADHD Child Evaluation
Association for Higher Access & Disability
Attention Deficit Hyperactivity Disorder
American Psychiatric Association
Autism-Spectrum Quotient
Autism Spectrum Disorder
Adult ADHD Self-report Rating Scale
Canadian ADHD Practice Guidelines
Cognitive Behavioural Therapy
Diagnostic Interview for ADHD in adults
Dialectical Behavioural Therapy
Disabled Students Allowance
Developmental co-ordination disorder
Diagnostic and Statistical Manual of Mental Disorders version 5
Emotional lability
Executive Functions
Institutions of Higher Education
The Higher Education Statistical Authority
Improving Access to Psychological Therapies
Institute of Employment Studies
Major Depressive Disorder
Math Disability
National Health Service
National Institute for Health and Care Excellence
Office for Students
Panic Disorders Severity Scale
Patient Health Questionnaire
Processing Speed
Penn State Worry Questionnaire
Quantified Behavior Test
Reding Disability
Special Educational Needs and Disabilities
Special Educational Needs
Specific Learning Disorders
SpLD Assessment and Standards Committee
Specific learning differences
The Simple Screening Instrument for Substance Abuse
UK Adult ADHD Network
United Kingdom of Great Britain and Northern Ireland
Wechsler Adult Intelligence Scale
Weiss Functional Impairment Rating Scale – Self Report
World Health Organisation
Working Memory
Writing Disability
The Royal College of Psychiatrists: Mental Health of Higher Education Students [College Report CR23]. London.
Arnett J. Emerging adulthood: the winding road from the late teens through the twenties. New York, NY: Oxford University Press; 2014.
Book Google Scholar
Arnett J. College students as emerging adults: the developmental implications of the college context. Emerg Adulthood. 2015;4(3):219–22.
Article Google Scholar
MacLeod KB, Brownlie EB. Mental health and transitions from adolescence to emerging adulthood: developmental and diversity considerations. Can J Community Ment Health. 2014;33(1):77–86.
Universities-UK. Minding our future: starting a conversation about the support of student mental health. London; 2018.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM). 5th ed; 2013.
World Health Organisation (WHO). International classification of diseases (ICD). 11th ed. Geneva; 2019.
Czamara D, Tiesler CM, Kohlböck G, Berdel D, Hoffmann B, Bauer C-P, et al. Children with ADHD symptoms have a higher risk for reading, spelling and math difficulties in the GINIplus and LISAplus cohort studies. PLoS One. 2013;8(5):e63859.
Article CAS PubMed PubMed Central Google Scholar
Davis NO, Kollins SH. Treatment for co-occurring attention deficit/hyperactivity disorder and autism spectrum disorder. Neurotherapeutics. 2012;9(3):518–30.
Fayyad J, Sampson NA, Hwang I, Adamowski T, Aguilar-Gaxiola S, Al-Hamzawi A, et al. The descriptive epidemiology of DSM-IV adult ADHD in the World Health Organization world mental health surveys. Atten Defic Hyperact Disord. 2017;9(1):47–65.
Article PubMed Google Scholar
Germanò E, Gagliano A, Curatolo P. Comorbidity of ADHD and dyslexia. Dev Neuropsychol. 2010;35(5):475–93.
Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatr. 2006;163(4):716–23.
Wadsworth SJ, DeFries JC, Willcutt EG, Pennington BF, Olson RK. Genetic etiologies of comorbidity and stability for Reading difficulties and ADHD: a replication study. Twin Res Hum Genet. 2016;19(6):647–51.
Article PubMed PubMed Central Google Scholar
Yoshimasu K, Barbaresi WJ, Colligan RC, Killian JM, Voigt RG, Weaver AL, et al. Written-language disorder among children with and without ADHD in a population-based birth cohort. Pediatrics. 2011;128(3):e605–12.
Langberg JM, Becker SP. ADHD treatment and long-term academic outcomes: response to Arnold and Colleagues. J Atten Disord. 2015;24(5):819–20.
Anastopoulos A, DuPaul G, Weyandt L, Morrissey-Kane E, Sommer J, Rhoads L, et al. Rates and patterns of comorbidity among first-year college students with ADHD. J Clin Child Adolesc Psychol. 2018;47(2):236–47.
Langberg JM, Molina BSG, Arnold LE, Epstein JN, Altaye M, Hinshaw SP, et al. Patterns and predictors of adolescent academic achievement and performance in a sample of children with attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2011;40(4):519–31.
Arnold L, Hodgkins P, Kahle J, Madhoo M. G K: long-term outcomes of ADHD: academic achievement and performance. J Atten Disord. 2015;24(1):73–85.
Asherson P, Buitelaar J, Faraone S, Rohde L. Adult attention-deficit hyperactivity disorder: key conceptual issues. Lancet Psychiatry. 2016;3(6):568–78.
Nigg JT. Attention-deficit/hyperactivity disorder and adverse health outcomes. Clin Psychol Rev. 2013;33(2):215–28.
Sedgwick J. University students with attention deficit hyperactivity disorder (ADHD): a literature review. Ir J Psychol Med. 2018;35(3):221–35.
Article CAS PubMed Google Scholar
Higher Education Statistical Agency (HESA), UK-domiciled student enrolments by disability and sex: For the academic years 2014/15–2018/19 at: https://www.hesa.ac.uk/data-and-analysis/students/table-15 . Accessed 31 July 2021.
Department for Education Department of Health. The special educational needs and disability (SEND) code of practice 0–25 years. London: HMSO; 2015.
Google Scholar
Hinshaw S, Scheffler R. The ADHD explosion: myths, medication, money, and Today’s push for performance vol. 67. New York: Oxford University Press; 2014.
Midgley H. Payment by results in nineteenth-century British education: a study in how priorities change. J Policy Hist. 2016;28(4):680–706.
Newcastle, Duke of. [The Newcastle Commission]. Report of the Royal Commissioners appointed to inquire into the state of popular education in England, vol. 1. London: HMSO; 1861.
Potts P. Medicine, morals and mental deficiency: the contribution of doctors to the development of special education in England. Oxf Rev Educ. 1983;9(3):181–96.
Copeland IC. The establishment of models of education for disabled children. Br J Educ Stud. 1995;43(2):179–200.
Ross D, Ross S. Hyperactivity: research, theory, and action. New York: Wiley; 1976.
The Egerton Royal Commission. Report of the Royal Commission on the blind, the deaf and dumb & c., of the United Kingdom. London: HMSO; 1889.
Petrina S. The medicalization of education: a Historiographic synthesis. Hist Educ Q. 2006;46(4):503–31.
Still G. The Goulstonian lectures ON SOME ABNORMAL PSYCHICAL CONDITIONS IN CHILDREN. Lancet. 1902;159(4102):1008–13.
Lange KW, Reichl S, Lange KM, Tucha L, Tucha O. The history of attention deficit hyperactivity disorder. Atten Defic Hyperact Disord. 2010;2(4):241–55.
British Medical Journal. Report of the Departmental Committee on Defective and Epileptic Children. 1940;1898(1):651–2.
Woodhouse J. Eugenics and the feeble-minded: the parliamentary debates of 1912-14. Hist Educ. 1982;11(2):127–37.
Binet A, Simon T. Méthodes nouvelles pour diagnostiquer l'idiotie, l’imbécillité et la débilité mentale [New methods for the diagnosis of the intellectual level of abnormal children to diagnose the idiocy, the imbecility, and the mental deficiency]. Atti del V congresso internazionale di psicologia tenuto in Roma dal 26 al 30 Aprile; 1905.
Binet A, Simon T. Le développement de l'intelligence chez les enfants. L'année Psychol. 1907;14(1):1–94.
Spearman C. "general intelligence," objectively determined and measured. Am J Psychol. 1904;15(2):201.
Radnor Report. Report of the Royal Commission on the care and control of the feeble-minded, VIII, cd 4202. London: HMSO; 1908.
Hearnshaw L. Cyril Burt: psychologist. Ithaca: Cornell University Press; 1979.
Burt C. Mental and scholastic tests (London County council). London: P.S. King and Son; 1922.
Burt C. The causal factors of juvenile crime. Br J Med Psychol. 1923;3(1):9–33.
Burt C. The Young delinquent, First edn. London: University of London Press; 1925.
Burt C. The backward child. London: University of London Press; 1937.
Bradley C. The behavior of children receiving benzedrine. Am J Psychiatr. 1937;94(3):577–85.
Lindsay G, Miller A. Psychological Services for Primary Schools. Harlow, Essex: UK; 1991.
Warnock H. Warnock Report of the Committee of Enquiry into the education of handicapped children and Young people. London; 1978.
Thorley G. Hyperkinetic syndrome of childhood: clinical characteristics. Br J Psychiatry. 1984;144(1):16–24.
Hill P, Taylor E. An auditable protocol for treating attention deficit/hyperactivity disorder. Arch Dis Child. 2001;84(5):404–9.
NICE (National Institute for Health and Care Excellence). Attention deficit hyperactivity disorder: diagnosis and management, vol. 2018. London; 2008.
Ewe LP. ADHD symptoms and the teacher–student relationship: a systematic literature review. Emot Behav Diffic. 2019;24(2):136–55.
Williams M, Pollard E, Takala H, Houghton A-M. Review of Support for Disabled Students in Higher Education in England. Brighton: Office for Students; 2019.
Reis SM, Renzulli JS. Intellectual Giftedness. In: Stenberg RJ, editor. The Cambridge Handbook of Intelligence: Cambridge University Press; 2020. p. 291–316.
Sternberg RJ. The Augmented Theory of Successful Intelligence. In: Sternberg RJ, editor. The Cambridge Handbook of Intelligence: Cambridge University Press; 2020. p. 679–708.
Sternberg R, Davidson J. Conceptions of giftedness, vol. 2005. Cambridge: Cambridge University Press; 1986.
von Stumm S, Hell B, Chamorro-Premuzic T. The hungry mind. Perspect Psychol Sci. 2011;6(6):574–88.
Canadian ADHD. Resource Alliance (CADDRA): Canadian ADHD practice guidelines., 4th edn. Canada.
Antshel K, Faraone S, Stallone K, Nave A, Kaufmann F, Doyle A, et al. Is attention deficit hyperactivity disorder a valid diagnosis in the presence of high IQ? Results from the MGH longitudinal family studies of ADHD. J Child Psychol Psychiatry. 2007;48(7):687–94.
Antshel K. Attention-deficit hyperactivity disorder in the context of a high intellectual quotient/giftedness. Dev Disabil Res Rev. 2008;14(4):293–9.
Barkley R, Poillion M. Attention deficit hyperactivity disorder: a handbook for diagnosis and treatment. New York: The Guildford Press; 1990.
Beljan P, Webb J, Amend E, Web N, Goerss J, Olenchak F. Misdiagnosis and dual diagnoses of gifted children and adults: ADHD, bipolar, OCD, Asperger’s, depression, and other disorders. Gifted Talented Int. 2006;21(2):83–6.
Rinn AN, Reynolds MJ. Overexcitabilities and ADHD in the gifted: an examination. Roeper Rev. 2012;34(1):38–45.
Dabrowski K. Positive Disintegration. Boston: Little, Brown; 1964.
Silverman LK. The construct of asynchronous development. Peabody J Educ. 1997;72(3):36–58.
Mullet DR, Rinn AN. Giftedness and ADHD: identification, misdiagnosis, and dual diagnosis. Roeper Rev. 2015;37(4):195–207.
Brown T, Reichel P, Quinlan D. Executive function impairments in high IQ adults with ADHD. J Atten Disord. 2009;13(2):161–7.
Minahim D, Rohde LA. Attention deficit hyperactivity disorder and intellectual giftedness: a study of symptom frequency and minor physical anomalies. Rev Bras Psiquiatr. 2015;37(4):289–95.
Milioni ALV, Chaim TM, Cavallet M, de Oliveira NM, Annes M, dos Santos B, et al. High IQ may “mask” the diagnosis of ADHD by compensating for deficits in executive functions in treatment-Naïve adults with ADHD. J Atten Disord. 2016;21(6):455–64.
Gomez R, Stavropoulos V, Vance A, Griffiths MD. Gifted children with ADHD: how are they different from non-gifted children with ADHD? Int J Ment Heal Addict. 2019;18(6):1467–81.
Baron-Cohen S, Ashwin E, Ashwin C, Tavassoli T, Chakrabrati B. Talent in autism: hyper-systemizing, hyper-attention to detail and sensory hypersensitivity. Philos Trans R Soc Lond Ser B Biol Sci. 2009;364(1522):1377–83.
Ruthsatz J, Urbach JB. Child prodigy: a novel cognitive profile places elevated general intelligence, exceptional working memory and attention to detail at the root of prodigiousness. Intelligence. 2012;40(5):419–26.
Lee KM, Olenchak FR. Individuals with a gifted/attention deficit/hyperactivity disorder diagnosis. Gift Educ Int. 2014;31(3):185–99.
Antshel K, Faraone S, Maglione K, Doyle A, Fried R, Seidman L, et al. Executive functioning in high-IQ adults with ADHD. Psychol Med. 2010;40(11):1909–18.
Rommelse N, Antshel K, Smeets S, Greven C, Hoogeveen L, Faraone SV, et al. High intelligence and the risk of ADHD and other psychopathology. Br J Psychiatry. 2017;211(6):359–64.
Young S, Adamou M, Asherson P, Coghill D, Colley B, Gudjonsson G, et al. Recommendations for the transition of patients with ADHD from child to adult healthcare services: a consensus statement from the UK adult ADHD network. BMC Psychiatry. 2016;16(1):301.
Jensen M. Personality traits, learning and academic achievements. J Educ Learn. 2015;4(4):91.
Rimfeld K, Ayorech Z, Dale PS, Kovas Y, Plomin R. Genetics affects choice of academic subjects as well as achievement. Sci Rep. 2016;6:26373.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Nutt DJ, Fone K, Asherson P, Bramble D, Hill P, Matthews K, et al. Evidence-based guidelines for management of attention-deficit/hyperactivity disorder in adolescents in transition to adult services and in adults: recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2006;21(1):10–41.
Bolea-Alamañac B, Nutt DJ, Adamou M, Asherson P, Bazire S, Coghill D, et al. Evidence-based guidelines for the pharmacological management of attention deficit hyperactivity disorder: update on recommendations from the British Association for Psychopharmacology. J Psychopharmacol (Oxford, England). 2014;28(3):179–203.
Husserl E. Ideas pertaining to a pure phenomenology and to a phenomenological philosophy. Netherlands: Springer; 1982.
Giorgi A. The theory, practice, and evaluation of the phenomenological method as a qualitative research procedure. J Phenomenol Psychol. 1997;28(2):235–60.
Pope D, Whiteley H, Smith C, Lever R, Wakelin D, Dudiak H, et al. Relationships between ADHD and dyslexia screening scores and academic performance in undergraduate psychology students: implications for teaching, learning and assessment. Psychol Learn Teach. 2007;6(2):114–20.
DuPaul GJ, Weyandt LL, O'Dell SM, Varejao M. College students with ADHD: current status and future directions. J Atten Disord. 2009;13(3):234–50.
Norvilitis JM, Ingersoll T, Jie Z, Shuhua J. Self-reported symptoms of ADHD among college students in China and the United States. J Atten Disord. 2007;11(5):558–67.
Du Rietz E, Cheung CHM, McLoughlin G, Brandeis D, Banaschewski T, Asherson P, et al. Self-report of ADHD shows limited agreement with objective markers of persistence and remittance. J Psychiatr Res. 2016;82:91–9.
Connell-Smith A, Hubble S. Widening participation strategy in higher education in England. London: House of Commons Library; 2018.
Association for Higher Education Access and Disability (AHEAD). Numbers of Students with Disabilities Studying in Higher Education in Ireland 2017/18. Dublin: AHEAD Educational Press; 2019.
Cortese S, Adamo N, Del Giovane C, Mohr-Jensen C, Hayes AJ, Carucci S, et al. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis. Lancet Psychiatry. 2018;5(9):727–38.
Fullen T, Jones SL, Emerson LM, Adamou M. Psychological treatments in adult ADHD: a systematic review. J Psychopathol Behav Assess. 2020;42(3):500–18.
Snowling MJ, Hulme C. Annual research review: the nature and classification of reading disorders--a commentary on proposals for DSM-5. J Child Psychol Psychiatry. 2012;53(5):593–607.
Gialluisi A, Andlauer TFM, Mirza-Schreiber N, Moll K, Hoffmann P, Ludwig KU, et al. Genome wide association scan identifies new variants associated with a cognitive predictor of dyslexia. Transl Psychiatry. 2018;9(77):1–15.
Dighe A, Kettles G. Developmental dyspraxia an overview. In: Reid G, editor. Dimensions of Dsylexia: assessment, teaching and the curriculum, vol. 2. Edinburgh, Scotland: Moray House School of Education; 1996.
Hosenbocus S, Chahal R. A review of executive function deficits and pharmacological management in children and adolescents. J Can Acad Child Adolesc Psychiatry. 2012;21(3):223–9.
PubMed PubMed Central Google Scholar
Diamond A. Executive functions. Annu Rev Psychol. 2013;64:135–68.
Friedman NP, Miyake A. Unity and diversity of executive functions: individual differences as a window on cognitive structure. Cortex. 2017;86:186–204.
Barkley R. Differential diagnosis of adults with ADHD: the role of executive function and self-regulation. J Clin Psychiatry. 2010;71(07):e17.
Brown T. Executive functions and attention deficit hyperactivity disorder: implications of two conflicting views. Int J Disabil Dev Educ. 2006;53(1):35–46.
Brown T. ADD/ADHD and impaired executive function in clinical practice. Curr Psychiatry Rep. 2008;10(5):407–11.
Dvorsky MR, Langberg JM. Predicting impairment in college students with ADHD: the role of executive functions. J Atten Disord. 2014;23(13):1624–36.
Hervey AS, Epstein JN, Curry JF. Neuropsychology of adults with attention-deficit/hyperactivity disorder: a Meta-analytic review. Neuropsychology. 2004;18(3):485–503.
Shanahan MA, Pennington BF, Yerys BE, Scott A, Boada R, Willcutt EG, et al. Processing speed deficits in attention deficit/hyperactivity disorder and Reading disability. J Abnorm Child Psychol. 2006;34(5):584–601.
Willcutt EG, Pennington BF, Olson RK, Chhabildas N, Hulslander J. Neuropsychological Analyses of Comorbidity Between Reading Disability and Attention Deficit Hyperactivity Disorder: In Search of the Common Deficit. Dev Neuropsychol. 2005;27(1):35–78.
Rose J. Identifying and teaching children and Young people with dyslexia and literacy difficulties: an independent Report. London: Department for Children, Schools and Families (DCSF); 2009.
Schwenk C, Sasanguie D, Kuhn J-T, Kempe S, Doebler P, Holling H. (non-)symbolic magnitude processing in children with mathematical difficulties: a meta-analysis. Res Dev Disabil. 2017;64:152–67.
Harrowell I, Hollén L, Lingam R, Emond A. The impact of developmental coordination disorder on educational achievement in secondary school. Res Dev Disabil. 2018;72:13–22.
Baddeley A, Hitch G. Working Memory. In: Bower G, editor. Psychology of Learning and Motivation, vol. 8. New York: Academic; 1974. p. 47–89.
Baddeley A. Exploring the central executive. Q J Exp Psychol A. 1996;49(1):5–28.
Baddeley A. The episodic buffer: a new component of working memory? Trends Cogn Sci. 2000;4(11):417–23.
Baddeley A. Working memory, thought, and action: Oxford University Press; 2007.
Baddeley A. Working memory: theories, models, and controversies. Annu Rev Psychol. 2012;63(1):1–29.
Schubert A-L, Hagemann D, Löffler C, Frischkorn GT. Disentangling the effects of processing speed on the association between age differences and fluid intelligence. J Intell. 2019;8(1):1.
Article PubMed Central Google Scholar
Jensen A. Clocking the mind: mental chronometry and individual differences. 1st ed. Amsterdam: Elsevier Science Ltd; 2006.
Mayes SD, Calhoun SL. Learning, attention, writing, and processing speed in typical children and children with ADHD, autism, anxiety, depression, and oppositional-defiant disorder. Child Neuropsychol. 2007;13(6):469–93.
Braaten E, Wiloughby B. Bright kids who can't keep up. New York: The Guilford Press; 2014.
McGrath LM, Pennington BF, Shanahan MA, Santerre-Lemmon LE, Barnard HD, Willcutt EG, et al. A multiple deficit model of reading disability and attention-deficit/hyperactivity disorder: searching for shared cognitive deficits. J Child Psychol Psychiatry. 2011;52(5):547–57.
Boada R, Willcutt E, Pennington B. Understanding the comorbidity between dyslexia and attention-deficit/hyperactivity disorder. Top Lang Disord. 2012;32(3):264–84.
DuPaul GJ, Gormley MJ, Laracy SD. Comorbidity of LD and ADHD: implications of DSM-5 for assessment and treatment. J Learn Disabil. 2012;46(1):43–51.
Lane SJ, Reynolds S. Sensory over-Responsivity as an added dimension in ADHD. Front Integr Neurosci. 2019;13:40.
Marco EJ, Hinkley LBN, Hill SS, Nagarajan SS. Sensory processing in autism: a review of neurophysiologic findings. Pediatr Res. 2011;69(5 Pt 2):48R–54R.
Stray LL, Kristensen Ø, Lomeland M, Skorstad M, Stray T, Tønnessen FE. Motor regulation problems and pain in adults diagnosed with ADHD. Behav Brain Funct. 2013;9(18):1–10.
Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi EVA, et al. The World Health Organization adult ADHD self-report scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35(2):245–56.
Allison C, Auyeung B, Baron-Cohen S. Toward brief “red flags” for autism screening: the short autism Spectrum quotient and the short quantitative checklist in 1,000 cases and 3,000 controls. J Am Acad Child Adolesc Psychiatry. 2012;51(2):202–212.e207.
British Dyslexia Association (BDA): The Adult Dyslexia Checklist, at: https://www.bdadyslexia.org.uk/dyslexia/how-is-dyslexia-diagnosed/dyslexia-checklists , Accessed 31 July 2021.
Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–76.
Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the penn state worry questionnaire. Behav Res Ther. 1990;28(6):487–95.
Centre for Substance Abuse Treatment. Substance Abuse Treatment for Persons with Co-occurring Disorders, Treatment Improvement Protocol (TIP) Series 42, Appendix H: Screening Instruments. Rockville: Substance Abuse and Mental Health Services Administration; 1994.
The National Collaborating Centre for Mental Health: The Improving Access to Psychological Therapies Manual, Updated August 2021, at: https://www.england.nhs.uk/publication/the-improving-access-to-psychological-therapies-manual/ . London, UK; 2018.
DIVA Foundation: The Diagnostic Interview for ADHD in Adults (DIVA-5), at: https://www.divacenter.eu/DIVA.aspx?id=523; 2019.
Young S, Gudjonsson GH. Growing out of ADHD. J Atten Disord. 2007;12(2):162–9.
Weiss MD. Weiss functional impairment rating scale (WFIRS) self-Report. Vancouver: University of British Columbia; 2000.
Mahdi S, Viljoen M, Massuti R, Selb M, Almodayfer O, Karande S, et al. An international qualitative study of ability and disability in ADHD using the WHO-ICF framework. Eur Child Adolesc Psychiatry. 2017;26(10):1219–31.
Sedgwick JA, Merwood A, Asherson P. The positive aspects of attention deficit hyperactivity disorder: a qualitative investigation of successful adults with ADHD. ADHD Atten Deficit Hyperactivity Disord. 2019;11(3):241–53.
Moss SB, Nair R, Vallarino A, Wang S. Attention deficit/hyperactivity disorder in adults. Prim Care. 2007;34(3):445–73.
Eysenck MW, Derakshan N, Santos R, Calvo MG. Anxiety and cognitive performance: Attentional control theory. Emotion. 2007;7(2):336–53.
Sparfeldt JR, Rost DH, Baumeister UM, Christ O. Test anxiety in written and oral examinations. Learn Individ Differ. 2013;24:198–203.
Zeidner M. Test anxiety: the state of the art. Boston: Springer; 1998.
Young S, Adamo N, Ásgeirsdóttir BB, Branney P, Beckett M, Colley W, et al. Females with ADHD: an expert consensus statement taking a lifespan approach providing guidance for the identification and treatment of attention-deficit/ hyperactivity disorder in girls and women. BMC Psychiatry. 2020;20(1):404.
Skirrow C, McLoughlin G, Kuntsi J, Asherson P. Behavioral, neurocognitive and treatment overlap between attention-deficit/hyperactivity disorder and mood instability. Expert Rev Neurother. 2009;9(4):489–503.
Skirrow C, Asherson P. Emotional lability, comorbidity and impairment in adults with attention-deficit hyperactivity disorder. J Affect Disord. 2013;147(1–3):80–6.
Vidal R, Valero S, Nogueira M, Palomar G, Corrales M, Richarte V, et al. Emotional lability: the discriminative value in the diagnosis of attention deficit/hyperactivity disorder in adults. Compr Psychiatry. 2014;55(7):1712–9.
Riley AW, Lyman LM, Spiel G, Döpfner M, Lorenzo MJ, Ralston** SJ: The family strain index (FSI). Reliability, validity, and factor structure of a brief questionnaire for families of children with ADHD. Eur Child Adolesc Psychiatry 2006, 15(S1):i72-i78.
Dougherty L. Children's emotionality and social status: a Meta-analytic review. Soc Dev. 2006;15(3):394–417.
Davidson RJ, Jackson DC, Kalin NH. Emotion, plasticity, context, and regulation: perspectives from affective neuroscience. Psychol Bull. 2000;126(6):890–909.
Yen J-Y, Ko C-H, Yen C-F, Wu H-Y, Yang M-J. The comorbid psychiatric symptoms of internet addiction: attention deficit and hyperactivity disorder (ADHD), depression, social phobia, and hostility. J Adolesc Health. 2007;41(1):93–8.
Breyer J, Botzet A, Winters K, Stinchfield R, August G, Realmuto G. Young adult gambling behaviors and their relationship with the persistence of ADHD. J Gambl Stud. 2009;25(2):227–38.
Baker L, Prevatt F, Proctor B. Drug and alcohol use in college students with and without ADHD. J Atten Disord. 2011;16(3):255–63.
Rooney M, Chronis-Tuscano A, Yoon Y. Substance use in college students with ADHD. J Atten Disord. 2011;16(3):221–34.
Arria A, Garnier-Dykstra L, Caldeira K, Vincent K, Winick E, O'Grady K. Drug use patterns and continuous enrollment in college: results from a longitudinal study. J Stud Alcohol Drugs. 2013;74(1):71–83.
Spera V, Pallucchini A, Carli M, Maiello M, Maremmani AGI, Perugi G, et al. Does Cannabis, cocaine and alcohol use impact differently on adult attention deficit/hyperactivity disorder clinical picture? J Clin Med. 2021;10(7):1481.
Cooper RE, Williams E, Seegobin S, Tye C, Kuntsi J, Asherson P. Cannabinoids in attention-deficit/hyperactivity disorder: a randomised-controlled trial. Eur Neuropsychopharmacol. 2017;27(8):795–808.
Carmona-Halty M, Schaufeli WB, Salanova M. Good relationships, good performance: the mediating role of psychological capital - a three-wave study among students. Front Psychol. 2019;10(306):1–5.
Dennis M, Francis DJ, Cirino PT, Schachar R, Barnes MA, Fletcher JM. Why IQ is not a covariate in cognitive studies of neurodevelopmental disorders. J Int Neuropsychol Soc. 2009;15(3):331–43.
Geertshuis SA. Slaves to our emotions: examining the predictive relationship between emotional well-being and academic outcomes. Act Learn High Educ. 2018;20(2):153–66.
Lewis M, Vance A, Maruff P, Wilson P, Cairney S. Differences in motor imagery between children with developmental coordination disorder with and without the combined type of ADHD. Dev Med Child Neurol. 2008;50(8):608–12.
Pekrun R, Goetz T, Perry RP, Kramer K, Hochstadt M, Molfenter S. Beyond test anxiety: development and validation of the test emotions questionnaire (TEQ). Anxiety Stress Coping. 2004;17(3):287–316.
Thornicroft G. Stigma and discrimination limit access to mental health care. Epidemiol Psichiatria Soc. 2008;17(1):14–9.
Kooij J, Bijlenga D, Salerno L, Jaeschke R, Bitter I, Balázs J, et al. Updated European consensus statement on diagnosis and treatment of adult ADHD. Eur Psychiatry. 2019;56(1):14–34.
Pescosolido BA, Martin JK, Lang A, Olafsdottir S. Rethinking theoretical approaches to stigma: a framework integrating normative influences on stigma (FINIS). Soc Sci Med. 2008;67(3):431–40.
Lebowitz MS. Stigmatization of ADHD. J Atten Disord. 2013;20(3):199–205.
Tatlow-Golden M, Prihodova L, Gavin B, Cullen W, McNicholas F. What do general practitioners know about ADHD? Attitudes and knowledge among first-contact gatekeepers: systematic narrative review. BMC Fam Pract. 2016;17(1):1–15.
Canu WH, Newman ML, Morrow TL, Pope DLW. Social appraisal of adult ADHD. J Atten Disord. 2007;11(6):700–10.
McKeague L, Hennessy E, O'Driscoll C, Heary C. Retrospective accounts of self-stigma experienced by young people with attention-deficit/hyperactivity disorder (ADHD) or depression. Psychiatr Rehabil J. 2015;38(2):158–63.
Faraone SV, Banaschewski T, Coghill D, Zheng Y, Biederman J, Bellgrove MA, et al. The world federation of ADHD international consensus statement: 208 evidence-based conclusions about the disorder. Neurosci Biobehav Rev. 2021;128:789–818.
Harrison A, Edwards M, Parker K. Identifying students faking ADHD: preliminary findings and strategies for detection. Arch Clin Neuropsychol. 2007;22(5):577–88.
Musso MW, Gouvier WD. “Why is this so hard?” a review of detection of malingered ADHD in college students. J Atten Disord. 2012;18(3):186–201.
SpLD Assessment and Standards Committee (SASC). Suitable tests for the assessment of specific learning difficulties in higher education, at: http://www.sasc.org.uk/(S(fre2zi45ou2m12vcc1nx43q0))/SASCDocuments/REVISED%20guidelines-March%202016.pdf . Accessed 31 July 2021. London; 2016.
Adler L, Spencer T, Levine L, Ramsey J, Tamura R, Kelsey D, et al. Diagnosing and treating adult ADHD and comorbid conditions. J Clin Psychiatry. 2008;69(11):e31.
NICE (National Institute for Health and Care Excellence). Common mental health problems: identification and pathways to care. London; 2011.
Denton CA, Tamm L, Schatschneider C, Epstein JN. The effects of ADHD treatment and Reading intervention on the fluency and comprehension of children with ADHD and word Reading difficulties: a randomized clinical trial. Sci Stud Read. 2020;24(1):72–89.
McLean A, Dowson J, Toone B, Young S, Bazanis E, Robbins TW, et al. Characteristic neurocognitive profile associated with adult attention-deficit/hyperactivity disorder. Psychol Med. 2004;34(4):681–92.
Solanto MV, Scheres A. Feasibility, acceptability, and effectiveness of a new cognitive-behavioral intervention for college students with ADHD. J Atten Disord. 2020;25(14):2068–82.
Barkley R. Neuropsychological testing is not useful in the diagnosis of ADHD: stop it (or prove it)! ADHD Rep. 2019;27(2):1–8.
Gioia GA, Isquith PK, Guy SC, Kenworthy L. Test review: behavior rating inventory of executive function. Child Neuropsychol. 2000;6(3):235–8.
Mowlem F, Agnew-Blais J, Taylor E, Asherson P. Do different factors influence whether girls versus boys meet ADHD diagnostic criteria? Sex differences among children with high ADHD symptoms. Psychiatry Res. 2019;272:765–73.
Faraone S, Kunwar A, Adamson J, Biederman J. Personality traits among ADHD adults: implications of late-onset and subthreshold diagnoses. Psychol Med. 2009;39(4):685–93.
Leucht S, Hierl S, Kissling W, Dold M, Davis JM. Putting the efficacy of psychiatric and general medicine medication into perspective: review of meta-analyses. Br J Psychiatry. 2012;200(2):97–106.
Rabiner DL, Anastopoulos AD, Costello EJ, Hoyle RH, McCabe SE, Swartzwelder HS. Motives and perceived consequences of nonmedical ADHD medication use by college students. J Atten Disord. 2008;13(3):259–70.
DuPaul GJ, Weyandt LL, Rossi JS, Vilardo BA, O’Dell SM, Carson KM, et al. Double-blind, placebo-controlled, crossover study of the efficacy and safety of Lisdexamfetamine Dimesylate in college students with ADHD. J Atten Disord. 2012;16(3):202–20.
Advokat C, Lane S, Luo C. College students with and without ADHD. J Atten Disord. 2010;15(8):656–66.
Lu Y, Sjölander A, Cederlöf M, D'Onofrio BM, Almqvist C, Larsson H, et al. Association between medication use and performance on higher education entrance tests in individuals with attention-deficit/hyperactivity disorder. JAMA Psychiatry. 2017;74(8):815–22.
Rabiner DL, Anastopoulos AD, Costello EJ, Hoyle RH, Esteban McCabe S, Swartzwelder HS. The misuse and diversion of prescribed ADHD medications by college students. J Atten Disord. 2009;13(2):144–53.
DeSantis AD, Webb EM, Noar SM. Illicit use of prescription ADHD medications on a college campus: a multimethodological approach. J Am Coll Heal. 2008;57(3):315–24.
Caisley H, Müller U. Adherence to medication in adults with attention deficit hyperactivity disorder and pro re nata dosing of psychostimulants: a systematic review. Eur Psychiatry. 2012;27(5):343–9.
Müller-Sedgwick U, Sedgwick-Müller JA. Drugs to treat attention deficit hyperactivity disorder (ADHD). In: Seminars in clinical psychopharmacology: Cambridge University Press; 2020. p. 392–432.
Cairncross M, Miller C. The effectiveness of mindfulness-based therapies for ADHD: a Meta-analytic review. J Atten Disord. 2016;24(5):627–43.
De Crescenzo F, Cortese S, Adamo N, Janiri L. Pharmacological and non-pharmacological treatment of adults with ADHD: a meta-review. Evid Based Ment Health. 2016;20(1):4–11.
Jensen CM, Amdisen BL, Jørgensen KJ, Arnfred SMH. Cognitive behavioural therapy for ADHD in adults: systematic review and meta-analyses. ADHD Atten Deficit Hyperactivity Disord. 2016;8(1):3–11.
Ramsay JR, Rostain AL. Cognitive-behavioral therapy for adult ADHD: Routledge; 2012.
Anastopoulos A, Langberg J, Eddy L, Silvia P, Labban J. A randomized controlled trial examining CBT for college students with ADHD. J Consult Clin Psychol. 2021;89(1):21–33.
Eddy LD, Anastopoulos AD, Dvorsky MR, Silvia PJ, Labban JD, Langberg JM. An RCT of a CBT intervention for emerging adults with ADHD attending college: functional outcomes. J Clin Child Adolesc Psychol. 2021;50(6):844–57.
Critchfield T, Kollins S. Temporal discounting: basic research and the analysis of socially important behavior. J Appl Behav Anal. 2001;34(1):101–22.
Scheres A, Solanto MV. Do ADHD symptoms, executive function, and study strategies predict temporal reward discounting in college students with varying levels of ADHD symptoms? A pilot study. Brain Sci. 2021;11(2):181.
Solanto MV. Cognitive behavioral therapy for adult ADHD: targeting executive dysfunction. New York: The Guildford Press; 2011.
Lopez PL, Torrente FM, Ciapponi A, Lischinsky AG, Cetkovich-Bakmas M, Rojas JI, et al. Cognitive-behavioural interventions for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst Rev. 2013;3(3):CD010840. https://doi.org/10.1002/14651858.CD010840.pub2 .
Hinshaw SP, Arnold LE. ADHD, multimodal treatment, and longitudinal outcome: evidence, paradox, and challenge. Cogn Sci. 2015;6(1):39–52.
Prevatt F, Lampropoulos GK, Bowles V, Garrett L. The use of between session assignments in ADHD coaching with college students. J Atten Disord. 2011;15(1):18–27.
Swartz SL, Prevatt F, Proctor BE. A coaching intervention for college students with attention deficit/hyperactivity disorder. Psychol Sch. 2005;42(6):647–56.
Parker DR, Hoffman SF, Sawilowsky S, Rolands L. Self-control in postsecondary settings. J Atten Disord. 2013;17(3):215–32.
Parker D, Hoffman S, Sawilowsky S, Rolands L. An examination of the effects of ADHD coaching on university students executive functioning. J Postsecondary Educ Disabil. 2011;24:115–32.
Young S, Bramham J. Cognitive-Behavioural therapy for ADHD in adolescents and adults: Wiley-Blackwell; 2012.
Burns D, Danall N, Holt M. Assessing the impact of the COVID-19 pandemic on student wellbeing at universities in the United Kingdom: a conceptual analysis. Front Educ. 2020;5:582882. https://doi.org/10.3389/feduc.2020.582882 .
Stathopoulou T, Mouriki A, Papliou O. Student well-being during the COVID-19 pandemic in Greece. Athens: National Centre for Social Research; 2020.
Van De Velde S, Buffel V, Bracke P, Van Hal G, Wouters E. The COVID-19 international student well-being study. Eur J Pub Health. 2021;31(Supplement_3).
Plakhotnik MS, Volkova NV, Jiang C, Yahiaoui D, Pheiffer G, McKay K, et al. The perceived impact of COVID-19 on student well-being and the mediating role of the university support: evidence from France, Germany, Russia, and the UK. Front Psychol. 2021;12:642689.
Frampton N, Smithies D. University Mental Health: Life in the Pandemic 2020/2021. Leeds: Student Minds; 2021.
Almendingen K, Morseth M, Gjølstad E, Brevik A, Tørris C. Student's experiences with online teaching following COVID-19 lockdown: a mixed methods explorative study. PLoS One. 2021;16(8):e0250378.
Al-Tammemi A, Akour A, Alfalah L. Is it just about physical health? An online cross-sectional study exploring the psychological distress Among University students in Jordan in the midst of COVID-19 pandemic. Front Psychol. 2020;11:562213.
Merzon E, Weiss MD, Cortese S, Rotem A, Schneider T, Craig SG, et al. The association between ADHD and the severity of COVID-19 infection. J Atten Disord. 2022;26(4):491–501. https://doi.org/10.1177/10870547211003659 .
Pollak Y, Shoham R, Dayan H, Gabrieli-Seri O, Berger I. Symptoms of ADHD predict lower adaptation to the COVID-19 outbreak: financial decline, low adherence to preventive measures, psychological distress, and illness-related negative perceptions. J Atten Disord. 2021:108705472110279.
Blackall M, Mistlin A. "Broken and Defeated": UK university students on the impact of COVID rules, The Guardian, at: https://www.theguardian.com/education/2021/jan/11/broken-and-defeated-uk-university-students-on-the-impact-of-covid-rules . 11 Jan 2021.
BBC News, Coronavirus: Inside the secret Covid rave scene: at: https://www.bbc.co.uk/news/av/uk-53283351 . 4 July, 2020.
Reuters, Scuffles and arrests as anti-lockdown protesters march through London: at: https://www.reuters.com/article/uk-britain-protests-idUSKBN2BC092 , 20 March, 2021.
Raghupathi V, Raghupathi W. The influence of education on health: an empirical assessment of OECD countries for the period 1995-2015. Arch Public Health. 2020;78:20.
Webb O, Wyness L, Cotton D. Enhancing Access, Retention, Attainment and Progression in Higher Education: A Review of the Literature Showing Demonstrable Impact, vol. 132. York: Higher Education Academy; 2017.
Clery S, Topper A. Grade point average and student outcomes. Data Notes. 2010;5(1):1–5.
Download references
Acknowledgements
We acknowledge JSM for facilitating the consensus meeting and preparing this manuscript, PA, UMS, for assistance in reviewing and editing drafts of this manuscript. We are grateful to Ms. Sue Curtis for recording the meeting and preparing the transcripts from the meeting.
This research did not receive any funding from public, private, or not-for-profit organisations or agencies.
Author information
Authors and affiliations.
Health and Community Services, Government of Jersey, St Helier, Jersey. Social, Genetic & Developmental Psychiatry, Institute of Psychiatry, Psychology & Neuroscience (IoPPN) & Florence Nightingale Faculty of Nursing, Midwifery & Palliative Care (FNFNM), King’s College London, London, UK
Jane A. Sedgwick-Müller
Adult Neurodevelopmental Service, Health and Community Services, Government of Jersey, St Helier, Jersey. Department of Psychiatry, University of Cambridge, Cambridge, UK
Ulrich Müller-Sedgwick
School of Human and Health Sciences, University of Huddersfield, Huddersfield, UK
Marios Adamou & Rebecca Champ
Natbrainlab, Forensic and Neurodevelopmental Sciences, Institute of Psychiatry, Psychology & Neuroscience (IoPPN), King’s College London, London, UK
Marco Catani
Psychology Department, Institute of Psychiatry, Psychology & Neuroscience (IoPPN), King’s College London, London, UK
Gísli Gudjónsson
Adult ADHD Service, Avon and Wiltshire Mental Health Partnership NHS Trust, Bristol, UK
Dietmar Hank
Adult ADHD and Autism Outpatient Service, South London & Maudsley NHS Foundation Trust, London, UK
Psychology Services Limited, Department of Psychology, Reykjavik University, Reykjavik, Iceland
Susan Young
Social, Genetic & Developmental Psychiatry, Institute of Psychiatry, Psychology & Neuroscience (IoPPN), King’s College London, London, UK
Philip Asherson
You can also search for this author in PubMed Google Scholar
Contributions
JSM conceived the work; PA, MC, RC were keynote speakers during the meeting; JSM, PA and UMS were involved in drafting the manuscript and critically revising it. A final draft was circulated by JSM to UMS, MA, MC, RC, GG, DH, MP, SY and PA, who endorsed the consensus and approved the manuscript.
Corresponding author
Correspondence to Jane A. Sedgwick-Müller .
Ethics declarations
Ethics approval and consent to participate.
All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not Applicable.
Competing interests
YES, “JSM, USM, MP, SY, PA have received honoraria and pharmaceutical funding for consultation, research awards, educational talks, study days and/or conference support. JSM is in receipt of an educational grant from the Royal College of Nursing (RCN) Foundation towards PhD tuition fees and received the 2020 RCN Muriel Fleet Award for outstanding professional development and 2020 Genius Within Award for Neurodiverse Research of the Year and all other authors have no other competing interests to disclose.”
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Sedgwick-Müller, J.A., Müller-Sedgwick, U., Adamou, M. et al. University students with attention deficit hyperactivity disorder (ADHD): a consensus statement from the UK Adult ADHD Network (UKAAN). BMC Psychiatry 22 , 292 (2022). https://doi.org/10.1186/s12888-022-03898-z
Download citation
Received : 29 September 2021
Accepted : 15 March 2022
Published : 22 April 2022
DOI : https://doi.org/10.1186/s12888-022-03898-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Attention-deficit/hyperactivity disorder
- Academic performance
- Academic achievement
- University students
- Educational outcomes
- Higher education
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Browser does not support script.
Understanding ADHD: Current Research and Practice
Key information, subject area:.
FutureLearn Online Courses
Course type:
Continuing Professional Development (CPD)
Credit level:
Not for credit
Available course dates:
From: 01 September 2023 To: 31 August 2024
Course overview
Ensure your knowledge of ADHD is up to date by exploring the latest research.
What is attention deficit hyperactivity disorder (ADHD)? What are the symptoms of ADHD? How is ADHD diagnosed? Get answers with this course that features fundamental information about ADHD, as well as the latest ADHD research.
Through the course you will learn about ADHD as a developmental disorder, considering controversies related to the condition. You will learn about the diagnosis and best practice treatment of ADHD as you build your empathy towards people with ADHD. You will also learn practical strategies to help the educational and personal development of people with ADHD.
What does this course cover?
- What ADHD is, and the controversies raised by the concept of ADHD
- Latest neuroscientific and psychiatric research based on the mechanisms, symptoms and impairments of ADHD
- ADHD as a developmental disorder throughout the lifespan: genes, environments (protective and risk factors)
- Latest neuroscientific and psychiatric research based on the various means of screening and assessing for child ADHD
- Latest neuroscientific and psychiatric research based on the mechanisms, diagnosis and treatment of adult ADHD
- Understanding best practice in treatment for ADHD Mechanisms and efficacy of psychosocial treatments, pharmacological treatments supporting positive outcomes for those with ADHD and their families
What will I achieve?
- Discuss the prevalence and impact of ADHD in children, adolescents and adults.
- Discuss ADHD as a disorder and how it differs from normal behaviour.
- Be able to critically assess key factors in the conceptualisation and understanding of the disorder.
- Discuss the core challenges faced by those with ADHD, their families and relevant professionals.
- Discuss wider issues related to ADHD, such as labelling and stigma from multiple perspectives.
- Demonstrate an empathic understanding of the experiences of people living with ADHD.
- Describe core principles, tools and techniques used in the screening and diagnosis of ADHD, and the factors that may impact on the accuracy of a diagnosis.
- Explain how ADHD is distinguished from, and relates to, other common neurodevelopmental, behavioural and mental health problems.
- Reflect upon and discuss current evidence for the genetic and environmental vulnerability for ADHD, and associated neurological mechanisms for ADHD.
- Critically discuss the current evidence base for both pharmaceutical and non-pharmaceutical interventions for ADHD.
- Evaluate the rationale, mechanism, and limitations of the primary medical and psychosocial treatments for ADHD.
- Evaluate practical strategies to support the educational and personal development of those living with ADHD.
- Be able to identify resources and relevant support services for those living with ADHD.
- Evaluate the biological and environmental risk factors for ADHD.
Who will I learn with?

Katya Rubia
Professor of Cognitive Neuroscience

Philip Asherson
Emeritus Professor of Neurodevelopmental Psychiatry

Edmund Sonuga-Barke
Professor of Developmental Psychology, Psychiatry and Neuroscience

Eric Taylor
Emeritus Professor of Child and Adolescent Psychiatry

Mark Kennedy
Lecturer in Mental Health Education
Who is this for?
This course is for people with ADHD and anyone working with children and adults with ADHD. This includes parents and close family members, teachers, and educational (learning disability) assessors in schools and higher education and occupational therapists.
What is the teaching schedule?
This course runs multiple times each year. Every run of a course has a set start date but you can join it and work through it after it starts. Please click the Apply button to find out when the next run will start.
Our partners
Future Learn
Course status:
Full fee £0

- Institute of Psychiatry, Psychology & Neuroscience
- Department of Basic & Clinical Neuroscience
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Special Collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 4, Issue 1
- What families in the UK use to manage attention-deficit/hyperactivity disorder (ADHD): a survey of resource use
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-5364-6022 Philippa Fibert 1 ,
- Clare Relton 2
- 1 Health Hawk , High Wycombe , UK
- 2 Institute of Population Health , Queen Mary University of London , London , UK
- Correspondence to Dr Philippa Fibert; philippafibert{at}gmail.com
Objective To identify interventions being used to manage attention-deficit/hyperactivity disorder (ADHD) in the UK.
Design A survey within the Sheffield Treatments for ADHD Research project. A convenience sample of participants in the UK who consented to join an observational cohort were asked closed questions about medication, behavioural change programmes and service use, and an open-ended question about what else they used.
Setting A broad variety of non-National Health Service, non-treatment seeking settings throughout the UK, including local authority organisations, schools, ADHD and autism spectrum condition support groups and social media.
Participants Families of children aged 5–18 with carer reported ADHD and Conners Global Index (CGI) T scores of 55+.
Results Responses from 175 families were analysed. The mean age of the children was 10.21 (2.44), and two-thirds (n=114) had additional diagnoses. The majority used medications to manage ADHD (n=120) and had participated in a parenting class (n=130). Just over a quarter (28%, n=49) did not use ADHD medications, and used sleep medications. Just under half had consulted psychologists (n=83), and 32 had participated in other talking therapies such as psychotherapy, counselling and cognitive–behavioural therapy. A few used aids such as reward charts or fiddle toys (n=17) and participated in activities (mostly physical) (n=14). A substantial minority (78/175) had used non-mainstream treatments, the most popular being homoeopathy (n=32), nutritional interventions (n=21) and bodywork such as massage or cranial osteopathy (n=9).
Conclusions Families reported use of a wide variety of treatments to help with management of their children with ADHD in addition to their use of mainstream treatments.
- child psychiatry
- therapeutics
- neuropathology
- health services research
- data collection
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjpo-2020-000771
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
What is known about the subject?
For many of those with attention-deficit/hyperactivity disorder (ADHD) mainstream interventions do not improve long-term outcomes.
Carers additionally try non-mainstream interventions to help their children.
Surveys documenting what carers try have been conducted in a variety of countries but not in the UK.
What this study adds?
Families with children with ADHD in the UK are using a wide variety of main and non-mainstream treatments, which are both publicly and privately funded, to help with ADHD management.
Nearly 70% of those surveyed reported using pharmaceutical medications, 74% had participated in a parenting class, and 45% reported use of non-mainstream treatments.
The most popular non-mainstream treatments used were nutrition, homoeopathy, massage and cranial osteopathy.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is one of the most commonly diagnosed and treated childhood psychiatric disorders. Children are hyperactive (fidgety and unable to sit still for long periods), and impulsive (doing things without stopping to think). They find it hard to concentrate and follow instructions, and to regulate their emotions. This results in problems at school, at home, and with their peers where they struggle to fit in, 1 and get into trouble. 2 Heterogeneity (non-uniformity) is a feature of ADHD expression. Children often have a wide range of other diagnoses and co-occurring problems such as autism spectrum conditions (ASCs) (50%–75%), 3 conduct disorders (24%), 4 sleep disorders (25%–50%), 5 tics (60%), 6 gut dysbiosis, 7 obesity (40%), 8 anxiety, depression (33%), 9 reading and other learning problems. 10
Treating ADHD is challenging. Interventions are offered to help manage symptoms. The National Health Service (NHS) offers National Institute for Health and Care Excellence (NICE) recommended treatments of behaviour change programmes and pharmaceutical medications. Recent NICE updates suggest also asking about diet and offering advice if relevant. While implemented, recommended treatments often palliate some symptoms making classroom and family life more manageable, however, their long-term effectiveness and ability to address important negative outcomes remains in doubt. 11 Adherence is poor and side effects of pharmaceutical medications common. 12
While the majority of carers of children with ADHD in the UK rely on NICE recommended treatments, a number try other treatments, identified by themselves rather than doctor recommendation, and usually requiring out of pocket payments. Such treatments are collectively described in a variety of ways, and their categorisation also varies.
For the purposes of this article such treatments will be referred to as ‘non-mainstream’. Other descriptive terms for non-mainstream are ‘complementary and/or complementary medicine’ referring to a broad set of healthcare practices that are not part of that country’s own tradition or conventional medicine and not fully integrated into the dominant healthcare system. 13 The term ‘integrative’ is used when conventional and complementary approaches are used in a coordinated way ( https://nccih.nih.gov ). Treatments move from non-mainstream to mainstream as their evidence base and/or acceptability grows.
Non-mainstream treatments are also described as ‘natural’. 14 Although doctors can be uncomfortable recommending treatments about which they are unknowledgeable and untrained, 15 there is a growing interest in using natural medicines particularly in paediatrics. 16 17
Carer use of non-mainstream treatments for ADHD has been found to be driven by a desire for alternatives to pharmaceutical medications, 17–19 ; to minimise symptoms of ADHD; for additional benefit combined with conventional treatment; to avoid prescribed medication side effects, 20 21 and dissatisfaction with conventional care. 22 Ninety per cent+ carers of children with ADHD surveyed hope to see more research on non-mainstream treatments conducted. 23
Surveys in several countries have sought to identify which and how frequently non-mainstream treatments are used to manage ADHD. Using Google Scholar, Web of Science and cross-referencing, 10 such surveys were found: three in Australia, five in the USA, one in Canada and one in Israel ( table 1 ). No surveys were identified in the UK. This survey seeks to address this gap. Data about resource use was collected from a convenience sample of families recruited to the Sheffield Treatments for ADHD Research (STAR) project. The project used Trials within Cohorts (TwiCs) methodology, 24 whereby first a large observational cohort of participants with the condition of interest was recruited and their outcomes of interest regularly measured.
- View inline
Non-mainstream treatment use (N-MT) according to surveys
This report describes the resource use reported by cohort participants at entry into the observational cohort ( online supplemental appendix 1 ). 25 Results of the pilot randomised controlled trials (RCTs) conducted within the cohort and detailed population characteristics are reported elsewhere. 26
Supplemental material
Patient and public involvement.
The STAR project was preceded by a case series. 27 Families with children with ADHD participating in this preceding study expressed frustration at the lack of helpful treatment options and a desire to support research testing new treatments which might help their children. These families contributed to the design of the STAR project including: the design and piloting of the study questionnaire where an extra open-ended question ‘use this space for anything else you would like to tell us’ was added (see online supplemental appendix 1 ); and the generation of an interactive hip-hop rap performance called Lost Voices based on participating family’s stories, which was widely shared on Facebook and helped increase recruitment. 28
To describe what families in the UK are using to manage their children with ADHD.
The STAR project (including the survey) was sponsored by the University of Sheffield (URMS number 143647), and approved under the University of Sheffield’s Ethics Review Procedure by the School of Health and Related Research (ScHARR) Research Ethics committee (REC) on 30/4/15, application number 003424 25 Informed consent was received from all carers and children.
Study design
This survey reports the responses from UK families with children with ADHD who agreed to participate in an observational cohort. 25 26
Recruitment
Families of children aged 5–18 with ADHD were recruited from a broad variety of non-NHS, non-treatment seeking settings, initially in Sheffield and then throughout the UK, between September 2015 and September 2016. These included local authority organisations, schools, ADHD and autism support groups, conferences, and social media.
Recruitment was via a questionnaire which could be completed on-line or on paper by carers and took approximately 10 min to complete ( online supplemental appendix 1 ). Carers were asked to provide the date, address and name of the doctor who diagnosed the child’s ADHD and complete the Conners Global ADHD Index (CGI). 29 To be included in the cohort children were required to have a CGI T score of at least 55 (denoting mild a-typicality). No restriction was placed on length of time since diagnosis.
Carers were asked questions intended to capture all treatments ever received by the child, not specifically for their ADHD: ‘ Please tell us about all your child’s diagnoses and any medications taken for them’; ‘how often have you visited/been visited by the doctor, hospital, social worker or police in the last 6 months’; ‘what else have you used to help your child in the past/now?: Family Action Parenting class (asked about on specific request from Sheffield Family Action); another parenting class? sessions with a psychologist?’; homoeopathy?’; (asked about due to inclusion/exclusion criteria for a subsequent RCT); anything else?’. This open-ended ‘anything else’ question was included to help identify all non-mainstream treatments that were or had been used. The final open-ended question ‘use this space for anything else you would like to tell us’ was included on patient and public involvement recommendation.
Participant characteristics
Questionnaires were completed by the carers of 194 children. Nineteen of these children had no reported diagnosis of ADHD, so their responses were excluded, therefore, the total number of children included in the survey was 175.
Approximately one-third (35%) reported a sole diagnosis of ADHD, while the remaining two-thirds (65%) reported one or more additional diagnoses of which the most common was an ASC ( table 2 ).
Diagnoses of cohort participants
The mean age of the children was 10.21 (2.44). Eighty-four per cent were boys and sixteen per cent girls. During the previous 6 months, 12 children had been involved with the police (range 1–20 visits per child). Fifteen children were involved with social workers (range 1–15 visits). Over half (n=104) had visited hospital (range 1–20 visits) and had visited doctors (n=117) (range 1–20 visits). Over half (56%) of children had a teaching assistant, of whom 22% had one full time.
Resource use
Nearly two-thirds of the children were taking a mainstream ADHD medication, of which most took a methylphenidate derivative such as Ritalin. Nearly one-third took sleep medications ( table 3 ).
Pharmaceutical medicines used by families
One-third of families had participated in behaviour focused therapies (range 1–5 therapies per family) ( table 4 ). The most frequently reported was consultation with a psychologist. Just under three quarters had participated in or were currently participating in parenting classes. Family Action is offered to all newly diagnosed families in Sheffield. Other classes mentioned were: 123 magic, triple P, positive parenting, teach, change 4 life, anger management and incredible years.
Other resource use by families
Carers also described a wide variety of other creative and talking therapies that they used to help modify or manage behaviour. For example, art therapy, which was being offered by Sheffield Child and Adult Mental Health Services at the time.
A broad variety of activities ranging from the more physical such as judo, to the more creative such as theatre school, were described (range 1–4 activities per child). Seventeen families reported using aids, were which were usually to help the child with an accompanying ASC diagnosis (ear defenders and weighted blankets); or if hyperactivity and lack of focus were the issue (fiddle toys and wobble cushions) ( table 4 ).
Non-mainstream resource use
Nearly half (45%, n=78) reported non-mainstream resource use (range 1–5 per family), of which the most commonly reported was homoeopathy. The next most commonly reported was a dietary intervention: either taking an over the counter nutritional supplement, or diet changes, mostly without the support of a nutritional specialist ( table 5 ).
Non-mainstream treatments used by families
There were responses from 61 participants to the open-ended question ‘use this space for anything else you would like to tell us’. Their free text comments were thematically analysed. Six categories emerged: friendships, school, home, family circumstances, medication and sleep.
Carers described how lack of friendships were an issue for their children: ‘My child gets excluded from parties, invitations to friend’s houses and parents actively try to keep their children away’. School was problematic for both children and their carers trying to help them: ‘today he didn't get up until I physically made him, he then missed his bus to school and then had an argument with other students during lunch break. When finally I got him organised to sit down and do some homework it turned out he'd lost it on the way home. Quite a typical day!’.
Home life was described as stressful, particularly in the mornings: ‘Home life very much affected by X to the point of being ruled by her behaviour…. still not dressed today at 5pm despite numerous prompts’. Family circumstances described were specific traumas and bereavements: ‘ X was removed from birth mum at birth, was in foster care until 17 months old when she was placed with us’.
Medication experiences were both positive: ‘The medication is an absolute God send. Without it our lives would be so stressful and I'm sure X wouldn’t be able to attend mainstream school’; and negative ‘can’t take any due to bad reaction on her stomach, tried 5 different ones’. Sleep problems were commonly mentioned: ‘Last night was a good night’s sleep for my son and he slept till after 6. This is a rarity as he can be awake and hyperactive from 2am.’. Many felt that ADHD is mis-understood and that the voices of families with ADHD not heard.
The number of families reporting that their children had codiagnoses suggest that in this regard, this convenience sample are broadly representative of the ADHD population, where co-diagnoses are estimated to occur in 40%–65%. 30 31
This survey reports high levels of health need and use of public resources. The majority of those surveyed used mainstream treatments such as pharmaceutical medications, behaviour management classes and psychological therapies. Seven per cent of families were involved with social workers; 6% of children had been excluded from school and 5% were currently, or had been involved with the police. Additionally, 45% of families had used non-mainstream treatments.
The most commonly used non-mainstream treatments were homoeopathy and nutrition. The role of nutrition is increasingly acknowledged in the aetiology, impact on, and treatment of, ADHD. Consideration of nutrition is now moving towards the mainstream, as exemplified by its recent inclusion in NICE guidelines. More surprising is the high use of homoeopathy. It is unclear whether use refers to over the counter homeopathic medicines such as Arnica for bruising, or Chamomilla for teething, or visits to a homeopath (available via the NHS in some parts of the UK), or both.
Sample sizes of surveys conducted in other countries range from 73 to 822. Ours was 175. At 31%, our non-mainstream treatment use is slightly less than median usage found in other surveys (range 12%–71%) ( table 1 ). Lower estimates are thought to be the result of narrower definitions of such treatments, 19 32 however, our inclusion of an open-ended question theoretically allowed for broad definition of non-mainstream treatments, and indeed included a diverse array. Reported use appears to vary by country, with higher use reported in Australia (range 64%–71%) and lower use in the USA (range 12%–54%). Surveys agree that treatments are predominantly used alongside pharmaceutical medications ( table 1 ).
The results of our survey broadly concur with those from other surveys. Although other surveys varied in the non-mainstream treatments they asked about, they commonly asked about dietary interventions (8/10), with some asking generally, and some specifically about supplements and dietary changes. Four surveys asked about herbs, homoeopathy or chiropractic/osteopathy; and three about acupuncture or yoga. According to the 10 surveys, the most popular treatments were supplements, dietary changes, acupuncture, homoeopathy, massage, craniosacral therapy, music therapy, equine therapy, secretin and chelation.
Popular treatments according to our survey were homoeopathy, nutrition (particularly supplementary fish oils), massage, osteopathy, aromatherapy, a variety of relaxation approaches, acupuncture and hypnotherapy. However, none in our survey reported using herbs. Unique to our survey was reported use of Cannabidiol oil, Epsom salts, metamorphic technique, reflexology, crystals and Bach flower remedies.
A limitation of our survey is the mixture of questions specifying a particular intervention (eg, have you done a parenting class/seen a psychologist/used homoeopathy) and more open questions (eg, what else have you done to help your child). There are advantages and disadvantages of each question type: the use of an open-ended question allowed the broad spectrum of treatments being used to be represented; however, it is likely that some utilised treatments were omitted which might have been remembered had a prompt list been provided.
Most interventions being used are under researched and the evidence produced low quality due to: poor internal validity (lack of blinded assessment, and small population sizes); poor external validity (lack of trials in representative populations and lack of measurement of long-term outcomes); and poor ecological validity (tested interventions do not represent core aspects of the therapy). In 2000, it was identified as a public health issue in the UK that we do not have adequate knowledge of the putative benefits of non-mainstream treatments. 33 We still have little information and just 0.0085% of research funding is allocated to testing Complementary and Alternative Medicine interventions in the UK. 34
Of the treatments used, elements of a nutritional approach are the most researched, particularly the ‘few foods diet’, artificial food colour elimination, fatty acid supplementation, single and multiple nutrients. Effect sizes are generally small. Researchers concur that the few foods diet may offer opportunities, but further large-scale, high-quality studies are needed. 35 It is unlikely that single nutrient or dietary interventions impact the complex array of biochemical pathways that may be aberrant in ADHD. Furthermore administration of one nutrient or approach may cause an imbalance in another. 7 The pilot RCT conducted in our cohort tested the effectiveness of offering a total nutritional approach combining supplementation, elimination, and healthy diet advice by a nutritional therapist. 26 A medium effect size was found, and the pragmatic trial design used may address some of these issues.
Homoeopathy is the next most researched treatment. Three RCTs testing the efficacy of individually tailored homoeopathic medicines, 36–38 and one testing the efficacy of a generic homeopathic product, 39 were synthesised in a Cochrane review 40 which overall found little evidence of efficacy and recommended development of optimal treatment protocols. Subsequently, two further RCTs testing the effectiveness of treatment by homoeopaths, 26 41 and one testing the efficacy of a generic homeopathic product, 42 have been conducted.
Families used their experience of participating in an observational cohort to describe a broad variety of resources and treatments they use to manage the condition over and above NHS recommended treatments. This is a convenience sample of participants in the UK who consented to recruit to a cohort, and it may be that dissatisfaction with conventional care drew them towards participation. Nevertheless, results from our survey do not deviate substantially from the results from population and clinical samples.
Development of robust evidence of the putative effectiveness of the non-mainstream treatments being used should be a priority given that they are being used by carers; paediatric doctors are increasingly turning to more natural treatments; long-term negative outcomes of those with ADHD are not being affected; and currently recommended treatments are palliative and associated with common side effects. Surveying carers is a useful means of identifying which treatments are being used and should subsequently be tested.
Acknowledgments
The work could not have been conducted without the support of all the participating families with children with ADHD.
- Peasgood T ,
- Bhardwaj A ,
- Biggs K , et al
- Simonoff E ,
- Kuntsi J , et al
- Storebø OJ ,
- Ramstad E ,
- Krogh HB , et al
- Gillberg C ,
- Gillberg IC ,
- Rasmussen P , et al
- Rucklidge JJ ,
- Johnstone JM
- Cortese S ,
- Moreira-Maia CR ,
- St Fleur D , et al
- Calhoun SL ,
- Bixler EO , et al
- DuPaul GJ ,
- Sayal K , et al
- Swanson JM ,
- Arnold LE ,
- Molina BSG , et al
- World Health Organization
- Huckstadt MR ,
- Burlaka I , et al
- Angkustsiri K ,
- Burlaka I ,
- Buskin S , et al
- Baumgaertel A
- Gross-Tsur V ,
- Kalish LA ,
- Bunce E , et al
- Bishop FL ,
- Yardley L ,
- Seshadri K ,
- Matthews TA , et al
- Torgerson D ,
- O'Cathain A , et al
- Peasgood T , et al
- Heirs M , et al
- ↵ Available: https://www.facebook.com/starsheffieldADHD/videos/677387002419685/
- Jensen PJ ,
- Richters JE , et al
- Shamseer L ,
- Hartling L , et al
- House of Lords Select Committee on Science and Technology
- Stevenson J ,
- Buitelaar J ,
- Cortese S , et al
- von Ammon K , et al
- Williams A-L ,
- Girard C , et al
- Strauss LC ,
- Dean ME , Cochrane Developmental, Psychosocial and Learning Problems Group
- Gopinadhan S ,
- Varanasi R , et al
- Stubberfield T ,
- Bussing R ,
- Gary FA , et al
- Rappaport LA ,
- Concannon PE ,
- Johnston C ,
- Hommersen P , et al
- Crismon ML ,
- Baumgartner J
- Kemper KJ ,
- Gardiner P ,
Contributors PF planned, conducted and analysed the survey and wrote the manuscript. CR helped design the research methodology and edit the manuscript.
Funding This work was supported by the Homeopathic Research Institute (Company Registration number 06230101; Charity Registration number 1132901), who had no role in the design, collection or analysis of data.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement Data are available on reasonable request. Data are stored using facilities provided by Google. Arrangement provided under contract with the University of Sheffield.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
New study on ADHD in adults with recurrent depression
6 January 2022

Researchers from the Wolfson Centre for Young People’s Mental Health have undertaken work to investigate the prevalence and impact of attention-deficit/hyperactivity disorder (ADHD) in recurrently depressed adult women.
The study, led by Dr Victoria Powell, found that 12.8% of women with a history of recurrent depression also had elevated ADHD symptoms. Additionally, a small percentage of the women sampled met the diagnostic criteria for ADHD, but none of the women had received a diagnosis of ADHD from a medical professional.
Dr Powell said: “In a sample of women in mid-life taken from a UK-based prospective cohort of adults with a history of recurrent depression, we investigated the prevalence of ADHD and the association of ADHD with clinical features of depression. “Those with attention-deficit/hyperactivity disorder may be at risk of a more chronic and impairing depression compared to those with depression alone according to studies of young people. However, no studies to date have examined ADHD in recurrently depressed adults in mid-life.

“In our study, higher ADHD symptoms appear to mark a worse clinical presentation for depression. Clinical implications include that in women with early-onset, impairing and recurrent depression, the possibility of underlying ADHD masked by depression needs to be considered.”
The study found that ADHD was associated with earlier onset, more impairing, and recurrent depression and that recurrently depressed women with elevated ADHD symptoms were more likely to be hospitalised than those without. The study also found that ADHD was associated with being on an antidepressant that is not a typical first choice antidepressant, suggesting that clinicians may have had difficulty finding an effective antidepressant medication for these women.
Dr Powell concluded: “We know those with ADHD can be at an increased risk of developing prolonged and impairing depression. This study is the first of its kind, with no studies to date, have examined ADHD and its impact on depression presentation in recurrently depressed adults in mid-life. The findings suggest that recurrent depression may in some cases mask ADHD symptoms in adult women.
“We hope that these findings will make a tangible difference in a clinical setting, particularly for women with recurrent depression that could potentially be masking underlying, undetected ADHD. I’m looking forward to continuing to work with colleagues here at the Wolfson Centre to undertake further studies that will have real-world implications and make a difference in the field of mental health research.”
The research paper, ADHD in adults with recurrent depression , is published in the Journal of Affective Disorders and is available to view online .
https://youtu.be/MA52qiPOJK0
Share this story
Related news.

Striding forward for youth mental health webinar
13 September 2021

Dr Victoria Powell
Research Associate, Division of Psychological Medicine and Clinical Neurosciences
The latest from Cardiff University.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Attention deficit...
Attention deficit/hyperactivity disorder (ADHD) in children: more focus on care and support, less on diagnosis
- Related content
- Peer review
- Luise Kazda , research fellow 1 2 3 ,
- Katy Bell , professor of clinical epidemiology 1 2 ,
- Rae Thomas , associate professor of evidence based healthcare and research education lead 2 4 5 ,
- Leah Hardiman , independent consumer representative 2 6 ,
- Iona Heath , former general practitioner 7 ,
- Alexandra Barratt , professor of public health 1 2
- 1 Sydney School of Public Health, Faculty of Medicine and Health, University of Sydney, NSW, Australia
- 2 Wiser Healthcare, Australia
- 3 NHMRC Healthy Environments and Lives (HEAL) National Research Network, Health Research Institute, University of Canberra, Canberra, ACT, Australia
- 4 Institute for Evidence Based Healthcare, Bond University, QLD, Australia
- 5 Tropical Australian Academic Health Centre, Townsville, QLD, Australia
- 6 Brisbane, QLD, Australia
- 7 London, UK
- Correspondence to: L Kazda Luise.Kazda{at}sydney.edu.au
ADHD diagnoses continue to increase, but Luise Kazda and colleagues argue that the push for diagnosis could be hampering access to care and support for children
Key messages
Diagnoses of attention deficit/hyperactivity disorder (ADHD) in children and adolescents have increased globally over the past 30 years
Diagnosing ADHD in children is assumed to result in better long term outcomes for them, but this is not well supported by evidence
Potential benefits of an ADHD diagnosis for access to interventions are often overemphasised in research and guideline development, whereas potential harms are generally overlooked
Providing symptom appropriate care and support for children with inattentive/hyperactive behaviours, regardless of diagnosis, might improve access to beneficial interventions while limiting harms from the diagnostic label
Robust studies on who is most likely to benefit, or be harmed, by an ADHD diagnosis are needed
The prevalence of attention deficit/hyperactivity disorder (ADHD) in children has been rising for several decades, 1 2 3 4 including in countries with previously low rates. 5 In Germany, for example, the prevalence of ADHD in children rose by 77% over 10 years, from 2.2% in 2004 to 3.8% in 2013. 6 Enhanced awareness of mental wellbeing and neurodiversity during the covid-19 pandemic has led to a change in public discourse around ADHD. 7 8
Highly viewed videos on social media describe a variety of ADHD symptoms and encourage viewers to seek diagnostic evaluation. 8 9 10 Many of the most highly viewed TikTok videos (the #adhd hashtag stands at over 30 billion views) are easy to understand and relatable, but most provide content created by non-healthcare professionals that is often misleading or wrong, 10 which can lead to “unrealistic expectations.” 8 Diagnosis of ADHD, however, depends on an assessment of the frequency and severity of hyperactive and inattentive behaviours that exist on a continuum and are often context specific ( box 1 ). 11 A 2022 analysis of two large Australian cohorts found that more than 26% of children with an ADHD diagnosis showed behaviours in the normal range in the months before diagnosis. 12 Regardless of hyperactive or inattentive behaviours, children born in 2004 were more likely to receive an ADHD diagnosis than those born four years earlier. 12 In general, higher rates of ADHD diagnosis do not seem to correspond with population based studies, which report generally stable, temporal trends in the prevalence of ADHD symptoms. 4 Rising rates of ADHD diagnosis without changes in behavioural symptom profiles suggest an epidemic of diagnosis, not an epidemic of ADHD.
Continuum of hyperactive and inattentive behaviours associated with ADHD
This categorisation is derived from the Diagnostic and Statistical Manual of Mental Disorders 5 , 11 which only provides categories for children that fulfil the minimum diagnostic criteria, not for those with symptoms below (or around) the threshold. We use it in the absence of an evidence based standard for judging severity of hyperactivity, impulsivity, and inattention. The thresholds between categories are subjective and context dependent—especially between “normal” and “borderline” behaviours. We propose a move away from the binary of “normal” versus ADHD behaviour.
“Normal” behaviours —Behaviours that are considered within normal limits (in local community and context), consistent with developmental level, and do not interfere with social or academic functioning
Borderline behaviours —Number of hyperactive/inattentive behaviours is just above or below diagnostic threshold and/or the behaviours only reduce level of social or academic functioning to a degree that results in negligible or minor impairments and/or are not persistent and/or only interfere with functioning in special, rare contexts. Some children in this category could fulfil the DSM-5 classification of mild ADHD, others might have symptoms below the official clinical threshold
Severe behaviours —Number of hyperactive/inattentive behaviours is more than the minimum required for diagnosis and/or (some of) the behaviours significantly interfere with social or academic functioning, resulting in marked impairment in more than one context. Children with these symptoms could fulfil the DSM-5 classification of moderate or severe ADHD.
Diagnoses and awareness are increasing in many high income countries in parallel with healthcare shortages. Waiting lists for psychiatric evaluations in countries such as the United Kingdom and Australia are long, 13 14 with some children having to wait years to be assessed in the public system. 15 Private clinics might have shorter wait times, but costs are high. 15 Gaining access to treatment and additional support—at school, for example—might help children with substantial and impairing hyperactive/inattentive behaviours. But for the increasingly large numbers of children with borderline behaviours ( box 1 ) who are seeking help, the focus on obtaining a diagnostic label could be causing net harm. An alternative approach is to provide targeted non-pharmaceutical interventions without the need for diagnosis and to provide more care and support to all children needing it.
Evidence for treatment is uncertain
A 2018 meta-analysis of 133 clinical trials in children and adolescents supports the short term efficacy of drug treatment (up to around 12 weeks) for ADHD symptoms in children. 16 It found that clinicians rated amphetamines, methylphenidate, and atomoxetine as beneficial for symptom control compared with placebo. Teachers rated methylphenidate and modafinil as beneficial. 16 But Cochrane reviews have questioned the quality of this evidence, 17 18 19 20 21 and other reviews have emphasised the scarcity of long term data. 16 22 The lack of high quality, long term evidence is apparent in clinical guidance—for example, the 2022 Australian Clinical Practice Guidelines for ADHD say that first line drug treatment is supported by only low quality evidence. 23 The benefit of treatment is even less clear for children with borderline symptoms, who have been under-represented in ADHD research. Of 334 studies in a 2021 scoping review of overdiagnosis of ADHD in children and adolescents, only five studies evaluated benefits and harms for children with borderline behaviours. 5
Medication is also offered as part of multimodal therapy, in combination with non-pharmacological interventions such as parent or family training or cognitive behavioural intervention. 19 But evidence on the effectiveness of combined treatments is inconsistent. 24 Australian guidelines mention this scarcity of direct evidence and recommend considering “availability, cost, preferences, and potential harms” in decision making. 23 One of the few large long term randomised controlled trials on the effects of combined treatments is the US Multimodal Treatment Study of ADHD, in which the effects of intensive medication management, behaviour modification therapy, combination of medication and behaviour management, or routine community care (often also medication) on ADHD symptoms were compared in 579 children. 25 The study initially ran as a randomised controlled trial over 14 months from 1992 to 1993, then continued as a longitudinal cohort study until 2013. ADHD symptoms improved in all children, with greater improvements in the intensive medication and combination treatment groups. 25 Combination treatment did not seem to provide additional benefits over medication alone. 25 Teacher rated inattentive symptoms (measured on inattention scale of SNAP-IV, range 0-3), for example, decreased with combination treatment from 2.16 (95% confidence interval 2.05 to 2.27) to 1.12 (0.99 to 1.25) and with medication from 2.27 (2.17 to 2.37) to 1.11 (0.97 to 1.25) at 14 months. 25 The superiority in symptom control with intensive medication or combination treatment diminished after the trial and was no longer observed by six years. 26 27 28 A mixed effects regression analysis of this cohort after six to eight years of follow-up found that severity of initial symptoms and socioeconomic status, but not type of treatment received, were the best predictors of long term outcomes. 27
Evidence on the potential harms of drug treatment for ADHD is also uncertain and mostly limited to short term follow-up. 19 20 29 30 There is moderate quality evidence from trials that ADHD drugs can lead to weight loss and sleep problems like insomnia in children. 29 Other reported adverse effects include decreased appetite or anorexia, abdominal pain, nausea or vomiting, tachycardia, tremors, and headaches. 19 20 29 Evidence on other adverse effects is often inconclusive (as with reduced or delayed growth 31 ), and although the relative risks might be higher, the effects are still rare in the short term (such as for seizures, psychotic symptoms, and cardiovascular events). 20 29 The effects of longer term drug use were recently examined in a large Swedish population based study. 32 Researchers found increased risks of hypertension and arterial disease associated with long term exposure to ADHD drugs.
Australian and UK guidelines additionally recommend non-pharmacological interventions, but the evidence base for these is also not strong. 23 33 Parent or family training that optimises parents’ behaviour management skills has low-to-moderate certainty evidence for improving hyperactivity and inattention among children under 5 years, 23 and cognitive behavioural therapy is supported by low certainty evidence. 23 Although research on the effects of non-pharmacological treatments is limited, these interventions are likely to have fewer harms than drugs. 33 As such, non-pharmacological interventions might be a lower risk option for children with milder symptom profiles.
Benefits and harms of ADHD diagnosis
Children with severe and impairing ADHD related behaviours might benefit from medication for symptom relief, and this (rightly) requires a diagnosis first. But diagnostic labels are themselves an intervention that might have both beneficial and harmful effects. 34 Diagnoses can guide actions, inform frameworks, and attribute rights. 35 Qualitative studies from high income settings indicate that an ADHD diagnosis can provide a sense of identity to children, relief to children and parents by providing an explanation for difficulties experienced, better understanding of oneself, and anticipation of support. 5 But the extent to which these findings are true for children in other settings and the duration of benefits beyond the time of diagnosis are difficult to ascertain.
Diagnostic labels can also be harmful. 36 37 A 2021 review found 29 primary studies that reported psychosocial harms—including perceptions of decreased ability to change and loss of control, self-fulfilling prophecy of failure, increased stigma, isolation, and exclusion—accompanying ADHD diagnosis in children. 5 One of these studies, a 2000-01 UK school based trial, screened 68 711 children aged 4-5 for ADHD symptoms and randomised schools to introduce either education (books about ADHD for teachers), identification (names of high scoring children were flagged with teachers), a combination of both, or no intervention. After five years, no improvement in outcomes was found for any group, but children in the identification group were twice as likely to have high parent reported scores for hyperactive/inattentive behaviours (odds ratio 2.11, 95% CI 1.12 to 4.00). 38 Evidence from observational studies indicates that an ADHD diagnosis does not protect children against adverse academic 39 or socioemotional outcomes 40 and has a negative effect on young adults’ ability to get and keep jobs. 41 A 2022 observational study of 746 Australian children used cohort data to emulate a randomised controlled trial. 42 43 Children with an ADHD diagnosis self-reported worse outcomes for academic self-concept, sense of school membership, self-efficacy, and negative social behaviours at age 14 years than their peers without diagnoses (matched for pre-diagnosis hyperactive/inattentive behaviour score, age, and sex). 42 They were more than twice as likely to self-harm. 42 As with any observational analysis, results could be influenced by unknown and unmeasured confounders. Nonetheless the findings are concerning.
Children with borderline symptoms might be at the greatest risk of experiencing net harm. In a 2017 US cohort study of 350 children, researchers found that those children with less severe ADHD related behaviours who had received an ADHD diagnosis (including those who had received medication) scored lower in reading and maths than their peers with similar levels of symptoms but without a diagnosis. 44 Limitations of this study include lack of verification of medical records, reliance on a short screening instrument for ADHD symptoms, and probable unmeasured confounders. Nevertheless, the findings are consistent with a hypothesis of diminishing returns, whereby the harms of diagnosis might outweigh the benefits for children with milder ADHD symptoms. 5
Focus on evidence and support, not on diagnosis
Evidence that all children given an ADHD diagnosis will benefit from the diagnosis is currently lacking. To improve the evidence base, we need well designed, pragmatic, randomised controlled trials and observational studies that evaluate the effects of a diagnosis (and any treatments offered) on wellbeing and long term outcomes.
An ADHD diagnosis is currently a gatekeeper to accessing both drug and non-drug treatment inside and outside the medical system in many jurisdictions. 35 As demand increases, the diagnostic process becomes a bottleneck, preventing timely interventions and adding to the stress experienced by families. Delays can add substantial out-of-pocket costs for people who seek out private providers, 15 who might be more likely to diagnose and treat ADHD than the public sector. 45
The status quo increases inequities in accessing care and threatens to deny or delay support to those who need it most but cannot afford to go outside the public system. It also puts children with borderline ADHD symptoms at highest risk of iatrogenic harm from diagnosis and drug treatment.
Educational and psychological interventions for children with hyperactive/inattentive behaviours and their families should focus on the child and not the diagnosis. A triage system could fast track children with severe and impairing behaviours, who might require pharmacological intervention, to be assessed by a clinician. Children with milder symptoms could be triaged to non-pharmacological interventions without a diagnosis . This would reduce the diagnosis bottleneck, providing a more agile response to children and their parents, while also avoiding harms from an unnecessary diagnostic label and drug treatment.
A stepped approach could be used with further treatments added sequentially as required. 46 Treatment might start with bibliotherapy for parents (targeted education), for example, progressing to group parenting education sessions, individual parent management training sessions, intensive behavioural intervention, and finally with diagnosis and medication if required. 46 Intervention pathways could be escalated and de-escalated in unbureaucratic ways that enable timely adjustments. Multidisciplinary teams in community health organisations or schools 47 could deliver psychological, behavioural, and case management services that focus on behaviours (rather than on diagnoses) to optimise children’s skills and functioning.
These approaches require community based, government funded organisations with the capability and capacity to deliver the initial triage assessment and non-pharmacological interventions without out-of-pocket costs to families. 15 School based systems might be one possibility, with teachers and a wide range of other specialists working together to support children. Such systems based approaches do not shift responsibilities but can facilitate access to a range of services and support by centring them around the child and family. They may require only modestly increased investments in education and, importantly, support hubs, but have the potential for high return on this investment. 48 This would especially benefit children and families from disadvantaged backgrounds, who might otherwise miss out on the care and support they need. 49
Complementary to the stepped approach is the need for truly inclusive educational environments that provide multi-tiered systems of support. These educational environments tackle the needs of all children, irrespective of their hyperactive/inattentive behaviours, without requiring a diagnosis. 50 An inclusive educational approach across three tiers of care and instruction starts by screening for children with a need for extra support and then sequentially introduces strategies for all students (tier 1; such as class-wide or school-wide behaviour rules and programmes), targeted interventions (tier 2; such as organisational skills training, daily report card), and finally, more intense individualised interventions (tier 3; such as parent training in behavioural management). 49 50
In Victoria, Australia, the Our Place initiative for children’s health and wellbeing has successfully followed a “place based approach to supporting the education, health, and development of all children and families in communities experiencing disadvantage by utilising the universal platform of a school,” bringing together a wide range of support services to meet children’s needs. 47 This initiative was initially funded through a modest AU$5m investment over ten years by a philanthropic foundation in partnership with the state government and service providers. The pilot site reported great success across a variety of domains, with improvements in student developmental vulnerabilities, health, behaviour and speech concerns, and absenteeism, while also improving student and parent engagement, motivation to learn, and academic achievements. 51 The programme has since been rolled out to more than ten other communities across Victoria. 52
Both stepped treatment and inclusive learning environments can be beneficial to all children as they cater for a continuum of behavioural needs. Regardless of diagnosis, all children with behaviours inhibiting their potential should be supported with effective interventions that have been co-designed and robustly evaluated. A tiered diagnostic process could allow those with severe and impairing symptoms to be prioritised for clinical assessment and possible diagnosis (with medication then offered if appropriate). For children without severe behaviours, a universal, diagnosis agnostic approach moves management away from binary thinking about “ADHD” versus “not-ADHD” behaviour and functioning. Such a move could both reduce overmedicalisation 53 and facilitate person centred support.
Contributors and sources: LK is an epidemiologist who recently completed a PhD candidature with a research focus on ADHD diagnosis trends and outcomes. KB is a clinical epidemiologist and health services researcher with expertise in the evaluation of the clinical effectiveness of health care. RT is a researcher-psychologist interested in improving evidence based decision making in clinical practice. LH is consumer representative who is passionate about translating evidence into practice for healthcare providers and consumers of health services. IH is a retired general practitioner in London and past president of the UK Royal College of General Practitioners with interests in medicalisation and justice in healthcare. AB is an epidemiologist recognised internationally as an expert in overdiagnosis research. All authors, apart from IH, are members of Wiser Healthcare, a research collaboration for reducing overdiagnosis and overtreatment. LK and AB developed the idea for this piece as part of discussions during PhD meetings. LK, KB, RT, and AB contributed to the initial conception of the work. All authors participated in developing the conceptual framework of the article and were involved in the design and analysis of the work. LK conducted the literature searches, drafted the first version of the manuscript, and is the guarantor. All authors revised it critically, provided important intellectual content, and approved the final version.
Patient involvement: LH, an experienced consumer representative with considerable expertise in maternal and child health services and in advocating for translation of evidence into practice for the benefit of consumers of health services, contributed as an author on this paper. Some authors have lived experience of ADHD.
Competing interests: We have read and understood BMJ policy on declaration of interests and have the following interests to declare: LK received a PhD scholarship from Wiser Healthcare (funded by the National Health and Medical Research Council (NHMRC) Program Grant 1113532 and CRE Grant 1104136). She now receives funding for her position from the NHMRC Special Initiative in Human Health and Environmental Change (Grant 2008937). KB receives funding from an NHMRC Investigator Grant 1174523.
- Dalsgaard S ,
- Nielsen HS ,
- Brault MC ,
- Davidovitch M ,
- Lundström S ,
- Gillberg C ,
- Lichtenstein P ,
- McGeechan K ,
- Langner I ,
- Scholle O ,
- Lindemann C ,
- Schröder C ,
- ↵ Monash Health. Pandemic triggers rise in ADHD referrals. 2021. https://monashhealth.org/latest-news/2021/12/20/pandemic-triggers-rise-in-adhd-referrals/
- ↵ Carter R. Patients harbouring ‘unrealistic expectations’ for ADHD diagnoses, doctors warn. AusDoc. 2023. https://www.ausdoc.com.au/news/tiktok-setting-unrealistic-expectations-for-adhd-diagnoses-doctors-warn/
- Abi-Jaoude E
- American Psychiatric Association
- ↵ Smith M. Is it really too easy to be diagnosed with ADHD? The Guardian 2023 17 May 2023. https://www.theguardian.com/commentisfree/2023/may/17/nhs-psychiatrist-adhd-underdiagnosis
- ↵ Kinsella E. Meet the Australians stuck waiting for mental healthcare as the pandemic takes its toll. ABC News. 2021. https://www.abc.net.au/news/2021-09-18/australia-mental-health-wait-times-covid-pandemic/100457162
- Asherson P ,
- Cortese S ,
- Del Giovane C ,
- Cândido RCF ,
- Menezes de Padua CA ,
- Junqueira DR
- Castells X ,
- Blanco-Silvente L ,
- Shamseer L ,
- Hartling L ,
- Storebø OJ ,
- Ramstad E ,
- Paludan-Müller AS ,
- Gøtzsche PC ,
- Jørgensen KJ
- Perroud N ,
- ↵ Australian ADHD Guideline Development Group. Australian evidence-based clinical practice guideline for attention deficit hyperactivity disorder (ADHD). 1st ed. Melbourne, Australia, 2022. https://adhdguideline.aadpa.com.au/
- ↵ National Institute for Health and Care Excellence. Attention deficit hyperactivity disorder: diagnosis and management. 2018. https://www.nice.org.uk/guidance/ng87
- The MTA Cooperative Group. Multimodal Treatment Study of Children with ADHD
- MTA Cooperative Group
- Molina BSG ,
- Hinshaw SP ,
- Swanson JM ,
- Arnold LE ,
- ↵ National Institute for Health and Care Excellence. Attention deficit hyperactivity disorder (update). [D] Evidence review for safety of pharmacological treatment. 2018. https://www.nice.org.uk/guidance/ng87/evidence/d-pharmacological-safety-pdf-4783686304
- ↵ Storebo OJ, Pedersen N, Ramstad E, et al. Methylphenidate for attention deficit hyperactivity disorder (ADHD) in children and adolescents - assessment of adverse events in non-randomised studies. Cochrane Database Syst Rev 2018;5:CD012069.
- Faraone SV ,
- Banaschewski T ,
- Coghill D ,
- ↵ National Guideline Centre. Attention deficit hyperactivity disorder (update) - Evidence review(s) for efficacy of nonpharmacological treatment and the impact of adverse events associated with nonpharmacological treatments of ADHD. NICE, 2018, NICE guideline NG87. https://www.nice.org.uk/guidance/ng87/evidence/e-nonpharmacological-efficacy-and-adverse-events-pdf-4783686305
- Michaleff ZA ,
- Glasziou P ,
- Vandvik PO ,
- Guidelines International Network (G-I-N) Preventing Overdiagnosis Working Group
- Glasziou PP
- Merrell C ,
- Metzger AN ,
- Hamilton LT
- O’Connor C ,
- McNicholas F
- Helgesson M ,
- Björkenstam E ,
- ↵ BMJ. The known unknowns of ADHD. https://www.youtube.com/live/mDoyg2L9v4g?si=XwZ3TDAH9MUQyPiY .
- Batstra L ,
- Nieweg EH ,
- Van Tol DG ,
- Hadders-Algra M
- ↵ Sahlberg P, Goldfeld S, Quach J, et al. Reinventing Australian schools for the better wellbeing, health and learning of every child. 2023. https://www.rch.org.au/uploadedFiles/Main/Content/ccchdev/2305_Reinventing-schools_Discussion-Paper.pdf
- ↵ Organisation for Economic Co-operation and Development. Investing in high-quality early childhood education and care (ECEC). https://www.oecd.org/education/school/48980282.pdf
- Fabiano GA ,
- ↵ Place O. Regenerating Doveton by investing in place. Jan 2020. https://ourplace.org.au/wp-content/uploads/2021/03/Our-Place-Regenerating-Doveton_Web.pdf
- Victoria Government

Help with our ADHD research
About this study.
At the National Centre for Mental Health (NCMH), we are trying to understand why some young people experience neurodevelopmental difficulties, such as Attention Deficit Hyperactivity Disorder (ADHD) or autism, and mental health problems, like depression or anxiety.
ADHD is a complex condition which can affect individuals in different ways. We are trying to understand more about ADHD and to help us do this, we are looking for volunteers to take part in research.
We need as many people as possible to take part –wherever you live in the UK.
Not much is known about what happens to children with neurodevelopmental and mental health difficulties as they get older. Linking the information you provide to other records will help us get an even better understanding of these difficulties now and improve treatment and support in the future.
To take part
If you are happy to take part in this study ple ase visit our online survey platform to ge t started.
What will I have to do?
If you decide to take part, we will ask you to provide us with some basic information about you, your child and their neurodevelopment and mental health in order to help us answer these important research questions.
The questions will ask about one child with an ADHD diagnosis. If you have more than one child with an ADHD diagnosis, the questionnaire can be completed multiple times.
Taking part is voluntary: it’s up to you to choose if you want to sign up.
If you join us, you’ll be asked whether you would be willing to:
- Provide us with your contact details (e.g. address, email address and phone number) and some personal information about you and your child (e.g. date of birth, ethnic group and employment status).
- Answer some questions about your child’s mental and physical health and lifestyle. This will take approximately 15-20 minutes.
- Allow us to contact you every 6-12 months, to invite you to provide more information about you and your child’s lifestyle, general health and mental health.
- Allow us to contact you in the future about other studies that you may want to take part in. There will be no obligation for you to take part in these future opportunities.
- Allow us to share anonymous information with other researchers if they have scientific and ethical approval for the questions that they would like to answer.
- To help make your participation even more valuable. We would like to link the information you have provided us with, to information that the NHS and other public organisations collect about you e.g. GP, hospital and education records.
Looking for more information first? We’ve put together the answers to some frequently asked questions.
This survey is led by the National Centre for Mental Health (NCMH). NCMH is a Welsh Government funded Research Centre, led by Cardiff, Swansea and Bangor Universities. It is being funded by Health and Care Research Wales, Welsh Government.
The Director of the National Centre for Mental Health is Professor Ian Jones.
You will have the opportunity to join the study once you have read through and understood the information.
We hope that learning more about neurodevelopmental and mental health difficulties will lead to new ways of diagnosing, treating or even preventing neurodevelopmental problems and mental illness. However, these remain long-term aims and you will not benefit directly from taking part in this study.
Only the study team will have access to your data and only they will contact you directly.
All information collected during the course of the research will be kept strictly confidential. There are strict laws that safeguard your privacy at every stage. In accordance with the General Data Protection Regulation (GDPR) and the Data Protection Act, you and your child’s personal information will be kept confidential by assigning a unique study code to the data.
Your name and identifying information about you or your child will not be passed on to anyone.
When you agree to take part and sign up, you will be asked to provide contact details and some other information about you and your child such as your age and ethnic group. You will also be asked to answer some questions about your child’s lifestyle, general health and mental health.
First, you need to join the study. This involves reading this information and then consenting below. This should take about five minutes. Take as much time as you need to decide whether you wish to take part.
Once you have joined, you will be asked some questions. This should take about 15-20 minutes to finish.
We know that we get the best data if you are able to complete these questions in one go, but if for some reason this isn’t possible then you can come back to the website later because you can save your answers once you have finished a set of questions.
We will also contact you every 6-12 months, to keep in touch and to ask you more questions about your child’s lifestyle, general health and mental health. We might ask you for information that you haven’t given before. Sometimes we will ask you the same questions as before so that we can see how things have changed.
As well as this regular contact, the study team may contact you from time to time, to ask if you would like to take part in new studies.
You may be contacted because you or your child have a specific condition (for example depression), or because of something that you have told us about (for example, your child’s age). These studies may be conducted by other research teams.
We will give you more information about these studies including why the research is being carried out, what you might be asked to do and how to sign up. It is up to you to decide whether you want to take part in these new studies.
You do not have to take part in this study.
If you do decide to take part you are still free to withdraw at any time without giving a reason.
If you decide to withdraw from this study, all details you have provided will be destroyed. These will not be used further in the research.
This is a long term study that will allow us to learn a lot about the causes and triggers of mental health and neurodevelopmental problems. The information you provide will be stored for use on a long term basis (at least 15 years).
You will not have any claim to any future commercial use of results from the study in which your data has been used.
To make the best use of resources we will share data (anonymised to exclude any personal details) with different groups of researchers from the NHS, universities and commercial companies, both within the UK and abroad. However, we would stress that those organizations will never obtain access to personal/ identifying information (for example, your name, address, date of birth).
Ethical approval has been obtained from the National Research Ethics Service and NHS (Research and Development) permission has also been obtained.
If you have further questions about the study please contact the study team:
National Centre for Mental Health
Cardiff University
Hadyn Ellis Building,
Maindy Road,
029 20688401
Yes, you can contact Dr Vanessa Davies on 029 2068 8340 or at [email protected] .
You can also write to her at:
Dr Vanessa Davies Institute Manager Neuroscience and Mental Health Research Institute 3rd Floor, Hadyn Ellis Building Maindy Road Cardiff CF24 4HQ
If you are happy to take part in this study please visit our online survey platform to get started.
Your javascript appears to be disabled
Please enable your javascript for an optimal viewing experience
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
ADHD articles from across Nature Portfolio
ADHD – attention deficit hyperactivity disorder – is a neurodevelopmental disorder that involves problems with attention, concentration and/or increased activity levels, resulting in problems with school, work and social situations. Individuals with ADHD also often experience trouble with impulse control.
Latest Research and Reviews
Discontinuation of psychotropic medication: a synthesis of evidence across medication classes.
- Christiaan H. Vinkers
- Ralph W. Kupka
- Jurjen J. Luykx
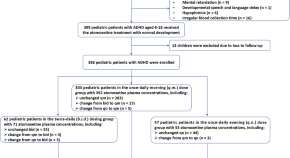
Individualized atomoxetine response and tolerability in children with ADHD receiving different dosage regimens: the need for CYP2D6 genotyping and therapeutic drug monitoring to dance together
- Hong-Li Guo

5-HT_FAsTR: a versatile, label-free, high-throughput, fluorescence-based microplate assay to quantify serotonin transport and release
- Lina Bukowski
- Markus Emanuel Strøm
- Steffen Sinning
Epigenome-wide association study identifies neonatal DNA methylation associated with two-year attention problems in children born very preterm
- Marie Camerota
- Barry M. Lester
- Todd M. Everson
ADHD medications use and risk of mortality and unintentional injuries: a population-based cohort study
- Helen-Maria Vasiliadis
- Carlotta Lunghi
- Alain Lesage
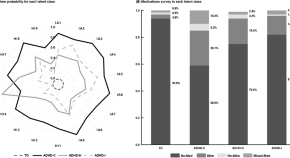
Stimulant medications in children with ADHD normalize the structure of brain regions associated with attention and reward
- Wenchao Zhang
News and Comment
Connecting clinical and genetic heterogeneity in ADHD
Understanding clinical heterogeneity in attention deficit hyperactivity disorder (ADHD) is important for improving personalized care and long-term outcomes. A study exploits the large scale and breadth of phenotyping of the iPSYCH cohort to link clinical heterogeneity to genetic heterogeneity in ADHD.
- Chloe X. Yap
- Jacob Gratten

Treatment dilemmas in childhood ADHD
Stimulants and α 2 -adrenergic agonists both improve symptoms of ADHD in preschool-age children, but they have different side effects.
- Karen O’Leary
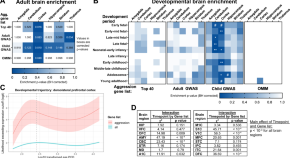
Leveraging aggression risk gene expression in the developing and adult human brain to guide future precision interventions
- Sarah L. Rader
- Alan S. Lewis
Molecular Psychiatry , August 2020: new impact factor, and highlights of recent advances in psychiatry, including an overview of the brain’s response to stress during infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)
- Julio Licinio
Polycystic ovarian syndrome and autism spectrum disorder in the offspring: Should the primary outcome have been different?
- Vikas Menon
- Chittaranjan Andrade
- Kandavel Thennarasu
First genetic risk loci for ADHD identified
- Charlotte Ridler

Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
ADHD medication can be lifesaving, scientists find

Medication used for ADHD can reduce the risk of premature death, says new research.
A study by Southampton scientists, with the Karolinska Institute in Sweden and Örebro University, Indiana University, and Bloomington in the USA, found the risk of dying from unnatural causes, such as accidents and overdoses, can be reduced by a quarter.
The report, published in JAMA, followed nearly 150,000 Swedes aged between six and 64 years old who were diagnosed with ADHD between 2007 and 2018.
Previous research has shown that people diagnosed with ADHD have an increased risk of premature death, however, it is not clear whether medications for ADHD affect this risk.
Researchers investigated the risk of death up to two years after diagnosis and compared those who started medication within three months of diagnosis – 56.7 per cent – with those who did not.
It showed that there is a link between initiation of medication and a lower risk of death.
Co-author Professor Samuele Cortese , an NIHR Research Professor and Professor of Child and Adolescent Psychiatry at Southampton, said the use of medications for ADHD is still controversial.
He added: “This study provides compelling data showing that ADHD medications reduce the risk of death due to unnatural causes.
“This study provides evidence useful to patients and clinicians when they need to decide as to whether a pharmacological treatment for ADHD should be used, taking into account expected benefits and possible risks.”
The risk of dying from unnatural causes was reduced by a quarter in the medicated group, the study reported.
Prof Cortese added: “As this is an observational study, it cannot establish a causal relationship, but the results suggest that early initiation of medication may be important for people with ADHD.
“At the same time, there are other health aspects to consider when prescribing these medications.”
In the next step, the scientists aim to further explore the long-term effects of ADHD medication.
The research team will also study the effects and mechanisms of different types of ADHD medications and how doses, duration of treatment and sex differences may affect them.
Read the study at jamanetwork.com/journals/jama/article-abstract/2816084 .
Articles that may also interest you
Study explores homeless women’s experiences of ‘period poverty’, understanding the relationship between our sleep, body clock and mental health, green space vital to student wellbeing during covid-19 pandemic.
ADHD Clinical Trials 2024
ADHD research studies recruiting patients in 2024 need your help. Receive premium care & cutting edge treatments by enrolling in ADD clinical trials today.
ADHD Clinical Trials
Here are the 6 most popular medical studies for adhd
Michael Bask Gill, B Sc
Last Reviewed: February 3rd, 2024
Behavioural Intervention
Video game therapy for adhd, this trial aims to assess if playing a video game called recollect can help to improve executive functioning in adults with adhd..
Cognitive Training for ADHD
This trial will test if a new computerized training intervention called central executive training (cet) can help improve symptoms for youth with adhd..
MRI for ADHD Treatment Response Prediction
This trial will test if certain brain markers can predict how well adults with adhd will respond to stimulant medications..
Methylphenidate compounds and /or Amphetamine compounds and/or Strattera or Guanfacine +1 More for Attention Deficit Hyperactivity Disorder (ADHD)
The purpose of this project is to evaluate the effectiveness of a structured aerobic exercise intervention for adults with attention-deficit/hyperactivity disorder (adhd) with and without medication and compare it to medication alone. participants will be randomly assigned to medication only + education, aerobic exercise intervention only, and combined aerobic exercise and medication groups. participants will be evaluated at baseline, following medication optimization (for medicated groups), following 8 weeks of intervention, after 3 months of follow-up, and after 6 months of follow-up. the investigators hypothesize that the combined group will have the best outcome at all evaluation points and that treatment gains will be maintained throughout the follow-up period if the assigned treatments are continued..
Behavioral Intervention
Motor attention training for adhd, this trial will test whether two interventions for adhd are feasible and effective in college students..
Central Nervous System Stimulant
Aptensio xr for attention deficit hyperactivity disorder (adhd), the primary objective of this study is to evaluate the long-term safety and tolerability of methylphenidate hydrochloride extended-release capsules (aptensio xr®) in children aged 4-5 years who have been diagnosed with attention-deficit/hyperactivity disorder (adhd). safety and tolerability will be evaluated by assessing treatment-emergent adverse events (teaes) blood pressure, pulse, height, weight, electrocardiograms (ecgs), laboratory the primary objective of this study is to evaluate the long-term (12-month) safety and tolerability of aptensio xr® in children aged 4 to less than 6 years who have been diagnosed with adhd. safety and tolerability will be evaluated by assessing treatment-emergent adverse events (teaes) blood pressure, pulse, height, weight, electrocardiograms (ecgs), laboratory values and columbia suicide severity rating scale (c-ssrs). disturbances in sleep (quantity and quality) patterns will also be assessed using the child sleep habits questionnaire (cshq). secondary objectives include assessment of long-term efficacy of aptensio xr®. secondary measures include: investigator administered attention-deficit/hyperactivity disorder rating scale preschool version (adhd-rs-iv preschool version) clinical global impressions-severity scale (cgi-s ) connors early childhood behavior-parent short form [conners ec beh-p(s)], popular filter options for adhd trials, attention deficit hyperactivity disorder (adhd) clinical trials.
View 82 Attention Deficit Hyperactivity Disorder (ADHD) medical studies.
Homeopathic Medicine
Individualized homeopathic medicine treatment +1 more for attention deficit hyperactivity disorder (adhd), this trial will explore if homeopathic treatment is an effective treatment for adhd, looking at the effects of homeopathic medicine, the homeopathic consultation, and an overall effect..
Cogmed Working Memory Training Program for Attention Deficit Hyperactivity Disorder (ADHD)
The overall objective of the current study is to determine whether computerized working memory (wm) training will enhance wm capacity in college students with attention deficit hyperactivity disorder (adhd). there are also four additional objectives. the first is to investigate whether the program's efficacy is impacted by the duration of the daily training sessions. the second is to determine whether improvements in wm will generalize to secondary outcome tasks, such as inhibitory control and planning. the third objective is to examine whether wm training will also ameliorate adhd symptoms of inattention and hyperactivity. the last objective is to investigate whether improvements will be maintained at a two month follow-up period. the investigators will also be assessing healthy control participants,who will not be receiving treatment, but will be used as a basis of comparison with the adhd participants, it is expected that the computerized wm training program will enhance wm capacity in college students with adhd. in addition, it is believed that these increases in wm capacity will also lead to improvements in other executive functions. it is also hypothesized that wm training will lead to a reduction in adhd symptomology. lastly, these improvements should be maintained at three month follow-up..
Corticosteroid
Atomoxetine for attention deficit hyperactivity disorder (adhd), the purpose of this study is to find out if children with attention-deficit, hyperactivity disorder (adhd) have a difference in how their brain cells "fire" or react. the investigators also want to find if brain cell "firing" can tell us how severe of symptoms a child has from adhd. finally, the investigators want to see if giving an adhd medication called atomoxetine can make the adhd symptoms in a child better and if the improvement shows a change in brain "firing"..
Cognitive Training
Cognitive remediation +1 more for attention deficit hyperactivity disorder (adhd), the objective of this study is to evaluate a novel sequenced combination of a promising, computerized cognitive training program targeting working memory (wm) deficits in children with attention-deficit/hyperactivity disorder (adhd) in combination with behavioral parent training, a well-established, evidence-based intervention for adhd. the combined active intervention, compared to the combined control intervention will result in improvement in primary psychosocial (i.e., parent/teacher reported child impairment; parental stress; parenting behavior; and observed child academic achievement) and psychiatric (parent/teacher rated adhd, odd, and cd symptoms; observed activity level and attention) outcomes at post-treatment and follow up assessment, with the combined active intervention resulting in greater improvements in these outcomes..
Behavioral contingency management +1 More for Attention Deficit Hyperactivity Disorder (ADHD)
Children with attention-deficit/hyperactivity disorder (adhd) comprise about 5-10% of the elementary school-age population. one place where children with adhd have great difficulty is in being accepted by peers and in making friends. it has unfortunately been very difficult for the field to find good treatments for peer relationship problems for this population. even when children with adhd do improve their behavior, it is common that peers do not seem to like the child with adhd any better. this may happen because children often have negative reputations with their classmates that are hard to change. that is, once a class of children get the impression that one child is disliked or the social outcast, even if that child's adhd symptoms get better, the peer group may not notice any of these improvements. it is hypothesized that the elementary school teacher may be able to help peers notice positive behavior changes in children with adhd when they do occur. this clinical trial will design and pilot-test an intervention that would train teachers in classroom practices to reduce the peer rejection of students with adhd. the pilot test will be conducted in a summer program created to be similar to a regular school classroom in structure. if the treatment seems to succeed in the summer program, then it will be tried in regular classrooms in a future study..
Shared Care for Attention Deficit Hyperactivity Disorder (ADHD)
Due to the shortage of child psychiatrists and the high prevalence of child mental health disorder, pediatricians and other pediatric primary care providers often assume responsibility for the management of various psychiatric disorders, including adhd, attention deficit hyperactivity disorder. however, pediatricians have not been well-trained during residency to deal with the complexities of adhd management. in addition, the system of care under which pediatricians practice do not afford the time availability that is required to properly manage a child with adhd. on the other hand, if a pediatrician wishes to refer a patient to a child mental health specialist, many obstacles, including but not limited to stigma, insurance issues, and long waiting lists, often interfere with the patient actually receiving services for his/her adhd. this research project seeks to examine an innovative model of care in which a child psychologist is located on the premises of a pediatric office and is available to share the care of patients with the pediatrician in order to address adhd. we hypothesize that parents as well as pediatricians will be more satisfied with this model of care and that patients will ultimately have better outcomes. the beginning of our pilot has shown under-identification to be a barrier to care as well, and thus we propose to implement a quality improvement initiative to screen children for psychosocial issues as well. as we have had trouble with recruitment and unfortunately have had more children randomized to tau than shared care, we propose in december 2007 a phase 2 of our study where all subjects, instead of randomization, are entered into shared care., attention deficit disorder clinical trials.
View 82 Attention Deficit Disorder medical studies.
Phase 3 Adhd Clinical Trials
View 84 phase 3 adhd medical studies.
ADHD Medication + Parent Training for ADHD Families
This trial will compare the effectiveness of treating adhd in children when their parent also has adhd, versus treating the child's adhd alone. they will also study the parents' adhd symptoms and how well they are able to engage in parent training..
Norepinephrine-Dopamine Reuptake Inhibitor
Centanafadine for adhd, this trial is to see if a new medicine for adhd is safe and tolerated by kids..
Centanafadine +1 More for Attention Deficit Hyperactivity Disorder (ADHD)
This trial will test how well centanafadine qd xr (a medication) works compared to placebo in treating children 4-12 years old with adhd..
CTx-1301 for Pediatric ADHD
This trial will study the efficacy and safety of a drug to treat adhd in children and teens aged 6-17..
Solriamfetol for ADHD
This trial tests if a drug is safe & effective for adults with adhd. results will show if it can help them concentrate & stay focused., adhd clinical trials with no placebo.
View 84 adhd medical studies that do not have a placebo group.
Methylphenidate Transdermal System for Attention Deficit Hyperactivity Disorder (ADHD)
Among children, attention-deficit/hyperactivity disorder (adhd) is associated with an increased risk for accidents, especially bicycle and pedestrian (leibson 2001; jensen 1988; discala 1998). anywhere from 40% to 80% of children diagnosed with adhd continue to display symptoms of the disorder into adolescence(barkley 1990; gittelman 1985). adolescents with adhd are also at an increased risk for driving-related accidents, being 2 to 4 times more likely to experience a motor vehicle accident (barkley 1993; barkley 1996; cox 2000), 4 times as likely to be at fault in the accident (barkley 1993), and over 3 times more likely to incur associated injuries as a result of the accident(murphy 1996). stimulant treatment with immediate-release methylphenidate (ir mph) has been demonstrated to improve driving performance in adolescents with adhd. hypothesis to be tested: main study: just as stimulant medication improves simulation and on-road driving performance of adhd teenagers, it is hypothesized that stimulant medication will improve routine driving performance. substudy - extended wear (15 hours) of daytrana will lead to safer driving late in the evening (22:00 and 01:00), when the most dangerous driving mishaps are most likely to occur, and the next morning at 09:00..
Mega Team - video game for ADHD, ASD, and CHD
This trial will test the effects of a cognitive-based video game intervention on children with neurodevelopmental disorders. the goal is to improve executive functioning, which includes abilities like regulating emotions, planning, and flexible thinking..
Tai Chi for ADHD in Children
This trialstudies if tai chi can help improve behavioral control in kids with adhd. results so far are promising., view more adhd trials.
See another 63 medical studies focused on adhd.
Long-acting stimulant
Placebo +2 More
Behavioral Parent Training (CLS Parent Group)
Adderall IR 10mg
Tolcapone +1 More
Cognitive training
Methylphenidate
Sprint Interval Training
Potassium Gluconate Oral Capsule
Tier 1 Classroom Management
Summer STRIPES
Transcranial Photobiomodulation
Fidget ball
Brainsonix Pulsar 1002
MATCH Protocol
Quillivant XR
SMS Intervention
Sensory-Play Based (SenPlay) Intervention
Intermittent Theta Burst Stimulation to the Left Dorsolateral Prefrontal Cortex
Mindfulness-Based ADHD Treatment for Children
Homework Organization and Planning Skills (HOPS) Intervention
Promoting Engagement with ADHD Pre-Kindergarteners (PEAK)
Cognitive-Behavioral Therapy Targeting Executive Dysfunction in College Students with ADHD
Central Executive Training (CET) +1 More
Methylphenidate Hydrochloride ER +2 More
Be Unstoppable in Life Together (BUILT)
2 mA transcranial direct current stimulation (tDCS)
Apollo System
Behavioral Parenting Intervention
Early Self-Regulation Intervention
Question prompt list +1 More
ADHD Therapy
SupporT for ADHD and Related Treatment
Serdexmethylphenidate (SDX) and dexmethylphenidate (d-MPH)
Placebo +1 More
Brief Parent Behavioral Intervention +1 More
Managing Challenging Behaviors in ADHD +1 More
Floreo Virtual Reality application +1 More
Formal mindfulness instruction +1 More
Flashed Light Therapy
Mobile Behavioral Parent Training
Mobile Behavioral Parent Training (mBPT)
El Faro Treatment Intervention
Daily Report Card +1 More
Amphetamine +2 More
Personalized ADHD Medication Experiment
UC-A +1 More
Team-Enhanced Collaborative Life Skills Program
Mindfulness Awareness Practices for ADHD (adapted)
View more adhd clinical trials
See more medical studies focusing on adhd
Frequently Asked Questions
Introduction to adhd
What are the top hospitals conducting adhd research.
In the realm of ADHD research and clinical trials, several hospitals have emerged as key players in advancing our understanding and treatment of this condition. Massachusetts General Hospital, located in Boston, leads the way with six ongoing ADHD trials and an impressive track record of 33 completed studies since their initial foray into ADHD research in 2001. Across the Atlantic, Hassman Research Institute based in Berlin has become a vital hub for ADHD trials as well. Though relatively new to the field with just four active trials and six overall studies since 2019, their dedication is undeniable.
Meanwhile, Alivation Research LLC located in Lincoln stands out with four active ADHD trials currently underway alongside seven previously conducted ones from their first recorded trial back in 2015. In Cincinnati's medical landscape, another institution making significant strides is Cincinnati Children's Hospital Medical Center where they boast involvement in four ongoing clinical tests alongside seventeen accomplished investigations dating back earlier to2003.The Seattle Children's Hospital also plays a crucial role within this sphere; while conducting three active ADHD trials at present it’s indeed noteworthy that theirs can be traced all the way back solely over eleven years ago to2009.
These hospitals signify not only breakthroughs but hope towards providing effective solutions for individuals affected by Attention Deficit Hyperactivity Disorder (ADHD). The collective efforts displayed among these leading institutions demonstrate unwavering commitment to unlocking greater insights into this neurodevelopmental disorder which affects millions worldwide. With each study undertaken comes potential advancements that could shape improved management strategies and brighter futures for those living with ADHD
Which are the best cities for adhd clinical trials?
When it comes to ADHD clinical trials, several cities have emerged as key players in the research field. Las Vegas, Nevada leads the pack with 12 active trials focusing on treatments like SPN-812 and Guanfacine hydrochloride (TAK-503). New york , New York follows closely behind with 10 ongoing studies examining therapies for adult ADHD patients such as centanafadine capsule. Boston, Massachusetts has 9 active trials investigating interventions like SMS Intervention and Solriamfetol 150 mg. Additionally, Cincinnati, Ohio is conducting 8 trials exploring treatments including Atomoxetine and Guanfacine hydrochloride (TAK-503), while Jacksonville, Florida offers 7 trials studying various ADHD therapies. These cities provide individuals with ADHD opportunities to participate in cutting-edge clinical research that could drive advancements in treatment options and improve quality of life.
Which are the top treatments for adhd being explored in clinical trials?
Exciting advancements are being made in the exploration of top treatments for ADHD through ongoing clinical trials. One notable intervention is SMS Intervention, which is currently being tested in three active trials and has a total of three ADHD trials since its initial listing in 2016. Additionally, there are two active trials investigating the effectiveness of ADHD Therapy, a treatment that entered the scene in 2023. Another intriguing avenue being explored is Tai Chi, with two active trials underway since its introduction to ADHD research in 2016. Finally, it's worth mentioning methylphenidate—a well-established player—which continues to show promise with two ongoing studies and an impressive track record of forty all -time ADHD trials dating back to 1998. As researchers delve deeper into these approaches, new possibilities may emerge for individuals affected by ADHD.
What are the most recent clinical trials for adhd?
Recent clinical trials have provided promising prospects for individuals with ADHD , offering potential advancements in treatment and care. Among these trials is the exploration of an experimental medication called CTx-1301, specifically a 37.5mg dexmethylphenidate tablet. The study aims to evaluate its efficacy in managing symptoms associated with ADHD, bringing hope to those seeking effective pharmaceutical interventions. Furthermore, another trial investigates the use of solriamfetol at a dose of 150 mg as a potential treatment option for ADHD patients. By delving into these innovative approaches through rigorous phases of testing, researchers aim to improve the lives and well-being of individuals living with this condition.
What adhd clinical trials were recently completed?
In the realm of ADHD research, recent clinical trials have reached significant milestones, bringing us closer to improved treatments for this neurodevelopmental disorder. In August 2021, Massachusetts General Hospital successfully completed a trial investigating the effectiveness of Solriamfetol 75 MG in managing ADHD symptoms. Similarly, Otsuka Pharmaceutical Development & Commercialization accomplished a trial testing Centanafadine in March 2021. These advancements highlight the commitment of researchers to finding novel solutions for individuals with ADHD and hold promise for enhancing their quality of life.
Other Trials to Consider
Centanafadine
Centanafadine (328.8 mg), pdc-1421 capsule, centanafadine capsule, centanafadine hydrochloride, solriamfetol 150 mg, guanfacine hydrochloride (tak-503), adapted mindful awareness practices (maps), mindfulness treatment, popular categories.
Autism Clinical Trials 2024
Bipolar Disorder Clinical Trials 2024
PMDD Clinical Trials 2024
Rexulti Clinical Trials
Seroquel Clinical Trials
Invega Clinical Trials
Spravato Clinical Trials
Latuda Clinical Trials
Lamictal Clinical Trials
Effexor Clinical Trials
Vraylar Clinical Trials
ECT Clinical Trials 2024
Systemic Juvenile Idiopathic Arthritis Clinical Trials
Scabies Clinical Trials 2023
Asd Clinical Trials 2023
Popular guides.
ADD/ADHD Online Information

2024 Award Application Forms Now Available
CHADD's Young Scientist Research Awards program recognizes researchers new to the ADHD field who are making contributions to the understanding of ADHD. Through the program, CHADD supports two researchers with:
- an unrestricted cash award of $1,000 each
- recognition in CHADD’s Attention magazine with a bio and summary of research submission
- recognition at the Annual International Conference on ADHD
- an allowance to cover most conference-related expenses (travel, hotel, registration)
- a one-year CHADD professional membership
- publicity through CHADD's social media posts and ADHD Weekly newsletter
- a description of the scientist's bio and research posted on the CHADD website
Applicants must be in the process of completing a doctoral degree (PhD, MD, DDS, or the equivalent) or must have completed such a degree or a clinical residency training within the last three years. Research may address any area relevant to ADHD, including, but not limited to: biological/genetic underpinnings of the disorder; treatment efficacy; impact on the individual or family; school or workplace accommodations; social stigma and discrimination; public health; and epidemiology.
The awards are supported through a number of individual donations. CHADD is grateful to all contributors to the Young Scientist Research Awards.
Information and application forms for the 2024 Young Scientist Research Awards can be downloaded here:
- General Information
- Application Form
- Recommendation Form
- Recipient's Agreement
- Application Check List
Applications are due on April 2, 2024.
If you have any questions regarding the Young Scientist Research Awards, please send an email to [email protected] or contact Rachel James at 301-306-7070, ext. 132.
Congratulations to all our Award Recipients!
Research studies, participate in a study.
Evidence-based research is at the foundation of CHADD's efforts to improve the lives of individuals affected by ADHD. CHADD is committed to supporting researchers who study the many facets of ADHD. Researchers often seek human subjects to participate in these studies as they learn more about ADHD's diagnosis, treatment, and its implications across the lifespan for children, adults and families.
As a service to CHADD members and the general public, CHADD is happy to provide this list for those who wish to participate in a research study. This list is not a comprehensive list of all studies . In each case, the researcher conducting the study has requested to be listed here, and the studies listed have been approved by CHADD's Professional Advisory Board.
To learn more about participating in research studies and clinical trials see The Center for Information and Study on Clinical Research Participation (CISCRP)'s Education Center , or the U.S. Food and Drug Administration (FDA)'s Clinical Trials: What Patients Need to Know .
RECENT STUDIES
U.s. web design system research study, interview/focus group study on resilience in neurodivergence, adhd identity development research study, black mothers’ adhd experiences, attitudes, and support-seeking decisions, special education rights survey, couples as parents study, post a study.
Research Study Guidelines (Revised October 2013)
CHADD's Professional Advisory Board Research Subcommittee must approve all requests from researchers seeking to recruit study participants through CHADD. This approval is required both for studies requesting to be posted on the CHADD Web site, as well as studies requesting to seek participants through a CHADD Local Chapter.
The following criteria will be used to determine if CHADD will approve such requests:
- Proposed study has scientific integrity and is directly related to advancing the body of knowledge regarding ADHD.
- Proposed study does not harm the mission of CHADD.
- If proposed study is federally funded or funded through a private, non-profit foundation, approved requests will be permitted at no charge.
- If proposed study is funded by source other than federal government or private non-profit foundation, approved requests will be charged an administrative fee of $100.
Note: CHADD is unable to consider for review research proposals that are undertaken independently and without institutional affiliation.
Requests to post research studies must contain the following:
- Purpose of the study;
- Methodology;
- Funding type (government, non-profit, for-profit) and source;
- Date after which new study participants will no longer be accepted;
- Contact name, with email address and/or phone number.
- Letter of approval from Institutional Review Board (IRB) for the Protection of Human Subjects.
- Curriculum vitae of investigator(s).
Scan all requested documents above into one pdf file and email to [email protected] .
If you have any questions please send an email to [email protected] or contact Rachel James at 1-301-306-7070, ext. 132.
- Visit the NRC on Social Media
The information provided by CHADD’s National Resource Center on ADHD is supported by Cooperative Agreement Number NU38DD000002 funded by the Centers for Disease Control and Prevention (CDC). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC or the Department of Health and Human Services (HHS).

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Science News
- Meetings and Events
- Social Media
- Press Resources
- Email Updates
- Innovation Speaker Series
NIH Researchers Identify Brain Connections Associated With ADHD in Youth
Large study finds atypical interactions between the frontal cortex and information processing centers deep in the brain
March 13, 2024 • Media Advisory
Researchers at the National Institutes of Health (NIH) have discovered that symptoms of attention-deficit/hyperactivity disorder (ADHD) are tied to atypical interactions between the brain’s frontal cortex and information processing centers deep in the brain. The researchers examined more than 10,000 functional brain images of youth with ADHD and published their results in the American Journal of Psychiatry . The study was led by researchers at NIH’s National Institute of Mental Health (NIMH) and National Human Genome Research Institute.
Luke Norman, Ph.D., a staff scientist in the NIMH Office of the Clinical Director, and colleagues analyzed brain images supplied by more than 8,000 youth with and without ADHD sourced from six different functional imaging datasets. Using these images, the researchers examined associations between functional brain connectivity and ADHD symptoms.
They found that youth with ADHD had heightened connectivity between structures deep in the brain involved in learning, movement, reward, and emotion (caudate, putamen, and nucleus accumbens seeds) and structures in the frontal area of the brain involved in attention and control of unwanted behaviors (superior temporal gyri, insula, inferior parietal lobe, and inferior frontal gyri).
While neuroscience researchers have long suspected that ADHD symptoms result from atypical interactions between the frontal cortex and these deep information-processing brain structures, studies testing this model have returned mixed findings, possibly due to the small nature of the studies, with only 100 or so subjects. Researchers suggest that the smaller studies may not have been able to reliably detect the brain interactions leading to the complex behaviors seen in ADHD.
The findings from this study help further our understanding of the brain processes contributing to ADHD symptoms—information that can help inform clinically relevant research and advancements.
Luke Norman, Ph.D., staff scientist in the NIMH Office of the Clinical Director and lead author of the paper
Norman, L. J., Sudre, G., Price, J., & Shaw, P. (2024). Subcortico-cortical dysconnectivity in ADHD: A voxel-wise mega-analysis across multiple cohorts. American Journal of Psychiatry . https://ajp.psychiatryonline.org/doi/10.1176/appi.ajp.20230026
About the National Institute of Mental Health (NIMH): The mission of the NIMH is to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery and cure. For more information, visit the NIMH website .
About the National Institutes of Health (NIH) : NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit the NIH website .
NIH…Turning Discovery Into Health ®
Is Seafood Good for Your Brain?
Fish and seafood are called brain food for good reason. Research suggests that improved memory is just one of many brain-boosting benefits associated with eating more fish and seafood, a dietitian explains.
This article is based on reporting that features expert sources.
Brain Health Benefits of Seafood

Getty Images
Rumor has it that one of the oldest known recipes in the Mediterranean – found in "Deipnosophistae" by the ancient Greek Athenaeus – is a recipe for fish ( grilled fish sprinkled with grated cheese). For millennia, seafood has played an important role in Mediterranean cuisine, health and culture. In fact, nutrition research over the last 20 years has revealed the increasing importance of including fish and seafood in an overall healthy diet . This was evident when a nutrition science panel met in 2008 to update Oldways’ original Mediterranean Diet Pyramid.
“One of the most notable updates was to make fish and seafood more prominent on the Mediterranean diet pyramid,” explains Oldways President Sara Baer-Sinnott.
Today, nutrition researchers recognize seafood as a staple food group in brain-healthy diets like the MIND diet and the Mediterranean diet. But what exactly does the research us about the link between seafood, cognition, mood and brain structure?
Omega-3s for Brain Health
DHA, or docosahexaenoic acid, is an omega-3 fatty acid that is a building block of our brain. In other words, just as calcium is to our bones, DHA is to our brains.
“The foods we eat become who we are by changing the composition of our brains,” explains Dr. Joseph Hibbeln, an omega-3 expert, psychiatrist and the Benjamin Meeker Distinguished Visiting Professor at the University of Bristol in the UK.
Seafood is the main source of DHA in the diet, so it’s not surprising that scientists are making note of links between eating seafood and brain health. Seafood also contains protein, essential vitamins and minerals, and EPA, or eicosapentaenoic acid, another type of omega-3 fatty acid that supports brain health.
A body of research has found that EPA and DHA reduce small proteins in the brain that promote inflammation and are associated with depression, Alzheimer’s disease and cognitive decline. Another study , in the American Journal of Preventive Medicine, found that people who regularly eat fish have more voluminous brains than those who do not. This study found that eating fish – baked or broiled – is associated with larger gray matter volumes in brain areas responsible for memory and cognition in healthy elderly people.
Eating fish at least twice a week may shield delicate blood vessels in the brain from subtle damage that can lead to mild cognitive impairment, dementia or stroke, according to research published in Neurology in 2021, adding to the growing evidence that seafood supports brain health.
Omega-3 levels can be measured in the body as a marker of how much seafood and/or omega-3 supplements people consume.
“Higher levels of omega-3 measured in plasma or red blood cells are associated with lower risk for developing Alzheimer’s and dementia ,” explains William Harris, president of the Fatty Acid Research Institute. His research quantifies these relationships in large cohort studies . While there hasn’t yet been a large randomized-controlled trial measuring seafood intake or omega-3 fatty acid intake as a way to prevent dementia , Harris explains that at this point, given the consistency of the evidence, “to withhold omega-3 fatty acids would not be ethical in a randomized controlled trial.”
Mental Health Benefits of Seafood
“The most pressing and immediate thing in peoples live is the behaviors and emotions that emerge when brain is deficient and critical nutrients,” says Hibbeln. In other words, keeping our brains nourished is just as important for our mental health as it is for our cognitive health.
An analysis of double-blind randomized controlled trials encompassing more than 10,000 patients across 35 studies found that giving patients EPA-predominant omega-3 fatty acids was able to produce significant clinical effects that were, in some cases, greater than what you would see from antidepressant medications .
Nearly 20 years ago, the American Psychiatric Association concluded that omega-3 fatty acids EPA and DHA have a protective effect in mood disorders like major depressive disorder and bipolar disorder . And yet still today, Hibbeln says that “the mental health benefits of omega-3 fatty acids are underknown, underutilized and under implemented” within the greater medical community.
Mercury Concerns
The Dietary Guidelines for Americans recommend that adults eat at least 8 ounces of seafood per week, but emphasize that pregnant or breastfeeding individuals should not exceed 12 ounces per week of a variety of seafood from choices that are lower in methylmercury. However, in the more than 20 years since cautionary advice on mercury and seafood was first issued in the U.S., dozens of studies have started to paint a more nuanced picture of this relationship.
Methylmercury was recognized as a neurotoxin when dangerously high levels from industrial contamination events in the 20th century were linked to overt, damaging effects on the brain and nervous system, particularly in young children. While overt harm from extreme exposures have not been reported again, considerable research has been conducted since then to better understand the relationship between seafood consumption during pregnancy, exposure from normal background levels of methylmercury in that seafood and neurodevelopment in children.
Over 30 such studies have now analyzed data from more than 200,000 mother-child pairs . The studies have found little evidence of harm to neurodevelopment associated with that consumption. Instead, the research points to over 50 incidences of benefits to children’s neurodevelopment, including improvements to IQ, from the women’s consumption of seafood as compared to children whose mothers ate less or no seafood during pregnancy.
In other words, the benefits of eating seafood outweigh any potential risks.
“What we see consistently in those studies is that over 12 ounces per week tends to be better than under 12 (ounces per week),” says Philip Spiller, former director of the then-Office of Seafood within the United States Food and Drug Administration and lead author of a recently published study that analyzed the research results. “The evidence is robust enough that messaging to pregnant women should emphasize the likelihood of benefits to their children’s neurodevelopment, that more is better than less, and should no longer emphasize cautionary behavior to avoid risk that the studies have not found.”
As it stands, nearly 90% of Americans are falling short of recommended seafood amounts according to the Dietary Guidelines for Americans.
“If you obsess on mercury you’re missing the big picture,” says Tom Brenna, PhD, professor of pediatrics, of chemistry, and of nutrition at the Dell Medical School and the College of Natural Sciences at the University of Texas at Austin, and Professor Emeritus at Cornell University. “The studies overall show great benefit, so the risk is not eating enough seafood.”
Buying and Cooking Seafood
Seafood cooks quicker than chicken, and yet this brain-healthy food group is surprisingly underutilized in home kitchens. At the supermarket, seafood can be found in fresh, frozen and canned forms – all of which can be used in delicious and nutritious meals. For people who are new to seafood, or any food for that matter, remember that taste preferences aren’t set in stone. Making an effort to try seafood often and in different forms is a great way to nurture a taste for this popular protein source.
When identifying seafood options higher in omega-3 content, Harris suggests remembering the acronym SMASH, which stands for salmon, mackerel, anchovies, sardines and herring. “Twice a week, eat a meal with one of these,” recommends Harris, noting that salmon is one of his go-to choices.
Baer-Sinnott suggests taking a cue from heritage diets, like the Mediterranean diet , to experience how seafood fits into healthy eating patterns rooted in tradition and culture. “Eating fish and seafood twice a week is good for your health and it is also easy and delicious,” says Baer-Sinnott. “With all of this evidence, why wouldn’t you?”
“Pick a fillet, throw some olive oil right in the pan and cook it a little bit on each side. Don’t overthink it,” assures Brenna. A sea of culinary possibility awaits.
7 Signs of Vitamin B12 Deficiency

The U.S. News Health team delivers accurate information about health, nutrition and fitness, as well as in-depth medical condition guides. All of our stories rely on multiple, independent sources and experts in the field, such as medical doctors and licensed nutritionists. To learn more about how we keep our content accurate and trustworthy, read our editorial guidelines .
Baer-Sinnott is president of Oldways, a nonprofit food and nutrition organization helping people live healthier, happier lives through cultural food traditions and lifestyles.
Brenna is a professor of pediatrics at Dell Medical School at the University of Texas in Austin. He is a former professor of human nutrition, chemistry, chemical biology and food science at Cornell University in Ithaca, New York.
Harris is president of the Fatty Acid Research Institute in South Dakota. He is also founder of OmegaQuant Analytics, LLC and the developer of the Omega-3 Index blood test.
Hibbeln is a board-certified psychiatrist, a nutritional neuroscientist, omega-3 expert and the Benjamin Meeker Distinguished Visiting Professor at the University of Bristol, UK.
Spiller is the former director of the Office of Seafood for the Center for Food Safety and Applied Nutrition, U.S. Food and Drug Administration.
Tags: brain health , diet and nutrition , food and drink
Most Popular

health disclaimer »
Disclaimer and a note about your health », you may also like, eggs: health benefits and recipes.
Janet Helm March 22, 2024

Best Anti-Cancer Foods
Ruben Castaneda and Heidi Godman March 22, 2024

Colon Cancer Diet
Ruben Castaneda and Shanley Chien March 20, 2024
Health Benefits and Recipes for Beans
Janet Helm March 15, 2024

Worst Foods for Gut Health
Ruben Castaneda and Elaine K. Howley March 12, 2024

Best Foods for Gut Health

Is Mushroom Coffee Good for You?
Keri Gans March 11, 2024
6 to 1 Grocery Shopping Method
Toby Amidor March 11, 2024
12 Best Superfoods for Older Adults
Christine Comizio and Elaine K. Howley March 7, 2024

Best Frozen Meals
Joan Salge Blake March 6, 2024

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

ADHD: Reviewing the Causes and Evaluating Solutions
Luis núñez-jaramillo.
1 División de Ciencias de la Salud, Universidad de Quintana Roo, Chetumal 77039, Quintana Roo, Mexico; xm.ude.oorqu@zenunl
Andrea Herrera-Solís
2 Laboratorio Efectos Terapéuticos de los Canabinoides, Subdirección de Investigación Biomédica, Hospital General Dr. Manuel Gea González, Calz. de Tlalpan 4800, Belisario Domínguez Secc 16, Tlalpan 14080, Ciudad de México, Mexico; moc.liamg@shaerdnaard
Wendy Verónica Herrera-Morales
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder in which patients present inattention, hyperactivity, and impulsivity. The etiology of this condition is diverse, including environmental factors and the presence of variants of some genes. However, a great diversity exists among patients regarding the presence of these ADHD-associated factors. Moreover, there are variations in the reported neurophysiological correlates of ADHD. ADHD is often treated pharmacologically, producing an improvement in symptomatology, albeit there are patients who are refractory to the main pharmacological treatments or present side effects to these drugs, highlighting the importance of developing other therapeutic options. Different non-pharmacological treatments are in this review addressed, finding diverse results regarding efficacy. Altogether, ADHD is associated with different etiologies, all of them producing changes in brain development, leading to the characteristic symptomatology of this condition. Given the heterogeneous etiology of ADHD, discussion is presented about the convenience of personalizing ADHD treatment, whether pharmacological or non-pharmacological, to reach an optimum effect in the majority of patients. Approaches to personalizing both pharmacological therapy and neurofeedback are presented.
1. Introduction
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder (NDD) presenting with inattention, hyperactivity, and impulsivity. It can be classified in three subtypes, depending on the intensity of the symptoms: predominantly inattentive, predominantly hyperactive–impulsive, and combined [ 1 , 2 ]. ADHD has a global prevalence of 5.9% to 7.1% in children and 1.2% to 7.3% in adults [ 3 ].
While most studies address ADHD in children from 7 to 17 years old, it is important to outline that this condition is also present in adults. It has been proposed that the number of adults with ADHD has increased over the last 20 years. A part of this increase is due to the permanence of ADHD symptoms in the adult age in 76% of diagnosed patients. ADHD implies important challenges for academic, personal, and job performance [ 4 ].
As for any other condition affecting brain function, in order to find an adequate treatment for ADHD, it is important to first understand its physiological basis. As with other NDDs, the causes of ADHD are aberrant neural development, affecting neurogenesis, synaptogenesis, myelination, and neuronal and glial proliferation and migration. Even though symptoms begin to appear in childhood, neuronal development is affected from early embryogenesis [ 5 ].
The etiology of ADHD is diverse—gestational, perinatal, and genetic factors have been associated with ADHD incidence. However, each patient presents only a few of them.
2. Environmental Factors Associated with ADHD
The incidence of ADHD is associated with a number of environmental factors during different stages of central nervous system (CNS) development, such as gestational and perinatal periods. In this section, we will address some of the environmental factors that have been associated with ADHD.
2.1. Preconceptional, Gestational, and Perinatal Conditions
Premature birth is an important risk factor for ADHD, since it has been reported that it occurs 2.6 to 4 times more frequently in babies born with low weight or very low weight. Premature birth is associated with alterations in neurogenesis and cell death [ 6 ], and these are in turn associated with reduced cortical expansion, as reported in ADHD patients [ 7 ]. One possible reason for increased risk of developing ADHD in preterm children is inflammation; an increase in inflammation-related molecules is associated with increased risk of developing ADHD symptoms [ 8 ].
Perinatal hypoxia is an environmental factor that increases the risk of developing AHDH, probably due to its effects on dopaminergic transmission and neurotropic signaling [ 9 ].
The intake of nutrients during gestation is very important for proper brain development. An important element during neural development is the polyunsaturated fatty acid docosahexaenoic acid (DHA), promoting proliferation and neural differentiation of neural progenitor cells. Decreased levels of DHA during brain development have been associated with ADHD and other neurodevelopmental disorders [ 10 ], and decreased levels of serum DHA levels have been reported in adult ADHD patients [ 11 ]. Additionally, malnutrition or immune activation in the pregnant mother is a risk factor for ADHD and other neurodevelopmental disorders [ 12 ]. High sucrose consumption during pregnancy is possibly related with ADHD incidence. A study performed on rats reported that high sucrose intake in pregnant rats led to the appearance of ADHD-like symptoms in the offspring, who showed increased locomotor activity, decreased attention, and increased impulsivity. Furthermore, the offspring also presented increased dopamine transporter (DAT) and a decrease in dopamine receptors and mRNA expression in the striatum [ 13 ].
Interestingly, there is evidence in a rat model of the influence of preconceptional conditions on ADHD incidence. Offspring of Female rats administered with ethanol for 8 weeks before mating presented ADHD-like symptoms such as hyperlocomotive activity, impulsivity, and attention deficit. These rats also presented low levels of striatal DAT and increased presence of norepinephrine transporter (NET) in the frontal cortex [ 14 ]. A later work by this group revealed that paternal preconceptional alcohol exposure also produced ADHD-like symptoms in the offspring, presenting decreased expression of DAT mRNA and DAT protein in the cortex and striatum. Furthermore, authors report epigenetic changes in both the sperm of these alcohol-exposed male rats and in the frontal cortex and striatum of the offspring, presenting increased methylation in a CpG region of DAT gene promoter, which is in agreement with the reduced expression of DAT in the offspring [ 15 ].
Another environmental factor associated with ADHD is pesticide exposure during development. A study addressing the issue, both at experimental and epidemiological levels, reported that exposure to the pesticide deltamethrin during gestation and lactation in rats led to ADHD-like symptoms, such as working memory and attention deficits, hyperactivity, and impulsive-like behavior. It also produced increased presence of DAT and D1 receptor in the striatum, as well as increased dopamine release and increased presence of D1 dopamine receptor in the nucleus accumbens. Interestingly, the authors also performed an epidemiological study in humans, revealing that children (6 to 15 years old) with detectable levels of pyrethroid metabolites in urine had more than twice the probability of being diagnosed with ADHD [ 16 ].
2.2. Heavy Metal Exposure
One of the most reported environmental factors associated with ADHD is exposure to neurotoxic heavy metals. A study performed on school children revealed that children (6–7 years old) with ADHD presented higher levels of salivary mercury. However, when including all age groups studied (12–13 years and 15–16 years), no significant correlation was found between increased salivary mercury and ADHD, although a mild tendency was observed [ 17 ].
In the case of manganese, both too high and too low blood levels are associated with cognitive deficits. High concentration of manganese in blood is associated with deficits in thinking, reading, and calculations, as well as with lower learning quotient (indicative of learning disability) and more errors in the continuous performance test (measuring attention and response inhibition). Conversely, low blood level of manganese is associated with a poorer performance in the Stroop test, which is used to assess cognitive inhibition [ 18 ]. Similarly, a study addressing the relationship between manganese in drinking water and ADHD found a higher risk of developing this condition (inattentive but not combined subtype) as exposure to manganese in drinking water increased [ 19 ]. However, a study on manganese in children’s deciduous teeth failed to find an association between this metal and cognitive deficits [ 20 ].
The presence of lead in children’s deciduous teeth is positively associated with hyperactivity or impulsivity, as well as inattention and oppositional or defiant disorder [ 20 ]. A study on children from a lead-contaminated region reported that blood levels of cadmium, lead, and manganese correlated with conduct problems and antisocial behavior [ 21 ]. Another work found a higher concentration of blood lead in ADHD children, which was correlated with hyperactivity–impulsivity symptoms but not with inattention [ 22 , 23 ]. Both genetic [ 24 ] and epigenetic [ 25 ] factors have been reported to contribute to lead-related pathogenesis of ADHD. Moreover, a study carried out in Argentina found that children with high blood concentrations of lead are more likely to develop ADHD [ 26 ].
A review on the effects of prenatal and childhood metal exposure on cognition found suggestive evidence of a relation between cadmium exposure and impaired cognitive ability in children. They did not find evidence of a relationship between cadmium exposure and ADHD [ 27 ]. A more recent study addressing cadmium exposure during pregnancy revealed that a higher blood cadmium concentration during pregnancy is associated with higher scores in ADHD diagnostic tests in female children at 6 years of age, but not in the case of male children [ 28 ].
A recently published work reported that ADHD children present higher urine concentrations of chromium, manganese, cobalt, nickel, copper, molybdenum, tin, barium, and lead [ 29 ]. A recent study analyzing serum concentrations of different metals in ADHD children reported low levels of chromium, manganese, and zinc, as well as increased copper/zinc ratios in these children [ 30 ]. A meta-analysis on the relation between blood and hair zinc and ADHD found no statistical difference between ADHD and control children [ 31 ].
Thus, there are a number of environmental factors associated with ADHD incidence. While environmental factors are not found in all ADHD cases, the data reviewed herein highlight the importance of environment in different developmental stages—and even before conception—in regard to the risk of developing ADHD.
3. Sleep Disorders and ADHD
Sleep deprivation, either acute or chronic, produces decreased cognitive functioning (one of the main traits of ADHD). Interestingly, it also produces the externalizing symptoms observed in ADHD patients. For example, a very tired child might become hyperactive, while in a sleepy adult in a condition where it is not possible to sleep (for example, while driving), the externalizing behavior will help them to remain awake. Thus, both of the core ADHD symptoms can be produced by sleep deprivation. Conversely, hyperactivity in children or high internal activity in adults in the evening might lead to sleep disruption [ 32 ].
Among the sleep disorders found in ADHD patients are delayed sleep phase disorders, insomnia, sleep-disordered breathing, increased motor activity during the night, sleep anxiety, clenching teeth, periodic limb movement, restless legs, increased sleep onset latency and shorter sleep time, night awakenings, narcolepsy, and parasomnias [ 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 ]. Among them, delayed sleep phase disorder is one of the most frequently found, being present in 73–78% of both ADHD children and adults. This condition consists of a delay between the sleep propensity cycle and the circadian cycle, leading to increased daytime sleepiness and decreased cognitive functioning [ 32 ].
Sleep disturbance have an impact on daytime vigilance, producing excessive sleepiness [ 32 , 37 , 39 ], and can exacerbate inattention, impulsivity, and hyperactivity as means to remain awake [ 32 , 37 ]. Additionally, stimulant medication might also cause sleep disturbances, although OROS methylphenidate produces less adverse effects on sleep [ 34 , 36 ]. LDX, a stimulant prodrug that undergoes hydrolysis in the bloodstream releasing d-amphetamine, and atomoxetine, a non-stimulant pharmacological treatment for ADHD, do not produce adverse effects on sleep [ 36 ].
Sleep disturbances in ADHD patients can produce significant impairments in attention, mood, and behavior [ 32 , 35 ]. Physiologically, there is evidence supporting an overlap between brain centers regulating sleep and those regulating attention and arousal, so it is possible that affectation of one of these systems also affects the other. Similarly, affectation of noradrenergic and dopaminergic pathways is found in both ADHD and sleep disturbances [ 40 ].
Conversely, during wake time, sleep disturbances produces symptoms resembling those observed in ADHD patients [ 35 , 41 , 42 ]. It is, thus, recommended to assess sleep disorders in patients with ADHD symptoms in order to avoid misdiagnosis [ 41 , 42 ].
The relationship between sleep disorders and ADHD is complex. While ADHD might produce sleep disorders, they could also be coincident conditions [ 36 ]. Moreover, sleep disorders have been proposed to be not only one of the intrinsic features of ADHD, but also might be one of its causes [ 32 , 36 ]. Another possible explanation for this interaction would be an underlying common neurological disease leading to both sleep disorders ad ADHD [ 36 ]. A recent review on the subject proposed that chronic sleep disorders are some of the main causes of ADHD symptoms [ 32 ]. The authors suggested that patients presenting ADHD symptoms should undergo quantification of sleep and sleep problems in order to rule them out as the sole cause of ADHD symptoms. Thus, ADHD treatment should address both the symptoms (with classic ADHD treatment) and the sleep problem [ 32 , 34 , 35 , 36 ], although the effect of this combined treatment still requires further research [ 32 ].
4. Genetic Factors Associated with ADHD
Different studies have revealed an important genetic influence in the etiology of ADHD [ 43 ]. It is a polygenic condition with an important number of genes involved, as confirmed by a genome-wide association study on ADHD reporting 12 significant loci associated with this condition [ 44 ]. Many of the genes reported to be associated with ADHD participate in processes such as neurotransmission, neuritogenesis, synaptogenesis, or receptor location in synapses [ 45 ]. In this review, we will focus on two genes, a neurotrophin (brain-derived neurotrophic factor –BDNF-) and a molecule involved in dopaminergic signaling (DAT).
Brain-derived neurotrophic factor (BDNF) is a neurotrophin with high expression in the brain that is highly concentrated in the hippocampus and cortex. It has an important role in neuronal development, being important for neuronal proliferation, migration, differentiation, and maturation, as well as for synaptogenesis [ 46 ].
BDNF has been implied in ADHD pathophysiology. It has been proposed that low levels of this neurotrophin may explain the reduction in brain volume observed in ADHD patients, and it has also been implied in dopaminergic system homeostasis. Some pharmacological treatments for ADHD promote the regulation of plasma BDNF levels [ 47 ].
4.1.1. Circulating BDNF
Since BDNF is able to cross the blood–brain barrier and plasma concentrations of BDNF are highly correlated with its levels on cerebrospinal fluid, a number of studies have searched for a difference in plasma concentrations of BDNF in ADHD patients when compared against controls. There are reports indicating a lower concentration of BDNF in plasma of ADHD patients, both in children [ 48 ] and adults [ 49 ]. In another study involving children, an increase in plasma BDNF was observed after 6 weeks of treatment with an effective dose of methylphenidate [ 50 ]. In accordance, a recent study revealed that methylphenidate treatment produces an increase in serum BDNF in boys with ADHD [ 51 ]. However, this has not always been replicated, since there are also articles reporting no difference in serum BDNF between children with ADHD and controls [ 52 , 53 , 54 ].
A recently published meta-analysis encompassing studies comparing BDNF levels in ADHD patients without any other comorbidity found no overall difference between ADHD patients and controls. However, when analyzing males and females separately, they found significantly higher levels of plasma BDNF in males with AHDH than in control males, while no difference was found between females with and without ADHD [ 55 ].
Thus, different and even contrary results have been obtained regarding BDNF concentrations in plasma or sera of ADHD patients. While this suggests that the link between BDNF and ADHD is not completely clear, other alternatives should be considered. For example, fluctuations in serum BDNF concentrations in morning and evening samples have been reported [ 56 ], meaning the lack of relation between peripheral BDNF concentration and ADHD might be due to the time of the day when the sample was obtained.
4.1.2. Genetics of BDNF
There are a number single nucleotide polymorphisms (SNP) of the BDNF gene that have been associated with ADHD. Among the most studied variations in the BDNF gene, there is a polymorphism called Val66Met (also known as rs6265), in which a change in codon 66 produces a substitution of the original amino acid (valine) by methionine. The anatomical effects of this variation are more apparent in the hippocampus and cortex [ 46 ]. While some studies have assessed the presence of this SNP in ADHD patients [ 57 , 58 , 59 ], other studies failed to find an association between this polymorphism and ADHD [ 46 , 60 , 61 , 62 , 63 ].
Another SNP of the BDNF gene whose association with ADHD is not conclusive is rs2030324, since some studies report an association between this polymorphism and ADHD [ 57 , 58 , 59 , 64 ], while other reports fail to find this association [ 46 , 60 , 61 , 62 , 63 ].
There are other SNPs of the BDNF gene that have been studied so far, with positive correlations being shown between ADHD and the presence of C270T (rs27656701) [ 58 , 61 ], rs11030101 [ 62 , 64 , 65 ], and rs10835210 [ 62 , 63 ]. There are also reports addressing SNPs of the BDNF gene for which no association with ADHD has been found, including rs12291186, rs7103411 [ 63 ], and rs7103873 [ 62 , 63 ].
Moreover, rare single nucleotide variants of BDNF gen have also been associated with a higher risk of developing ADHD [ 66 ]. However, this is an area that requires further research.
As observed with peripheral BDNF concentrations, genetic variants of the BDNF gene have been associated with ADHD in numerous cases, although in some cases there are contradictory results in different articles (see Table 1 ). Moreover, some of the genetic variants of the BDNF gene associated with ADHD have also been studied in association with other neurological conditions and treatments. For example, C270T is reported to be associated with intellectual disabilities [ 58 ]. Moreover, rs11030101 is associated with a better response to electroconvulsive shock therapy for treatment-resistant depression [ 67 ], with body weight gain in schizophrenic patients treated with atypical antipsychotics [ 68 ], as well as with the presence of major depressive disorder [ 69 ], schizophrenia, and bipolar disorder [ 70 ], although there is another publication in which no evidence of association between this SNP and bipolar disorder was found [ 71 ]. Additionally, rs10835210 has been associated with bipolar disorder, schizophrenia [ 70 ], and phobic disorders [ 72 ].
Polymorphisms of the BDNF gene studied in relation with ADHD incidence. * Polymorphisms for which contradictory results have been reported. rs, reference SNP ID number.
For rs6265 (Val66Met), there are many articles addressing the association of this SNP with different conditions, and in some of them it has been found. For example, some articles report an association of this SNP with major depressive disorder [ 69 , 73 ], while other studies fail to find this association [ 74 , 75 ]. An association has also been reported between rs6265 and amnestic mild cognitive impairment, as well as with the transition from this condition to Alzheimer’s disease [ 76 ]. However, in patients with early-stage breast cancer, this SNP is associated with a lower probability of presenting cognitive impairment after chemotherapy [ 77 ].
4.1.3. Other Neurotrophines
While BDNF has been widely studied in association with ADHD, it is not the only neurotrophin studied in relation with this condition, given the important role of neurotrophines in central nervous system development and synaptic plasticity. In this regard, there are studies addressing the participation of fibroblast growth factor (FGF), vascular endothelial growth factor, insulin-like growth factor (IGF2) [ 47 ], glial-derived neurotrophic factor (GDNF), nerve growth factor (NGF), and neurotrophin-3 (NTF-3) [ 47 , 53 ] in ADHD pathophysiology.
BDNF is a molecule highly involved in synaptic plasticity and has an undisputed role in central nervous system development. Therefore, it is not surprising to find a number of studies associating alterations in the presence of this neurotrophin in serum, or different SNPs of its gene, with ADHD. However, its role in ADHD development is not a constant for every sample of ADHD patients studied so far, and for many of the aspects of this molecule (serum levels, SNPs) there are reports indicating associations, with others finding no association at all. This does not mean that the alterations associated with this molecule are not important for ADHD, but rather highlight the variable etiology of this condition.
4.2. Dopaminergic System
The dopaminergic system emerges in early stages of CNS embryonic development, and an imbalance in this system might affect brain development. It is related with cell proliferation, neuronal differentiation and migration, synaptogenesis, and neurogenesis. Thus, it is not surprising that a role of this neurotransmitter system has been reported in different neurological diseases, including ADHD [ 78 ].
One of the most studied molecules of the dopaminergic system in relation to ADHD is DAT, a molecule responsible for dopamine reuptake, and the main target of two commonly used pharmacological treatments for ADHD, methylphenidate and amphetamines [ 78 ]. Genetic studies support the importance of this neurotransmission system for ADHD. Mice heterozygous for the DAT gene (+/− heterozygotes) are reported to present altered attentional function [ 79 , 80 ] and hyperactivity [ 80 ], while rat models with this heterozygous genotype do not present major affectations [ 81 , 82 ]. However, DAT knockout rats present hyperactivity [ 81 , 82 ], as well as a dysregulation in frontostriatal BDNF function [ 82 ]. Hyperactivity in these rats can be counteracted by amphetamine, haloperidol, and methylphenidate [ 82 ].
In humans, ADHD patients present lower DAT availability in the basal ganglia, caudate nucleus, and putamen [ 83 ]. The DAT gene presents a variable tandem repeat region (VNTR) at the untranslated 3′region, and there are different alleles for this VNTR, with the 9-repeat and 10-repeat alleles being the most frequently encountered. The reported effects of this VNTR on DAT expression vary in different articles, however the most recent results indicate that the 9-repeat allele is associated with a higher DAT expression than the 10-repeat allele. [ 84 ]. The possible association between this VNTR and ADHD has been addressed in various studies. For example, an analysis of both patients and the literature found an association of the 10-repeat/10-repeat genotype with ADHD only in adolescents [ 85 ], studies performed in children reported an association between the 10-repeat/10-repeat genotype and ADHD [ 86 , 87 ], while a recently published meta-analysis reported an association of the 10-repeat allele with ADHD in children and adolescents, specifically in European population [ 88 ]. However, there are also reports indicating no association at all between ADHD and the VNTR of DAT gene (9-repeat/10-repeat, 10-repeat/10-repeat, and 10-repeat/11-repeat genotypes) [ 89 ], no association between the 10-repeat/10-repeat allele with ADHD [ 90 ], and no association between ADHD and the 9-repeat or the 10-repeat alleles for this polymorphism [ 91 ]. The last three studies were performed in children.
Additionally, the relevance of this VNTR has been studied in relation to cognitive function in healthy subjects. Again, mixed results were found. A meta-analysis published in 2016 addressing studies performed in healthy subjects did not find any association between DAT VNTR and different cognitive functions, such as executive functions, inhibition, attention, and long-term declarative memory [ 92 ]. A study performed in children aged 3 to 5 years old addressing the presence of the 9-repeats and 10-repeats alleles revealed that the presence of the 10-repeat allele of the DAT gene is associated with diminished ability to voluntarily regulate reactivity in healthy children [ 93 ]. A recent study on both ADHD and healthy children reported an effect of the specific genotype in the performance of children on attentional switching when studying the whole research sample, in which children carrying the 9-repeat allele performed worse than those carrying the 10-reapet homozygous or the 10-repeat/11-repeat heterozygous allele [ 91 ]
The participation of the dopaminergic system in the pathophysiology of ADHD has been widely reported [ 78 ]. Herein, we study a particular variation of the DAT gene, a VNTR in the 3′ region of the gene, finding articles supporting a role of this polymorphism in ADHD, as well as works failing to find an association between this VNTR and ADHD. This does not imply a lack of importance of this variation, but rather highlights the variability in the genetic etiology of this condition. Moreover, while the dopaminergic system is highly involved in the pathophysiology of ADHD, given its role in CNS development, it is also strongly related with other neuropsychiatric conditions, such as autism [ 78 , 94 , 95 ] and schizophrenia [ 78 , 94 , 96 , 97 ].
5. Changes in Brain Structure and Function in ADHD Patients
As an NDD, ADHD involves alterations of mechanisms such as neurogenesis and synaptogenesis. There are a number of possible mechanisms through which these alterations take place, both environmental and genetic, some of which have been mentioned in the present review. In the end, all of these altered mechanisms produce an altered brain function affecting attention and impulse control, functions regulated by the central nervous system. Understanding the changes in brain function associated with ADHD might shed some light not only on the functional causes of this condition, but also on possible ways to deal with it.
5.1. Brain Imaging Studies
Children with ADHD present atypical connectivity in reward circuitry when compared with control children. Increased connectivity of the nucleus accumbens with the prefrontal cortex was observed to be associated with greater impulsivity [ 98 ].
Hypofunction and abnormal cortico-striatal pathways of the cortico-striato-thalamo-cortical (CSTC) circuit are associated with ADHD. Five different CSTC circuits have been reported: the sustained attention circuit, emotion circuit, selective attention circuit, hyperactivity circuit, and impulsivity–compulsivity circuit. Four of them (except emotion circuit) have been related with ADHD diagnostic criteria. However, pathogenesis of the emotion circuit is also related with ADHD [ 99 ]
A study on ADHD children reported significantly decreased white matter volume, as well as decreased volume in the cortex and caudate nucleus, although it did not reach statistical significance. Cortical thickness was reduced in ADHD patients bilaterally in the frontal cortex and in the right cingulate cortex, structures related with executive function and attention. Regarding default mode network, functional connectivity was reduced in ADHD children in the anterior and posterior cingulate cortexes, lateral prefrontal cortex, left precuneus, and thalamus. However, connectivity was increased in the bilateral posterior medial frontal cortex [ 100 ].
A study on male adolescents with ADHD and controls reported decreased gray matter volume in the left anterior cingulate cortex and bilateral decreases in the occipital cortex, hippocampus–amygdala complex, and cerebellum in ADHD adolescents [ 101 ]. Such decreases in cerebellar volume have been previously reported in both female and male ADHD patients [ 102 ].
An important issue with many of the imaging studies in ADHD patients has been small sample size. A large-scale study performed on children, adolescents, and adults with ADHD reported decreased surface area in children, mainly in the frontal, cingulate, and temporal regions. This effect was more pronounced in younger children (4–9 years old). Moreover, cortical thickness in ADHD children is also reduced in the fusiform gyrus and temporal lobe, an effect more prominent in children of 10 and 11 years old. No change in surface area or cortical thickness was observed in adolescent or adult ADHD patients [ 103 ].
There are important changes in brain morphology in ADHD patients. An elegant study performed in ADHD patients and controls from 6 to 28 years of age analyzed differences in neurodevelopmental trajectories. This study reported that ADHD patients present overall reduced cortical volume, mainly in frontal lobes, and primarily due to a decrease in surface area and gyrification. Interestingly, although both groups presented maturational changes due to age, they presented different trajectories for these changes, suggesting that ADHD is associated with developmentally persistent changes in the whole cortex, mostly due to decreased surface expansion (reduced surface area and less convolution) [ 7 ].
When comparing children with comorbid epilepsy and ADHD with control children, a widespread decrease in cortical thickness is observed, along with decreased volume in some subcortical structures and the brainstem. These alterations were observed early in the course of epilepsy, thus the authors suggested that neurodevelopmental changes occurred before epilepsy onset [ 104 ]. In children with comorbid autism spectrum disorder and ADHD, when compared with typically developing controls, presented significantly lower volumes in left postcentral gyrus. This was observed through magnetic resonance imaging in both children and preadolescents, but was absent in adolescents. The authors suggested that pathophysiology in these comorbid patients may be related to somatosensory deficits and delayed maturation in this area [ 105 ].
5.2. Quantitative Electroencephalography
All these changes lead to alterations in brain function. A frequently used technique for the study of brain activity is quantitative electroencephalography (qEEG), since it has a low cost, a high temporal resolution, and does not need special facilities to be performed. Furthermore, qEEG has also been used to determine the effects of pharmacological treatments on brain activity in order to assess effectiveness [ 106 , 107 ], to choose the correct pharmacological option for a patient [ 108 ], to study the effects of previous pharmacological treatments on the current one [ 109 , 110 ], as well as to determine a possible cognitive effect of the chosen pharmacological treatment [ 111 ].
During the last decades, several studies have performed qEEG analyses on ADHD patients. A review on the subject published in 2012 addressed the main associations between brain activity and ADHD, including increased frontocentral theta activity. Another frequently reported factor, although not always replicated, is an increased theta/beta ratio. For beta and alpha bands, most of the reports have indicated decreased activity, although there are also reports that have indicated increased activity in these frequency bands in ADHD patients [ 112 ]. One of the most used indicators for ADHD is the theta/beta ratio in the Cz region. It has been reported that ADHD children (inattentive and combined subtypes) present increased theta/beta ratios [ 1 ]. Another study found that children with ADHD presented more delta and theta activity [ 113 ]. However, some authors have mentioned that this measure is not necessarily useful for diagnosis, since among other issues, it presents variations according to age [ 114 ].
Another example of the influence of age on brain electrical activity associated with ADHD is a study comparing children with and without ADHD, as well as adults with and without ADHD. Interestingly, children with ADHD presented higher delta and theta activity than control children, while in adults no difference was found between ADHD group and controls in the frequency bands analyzed [ 115 ]. Among the few differences in qEEG activity found in adults with ADHD is a higher gamma activity (39.25–48 Hz), suggesting a functional alteration in dorsal attention network [ 116 ].
ADHD patients often present comorbidities [ 117 ], which might influence qEEG in a different way to the findings in ADHD only patients. For example, children with ADHD and problematic Internet use present differences in qEEG when compared to ADHD only patients. However, no differences were found between ADHD only patients and ADHD patients with depression [ 118 ]. Another study found that adolescents with ADHD and Internet gaming disorder presented lower relative delta power and greater relative beta power than adolescents with ADHD only [ 119 ].
It is noteworthy that although a number of studies have been published regarding neurophysiological correlates of ADHD through qEEG, there are still some differences in the results reported by different authors. Beyond possible methodological differences, there are a number of factors reported to influence qEEG activity in ADHD patients, which might be responsible—at least in part—for the differences reported so far, and which might be of importance when using qEEG information to choose or design a therapeutic approach. These factors include comorbidities [ 4 , 120 ] and the ages of the patients [ 114 , 116 , 121 ]. Other factors reported to affect qEEG activity in other populations and conditions are ethnicity [ 122 , 123 , 124 , 125 , 126 ], sociocultural environment during development [ 127 , 128 ], and the degree of advancement of a psychiatric condition, as reported for alcohol dependence [ 129 , 130 , 131 ].
6. Therapeutic Approaches
6.1. pharmacological treatment.
Both stimulant and non-stimulant pharmacological treatments have proven to be effective in diminishing ADHD symptoms in children and adolescents [ 132 , 133 ], although stimulant medication seems to have greater effectiveness [ 133 , 134 ]. Herein, we will address one frequently used stimulant (methylphenidate) and one frequently used non-stimulant (atomoxetine)
6.1.1. Methylphenidate
Methylphenidate is one of the most used drugs for ADHD treatment. It has been present in the market for 50 years and it reduces excessive hyperactivity, impulsivity, and inattention in children and adolescents with ADHD. In the United States, it is prescribed to 8% of children and adolescents under 15 years of age and to around 3% to 5% of the same population in Europe [ 135 ].
Methylphenidate blocks DAT and NET, reducing reuptake and producing an increase in available dopamine and norepinephrine in the synaptic cleft [ 135 , 136 , 137 ], leading to increased dopamine and norepinephrine transmission in the prefrontal cortex [ 132 ]. A meta-analysis on the effects of methylphenidate treatment on ADHD in adults found it effective in improving neurocognitive performance, accomplishing better results than placebo groups in terms of working memory, reaction time variability, vigilance, driving, and response inhibition [ 136 ].
6.1.2. Atomoxetine
Atomoxetine has been reported to be effective for ADHD treatment [ 138 ], being more effective in adults than in children [ 134 ].
Atomoxetine blocks norepinephrine reuptake, producing increased presence of norepinephrine and dopamine in prefrontal cortex [ 132 ]. Since atomoxetine does not produce an increase of dopamine or norepinephrine in the nucleus accumbens, it lacks abuse potential [ 132 , 139 ]. This drug is associated with improvements in quality of life in children adolescents and adults, although this parameter is not further increased with long-term use [ 139 ].
6.1.3. Adverse Effects
Both stimulant and non-stimulant pharmacological treatments for ADHD produce adverse effects in a percentage of treated patients. The main adverse effects found for these drugs (% of patients treated with stimulants/% of patients treated with non-stimulants) are decreased appetite (28.6%/14.2%), nausea (7.9%/10.3%), headache (14.5%/20.8%), insomnia (12.3%/8.6%), nasopharyngitis (6.0%/7.1%), dizziness (5.1%/10.0%), abdominal pain (7.8%/11.5%), irritability (9.3%/6.9%), and somnolence (4.4%/34.1%) [ 133 ].
A systematic review on the adverse effects of methylphenidate in children and adolescents revealed that about 1 in 100 patients present serious adverse events after methylphenidate treatment (including death, cardiac problems and psychiatric disorders), while more than half of the patients treated with methylphenidate suffer one or more adverse events. The authors concluded that it is important to identify subgroups of patients who might be harmed by methylphenidate treatment and highlight the importance of remaining alert to possible adverse events in patients with this treatment [ 135 ]. There might also be uncommon adverse effects. For example, there is a report of 3 cases of systemic sclerosis associated with methylphenidate treatment [ 140 ]. The authors of the last study suggested that patients with signs of autoimmune or vasospastic conditions should be briefed about this possible side effect before commencing methylphenidate treatment.
A systematic review on possible adverse effects of atomoxetine, including decreased growth rate, cardiovascular and hepatic effects, aggression, psychosis, seizures, and suicidal ideation, determined that evidence indicates it is safe to use in ADHD patients [ 141 ]. Furthermore, the presence of comorbidities does not interfere with treatment efficacy, nor does treatment exacerbate comorbid symptoms [ 142 , 143 ]. However, it is important to be alert to other possible adverse effects. A case report and review indicated that the appearance of tics is a common side effect of atomoxetine treatment [ 144 ].
Methylphenidate and atomoxetine are known to increase heart rate and blood pressure, raising concern regarding possible cardiovascular effects of these drugs in ADHD patients. A review on the cardiovascular effects of these drugs in healthy subjects found the drug to be safe to use. Most of these studies were performed in children and adolescents, although there have also been some studies performed on adults, with no serious risk being reported in these subjects either. However, patient blood pressure and heart rate should be monitored on a regular basis. Moreover, careful follow-up should be performed for patients presenting certain cardiovascular conditions [ 145 ].
Weight loss has also been reported after atomoxetine treatment, occurring during the first two years of treatment. However, evidence suggests this decrease begins to be compensated between 2 and 5 years after the beginning of treatment [ 141 ]. Similarly, methylphenidate has been associated with adverse effects such as anorexia, weight loss, and insomnia [ 146 ].
A comparative study on short-term effects of methylphenidate and atomoxetine on ADHD reported significantly higher weight loss in children treated with atomoxetine [ 147 ]. However, a more recent study reported that children present significantly more weight loss after methylphenidate than after atomoxetine treatment [ 148 ].
A meta-analysis on gastrointestinal adverse effects of methylphenidate reported increased risk of decreased appetite, weight loss, and abdominal pain in children and adolescents under this pharmacological treatment [ 149 ].
A comparison between the presence of adverse effects after methylphenidate and atomoxetine treatments in ADHD children indicated methylphenidate as a safer option, since children under atomoxetine treatment presented higher incidence rates of anorexia, nausea, somnolence, dizziness, and vomiting than children under methylphenidate treatment [ 147 ]. A more recent study reported similar results, since children treated with atomoxetine presented higher incidence rates of mild adverse effects, such as decreased appetite, weight loss, dyspepsia, abdominal pain, stomach ache, irritability, mood disorders, and dizziness. As for severe adverse effects, patients under atomoxetine treatment presented higher incidence rates of gastrointestinal, neuropsychiatric, and cardiovascular effects [ 150 ].
6.1.4. Long-Term Adverse Effects
Long-term adverse effects of methylphenidate are the subject of intense study, given that it is the first-line stimulant drug used for ADHD treatment in children, adolescents, and adults [ 11 , 151 ]. A review on the subject addressed different adverse effects studied in patients after long-term (over one year) administration of methylphenidate, including low mood or depression, anxiety, irritability or emotional reactivity, suicidal behavior or ideation, bipolar disorder, psychotic symptoms, substance use disorders, tics, seizures or EEG abnormalities, and sleep disorders. The authors concluded that existing information indicates that methylphenidate is safe to use, although caution should be taken when prescribing this drug to specific groups, such as preschool children, patients prone to psychosis or tics, and high-risk adolescents [ 152 ]. However, the need for more studies on the long-term effects of treatment with this drug is highlighted, since studies in humans are rather scarce and with a high degree of heterogeneity in terms of methodological approach [ 151 , 152 ].
6.1.5. Long-Term Therapeutic Effect
Given that ADHD is a chronic disorder and that many of the children presenting ADHD will still present symptoms in adulthood, it is particularly important to determine the long-term effectiveness of pharmacological treatments. However, very few studies address this issue, and no conclusion can yet be drawn regarding the long-term effects (years) of pharmacological treatment of ADHD on symptom reduction and quality of life. Thus, the long-term efficacy of drug treatment for ADHD remains under debate [ 153 , 154 , 155 , 156 ]
Current pharmacological treatments for ADHD have proven to be safe and effective. The efficacy of these treatments on ADHD symptoms is clear, and thus pharmacological therapy is often used to treat ADHD patients [ 136 , 138 , 141 , 152 ]. However, there are also some drawbacks to this therapeutic approach, including the time required to reach the effective dose for each patient [ 3 , 157 ]; the lack of response in some patients [ 121 , 158 , 159 , 160 ]; the unresolved issue of long-term effectiveness (of great importance given that in many cases the treatment must go on for years) [ 153 , 154 , 155 , 156 ]; the presence of adverse effects, which although not life threatening in most cases, are nevertheless upsetting [ 133 , 135 , 144 ]; and the existence of specific groups of patients with whom a greater caution must be taken [ 140 , 145 , 152 ]. Altogether, these drawbacks have led to the search of new therapeutic approaches. One of the strategies studied so far is the possibility of using other drugs to treat ADHD, including drugs interacting with serotoninergic (metadoxine, paroxetine, duloxetine, buspirone), glutamatergic (memantine), cholinergic (AZD3480, AZD1446, lobeline, galantamine, mecamylamine), histaminergic (mk-0249), and catecholaminergic neurotransmission systems (modafinil, droxidopa, desipramine, bupropion, nomifensine, reboxetine, venlafaxine, duloxetine, guanfacine, aripiprazol, dasotraline, selegiline), as well as lithium [ 161 ].
6.2. Non-Pharmacological Therapies
Pharmacological therapy is effective although presents some inconveniences, including the existence of adverse effects in some patients and lack of effect in others. Therefore, there are also different non-pharmacological approaches for ADHD treatment.
6.2.1. Behavioral Parent Training
The goal of parent training is to equip parents with techniques that will be useful in managing ADHD-related behavior presented by their children. A systematic review published on 2011 found no reliable effect of ADHD children’s behavior, although it may lead to increased confidence and decreased stress in parents [ 162 ]. Later studies found an effect of behavioral parent training on ADHD symptoms, which is not increased by previous working memory training, although this combination did produce positive effects on working memory storage and processing [ 163 ]. It is noteworthy that cognitive functioning of both parents and children influences the effectiveness of this therapeutic approach on ADHD symptoms. Better working memory in children and higher parental response caution presented an association with improvements in inattention. As for conduct problems, better parental self-regulation was associated with a better result in this area. However, none of the measured cognitive functions in children or parents were associated with improvements in hyperactivity [ 164 ]. Moreover, behavioral parent training improves coexistence at home, since a reduction in the frequency and severity of problematic situations is produced, along with a reduction of stress in parents [ 165 ].
6.2.2. Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) has also been used to treat ADHD. A review performed on the subject found CBT to be effective in reducing ADHD symptoms in adults, however only when improvement was evaluated by the patient and not when evaluated by the clinician [ 166 ], although a more recent meta-analysis on the subject reported a good effect of CBT on ADHD adults [ 167 ]. A Cochrane systematic review concluded that CBT has a positive effect on ADHD symptoms, either alone or in conjunction with other therapies, although considered the evidence to be low-quality in accordance with the Grading of Recommendations Assessment, Development and Evaluation (GRADE) working group approach. [ 168 ]. A meta-analysis found that CBT is one of the most effective non-pharmacological options to treat ADHD, ranking just after physical exercise [ 169 ]. A later systematic review confirmed the effects of CBT on ADHD symptoms [ 170 ]. A recent study reported CBT to be effective in reducing ADHD symptoms in patients, either with or without conjunct medication [ 171 ].
6.2.3. Attention Training Techniques
Attention training techniques are often used to improve life quality and increase well-being. Given the effect of these techniques on brain activity, as well as on attention and self-regulation, their use to reduce ADHD symptoms and improve life quality in these patients is currently under study [ 172 ].
Mindfulness can be defined as paying attention to the present, an activity that implies sustained attention. A systematic review on the effects of mindfulness-based interventions on ADHD found that such approaches were popular among adults with ADHD, finding improvements in attention, although the effects of such approaches in children and adolescents are still unclear [ 173 ]. A recent meta-review reported a large effect size of mindfulness on ADHD [ 174 ]. A review on the effects of mindfulness-based cognitive therapy on ADHD adults reported good effects of this therapeutic approach, especially when used in conjunction with pharmacological therapy [ 175 ], while a systematic review analyzing the effects of meditation-based techniques (either on parents and children or on children only) on ADHD children could not draw a clear conclusion regarding beneficial effects [ 176 ].
Adult ADHD patients that underwent an 8-week mindfulness awareness practice period presented decreased ADHD, depression, and anxiety symptoms [ 177 ]. Similarly, a study performed with children revealed that an 8-week period of mindfulness-oriented meditation produced improvements in the performance of neuropsychological tests, as well as in ADHD symptoms. Although encouraging, the authors stated that the results are still preliminary, given the small number of children participating in the study [ 178 ]. There are also results indicating that this technique produces an improvement in ADHD symptoms in ADHD children with oppositional defiant disorder [ 179 ].
6.2.4. Neurofeedback
Neurofeedback (NFB) is a therapy in which patients learn to modify EEG patterns through operant conditioning. There are articles reporting the induction of plastic changes after NFB training [ 180 , 181 , 182 , 183 ], supporting a theory explaining the effects of NFB on different brain disorders through the induction of synaptic plasticity, leading to an homeostatic set point. Additionally, besides some unusual cases of headache, no collateral effects have been reported with this technique. One of the most interesting aspects of NFB is the induction of plastic changes from within the brain under normal physiological conditions, without the need for an external stimuli such as pharmacological treatments or transcranial stimulation to alter brain activity, thus the probability of adverse effects is minimal [ 181 ].
Specific NFB protocols have been developed over the decades. These protocols were designed based on articles reporting specific qEEG variations in neurological patients or qEEG patterns associated with cognitive function. Some of these standardized protocols have been studied in terms of their ability to treat ADHD [ 184 ].
Several articles have addressed the use of NFB in ADHD patients. The results have been mixed and numerous meta-analyses have been published on the subject. The conclusions of these meta-analyses have also been mixed. There are meta-analyses reporting good effects of NFB on ADHD [ 185 , 186 , 187 ], not finding reliable effects [ 188 ], not reaching a conclusion on the subject of efficacy [ 189 ], finding a minor effect of this therapeutic approach significantly below what is observed with pharmacological treatment [ 190 ], or finding a minor effect only in the presence of pharmacological treatment [ 191 ].
An overview of recent publications gave the same impression. Some reports found effects of NFB theta/beta or theta/alpha protocols on ADHD, measurable at follow-up 8 weeks or 12 months after treatment completion [ 192 , 193 ]. Other reports found no effect [ 194 , 195 , 196 ]. Moreover, there are reports revealing a minor effect of NFB, below the effect levels of other therapeutic approaches [ 197 , 198 , 199 ].
NFB is a therapeutic approach widely studied for ADHD treatment. The results so far have been mixed. However, given the absence of side effects and its ability to induce synaptic plasticity [ 181 ], it is an option worth keeping in mind.
6.2.5. Other Non-Pharmacological Approaches
The use of non-pharmacological supplementations, such as polyunsaturated fatty acids, peptides, amino acids, plat extracts, probiotics, micronutrients, and herbal supplementation, is currently being studied in order to determine their usefulness in treating ADHD. However, further research is still needed in this area [ 200 ].
A study performed in ADHD children under methylphenidate treatment for whom zinc supplementation was added reported no significant effect of zinc supplementation on the total score for a parent’s questionnaire for ADHD or in the hyperactivity and impulsivity subscales. However, zinc-supplemented children present improvements in inattention scores [ 201 ].
A meta-analysis on non-pharmacological interventions for ADHD patients found that physical exercise produced a good effect on ADHD cognitive symptoms, especially aerobic exercise targeting executive functions [ 169 ].
7. Treatment Personalization
In the first sections of this review, we addressed some of the factors associated with ADHD incidence, ranging from a variety of environmental factors to the presence of different genetic polymorphisms. However, these different etiologies are not always present, since patients might present one or another (see Section 2 and Section 3 ). Similarly, while there are some changes in brain activity associated with ADHD, they are not always the same (see Section 4 ). Accordingly, there is also variation in the response of patients to both pharmacological and non-pharmacological treatments (see Section 5 ).
Since the etiology of ADHD could be very different from patient to patient, the precise nature of the physiological changes underlying the clinical manifestations of ADHD in each case could be slightly different, affecting the effectiveness of the chosen treatment and possibly explaining the variation in the effect of the same treatment on different patients. This can be observed in the variations in qEEG activity observed in different studies [ 112 , 113 , 114 , 116 , 121 ]. However, the design of personalized treatments based on specific characteristics of each patient could lead to better clinical results. In this regard, strategies to adjust therapeutic approaches based on patients’ characteristics have been used for both pharmacological and non-pharmacological therapies.
Selecting the appropriate pharmacological treatment and the dose to be used takes some time, given the large inter-individual variability regarding treatment efficacy, leading to a delay in reaching a therapeutic effect, and in some cases producing an early termination of treatment due to frustration, either by the provider or the family [ 157 ]. Moreover, there is some variability regarding patient response to methylphenidate, including patients that do not achieve adequate symptom control or experience adverse effects with commonly used doses. Therefore, dose optimization has been proposed as a means to achieve an adequate effect for most of the patients, enhancing both the efficacy and safety of methylphenidate treatment [ 3 ]. This has led to the search for strategies to find adequate treatments for each patient, such as pharmacogenomics, in which a patient’s genotype for a particular gene is used to predict the effects of medication in that patient. However, in spite of the progress that has already been made, no pharmacogenomic test so far has been found to be helpful in treatment selection [ 157 ].
Treatment resistance has been reported for both atomoxetine [ 158 ] and methylphenidate [ 121 , 159 , 160 ]. For this reason, qEEG can be used as a source of information to determine at an earlier point whether methylphenidate [ 121 , 160 , 202 ] or atomoxetine [ 107 , 202 ] is effective or if an alternative treatment is needed for a patient.
Most of the reports on the use of NFB for ADHD use a standardized protocol, either equal for all participants or adapted to each patients after qEEG analysis. However, there is another more personalized approach known as qEEG-informed (or qEEG-guided) NFB. In this variant of NFB, rather than selecting a particular protocol (for example, theta/beta ratio) and applying it to all participants, subjects receive a NFB protocol selected for them after qEEG analysis. This type of NFB has been successfully used in schizophrenia [ 203 ], obsessive compulsive disorder [ 204 ], migraine [ 205 ], dementia [ 206 ], and with learning-disabled children [ 207 , 208 ].
There are so far only two studies applying qEEG-informed NFB in ADHD patients, so it is not yet possible to perform a meta-analysis on the effects of this type of NFB on ADHD. However, a positive effect of NFB has been reported in both published studies [ 209 , 210 ].
8. Discussion
ADHD is an NDD with a complex etiology. While it is clear that its main cause is alterations in neurodevelopmental processes such as synaptogenesis, myelination, and neurogenesis [ 5 ], the causes of these neurodevelopmental alterations are diverse. In some cases they might be associated with environmental factors such as premature birth [ 6 ], perinatal problems [ 9 ], nutrition during pregnancy [ 10 ], or exposure to heavy metals [ 17 , 18 , 19 , 26 , 27 , 29 ]. Additionally, there is strong evidence of genetic influence on ADHD [ 43 , 44 ], and an interaction between environmental and genetic factors cannot be discarded.
The purpose of this review is not to fully describe all factors associated with ADHD appearance, but rather to address some of the main etiologies described so far, in order to clarify the high diversity of factors associated with this NDD. When analyzing the different sections of this review, one thing becomes evident—that ADHD patients are diverse regarding the etiology of their condition and their responses to treatment. This heterogeneity outlines the high variability in patients’ particular conditions regarding ADHD symptom manifestation and treatment, since it is probable that the underlying neurophysiological alterations for each patient are at least slightly different. Thus, standardized treatment (either pharmacological or non-pharmacological) may not be equally efficient in all cases.
Moreover, there could be other factors that are usually disregarded in relation with ADHD incidence, but which might play an important role in this condition. Recently, the gut microbiome has been the subject of intense research as an ADHD-associated factor, and even though further research is needed in order to determine its precise influence on ADHD, there are already reports indicating a possible link between them [ 211 , 212 , 213 , 214 ].
In the end, all of these factors produce changes in brain structure and function [ 1 , 7 , 112 , 113 , 114 , 115 ], leading to the symptomatology observed in ADHD patients. Therapeutic approaches to treat this condition have the objective of compensating such alterations in order to reduce symptoms and improve quality of life. However, as we have observed in this review, not all patients present the same neurophysiological changes. Studies performed on qEEG activity have yielded different results regarding brain electrical activity in ADHD patients [ 4 , 112 , 114 , 120 ]. Additionally, both brain imaging and qEEG techniques have revealed that changes are not consistent throughout the lifespan, being different in children and adults [ 114 , 115 , 116 , 121 ]. Therefore, there is a need for treatment personalization for each ADHD patient in order to achieve greater effect with minimal adverse effects.
Pharmacological treatments, both stimulants and non-stimulants have proven to be effective and safe for ADHD patients [ 132 , 133 ], and thus are widely prescribed to treat this condition. However, the pharmacological approach to ADHD treatment has some drawbacks, mostly regarding difficulties in reaching effectiveness in all patients [ 3 , 121 , 157 , 158 , 159 , 160 ] and the presence of adverse effects [ 133 , 135 , 144 ].
The search for other therapeutic options has led to the assessment of the effects of other drugs on ADHD [ 161 ], as well as the design of non-pharmacological treatments, such as behavioral parent training, CBT, attention-improving techniques, and NFB.
The effects of behavioral parent training on ADHD symptoms in children are not consistent, with some articles finding effects [ 163 ] and others not finding any [ 162 ]. However, behavioral parent training does reduce stress in parents and promotes a better coexistence at home, which is favorable for children [ 162 , 165 ]. In the case of CBT, there is more evidence indicating a good effect in reducing ADHD symptoms [ 167 , 168 , 169 , 170 , 171 ]
Attention training techniques are still under intense study. There is some evidence regarding the effect of this technique on ADHD in adults [ 173 , 175 ], while in children and adolescents the results are not clear so far [ 173 , 176 ].
A number of studies on the effect of NFB on ADHD symptoms have yielded different results, either finding a positive effect [ 185 , 186 , 187 , 192 , 193 ], a mild effect [ 190 , 197 , 198 , 199 ], or no effect at all [ 188 , 194 , 195 , 196 ]. However, NFB has a number of advantages that encourage the search for an adequate protocol to treat ADHD patients. It is targeted directly to change brain activity associated with the condition under treatment, it has virtually no side effects, and the therapeutic effect is due to the induction of plastic changes in the central nervous system, thus it might establish a long-term changes [ 180 , 181 , 182 , 183 ].
9. Conclusions
In the present review, we have gone through some of the factors associated with ADHD, and it is clear that a great heterogeneity exists in the etiology of this condition. Therapeutic approaches, although functional in many cases, also show heterogeneity in their effects in certain groups of patients. The diverse range of effects of the therapeutic approaches used should not be a surprise, given the diversity of etiologies found in ADHD. Even though clinical manifestations of this condition might be similar (diagnosis is based on the presence certain symptoms), the same clinical manifestations could occur with different underlying physiological changes, considering the variations in qEEG activity in different groups of patients [ 112 , 113 , 114 , 116 , 121 ]. Thus, these neurophysiological changes presented by patients may not necessarily respond in equal form to a given therapeutic approach. Given the inter-personal variance in the etiology of ADHD, it is advisable to personalize the therapeutic approach. Regarding pharmacological therapies, dosage optimization [ 3 ], pharmacogenomics [ 157 ], and the use of qEEG to select the adequate drug for a given patient have been proposed [ 107 , 121 , 160 , 202 ].
Regarding non-pharmacological options, the use of qEEG-informed NFB has been proposed for personalized treatment in ADHD patients. The studies carried out to date have shown positive results [ 209 , 210 ], although the number of studies is still too small to draw a conclusion. However, given the advantages of NFB [ 181 ] and the positive effects of this approach reported for other conditions [ 203 , 204 , 205 , 206 , 207 , 208 ], it is worth performing further studies on the effectiveness of this type of NFB on ADHD.
Author Contributions
Conceptualization, L.N.-J. and W.V.H.-M. writing—reviewing and editing, L.N.-J., W.V.H.-M., and A.H.-S. All authors have read and agreed to the published version of the manuscript.
This research received no external funding
Conflicts of Interest
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Work & Careers
- Life & Arts
UK dementia adviser wants half a million volunteers for clinical trials

- UK dementia adviser wants half a million volunteers for clinical trials on x (opens in a new window)
- UK dementia adviser wants half a million volunteers for clinical trials on facebook (opens in a new window)
- UK dementia adviser wants half a million volunteers for clinical trials on linkedin (opens in a new window)
- UK dementia adviser wants half a million volunteers for clinical trials on whatsapp (opens in a new window)
Ian Johnston and Michael Peel in London
Roula Khalaf, Editor of the FT, selects her favourite stories in this weekly newsletter.
The UK should recruit half a million people to help it become a hub for clinical trials of the next generation of dementia drugs, the top scientific adviser to a new government-backed initiative on neurodegenerative disorders has urged.
A big database of potential participants would make the country an attractive location for pharma companies to carry out tests, accelerating the UK’s access to medicines and providing potential treatments for its almost 1mn dementia sufferers, said neuroscientist Ruth McKernan.
McKernan will chair the scientific advisory board of the UK’s new Neurodegeneration Initiative. It is part of an official push to be announced on Wednesday to capitalise on scientific breakthroughs that for the first time promise to bring diagnostics and therapies for the debilitating condition within reach.
“If we’re able to accelerate how patients get into clinical trials and how those clinical trials get conducted, then it will encourage pharma companies to come here,” McKernan told the Financial Times, adding “it would be great to have half a million” volunteers.
“It will encourage them to make sure the medicines are available here and it’s a route for people to get tested with the new medicines in development.”
The Neurodegeneration Initiative will have the job of promoting more and quicker trials of potential dementia diagnostics and treatments. McKernan is a former head of Innovate UK and currently a venture partner at life sciences venture capital firm SV Health Investors.
The government is aiming to establish a cohort of 20,000 pre-screened people, deemed to be at risk of dementia or with mild cognitive impairment, who could be fast-tracked into clinical trials.
McKernan did not set a timeline for reaching the half a million prospective clinical trial cohort, which she said was a personal view and not an official target.
The government is also pledging £6mn in funding for UK early-stage biotechs working on diagnostics for neurodegenerative diseases and facilitating clinical trials. It has pledged to double funding for dementia research to £160mn a year by 2025.
Researchers have made striking advances on both potential diagnostics and treatments for diseases leading to dementia, a condition estimated to affect more than 55mn people worldwide.
Scientists have identified potential “biomarkers” — biochemical signs in the body — that may indicate a person is in the early stages of dementia or at an elevated risk of developing it.
The signals are a “big step forward in neuroscience”, McKernan said, adding that the UK dementia effort could help accelerate work on identifying other biomarkers. These could be used with trial participants to monitor disease progression, she added.
The comments come as the UK regulator, the Medicines and Healthcare products Regulatory Agency, is assessing the first treatments to target a plaque that triggers Alzheimer’s, the biggest cause of dementia.
The drugs, developed by Japanese pharma company Eisai and US company Eli Lilly, tackle the build-up of amyloid plaques in the brain that trigger the disease, rather than address symptoms like current treatments.
McKernan said it was likely that further anti-dementia drugs would be developed, drawing parallels with how cancer treatments had evolved.
“We’re about 20 years behind cancer,” she said. “I think the number of specific drugs we have in cancer and the way that patients are treated with different drugs at different stages of the disease will be the future for dementia.”
New treatments being developed for Alzheimer’s offered the best hope yet of ending “the devastation this condition inflicts on people and society”, said Hilary Evans, co-chair of the Dame Barbara Windsor Dementia Mission and chief executive of Alzheimer’s Research UK. “Now we must keep up this momentum and ensure the UK is at the forefront of tackling dementia for years to come.’’
Promoted Content
Follow the topics in this article.
- Dementia Add to myFT
- Pharmaceuticals sector Add to myFT
- Drugs research Add to myFT
- Healthcare Add to myFT
- Medical science Add to myFT
International Edition

COMMENTS
ADHD Research Lab. The ADHD research lab conducts research on Attention Deficit Hyperactivity Disorder with a particular focus on adults with the condition, who are often under-represented in research. Around 3% of adults worldwide have ADHD and there are relatively fewer treatment options available to them compared to children with the condition.
17 July 2023. Both ADHD diagnoses and prescriptions for ADHD medication have increased significantly over the past two decades, except in children under five, finds a new study by UCL researchers. The research, published in BJPsych Open, reviewed data from 7 million individuals aged three to 99, from IQVIA Medical Research Data, a UK primary ...
The research reviewed 7 million individuals aged three to 99 between 2000 and 2018. It used data from the IQVIA Medical Research Data, a UK primary care database. Researchers from University College London (UCL) found: 35,877 had an ADHD diagnosis; 18,518 received prescriptions for ADHD medication; a 20-fold increase in ADHD diagnoses
Probably, the most crucial area of future treatment research in ADHD will be to gain insight into the long-term positive and negative effects of treatments, using randomised trials with withdrawn designs, as well as additional population-based studies with self-controlled methodologies and longitudinal follow-up studies.
INTRODUCTION. The worldwide prevalence of attention deficit/hyperactivity disorder (ADHD) in children and young people is approximately 5% (National Collaborating Centre for Mental Health (UK), 2009), although estimates vary.A recent population-based study in the UK reported a prevalence of 1.6% in 5-19 year olds (NHS Digital, 2018).ADHD is an early-onset neurodevelopmental disorder ...
Attention deficit hyperactivity disorder (ADHD) is associated with poor educational outcomes that can have long-term negative effects on the mental health, wellbeing, and socio-economic outcomes of university students. Mental health provision for university students with ADHD is often inadequate due to long waiting times for access to diagnosis and treatment in specialist National Health ...
Discuss the prevalence and impact of ADHD in children, adolescents and adults. Discuss ADHD as a disorder and how it differs from normal behaviour. Be able to critically assess key factors in the conceptualisation and understanding of the disorder. Discuss the core challenges faced by those with ADHD, their families and relevant professionals.
Design A survey within the Sheffield Treatments for ADHD Research project. A convenience sample of participants in the UK who consented to join an observational cohort were asked closed questions about medication, behavioural change programmes and service use, and an open-ended question about what else they used.
ADHD or attention deficit hyperactivity disorder is a common neurodevelopmental condition which affects around 6% of children and 3% of adults worldwide. It is characterised by developmentally inappropriate levels of inattention, impulsivity and hyperactivity. ADHD is also considered a form of neurodiversity, along with Autism Spectrum ...
Dr Powell concluded: "We know those with ADHD can be at an increased risk of developing prolonged and impairing depression. This study is the first of its kind, with no studies to date, have examined ADHD and its impact on depression presentation in recurrently depressed adults in mid-life. The findings suggest that recurrent depression may ...
Attention Deficit Hyperactivity Disorder (ADHD) is estimated to affect 3.5% of the global workforce. Despite the high prevalence rate, little is known about how best to support adults with ADHD (ADHDers) at work. Relevant research is dispersed across different disciplines such as medicine, health studies and psychology.
The most effective way to provide these data are through observational studies using large registry and research databases that can provide complementary data to that from clinical trials and meta-analyses. ... Thapar A, Sibley M, Arseneault L, Hechtman L, et al. Life span studies of ADHD-conceptual challenges and predictors of persistence and ...
ADHD diagnoses continue to increase, but Luise Kazda and colleagues argue that the push for diagnosis could be hampering access to care and support for children ### Key messages The prevalence of attention deficit/hyperactivity disorder (ADHD) in children has been rising for several decades,1234 including in countries with previously low rates.5 In Germany, for example, the prevalence of ADHD ...
ADHD exists in adults, but … The syndrome now known as ADHD was originally conceptualized as a childhood disorder, and various terms were used to describe it (Barkley, Citation 2015).By the late 1970s, studies following children with the syndrome into adulthood were beginning to be published (Conrad & Potter, Citation 2000).Researchers noted that although many children "outgrew" their ...
ADHD increases the risk of substance misuse disorders 1.5-fold (2.4-fold for smoking) and problematic media use 9.3-fold in adolescence 55 56 and increases the risk of becoming obese 1.23-fold for adolescent girls. 57 58 59 It is also associated with different forms of dysregulated eating in children and adolescents.
ADHD is a complex condition which can affect individuals in different ways. We are trying to understand more about ADHD and to help us do this, we are looking for volunteers to take part in research. We need as many people as possible to take part -wherever you live in the UK.
Stimulants and α 2-adrenergic agonists both improve symptoms of ADHD in preschool-age children, but they have different side effects. Karen O'Leary Research Highlights 13 May 2021 Nature Medicine
Medication used for ADHD can reduce the risk of premature death, says new research. A study by Southampton scientists, with the Karolinska Institute in Sweden and Örebro University, Indiana University, and Bloomington in the USA, found the risk of dying from unnatural causes, such as accidents and overdoses, can be reduced by a quarter.
Aston University - Birmingham. Researchers at Aston University are looking for individuals to participate in a study exploring cognition and mental health in neurodevelopmental conditions, such as ADHD. If you are interested, please contact doctoral researcher Karin Madericova at [email protected].
In the realm of ADHD research and clinical trials, several hospitals have emerged as key players in advancing our understanding and treatment of this condition. Massachusetts General Hospital, located in Boston, leads the way with six ongoing ADHD trials and an impressive track record of 33 completed studies since their initial foray into ADHD ...
Research participants required: Evaluating the impact of a wearable on Anxiety and Focus amongst adults with ADHD. Research participants required: 20 min video or phone call - Covid Experience. 2 London UK Studies On Non Medication Treatments For ADHD. UK Survey Mapping Adult ADHD Services In The UK. Potential Research To Help Individuals With ...
Most studies focused on young or middle-aged adults and most participants were male; more research is needed on how ADHD may impact older adults and other gender identities. Although long considered to disproportionately affect male children at approximately 3:1 ( 70 ), ADHD in adults has been reported to have gender ratios of 1.5:1 ( 71 ).
Evidence-based research is at the foundation of CHADD's efforts to improve the lives of individuals affected by ADHD. CHADD is committed to supporting researchers who study the many facets of ADHD. Researchers often seek human subjects to participate in these studies as they learn more about ADHD's diagnosis, treatment, and its implications ...
Researchers suggest that the smaller studies may not have been able to reliably detect the brain interactions leading to the complex behaviors seen in ADHD. The findings from this study help further our understanding of the brain processes contributing to ADHD symptoms—information that can help inform clinically relevant research and ...
For people with ADHD, the 2-year mortality risk is nearly 20% lower for people who take medication to treat the disorder, according to a new study.
An analysis of double-blind randomized controlled trials encompassing more than 10,000 patients across 35 studies found that giving patients EPA-predominant omega-3 fatty acids was able to produce ...
ADHD has a global prevalence of 5.9% to 7.1% in children and 1.2% to 7.3% in adults . While most studies address ADHD in children from 7 to 17 years old, it is important to outline that this condition is also present in adults. It has been proposed that the number of adults with ADHD has increased over the last 20 years.
The UK should recruit half a million people to help it become a hub for clinical trials of the next generation of dementia drugs, the top scientific adviser to a new government-backed initiative ...