- Share full article
Advertisement
Supported by

England Overhauls Medical Care for Transgender Youth
The National Health Service is closing England’s sole youth gender clinic, which had been criticized for long wait times and inadequate services.

By Azeen Ghorayshi
The National Health Service in England announced on Thursday that it was shutting down the country’s only youth gender clinic in favor of a more distributed and comprehensive network of medical care for adolescents seeking hormones and other gender treatments.
The closure followed an external review of the Tavistock clinic in London, which has served thousands of transgender patients since the 1990s. The review , which is ongoing, has raised several concerns, including about long wait times, insufficient mental health support and the surging number of young people seeking gender treatments.
The overhaul of services for transgender young people in England is part of a notable shift in medical practice across some European countries with nationalized health care systems. Some doctors there are concerned about the increase in numbers as well as the dearth of data on long-term safety and outcomes of medical transitions.
In the United States, doctors specializing in gender care for adolescents have mixed feelings about the reforms in Europe. Although many agree that more comprehensive health care for transgender youth is badly needed, as are more studies of the treatments, they worry that the changes will fuel the growing political movement in some states to ban such care entirely.
“How do we draw the line so that we keep care individualized while maintaining safety standards for everyone? That’s what we’re trying to sort out,” said Dr. Marci Bowers, a gynecologic and reconstructive surgeon and the incoming president of the World Professional Association for Transgender Health, who is transgender. “It’s the people on the ground who need to make these decisions, not people in Washington or state legislatures.”
The N.H.S. said current patients at the Tavistock clinic could continue to receive care there before transferring to two new hubs at children’s hospitals in London and Manchester. The new clinics will expand the country’s gender services while making sure children are adequately treated for autism, trauma and mental health issues. The specialists will also carry out clinical research on gender medications.
There are “critically important unanswered questions” about the use of puberty blockers, wrote Dr. Hilary Cass, head of the external review of the country’s youth gender identity services, in a letter to the head of N.H.S. England last week.
Puberty blockers, which are largely reversible, are intended to buy younger patients time to make weighty decisions about permanent medical changes. But Dr. Cass questioned whether most adolescents prescribed these drugs were given the support to reverse course, should they choose to.
Tavistock received more than 5,000 patient referrals in 2021, up from just 250 in 2011. The types of patients seeking referrals have also shifted over the past decade. When the clinic opened, it primarily served children who were assigned male at birth. Last year, two-thirds of its patients were assigned female at birth.
It is unclear why the number of patients has surged so drastically or why transgender boys are driving the increase.
Transgender advocates in Britain welcomed the changes but emphasized that many questions still remained about how they would affect care for young people.
“We are optimistic, cautiously optimistic, about the news,” said Susie Green, chief executive of Mermaids, an advocacy group for transgender and gender-diverse youth. “There is a two-and-a-half-year waiting list to be seen for your first appointment. We’ve seen the distress caused to young people because of that.”
But Ms. Green, who has a transgender adult daughter, said the group was concerned about whether mental health services would be prioritized over medical care. Gender diversity, she said, should not be treated as a mental disorder.
“We would not want any further barriers to be put in place in terms of access to medical intervention,” Ms. Green said.
In 2020, a former patient at Tavistock, Keira Bell, joined a highly publicized lawsuit against the clinic. She claimed that she was put on puberty blockers at 16 “after a series of superficial conversations with social workers,” and had her breasts removed at age 20, decisions she later regretted.
A high court initially ruled that children under 16 were unlikely to be mature enough to consent to such medical interventions. But that decision was reversed in September of last year, with judges ruling that “it was for clinicians rather than the court to decide” whether a young patient could provide informed consent.
In 2020, employees at Tavistock raised concerns about medical care at the clinic, prompting the N.H.S. to commission Dr. Cass, a pediatrician in London who was not affiliated with the clinic, for an external review. Her interim report was released in February of this year.
Sweden’s national health service determined this year that gender-related medical care for young people should only be provided in exceptional cases when children have clear distress over their gender, known as dysphoria. All adolescents who receive treatment will be required to be enrolled in clinical trials in order to collect more data on side effects and long-term outcomes. Finland took a similar stance last year.
“Our position is we cannot see this as just a rights issue,” Dr. Thomas Linden, director of the country’s National Board of Health and Welfare, said in a February interview. “We have to see patient safety and precision in the judgment. We have to be really to some degree sure that we are giving the right treatments to the right person.”
While these European countries have put some limits around transgender care, their approaches are far more permissive than those in some conservative U.S. states. A recent Alabama law made it a felony for doctors to prescribe puberty-blockers and hormones to minors. In Texas, parents who allow their children to receive gender treatments have been investigated for child abuse . Both states are tied up in court battles with civil rights groups.
Some American doctors worried that the changing standards in Europe would bolster the notion that gender treatments are dangerous for young people.
“My fear is that this is going to be interpreted as another notch against providing gender-affirming care for kids,” said Dr. Angela Goepferd, medical director of the Gender Health Program at Children’s Minnesota hospital. More services are needed, they said, not less. “That’s our challenge here.”
Azeen Ghorayshi covers the intersection of sex, gender and science for The Times. More about Azeen Ghorayshi
How to find an NHS gender dysphoria clinic
Trans and non-binary people's general health needs are the same as anyone else's. But trans people may have specific health needs in relation to gender dysphoria.
Your particular needs may be best addressed by transgender health services offered by NHS gender dysphoria clinics (GDCs).
All NHS GDCs are commissioned by NHS England, who set the service specifications for how they work.
A GP or another health professional can refer you directly to one of the GDCs. You do not need an assessment by a mental health service first. Neither does the GP need prior approval from their integrated care board (ICB).
The websites of the clinics listed on this page also have useful information for you to think about before you see a GP.
Children and young people's gender services
Children and young people should be referred to the National Referral Support Service for the NHS Children and Young People's Gender Service .
These NHS services specialise in helping young people with gender identity issues. They take referrals from anywhere in England.
Gender dysphoria clinics in London and the southeast
The Tavistock and Portman NHS Foundation Trust: Gender Dysphoria Clinic for Adults
Lief House 3 Sumpter House Finchley Road London NW3 5HR
Phone: 020 8938 7590
Email: [email protected]
The GDC website has an overview of information useful for anyone with gender identity needs, not just those in the area.
Gender dysphoria clinics in the north
Sheffield Health and Social Care NHS Foundation Trust Gender Dysphoria Service
Porterbrook Clinic Michael Carlisle Centre 75 Osborne Road Sheffield S11 9BF
Phone: 0114 271 6671
Email: [email protected]
The Sheffield clinic's website includes information about referrals, clinic opening hours and links to eligibility criteria.
Leeds and York Partnership NHS Foundation Trust Gender Dysphoria Service
Management Suite 1st Floor The Newsam Centre Seacroft Hospital York Road Leeds LS14 6WB
Phone: 0113 855 6346
Email: [email protected]
The Leeds clinic's website covers referrals, commonly used medicines and information on the clinic's Gender Outreach workers.
Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust Northern Region Gender Dysphoria Service
Benfield House Walkergate Park Benfield Road Newcastle NE6 4PF
Phone: 0191 287 6130
Email: [email protected]
The Northern Region Gender Dysphoria Service website has a range of leaflets, including information about referral, hormones and support groups.
Gender dysphoria clinics in the Midlands
Northamptonshire Healthcare NHS Foundation Trust Gender Dysphoria Clinic
Danetre Hospital H Block London Road Daventry Northamptonshire NN11 4DY
Phone: 03000 272858
Email: [email protected]
Visit the Northampton clinic's website for more information about how to get a referral and the role of the GP.
Nottinghamshire Healthcare NHS Foundation Trust The Nottingham Centre for Transgender Health
12 Broad Street Nottingham NG1 3AL
Phone: 0115 876 0160
Email: [email protected]
Visit The Nottingham Centre for Transgender Health website for more information about how to get a referral.
Gender dysphoria clinics in the southwest
Devon Partnership NHS Trust West of England Specialist Gender Dysphoria Clinic
The Laurels 11-15 Dix's Field Exeter EX1 1QA
Phone: 01392 677 077
Email: [email protected]
The Laurels' website has information about the types of services on offer and the help available during transition.
New gender dysphoria services in 2020
In 2020 new NHS gender dysphoria services for adults will open in Greater Manchester, London and Merseyside.
These services will be delivered by healthcare professionals with specialist skills and based in local NHS areas, such as sexual health services. Full details will be available once each service is opened.
Initially, access to these services will be available to people who are already on a waiting list to be seen at one of the established gender dysphoria clinics.
NHS England will assess how useful these new pilot services are.
Page last reviewed: 13 May 2020 Next review due: 13 May 2023
+44 204 513 2244
[email protected]
About MtF Gender Confirmation Surgery
Home » About Gender Reassignment Surgery
MtF Gender Reassignment Surgery FAQ’s
How much does mtf gender reassignment surgery cost, what happens at the consultation for mtf gender reassignment surgery, how do i prepare for my surgery, what happens on the day of surgery, what aftercare will be provided for me, what happens if there is a complication.
- The patient ignored the post-operative instructions.
- The patient failed to attend for the agreed postoperative examinations.
- The patient sustained physical injury out of our control.
- FFS – Facial Feminisation Surgery
- Hairline Lowering Foreheadplasty
- Brow Contouring
- Rhinoplasty
- Cheek Augmentation
- Chin Reduction / Shaping surgery
- Jaw Contouring Surgery
- Upper Lip Lift
- Lip Enhancement / Augmentation
- Thyroid cartilage reduction / Tracheal Shave
- Breast Augmentation
- Buttock Enhancement
- Body – Silhouette Shaping
- Revision genital surgery
- Revision neovaginal surgery
- Scar revision surgery
- Hormone Therapy
- Speech and communication therapy
- Psychological assessment, counselling, psychotherapy

Shane’s Top Surgery Testimonial

Do I really need Facial Feminisation Surgery?

Diary Meets… Gaynor Mary Warren-Wright

LGBTQ+ History Month 2022: Defining History

How does dilation work after Gender Confirmation Surgery?

Finding Gaynor: an uplifting story of embracing one’s true self
@londontransclinic
Londontransclinic.

- International edition
- Australia edition
- Europe edition

‘We actually don’t know much’: the scientists trying to close the knowledge gap in trans healthcare
Researchers are running trials on how hormone therapies affect trans people that will also benefit healthcare for the wider population
W hen Cameron Whitley was diagnosed with kidney failure seven years ago, the news came as a shock. But the situation was about to get worse. His doctor decided the diagnosis meant Whitley’s hormone therapy had to stop.
As a transgender man, now 42, who had taken testosterone for 10 years, the impact was brutal.
“Not only was I struggling with this new diagnosis that I’m in stage four kidney failure, now I’m being told that I can no longer have hormones,” said Whitley, an associate professor in the department of sociology at Western Washington University. “I cannot describe how horrible that moment was.”
Crucially, he says, the decision was completely unnecessary. “We call this within the medical community ‘ trans broken arm syndrome ’,” he said.

The term refers to medical situations – such as having a broken arm – that are unconnected to gender identity, yet healthcare providers act on the basis there is a connection.
“We didn’t have any established sense that being on hormones would be problematic. The hormones are not processed through the kidneys. So there was nothing that made it [necessary to stop them], but that was the first thing that was done,” he said.
Whitely has since transferred his care over to the University of Pennsylvania, which he described as “awesome [with] wonderful trans-competent care”.
An increase in the number of people coming out as transgender has led to growing use of hormone therapies, which help to change the body’s physical characteristics towards a certain gender.
But as Whitley found out, misunderstandings and knowledge gaps about their impact abound.
While hormone therapies are today best known for their use in contraception or to manage symptoms of menopause in cisgender women, they have for decades been given to people undergoing gender reassignment. The German doctor Magnus Hirschfeld was one of the first to offer such medications to his patients at his Institute for Sexual Research in Berlin, which he opened in 1919.
Many people who are trans say such “cross-sex” or “gender affirming” hormone therapies are crucial: allowing them to live in a way that makes them happy and significantly reducing the risk of depression and suicide.
However, their use in younger people with gender dysphoria is controversial, not least because of their potential impact on fertility and the irreversible changes they can produce.
Until recently, gender-affirming hormone therapies in England could be given on the NHS after the age of 16, and individuals must have been on drugs known as puberty blockers for at least a year.
Puberty blockers pause the physical changes associated with adolescence, but have themselves been a key focus of concern when it comes to the medical treatment of children with gender dysphoria due to questions about their safety and clinical effectiveness.
New rules released by NHS England this month mean puberty blockers will no longer be used in treatments for under-18s with gender dysphoria, except as part of a clinical trial. A spokesperson for NHS England said amendments to the cross-sex hormones policy are being finalised in light of the new rules.
But away from the public debate about who should have hormone therapies and when, growing numbers of researchers are beginning to delve into their impact on the body in a bid to improve healthcare for trans people – and for the wider population.
For trans men, hormone therapy typically involves taking testosterone – enabling the growth of facial hair and a deepening of the voice, amid other changes – while for trans women it typically means taking oestradiol, which promotes the growth of breasts and an increase in body fat.
While such medications are known to change external appearances, how they might affect other aspects of the body – from the way internal organs work, to blood pressure and even risk factors for diseases – has been unclear. And that isn’t just true for trans patients.
“Regardless of the type of [hormone] therapy and who is using it, we actually surprisingly as a healthcare profession don’t know much,” said Dr Sofia Ahmed of the University of Alberta, who is looking at the impact of hormone therapy on kidney and cardiovascular health in transgender people.

“In using hormonal contraception, for example, we know it prevents pregnancy, but we have a limited understanding of how it affects kidney function, blood pressure, cardiovascular health – and that holds true for truly any kind of hormone therapy.”
For trans people taking hormone therapies, medics have raised particular concerns over standard “healthy” ranges for metrics such as blood pressure, kidney filtration rates or liver function.
These ranges are known to differ between cisgender men and women, but it is unclear what a “healthy” range is for trans men and women taking hormones – a situation doctors have said could put trans patients at risk of receiving the wrong dose of a medication, diseases being missed or even conditions being erroneously diagnosed.
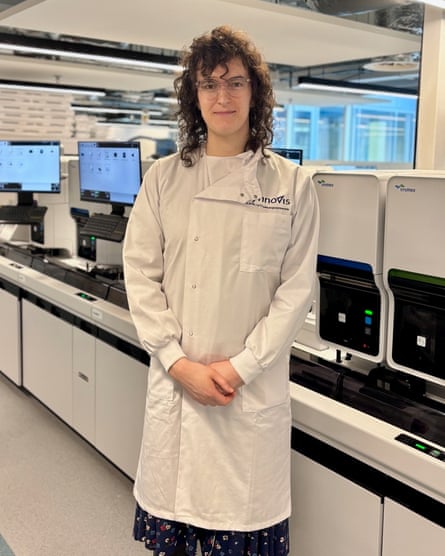
Among those attempting to resolve the issue is Devon Buchanan, a clinical scientist with Synnovis who is running a trial based at King’s College hospital that began in April 2021 and is recruiting 240 trans and non-binary people.
“We know that those ‘normal’ ranges are affected by gender affirming hormone therapy which a lot of trans people take and is very important to them,” she said.
Many previous studies have been small and the results unclear. “We wanted to cover a wide variety of tests and also have a larger sample size so that we could be more sure about the results,” said Buchanan.
Studies have also suggested rates of obesity in trans people are higher than among those who are cisgender, but the reason for such disparities is unclear. Dr Sascha Heinitz of the University of Leipzig is examining the effects of hormone therapy on eating behaviour, metabolism, energy balance and the cardiovascular system in transgender people.
He and colleagues are following 20 trans men and 20 trans women, and the same number of cisgender participants, over a two- to five-year period.
“We [are] just trying to understand [whether], during gender affirming hormone therapy, [are] there any changes going on that increase the risk of developing these diseases,” he said.
Even if evidence points to a greater metabolic risk in individuals receiving hormone therapy , as some research has suggested, further work will be needed to explore the extent to which that could be down to physiological response of the body to therapy, changes to experiences of gender dysphoria, or behavioural changes around consumption of food, Heinitz noted.
Also in Germany, Dr Sofia Forslund-Startceva of the Max Delbruck Center in Berlin and colleagues are running a clinical trial with 200 transgender people to explore whether risk factors for cardiovascular disease relating to changes in the makeup of the gut microbiome that are known in cis men and women emerge as trans men and women take hormone therapy.
“In so doing, we can both learn more about the mechanisms underlying health disparities between cis men and cis women, and learn more on when and where and after how long in transition a trans person [is] better treated as someone of their reassigned sex as of their birth assigned sex,” she said.
Such research could also help to achieve personalised medicine by offering insights into the relationship between health and changing levels of various hormones.
For example, risk factors for various diseases are known to increase among post menopausal cisgender women, who have lower oestrogen levels and higher levels of hormones known as FSH and LH compared with those who are younger.
“Where I would like to see this going, both in cisgender medicine, in intersex care and in trans care, is perhaps to recognise the importance of sex and gender in medicine and healthcare,” she said, adding “maleness” and “femaleness” can exist in individuals to different degrees.
In other words, given levels of sex hormones can undergo a profound shift across an individual’s lifespan, whether cisgender or transgender, understanding their impact could have important implications for everyone’s healthcare.
Work in transgender health is still a relatively new field, and funding can be a struggle, as can recruiting a meaningful number of participants who are representative of the community.
And research does not occur in a vacuum: around the world transgender issues are a hot political and social topic, whether it’s the age at which individuals can access hormone therapy or who can use single-sex spaces.
“It is my experience, also from my outpatient clinic, that there is not only lack of knowledge, but also lack of interest, and also people who do not want to treat transgender individuals,” said Heinitz. “I think some people just don’t want to touch the topic because it’s too hot.”

Forslund-Startceva said her impression was not that the topic was avoided out of any fear of controversy. “That said, there may be a reluctance at least on the part of some [who see themselves as trans allies] to approach it since they fear as outsiders to the demographic that they would not be able to research accountably,” she said.
Some advocate the “nothing about us without us” approach, stressing teams without transgender members risk misunderstanding the community they are seeking to work with, could end up failing to ask the best questions to inform their research, and might run into problems when it comes to communicating results in a nuanced and comprehensive way.
“[The latter] matters when research becomes weaponised so quickly, because people will latch on to potential interpretations and misinterpretations and use them one way or the other as culture war tools that can do a lot of damage,” said Forslund-Startceva.
But the value of lived experience among researchers is contested. “You cannot bring anything personal into [the research] except for inter-individual contact, being friendly and nice,” said Heinitz.
“To have transgender individuals in this field is great. Not to have them would be not so good. But I mean, it’s not important to have subjects with kidney disease conducting a study on kidney disease.”
Despite the challenges, scientists say the possibilities of the new wave of research into hormone therapies is exciting, offering the chance to fundamentally change healthcare for the transgender community and more widely. “It has multiple layers,” said Heinitz. “It’s a beautiful field, I think.”
Forslund-Startceva agreed. “We start in the understanding that health and disease risks and responses differ between cis men and cis women, but one cannot easily entangle different components of sex or gender – is it due to lifestyle, hormones or genetics?”
- Transgender
- Medical research

Children to stop getting puberty blockers at gender identity clinics, says NHS England

Green party sacking of spokesperson over trans rights views was procedurally unfair, court rules

Sunak refuses to apologise to Brianna Ghey’s father over PMQs trans jibe

Minister defends Sunak’s transgender jibe amid calls for apology

Brianna Ghey’s father demands apology from Sunak over transgender remark

Whether driven by Sunak’s callousness or clumsiness, trans jibe is PM’s new normal

Starmer condemns Sunak over trans rights jibe during PMQs visit by Brianna Ghey’s mother

Trans people in England more likely to have long-term poor mental health – study
Most viewed.
- Media & Government
- News and Views
The history of gender reassignment surgeries in the UK
For Pride Month, we are recognising the plastic surgeons who pioneered gender reassignment surgeries (GRS) in the UK. Gender reassignment surgery, also known as gender confirmation surgery or gender affirmation surgery, is a sub-speciality within plastic surgery, developed based on reconstructive procedures used in trauma and in congenital malformations. The specific procedures used for GRS have only been practised in the last 100 years.
Over the last decade, there has been an increase in society acknowledgement and acceptance of gender diverse persons. This catalysed an increase in referrals to gender identity clinics and an increase in the number of gender affirmation surgeries. GRS help by bringing fulfilment to many people who experience gender dysphoria. Gender dysphoria - a distress caused by the incongruence of a person's gender identity and their biological sex, drives the person to seek medical or surgical intervention to align some or all of their physical appearance with their gender identity. Patients with gender dysphoria experience higher rates of psychiatric disorders such as depression and anxiety. Gender-affirming medical intervention tends to resolve the psychiatric disorders that are a direct consequence of gender dysphoria.
Norman Haire (1892-1952) was a medical practitioner and a Sexologist. In his book, The Encyclopaedia of Sexual Knowledge (1933), he describes the first successful GRS. His patient, Dora Richter underwent 3 procedures reassigning from male to female between 1922-1931. The procedures included a vaginoplasty (surgical procedure where a vagina is created).
In the UK, gender reassignment surgeries were pioneered by Sir Harold Gillies. Harold Gillies is most famous for the development of a new method of facial reconstructive surgery, in 1917. During the Second World War, he organized plastic surgery units in various parts of Britain and inspired colleagues to do the same, training many doctors in this field. During the war, Gillies performed genital reconstruction surgeries for wounded soldiers.
British physician Laurence Michael Dillon (born Laura Maude Dillon) felt that they were not truly a woman. Gillies performed the first phalloplasty (surgery performed to construct the penis) on Dillon in 1946. In transitioning from female to male, Dillon underwent a total of 13 operations, over a period of 4 years.
Roberta Cowell (born Robert Marshall Cowell) is the first known Brit to undergo male to female GRS. After meeting Dillon and becoming close, Dillon operated illegally on Cowell. The operation helped her obtain documents confirming that she was intersex and have her birth gender formally re-registered as female. The operation that helped her transition was forbidden as it was considered “disfiguring” of a man who was otherwise qualified to serve in the military. Consequently, Gillies, assisted by American surgeon Ralph Millard performed a vaginoplasty on Roberta in 1951. The technique pioneered by Harold Gillies remained the standard for 40 years.
Gillies requested no publicity for his gender affirmation work. In response to the objections received from his peers, he replied that he was satisfied by the patient's written sentiments: “To Sir Harold Gillies, I owe my life and my happiness”. “If it gives real happiness,” Gillies wrote of his procedures, “that is the most that any surgeon or medicine can give.” These words highlight the importance of plastic surgery in the mental wellbeing of transgender patients.
The BAPRAS Collection and Archive has an extraordinary assembly of fascinating archive and historical surgical instruments dating from 1900. Visit https://www.bapras.org.uk/professionals/About/bapras-archive or email [email protected] for more information.
Please refer to our Privacy policy for important information on the use of cookies. By continuing to use this website, you agree to this.
Sorry, your browser isn't supported
Please click here to find out about upgrading.
You can also view the BAPRAS website on your tablet or mobile.
French Senate Report: Sex Change Surgery for Minors Could be ‘Greatest Ethical Scandal in the History of Medicine’’
As with “The Science™” behind covid and global warming, the French report indicated that reasoned debate was silenced and challenges to the woke ideology were dismissed.

- Facebook Messenger
History provides us with many examples of dreadful and horrific medical scandals and practices: The Tuskegee syphilis study, lobotomies for mental illness, and bloodletting as a cure-all , to name a few.
Recently, the French Senate added another one to the list: Sex reassignment surgery for minors .
French Senators want to ban gender transition treatments for under-18s, after a report described sex reassignment in minors as potentially “one of the greatest ethical scandals in the history of medicine”. googletag.cmd.push(function() { googletag.display('div-gpt-ad-1438094929688-2'); }); googletag.cmd.push(function() { googletag.display("div-hre-Legal-Insurrection-2605"); }); The report, commissioned by the opposition centre-Right Les Republicains (LR) party, documents various practices by health professionals, which it claims are indoctrinated by a “trans-affirmative” ideology under the sway of experienced trans-activist associations. The report, which cites a “tense scientific and medical debate”, accuses such associations of encouraging gender transition in minors via intense propaganda campaigns on social media. Jacqueline Eustache-Brinio, an LR senator who led the working group behind the report, concluded that “fashion plays a big role” in the rise of gender reassignment treatments.
Over a year ago, I did a detailed analysis of the devastating harm that could result from children using hormone-blocking therapies . While I have no medical degree, it takes only a modicum of basic understanding of biology and common sense to see that the rationale behind pressing for children to be permitted to receive these treatments (even at parental request) went against the Hippocratic Oath not to harm.
However, as with “The Science™” behind COVID and global warming, the reasoned debate was silenced, and challenges to the woke ideology were dismissed entirely. The French report explicitly points to the militant ideology promoting gender reassignment surgeries .
The report, which is detailed and well-argued, points to a number of abuses by health professionals, indoctrinated by a “trans-affirmative” ideology and subject to the influence of experienced trans activist associations. The report’s authors accuse these associations of unreasonably encouraging gender transition in minors via an intense propaganda campaign on social media. The scandal has been brewing for several months, thanks to the mobilisation of psychologists, psychiatrists, educators, and parents, who have denounced the ravages of this militant ideology among fragile and suffering young people, to whom gender transition is proposed as a miracle solution to the psychological problems they may be experiencing.
The report notes that trans activists have stifled debate, undermined science, and inserted themselves in between parents and children in the name of preventing discrimination: — “In France, as abroad, it appears that the scientific and medical debate on the subject is tense.… pic.twitter.com/wnCiijRFhT — Michael Shellenberger (@shellenberger) March 24, 2024
And, like the pseudoscience behind COVID and global warming, real scientists are now being heard, and hard data is being used to reverse the poor policy. France isn’t the only European nation beginning to set limits on when gender reassignment treatments can begin.
England has set the age to 16 .
The National Health Service England recently cemented a policy first issued on an interim basis almost a year ago that sets a minimum age at which puberty blockers can be started, along with other requirements. NHS England says there is not enough evidence about their long-term effects, including “sexual, cognitive or broader developmental outcomes.” Starting April 1, NHS England will not prescribe puberty blockers — drugs that suppress sex hormones during puberty — as a “routine treatment” to children and other young people seeking gender transitions. In practice, the decision also applies to Wales, which does not have any NHS gender clinics for children. Northern Ireland says it will adopt England’s policy; Scotland is weighing it.
Also, a report from the Netherlands indicates people with issues related to gender are sent to surgeries and intense medical treatment too quickly .
However, some of them would benefit more from treatment by their family doctor or psychological help, the Dutch daily Volkskrant writes based on a report from the Radboud University. The researchers speak of a “mismatch between the offered specialised care and the need of transgender people themselves.” Gender clinics often focus mainly on medical treatment with hormones and surgery, the newspaper writes. And some people have no need for that. Some would rather explore their gender identity than treat it, the Dutch daily NRC cites the report.
I don’t know if we have passed “peak woke.” However, I am hopeful we have passed peak “woke science.”

Donations tax deductible to the full extent allowed by law.
“However, as with “The Science™” behind COVID and global warming” Yeah not doing your credibility much good here
Ty Leslie.. I was curious about the image.. It was from a planned parenthood video. SMH At least they got some flack for it. Puberty is not an illness that you can fix with meds. TID…
https://www.dailymail.co.uk/video/news/video-2791817/Video-Planned-Parenthood-ad-puberty-blockers-spurs-massive-backlash.html
Leave a Comment
Leave a reply cancel reply.

CONTRIBUTORS
Sr. Contrib Editor
Contrib Editor
Weekend Editor
Editor Emerita
- Learn more about the Contributors

The NHS Ends the "Gender-Affirmative Care Model" for Youth in England
Following extensive stakeholder engagement and a systematic review of evidence , England’s National Health Service (NHS) has issued new draft guidance for the treatment of gender dysphoria in minors, which sharply deviates from the “gender-affirming” approach. The previous presumption that gender dysphoric youth <18 need specialty “transgender healthcare” has been supplanted by the developmentally-informed position that most need psychoeducation and psychotherapy. Eligibility determination for medical interventions will be made by a centralized Service and puberty blockers will be delivered only in research protocol settings. The abandonment of the "gender-affirming" model by England had been foreshadowed by The Cass Review's interim report , which defined "affirmative model" as a "model of gender healthcare that originated in the USA."
The reasons for the restructuring of gender services for minors in England are 4-fold. They include (1) a significant and sharp rise in referrals; (2) poorly-understood marked changes in the types of patients referred; (3) scarce and inconclusive evidence to support clinical decision-making, and (4) operational failures of the single gender clinic model, as evidenced by long wait times for initial assessment, and overall concern with the clinical approach.
The new NHS guidance recognizes social transition as a form of psychosocial intervention and not a neutral act, as it may have significant effects on psychological functioning. The NHS strongly discourages social transition in children, and clarifies that social transition in adolescents should only be pursued in order to alleviate or prevent clinically-significant distress or significant impairment in social functioning , and following an explicit informed consent process . The NHS states that puberty blockers can only be administered in formal research settings, due to the unknown effects of these interventions and the potential for harm. The NHS has not made an explicit statement about cross-sex hormones , but signaled that they too will likely only be available in research settings. The guidelines do not mention surgery , as surgery has never been a covered benefit under England’s NHS for minors.
The new NHS guidelines represent a repudiation of the past decade’s approach to management of gender dysphoric minors. The “gender-affirming” approach, endorsed by WPATH and characterized by the conceptualization of gender-dysphoric minors as “transgender children” has been replaced with a holistic view of identity development in children and adolescents. In addition, there is a new recognition that many gender-dysphoric adolescents suffer from mental illness and neurocognitive difficulties, which make it hard to predict the course of their gender identity development.
The key highlights of the NHS new guidance are provided below.*
1. Eliminates the “gender clinic” model of care and does away with “affirmation”
- The NHS has eliminated the “gender clinic” model of care where children are seen solely by a specialist gender dysphoria practitioner, replacing it with standard care in children’s hospital settings.
- Rather than “affirming” a transgender identity of young person, staff are encouraged to maintain a broad clinical perspective and to “embed the care of children and young people with gender uncertainty within a broader child and adolescent health context.”
- “Affirmation” has been largely eliminated from the language and the approach. What remains is the guidance to ensure that “assessments should be respectful of the experience of the child or young person and be developmentally informed.”
- Medical transition services will only be available through a centralized specialty Service, established for higher-risk cases. However, not all referred cases to the Service will be accepted, and not all accepted cases will be cleared for medical transition.
- Treatment pathway will be shaped, among other things, by the “clarity, persistence and consistency of gender incongruence, the presence and impact of other clinical needs, and family and social context.”
- The care plan articulated by the Service will be tailored to the specific needs of the individual following careful therapeutic exploration and “may require a focus on supporting other clinical needs and risks with networked local services.”
2. Classifies social gender transition as an active intervention eligible for informed consent
- The NHS is strongly discouraging social gender transition in prepubertal children.
- diagnosis of persistent and consistent gender dysphoria
- consideration and mitigation of risks associated with social transition
- clear and full understanding of the implications of social transition
- a determination of medical necessity of social transition to alleviate or prevent clinically significant distress or impairment in social functioning
- All adolescents will need to provide informed consent to social gender transition.
3. Establishes psychotherapy and psychoeducation as the first and primary line of treatment
- All gender dysphoric youth will first be treated with developmentally-informed psychotherapy and psychoeducation by their local treatment teams.
- Extensive focus has been placed on careful therapeutic exploration, and addressing the broader range of medical conditions in addition to gender dysphoria.
- For those wishing to pursue medical transition, eligibility for hormones will be determined by a centralized Service, upon referral from a GP (general practitioner) or another NHS provider.
4. Sharply curbs medical interventions and confines puberty blockers to research-only settings
- The NHS guidance states that the risks of puberty blockers are unknown and that they can only be administered in formal research settings. The eligibility for research settings is yet to be articulated.
- The NHS guidance leaves open that similar limitations will be imposed on cross-sex hormones due to uncertainty surrounding their use, but makes no immediate statements about restriction in cross-sex hormones use outside of formal research protocols.
- Surgery is not addressed in the guidance as the NHS has never considered surgery appropriate for minors.
5. Establishes new research protocols
- All children and young people being considered for hormone treatment will be prospectively enrolled into a research study.
- The goal of the research study to learn more about the effects of hormonal interventions, and to make a major international contribution of the evidence based in this area of medicine.
- The research will track the children into adulthood.
6. Reinstates the importance of “biological sex”
- The NHS guidance defines “gender incongruence” as a misalignment between the individual’s experience of their gender identity and their biological sex.
- The NHS guidance refers to the need to track biological sex for research purposes and outcome measures.
- Of note, biological sex has not been tracked by GIDS for a significant proportion of referrals in 2020-2021.
7. Reaffirms the preeminence of the DSM-5 diagnosis of “gender dysphoria” for treatment decisions
- The NHS guidance differentiates between the ICD-11 diagnosis of “gender incongruence,” which is not necessarily associated with distress, and the DSM-5 diagnosis of “gender dysphoria,” which is characterized by significant distress and/or functional impairments related to “gender incongruence."
- The NHS guidance states that treatments should be based on the DSM-5 diagnosis of “gender dysphoria.”
- Of note, WPATH SOC8 has made the opposite recommendation, instructing to treat based on the provision of the ICD-11 diagnosis of “gender incongruence.” “Gender incongruence” lacks clinical targets for treatment, beyond an individual’s own desire to bring their body into alignment with their internally-held view of their gender identity.
8. Clarifies the meaning of “multidisciplinary teams” as consisting of a wide range of clinicians with relevant expertise, rather than only “gender dysphoria” specialists
- The NHS guidance clarifies that a true multidisciplinary team is comprised not only of “gender dysphoria specialists,” but also of experts in pediatrics, autism, neurodisability and mental health, to enable holistic support and appropriate care for gender dysphoric youth.
- neurodevelopmental disorders such as autistic spectrum conditions
- mental health disorders including depressive conditions, anxiety and trauma
- endocrine conditions including disorders of sexual development pharmacology in the context of gender dysphoria
- risky behaviors such as deliberate self-harm and substance use
- complex family contexts including adoptions and guardianships
- a number of additional requirements for the multidisciplinary team composition and scope of activity have been articulated by the NHS.
9. Establishes primary outcome measures of “distress” and “social functioning”
- The rationale for medical interventions for gender-dysphoric minors has been a moving target, ranging from resolution of gender dysphoria to treatment satisfaction. The NHS has articulated two main outcome measures of treatment: clinically significant distress and social functioning .
- This is an important development, as it establishes primary outcome measures that can be used by researchers to assess comparative effectiveness of various clinical interventions.
10. Asserts that those who choose to bypass the newly-established protocol will not be supported by the NHS
- Families and youth planning to obtain hormones directly from online or another external non-NHS source will be strongly advised about the risks.
- Those choosing to take hormones outside the newly established NHS protocol will not be supported in their treatment pathway by NHS providers.
- Child safeguarding investigations may also be initiated if children and young people have obtained hormones outside the established protocols.
With the new NHS guidance, England joins Finland and Sweden as the three European countries who have explicitly deviated from WPATH guidelines and devised treatment approaches that sharply curb gender transition of minors. Psychotherapy will be provided as the first and usually only line of treatment for gender dysphoric youth.
The full text of the NHS guidance can be accessed here .
* This is a transitional protocol as the NHS works to establish a more mature network of children’s hospitals capable of caring for special needs of gender dysphoric youth. A fuller service specification will be published in 2023-4 following the publication of the Cass Review’s final report .
- Latest Latest
- The West The West
- Sports Sports
- Opinion Opinion
- Magazine Magazine
Perspective: The tide has turned in the UK on gender-affirming treatment for children
Legal action over puberty blockers prescribed to minors will likely reverberate across the atlantic.

By Valerie Hudson
Over the past few weeks, an amazing turn of the tide has occurred in the United Kingdom, one which has profound ramifications for the United States. It involves The Tavistock Clinic in England, the hub of gender-affirming treatment under the country’s National Health Service.
The term “gender-affirming treatment” refers to the steps of treating gender dysphoria first with puberty blockers, then with cross-sex hormones and finally, for a sizable number of patients, with sex reassignment surgery.
“Affirming” means that any questioning of whether this stepladder of treatment is appropriate for a particular person expressing gender dysphoria was considered inappropriate, practically akin to “ conversion therapy ,” which has been outlawed in most Western countries.
The first clues that all was not going to end well for the Tavistock model were cases of Keira Bell and Sonia Appleby , both decided several months ago. In the Appleby case, Sonia Appleby was employed in the clinic as the “safeguarding lead” for gender dysphoric children being treated at Tavistock. She raised concerns that medics were not keeping careful records, not screening children for mental health comorbidities, and were being inconsistent in their treatment of children. She was then officially reprimanded — for trying to do her job. The court awarded her damages.
In the more famous Bell case, Keira Bell is the young woman treated at Tavistock who brought suit because she felt she was fast-tracked for gender affirmation treatment by the clinic, even though as a minor she had little understanding of the long-term consequences of what she was supposedly consenting to undergo. Now detransitioned, Bell accused Tavistock of shunting children along a treatment path to irreversible changes they could not possibly understand, such as sterility, bone loss, altered brain development and even inability to ever experience sexual climax.
From Bell’s standpoint, she and other children had been experimented upon in the most cruel fashion. The verdict was unanimously in her favor. The high court found much of the treatment is not based on solid evidence at all, and that children under 16 simply could not consent to a treatment with such major and irreversible consequences.
These two cases presaged the next development, which is known in the U.K. as the Cass Report . Dr. Hilary Cass, a former president of the Royal College of Paediatrics and Child Health, was tasked by the Boris Johnson government with reviewing practices at Tavistock. Cass undertook a comprehensive literature review, a qualitative study of patients and clinicians at Tavistock, and a quantitative study of 9,000 patient outcomes. What she and her team found was disturbing . The evidence base for the treatment Tavistock was providing was found to be shaky and had already been repudiated by several other Western European countries, including Finland , Sweden and France .
Cass also found there was almost no follow-up of patients, and thus very little understanding of whether Tavistock’s treatment helped patients or not. In interviews, a number of patients and staff expressed concerns over the one-size-fits-all approach. Cass recommended, and the government agreed, that Tavistock be shuttered, that regional centers to treat gender dysphoria in a more whole-of-care fashion be established, and that a firm evidence base be established before puberty blockers, in particular, were used on children.
This week, the big news hit. A law firm in the U.K. is launching a class-action suit against Tavistock, and it anticipates that more than 1,000 clients will be joining the suit. The suit will accuse Tavistock of “multiple failures of duty of care” with regard to its pediatric patients suffering from gender dysphoria. The clinic will also be charged with having “recklessly prescribed puberty blockers with harmful side effects and (having) adopted an ‘unquestioning, affirmative approach’ to children identifying as transgender.”
The days of the “affirmation-only-no-debate” approach to pediatric gender dysphoric patients is over, at least in the U.K. This great turning of the tide in Britain has taken place in the space of approximately 11 months.
Will the same happen in the United States? I believe it will for pediatric cases. While most Americans take a live-and-let-live attitude toward adult transition, the increasing evidence that puberty blockers do not simply “press pause” on puberty and may have seriously damaging and irreversible effects on children who cannot meaningfully consent, is becoming too great to ignore. The American Association of Pediatrics is already embroiled in a civil war over the issue. In addition to states such as Florida and Texas pursuing investigations of clinicians and pharmaceutical companies, the law firm Girard Sharp appears poised to launch a similar class-action suit; the firm is soliciting reports of adverse effects of puberty blockers from the guardians and parents of children who have been treated with them.
What is currently termed “gender-affirming treatment” for pediatric patients is likely to one day be seen as one of the greatest medical scandals of the 21st century. The light that will be shone on the practice in U.S. courtrooms will see to that, as happened in the U.K.
Valerie M. Hudson is a university distinguished professor at The Bush School of Government and Public Service at Texas A&M University and a Deseret News contributor. Her views are her own.
England is limiting gender transitions for youths. U.S. legislators are watching

Legislators in at least two U.S. states are citing a recent decision in England to restrict gender transitions for young people as support for their own related proposals.
They weren’t the first to turn to other countries, notably in Europe, for policy and research ideas. Lawmakers across the U.S., where at least 23 states now have tightened or removed access to transgender health care for minors, have routinely cited non-U.S. research or policies as justification for their legislation.
Yet leading health organizations in the United States and Europe continue to decisively endorse gender-affirming care for both transgender youths and adults.
Among other things, they argue that restrictions on things like hormone therapy tend to single out transgender youths, even though other young people also can benefit from them. And transgender advocates and allies see a political attempt to erase them, cloaked as concern for children.
What did England change and why?
England, through rules put forth by its public health system, is limiting the ability of people younger than 16 to begin a medical gender transition.
The National Health Service England recently cemented a policy first issued on an interim basis almost a year ago that sets a minimum age at which puberty blockers can be started, along with other requirements. NHS England says there is not enough evidence about their long-term effects, including “sexual, cognitive or broader developmental outcomes.”
Starting April 1, NHS England will not prescribe puberty blockers — drugs that suppress sex hormones during puberty — as a “routine treatment” to children and other young people seeking gender transitions. In practice, the decision also applies to Wales, which does not have any NHS gender clinics for children. Northern Ireland says it will adopt England’s policy; Scotland is weighing it.
But it’s not a blanket, nationwide restriction. NHS England is just one health provider in the country, albeit a major one.
Puberty blockers are available for a cost at a few private clinics. And young people already taking them through the NHS — fewer than 100 in England, according to the BBC — can continue. The drugs will also be available to participants in clinical trials.
Britain’s Conservative government, which has been broadly critical of youth gender transitions, welcomed the NHS England decision. Even so, a proposal in Parliament to flatly make it illegal to provide puberty blockers to those under 16 is unlikely to become law.
The use of puberty blockers is not limited to gender transitions, but they can be an early step in one. They can pause puberty for gender-questioning youths until they are old enough to decide, after discussions with their families and health providers, on treatments that bring more-permanent changes.
What are U.S. legislators saying?
U.S. legislators and statehouse bills seeking to restrict transgender health care have often cited European science and policy, from countries including Finland, France, Sweden and Norway, as well as the U.K.
In Kansas, state Sen. Beverly Gossage cited England’s new policy last week when briefing fellow Republicans on a bill that would ban gender-affirming care for minors.
“In England, they’ve declared that there could be no gender-affirming care other than therapy for children because the scientific proof is not there,” Gossage said in comments that mischaracterized the NHS England guidelines. They do call for starting with counseling, as do those of other leading health organizations.
Republican leaders expect the ban to pass this week and hope they can override any veto by Gov. Laura Kelly, a Democrat.
In Georgia, Republican state Sen. Ben Watson pointed to Europe as he pushed a ban on gender-affirming care for children: “In light of the information and what’s been going on, not only in Europe, in the U.K., but here in the United States, this is the change that I’m proposing.”
'Deep concerns about hostility and harm'
Puberty blockers for adolescents who meet certain criteria are endorsed by major U.S. medical groups, along with the World Professional Association for Transgender Health, when administered properly. Those criteria include no age requirement.
“Puberty blockers have been prescribed for more than 40 years for safe and effective treatment of medical conditions including early puberty. The fact that NHS England is targeting only trans and gender diverse youth with this policy raises deep concerns about hostility and harm to LGTBQ+ people and their families,” WPATH and the European Association for Transgender Health said in a statement last week.
“Decisions about healthcare must be driven by clinical evidence, not by politics,” the statement continued. “The NHS has provided no indication what criteria it will use to monitor the harm its decision may cause, putting youth and families at enormous risk for no legitimate medical purpose.”
Last year, the American Academy of Pediatrics, which represents 67,000 pediatricians, unanimously voted to reaffirm its pro-stance on gender-affirming care for transgender children, including hormone treatments when appropriate.
Iridescent Riffel, a 27-year-old transgender woman and activist from Lawrence, Kansas, said she views the English policy as too conservative.
Puberty blockers help prevent people from developing physical features not in line with their gender identity, such as beards or breasts. For most teenagers, puberty is well underway or nearly complete by age 16. Treatments to alter physical features later in life to align with one’s identity can be costly and painful.
Transgender youths may find it harder to begin the process of social transitioning — or how a trans person changes how they present themselves to other people — once they start puberty, she said.
“It’s not just, ‘Oh, I’m uncomfortable with my body.’ It’s, ‘How are people perceiving me? Am I going to get judged? Are people going to judge me? Am I going to be unsafe for going out this way?’” she said.
A ban on gender-affirming care isn’t the true goal, Riffel said. Instead, it’s, “We just don’t want to see trans people in public life at all.”
The Associated Press
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
- Health and social care
- Public health
- Population screening programmes
- NHS abdominal aortic aneurysm (AAA) programme
- NHS population screening: information for transgender people
- NHS England
NHS population screening: information for trans and non-binary people
Updated 4 January 2023
Applies to England

© Crown copyright 2023
This publication is licensed under the terms of the Open Government Licence v3.0 except where otherwise stated. To view this licence, visit nationalarchives.gov.uk/doc/open-government-licence/version/3 or write to the Information Policy Team, The National Archives, Kew, London TW9 4DU, or email: [email protected] .
Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned.
This publication is available at https://www.gov.uk/government/publications/nhs-population-screening-information-for-transgender-people/nhs-population-screening-information-for-trans-people
This information is for trans (transgender) and non-binary people in England. It tells you about the adult NHS screening programmes that are available in England and explains who we invite for screening.
We use trans as an umbrella term to embrace the diverse range of identities outside the traditional male/female definitions. These include transgender, gender fluid and non-binary. Find more trans health information on NHS.UK .
Screening for trans people at a glance
Trans women and non-binary people assigned male at birth who are registered with a GP as female:
- are invited for breast screening
- are invited for bowel cancer screening
- do not need cervical screening as they do not have a cervix
- are not routinely invited for abdominal aortic aneurysm ( AAA ) screening but can request screening
Trans women and non-binary people assigned male at birth who are registered with a GP as male:
- are not routinely invited for breast screening but can request screening
- are invited for AAA screening
Trans men and non-binary people assigned female at birth who are registered with a GP as female:
- are invited for cervical screening
- are not invited for AAA screening
Trans men and non-binary people assigned female at birth who are registered with a GP as male:
- are not routinely invited for cervical screening but can request screening
- are invited for AAA screening but do not have a high risk of AAA
Trans men who are pregnant should be offered the same antenatal and newborn screening tests as all other pregnant individuals.
Breast screening
Breast screening is a free NHS test that is carried out at breast screening centres and at mobile breast screening units across England.
Breast screening can find cancers when they are too small to see or feel. Finding and treating cancer early gives you the best chance of survival. Screening will miss some cancers, and some cancers cannot be cured.
Taking part in breast screening is your choice. You can find out more information from your GP or by visiting NHS.UK .
Breast screening invitation process
All individuals from 50 up to their 71st birthday who are registered as female with their GP are automatically invited to breast screening. When you are due for screening, we will send you an invitation letter. It is not possible for individuals registered as male to have mammograms as part of the NHS Breast Screening Programme, but your GP can refer you for mammograms at a hospital near you (see the information for people registered as male below).
We invite you for breast screening every 3 years. Your first invitation will arrive sometime between the ages of 50 and 53. If you are trans it is important that your GP makes sure that your records are up to date so you are invited for screening correctly.
If you do not want to be invited for breast screening, you need to contact your local breast screening office. They will explain how you can opt out of breast screening.
It is important that you feel that you are treated with dignity and respect at all times.
Let your screening service know if you would:
- like your appointment at the beginning or end of a clinic
- prefer to be screened at your local breast screening centre rather than a mobile breast screening unit
Visit NHS.UK for your service’s contact details.

Trans men and non-binary people assigned female at birth
Registered with a gp as female.
If you are aged from 50 years up to your 71st birthday and registered with a GP as female, you will be routinely invited for breast screening. We recommend you consider having breast screening if you have not had chest reconstruction (top surgery) or still have breast tissue.
If you are worried about visiting a breast screening unit you can ring to arrange a more suitable appointment. For example, we can arrange for you to have an appointment at the beginning or end of a clinic.
Registered with a GP as male
If you are registered with a GP as male, you will not be invited for breast screening. If you have not had chest reconstruction (top surgery) and are aged 50 or over we suggest you talk to your GP . They can arrange a referral for you to have mammograms at a hospital near you.
You should keep aware of the symptoms of breast cancer , and contact your GP if you notice any unusual changes.
If you have had chest reconstruction (top surgery), we advise you have a conversation with your surgeon about the amount of breast tissue you have remaining. If they confirm you still have breast tissue, you can ask your GP to refer you for mammograms at a hospital near you.
Trans women and non-binary people assigned male at birth
Registered with a gp as a female.
If you are aged from 50 up to your 71st birthday and registered with a GP as female, you will be routinely invited for screening. Long-term hormone therapy can increase your risk of developing breast cancer so it is important that you consider going for breast screening when you are invited.
If you are registered with a GP as male, you will not be invited for breast screening.
If you have been on long-term hormone therapy you may be at increased risk of developing breast cancer. Your GP can arrange a referral for you to have mammograms at a hospital near you.
Breast screening test
A breast X-ray called a mammogram is used to look for signs of cancer. Each breast is pressed firmly between the plates of an X-ray machine for a few seconds. The pressure is needed to get good images and also reduce the radiation dose. Your test will be carried out by a specially trained female mammographer.
Some people say having a mammogram is uncomfortable and a few may find it painful, but the discomfort should pass quickly.
Breast screening usually involves 2 X-rays of each breast. People who have implants are offered the choice of additional X-rays so the mammographer can see as much breast tissue as possible.
Preparation
If you are a trans man or non-binary person assigned female at birth who is registered with a GP as female, has not had chest reconstruction (top surgery) and wears a binder, you will need to remove this before having your mammogram.
Private changing facilities will be available so that you can remove your binder just before having your mammogram. If you have any concerns about your appointment, you can contact your local breast screening service.
Breast screening results
For most people the mammograms will show no signs of cancer. If changes are seen on your X-rays, you will be recalled to an assessment clinic for more tests which will include:
- a breast examination
- more X-rays or ultrasound scans
You may also have a biopsy, where a small sample of tissue is taken from the breast with a needle.
Sometimes breast screening can pick up cancers that would never have caused harm, so people are treated for breast cancer that would never have been life-threatening.
Reducing your risk
Screening reduces the number of deaths from breast cancer by finding signs of disease at an early stage.
It is important to know what is normal for your body. If you notice any changes report them to your GP .
Cervical screening
Cervical screening (also known as a smear test) is a free NHS test that is carried out at your GP surgery or at some sexual health clinics. The test looks for early changes in the cells of the cervix.
Cervical screening aims to prevent cancer from developing in the cervix (neck of the womb).
It is important to go for screening as finding changes before they become cancer gives you the best chance of successful treatment.
Nearly all cervical cancers are caused by human papillomavirus ( HPV ). HPV is a very common virus – most people will be infected with it at some point in their life. It can be passed on through any type of sexual activity.
Screening will not prevent all cancers and not all cancers can be cured.
Taking part in cervical screening is your choice. You can find out more information from your GP or by visiting NHS.UK .
Cervical screening invitation process
We invite people registered as female for cervical screening every 3 years from the age of 25 to 49 and every 5 years from the ages of 50 to 64. We also invite people who are over 65 who have not been screened since age 50 or those who have recently had abnormal tests.
We send an invitation letter when the cervical screening test is due, asking you to make an appointment.
If you are trans it is important that your GP contacts the NHS Cervical Screening Programme so you are invited for screening correctly. If you do not want to be invited for screening you should contact your GP . They will be able to remove you from the cervical screening invitation list.
It is important that you feel that you are treated with dignity and respect at all times. If you are worried about having cervical screening, talk to your doctor or practice nurse.
If you are aged 25 to 64 and registered with a GP as female, you will be routinely invited for cervical screening. We recommend that you consider having cervical screening if you have not had a total hysterectomy and still have a cervix.
If you are aged 25 to 64 and registered with a GP as male, you will not be invited for cervical screening. However, if you have not had a total hysterectomy and still have a cervix, you should still consider having cervical screening. This is especially important if you have had any abnormal cervical screening results in the past. If this applies to you, let your GP or practice nurse know so you can talk to them about having the test.
If you are a trans woman or non-binary person assigned male at birth, you will not need to be screened as you do not have a cervix.
If you are registered with a GP as female, you will be routinely invited for cervical screening unless your GP has already told us you’re not eligible. We can update our records so you are not invited unnecessarily.
If you are registered with a GP as male, you will not be invited for cervical screening.
Cervical screening test
The nurse or doctor will put an instrument called a speculum into the vagina to help them see the cervix. They will then take a sample of cells with a soft brush.
If you are a trans man who has taken long-term testosterone, you may find screening uncomfortable or painful. You may want to talk to your doctor or nurse about using a different size speculum and some extra lubrication.
Cervical screening results
For most people their test results are normal. If cell changes are found you may need another cervical screening test, or an appointment at a colposcopy clinic where the cervix is looked at in detail.
Nearly all cervical cancers are caused by a virus called human papillomavirus ( HPV ) which is passed on through any type of sexual activity. If you are worried about your risk of developing cervical cancer you may want to speak to your GP or practice nurse.
We recommend you consider going for cervical screening every time you are invited, even if you have had a previous normal result.
Let your GP or practice nurse know if you think you should be invited for screening.
Even if you have had the HPV vaccine we still recommend you consider going for cervical screening when invited.
Consider stopping smoking, as smoking increases your risk of cervical cancer.
If you have symptoms such as unusual vaginal discharge or bleeding, or pain during or after sex, please speak to your doctor even if you have had a normal cervical screening result.
AAA screening
AAA screening is a free NHS test that is carried out in the community, including hospitals, health clinics and GP practices.
AAA screening involves a simple ultrasound scan to measure the abdominal aorta.
The aorta is the main blood vessel that supplies blood to the body. Sometimes the wall of the aorta in the abdomen can become weak and stretch to form an abdominal aortic aneurysm ( AAA ). There is a risk that an AAA may split or tear (rupture).
There is a high risk of dying from a ruptured AAA . Finding an aneurysm early gives you the best chance of treatment and survival. AAA screening reduces your risk of dying from a ruptured AAA .
Taking part in AAA screening is your choice. You can find out more information about AAA screening from your GP or by visiting NHS.UK .
AAA screening invitation process
AAAs are far more common in men aged over 65 than in women and younger men. That’s why the NHS AAA Screening Programme only invites for screening individuals registered as male. However, any trans woman will have the same risk as a man and should consider accessing screening.
Individuals registered as male are invited for an ultrasound scan to check the size of their abdominal aorta when they are 65.
Individuals over 65 can request a scan by contacting their local AAA screening service directly. Visit NHS.UK for contact details.
If you are trans it is important that your GP contacts the NHS AAA Screening Programme so you are invited for screening correctly. If you do not want to be invited for AAA screening, you will need to let us know.
If you are not sure if you should be screened or not, contact your local screening office. You will find your local screening office number and more information about clinic locations on NHS.UK .
Trans men and non-binary people assigned female at birth do not have the same risk of AAA as people assigned male at birth.
If you are registered with a GP as female, you will not be invited for AAA screening.
If you are a trans man aged 65 who is registered with a GP as male, you will be sent an appointment to attend for AAA screening. You can have AAA screening if you wish even though your risk is lower. If the clinic location or appointment time is not suitable, you can contact your local screening office to change this. You will find your local screening office phone number on your invitation letter.
If you are registered with a GP as female, you will not be invited for screening. However, if you are 65, you will have the same risk as a man aged 65 and should consider accessing screening. You can contact us to arrange a suitable appointment. Visit NHS.UK for contact details.
If you are aged 65 and registered with a GP as male, you will be invited for AAA screening.
Any trans woman or non-binary person assigned male at birth will have the same AAA risk as a man and should consider accessing screening.
AAA screening test
The test is a simple ultrasound scan of your abdomen to measure the size of the aorta. Your screening appointment usually takes about 10 to 15 minutes.
The screener will check your personal details and ask for your consent (permission) to do the ultrasound scan.
You will be asked to lie on your back and lift up your top. You will not need to undress completely. If you are wearing a binder, you may be asked to remove it.
The ultrasound scan is usually painless. It can be slightly uncomfortable as the screener may need to apply some pressure.
AAA screening results
The screener will give you your results following your scan.
It is not always possible to see your aorta at your screening test so you may be referred to hospital.
If your aorta is found to be bigger than normal, you will need regular scans to check if it is growing. Some people never need surgery for their AAA .
If your AAA is large you will be referred to a specialist team to discuss planned surgery. Large AAAs can be treated successfully with surgery.
Consider taking part in AAA screening and follow-up when you are invited.
You should also consider:
- stopping smoking
- drinking less alcohol
It is also important to maintain a healthy weight through a healthy diet and physical activity.
Bowel cancer screening
Bowel cancer screening starts with a test kit that is offered for use at home. If the result shows further tests are needed, you are offered a colonoscopy (an examination of the bowel).
Bowel cancer screening reduces your risk of dying from bowel cancer.
Finding cancer early gives you the best chance of survival.
Screening will miss some cancers, and some cancers cannot be cured.
Taking part in bowel cancer screening is your choice. You can find out more information from your GP or by visiting NHS.UK .
Bowel cancer screening invitation process
Both men and women are routinely invited for screening.
Bowel cancer screening is offered every 2 years from the ages of 60 to 74. This age range is gradually being extended down to age 50. People aged 75 and over can request a test kit every 2 years by calling the free programme helpline on 0800 707 60 60.
The home test kit
A bowel screening test kit and information pack will be sent to you when you are due for screening. You are asked to collect one or more samples of your poo using the test kit provided.
You will need to complete the test kit within the timeframe on the instructions and return it using the freepost packaging provided.
The test looks for tiny amounts of blood in the sample which you may not be able to see and which could be a sign of bowel cancer. You can contact the free NHS Bowel Cancer Screening Programme helpline for advice on 0800 707 60 60.
Results from the test kit
If blood is found, you will be referred for further tests. This may involve you having a colonoscopy, which looks at the lining of the bowel using a flexible camera. You may find this more uncomfortable if you have had gender reassignment surgery.
To reduce your risk of bowel cancer you should:
- consider taking part in screening, even if you have had a previous normal result
- try to eat a high-fibre diet with plenty of fruit and vegetables, take regular physical exercise and stop smoking
- visit your GP if you notice blood in your poo, a change in your bowel habit over a number of weeks or unexplained weight loss
Bowel cancer can run in families. If you are worried about your risk please speak to your GP .
Your personal information
It is your decision whether or not to have any of these tests.
The NHS Screening Programmes use personally identifiable information about you to ensure you are invited for screening at the right time. NHS England also uses your information to ensure you receive high quality care.
Find out more about how your information is used and protected, and your options . Find out how to opt out of screening .
Is this page useful?
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. We’ll send you a link to a feedback form. It will take only 2 minutes to fill in. Don’t worry we won’t send you spam or share your email address with anyone.
Utility Menu
- Request an Appointment
Popular Searches
- Adult Primary Care
- Orthopedic Surgery
GenderCare Center
At our center, we provide comprehensive care and support for people across the gender spectrum, from surgery to behavioral health to community resources.
Contact Us:
For all inquiries, patients, and providers.
Please contact us via phone, email, or fax.
Phone: 617.638.1833
Email: [email protected]
Fax: 617.414.7158
Select your language:
Our mission is to provide accessible, individualized, and comprehensive gender-affirming care for the communities we serve while also advancing education, research, and advocacy efforts across New England and beyond.
Non-Surgical GenderCare Services
Surgical gendercare services, patient resources, gender affirming healthcare map of new england, catch - child and adolescent transgender center for health, medical records, ways to support.
Private donations are essential in maintaining the level of care that our patients require and deserve. All donations are helpful in supporting project infrastructure of the GenderCare Center along with helping us develop and distribute best practice guidance for patients everywhere. Whether you are a patient, a parent, another relative, a thoughtful neighbor, a corporation, or a community organization, your contribution will greatly help BMC to continue its life-altering work.
Under “Gift Designation”, select “Direct my gift to”, choose “Other” from the dropdown box, and then write in the Center for Transgender Medicine and Surgery in the blank box below.
Please visit the BUMC Transgender Medicine Research Group website for information regarding ongoing clinical research on medical topics regarding transgender-identified individuals.
Latest from HealthCity
New research identifies actionable gaps in care for trans patients.
"The thing that really keeps me awake at night is that...compassion must guide knowledge and knowledge must guide compassion."
The "Colorado Option" Raises Concerns of LGBTQ Provider Privacy in Path to Health Equity
Allowing patients to search for providers by demographic information is a start but not a quick fix to creating culturally responsive healthcare
How a Surgical Oncologist Overcame His Own Hesitancy to Help His Patient Get Vaccinated
Broaching the topic with unvaccinated patients can be stressful. One BMC specialist says clinicians owe it to patients to overcome their own unease.
How to Talk with Unvaccinated Patients About Getting the COVID-19 Vaccine
More than 99% of COVID-19 deaths are among unvaccinated people. A new survey offers experts insights on how to talk with undecided patients.
Emergency Departments Have an Opportunity to Boost HIV Testing
To quell a rising epidemic, BMC has embedded HIV counselors in the ED to increase declining testing rates and connect people to effective treatment.
Seeking Health Justice for Black Americans Amid COVID-19 Pandemic
A panel examined white supremacy culture and how it drives inequities in COVID-19 testing, care, and vaccine access and offered paths for change.
The Johnson & Johnson Vaccine's Differences Are Pros, Not Cons
With a single dose, less strict storage requirements, and high efficacy against death, the new COVID-19 vaccine could help fill gaps in access.
Why Aren’t People Participating in COVID-19 Contact Tracing?
Contact tracing can help stop the spread of communicable diseases — but experts should take inequities into account for it to be useful for COVID-19.
4 Transformative Takeaways on Equitable Healthcare From TEDx
Healthcare experts share forward-thinking views on the medical community’s role in providing effective, authentic, and sustainable care.
Testing, Tracing, and Rebuilding Ties Key to Healthcare Reopening
Infection tracing study looks for sources and susceptibility in healthcare workers’ COVID infections.
COVID-19 and Racism: Changing Predictable Outcomes
Experts raise concerns for post-pandemic repercussions and call for prioritization of the social determinants within medicine.
Tackling Racism and Representation in the Health Sciences
Carving out space for a collaborative approach can accelerate the health industry's improvement in diversity, inclusion, and representation.
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Buyline Personal Finance
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- March Madness
- AP Top 25 Poll
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
England is limiting gender transitions for youths. US legislators are watching
FILE - The rainbow flag, a symbol of the LGBTQ+ community, flies over a building next to Nelson’s Column monument, right, in Trafalgar Square, central London, Britain, March 28, 2014. Legislators in at least two U.S. states are citing England’s recent decision to severely restrict gender transitions for young people as support for their own related bills. (AP Photo/Lefteris Pitarakis, File)
- Copy Link copied
Legislators in at least two U.S. states are citing a recent decision in England to restrict gender transitions for young people as support for their own related proposals.
They weren’t the first to turn to other countries, notably in Europe, for policy and research ideas. Lawmakers across the U.S., where at least 23 states now have tightened or removed access to transgender health care for minors, have routinely cited non-U.S. research or policies as justification for their legislation.
Yet leading health organizations in the United States and Europe continue to decisively endorse gender-affirming care for both transgender youths and adults.
Among other things, they argue that restrictions on things like hormone therapy tend to single out transgender youths, even though other young people also can benefit from them. And transgender advocates and allies see a political attempt to erase them, cloaked as concern for children.

Some information and perspectives on the global patchwork of health and public policies on gender-affirming care:
WHAT DID ENGLAND CHANGE AND WHY?
England, through rules put forth by its public health system, is limiting the ability of people younger than 16 to begin a medical gender transition.
The National Health Service England recently cemented a policy first issued on an interim basis almost a year ago that sets a minimum age at which puberty blockers can be started, along with other requirements. NHS England says there is not enough evidence about their long-term effects, including “sexual, cognitive or broader developmental outcomes.”
Starting April 1, NHS England will not prescribe puberty blockers — drugs that suppress sex hormones during puberty — as a “routine treatment” to children and other young people seeking gender transitions. In practice, the decision also applies to Wales, which does not have any NHS gender clinics for children. Northern Ireland says it will adopt England’s policy; Scotland is weighing it.
But it’s not a blanket, nationwide restriction. NHS England is just one health provider in the country, albeit a major one.
Puberty blockers are available for a cost at a few private clinics. And young people already taking them through the NHS — fewer than 100 in England, according to the BBC — can continue. The drugs will also be available to participants in clinical trials.
Britain’s Conservative government, which has been broadly critical of youth gender transitions, welcomed the NHS England decision. Even so, a proposal in Parliament to flatly make it illegal to provide puberty blockers to those under 16 is unlikely to become law.
The use of puberty blockers is not limited to gender transitions, but they can be an early step in one. They can pause puberty for gender-questioning youths until they are old enough to decide, after discussions with their families and health providers, on treatments that bring more-permanent changes.
WHAT ARE US LEGISLATORS SAYING?
U.S. legislators and statehouse bills seeking to restrict transgender health care have often cited European science and policy, from countries including Finland, France, Sweden and Norway, as well as the U.K.
In Kansas, state Sen. Beverly Gossage cited England’s new policy last week when briefing fellow Republicans on a bill that would ban gender-affirming care for minors.
“In England, they’ve declared that there could be no gender-affirming care other than therapy for children because the scientific proof is not there,” Gossage said in comments that mischaracterized the NHS England guidelines. They do call for starting with counseling, as do those of other leading health organizations.
Republican leaders expect the ban to pass this week and hope they can override any veto by Gov. Laura Kelly, a Democrat.
In Georgia, Republican state Sen. Ben Watson pointed to Europe as he pushed a ban on gender-affirming care for children: “In light of the information and what’s been going on, not only in Europe, in the U.K., but here in the United States, this is the change that I’m proposing.”
‘DEEP CONCERNS ABOUT HOSTILITY AND HARM’
Puberty blockers for adolescents who meet certain criteria are endorsed by major U.S. medical groups, along with the World Professional Association for Transgender Health, when administered properly. Those criteria include no age requirement.
“Puberty blockers have been prescribed for more than 40 years for safe and effective treatment of medical conditions including early puberty. The fact that NHS England is targeting only trans and gender diverse youth with this policy raises deep concerns about hostility and harm to LGTBQ+ people and their families,” WPATH and the European Association for Transgender Health said in a statement last week.
“Decisions about healthcare must be driven by clinical evidence, not by politics,” the statement continued. “The NHS has provided no indication what criteria it will use to monitor the harm its decision may cause, putting youth and families at enormous risk for no legitimate medical purpose.”
Last year, the American Academy of Pediatrics, which represents 67,000 pediatricians, unanimously voted to reaffirm its pro-stance on gender-affirming care for transgender children, including hormone treatments when appropriate.
Iridescent Riffel, a 27-year-old transgender woman and activist from Lawrence, Kansas, said she views the English policy as too conservative.
Puberty blockers help prevent people from developing physical features not in line with their gender identity, such as beards or breasts. For most teenagers, puberty is well underway or nearly complete by age 16. Treatments to alter physical features later in life to align with one’s identity can be costly and painful.
Transgender youths may find it harder to begin the process of social transitioning — or how a trans person changes how they present themselves to other people — once they start puberty, she said.
“It’s not just, ‘Oh, I’m uncomfortable with my body.’ It’s, ‘How are people perceiving me? Am I going to get judged? Are people going to judge me? Am I going to be unsafe for going out this way?’” she said.
A ban on gender-affirming care isn’t the true goal, Riffel said. Instead, it’s, “We just don’t want to see trans people in public life at all.”
McMillan reported from northeastern Pennsylvania. Contributing to this report were Associated Press writers Jill Lawless in London, John Hanna in Topeka, Kansas, and Jeff Amy in Atlanta.

IMAGES
COMMENTS
You can contact the Gender Recognition Panel admin team. They cannot help you update your driving licence, update your passport or change your name. Gender Recognition Panel. GRPenquiries@justice ...
You can still apply through this route even if you do have a gender dysphoria diagnosis, so long as you meet all the requirements. However, you do not need to have had any gender affirmation ...
Treatment Gender dysphoria. Treatment. Treatment for gender dysphoria aims to help people live the way they want to, in their preferred gender identity or as non-binary. What this means will vary from person to person, and is different for children, young people and adults. Waiting times for referral and treatment are currently long.
Ministers have ruled out changes to make it easier for transgender people in England and Wales to have their gender legally recognised. They have rejected calls for people to be able to self ...
The Gender Recognition (Disclosure of Information) (England) Order 2022 (the order) is a statutory instrument that prescribes that those facilitating, assisting or undertaking the research on ...
The percentage of the population aged 16 years and over who reported that their gender identity was different from their sex at birth was slightly higher in England (0.55%) than it was in Wales (0.40%). Within England, the region with the highest percentage who reported that their gender identity was different from their sex at birth was London ...
About 7,000 certificates have been issued in England, Wales and Scotland. Image source, ... including gender reassignment and sex - and protects those groups from discrimination.
A 14-year-old transgender boy is starting legal proceedings against NHS England over delays to gender reassignment treatment. The teenager has waited over a year for referral to the only NHS ...
NHS England has acted unlawfully by making thousands of patients with gender dysphoria ... of seeking gender reassignment but due to "rapidly increasing demand and limited specialist services ...
A landmark test case to establish whether children can give informed consent to medical treatment for gender reassignment begins in the high court this week. Lawyers acting for Susan Evans, a ...
England Overhauls Medical Care for Transgender Youth. The National Health Service is closing England's sole youth gender clinic, which had been criticized for long wait times and inadequate ...
Devon Partnership NHS Trust West of England Specialist Gender Dysphoria Clinic. The Laurels 11-15 Dix's Field Exeter EX1 1QA. Phone: 01392 677 077. Email: [email protected]. The Laurels' website has information about the types of services on offer and the help available during transition.
The user requirement for data on those with the protected characteristic of gender reassignment is strengthened by the Equality Act 2010. ... Statistician's recommendation, be a predominantly "online census of all households and communal establishments in England and Wales in 2021, as a modern successor to the traditional, paper-based ...
What the Equality Act says about gender reassignment discrimination. The Equality Act 2010 says that you must not be discriminated against because of gender reassignment. In the Equality Act, gender reassignment means proposing to undergo, undergoing or having undergone a process to reassign your sex. To be protected from gender reassignment ...
Monday 08:00-20:00. Tuesday 08:00-20:00. Wednesday 08:00-20:00. Thursday 08:00-20:00. Friday 08:00-20:00. Saturday CLOSED. Sunday CLOSED. MtF gender confirmation surgery GCS or gender reassignment surgery, the final stage in the physical transitioning of a transgender person.
Until recently, gender-affirming hormone therapies in England could be given on the NHS after the age of 16, and individuals must have been on drugs known as puberty blockers for at least a year.
Chris Jones, Ofsted's Director, Corporate Strategy, discusses research on teaching about the protected characteristics of sex, sexual orientation and gender reassignment in England's schools.
The procedures included a vaginoplasty (surgical procedure where a vagina is created). In the UK, gender reassignment surgeries were pioneered by Sir Harold Gillies. Harold Gillies is most famous for the development of a new method of facial reconstructive surgery, in 1917. During the Second World War, he organized plastic surgery units in ...
France isn't the only European nation beginning to set limits on when gender reassignment treatments can begin. England has set the age to 16 . The National Health Service England recently cemented a policy first issued on an interim basis almost a year ago that sets a minimum age at which puberty blockers can be started, along with other ...
Following extensive stakeholder engagement and a systematic review of evidence, England's National Health Service (NHS) has issued new draft guidance for the treatment of gender dysphoria in minors, which sharply deviates from the "gender-affirming" approach. The previous presumption that gender dysphoric youth under 18 need specialty "transgender healthcare" has been supplanted by ...
A law firm in the U.K. is launching a class-action suit against Tavistock, and it anticipates that more than 1,000 clients will be joining the suit. The suit will accuse Tavistock of "multiple failures of duty of care" with regard to its pediatric patients suffering from gender dysphoria. The clinic will also be charged with having ...
Britain's Conservative government, which has been broadly critical of youth gender transitions, welcomed the NHS England decision. Even so, a proposal in Parliament to flatly make it illegal to ...
Gender Reassignment Policy. 1. SCOPE. This policy sets out UGLE's approach to the issues raised for Freemasonry by gender reassignment. It is intended to help guide Lodges in their decision making. It does not impose binding rules and although it gives some general guidance on discrimination law it does not constitute legal advice.
You may find this more uncomfortable if you have had gender reassignment surgery. Reducing your risk. ... NHS England also uses your information to ensure you receive high quality care.
A move to irreversible sex reassignment surgery (gender affirmation surgery) may follow a few years later for some individuals, typically at an age greater than 18 years and is ... (masculinising or feminising hormones) as part of the Children and Young People's Gender Service Author: NHS England Subject: Prescribing of Gender Affirming ...
Contact Us617.638.1833. Select your language: English. Español. Our mission is to provide accessible, individualized, and comprehensive gender-affirming care for the communities we serve while also advancing education, research, and advocacy efforts across New England and beyond.
England, through rules put forth by its public health system, is limiting the ability of people younger than 16 to begin a medical gender transition. The National Health Service England recently cemented a policy first issued on an interim basis almost a year ago that sets a minimum age at which puberty blockers can be started, along with other ...