Overview and General Information about Oral Presentation
- Daily Presentations During Work Rounds
- The New Patient Presentation
- The Holdover Admission Presentation
- Outpatient Clinic Presentations
- The structure of presentations varies from service to service (e.g. medicine vs. surgery), amongst subspecialties, and between environments (inpatient vs. outpatient). Applying the correct style to the right setting requires that the presenter seek guidance from the listeners at the outset.
- Time available for presenting is rather short, which makes the experience more stressful.
- Individual supervisors (residents, faculty) often have their own (sometimes quirky) preferences regarding presentation styles, adding another layer of variability that the presenter has to manage.
- Students are evaluated/judged on the way in which they present, with faculty using this as one way of gauging a student’s clinical knowledge.
- Done well, presentations promote efficient, excellent care. Done poorly, they promote tedium, low morale, and inefficiency.
General Tips:
- Practice, Practice, Practice! Do this on your own, with colleagues, and/or with anyone who will listen (and offer helpful commentary) before you actually present in front of other clinicians. Speaking "on-the-fly" is difficult, as rapidly organizing and delivering information in a clear and concise fashion is not a naturally occurring skill.
- Immediately following your presentations, seek feedback from your listeners. Ask for specifics about what was done well and what could have been done better – always with an eye towards gaining information that you can apply to improve your performance the next time.
- Listen to presentations that are done well – ask yourself, “Why was it good?” Then try to incorporate those elements into your own presentations.
- Listen to presentations that go poorly – identify the specific things that made it ineffective and avoid those pitfalls when you present.
- Effective presentations require that you have thought through the case beforehand and understand the rationale for your conclusions and plan. This, in turn, requires that you have a good grasp of physiology, pathology, clinical reasoning and decision-making - pushing you to read, pay attention, and in general acquire more knowledge.
- Think about the clinical situation in which you are presenting so that you can provide a summary that is consistent with the expectations of your audience. Work rounds, for example, are clearly different from conferences and therefore mandate a different style of presentation.
- Presentations are the way in which we tell medical stories to one another. When you present, ask yourself if you’ve described the story in an accurate way. Will the listener be able to “see” the patient the same way that you do? Can they come to the correct conclusions? If not, re-calibrate.
- It's O.K. to use notes, though the oral presentation should not simply be reduced to reading the admission note – rather, it requires appropriate editing/shortening.
- In general, try to give your presentations on a particular service using the same order and style for each patient, every day. Following a specific format makes it easier for the listener to follow, as they know what’s coming and when they can expect to hear particular information. Additionally, following a standardized approach makes it easier for you to stay organized, develop a rhythm, and lessens the chance that you’ll omit elements.

Specific types of presentations
There are a number of common presentation-types, each with its own goals and formats. These include:
- Daily presentations during work rounds for patients known to a service.
- Newly admitted patients, where you were the clinician that performed the H&P.
- Newly admitted patients that were “handed off” to the team in the morning, such that the H&P was performed by others.
- Outpatient clinic presentations, covering several common situations.
Key elements of each presentation type are described below. Examples of how these would be applied to most situations are provided in italics. The formats are typical of presentations done for internal medicine services and clinics.
Note that there is an acceptable range of how oral presentations can be delivered. Ultimately, your goal is to tell the correct story, in a reasonable amount of time, so that the right care can be delivered. Nuances in the order of presentation, what to include, what to omit, etc. are relatively small points. Don’t let the pursuit of these elements distract you or create undue anxiety.
Daily presentations during work rounds of patients that you’re following:
- Organize the presenter (forces you to think things through)
- Inform the listener(s) of 24 hour events and plan moving forward
- Promote focused discussion amongst your listeners and supervisors
- Opportunity to reassess plan, adjust as indicated
- Demonstrate your knowledge and engagement in the care of the patient
- Rapid (5 min) presentation of the key facts
Key features of presentation:
- Opening one liner: Describe who the patient is, number of days in hospital, and their main clinical issue(s).
- 24-hour events: Highlighting changes in clinical status, procedures, consults, etc.
- Subjective sense from the patient about how they’re feeling, vital signs (ranges), and key physical exam findings (highlighting changes)
- Relevant labs (highlighting changes) and imaging
- Assessment and Plan : Presented by problem or organ systems(s), using as many or few as are relevant. Early on, it’s helpful to go through the main categories in your head as a way of making sure that you’re not missing any relevant areas. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
Example of a daily presentation for a patient known to a team:
- Opening one liner: This is Mr. Smith, a 65 year old man, Hospital Day #3, being treated for right leg cellulitis
- MRI of the leg, negative for osteomyelitis
- Evaluation by Orthopedics, who I&D’d a superficial abscess in the calf, draining a moderate amount of pus
- Patient appears well, states leg is feeling better, less painful
- T Max 101 yesterday, T Current 98; Pulse range 60-80; BP 140s-160s/70-80s; O2 sat 98% Room Air
- Ins/Outs: 3L in (2 L NS, 1 L po)/Out 4L urine
- Right lower extremity redness now limited to calf, well within inked lines – improved compared with yesterday; bandage removed from the I&D site, and base had small amount of purulence; No evidence of fluctuance or undrained infection.
- Creatinine .8, down from 1.5 yesterday
- WBC 8.7, down from 14
- Blood cultures from admission still negative
- Gram stain of pus from yesterday’s I&D: + PMNS and GPCs; Culture pending
- MRI lower extremity as noted above – negative for osteomyelitis
- Continue Vancomycin for today
- Ortho to reassess I&D site, though looks good
- Follow-up on cultures: if MRSA, will transition to PO Doxycycline; if MSSA, will use PO Dicloxacillin
- Given AKI, will continue to hold ace-inhibitor; will likely wait until outpatient follow-up to restart
- Add back amlodipine 5mg/d today
- Hep lock IV as no need for more IVF
- Continue to hold ace-I as above
- Wound care teaching with RNs today – wife capable and willing to assist. She’ll be in this afternoon.
- Set up follow-up with PMD to reassess wound and cellulitis within 1 week
The Brand New Patient (admitted by you)
- Provide enough information so that the listeners can understand the presentation and generate an appropriate differential diagnosis.
- Present a thoughtful assessment
- Present diagnostic and therapeutic plans
- Provide opportunities for senior listeners to intervene and offer input
- Chief concern: Reason why patient presented to hospital (symptom/event and key past history in one sentence). It often includes a limited listing of their other medical conditions (e.g. diabetes, hypertension, etc.) if these elements might contribute to the reason for admission.
- The history is presented highlighting the relevant events in chronological order.
- 7 days ago, the patient began to notice vague shortness of breath.
- 5 days ago, the breathlessness worsened and they developed a cough productive of green sputum.
- 3 days ago his short of breath worsened to the point where he was winded after walking up a flight of stairs, accompanied by a vague right sided chest pain that was more pronounced with inspiration.
- Enough historical information has to be provided so that the listener can understand the reasons that lead to admission and be able to draw appropriate clinical conclusions.
- Past history that helps to shed light on the current presentation are included towards the end of the HPI and not presented later as “PMH.” This is because knowing this “past” history is actually critical to understanding the current complaint. For example, past cardiac catheterization findings and/or interventions should be presented during the HPI for a patient presenting with chest pain.
- Where relevant, the patient's baseline functional status is described, allowing the listener to understand the degree of impairment caused by the acute medical problem(s).
- It should be explicitly stated if a patient is a poor historian, confused or simply unaware of all the details related to their illness. Historical information obtained from family, friends, etc. should be described as such.
- Review of Systems (ROS): Pertinent positive and negative findings discovered during a review of systems are generally incorporated at the end of the HPI. The listener needs this information to help them put the story in appropriate perspective. Any positive responses to a more inclusive ROS that covers all of the other various organ systems are then noted. If the ROS is completely negative, it is generally acceptable to simply state, "ROS negative.”
- Other Past Medical and Surgical History (PMH/PSH): Past history that relates to the issues that lead to admission are typically mentioned in the HPI and do not have to be repeated here. That said, selective redundancy (i.e. if it’s really important) is OK. Other PMH/PSH are presented here if relevant to the current issues and/or likely to affect the patient’s hospitalization in some way. Unrelated PMH and PSH can be omitted (e.g. if the patient had their gall bladder removed 10y ago and this has no bearing on the admission, then it would be appropriate to leave it out). If the listener really wants to know peripheral details, they can read the admission note, ask the patient themselves, or inquire at the end of the presentation.
- Medications and Allergies: Typically all meds are described, as there’s high potential for adverse reactions or drug-drug interactions.
- Family History: Emphasis is placed on the identification of illnesses within the family (particularly among first degree relatives) that are known to be genetically based and therefore potentially heritable by the patient. This would include: coronary artery disease, diabetes, certain cancers and autoimmune disorders, etc. If the family history is non-contributory, it’s fine to say so.
- Social History, Habits, other → as relates to/informs the presentation or hospitalization. Includes education, work, exposures, hobbies, smoking, alcohol or other substance use/abuse.
- Sexual history if it relates to the active problems.
- Vital signs and relevant findings (or their absence) are provided. As your team develops trust in your ability to identify and report on key problems, it may become acceptable to say “Vital signs stable.”
- Note: Some listeners expect students (and other junior clinicians) to describe what they find in every organ system and will not allow the presenter to say “normal.” The only way to know what to include or omit is to ask beforehand.
- Key labs and imaging: Abnormal findings are highlighted as well as changes from baseline.
- Summary, assessment & plan(s) Presented by problem or organ systems(s), using as many or few as are relevant. Early on, it’s helpful to go through the main categories in your head as a way of making sure that you’re not missing any relevant areas. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
- The assessment and plan typically concludes by mentioning appropriate prophylactic considerations (e.g. DVT prevention), code status and disposition.
- Chief Concern: Mr. H is a 50 year old male with AIDS, on HAART, with preserved CD4 count and undetectable viral load, who presents for the evaluation of fever, chills and a cough over the past 7 days.
- Until 1 week ago, he had been quite active, walking up to 2 miles a day without feeling short of breath.
- Approximately 1 week ago, he began to feel dyspneic with moderate activity.
- 3 days ago, he began to develop subjective fevers and chills along with a cough productive of red-green sputum.
- 1 day ago, he was breathless after walking up a single flight of stairs and spent most of the last 24 hours in bed.
- Diagnosed with HIV in 2000, done as a screening test when found to have gonococcal urethritis
- Was not treated with HAART at that time due to concomitant alcohol abuse and non-adherence.
- Diagnosed and treated for PJP pneumonia 2006
- Diagnosed and treated for CMV retinitis 2007
- Became sober in 2008, at which time interested in HAART. Started on Atripla, a combination pill containing: Efavirenz, Tonofovir, and Emtricitabine. He’s taken it ever since, with no adverse effects or issues with adherence. Receives care thru Dr. Smiley at the University HIV clinic.
- CD4 count 3 months ago was 400 and viral load was undetectable.
- He is homosexual though he is currently not sexually active. He has never used intravenous drugs.
- He has no history of asthma, COPD or chronic cardiac or pulmonary condition. No known liver disease. Hepatitis B and C negative. His current problem seems different to him then his past episode of PJP.
- Review of systems: negative for headache, photophobia, stiff neck, focal weakness, chest pain, abdominal pain, diarrhea, nausea, vomiting, urinary symptoms, leg swelling, or other complaints.
- Hypertension x 5 years, no other known vascular disease
- Gonorrhea as above
- Alcohol abuse above and now sober – no known liver disease
- No relevant surgeries
- Atripla, 1 po qd
- Omeprazole 20 mg, 1 PO, qd
- Lisinopril 20mg, qd
- Naprosyn 250 mg, 1-2, PO, BID PRN
- No allergies
- Both of the patient's parents are alive and well (his mother is 78 and father 80). He has 2 brothers, one 45 and the other 55, who are also healthy. There is no family history of heart disease or cancer.
- Patient works as an accountant for a large firm in San Diego. He lives alone in an apartment in the city.
- Smokes 1 pack of cigarettes per day and has done so for 20 years.
- No current alcohol use. Denies any drug use.
- Sexual History as noted above; has sex exclusively with men, last partner 6 months ago.
- Seated on a gurney in the ER, breathing through a face-mask oxygen delivery system. Breathing was labored and accessory muscles were in use. Able to speak in brief sentences, limited by shortness of breath
- Vital signs: Temp 102 F, Pulse 90, BP 150/90, Respiratory Rate 26, O2 Sat (on 40% Face Mask) 95%
- HEENT: No thrush, No adenopathy
- Lungs: Crackles and Bronchial breath sounds noted at right base. E to A changes present. No wheezing or other abnormal sounds noted over any other area of the lung. Dullness to percussion was also appreciated at the right base.
- Cardiac: JVP less than 5 cm; Rhythm was regular. Normal S1 and S2. No murmurs or extra heart sounds noted.
- Abdomen and Genital exams: normal
- Extremities: No clubbing, cyanosis or edema; distal pulses 2+ and equal bilaterally.
- Skin: no eruptions noted.
- Neurological exam: normal
- WBC 18 thousand with 10% bands;
- Normal Chem 7 and LFTs.
- Room air blood gas: pH of 7.47/ PO2 of 55/PCO2 of 30.
- Sputum gram stain remarkable for an abundance of polys along with gram positive diplococci.
- CXR remarkable for dense right lower lobe infiltrate without effusion.
- Monitored care unit, with vigilance for clinical deterioration.
- Hypertension: given significant pneumonia and unclear clinical direction, will hold lisinopril. If BP > 180 and or if clear not developing sepsis, will consider restarting.
- Low molecular weight heparin
- Code Status: Wishes to be full code full care, including intubation and ICU stay if necessary. Has good quality of life and hopes to return to that functional level. Wishes to reconsider if situation ever becomes hopeless. Older brother Tom is surrogate decision maker if the patient can’t speak for himself. Tom lives in San Diego and we have his contact info. He is aware that patient is in the hospital and plans on visiting later today or tomorrow.
- Expected duration of hospitalization unclear – will know more based on response to treatment over next 24 hours.
The holdover admission (presenting data that was generated by other physicians)
- Handoff admissions are very common and present unique challenges
- Understand the reasons why the patient was admitted
- Review key history, exam, imaging and labs to assure that they support the working diagnostic and therapeutic plans
- Does the data support the working diagnosis?
- Do the planned tests and consults make sense?
- What else should be considered (both diagnostically and therapeutically)?
- This process requires that the accepting team thoughtfully review their colleagues efforts with a critical eye – which is not disrespectful but rather constitutes one of the main jobs of the accepting team and is a cornerstone of good care *Note: At some point during the day (likely not during rounds), the team will need to verify all of the data directly with the patient.
- 8-10 minutes
- Chief concern: Reason for admission (symptom and/or event)
- Temporally presented bullets of events leading up to the admission
- Review of systems
- Relevant PMH/PSH – historical information that might affect the patient during their hospitalization.
- Meds and Allergies
- Family and Social History – focusing on information that helps to inform the current presentation.
- Habits and exposures
- Physical exam, imaging and labs that were obtained in the Emergency Department
- Assessment and plan that were generated in the Emergency Department.
- Overnight events (i.e. what happened in the Emergency Dept. and after the patient went to their hospital room)? Responses to treatments, changes in symptoms?
- How does the patient feel this morning? Key exam findings this morning (if seen)? Morning labs (if available)?
- Assessment and Plan , with attention as to whether there needs to be any changes in the working differential or treatment plan. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
- Chief concern: 70 yo male who presented with 10 days of progressive shoulder pain, followed by confusion. He was brought in by his daughter, who felt that her father was no longer able to safely take care for himself.
- 10 days ago, Mr. X developed left shoulder pain, first noted a few days after lifting heavy boxes. He denies falls or direct injury to the shoulder.
- 1 week ago, presented to outside hospital ER for evaluation of left shoulder pain. Records from there were notable for his being afebrile with stable vitals. Exam notable for focal pain anteriorly on palpation, but no obvious deformity. Right shoulder had normal range of motion. Left shoulder reported as diminished range of motion but not otherwise quantified. X-ray negative. Labs remarkable for wbc 8, creat 2.2 (stable). Impression was that the pain was of musculoskeletal origin. Patient was provided with Percocet and told to see PMD in f/u
- Brought to our ER last night by his daughter. Pain in shoulder worse. Also noted to be confused and unable to care for self. Lives alone in the country, home in disarray, no food.
- ROS: negative for falls, prior joint or musculoskeletal problems, fevers, chills, cough, sob, chest pain, head ache, abdominal pain, urinary or bowel symptoms, substance abuse
- Hypertension
- Coronary artery disease, s/p LAD stent for angina 3 y ago, no symptoms since. Normal EF by echo 2 y ago
- Chronic kidney disease stage 3 with creatinine 1.8; felt to be secondary to atherosclerosis and hypertension
- aspirin 81mg qd, atorvastatin 80mg po qd, amlodipine 10 po qd, Prozac 20
- Allergies: none
- Family and Social: lives alone in a rural area of the county, in contact with children every month or so. Retired several years ago from work as truck driver. Otherwise non-contributory.
- Habits: denies alcohol or other drug use.
- Temp 98 Pulse 110 BP 100/70
- Drowsy though arousable; oriented to year but not day or date; knows he’s at a hospital for evaluation of shoulder pain, but doesn’t know the name of the hospital or city
- CV: regular rate and rhythm; normal s1 and s2; no murmurs or extra heart sounds.
- Left shoulder with generalized swelling, warmth and darker coloration compared with Right; generalized pain on palpation, very limited passive or active range of motion in all directions due to pain. Right shoulder appearance and exam normal.
- CXR: normal
- EKG: sr 100; nl intervals, no acute changes
- WBC 13; hemoglobin 14
- Na 134, k 4.6; creat 2.8 (1.8 baseline 4 m ago); bicarb 24
- LFTs and UA normal
- Vancomycin and Zosyn for now
- Orthopedics to see asap to aspirate shoulder for definitive diagnosis
- If aspiration is consistent with infection, will need to go to Operating Room for wash out.
- Urine electrolytes
- Follow-up on creatinine and obtain renal ultrasound if not improved
- Renal dosing of meds
- Strict Ins and Outs.
- follow exam
- obtain additional input from family to assure baseline is, in fact, normal
- Since admission (6 hours) no change in shoulder pain
- This morning, pleasant, easily distracted; knows he’s in the hospital, but not date or year
- T Current 101F Pulse 100 BP 140/80
- Ins and Outs: IVF Normal Saline 3L/Urine output 1.5 liters
- L shoulder with obvious swelling and warmth compared with right; no skin breaks; pain limits any active or passive range of motion to less than 10 degrees in all directions
- Labs this morning remarkable for WBC 10 (from 13), creatinine 2 (down from 2.8)
- Continue with Vancomycin and Zosyn for now
- I already paged Orthopedics this morning, who are en route for aspiration of shoulder, fluid for gram stain, cell count, culture
- If aspirate consistent with infection, then likely to the OR
- Continue IVF at 125/h, follow I/O
- Repeat creatinine later today
- Not on any nephrotoxins, meds renaly dosed
- Continue antibiotics, evaluation for primary source as above
- Discuss with family this morning to establish baseline; possible may have underlying dementia as well
- SC Heparin for DVT prophylaxis
- Code status: full code/full care.
Outpatient-based presentations
There are 4 main types of visits that commonly occur in an outpatient continuity clinic environment, each of which has its own presentation style and purpose. These include the following, each described in detail below.
- The patient who is presenting for their first visit to a primary care clinic and is entirely new to the physician.
- The patient who is returning to primary care for a scheduled follow-up visit.
- The patient who is presenting with an acute problem to a primary care clinic
- The specialty clinic evaluation (new or follow-up)
It’s worth noting that Primary care clinics (Internal Medicine, Family Medicine and Pediatrics) typically take responsibility for covering all of the patient’s issues, though the amount of energy focused on any one topic will depend on the time available, acuity, symptoms, and whether that issue is also followed by a specialty clinic.
The Brand New Primary Care Patient
Purpose of the presentation
- Accurately review all of the patient’s history as well as any new concerns that they might have.
- Identify health related problems that need additional evaluation and/or treatment
- Provide an opportunity for senior listeners to intervene and offer input
Key features of the presentation
- If this is truly their first visit, then one of the main reasons is typically to "establish care" with a new doctor.
- It might well include continuation of therapies and/or evaluations started elsewhere.
- If the patient has other specific goals (medications, referrals, etc.), then this should be stated as well. Note: There may well not be a "chief complaint."
- For a new patient, this is an opportunity to highlight the main issues that might be troubling/bothering them.
- This can include chronic disorders (e.g. diabetes, congestive heart failure, etc.) which cause ongoing symptoms (shortness of breath) and/or generate daily data (finger stick glucoses) that should be discussed.
- Sometimes, there are no specific areas that the patient wishes to discuss up-front.
- Review of systems (ROS): This is typically comprehensive, covering all organ systems. If the patient is known to have certain illnesses (e.g. diabetes), then the ROS should include the search for disorders with high prevalence (e.g. vascular disease). There should also be some consideration for including questions that are epidemiologically appropriate (e.g. based on age and sex).
- Past Medical History (PMH): All known medical conditions (in particular those requiring ongoing treatment) are listed, noting their duration and time of onset. If a condition is followed by a specialist or co-managed with other clinicians, this should be noted as well. If a problem was described in detail during the “acute” history, it doesn’t have to be re-stated here.
- Past Surgical History (PSH): All surgeries, along with the year when they were performed
- Medications and allergies: All meds, including dosage, frequency and over-the-counter preparations. Allergies (and the type of reaction) should be described.
- Social: Work, hobbies, exposures.
- Sexual activity – may include type of activity, number and sex of partner(s), partner’s health.
- Smoking, Alcohol, other drug use: including quantification of consumption, duration of use.
- Family history: Focus on heritable illness amongst first degree relatives. May also include whether patient married, in a relationship, children (and their ages).
- Physical Exam: Vital signs and relevant findings (or their absence).
- Key labs and imaging if they’re available. Also when and where they were obtained.
- Summary, assessment & plan(s) presented by organ system and/or problems. As many systems/problems as is necessary to cover all of the active issues that are relevant to that clinic. This typically concludes with a “health care maintenance” section, which covers age, sex and risk factor appropriate vaccinations and screening tests.
The Follow-up Visit to a Primary Care Clinic
- Organize the presenter (forces you to think things through).
- Accurately review any relevant interval health care events that might have occurred since the last visit.
- Identification of new symptoms or health related issues that might need additional evaluation and/or treatment
- If the patient has no concerns, then verification that health status is stable
- Review of medications
- Provide an opportunity for listeners to intervene and offer input
- Reason for the visit: Follow-up for whatever the patient’s main issues are, as well as stating when the last visit occurred *Note: There may well not be a “chief complaint,” as patients followed in continuity at any clinic may simply be returning for a visit as directed by their doctor.
- Events since the last visit: This might include emergency room visits, input from other clinicians/specialists, changes in medications, new symptoms, etc.
- Review of Systems (ROS): Depth depends on patient’s risk factors and known illnesses. If the patient has diabetes, then a vascular ROS would be done. On the other hand, if the patient is young and healthy, the ROS could be rather cursory.
- PMH, PSH, Social, Family, Habits are all OMITTED. This is because these facts are already known to the listener and actionable aspects have presumably been added to the problem list (presented at the end). That said, these elements can be restated if the patient has a new symptom or issue related to a historical problem has emerged.
- MEDS : A good idea to review these at every visit.
- Physical exam: Vital signs and pertinent findings (or absence there of) are mentioned.
- Lab and Imaging: The reason why these were done should be mentioned and any key findings mentioned, highlighting changes from baseline.
- Assessment and Plan: This is most clearly done by individually stating all of the conditions/problems that are being addressed (e.g. hypertension, hypothyroidism, depression, etc.) followed by their specific plan(s). If a new or acute issue was identified during the visit, the diagnostic and therapeutic plan for that concern should be described.
The Focused Visit to a Primary Care Clinic
- Accurately review the historical events that lead the patient to make the appointment.
- Identification of risk factors and/or other underlying medical conditions that might affect the diagnostic or therapeutic approach to the new symptom or concern.
- Generate an appropriate assessment and plan
- Allow the listener to comment
Key features of the presentation:
- Reason for the visit
- History of Present illness: Description of the sequence of symptoms and/or events that lead to the patient’s current condition.
- Review of Systems: To an appropriate depth that will allow the listener to grasp the full range of diagnostic possibilities that relate to the presenting problem.
- PMH and PSH: Stating only those elements that might relate to the presenting symptoms/issues.
- PE: Vital signs and key findings (or lack thereof)
- Labs and imaging (if done)
- Assessment and Plan: This is usually very focused and relates directly to the main presenting symptom(s) or issues.
The Specialty Clinic Visit
Specialty clinic visits focus on the health care domains covered by those physicians. For example, Cardiology clinics are interested in cardiovascular disease related symptoms, events, labs, imaging and procedures. Orthopedics clinics will focus on musculoskeletal symptoms, events, imaging and procedures. Information that is unrelated to these disciples will typically be omitted. It’s always a good idea to ask the supervising physician for guidance as to what’s expected to be covered in a particular clinic environment.
- Highlight the reason(s) for the visit
- Review key data
- Provide an opportunity for the listener(s) to comment
- 5-7 minutes
- If it’s a consult, state the main reason(s) that the patient was referred as well as who referred them.
- If it’s a return visit, state the reasons why the patient is being followed in the clinic and when the last visit took place
- If it’s for an acute issue, state up front what the issue is Note: There may well not be a “chief complaint,” as patients followed in continuity in any clinic may simply be returning for a return visit as directed
- For a new patient, this highlights the main things that might be troubling/bothering the patient.
- For a specialty clinic, the history presented typically relates to the symptoms and/or events that are pertinent to that area of care.
- Review of systems , focusing on those elements relevant to that clinic. For a cardiology patient, this will highlight a vascular ROS.
- PMH/PSH that helps to inform the current presentation (e.g. past cardiac catheterization findings/interventions for a patient with chest pain) and/or is otherwise felt to be relevant to that clinic environment.
- Meds and allergies: Typically all meds are described, as there is always the potential for adverse drug interactions.
- Social/Habits/other: as relates to/informs the presentation and/or is relevant to that clinic
- Family history: Focus is on heritable illness amongst first degree relatives
- Physical Exam: VS and relevant findings (or their absence)
- Key labs, imaging: For a cardiology clinic patient, this would include echos, catheterizations, coronary interventions, etc.
- Summary, assessment & plan(s) by organ system and/or problems. As many systems/problems as is necessary to cover all of the active issues that are relevant to that clinic.
- Reason for visit: Patient is a 67 year old male presenting for first office visit after admission for STEMI. He was referred by Dr. Goins, his PMD.
- The patient initially presented to the ER 4 weeks ago with acute CP that started 1 hour prior to his coming in. He was found to be in the midst of a STEMI with ST elevations across the precordial leads.
- Taken urgently to cath, where 95% proximal LAD lesion was stented
- EF preserved by Echo; Peak troponin 10
- In-hospital labs were remarkable for normal cbc, chem; LDL 170, hdl 42, nl lfts
- Uncomplicated hospital course, sent home after 3 days.
- Since home, he states that he feels great.
- Denies chest pain, sob, doe, pnd, edema, or other symptoms.
- No symptoms of stroke or TIA.
- No history of leg or calf pain with ambulation.
- Prior to this admission, he had a history of hypertension which was treated with lisinopril
- 40 pk yr smoking history, quit during hospitalization
- No known prior CAD or vascular disease elsewhere. No known diabetes, no family history of vascular disease; He thinks his cholesterol was always “a little high” but doesn’t know the numbers and was never treated with meds.
- History of depression, well treated with prozac
- Discharge meds included: aspirin, metoprolol 50 bid, lisinopril 10, atorvastatin 80, Plavix; in addition he takes Prozac for depression
- Taking all of them as directed.
- Patient lives with his wife; they have 2 grown children who are no longer at home
- Works as a computer programmer
- Smoking as above
- ETOH: 1 glass of wine w/dinner
- No drug use
- No known history of cardiovascular disease among 2 siblings or parents.
- Well appearing; BP 130/80, Pulse 80 regular, 97% sat on Room Air, weight 175lbs, BMI 32
- Lungs: clear to auscultation
- CV: s1 s2 no s3 s4 murmur
- No carotid bruits
- ABD: no masses
- Ext; no edema; distal pulses 2+
- Cath from 4 weeks ago: R dominant; 95% proximal LAD; 40% Cx.
- EF by TTE 1 day post PCI with mild Anterior Hypokinesis, EF 55%, no valvular disease, moderate LVH
- Labs of note from the hospital following cath: hgb 14, plt 240; creat 1, k 4.2, lfts normal, glucose 100, LDL 170, HDL 42.
- EKG today: SR at 78; nl intervals; nl axis; normal r wave progression, no q waves
- Plan: aspirin 81 indefinitely, Plavix x 1y
- Given nitroglycerine sublingual to have at home.
- Reviewed symptoms that would indicate another MI and what to do if occurred
- Plan: continue with current dosages of meds
- Chem 7 today to check k, creatinine
- Plan: Continue atorvastatin 80mg for life
- Smoking cessation: Doing well since discharge without adjuvant treatments, aware of supports.
- Plan: AAA screening ultrasound
- Log In Username Enter your ACP Online username. Password Enter the password that accompanies your username. Remember me Forget your username or password ?
- Privacy Policy
- Career Connection
- Member Forums
© Copyright 2024 American College of Physicians, Inc. All Rights Reserved. 190 North Independence Mall West, Philadelphia, PA 19106-1572 800-ACP-1915 (800-227-1915) or 215-351-2600
If you are unable to login, please try clearing your cookies . We apologize for the inconvenience.
Preparing the Research Presentation
If you have never presented a paper at a scientific meeting, you should read this article. Even if you have presented before, it is likely that this article contains information that will improve your presentation. This article contains a set of practical, proven steps that will guide your preparation of the presentation. Our assumptions are that you will schedule appropriate planning and preparation time, are interested in doing the best job possible, and know that a quality presentation is a combination of good research and communication skills. This and subsequent articles will focus on planning, preparation, creating visual aids (slides), and presentation skills for a scientific presentation. The intent of this series of articles is to help you make a favorable impression at the scientific meeting and reap the rewards, personal and professional, of a job well done.
To begin with, you need to create an outline of the topics you might present at the meeting. Your outline should follow the IMRAC format (introduction, methods, results, and conclusion). This format is chosen because your audience understands it and expects it. If you have already prepared a paper for publication, it can be a rich source of content for the topic outline.
To get you started, we have prepared a generic outline to serve as an example. We recognize that a generic outline does not necessarily adapt to all research designs, but we ask you to think, "How can I adapt this to my situation?" To help you visualize the content you might include in the outline, two types of examples have been included, one that describes a cross-sectional study using a survey methodology (example A), and a second using a combination of a case-control and cohort designs (example B).
Use the Preparing the Research Presentation Checklist to assist you in preparing the topic outline.
Advertisement
How to Prepare an Outstanding Journal Club Presentation
- Request Permissions
Rishi Sawhney; How to Prepare an Outstanding Journal Club Presentation. The Hematologist 2006; 3 (1): No Pagination Specified. doi: https://doi.org/10.1182/hem.V3.1.1308
Download citation file:
- Ris (Zotero)
- Reference Manager
Dr. Sawhney is a member of the ASH Trainee Council and a Fellow at the Medical University of South Carolina.
Journal club presentations provide a forum through which hematology trainees keep abreast of new developments in hematology and engage in informal discussion and interaction. Furthermore, honing presentation skills and mastering the ability to critically appraise the evidence add to our armamentarium as clinicians. Outlined here is a systematic approach to preparing a journal club presentation, with emphasis on key elements of the talk and references for electronic resources. Use of these tools and techniques will contribute to the success of your presentation.
I. ARTICLE SELECTION:
The foundation of an outstanding journal club presentation rests on the choice of an interesting and well-written paper for discussion. Several resources are available to help you select important and timely research, including the American College of Physicians (ACP) Journal Club and the Diffusion section of The Hematologist . McMaster University has created the McMaster Online Rating of Evidence (MORE) system to identify the highest-quality published research. In fact, the ACP Journal Club uses the MORE system to select their articles 1 . Specific inclusion criteria have been delineated in order to distinguish papers with the highest scientific merit 2 . Articles that have passed this screening are then rated by clinicians on their clinical relevance and newsworthiness, using a graded scale 3 . With the help of your mentors and colleagues, you can use these criteria and the rating scale as informal guidelines to ensure that your chosen article merits presentation.
II. ARTICLE PRESENTATION:
Study Background: This section provides your audience with the necessary information and context for a thoughtful and critical evaluation of the article's significance. The goals are 1) to describe the rationale for and clinical relevance of the study question, and 2) to highlight the preclinical and clinical research that led to the current trial. Review the papers referenced in the study's "Background" section as well as previous work by the study's authors. It also may be helpful to discuss data supporting the current standard of care against which the study intervention is being measured.
Study Methodology and Results: Clearly describe the study population, including inclusion/exclusion criteria. A diagrammatic schema is easy to construct using PowerPoint software and will help to clearly illustrate treatment arms in complex trials. Explain the statistical methods, obtaining assistance from a statistician if needed. Take this opportunity to verbally and graphically highlight key results from the study, with plans to expand on their significance later in your presentation.
Author's Discussion: Present the authors' conclusions and their perspective on the study results, including explanations of inconsistent or unexpected results. Consider whether the conclusions drawn are supported by the data presented.
III. ARTICLE CRITIQUE:
This component of your presentation will define the success of your journal club. A useful and widely accepted approach to this analysis has been published in JAMA's series "User's guide to the medical literature." The Centre for Health Evidence in Canada has made the complete full-text set of these user's guides available online 4 . This site offers review guidelines for a menu of article types, and it is an excellent, comprehensive resource to focus your study critique. A practical, user-friendly approach to literature evaluation that includes a worksheet is also available on the ASH Web site for your use 5 .
While a comprehensive discussion of scientific literature appraisal is beyond the scope of this discussion, several helpful tips warrant mention here. In assessing the validity of the study, it is important to assess for potential sources of bias, including the funding sources and authors' affiliations. It is also helpful to look for accompanying editorial commentary, which can provide a unique perspective on the article and highlight controversial issues. You should plan to discuss the trade-offs between potential benefits of the study intervention versus potential risks and the cost. By utilizing the concept of number needed to treat (NNT), one can assess the true impact of the study intervention on clinical practice. Furthermore, by incorporating the incidence rates of clinically significant toxicities with the financial costs into the NNT, you can generate a rather sophisticated analysis of the study's impact on practice.
IV. CONCLUSIONS, IMPLICATIONS, AND FUTURE DIRECTIONS:
Restate the authors' take-home message followed by your own interpretation of the study. Provide a personal perspective, detailing why you find this paper interesting or important. Then, look forward and use this opportunity to "think outside the box." Do you envision these study results changing the landscape of clinical practice or redirecting research in this field? If so, how? In articles about therapy, future directions may include moving the therapy up to first-line setting, assessing the drug in combination regimens or other disease states, or developing same-class novel compounds in the pipeline. Searching for related clinical trials on the NIH Web site 6 can prove helpful, as can consultation with an expert in this field.
Good journal club discussions are integral to the educational experience of hematology trainees. Following the above approach, while utilizing the resources available, will lay the groundwork for an outstanding presentation.
WEB BASED REFERENCES
www.acpjc.org
hiru.mcmaster.ca/more/InclusionCriteria.htm
hiru.mcmaster.ca/more/RatingFormSample.htm
www.cche.net/main.asp
www.hematology.org/Trainees
www.cancer.gov/clinicaltrials
- Previous Article
- Next Article
Email alerts
Affiliations.
- Current Issue
- About The Hematologist
- Advertising in The Hematologist
- Editorial Board
- Permissions
- Submissions
- Email Alerts
- ASH Publications App
American Society of Hematology
- 2021 L Street NW, Suite 900
- Washington, DC 20036
- TEL +1 202-776-0544
- FAX +1 202-776-0545
ASH Publications
- Blood Advances
- Hematology, ASH Education Program
- ASH Clinical News
- The Hematologist
- Publications
- Privacy Policy
- Cookie Policy
- Terms of Use
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Presentation Skills Toolkit for Medical Students
New section.
The ability to design and deliver an effective presentation is an important skill for all learners to develop. The Undergraduate Medical Education Section of the Group on Educational Affairs developed this toolkit as a resource for medical students and health professions trainees as you learn to create and give effective presentations in the classroom, in the clinical setting, and at academic meetings and conferences. In this toolkit, you’ll find helpful resources on developing and delivering formal lectures and presentations, poster and oral abstract presentations, patient presentations, and leading small group sessions.
Please note: Availability of resources may change over time. To suggest edits or updates, email [email protected] .
On this page:
Formal lectures and presentations, posters and abstracts, patient presentations.
- Leading Small Groups
Traditional academic presentations in medicine and the biomedical sciences are necessarily dense with complex content. Thus, slides tend to be wordy, and presenters may use their slides as cue cards for themselves rather than as tools to facilitate learning for their audience. With the necessary resources, medical students (and presenters at all levels) can better identify appropriate learning objectives and develop presentations that help learners meet those objectives. Organization of content, clarity of slide design, and professional delivery are all essential components to designing and giving effective formal presentations.
Achieving all of these elements can make creating and delivering a formal presentation challenging. The strategies and resources below can help you develop a successful formal presentation.

View long description of infographic .
Strategies for success
- Define the objectives of the presentation. Always define learning objectives for each of your lectures to make it clear what knowledge or skills the audience should acquire from your presentation. The best learning objectives define specific, measurable, or observable knowledge or skill gains. Furthermore, consider how to communicate the importance of the topic to your audience and how information should be arranged to best communicate your key points.
- Design an effective slide set. You should begin creating your slides only after defining your objectives and key points. The slides should support your talk but not be your talk. Keep slides simple. The audience should be able to review a slide and grasp key points quickly. Avoid lengthy text and distracting decorative fonts, clip art, graphs, and pictures. If additional wording or images are necessary, consider handouts or alternative methods of sharing this information. Lastly, design your slide deck to emphasize the key points, revisiting your outline as necessary, and summarize concepts at regular intervals throughout your presentation to strengthen knowledge gains.
- Practice your performance. Effective public speaking starts with preparation and practice. Ensure there is enough time to create your lecture and a supporting slide deck. Know your lecture material and slides without prompts! Understand the audience and learning climate (the size and knowledge level of your audience) and be prepared for the venue (virtual, in-person, or both, lecture hall or classroom). Think about what effective audience engagement may look like and how to incorporate audience response systems, polling, etc., into the lecture.
- Create a positive learning environment. Anticipate questions and allocate sufficient time to answer them. Always repeat the questions being asked for the audience’s benefit and to ensure your understanding. Some questions may be challenging, so be prepared and answer honestly. It is acceptable not to know an answer.
- Demonstrate professionalism in presenting. Exhibit professionalism by being punctual and having appropriate time management. Remember that mistakes happen; be kind to yourself and remain calm and collected. Be enthusiastic: If you can enjoy the experience, so will your audience. Finally, be open to feedback following your presentation.
Additional resources
Below is a collection of resources that further address the elements of creating and delivering a formal presentation. Each resource addresses a specific presentation skill or set of skills listed above and can be used to develop your understanding further.
- Healthy Presentations: How to Craft Exceptional Lectures in Medicine, the Health Professions, and the Biomedical Sciences (requires purchase, book). This illustrated book is a practical guide for improving scientific presentations. It includes specific, practical guidance on crafting a talk, tips on incorporating interactive elements to facilitate active learning, and before-and-after examples of improved slide design. (Skills addressed: 1-3)
- American College of Physicians: Giving the Podium Presentation (freely available, website). This guide includes recommendations related to presentation delivery, including tips on what to wear, how to prepare, answering questions, and anticipating the unexpected. (Skills addressed: 3-5)
- The 4 Ps of Giving a Good Presentation (freely available, PDF). This simple guide on public speaking from the University of Hull covers such topics as positive thinking, preparing, practice, and performing. (Skills addressed: 3-5)
- Zoom Guides (freely available, website). This website from the University of California, San Francisco is one of many great resources created by universities for presenting on a virtual platform, specifically Zoom. (Skills addressed: 3-5)
- Writing Learning Objectives (freely available, PDF). This excellent resource from the AAMC defines Bloom’s Taxonomy and provides verbiage for creating learning objectives. (Skill addressed: 1)
- Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83 (freely available, article). This AMEE Guide explains and explores the more commonly used adult learning theories and how they can be used to enhance learning. It presents a model that combines many of the theories into a flow diagram that can be followed by those planning a presentation. (Skill addressed: 1)
- Assertion-Evidence Approach (freely available, website). This approach to slide design incorporates clear messaging and the strategic combination of text and images. (Skill addressed: 2)
- Multimedia Learning (requires purchase, book). This book outlines the learning theories that should guide all good slide design. It is an accessible resource that will help presenters of all levels create slide decks that best facilitate learning. (Skill addressed: 2)
- Collaborative Learning and Integrated Mentoring in the Biosciences (CLIMB) (freely available, website). This website from Northwestern University shares slide design tips for scientific presentations. Specific tips include simplifying messages and annotating images and tables to facilitate learning. (Skill addressed: 2)
- Clear and to the Point (freely available, online book). This book describes 8 psychological principles for constructing compelling PowerPoint presentations. (Skill addressed: 2)
Return to top ↑
Presenting the results of the research projects, innovations, and other work you have invested in at regional and national meetings is a tremendous opportunity to advance heath care, gain exposure to thought leaders in your field, and put your evidence-based medicine and communication skills into practice in a different arena. Effective scientific presentations at meetings also provide a chance for you to interact with an engaged audience, receive valuable feedback, be exposed to others’ projects, and expand your professional network. Preparation and practice are integral to getting the most out of these experiences.
The strategies and resources below will help you successfully present both posters and abstracts at scientific meetings.
Strategies for success
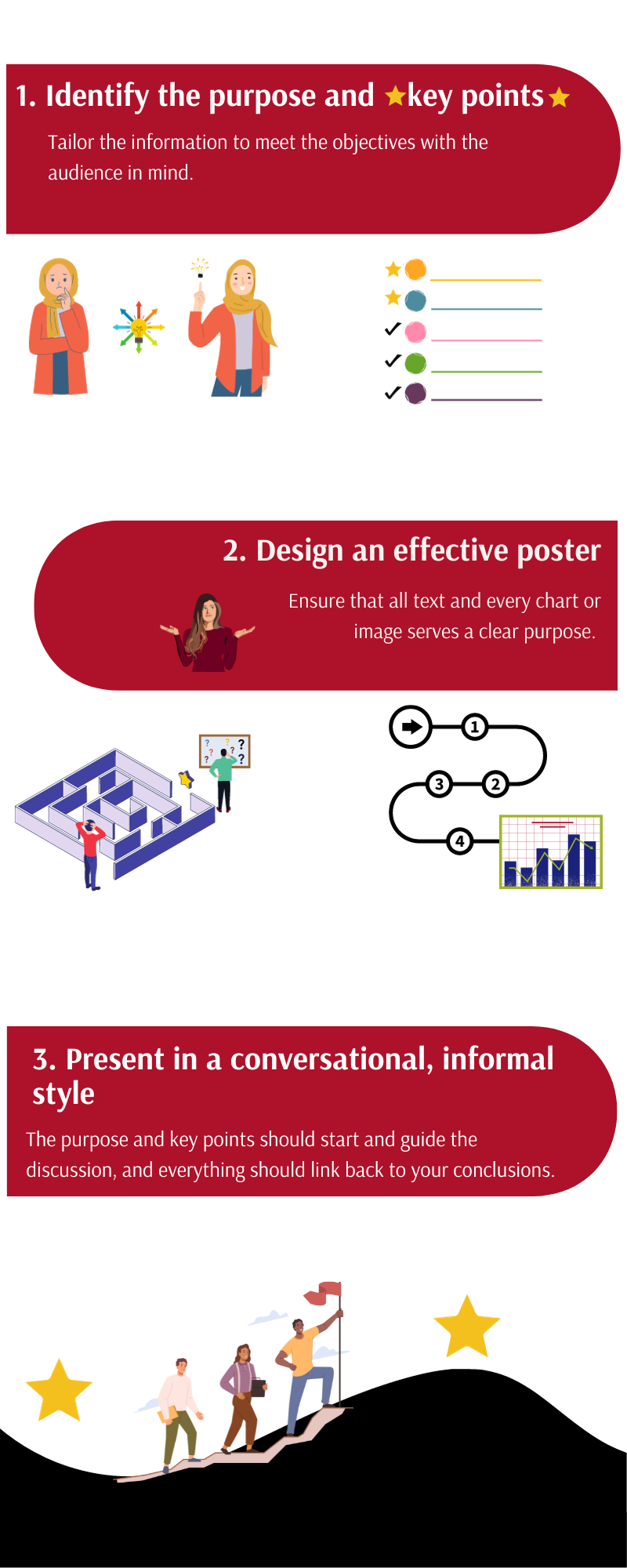
- Identify a poster’s/abstract’s purpose and key points . Determine the purpose of sharing your work (feedback vs. sharing a new methodology vs. disseminating a novel finding) and tailor the information in your poster or abstract to meet that objective. Identify one to three key points. Keep in mind the knowledge and expertise of the intended audience; the amount of detail that you need to provide at a general vs. specialized meeting may vary.
- Design an effective poster . Design your poster to follow a logical flow and keep it uncluttered. The methods and data should support your conclusions without extraneous information; every chart or image should serve a purpose. Explicitly outline the key takeaways at the beginning or end.
- Present in a conversational, informal style . Imagine you are explaining your project to a colleague. The purpose of your work and key points should guide your presentation, and your explanation of the methods and data should link to your conclusions. Be prepared to discuss the limitations of your project, outline directions for future research, and receive feedback from your audience. Treat feedback as an opportunity to improve your project prior to producing a manuscript.
Additional resources
These resources support the development of the skills mentioned above, guiding you through the steps of developing a poster that frames your research in a clear and concise manner. The videos provide examples that can serve as models of effective poster and abstract presentations.
- How to design an outstanding poster (freely available, article). This article outlines key items for laying out an effective poster, structuring it with the audience in mind, practicing your presentation, and maximizing your work’s impact at meetings. (Skills addressed: 1-3)
- Giving an Effective Poster Presentation (freely available, video). This video shows medical students in action presenting their work and shares strategies for presenting your poster in a conversational style, preparing for questions, and engaging viewers. (Skills addressed: 2,3)
- Better Scientific Poster (freely available, toolkit). This toolkit includes strategies and templates for creating an effective and visually interesting scientific poster. Virtual and social media templates are also available. (Skill addressed: 2)
As with all presentations, it can be very helpful to practice with colleagues and/or mentors before the meeting. This will allow you to get feedback on your project, style, and poster design prior to sharing it with others outside of your institution. It can also help you prepare for the questions you may get from the audience.
Patient presentation skills are valuable for medical students in the classroom and in the care of patients during clinical rotations. Patient presentations are an integral part of medical training because they combine communication skills with knowledge of disease manifestations and therapeutic strategies in a clinical scenario. They are used during active learning in both the preclinical and clinical phases of education and as students advance in training and interact with diverse patients.
Below are strategies for delivering effective patient presentations.

- Structure the presentation appropriately . The structure of your narrative is important; a concise, logical presentation of the relevant information will create the most impact. In the clinical setting, preferences for presentation length and style can vary between specialties and attendings, so understanding expectations is vital.
- Synthesize information from the patient encounter . Synthesis of information is integral for effective and accurate delivery that highlights relevant points. Being able to select pertinent information and present it in an efficient manner takes organization and practice, but it is a skill that can be learned.
- Deliver an accurate, engaging, and fluent oral presentation . In delivering a patient presentation, time is of the essence. The overall format for the presentation is like a written note but usually more concise. Succinctly convey the most essential patient information in a way that tells the patient’s story. Engage your listeners by delivering your presentation in an organized, clear, and professional manner with good eye contact. Presentations will go more smoothly with careful crafting and practice.
- Adjust presentations to meet team, patient, and setting needs . Adaptability is often required in the clinical setting depending on attending preferences, patient needs, and location, making it imperative that you are mindful of your audience.
The resources below provide samples of different types of patient presentations and practical guides for structuring and delivering them. They include tips and tricks for framing a case discussion to deliver a compelling story. Resources that help with adjusting patient presentations based on the setting, such as bedside and outpatient presentations, are also included.
- A Guide to Case Presentations (freely available, document). This practical guide from the Ohio State University discusses basic principles of presentations, differences between written and oral communication of patient information, organization, and common pitfalls to avoid. (Skills addressed: 1-3)
- Verbal Case Presentations: A Practical Guide for Medical Students (freely available, PDFs). This resource from the Augusta University/University of Georgia Medical Partnership provides a practical guide to crafting effective case presentations with an explanation of the goals of each section and additional tips for framing the oral discussion. It also provides a full sample initial history and physical examination presentation. (Skills addressed: 1-4)
- Patient Presentations in Emergency Medicine (freely available, video). This training video for medical students from the Society for Academic Emergency Medicine demonstrates how to tell a compelling story when presenting a patient’s case. The brief video offers handy dos and don'ts that will help medical students understand how best to communicate in the emergency department efficiently and effectively. These skills can also be applied to patient presentations in other specialties. (Skills addressed: 1-4)
Additional information and support on effectively constructing and delivering a case presentation can be found through various affinity support and mentorship groups, such as the Student National Medical Association (SNMA), Latino Medical Student Association (LMSA), and Building the Next Generation of Academic Physicians (BNGAP).
Leading Small Groups
For physicians, working within and leading small groups is an everyday practice. Undergraduate medical education often includes small group communication as well, in the form of problem-based learning groups, journal clubs, and study groups. Having the skills to form, maintain, and help small groups thrive is an important tool for medical students.
Below are strategies to provide effective small group leadership.
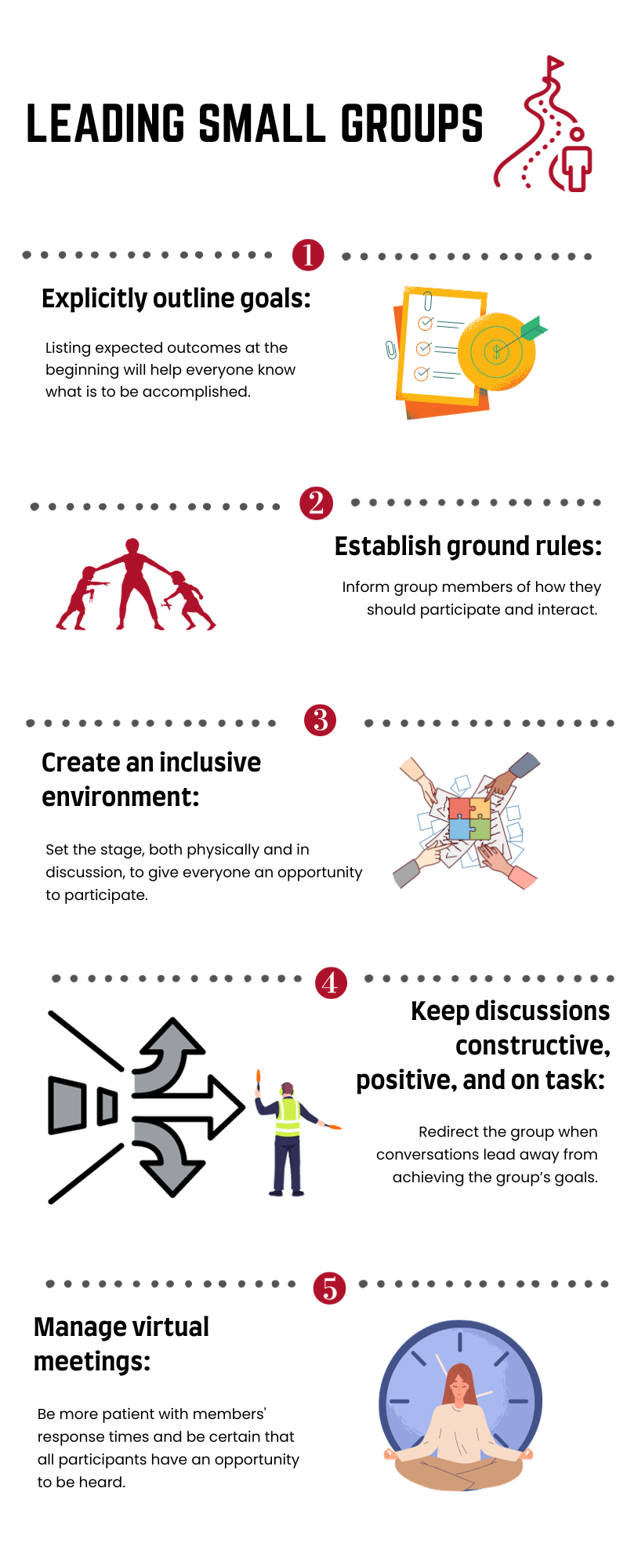
- Outline goals/outcomes . Delineating the goals of a meeting ensures that everyone understands the outcome of the gathering and can help keep conversations on track. Listing goals in the agenda will help all participants understand what is to be accomplished.
- Establish ground rules . Establishing explicit procedural and behavioral expectations serves to solidify the framework in which the conversation will take place. These include items such as attendance and how people are recognized as well as the way group members should treat each other.
- Create an inclusive environment . In addition to setting expectations, group leaders can take steps to help all participants feel that their perspectives are valuable. Setting up the room so that everyone sits around a table can facilitate conversations. Having individuals introduce themselves can let the group understand everyone’s background and expertise. In addition, running discussions in a “round-robin style” (when possible) may help every person have an opportunity to express themselves.
- Keep discussions constructive, positive, and on task . As meetings evolve, it can be easy for conversations to drift. Reminding the group of goals and frequently summarizing the discussion in the context of the planned outcomes can help redirect meetings when needed.
- Manage virtual meetings . Online meetings present their own challenges. Adequate preparation is key, particularly working through technological considerations in advance. Explicitly discussing goals and ground rules is even more important in the virtual environment. Group leaders should be more patient with members’ response times and be especially diligent that all participants have an opportunity to be heard.
The resources listed below outline additional helpful points, expanding on the skills described above and providing additional perspectives on managing small group meetings of different types.
- Communication in the Real World: Small Group Communication (freely available, online module). This chapter includes an overview of managing small groups, including understanding the types and characteristics, group development, and interpersonal dynamics. (Skills addressed: 3,4)
- Conversational Leadership (freely available, online book chapter). This short online resource provides guidance for determining group size and seating to best facilitate participation by all group members. (Skill addressed: 4)
- Tips on Facilitating Effective Group Discussion (freely available, PDF). This resource from Brown University provides tips for effective group facilitation, creating an environment conducive for discussions, keeping conversations positive, and managing common problems. Also included is a valuable list of references for further exploration. (Skills addressed: 1-4)
- Facilitating Effective Discussions: Self-Checklist (freely available, online checklist). This checklist from Brown University provides an easy-to-use, practical framework for preparing for, performing, and reflecting on small group facilitation. (Skills addressed: 1-4)
- Sample Guidelines for Classroom Discussion Agreements (freely available, PDF). These guidelines from Brown University give useful tips for managing classroom discussions, including when disagreements occur among group participants. (Skill addressed: 2)
- Fostering and assessing equitable classroom participation (freely available, online article). This online resource from Brown University includes methods to maximize group members’ participation in discussions and to communicate expectations. Also included is a valuable list of references for further exploration. (Skill addressed: 3)
- Facilitating small group learning in the health professions (freely available, online article). The aim of this paper published in BMC Medical Education is to provide students involved in peer/near peer teaching with an overview of practical approaches and tips to improve learner engagement when facilitating small groups. It includes a discussion of the roles of facilitators, strategies for fostering interactions among the group, and methods for resolving common problems. (Skills addressed: 1-4)
- Facilitating a Virtual Meeting (freely available, PDF). This infographic from the University of Nebraska Medical Center includes key points to consider when facilitating an online meeting, including technical considerations, preparation, and follow-up. (Skill addressed: 5)
- Most universities have a communication department with faculty who specialize in small group communication. You may also find that these individuals are a valuable resource.
This toolkit was created by a working group of the Undergraduate Medical Education (UME) Section of the Group on Educational Affairs (GEA).
Working Group Members
- Geoffrey Talmon, MD, University of Nebraska Medical Center
- Jason Kemnitz, EdD, University of South Dakota Sanford School of Medicine
- Lisa Coplit, MD, Frank H. Netter School of Medicine at Quinnipiac University
- Rikki Ovitsh, MD, SUNY Downstate College of Medicine
- Susan Nofziger, MD, Northeast Ohio Medical University
- Amy Moore, MEd, Cleveland Clinic Lerner College of Medicine
- Melissa Cellini, MD, New York Medical College
- Richard Haspel, MD, Harvard Medical School
- Christine Phillips, MD, Boston University School of Medicine
- Arvind Suresh, Geisel School of Medicine at Dartmouth
- Emily Green, PhD, MA, Warren Alpert Medical School of Brown University
- Holly Meyer, PhD, MS, Uniformed Services University of the Health Sciences
- Karina Clemmons, EdD, University of Arkansas for Medical Sciences
- Shane Puckett, EdD, University of South Florida
- Angela Hairrell, PhD, Burnett School of Medicine at Texas Christian University
- Arkene Levy Johnston, PhD, Kiran C. Patel College of Allopathic Medicine
- Sarah Collins, PhD, UT Southwestern Medical Center
- Patrick Fadden, MD, Virginia Commonwealth University School of Medicine
- Lia Bruner, MD, Augusta University - University of Georgia Medical Partnership
- Jasna Vuk, MD, PhD, University of Arkansas for Medical Sciences
- Pearl Sutter, University of Connecticut School of Medicine
- Kelly Park, Baylor University Medical Center
The Oral Case Presentation
- Letter to the Editor
- Published: 25 April 2022
- Volume 38 , page 1076, ( 2023 )
Cite this article
- Andrew P. J. Olson MD 1 ,
- Laura Zwaan PhD 2 &
- Joseph Rencic MD 3
827 Accesses
1 Altmetric
Explore all metrics
Avoid common mistakes on your manuscript.
Dear Editor,
We read with great interest the paper by Rodin et al. 1 that describes an approach to preparing for oral presentations during clinical education experiences. We applaud the authors’ comprehensive approach and the development of a tool that early learners will find useful in decreasing the non-germane cognitive load of preparing for and then delivering case presentations, which are both a source of significant stress but also an incredibly important learning opportunity.
While we share the authors’ enthusiasm for innovation in this space, we have two suggestions that, if considered, could substantially improve the uptake and potentially the effectiveness of this intervention.
First, it has become clear that the Electronic Health Record (EHR) is “where it happens” in modern health care. Input, searching, retrieval, and provenance of clinical information in the EHR are fundamental processes in which modern learners (and practitioners) must be competent. Thus, this tool and other similar tools may be best developed within the EHR, emphasizing entry, search, and retrieval of information from the highest fidelity and most efficient areas of the EHR possible. While such “external brains” are helpful, teaching health care professionals to harness the power of the EHR is the way of the future, as the authors mention.
Second, we agree that it is important to encourage presenters to prepare a differential diagnosis for each patient using a formal rubric. However, the approach could be improved by adopting evidence-based strategies that have shown to improve diagnostic performance. While the VINDICATE and other systems-based approaches are oft-discussed, the literature supports use of structured reflection tools in improving diagnostic performance of present and future cases . 2 , 3 Structured reflection tools have consistently shown to improve learning and increase diagnostic accuracy in experimental settings using clinical vignettes . 4 , 5 The approach encourages the prioritization and appraisal of potential diagnoses with special attention to features that “don’t” fit rather than developing an exhaustive, non-prioritized list of esoteric diagnoses . 5 Such a strategy could easily be incorporated into the authors’ proposed tool.
Incorporating these evidence-based modifications could improve both student learning and diagnostic performance.
Rodin, R., Rohailla, S. & Detsky, A.S. The Oral Case Presentation: Time for a “Refresh”. J GEN INTERN MED 36, 3852–3856 (2021). https://doi.org/10.1007/s11606-021-06964-6
Article PubMed PubMed Central Google Scholar
Prakash S, Sladek RM, Schuwirth L. Interventions to improve diagnostic decision making: a systematic review and meta-analysis on reflective strategies. Med Teach 2019;41:517–24. https://doi.org/10.1080/0142159X.2018.1497786
Article PubMed Google Scholar
Norman GR, Monteiro SD, Sherbino J, et al. The causes of errors in clinical reasoning: cognitive biases, knowledge deficits, and dual process thinking. Academic Medicine 2017;92:23–30.
Mamede S, Schmidt HG, Penaforte JC. Effects of reflective practice on the accuracy of medical diagnoses. Medical Education 2008;42:468–75. https://doi.org/10.1111/j.1365-2923.2008.03030.x
Mamede S, van Gog T, Sampaio AM, et al. How can students’ diagnostic competence benefit most from practice with clinical cases? The effects of structured reflection on future diagnosis of the same and novel diseases. Academic Medicine 2014;89:121–7. https://doi.org/10.1097/ACM.0000000000000076
Download references
Author information
Authors and affiliations.
Departments of Medicine and Pediatrics, University of Minnesota Medical School, Minneapolis, MN, USA
Andrew P. J. Olson MD
Erasmus MC, Institute of Medical Education Research Rotterdam (iMERR), Rotterdam, The Netherlands
Laura Zwaan PhD
Department of Medicine, Boston University School of Medicine, Boston, MA, USA
Joseph Rencic MD
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Andrew P. J. Olson MD .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Olson, A.P.J., Zwaan, L. & Rencic, J. The Oral Case Presentation. J GEN INTERN MED 38 , 1076 (2023). https://doi.org/10.1007/s11606-022-07611-4
Download citation
Received : 20 December 2021
Accepted : 12 April 2022
Published : 25 April 2022
Issue Date : March 2023
DOI : https://doi.org/10.1007/s11606-022-07611-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
Medical Presentations: How to Present Effectively on Urgent Topics

In the face of the pandemic that consumed 2020, we saw an uptick in medical presentations. And rightfully so. The world was in a state of panic over the unknown of a new virus, people were craving information, and organizations like the World Health Organization (WHO) were scrambling to provide data and resources to help address questions and concerns. Whether it was news stories, or medical research, the world needed to understand what we were up against with COVID-19. Naturally, presentations helped to deliver that information. But this isn’t the first time a virus or disease has rattled communities, and it’s certainly not the first time professionals have used medical presentations to educate the masses. Medical presentations are a helpful tool for medical professionals, research clinics, and organizations to help inform and educate their communities on a wide variety of urgent topics. This can include patient treatment, clinical trial research and results, training for medical staff, general education, medical research, or important data regarding diseases.
While medical presentations tend to be fundamentally different from normal presentations in that they include critical and sensitive information, there are still design best practices just like any other deck. That said, what works for a sales pitch might not resonate well with a medical presentation.
Keep these five things in mind when you want to present effectively on urgent medical presentation topics.
Consider your audience
You may be presenting to a group of doctors within your organization to get the team up to speed on new practices, sharing treatment plans with a patient, or educating the community on new health threats. How you structure your medical presentation is not a one-size-fits-all situation. How you talk to internal staff, versus how you would deliver information to a scared patient is not the same. When you’re crafting your message, consider your audience, and tailor the narrative to their overarching concerns and needs.
Keep things straightforward
Unless you’re presenting to third year residents, your audience probably won’t be able to digest complicated medical terminology. It’s important to avoid medical jargon, complex definitions, or overcomplicated explanations that will confuse your audience. Instead, break things down in layman's terms and relate the information back to your audience and how it will affect them. Keeping things straightforward, and clear, will help your audience digest and process the information quicker. The end goal is that your audience leaves with clarity, feeling more educated on the topic and its urgency.
Use icons to reflect the urgency of the situation
The use of visual aids, such as compelling images or meaningful icons, can help paint the picture of urgency in any presentation. Things like clocks, alarms, lightning bolts, or exclamation points can depict emergencies and symbolize something significant in your presentation. The use of impactful visuals will help engage your audience and let them know what they absolutely need to pay attention to. It helps you control the narrative, and highlight any pertinent information or key takeaways.
Beautiful.ai’s free library of hundreds of thousands of images and icons can help take your presentation to the next level. Our custom icons were thoughtfully created by one of our in-house designers, and are a great way to compliment your data and add urgency to your slide .
Hit them with the facts
In most medical presentations, factual data carries the slides. Whether it’s a survey, research results, or statistics about a particular disease, numerical data will help people understand the urgency or severity of the topic. For example, it was common for nearly every COVID-19 presentation or article to include statistics of the percentage of the population infected, which regions were seeing the greatest spikes in cases, death tolls by county, and data relevant to high-risk individuals. While the numbers may not always be fun— especially as they pertain to a pandemic— they paint a clear picture of what the audience needs to understand. Seeing scary statistics can put into perspective just how real the situation is.
Using the proper charts, graphs , or infographics allows you to dictate exactly what information the audience is consuming. Data visualization with infographics can also help the audience understand and retain otherwise complicated data. However, even with the best charts, you can still overwhelm the audience with information. Opt to include only the most relevant info and useful data.
Allow time to process
Regardless of what you’re presenting— big or small— you should leave time at the end for questions. Medical presentations can be paralyzing, and your audience will likely be seeking more answers. Give your audience a minute or two following the presentation to process what they learned, and then give them a chance to ask questions. You may need to elaborate on specific slides, or revisit a piece of data, to help provide clarification. When it comes to urgent topics, you want your audience to leave feeling more knowledgeable and at ease than they were prior to tuning in.

Jordan Turner
Jordan is a Bay Area writer, social media manager, and content strategist.
Recommended Articles
Using beautiful.ai to give data-driven presentations, the 7 essential presentation tips for non-designers, how to write bullet points your team will actually read, how to use video to engage your audience.
- Paper Presentations
Presented paper on on comparative study between 0.5 % Ropivacaine with Fentanyl and 0.5 % bupivacaine with fentanyl in USG guided supraclavicular Block in Upper Limb Surgeeries
Presented e-paper on the effect of ketamine in lowering the incidence and severity of post op sore throat after endotrttacheal in patients receiving GA on 19 DEC 2020 at TNISA PG Conclave
Ashish , Logeshwari P
Presented an e-poster on’A randomised control study comparing effect of intravenous dexmedetomidine vs IV esmolol omn attenuation of pressor response to laryngoscopy and endotracheal intubatiion’ and e-paper on ‘the effectiven3ess of dexmedetomidine as an additive to Ropivacaine in supraclavicular brachial plexus block.
Presented e-paper on MAHAYUVAISACON 21 on 20 th Feb 2021 titled as “the effect of nebulised ketamine in decreasing the incidence and severity of post operative sore throat after endotracheal intubation in patients receiving general anaesthesia.
Biochemistry
Made presentation on scientists and clinicians preceptorship for translational research in Webinar 'Biology to Omics' organized by TMS-ACTREC, Navi Mumbai during March 10-12, 2021
Community Medicine
Sero Surveillance in the Wardha District of central India to monitor
SARS Cov 2 infection status among asymptomatic General population
International conference Conquering COVID-19 , at Kasibai Navle
Medical College, Pune.18-19 December 2020
Participated in 5th National IAPSM postgraduate quiz Competition 48th Annual National Conference of Indian Association of Preventive and Social Medicine (IAPSMCON),PGIMER, Chandigarh,19-21 March 2021
Kolhe R , Gupta SS
Relationship of Father's engagement in responsive caregiving with child development a cohort study - presented at IAPSMCON 2021, PGIMER, Chandigarh, 19-21 March,21(poster presentation)
48th Annual National Conference of Indian Association of Preventive and Social Medicine (IAPSMCON),PGIMER, Chandigarh,19-21 March 2021 - Participated in (WAR OF VIDEO COMPETITION) “MAHASANGAM”
2nd IAPSM Young Leaders National Conclave,26-27 March 2021 Participated in (Worth A Thousand Word: Public Health Photography Competition)
Forensic Medicine
Moderate a session topic- crime scene examination-role of doctor in state conference of MLAM“forensicon 2020 on 10 th april 2021 Organized by Department of Forensic Medicine &Toxicology, TNMC & BYL charitable , hospital, Mumbai
Khandekar I L
Chaired a session in 42 nd Annual National conference of IAFM “FORENSIC MEDICON 2021” organized at SCB medical college cuttack, odisha from 23 rd - 24 th Jan 2021,
Moderate a session topic- Non uniformity of medical & medicolegal certificates in state. in state conference of MLAM“ forensicon 2020 on 10 th april 2021 Organized by Department of Forensic Medicine &Toxicology, TNMC & BYL charitable , hospital, Mumbai
Politics of Science in a Pandemic: Impact of Evidence Based Medicine (Guest Speaker)
8 th National Bioethics Conference, 12 December 2020
SP Kalantri
Predictors of Mortality in Venomous Snakebites: Sevagram Story (Guest Speaker)
Amrita Institute of Medical Science (AIMS) Kochi. Amrita National Conference on Snakebite. 22 November 2020
How Covid Vaccines Are Being Developed: Clinical Trials in India (Guest Speaker)
BOOM, 6 August 2020
Aarupadai Veedu Medical College & Hospital. AVMC Webinar Series – ‘Forefront of Future Frontiers’ (Guest Speaker)
Clinical Trials in COVID -19: The Science and Ethics’, 31 July 2020
The Need for Evidence Based Medicine in Treating Covid19 (Guest Speaker)
20 July 2020
14th National Cancer Grid webinar on COVID19 Preparedness (Guest Speaker)
Research Priorities for COVID-19, 18 July 2020
Can Alternative Medicine Be Subject To Modern Rigour? (Guest Speaker)
The Hindu Podcast by Jacob Koshy,3 July 2020
Webinar: Ethical Challenges of Research in a Pandemic (Guest Speaker)
Sunoindia podcast, 27 June 2020
The Why, How & What of Research during COVID era (Guest Speaker)
11 th National Cancer Grid webinar on COVID-19 preparedness, 20 June 2020
Covid and Rural India: Wardha Story (Guest Speaker)
Podcast: SoundCloud by Rukmini S, 10 June 2020
Hydroxychloroquine: More Questions than Answers (Guest Speaker)
BOOM, 5 June 2020
TheEvidence and/or Lack of Evidence for the Effectiveness of Hydroxychloroquinein Treating COVID-19
BBC (British Broadcasting Corporation) Talk , 20 May 2020
Dr. Amrish Saxena
Poster Presentation on Magnitude and determinants of depression in chronic kidney disease patients on maintenance hemodialysis in rural tertiary care hospital at ISN-WZ 2020, 36 th Annual ISN West Zone Conference, Nagpur, 19 th & 20 th September, 26 th & 27 th September 2020.
Microbiology
Presented a paper (Oral Presentation) on “Co infection of pneumocystis
carinii and cryptococcus neoformans” in the 2 nd Annual Conference of
Vidarbha Association of Medical Microbiology VAMMCON-2021 (online) held at Akola on 20 th and 21 st February, 2021
Maraskolhe D
Presented a paper (Oral Presentation) on “Are tuberculosis patients at greater risk of acquiring COVID-19 MGIMS data and Review of literature” in the 2 nd Annual Conference of Vidarbha Association of Medical Microbiology VAMMCON-2021 (online) held at Akola on 20 th and 21 st February, 2021 and received Dr. Ashok Pathak Junior Best Oral Paper Award
Obstetrics and Gynaecology
Presentation on Elderly Girls and How can we keep the rural work force we have ?” Unwanted pregnancies in adolescent girls – Global Challenges
Virtual 17 th WONCA World Health Rural Conference (Speaker)
Primary Care and Rural Health Bangladesh (PCRHB), Bangladesh, 15 th -18 th April, 2020
Critical Obstetric Care (Transfusion protocol, use of anticoagulants, Labour and Delivery in ICU training Webcast conference ( Panelist)
FOGSI 26 th April, 2020
4 th Global Virtual summit featuring wizard of endoscopy
Indian association of Gynaecology Endoscopist 21 st June, 2020
Mid Life Health Issue (Panelist)
Mid life Health committee Online conference (Chairperson nominee) Amravati Obstetrics and Gynaecology Society, Amravati, 12 th August, 2020
Management of worst Obstetric emergencies, PPH Online workshop on “ PPH Management” ( Panelist)
Ghaziabad Obstetrics and Gynaecological Society 13 th August, 2020
Hypertensive DS of Pregnancy Online Conference on “Hypertensive Pregnancy” (Panelist)
Nagpur Obstetrics and Gynaecological Society, Nagpur, 18 th August, 2020
USG in Infertility E-conference on “USG in Infertility “The Third Eye” ( Guest lecture)
Revari Obstetrics and Gynaecological Society, Rewari, Haryana, 4 th Sept, 2020
Classic For Clinician - RH Incompatibility in Obstetrics
Classic for Clinician Webinar Series 2, 25th November, 2020
NHM-UNICEF-NQOCN Webinar on Management of Post Partum Haemorrhage With Bundle Approach -Management Of Mother And Newborn In Labour Room
NQOCN with support of UNICEF, 28th November, 2020
Family Integrated Care
NQOCN 14 th December, 2020
Gestational Diabetes – Early intervention key to best Outcome
Rewari Obst & Gynaec Society, 11th January, 2021
Virtual conference on High risk pregnancy, infertility and Gynaecologic
Pune Obstetric and Gynaecology Society, 5 th -7 th March, 2021
Appropriate Blood and Blood Product Transfusion Guidelines PPH- Prevent the Catastrophe Part -5
Association of Madhya Pradesh Obst & Gynae Society and Raipur Obst & Gynae society 9th March, 2021
Amenorrhoea - Clinician's Perspective 29 th Annual POGS Conference “REEDIFY 2021” (Panelist)
Organised by Pune Obstetrics and Gynaecological Society, Pune, 5 th -7 th March, 2021
Maternal Health Care Bundles Classic for Clinician Webinar Series
25th March, 2021
Case Presentation & Table Viva Orator- Respectful Maternity Care (Late Dr. Leela Dube Oration) Virtual PG Force-2021 Nagpur Obstetrics and Gynaecology (Faculty)
Organized by Dept of OBGY, NKP Salve Institute of Medical Sciences & Research Centre & Lata Mangeshkar Hospital, Nagpur in Association with Nagpur Obstetrics and Gynaecology Society, Nagpur 16 th -21 st March, 2021
PMNCH Call to action on COVID 19 Webinar on PMNCH Stratergry outline
WHO 30th March, 2021
Infertility E-conference on “Roll of USG in Pregnancy” ( Chief Guest) Rewari Obst & Gynaec Society Rewari, Haryana 4 th September, 2020
Unwanted Pregnancies in Adolescent Girl, Global Challenges For Safe Baby, Safe Childhood, Safe Motherhood, Safe Womenhood, Maternity Violence must stop. How?
Rural Tribal Elderly Women’s suffering in a low resource region
Workshop-How Can We Keep the Rural Workforce We Have?”: A
Workshop on Rural Workforce Retention
TUFH Network : Primary Health Care: A Path towards Social Justice-
System and Community Based response to Covid-19,
Mexico, 23 rd -25 th September,2020
"Partograph and its interpretation: Risk for mother and Newborn"
NQOCN for Madhya Pradesh 15 th September, 2020
Developing prospective authors from QI teams across India for preparing QI reports for publication in peer reviewed journals
NQOCN 27 th October, 2020
Checklist For Immediate Postpartum Vigilence- For Mother And Newborn
Nqocn 10 th December, 2020
The Nuances of Infertility Webinar on The Nuances of Infertility ( Chaired the Session)
Nagpur Obstetrics and Gynaecology Society, Nagpur, 23 rd December, 2020
Triaging and Emergency Management in Obstetrics emergency (Guest Speaker) Topic of Webinar- Respectful Maternity Care in Covid/ Non-Covid era: Pregnant Women deserves the Quality Care in any Situation
13th February, 2021
Post natal care – recent advances (Guest speaker) Topic of Webinar- Respectful Maternity Care in Covid/ Non-Covid era: Pregnant Women deserves the Quality Care in any Situation - Day 4
27th February, 2021
Infection Prevention Practices- Covid/ Non Covid Topic of Webinar- Respectful Maternity Care in Covid/ Non-Covid era:
Pregnant Women deserves the Quality Care in any Situation
31st March, 2021
Ophthalmology
Diabetic Retinopathy Screening by Teleophthalmology (Guest Speaker)
Annual Delhi Ophthalmic Society International Hybrid Conference of 19 th December, 2020
Enhancing Clincal Skills in Ophthalmology using OSCE’s (Guest Speaker)
Annual Delhi Ophthalmic Society International Hybrid Conference of 18 th December, 2020
Lens Induced Glaucoma
Annual Delhi Ophthalmic Society International Hybrid Conference of
19 th December, 2020
Tayde D , Shukla A K, Singh S, Sheikh A, Lilhare K
Correlation between ablation depth and change in corneal curvature after
LASIK surgery”
45 th Virtual Annual Conference VOS-VRCON 2020 of the Vidarbha Ophthalmic Society from 26 th & 27 th December, 2020
More A , Shukla A K, Singh S, Sheikh A, Bhosale N
Management of Diabetic Patients with Vision Threatening Diabetic
Retinopathy in Rural Vidarbha region”
Peddawad S , Shukla A K, Singh S, Sheikh A, Bhosale N
Screening for vitamin A deficiency in tribal Maharashtra (Melghat)”
Bhosale N , Shukla A K, Singh S, More A
Visual outcome after small incision cataract surgery (SICS) in diabetic and non-diabetic patients”
Rathi N , Singh S, Shukla A K, Tayde D
Corneal topographic patterns in myopic eyes”
Taneshwari S , Dhabarde A, Shukla A K, Pednekar N, Sarode K
Analysis of Causes of Protposis in a Rural Based Tertiary Care Hospital
Tejashree B , Shukla A K, Singh S, Bang P, Peddawad S
An Insight into the Burden of Concomitant Strabismus among Primary School Children in Central India”
Yadav V , Shukla A K, Singh S, Tayde D, Malwe G
A case of lid ptosis and total ophthalmoplegia Annual Delhi Ophthalmic
Society International Hybrid Conference of 18 th December, 2020
Study of change in contrast sensitivity and corneal aberration in eyes
undergoing LASIK (Laser in situ Keratomileusis)
Bhosale N , Shukla A K, Singh S, More A, Malwe G
Bilateral Optic neuropathy: a rare presentation of Systemic lupus erythematosus ( e Poster)
Rosai Dorfmann Disease of Orbit” ( e Poster)
A case of optic nerve head drusens mimicking optic disc oedema” ( e Poster)
Yadav V , Shukla A K, Singh S, Tayde D, Chauragade S
An unusual presentation of mucormycosis in a known diabetic 45 th Virtual
Annual Conference VOS-VRCON 2020 of the Vidarbha Ophthalmic Society from 26 th & 27 th December, 2020
CISP II Workshop (Convener and Resource Person)
28—29 August 2020 at MGIMS, Sevagram
Graduate Medical Education Regulation (2019) on 28 th August 2020
Alignment & Integration on 29 th August 2020
Skills training on 29 th August 2020
Panel discussion on the impact of the corona pandemic on medical
education in the country. ( Panelist )
The Indian Medical Association- Indian Medical Students Network and the Medical Students Association of India, 14 Jun 2020
Enhancing learner engagement in online sessions. (Guest speaker)
Medical Education Unit, NKP Salve Institute of Medical Sciences and Lata Mangeshkar Hospital, Nagpur, 27 May 2020
Case based learning in Pathology . (Resource person)
E-course on Competency based learning in Pathology. 6 May 2020
Online teaching learning: Modalities for student engagement. (Guest speaker)
Webinar by Indian Association of Public Health Dentistry, 16 May 2020
Anshu Attention please: Tips for enhancing learner engagement online. (Guest speaker)
Webinar organized by Academy of Health Professions Educators, 19 April 2020
MGIMS Sevagram's Village Adoption Scheme and Social Service Camp for medical students. (Guest speaker)
Organized by the Network Towards Unity for Health (TUFH) Social Accountability Institute. 14 Apr 2020
Enhancing student engagement in online teaching. (Guest speaker)
Medical Education Unit, MGIMS, Sevagram, 17 Aug 2020
Enhancing student engagement in online teaching: Tips and tools (Guest speaker)
Centre for Continuing Education and Inter professional Development (CCEID), Manipal Academy of Higher Education, 25 Jul 2020.
Effective strategies for online learning. (Resource person)
Personal and Professional Development Group of Melaka Manipal Medical College for Malaysian students of I MBBS, 11 Jul 2020
Should a pathologist be a jack of all trades or a master of one? (Debate,
Invited speaker)
Vidarbha Association of Pathologists and Microbiologists, Nagpur, 20 Dec 2020
Pharmacology
National Level e-poster competition
Dr. P.R. Pote Patil College of Pharmacy, Amravati, June 2020
Gorjelwar P
Transfusion-Related Adverse Reactions in patients admitted in medicine department at Tertiary Care Teaching Hospital of Central India
Virtually Online, IPCON 2021 Date: 25 Feb 2021
Gorjelwar P & Kale R
Poster presentation in National Level e poster competition on Proposed
treatment of Covid 19
PR Pote Patil College of Pharmacy, Amravati, 31 st May 2020
Singh Rajput A
To study the effect of wound healing activity of Musa Balbisiana Sp.peel as anti-inflamatory activity on wistar Rats
2 nd World Congress on infectious Disease & Antibiotics 2020
J.N. Tata Auditorium, Indian institute of Science, Bengluru, 17 th Oct 2020
Knowledge attitude and practice towards covid 19 among medical students: a questionnaire based study (Poster Presentation)
Asian ACPCON 2021 organised by American college of physician- india chapter supported by acp chapters, 6 th 7 th feb 2021
International Webinar on Cardiovascular & VO 2 Max Assessment”
AD Instruments, South East Asia, 9 Sep 2020
Webinar : IPS community psychiatry seminar “Healthy eating, under nutrition and obesity among Indian children and adolescent (Guest Speaker)
Organized by : Dr.KS Shubrata, 2 nd May 2020
Annual National CME of industrial Psychiatry of India “Mental Health Issues in IT Industry” Theme - Current and emerging mental health issues in different industries, on 12/12/2020 (Guest Speaker)
KK Mishra, Ahmed
Title – ‘Absenteeism in Health Care Industries’ (Award Paper)
18 th ANCAIPI” held at DY Patil, Pune on 4 th to 6 th March 2021.
“IK Mujawar Award Poster”
Annual Conference IPS West Zone 2 nd & 4 th Oct. 2020.(Webinar)
Radiotherapy
Palliative radiotherapy to triage patients for radical treatment in locally
advanced oral cavity cancer during COVID CRISIS’ Annual Conference of
Association of Radiation Oncologist of Maharashtra, 19 Dec 2020
Clinical outcomes of reirradiation of brain metastasis with erlotinib in
metastatic adenocarcinoma lung’ 10 th Annual Conference of Indian Society
for study of lung cancer, Association of Radiation Oncologist, 26 Sept 2020
Covid 19 a double edge sword for cancer patients’
The Federation of Obstetric & Gynecological Societies of India and POGS international Conference of Indian society for study of lung cancer, Association of Radiation Oncologist, 11 Dec 2020
Efficacy and outcomes of hypofractionation in locally advanced head and neck cancer’
Annual Conference of Association of Radiation Oncologist of India North zone, 2 Oct 2020
Evaluation of nasogastric tube feeding during radiotherapy in head and neck cancer patients’
Annual Conference of Association of Oncologist of North East India, 19 Jan 2021
Left Coronary Artery Dose Exposure Predicts Major Adverse Cardiac Events in Coronary Heart Disease Negative Lung Cancer Patients’
Best of ASTRO 2020, 15 Aug 2020
The Dutch Lung Cancer Audit-Radiotherapy (DLCA-R): Real-World Data on
Elderly Stage III Non-Small Cell Lung Cancer Treated with Definitive
Chemoradiation
Best of ASTRO 2020 16 Aug 2020
Changing Paradigm in Radiotherapy of Postmastectomy Breast Cancer patients A comparative study of 3DCRT vs IMRT : Dosimetry,Toxicity and Outcome at the end of 4 years’
Annual Conference of Indian Society of Medical and Paediatric Oncology, 6 Nov 2020
How to optimally utilize the waiting time/area of patients while they are in
waiting hall before their RT commences for the purpose of patient education 43rd Indian Cooperative Oncology Network Virtual Conference, 9 Oct 2020
Role of prophylactic nasogastric feeding tube to maintain nutrition during
radiotherapy in head and neck cancer patients” Virtual Symposium on
Nutrition in Cancer Care & Management of Mucositis to be held on Friday,
26th February 2021
Kale P, Kalbande P , Rangari P , Datta NR
An evaluation of cost-effective nutrition supplement using homemade recipes vs commercially available formulations in cancer patients on liquid diet from low-middle-income group countries”
Virtual Symposium on Nutrition in Cancer Care & Management of Mucositis to be held on Friday, 26th February 2021
Skin & VD
Puzzling papules on the neck: Cutaneous metastasis from the breast ( e-Poster)
49th National Conference of IADVL, 5th to 7th February, 2021
Patrick S , Kar S, Gangane N, Deshmukh A
Lepromatous Hansen’s disease simulating Still’s Disease: a parodying case
report with diagnostic conundrum (e-Poster)
Manwar P , Kar S, Sawant A, Patrick S, Nandwani S
Blaschkolinear Atrophoderma of Pasini and Pierni with shortening of foot –A
Rare Entity ( e-Poster)
Nandwani S , Kar S, Sawant A, Patrick S, Manwar P
Leprosy presenting as a diagnostic challenge in a case of HIV with Pulmonary Tuberculosis at a rural tertiary care hospital (e-Poster)
Approach to obstructive Jaundice (Guest Lecture)
ASICON-2020 (virtual) from 14 - 19 th Dec. 2020
- Departments
- NAAC Cycle 3
- Courses Attended
- Academic Activities Conducted
- CME Attended
- Conference Attended
- Students Activities
- Student Awards
- Academy of Medical Sciences
- Medical Education Unit
- Institutional Ethics Committee
- Internal Quality Assurance Cell
- Dr Sushila Nayar School of Public Health
- UG Students
- PG Students
- Teaching Staff
- Non-Teaching Staff
- Senior Residents
- Non PG Junior Residents
- Outpatient Services
- Inpatient Services
- Accident and Emergency
- Investigation Facilities
- Information Technology
- Hospital in Numbers
- Hospital Charges
- Life Saving Equipment
- Bio Medical Waste
- Institutional Research
- Student Research
- In-house Publication
- Journal of MGIMS
- Publications
- Community Activities
- Community Based Medical Education
- Social Impact
- Government Approval
- History and Heritage
- Our Founder
- Administration
- Citizen Charter
- Life at Sevagram
- Anti-Ragging
- Right to Information
- Women's Complaints Committee
- Annual Report
- Employe's Information
- Audited Statements
- Foreign Contributions
- Human Rights Complaints
- Mandatory Disclosure
- Getting Here
- NMC Disclosure
- MUHS Mandate
Tools for the Patient Presentation
The formal patient presentation.
- Posing the Clinical Question
- Searching the Medical Literature for EBM
Sources & Further Reading
First Aid for the Wards
Lingard L, Haber RJ. Teaching and learning communications in medicine: a rhetorical approach . Academic Medicine. 74(5):507-510 1999 May.
Lingard L, Haber RJ. What do we mean by "relevance"? A clinical and rhetorical definition with implications for teaching and learning the case-presentation format . Academic Medicine. 74(10):S124-S127.
The Oral Presentation (A Practical Guide to Clinical Medicine, UCSD School of Medicine) http://meded.ucsd.edu/clinicalmed/oral.htm
"Classically, the formal oral presentation is given in 7 minutes or less. Although it follows the same format as a written report, it is not simply regurgitation. A great presentation requires style as much as substance; your delivery must be succinct and smooth. No time should be wasted on superfluous information; one can read about such matters later in your admit note. Ideally, your presentation should be formulated so that your audience can anticipate your assessment and plan; that is, each piece of information should clue the listener into your thinking process and your most likely diagnosis." [ Le, et al, p. 15 ]
Types of Patient Presentations
New Patient
New patients get the traditional H&P with assessment and plan. Give the chief complaint and a brief and pertinent HPI. Next give important PMH, PSH, etc. The ROS is often left out, as anything important was in the HPI. The PE is reviewed. Only give pertinent positives and negatives. The assessment and plan should include what you think is wrong and, briefly, why. Then, state what you plan to do for the patient, including labs. Be sure to know why things are being done: you will be asked.
The follow-up presentation differs from the presentation of a new patient. It is an abridged presentation, perhaps referencing major patient issues that have been previously presented, but focusing on new information about these issues and/or what has changed. Give the patient’s name, age, date of admission, briefly review the present illness, physical examination and admitting diagnosis. Then report any new finding, laboratory tests, diagnostic procedures and changes in medications.
The attending physician will ask the patient’s permission to have the medical student present their case. After making the proper introductions the attending will let the patient know they may offer input or ask questions at any point. When presenting at bedside the student should try to involve the patient.
Preparing for the Presentation
There are four things you must consider before you do your oral presentation
- Occasion (setting and circumstances)
Ask yourself what do you want the presentation to do
- Present a new patient to your preceptor : the amount of detail will be determined by your preceptor. It is also likely to reflect your development and experience, with less detail being required as you progress.
- Present your patient at working or teaching rounds : the amount of detail will be determined by the customs of the group. The focus of the presentation will be influenced by the learning objectives of working responsibilities of the group.
- Request a consultant’s advice on a clinical problem : the presentation will be focused on the clinical question being posed to the consultant.
- Persuade others about a diagnosis and plan : a shorter presentation which highlights the pertinent positives and negatives that are germane to the diagnosis and/or plan being suggested.
- Enlist cooperation required for patient care : a short presentation focusing on the impact your audience can have in addressing the patient’s issues.
Preparation
- Patient evaluation : history, physical examination, review of tests, studies, procedures, and consultants’ recommendations.
- Selected reading : reference texts; to build a foundational understanding.
- Literature search : for further elucidation of any key references from selected reading, and to bring your understanding up to date, since reference text information is typically three to seven years old.
- Write-up : for oral presentation, just succinct notes to serve as a reminder or reference, since you’re not going to be reading your presentation.
Knowledge (Be prepared to answer questions about the following)
- Pathophysiology
- Complications
- Differential diagnosis
- Course of conditions
- Diagnostic tests
- Medications
- Essential Evidence Plus
Template for Oral Presentations
Chief Complaint (CC)
The opening statement should give an overview of the patient, age, sex, reason for visit and the duration of the complaint. Give marital status, race, or occupation if relevant. If your patient has a history of a major medical problem that bears strongly on the understanding of the present illness, include it. For ongoing care, give a one sentence recap of the history.
History of Present Illness (HPI)
This will be very similar to your written HPI. Present the most important problem first. If there is more than one problem, treat each separately. Present the information chronologically. Cover one system before going onto the next. Characterize the chief complaint – quality, severity, location, duration, progression, and include pertinent negatives. Items from the ROS that are unrelated to the present problem may be mentioned in passing unless you are doing a very formal presentation. When you do your first patient presentation you may be expected to go into detail. For ongoing care, present any new complaints.
Review of Systems (ROS)
Most of the ROS is incorporated at the end of the HPI. Items that are unrelated to the present problem may be briefly mentioned. For ongoing care, present only if new complaints.
Past Medical History (PMH)
Discuss other past medical history that bears directly on the current medical problem. For ongoing care, have the information available to respond to questions.
Past Surgical History
Provide names of procedures, approximate dates, indications, any relevant findings or complications, and pathology reports, if applicable. For ongoing care, have the information available to respond to questions.
Allergies/Medications
Present all current medications along with dosage, route and frequency. For the follow-up presentation just give any changes in medication. For ongoing care, note any changes.
Smoking and Alcohol (and any other substance abuse)
Note frequency and duration. For ongoing care, have the information available to respond to questions.
Social/Work History
Home, environment, work status and sexual history. For ongoing care, have the information available to respond to questions.
Family History Note particular family history of genetically based diseases. For ongoing care, have the information available to respond to questions.
Physical Exam/Labs/Other Tests
Include all significant abnormal findings and any normal findings that contribute to the diagnosis. Give a brief, general description of the patient including physical appearance. Then describe vital signs touching on each major system. Try to find out in advance how thorough you need to be for your presentation. There are times when you will be expected to give more detail on each physical finding, labs and other test results. For ongoing care, mention only further positive findings and relevant negative findings.
Assessment and Plan
Give a summary of the important aspects of the history, physical exam and formulate the differential diagnosis. Make sure to read up on the patient’s case by doing a search of the literature.
- Include only the most essential facts; but be ready to answer ANY questions about all aspects of your patient.
- Keep your presentation lively.
- Do not read the presentation!
- Expect your listeners to ask questions.
- Follow the order of the written case report.
- Keep in mind the limitation of your listeners.
- Beware of jumping back and forth between descriptions of separate problems.
- Use the presentation to build your case.
- Your reasoning process should help the listener consider a differential diagnosis.
- Present the patient as well as the illness .
- << Previous: Home
- Next: Posing the Clinical Question >>
- Last Updated: Jul 19, 2023 10:52 AM
- URL: https://rowanmed.libguides.com/tools
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Clin Med (Lond)
- v.16(2); 2016 Apr
Syphilis: presentations in general medicine
Farai nyatsanza.
A Jefferiss Wing for Sexual Health, Imperial College NHS Healthcare Trust, London, UK
Craig Tipple
B Jefferiss Wing for Sexual Health, Imperial College NHS Healthcare Trust, London, UK
Syphilis is caused by the spirochete bacterium Treponema pallidum and can be transmitted both sexually and from mother to child. T pallidum can infect any organ and produces a clinical disease with a relapsing and remitting course. It is not hard to see, therefore, why it is often described as the great mimic. In this review, we provide an update of modern syphilis epidemiology, clinical presentations, and testing and treatment strategies.
- The incidence of syphilis has increased significantly over the last 15 years. The majority of cases are among men who have sex with men (MSM) aged 25–35 of whom 40% are HIV positive.
- Syphilis is a systemic disease from the outset and can involve any organ. It typically presents with a genital ulcer or a rash but its manifestations are protean.
- For MSM presenting unwell with a rash, primary HIV infection is a key differential diagnosis and all patients with suspected syphilis should also be tested for HIV.
- Diagnosis is confirmed serologically using two specific treponemal tests followed by a non-treponemal test to assess disease stage and to allow treatment monitoring.
- Penicillin G treatment remains effective as does oral doxycycline, but macrolide antibiotics should be avoided due to widespread resistance.
Introduction
Syphilis is caused by the bacterium Treponema pallidum subspecies pallidum . 1 This motile, gram-negative spirochete can be transmitted both sexually and from mother to child, and can invade virtually any organ or structure in the human body. The disease, which should be considered systemic throughout, is characterised by overlapping clinical stages and a relapsing and remitting course. This potentially diverse presentation led Sir William Osler to call syphilis ‘the great imitator’ and, together with a greatly increased incidence over the last 15 years, explains its importance to the general physician.
Epidemiology
Syphilis emerged in Europe after 1492 following the return of Columbus from the New World, although its presence in Europe prior to his return is still debated. Paleontological findings have been joined by data from gene sequence analysis of T pallidum subspecies and strains to both support and refute the ‘Columbian’ theory. 1,2 No matter the origin, syphilis spread rapidly through Europe in the 15th century. By the end of Queen Victoria's reign, around 1:10 sexually active adults in London were thought to be infected, although the true prevalence wasn't known until the description of the first serologic test by Auguste Wasserman in 1906. 3
Incidence in the UK declined greatly following the widespread use of penicillin in the early 1950s. Unfortunately, the last 15 years have seen a 10-fold increase in cases, with 4,317 reported new infections in 2014 – the highest for over 40 years. This rise is predominantly among men who have sex with men (MSM), who account for 80.6% of cases. 4 Enhanced surveillance data show that the general profile is one of white MSM aged 25–34, reporting high numbers of sexual partners, condomless sex, recreational drug use and the use of social networking apps to find sexual partners. Approximately 40% are co-infected with HIV-1. 5 Over a similar period, there has been a decline of 16% in female cases from 317 in 2003 to 265 in 2012. In 2011, the overall incidence of congenital syphilis in England was 0.0025/1,000 births. Cases predominated among women not accessing healthcare due to cultural barriers and social deprivation. 6
Clinical presentation
The clinical course of syphilis is one of overlapping clinical stages which begin 9–90 (median 21) days following direct contact with an infectious lesion (Fig (Fig1 1 ).

The clinical stages of syphilis. The clinical stages of syphilis from contact with T pallidum through to development of tertiary disease. During the first year of latent infection, 25% of patients will relapse to the secondary stage.
Primary syphilis
Primary syphilis is characterised by a papule at the point of entry of the bacterium that breaks down into an ulcer (chancre). Although classically anogenital, it can be in the mouth (30% of cases are transmitted through orogenital contact), rectum, cervix or other such clinically ‘quieter’ locations. A chancre is typically painless, 0.5–2 cm in diameter, firm or rubbery, and associated with regional lymphadenopathy (Fig (Fig2). 2 ). It usually heals over a 4–6 week period. Atypical presentations with multiple or painful ulcers can occur, especially in the context of HIV-1 co-infection. 7 Important differential diagnoses are herpes simplex virus and lymphogranuloma venerum.

Clinical pictures of patients with early syphilis. Clinical photographs of patients with early syphilis: a) typical maculopapular rash on the chest; b) skin with secondary syphilis rash at high magnification; c) penile chancre. Images obtained from the Wellcome Photo Library (N0000562, N0000822 and N0000823) and reproduced with permission.
Secondary syphilis
The secondary stage of infection begins 4–10 weeks after the ulcer has healed, although this is highly variable and the primary and secondary stages can be concurrent. The hallmark sign is a maculopapular rash (seen in 50–70% of patients) that may affect the palms and soles (Fig (Fig2 2 ). 8 Other signs and symptoms are described in Table Table1. 1 . The rash and especially the moist lesions of secondary syphilis are infectious. Given the shared epidemiology of HIV and syphilis, primary HIV infection is an important differential diagnosis in MSM presenting with a rash.
The clinical manifestations of syphilis.
Latent syphilis
In the absence of treatment, features of secondary syphilis typically regress within three months and the disease becomes latent and non-infectious. Clinical relapses may occur during the first two years of latency (early latent disease), but are rare thereafter (late latent disease). 9
Tertiary disease
Following the latent stage (typically 15–30 years), signs and symptoms of tertiary infection may occur. These are now rare due to the lower prevalence of the disease 15–30 years ago and the widespread use of treponemocidal and treponemostatic antibiotics (penicillins, tetracyclines, macrolides, cephalosporins) for other infections. Tertiary disease is typically divided into gummatous (the most common), cardiovascular and neurological disease. Deep-seated and destructive gumma can occur in any organ but mainly affect the skin and bones. Cardiovascular syphilis mainly affects the aortic valve and ascending aorta most commonly causing aortic dilatation and regurgitation. Neurological features are discussed below.
Neurological involvement
Neurological involvement can occur at any stage. During the early stages of syphilis, the meninges, vasculature, cranial nerves (particularly II and VIII) and the eyes are most commonly affected. In the tertiary stage, the most common forms involve the brain and spinal cord parenchyma. Each form has characteristic clinical findings, although some overlap may occur (Table (Table1). 1 ). All patients with suspected or confirmed syphilis and neurological symptoms should undergo a full neurological examination. 9
Serologic tests can be used to diagnose all stages of syphilis. They consist of treponemal tests (TT) such as the Treponema pallidum particle agglutination (TPPA) assay or the IgM/IgG enzyme immunoassay (EIA) and non-treponemal (anti-cardiolipin) tests (NTT) such as rapid plasma reagin (RPR) or venereal disease research laboratory (VDRL) tests (NB VDRL testing is no longer widely available in the UK). 10 TT are often the first to become positive (from two weeks after infection) and usually remain positive for life. NTT are performed quantitatively and are used to monitor treatment response. They give an indication of disease stage as higher titres are associated with more active (early) infection and lower titres indicate quieter (latent) or previously treated infection. NTT are subject to both biologic false positive (pregnancy, recent vaccination, autoimmune disease) and false negative (at very high titres due to a prozone phenomenon) results. It is also important to note that NTT may be negative in early primary infection.
There are two testing algorithms in use termed ‘conventional’ and ‘reverse’. The reverse algorithm is used in the UK and begins with an EIA followed by confirmation with a second TT (TPPA). Stage of disease is then assessed with the RPR titre. 11 This method has the advantage of an automatable screening test (EIA) but can have a lower positive predictive value in low prevalence populations. It is noteworthy that other treponemal infections (yaws, pinta, bejel) are serologically indistinct from venereal syphilis.
Serologic tests can be performed on cerebrospinal fluid (CSF). A positive NTT is highly specific for neurosyphilis but lacks sensitivity. A negative TT on a CSF sample with a negligible red blood cell count (visible blood contamination can lead to false positive results) effectively excludes neurosyphilis.
In the genitourinary medicine (GUM) clinic, primary and secondary syphilis can also be diagnosed by the direct identification of T pallidum using darkground microscopy (DGM) or polymerase chain reaction (PCR). 10 With optimal conditions, DGM can have a sensitivity of 80%. 12 Due to contamination by commensal treponemes, such as Treponema denticola , the specificity of DGM for oral and rectal lesions is low. T pallidum PCR has a characteristically high sensitivity (80–100%) and specificity (92.1–99.8%). 13
Patients with signs or symptoms of syphilis should be referred to a GUM physician. The current recommended antimicrobial treatment of syphilis is well explained in the national treatment guideline. 9 Basic management considerations are as follows.
- Benzylpenicillin (penicillin G) was first used to treat syphilis in 1943 and penicillin is still the first-line treatment for all stages of syphilis. 9 Duration and route vary according to stage but in the absence of neurological involvement depot parental preparations of penicillin are first line. In patients with allergy, doxycycline and ceftriaxone are alternative treatments.
- Patients with syphilis are at risk of other sexually transmitted infections (STIs). A full sexual history should be taken and STI screening, including an HIV test, should be offered.
- An RPR titre should be sent on the first day of treatment as a four-fold (two dilution) reduction in titre is the established serologic measure of treatment success.
- Patients should abstain from sexual contact for two weeks following treatment for early syphilis. 15 All sexual contacts within the last three months should be contacted and tested.
- HIV-1 infected patients with CD4 counts <350 cells/ml and/or RPR titres ≥1:32 may be at increased risk of neurological involvement.
- Patients with symptomatic disease should be warned about Jarisch–Herxheimer reaction (JHR) prior to treatment. The JHR is a self-limiting acute febrile illness which typically begins 12 hours after treatment and is complete 12 hours later. 9 It is a particular concern in pregnancy and in patients with neurological or cardiovascular involvement. 16 Steroids can be given before and during the first few days of treatment for neurological and cardiovascular syphilis. In most cases, rest and paracetamol suffice.

Antimicrobial resistance
Despite over 70 years of use, T pallidum remains sensitive to penicillin. 17 Azithromycin was proven an effective treatment for early disease in two randomised controlled trials. 18,19 Unfortunately, 60–80% of T pallidum strains in the UK are macrolide resistant thus it cannot be used reliably. 20 As yet, there has been no description of tetracycline resistance in T pallidum .
Managing syphilis: a worked example
A 78 year-old Jamaican gentleman with memory impairment had syphilis serology sent as part of a dementia screen. The result returned as EIA positive, TPPA positive and RPR negative.
Key history
- Where possible, take a sexual history in a confidential environment. 14
- If yes, ascertain if this treatment was adequate (compliance, treatment given, partners treated?).
- If previously negative, then this could be new infection.
- If yes, then serologic results may be secondary to yaws. If there is a clear history of treatment and the RPR is negative then patient may not require further treatment.
- Previous symptoms consistent with primary or secondary syphilis? Current symptoms consistent with tertiary disease (other than memory impairment)?
Examination
- Seek other signs of late neurosyphilis in addition to gummatous and cardiovascular disease. Be mindful of the possibility of late congenital syphilis, signs of which are detailed elsewhere. 9
- Liaise with GUM team.
- Relevant neurological signs should prompt CSF examination (with prior brain imaging such as CT or MRI). If the patient cannot tolerate lumbar puncture, then consider presumptive neurosyphilis treatment. This patient had a negative serum RPR, thus late neurosyphilis is highly unlikely.
- Offer screening to past and present sexual partners (if contactable) and children if there is no evidence of the mother of the children being tested.
Syphilis has re-emerged as an important sexually transmitted infection. Timely diagnosis and treatment is necessary to prevent onward transmission and the development of irreversible tissue damage. Suspicion of the infection should prompt serologic testing and referral to a GUM physician.
Acknowledgements
The authors thank Dr David Goldmeier for his helpful input during the preparation of this manuscript.
- Associated Hospital
- Medical Program Regulations
Research Areas
- Student Life
- Centre of Excellence
- Leadership Team

Department of General Medicine
- The Department of General Medicine holds expert and experienced faculty who graduated from prestigious institutes who constantly update themselves and work to achieve the benchmark in the realm of knowledge and teaching.
- If specialties form the cornerstones of medicine, then general medicine provides the fundamental base for the diagnosis and treatment of patients.
- This department works round-the-clock, taking care of around 50,000 outpatients and 10,000 inpatients in the department of general medicine, and brings students in vital medical contact with patients.
- Here students gain sound knowledge of the various systems in use in the hospital for patient monitoring and care. This exposure is supplemented by theoretical sessions with the help of advanced teaching techniques and learning aids that are present in all the lecture halls.
- These facilities are put to good use by the practicing faculty that make up this department. The faculty members, besides practicing medicine, conduct Continuing Medical Education (CME) programs and attend national and international conferences to exchange knowledge on the progress made in different areas of medicine.

Quick Access
Infrastructure.
- Teaching Learning Method
Achievements and Awards

- The Department of General Medicine sees itself as setting benchmarks in the quality of patient care, training care doctors and physicians to international standards, and being a leader in meaningful, translational research that benefits the community and country

Our Mission
- To provide affordable, quality health care and medical leadership for the community in which it is situated.
- To impart excellent medical education to create a community of caring, ethical, and world-class physicians.
- To encourage research that is relevant and original, thus furthering medical knowledge.
- To contribute to the strength of the institution by developing strong communication across all departments.
- MBBS - 250 students per year
- Clinical class daily from 8.00 am – 11.00 am.
- Early clinical introduction class for 1st-semester students on Saturdays
- Elective posting in diabetology for the 6th semester
- MD - 25 Students per year
- Clinical (case presentation and discussion)
- Journal Club
- Group Discussion
- Clinico pathological class
- Grand Rounds
- Guest Lectures
- 2 full-time scholars undergoing a Ph.D. program in diabetes and microbiota research under Dr J S Kumar.
- Lecture halls – 1
- Clinical Demo rooms - 9 ( each 50 to 60 sq m )
- Library – 1 ( 100.17sq.m )
- Live streaming with WIFI connection available
- Audio-visual equipment available
- Bedside Ultrasonography and Echocardiography
Dr. J.s.kumar
Professor & head Associate dean (pg academics)
Dr. K.T.Jayakumar
Dr. k.subramaniyan, dr. k. madhavan, dr. s.n.meenakshi sundari, dr. t.a.vidhya, dr. g.kothai, dr. g. gopikrishna.
Associate Professor
Dr. R. Nanda Kumar
Dr. nirmala devi, dr. v. vrindha, dr. rm ramachandran.
Assistant Professor
Dr.J.Aarthi
Dr. ashwin narayanan, dr. sivaprakash s, dr.akita gopinath.
Senior Resident
Dr.Purnima.R
M.B.B.S ., DNB (GEN MEDICINE).
Dr.Baddepudi Thanmayee Reddy
M.B.B.S ., M.D ( General Medicine )
Dr. Aniket Sinha
Dr. cherukuri naga sekhar, dr.niveda srivatsa, dr. radhika m l v, dr. vishnupriya vuchuru, dr. reena jose d.
Asst. Professor
Dr.Manoj Kumar M
Dr. mythili k, dr. kavin kumar s, dr. aswin c, dr. vaishnavi r, dr. mohamed sajad akbar, dr.sreeuthra b, dr.ch.nagasekhar.
- Flipped classroom - Small group teaching with prior study material
- Simulation-based teaching: Mannequins and computer-assisted learning
- Integrated Teaching - Vertical and Horizontal Teaching for MBBS Students
- Group discussions - Regularly
- Journal clubs and Seminars for PGs - Twice in a week
- Video demonstrations - Journal Club – Discussion
- Mentoring - Group of students assigned for all the faculties
- Feedback and counseling - After every internal assessment test
- Ongoing Research Projects
- Research Publication
Scope of Services
- Hand Surgery
- Micro Vascular Surgery
- Oncoplastic Surgery [ Cancer Reconstruction ]
- 24x7 Trauma care
- Cleft lip, Cleft palate & craniofacial anomaly Surgery
- Lymphedema care
- Complex wound management
- Aesthetic Surgery
- Smile Train Project
- Facio Maxillary Trauma

Testimonials

SRM Medical College Hospital And Research Centre, SRM Nagar,Potheri, Chengalpattu, Tamil Nadu 603203.
For Admissions, Contact
7418907444 7418905444
044-4743-2350
Quick Links

MINI REVIEW article
This article is part of the research topic.
Insights in Cardiology from Caring for a Diverse Community: Perspectives from Inova Schar Heart and Vascular
Management of Peripheral Arterial Disease in the Context of a Multidisciplinary Limb Program Provisionally Accepted

- 1 Inova Schar Heart and Vascular, United States
The final, formatted version of the article will be published soon.
Peripheral artery disease, or PAD, continues to increase in prevalence worldwide due to risk factors such as advanced age, diabetes mellitus, and obesity. Critical limb ischemia (CLTI) is the advanced form of PAD that can result in lack of healing and limb loss as the most devastating consequence. Patients with PAD, especially CLTI, benefit from multidisciplinary care to optimize outcomes by reducing cardiovascular morbidity and mortality as well as prevent lower extremity amputation. Collaboration between various specialties allows a focus on problems involved in treating the patient with PAD including prevention, screening, medical care, wound care, infection, and revascularization when needed. Although, there is not a clear definition or consensus on the structure of the PAD team, certain guidelines are applicable to most clinical scenarios emphasizing "provider champions" to lead the clinical program. A vascular specialist (vascular surgery, interventional radiology, interventional cardiology) and a soft tissue specialist (podiatry, plastic surgery) are the typical "champions" with orthopedics, general surgery, vascular medicine, diabetology/endocrinology, infectious disease, nephrology, and rehabilitation medicine often involved. The team should also include wound nurses, nutritionists, occupational therapists, orthotists, pharmacists, physical therapists, prosthetists, and social workers. This paper is a brief overview of the structure of the multidisciplinary team with key components and functions of such a team to optimize treatment outcomes for PAD and CLTI.
Keywords: artery, multidisciplinary, Amputation, vascular, CLTI
Received: 11 Jan 2024; Accepted: 11 Apr 2024.
Copyright: © 2024 Neville. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Mx. Richard Neville, Inova Schar Heart and Vascular, Falls Church, United States
People also looked at
This paper is in the following e-collection/theme issue:
Published on 11.4.2024 in Vol 26 (2024)
Evaluating the Digital Health Experience for Patients in Primary Care: Mixed Methods Study
Authors of this article:

Original Paper
- Melinda Ada Choy 1, 2 , BMed, MMed, DCH, MD ;
- Kathleen O'Brien 1 , BSc, GDipStats, MBBS, DCH ;
- Katelyn Barnes 1, 2 , BAPSC, MND, PhD ;
- Elizabeth Ann Sturgiss 3 , BMed, MPH, MForensMed, PhD ;
- Elizabeth Rieger 1 , BA, MClinPsych, PhD ;
- Kirsty Douglas 1, 2 , MBBS, DipRACOG, Grad Cert HE, MD
1 School of Medicine and Psychology, College of Health and Medicine, The Australian National University, Canberra, Australia
2 Academic Unit of General Practice, Office of Professional Leadership and Education, ACT Health Directorate, Canberra, Australia
3 School of Primary and Allied Health Care, Monash University, Melbourne, Australia
Corresponding Author:
Melinda Ada Choy, BMed, MMed, DCH, MD
School of Medicine and Psychology
College of Health and Medicine
The Australian National University
Phone: 61 51244947
Email: [email protected]
Background: The digital health divide for socioeconomic disadvantage describes a pattern in which patients considered socioeconomically disadvantaged, who are already marginalized through reduced access to face-to-face health care, are additionally hindered through less access to patient-initiated digital health. A comprehensive understanding of how patients with socioeconomic disadvantage access and experience digital health is essential for improving the digital health divide. Primary care patients, especially those with chronic disease, have experience of the stages of initial help seeking and self-management of their health, which renders them a key demographic for research on patient-initiated digital health access.
Objective: This study aims to provide comprehensive primary mixed methods data on the patient experience of barriers to digital health access, with a focus on the digital health divide.
Methods: We applied an exploratory mixed methods design to ensure that our survey was primarily shaped by the experiences of our interviewees. First, we qualitatively explored the experience of digital health for 19 patients with socioeconomic disadvantage and chronic disease and second, we quantitatively measured some of these findings by designing and administering a survey to 487 Australian general practice patients from 24 general practices.
Results: In our qualitative first phase, the key barriers found to accessing digital health included (1) strong patient preference for human-based health services; (2) low trust in digital health services; (3) high financial costs of necessary tools, maintenance, and repairs; (4) poor publicly available internet access options; (5) reduced capacity to engage due to increased life pressures; and (6) low self-efficacy and confidence in using digital health. In our quantitative second phase, 31% (151/487) of the survey participants were found to have never used a form of digital health, while 10.7% (52/487) were low- to medium-frequency users and 48.5% (236/487) were high-frequency users. High-frequency users were more likely to be interested in digital health and had higher self-efficacy. Low-frequency users were more likely to report difficulty affording the financial costs needed for digital access.
Conclusions: While general digital interest, financial cost, and digital health literacy and empowerment are clear factors in digital health access in a broad primary care population, the digital health divide is also facilitated in part by a stepped series of complex and cumulative barriers. Genuinely improving digital health access for 1 cohort or even 1 person requires a series of multiple different interventions tailored to specific sequential barriers. Within primary care, patient-centered care that continues to recognize the complex individual needs of, and barriers facing, each patient should be part of addressing the digital health divide.
Introduction
The promise of ehealth.
The rapid growth of digital health, sped up by the COVID-19 pandemic and associated lockdowns, brings the promise of improved health care efficiency, empowerment of consumers, and health care equity [ 1 ]. Digital health is the use of information and communication technology to improve health [ 2 ]. eHealth, which is a type of digital health, refers to the use of internet-based technology for health care and can be used by systems, providers, and patients [ 2 ]. At the time of this study (before COVID-19), examples of eHealth used by patients in Australia included searching for web-based health information, booking appointments on the web, participating in online peer-support health forums, using mobile phone health apps (mobile health), emailing health care providers, and patient portals for electronic health records.
Digital health is expected to improve chronic disease management and has already shown great potential in improving chronic disease health outcomes [ 3 , 4 ]. Just under half of the Australian population (47.3%) has at least 1 chronic disease [ 5 ]. Rates of chronic disease and complications from chronic disease are overrepresented among those with socioeconomic disadvantage [ 6 ]. Therefore, patients with chronic disease and socioeconomic disadvantage have a greater need for the potential benefits of digital health, such as an improvement in their health outcomes. However, there is a risk that those who could benefit most from digital health services are the least likely to receive them, exemplifying the inverse care law in the digital age by Hart [ 7 ].
Our Current Understanding of the Digital Health Divide
While the rapid growth of digital health brings the promise of health care equity, it may also intensify existing inequities [ 8 ]. The digital health divide for socioeconomic disadvantage describes a pattern in which patients considered socioeconomically disadvantaged who are already marginalized through poor access to traditional health care are additionally hindered through poor access to digital health [ 9 ]. In Australia, only 67.4% of households in the lowest household income quintile have home internet access, compared to 86% of the general population and 96.9% of households in the highest household income quintile [ 10 ]. Survey-based studies have also shown that even with internet access, effective eHealth use is lower in populations considered disadvantaged, which speaks to broader barriers to digital health access [ 11 ].
The ongoing COVID-19 global pandemic has sped up digital health transitions with the rapid uptake of telephone and video consultations, e-prescription, and the ongoing rollout of e-mental health in Australia. These have supported the continuation of health care delivery while limiting physical contact and the pandemic spread; however, the early evidence shows that the digital health divide remains problematic. A rapid review identified challenges with reduced digital access and digital literacy among the older adults and racial and ethnic minority groups, which are both groups at greater health risk from COVID-19 infections [ 12 ]. An Australian population study showed that the rapid uptake of telehealth during peak pandemic was not uniform, with the older adults, very young, and those with limited English language proficiency having a lower uptake of general practitioner (GP) telehealth services [ 13 ].
To ensure that digital health improves health care outcome gaps, it is essential to better understand the nature and nuance of the digital health divide for socioeconomic disadvantage. The nature of the digital health divide for socioeconomic disadvantage has been explored primarily through quantitative survey data, some qualitative papers, a few mixed methods papers, and systematic reviews [ 11 , 14 - 16 ]. Identified barriers include a lack of physical hardware and adequate internet bandwidth, a reduced inclination to seek out digital health, and a low ability and confidence to use digital health effectively [ 16 ]. The few mixed methods studies that exist on the digital health divide generally triangulate quantitative and qualitative data on a specific disease type or population subgroup to draw a combined conclusion [ 17 , 18 ]. These studies have found digital health access to be associated with education, ethnicity, and gender as well as trust, complementary face-to-face services, and the desire for alternative sources of information [ 17 , 19 ].
What This Work Adds
This project sought to extend previous research by using an exploratory mixed methods design to ensure that the first step and driver of our survey of a larger population was primarily shaped by the experiences of our interviewees within primary care. This differs from the triangulation method, which places the qualitative and quantitative data as equal first contributors to the findings and does not allow one type of data to determine the direction of the other [ 18 ]. We qualitatively explored the experience of digital health for patients with socioeconomic disadvantage and chronic disease and then quantitatively measured some of the qualitative findings via a survey of the Australian general practice patient population. Our key objective was to provide comprehensive primary mixed methods data, describing the experience and extent of barriers to accessing digital health and its benefits, with a focus on the digital health divide. We completed this research in a primary care context to investigate a diverse community-based population with conceivable reasons to seek digital help in managing their health. Findings from this mixed methods study were intended to provide health care providers and policy makers with a more detailed understanding of how specific barriers affect different aspects or steps of accessing digital health. Ultimately, understanding digital health access can influence the future design and implementation of digital health services by more effectively avoiding certain barriers or building in enablers to achieve improved digital health access not only for everyone but also especially for those in need.
Study Design
We conducted a sequential exploratory mixed methods study to explore a complex phenomenon in depth and then measure its prevalence. We qualitatively explored the experience of digital health for patients with chronic disease and socioeconomic disadvantage in the first phase. Data from the first phase informed a quantitative survey of the phenomenon across a wider population in the second phase [ 18 ]. Both stages of research were conducted before the COVID-19 pandemic in Australia.
Recruitment
Qualitative phase participants.
The eligibility criteria for the qualitative phase were as follows: English-speaking adults aged ≥18 years with at least 1 self-reported chronic disease and 1 marker of socioeconomic disadvantage (indicated by ownership of a Health Care Card or receiving a disability pension, unemployment, or a user of public housing). A chronic disease was defined to potential participants as a diagnosed long-term health condition that had lasted at least 6 months (or is expected to last for at least 6 months; examples are listed in Multimedia Appendix 1 ). The markers of socioeconomic disadvantage we used to identify potential participants were based on criteria typically used by local general practices to determine which patients can have lower or no out-of-pocket expenses. Apart from unemployment, the 3 other criteria to identify socioeconomic disadvantage are means-tested government-allocated public social services [ 20 ]. Qualitative phase participants were recruited from May to July 2019 through 3 general practices and 1 service organization that serve populations considered socioeconomically disadvantaged across urban, regional, and rural regions in the Australian Capital Territory and South Eastern New South Wales. A total of 2 recruitment methods were used in consultation with and as per the choice of the participating organizations. Potential participants were either provided with an opportunity to engage with researchers (KB and MAC) in the general practice waiting room or identified by the practice or organization as suitable for an interview. Interested participants were given a detailed verbal and written description of the project in a private space before providing written consent to be interviewed. All interview participants received an Aus $50 (US $32.68) grocery shopping voucher in acknowledgment of their time.
Quantitative Phase Participants
Eligibility for the quantitative phase was English-speaking adults aged ≥18 years. The eligibility criteria for the quantitative phase were deliberately broader than those for the qualitative phase to achieve a larger sample size within the limitations of recruitment and with the intention that the factors of socioeconomic disadvantage and having a chronic disease could be compared to the digital health access of a more general population. The quantitative phase participants were recruited from November 2019 to February 2020. Study information and paper-based surveys were distributed and collected through 24 general practices across the Australian Capital Territory and South Eastern New South Wales regions, with an option for web-based completion.
Ethical Considerations
Qualitative and quantitative phase research protocols, including the participant information sheet, were approved by the Australian Capital Territory Health Human Research Ethics Committee (2019/ETH/00013) and the Australian National University Human Research Ethics Committee (2019/ETH00003). Qualitative phase participants were given a verbal and written explanation of the study, including how and when they could opt out, before they provided written consent. All interview participants received an Aus $50 (US $32.68) grocery shopping voucher in acknowledgment of their time. Quantitative participants were given a written explanation and their informed consent was implied by return of a completed survey. Participants in both phases of the study were told that all their data was deidentified. Consent was implied through the return of a completed survey.
Qualitative Data Collection and Analysis
Participants were purposively sampled to represent a range in age, gender, degree of socioeconomic disadvantage, and experience of digital health. The sampling and sample size were reviewed regularly by the research team as the interviews were being completed to identify potential thematic saturation.
The interview guide was developed by the research team based on a review of the literature and the patient dimensions of the framework of access by Levesque et al [ 21 ]. The framework by Levesque et al [ 21 ] is a conceptualization of health care access comprising 5 service and patient dimensions of accessibility and ability. The patient dimensions are as follows: (1) ability to perceive, (2) ability to seek, (3) ability to reach, (4) ability to pay, and (5) ability to engage [ 21 ]. The key interview topics included (1) digital health use and access, including facilitators and barriers; (2) attitudes toward digital health; and (3) self-perception of digital health skills and potential training. The interview guide was reviewed for face and content validity by the whole research team, a patient advocate, a digital inclusion charity representative, and the general practices where recruitment occurred. The questions and guide were iteratively refined by the research team to ensure relevance and support reaching data saturation. The interview guide has been provided as Multimedia Appendix 1 . The interviews, which took 45 minutes on average, were taped and transcribed. An interview summary sheet and reflective journal were completed by the interviewer after each interview to also capture nonverbal cues and tone.
Interview transcriptions were coded and processed by inductive thematic analysis. Data collection and analysis were completed in parallel to support the identification of data saturation. Data saturation was defined as no significant new information arising from new interviews and was identified by discussion with the research team [ 22 ]. The 2 interviewers (MAC and KB) independently coded the first 5 transcripts and reflected on them with another researcher (EAS) to ensure intercoder validity and reliability. The rest of the interviews were coded independently by the 2 interviewers, who regularly met to reflect on emerging themes and thematic saturation. Data saturation was initially indicated after 15 interviews and subsequently confirmed with a total of 19 interviews. Coding disagreements and theme development were discussed with at least 1 other researcher (EAS, ER, and KD). Thematic saturation and the final themes were agreed upon by the entire research team.
Quantitative Survey Development
The final themes derived in the qualitative phase of the project guided the specific quantitative phase research questions. The final themes were a list of ordered cumulative barriers experienced by participants in accessing digital health and its benefits ( Figure 1 ). The quantitative survey was designed to test the association between barriers to access and the frequency of use of digital health as a proxy measure for digital health access.

In the survey, the participants were asked about their demographic details, health and chronic diseases, knowledge, use and experience of digital health tools, internet access, perception of digital resource affordability, trust in digital health and traditional health services, perceived capability, health care empowerment, eHealth literacy, and relationship with their GP.
Existing scales and questions from the literature and standardized Australian-based surveys were used whenever possible. We used selected questions and scales from the Australian Bureau of Statistics standards, the eHealth Literacy Scale (eHEALS), the eHealth Literacy Questionnaire, and the Southgate Institute for Health Society and Equity [ 17 , 23 - 26 ]. We adapted other scales from the ICEpop Capability Measure for Adults, the Health Care Empowerment Inventory (HCEI), the Patient-Doctor Relationship Questionnaire, and the Chao continuity questionnaire [ 23 , 27 - 29 ]. Where an existing scale to measure a barrier or theme did not exist, the research team designed the questions based on the literature. Our questions around the frequency of digital health use were informed by multiple existing Australian-based surveys on general technology use [ 30 , 31 ]. Most of the questions used a Likert scale. Every choice regarding the design, adaptation, or copy of questions for the survey was influenced by the qualitative findings and decided on by full agreement among the 2 researchers who completed and coded the interviews. A complete copy of the survey is provided in Multimedia Appendix 2 .
Pilot-testing of the survey was completed with 5 patients, 2 experts on digital inclusion, and 3 local GPs for both the paper surveys and web-based surveys via Qualtrics Core XM (Qualtrics LLC). The resulting feedback on face and content validity, functionality of the survey logic, and feasibility of questionnaire completion was incorporated into the final version of the survey.
The survey was offered on paper with a participant information sheet, which gave the patients the option to complete the web-based survey. The survey was handed out to every patient on paper to avoid sampling bias through the exclusion of participants who could not complete the web-based survey [ 32 ].
Quantitative Data Treatment and Analysis
Data were exported from Qualtrics Core XM to an SPSS (version 26; IBM Corp) data set. Data cleaning and screening were undertaken (KB and KO).
Descriptive statistics (number and percentage) were used to summarize participant characteristics, preference measures, and frequency of eHealth use. Significance testing was conducted using chi-square tests, with a threshold of P <.05; effect sizes were measured by the φ coefficient for 2×2 comparisons and Cramer V statistic for all others. Where the cells sizes were too small, the categories were collapsed for the purposes of significance testing. The interpretation of effect sizes was as per the study by Cohen [ 33 ]. The analysis was conducted in SPSS and SAS (version 9.4; SAS Institute).
Participant Characteristics
Participants’ self-reported characteristics included gender, indigenous status, income category, highest level of education, marital status, and language spoken at home.
Age was derived from participant-reported year of birth and year of survey completion as of 2019 and stratified into age groups. The state or territory of residence was derived from the participant-reported postcode. The remoteness area was derived using the postcode reported by the participants and mapped to a modified concordance from the Australian Bureau of Statistics. Occupation-free text responses were coded using the Australian Bureau of Statistics Census statistics level 1 and 2 descriptors. The country of birth was mapped to Australia, other Organisation for Economic Cooperation and Development countries, and non–Organisation for Economic Cooperation and Development countries.
Frequency of eHealth Use
A summary measure of the frequency of eHealth use was derived from the questions on the use of different types of eHealth.
Specifically, respondents were asked if they had ever used any form of web-based health (“eHealth“) and, if so, to rate how often (never, at least once, every now and then, and most days) against 6 types of “eHealth” (searching for health information online, booking appointments online, emailing health care providers, using health-related mobile phone apps, accessing My Health Record, and accessing online health forums). The frequency of eHealth use was then classified as follows:
- High user: answered “most days” to at least 1 question on eHealth use OR answered “every now and then” to at least 2 questions on eHealth use
- Never user: answered “no” to having ever used any form of eHealth OR “never” to all 6 questions on eHealth use
- Low or medium user: all other respondents.
The frequency of eHealth use was reported as unweighted descriptive statistics (counts and percentages) against demographic characteristics and for the elements of each of the themes identified in phase 1.
Overview of Key Themes
Data were reported against the 6 themes from the phase 1 results of preference, trust, cost, structural access, capacity to engage, and self-efficacy. Where the components of trust, cost, capacity to engage, and self-efficacy had missing data (for less than half of the components only), mean imputation was used to minimize data loss. For each theme, the analysis excluded those for whom the frequency of eHealth use was unknown.
Preference measures (survey section D1 parts 1 to 3) asked participants to report against measures with a 4-point Likert scale (strongly disagree, disagree, agree, and strongly agree). Chi-square tests were conducted after the categories were condensed into 2 by combining strongly disagree and as well as combining strongly agree and agree.
Summary measures for trust were created in 4 domains: trust from the eHealth Literacy Questionnaire (survey section D1 parts 4 to 8), trust from Southgate—GPs, specialists, or allied health (survey section D2 parts 1 to 5), trust from Southgate—digital health (survey section D2 parts 6, 7, 9, and 10), and trust from Southgate—books or pamphlets (survey section D2 part 8). The data were grouped as low, moderate, and high trust based on the assigned scores from the component data. Chi-square tests were conducted comparing low-to-moderate trust against high trust for GP, specialists, or allied health and comparing low trust against moderate-to-high trust for book or pamphlet.
Summary measures for cost were created from survey item C10. To measure cost, participants were asked about whether they considered certain items or services to be affordable. These included cost items mentioned in the qualitative phase interviews relating to mobile phones (1 that connects to the internet, 1 with enough memory space to download apps, downloads or apps requiring payment, repairs, and maintenance costs), having an iPad or tablet with internet connectivity, a home computer or laptop (owning, repairs, and maintenance), home fixed internet access, and an adequate monthly data allowance. These 9 items were scored as “yes definitely”=1 or 0 otherwise. Chi-square tests were conducted with never and low or medium eHealth users combined.
Structural Access
Structural access included asking where the internet is used by participants (survey section C8) and factors relating to internet access (survey section C8 parts 1-3) reporting against a 4-point Likert scale (strongly disagree, disagree, agree, and strongly agree). Chi-square tests were conducted with strongly disagree, disagree, agree, or strongly agree, and never, low, or medium eHealth use combined.
Capacity to Engage
Summary measures for capacity to engage were created from survey section E1. To measure the capacity to engage, participants were asked about feeling “settled and secure,” “being independent,” and “achievement and progress” as an adaptation of the ICEpop Capability Measure for Adults [ 27 ], reporting against a 4-point Likert-like scale. Responses were scored from 1 (“I am unable to feel settled and secure in any areas of my life”) to 4 (“I am able to feel settled and secure in all areas of my life”).
The summary capacity measure was derived by the summation of responses across the 3 questions, which were classified into 4 groups, A to D, based on these scores. Where fewer than half of the responses were missing, mean imputation was used; otherwise, the record was excluded. Groups A and B were combined for significance testing.
Self-Efficacy
Summary measures for self-efficacy were adapted from the eHEALS (E3) and the HCEI (E2) [ 23 , 24 ].
Survey section E3—eHEALS—comprised 8 questions, with participants reporting against a 5-point Likert scale for each (strongly disagree, disagree, neither, agree, and strongly agree). These responses were assigned 1 to 5 points, respectively. The summary eHEALS measure was derived by the summation of responses across the 8 questions, which were classified into 5 groups, A to E, based on these scores. Where fewer than half of the responses were missing, mean imputation was used; otherwise, the record was excluded. Groups A to C and D to E were combined for significance testing.
Survey section E2—HCEI—comprised 5 questions, with participants reporting against a 5-point Likert scale for each (strongly disagree, disagree, neither, agree, and strongly agree). Strongly disagree and disagree and neither were combined, and similarly agree and strongly agree were combined for significance testing.
Qualitative Results
The demographic characteristics of the patients that we interviewed are presented in Table 1 .
The key barriers found to accessing digital health included (1) strong patient preference for human-based health services; (2) low trust in digital health services; (3) high financial costs of necessary tools, maintenance, and repairs; (4) poor publicly available internet access options; (5) reduced capacity to engage due to increased life pressures; and (6) low self-efficacy and confidence in using digital health.
Rather than being an equal list of factors, our interviewees described these barriers as a stepped series of cumulative hurdles, which is illustrated in Figure 1 . Initial issues of preference and trust were foundational to a person even when considering the option of digital health, while digital health confidence and literacy were barriers to full engagement with and optimal use of digital health. Alternatively, interviewees who did use digital health had been enabled by the same factors that were barriers to others.
a GP: general practitioner.
b Multiple answers per respondent.
Strong Patient Preference for Human-Based Health Services
Some patients expressed a strong preference for human-based health services rather than digital health services. In answer to a question about how digital health services could be improved, a patient said the following:
Well, having an option where you can actually bypass actually having to go through the app and actually talk directly to someone. [Participant #10]
For some patients, this preference for human-based health services appeared to be related to a lack of exposure to eHealth. These patients were not at all interested in or had never thought about digital health options. A participant responded the following to the interviewer’s questions:
Interviewer: So when...something feels not right, how do you find out what’s going on?
Respondent: I talk to Doctor XX.
Interviewer: Do you ever Google your symptoms or look online for information?
Respondent: No, I have never even thought of doing that actually. [Participant #11]
For other patients, their preference for human-based health care stemmed from negative experiences with technology. These patients reported actively disliking computers and technology in general and were generally frustrated with what they saw as the pitfalls of technology. A patient stated the following:
If computers and internet weren’t so frigging slow because everything is on like the slowest speed network ever and there’s ads blocking everything. Ads, (expletive) ads. [Participant #9]
A patient felt that he was pushed out of the workforce due his inability to keep up with technology-based changes and thus made a decision to never own a computer:
But, you know, in those days when I was a lot younger those sorts of things weren’t about and they’re just going ahead in leaps and bounds and that’s one of the reasons why I retired early. I retired at 63 because it was just moving too fast and it’s all computers and all those sorts of things and I just couldn’t keep up. [Participant #17]
Low Trust in Digital Health Services
Several patients described low trust levels for digital and internet-based technology in general. Their low trust was generally based on stories they had heard of other people’s negative experiences. A patient said the following:
I don’t trust the internet to be quite honest. You hear all these stories about people getting ripped off and I’ve worked too hard to get what I’ve got rather than let some clown get it on the internet for me. [Participant #11]
Some of this distrust was specific to eHealth. For example, some patients were highly suspicious of the government’s motives with regard to digital health and were concerned about the privacy of their health information, which made them hesitant about the concept of a universal electronic health record. In response to the interviewer’s question, a participant said the following:
Interviewer: Are there any other ways you think that eHealth might help you?
Respondent: I’m sorry but it just keeps coming back to me, Big Brother. [Participant #7]
Another participant said the following:
I just would run a mile from it because I just wouldn’t trust it. It wouldn’t be used to, as I said, for insurance or job information. [Participant #16]
High Financial Costs of the Necessary Tools, Maintenance, and Repairs
A wide variety of patients described affordability issues across several different aspects of the costs involved in digital health. They expressed difficulty in paying for the following items: a mobile phone that could connect to the internet, a mobile phone with enough memory space to download apps, mobile phone apps requiring extra payment without advertisements, mobile phone repair costs such as a broken screen, a computer or laptop, home internet access, and adequate monthly data allowance and speeds to functionally use the internet. Current popular payment systems, such as plans, were not feasible for some patients. A participant stated the following:
I don’t have a computer...I’m not in the income bracket to own a computer really. Like I could, if I got one on a plan kind of thing or if I saved up for x-amount of time. But then like if I was going on the plan I’d be paying interest for having it on like lay-buy kind of thing, paying it off, and if it ever got lost or stolen I would still have to repay that off, which is always a hassle. And yeah. Yeah, I’m like financially not in the state where I’m able to...own a computer right now as I’m kind of paying off a number of debts. [Participant #9]
Poor Publicly Available Internet Access Options
Some patients described struggling without home internet access. While they noted some cost-free public internet access points, such as libraries, hotel bars, and restaurants, they often found these to be inconvenient, lacking in privacy, and constituting low-quality options for digital health. A patient stated the following:
...it’s incredibly slow at the library. And I know why...a friend I went to school with used to belong to the council and the way they set it up, they just got the raw end of the stick and it is really, really slow. It’s bizarre but you can go to the X Hotel and it’s heaps quicker. [Participant #15]
In response to the interviewer's question, a participant said the following:
Interviewer: And do you feel comfortable doing private stuff on computers at the library...?
Respondent: Not really, no, but I don’t have any other choice, so, yeah. [Participant #9]
Reduced Capacity to Engage Due to Increased Life Pressures
When discussing why they were not using digital health or why they had stopped using digital health, patients often described significant competing priorities and life pressures that affected their capacity to engage. An unemployed patient mentioned that his time and energy on the internet were focused primarily on finding work and that he barely had time to focus on his health in general, let alone engage in digital health.
Other patients reported that they often felt that their ability to learn about and spend time on digital health was taken up by caring for sick family members, paying basic bills, or learning English. Some patients said that the time they would have spent learning digital skills when they were growing up had been lost to adverse life circumstances such as being in jail:
So we didn’t have computers in the house when I was growing up. And I didn’t know I’ve never...I’ve been in and out of jail for 28 odd years so it sort of takes away from learning from this cause it’s a whole different… it’s a whole different way of using a telephone from a prison. [Participant #11]
Low Self-Efficacy and Confidence in Starting the Digital Health Process
Some patients had a pervasive self-perception of being slow learners and being unable to use technology. Their stories of being unconfident learners seemed to stem from the fact that they had been told throughout their lives that they were intellectually behind. A patient said the following:
The computer people...wouldn’t take my calls because I’ve always been dumb with that sort of stuff. Like I only found out this later on in life, but I’m actually severely numerically dyslexic. Like I have to triple-check everything with numbers. [Participant #7]
Another patient stated the following:
I like went to two English classes like a normal English class with all the kids and then another English class with about seven kids in there because I just couldn’t I don’t know maybe because I spoke another language at home and they sort of like know I was a bit backward. [Participant #6]
These patients and others had multiple missing pieces of information that they felt made it harder to engage in digital health compared to “easier” human-based services. A patient said the following:
Yeah I’ve heard of booking online but I just I don’t know I find it easier just to ring up. And I’ll answer an email from a health care provider but I wouldn’t know where to start to look for their email address. [Participant #11]
In contrast, the patients who did connect with digital health described themselves as independent question askers and proactive people. Even when they did not know how to use a specific digital health tool, they were confident in attempting to and asking for help when they needed it. A patient said the following:
I’m a “I will find my way through this, no matter how long it takes me” kind of person. So maybe it’s more my personality...If I have to ask for help from somewhere, wherever it is, I will definitely do that. [Participant #3]
Quantitative Results
A total of 487 valid survey responses were received from participants across 24 general practices. The participant characteristics are presented in detail in Table S1 in Multimedia Appendix 3 .
The mean age of the participants was approximately 50 years (females 48.9, SD 19.4 years; males 52.8, SD 20.0 years), and 68.2% (332/487) of the participants identified as female. Overall, 34.3% (151/439) of respondents reported never using eHealth, and 53.8% (236/439) reported high eHealth use.
There were statistically significant ( P <.05) differences in the frequency of eHealth use in terms of age group, gender, state, remoteness, highest level of education, employment status, occupation group, marital status, and language spoken at home, with effect sizes being small to medium. Specifically, high eHealth characteristics were associated with younger age, being female, living in an urban area, and being employed.
Table 2 presents the frequency of eHealth use against 3 internet preference questions.
Preference for using the internet and technology in general and for health needs in particular were significantly related to the frequency of eHealth use ( P <.05 for each), with the effect sizes being small to medium.
a Excludes those for whom frequency of eHealth use is unknown.
b Chi-square tests conducted with strongly disagree and disagree combined, and agree and strongly agree combined.
Table 3 presents the frequency of eHealth use against 4 measures of trust.
The degree of trust was not statistically significantly different for the frequency of eHealth use for any of the domains.
b eHLQ: eHealth Literacy Questionnaire.
c Derived from survey question D1, parts 4 to 8. Mean imputation used where ≤2 responses were missing. If >2 responses were missing, the records were excluded.
d Derived from survey question D2, parts 1 to 5. Mean imputation used where ≤2 responses were missing. If >2 responses were missing, the records were excluded.
e Chi-square test conducted comparing low-to-moderate trust against high trust.
f Derived from survey question D2, parts 6, 7, 9, and 10. Mean imputation used where ≤2 responses were missing. If >2 responses were missing, the records were excluded.
g Derived from survey question D2 part 8.
h Chi-square test conducted comparing low trust against moderate-to-high trust.
Affordability of items and services was reported as No cost difficulty or Cost difficulty. eHealth frequency of use responses were available for 273 participants; among those with no cost difficulty , 1% (2/204) were never users, 14.2% (29/204) were low or medium users, and 84.8% (173/204) were high users of eHealth; among those with cost difficulty , 1% (1/69) were never users, 26% (18/69) were low or medium users, and 73% (50/69) were high users. There was a statistically significant difference in the presence of cost as a barrier between never and low or medium eHealth users compared to high users ( χ 2 1 =5.25; P =.02), although the effect size was small.
Table 4 presents the frequency of eHealth use for elements of structural access.
Quality of internet access and feeling limited in access to the internet were significantly associated with frequency of eHealth use ( P <.05), although the effect sizes were small.
b N/A: not applicable (cell sizes insufficient for chi-square test).
c Chi-square tests conducted with strongly disagree and disagree combined, agree and strongly agree combined, and never and low or medium categories combined.
Table 5 presents the frequency of eHealth use against respondents’ capacity to engage.
Capacity to engage was not significantly different for the frequency of eHealth use ( P =.54).
b Derived from survey item E1. Where 1 response was missing, the mean imputation was used. If >1 response was missing, the record was excluded.
c Chi-square tests conducted with groups A and B combined.
Table 6 presents the frequency of eHealth use for elements of self-efficacy.
Statistically significant results were observed for the relationship between self-efficacy by eHEALS (moderate effect size) and frequency of eHealth use as well as for some of the questions from the HCEI (reliance on health professionals or others to access and explain information; small effect size; P <.05).
b eHEALS: eHealth Literacy Scale.
c eHEALS derived from item E3 (8 parts). Where ≤ 4 responses were missing, mean imputation was used. If >4 responses were missing, the records were excluded. Groups A to C as well as groups D to E were combined for the chi-square test.
d Strongly disagree, disagree, neither, and agree or strongly agree combined for significance testing.
Principal Findings
This paper reports on the findings of a sequential exploratory mixed methods study on the barriers to digital health access for a group of patients in Australian family medicine, with a particular focus on chronic disease and socioeconomic disadvantage.
In the qualitative first phase, the patients with socioeconomic disadvantage and chronic disease described 6 cumulative barriers, as demonstrated in Figure 1 . Many nonusers of digital health preferred human-based services and were not interested in technology, while others were highly suspicious of the technology in general. Some digitally interested patients could not afford quality hardware and internet connectivity, a barrier that was doubled by low quality and privacy when accessing publicly available internet connections. Furthermore, although some digitally interested patients had internet access, their urgent life circumstances left scarce opportunity to access digital health and develop digital health skills and confidence.
In our quantitative second phase, 31% (151/487) of the survey participants from Australian general practices were found to have never used a form of digital health. Survey participants were more likely to use digital health tools frequently when they also had a general digital interest and a digital health interest. Those who did not frequently access digital health were more likely to report difficulty affording the financial costs needed for digital access. The survey participants who frequently accessed digital health were more likely to have high eHealth literacy and high levels of patient empowerment.
Comparison With Prior Work
In terms of general digital health access, the finding that 31% (151/487) of the survey participants had never used one of the described forms of eHealth is in keeping with an Australian-based general digital participation study that found that approximately 9% of the participants were nonusers and 17% rarely engaged with the internet at all [ 34 ]. With regard to the digital health divide, another Australian-based digital health divide study found that increased age, living in a lower socioeconomic area, being Aboriginal or Torres Strait Islander, being male, and having no tertiary education were factors negatively associated with access to digital health services [ 17 ]. Their findings correspond to our findings that higher-frequency users of eHealth were associated with younger age, being female, living in an urban area, and being employed. Both studies reinforce the evidence of the digital health divide based on gender, age, and socioeconomic disadvantage in Australia.
With regard to digital health barriers, our findings provide expanded details on the range of digital health items and services that present a cost barrier to consumers. Affordability is a known factor in digital access and digital health access, and it is measured often by general self-report or relative expenditure on internet access to income [ 30 ]. Our study revealed the comprehensive list of relevant costs for patients. Our study also demonstrated factors of cost affordability beyond the dollar value of an item, as interviewees described the struggle of using slow public internet access without privacy features and the risks involved in buying a computer in installments. When we reflected on the complexity and detail of the cost barrier in our survey, participants demonstrated a clear association between cost and the frequency of digital health use. This suggests that a way to improve digital health access for some people is to improve the quality, security, and accessibility of public internet access options as well as to provide free or subsidized hardware, internet connection, and maintenance options for those in need, work that is being done by at least 1 digital inclusion charity in the United Kingdom [ 35 ].
Many studies recognize the factors of eHealth literacy and digital confidence for beneficial digital health access [ 36 ]. Our interviews demonstrated that some patients with socioeconomic disadvantage have low digital confidence, but that this is often underlined by a socially reinforced lifelong low self-confidence in their intellectual ability. In contrast, active users, regardless of other demographic factors, described themselves as innately proactive question askers. This was reinforced by our finding of a relationship between health care empowerment and the frequency of eHealth use. This suggests that while digital health education and eHealth literacy programs can improve access for some patients, broader and deeper long-term solutions addressing socioeconomic drivers of digital exclusion are needed to improve digital health access for some patients with socioeconomic disadvantage [ 8 ]. The deep permeation of socially enforced low self-confidence and lifelong poverty experienced by some interviewees demonstrate that the provision of free hardware and a class on digital health skills can be, for some, a superficial offering when the key underlying factor is persistent general socioeconomic inequality.
The digital health divide literature tends to identify the digital health divide, the factors and barriers that contribute to it, and the potential for it to widen if not specifically addressed [ 16 ]. Our findings have also identified the divide and the barriers, but what this study adds through our qualitative phase in particular is a description of the complex interaction of those barriers and the stepped nature of some of those barriers as part of the individual’s experience in trying to access digital health.
Strengths and Limitations
A key strength of this study is the use of a sequential exploratory mixed methods design. The initial qualitative phase guided a phenomenological exploration of digital health access experiences for patients with chronic disease and socioeconomic disadvantage. Our results in both study phases stem from the patients’ real-life experiences of digital health access. While some of our results echo the findings of other survey-based studies on general digital and digital health participation, our method revealed a greater depth and detail of some of these barriers, as demonstrated in how our findings compare to prior work.
As mentioned previously, the emphasis of this study on the qualitative first phase is a strength that helped describe the interactions between different barriers. The interviewees described their experiences as cumulative unequal stepped barriers rather than as producing a nonordered list of equal barriers. These findings expand on the known complexity of the issue of digital exclusion and add weight to the understanding that improving digital health access needs diverse, complex solutions [ 17 ]. There is no panacea for every individual’s digital health access, and thus, patient-centered digital health services, often guided by health professionals within the continuity of primary care, are also required to address the digital health divide [ 37 ].
While the sequential exploratory design is a strength of the study, it also created some limitations for the second quantitative phase. Our commitment to using the qualitative interview findings to inform the survey questions meant that we were unable to use previously validated scales for every question and that our results were less likely to lead to a normal distribution. This likely affected our ability to demonstrate significant associations for some barriers. We expect that further modeling is required to control for baseline characteristics and determine barrier patterns for different types of users.
One strength of this study is that the survey was administered to a broad population of Australian family medicine patients with diverse patterns of health via both paper-based and digital options. Many other digital health studies use solely digital surveys, which can affect the sample. However, we cannot draw conclusions from our survey about patients with chronic disease due to the limitations of the sample size for these subgroups.
Another sample-based limitation of this study was that our qualitative population did not include anyone aged from 18 to 24 years, despite multiple efforts to recruit. Future research will hopefully address this demographic more specifically.
While not strictly a limitation, we recognize that because this research was before COVID-19, it did not include questions about telehealth, which has become much more mainstream in recent years. The patients may also have changed their frequency of eHealth use because of COVID-19 and an increased reliance on digital services in general. Future work in this area or future versions of this survey should include telehealth and acknowledge the impact of COVID-19. However, the larger concept of the digital health divide exists before and after COVID-19, and in fact, our widespread increased reliance on digital services makes the digital divide an even more pressing issue [ 12 ].
Conclusions
The experience of digital health access across Australian primary care is highly variable and more difficult to access for those with socioeconomic disadvantage. While general digital interest, financial cost, and digital health literacy and empowerment are clear factors in digital health access in a broad primary care population, the digital health divide is also facilitated in part by a stepped series of complex and cumulative barriers.
Genuinely improving digital health access for 1 cohort or even 1 person requires a series of multiple different interventions tailored to specific sequential barriers. Given the rapid expansion of digital health during the global COVID-19 pandemic, attention to these issues is necessary if we are to avoid entrenching inequities in access to health care. Within primary care, patient-centered care that continues to recognize the complex individual needs of, and barriers facing, each patient should be a part of addressing the digital health divide.
Acknowledgments
The authors are thankful to the patients who shared their experiences with them via interview and survey completion. The authors are also very grateful to the general practices in the Australian Capital Territory and New South Wales who kindly gave their time and effort to help organize interviews, administer, and post surveys in the midst of the stress of day-to-day practice life and the bushfires of 2018-2019. The authors thank and acknowledge the creators of the eHealth Literacy Scale, the eHealth Literacy Questionnaire, the ICEpop Capability Measure for Adults, the Health Care Empowerment Inventory, the Patient-Doctor Relationship Questionnaire, the Chao continuity questionnaire, and the Southgate Institute for Health Society and Equity for their generosity in sharing their work with the authors [ 17 , 19 - 25 ]. This study would not have been possible without the support of the administrative team of the Academic Unit of General Practice. This project was funded by the Royal Australian College of General Practitioners (RACGP) through the RACGP Foundation IPN Medical Centres Grant, and the authors gratefully acknowledge their support.
Data Availability
The data sets generated during this study are not publicly available due to the nature of our original ethics approval but are available from the corresponding author on reasonable request.
Authors' Contributions
MAC acquired the funding, conceptualized the project, and organized interview recruitment. MAC and KB conducted interviews and analyzed the qualitative data. EAS, ER, and KD contributed to project planning, supervision and qualitative data analysis. MAC, KB and KO wrote the survey and planned quantitative data analysis. MAC and KB recruited practices for survey administration. KO and KB conducted the quantitative data analysis. MAC and KO, with KB drafted the paper. EAS, ER, and KD helped with reviewing and editing the paper.
Conflicts of Interest
None declared.
Phase 1 interview guide.
Phase 2 survey: eHealth and digital divide.
Phase 2 participant characteristics by frequency of eHealth use.
- Eysenbach G. What is e-health? J Med Internet Res. 2001;3(2):E20. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Iyawa GE, Herselman M, Botha A. Digital health innovation ecosystems: from systematic literature review to conceptual framework. Procedia Comput Sci. 2016;100:244-252. [ FREE Full text ] [ CrossRef ]
- Berrouiguet S, Baca-García E, Brandt S, Walter M, Courtet P. Fundamentals for future mobile-health (mHealth): a systematic review of mobile phone and web-based text messaging in mental health. J Med Internet Res. Jun 10, 2016;18(6):e135. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Shen H, van der Kleij RM, van der Boog PJ, Chang X, Chavannes NH. Electronic health self-management interventions for patients with chronic kidney disease: systematic review of quantitative and qualitative evidence. J Med Internet Res. Nov 05, 2019;21(11):e12384. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Australia's health 2018. Australian Institute of Health and Welfare. 2018. URL: https://www.aihw.gov.au/reports/australias-health/australias-health-2018/contents/table-of-contents [accessed 2024-04-04]
- Australian Institute of Health and Welfare. Chronic Diseases and Associated Risk Factors in Australia, 2006. Canberra, Australia. Australian Institute of Health and Welfare; 2006.
- Hart JT. The inverse care law. The Lancet. Feb 27, 1971;297(7696):405-412. [ CrossRef ]
- Davies AR, Honeyman M, Gann B. Addressing the digital inverse care law in the time of COVID-19: potential for digital technology to exacerbate or mitigate health inequalities. J Med Internet Res. Apr 07, 2021;23(4):e21726. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Choi NG, Dinitto DM. The digital divide among low-income homebound older adults: internet use patterns, eHealth literacy, and attitudes toward computer/internet use. J Med Internet Res. May 02, 2013;15(5):e93. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Household use of information technology. Australian Bureau of Statistics. 2018. URL: https://tinyurl.com/4efm6u92 [accessed 2024-03-24]
- Kontos E, Blake KD, Chou WY, Prestin A. Predictors of eHealth usage: insights on the digital divide from the health information national trends survey 2012. J Med Internet Res. Jul 16, 2014;16(7):e172. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Litchfield I, Shukla D, Greenfield S. Impact of COVID-19 on the digital divide: a rapid review. BMJ Open. Oct 12, 2021;11(10):e053440. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Butler DC, Joshy G, Douglas KA, Sayeed MS, Welsh J, Douglas A, et al. Changes in general practice use and costs with COVID-19 and telehealth initiatives: analysis of Australian whole-population linked data. Br J Gen Pract. Apr 27, 2023;73(730):e364-e373. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Arsenijevic J, Tummers L, Bosma N. Adherence to electronic health tools among vulnerable groups: systematic literature review and meta-analysis. J Med Internet Res. Feb 06, 2020;22(2):e11613. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kontos EZ, Bennett GG, Viswanath K. Barriers and facilitators to home computer and internet use among urban novice computer users of low socioeconomic position. J Med Internet Res. Oct 22, 2007;9(4):e31. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Latulippe K, Hamel C, Giroux D. Social health inequalities and eHealth: a literature review with qualitative synthesis of theoretical and empirical studies. J Med Internet Res. Apr 27, 2017;19(4):e136. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Foley K, Freeman T, Ward P, Lawler A, Osborne R, Fisher M. Exploring access to, use of and benefits from population-oriented digital health services in Australia. Health Promot Int. Aug 30, 2021;36(4):1105-1115. [ CrossRef ] [ Medline ]
- Cresswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA. SAGE Publications; 2007.
- Tappen RM, Cooley ME, Luckmann R, Panday S. Digital health information disparities in older adults: a mixed methods study. J Racial Ethn Health Disparities. Feb 2022;9(1):82-92. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Who can get a card. Services Australia. URL: https://www.servicesaustralia.gov.au/who-can-get-health-care-card?context=21981 [accessed 2023-11-03]
- Levesque JF, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. Mar 11, 2013;12:18. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Bryant A, Charmaz K. The SAGE Handbook of Grounded Theory, Paperback Edition. Thousand Oaks, CA. SAGE Publications; 2010.
- Johnson MO, Rose CD, Dilworth SE, Neilands TB. Advances in the conceptualization and measurement of health care empowerment: development and validation of the health care empowerment inventory. PLoS One. 2012;7(9):e45692. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Norman CD, Skinner HA. eHEALS: the eHealth literacy scale. J Med Internet Res. Nov 14, 2006;8(4):e27. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kayser L, Karnoe A, Furstrand D, Batterham R, Christensen KB, Elsworth G, et al. A multidimensional tool based on the eHealth literacy framework: development and initial validity testing of the eHealth Literacy Questionnaire (eHLQ). J Med Internet Res. Feb 12, 2018;20(2):e36. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Standards. Australian Bureau of Statistics. URL: https://www.abs.gov.au/statistics/standards [accessed 2024-04-04]
- Al-Janabi H, Flynn TN, Coast J. Development of a self-report measure of capability wellbeing for adults: the ICECAP-A. Qual Life Res. Feb 2012;21(1):167-176. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Van der Feltz-Cornelis CM, Van Oppen P, Van Marwijk HW, De Beurs E, Van Dyck R. A patient-doctor relationship questionnaire (PDRQ-9) in primary care: development and psychometric evaluation. Gen Hosp Psychiatry. 2004;26(2):115-120. [ CrossRef ] [ Medline ]
- Chao J. Continuity of care: incorporating patient perceptions. Fam Med. 1988;20(5):333-337. [ Medline ]
- Wilson CK, Thomas J, Barraket J. Measuring digital inequality in Australia: the Australian digital inclusion index. JTDE. Jun 30, 2019;7(2):102-120. [ CrossRef ]
- Digital participation: a view of Australia's online behaviours. Australia Post. Jul 2017. URL: https://auspost.com.au/content/dam/auspost_corp/media/documents/white-paper-digital-inclusion.pdf [accessed 2024-04-04]
- Poli A, Kelfve S, Motel-Klingebiel A. A research tool for measuring non-participation of older people in research on digital health. BMC Public Health. Nov 08, 2019;19(1):1487. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences Second Edition. London, UK. Routledge; 1988.
- Borg K, Smith L. Digital inclusion and online behaviour: five typologies of Australian internet users. Behav Inf Technol. Feb 15, 2018;37(4):367-380. [ CrossRef ]
- Mathers A, Richardson J, Vincent S, Joseph C, Stone E. Good Things Foundation COVID-19 response report. Good Things Foundation. 2020. URL: https://tinyurl.com/2peu3kak [accessed 2024-04-04]
- Norman CD, Skinner HA. eHealth literacy: essential skills for consumer health in a networked world. J Med Internet Res. Jun 16, 2006;8(2):e9. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Neves AL, Burgers J. Digital technologies in primary care: implications for patient care and future research. Eur J Gen Pract. Dec 11, 2022;28(1):203-208. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by T Leung; submitted 03.07.23; peer-reviewed by T Freeman, H Shen; comments to author 16.08.23; revised version received 30.11.23; accepted 31.01.24; published 11.04.24.
©Melinda Ada Choy, Kathleen O'Brien, Katelyn Barnes, Elizabeth Ann Sturgiss, Elizabeth Rieger, Kirsty Douglas. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 11.04.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
This is a potential security issue, you are being redirected to https://csrc.nist.gov .
You have JavaScript disabled. This site requires JavaScript to be enabled for complete site functionality.
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Migrating Some Legacy e-Governance Applications to Post-Quantum Cryptography
Description.
This paper speaks about our experience in adding support for post-quantum cryptography to a number of software components underlying and supporting the e-Governance processes of Estonia. In the paper, we briefly introduce our approach with state of the art of post-quantum engineering and our methodology. Then, we describe several Estonia’s e-Government-related projects and provide an experience report about our efforts to make them quantum safe. We present some engineering problems we had to tackle with, different project-specific approaches, etc. Overall, we believe that this paper would be beneficial for the general audience interested in practical adoption of post-quantum cryptography.
Presented at
Event details.
Fifth PQC Standardization Conference

IMAGES
VIDEO
COMMENTS
Background: This systematic review aimed to extract recommendations from expert opinion articles on how to give a medical research presentation on a scientific conference and to determine whether the experts agree on what makes an effective or poor presentation. Methods: Presentation-related terms were searched within article titles listed in PubMed, restricting the search to English-language ...
Be 'pointer aware', that is don't point it at the audience. Try to control wild tremors by, if necessary, leaning on the podium to support your arm. The aim should be to inspire confidence in the paper being presented. The audience should be watching and listening to you, not just staring at the screen. 9.4.
Overview and General Information about Oral Presentation . Daily Presentations During Work Rounds; The New Patient Presentation ... In addition, the world of medicine presents some additional challenges, including: The structure of presentations varies from service to service (e.g. medicine vs. surgery), amongst subspecialties, and between ...
To begin with, you need to create an outline of the topics you might present at the meeting. Your outline should follow the IMRAC format (introduction, methods, results, and conclusion). This format is chosen because your audience understands it and expects it. If you have already prepared a paper for publication, it can be a rich source of ...
We sought to empirically identify what features of a scientific oral presentation experienced reviewers focus on when asked to identify the best features and areas to improve. ... Division of General Internal Medicine, 732 Faculty Office Tower, 510 Twentieth Street South, Birmingham, AL 35294-3407 ... How to present a scientific paper before a ...
The foundation of an outstanding journal club presentation rests on the choice of an interesting and well-written paper for discussion. Several resources are available to help you select important and timely research, including the American College of Physicians (ACP) Journal Club and the Diffusion section of The Hematologist.McMaster University has created the McMaster Online Rating of ...
Some programs do not use powerpoints or want your presentation under 5 mins.Regardless of the timing and format, every journal club presentation can be approached in this general format:Step 1: IntroductionExplain the clinical question that prompted you to consult the literature and what drew you to the article.Step 2: Who wrote the paper ...
The ability to design and deliver an effective presentation is an important skill for all learners to develop. The Undergraduate Medical Education Section of the Group on Educational Affairs developed this toolkit as a resource for medical students and health professions trainees as you learn to create and give effective presentations in the classroom, in the clinical setting, and at academic ...
Presentations are generally short and sharp, and careful preparation is key to ensure that the premise, findings, and relevance of your work are successfully conveyed. For most conference papers, the structure will mirror that of a scientific manuscript, with an introduction, materials and methods, results, discussion, and conclusions.
Despite enormous changes in medicine over the last 50 years, the oral presentation of newly admitted patients remains a core activity in academic teaching hospitals. With increased pace and complexity of care, it is time to refresh this tradition, as its efficiency and utility in contemporary practice are open to question. In this paper, we suggest a revised structure to help presenters ...
We read with great interest the paper by Rodin et al. 1 that describes an approach to preparing for oral presentations during clinical education experiences. We applaud the authors' comprehensive approach and the development of a tool that early learners will find useful in decreasing the non-germane cognitive load of preparing for and then delivering case presentations, which are both a ...
The art of presenting. The oral case presentation is a time-honoured tradition whereby a trainee presents a new admission to the attending physician. We describe the presentation styles of students, residents and staff physicians and offer pointers on how to present like stereotypical members of each group. Although the case presentation occurs ...
Medical presentations are a helpful tool for medical professionals, research clinics, and organizations to help inform and educate their communities on a wide variety of urgent topics. This can include patient treatment, clinical trial research and results, training for medical staff, general education, medical research, or important data ...
Presented a paper (Oral Presentation) on "Co infection of pneumocystis. carinii and cryptococcus neoformans" in the 2 nd Annual Conference of. Vidarbha Association of Medical Microbiology VAMMCON-2021 (online) held at Akola on 20 th and 21 st February, 2021. Maraskolhe D.
General Surgery articles covering presentation, surgical treatment, prognosis, and follow-up. Peer reviewed and up-to-date recommendations written by leading experts.
Introduction. Syphilis is caused by the bacterium Treponema pallidum subspecies pallidum . 1 This motile, gram-negative spirochete can be transmitted both sexually and from mother to child, and can invade virtually any organ or structure in the human body. The disease, which should be considered systemic throughout, is characterised by ...
A clinical and rhetorical definition with implications for teaching and learning the case-presentation format. Academic Medicine. 74(10):S124-S127. The Oral Presentation (A Practical Guide to Clinical Medicine, UCSD School of Medicine) ... Give a brief, general description of the patient including physical appearance. Then describe vital signs ...
Syphilis: presentations in general medicine. F. Nyatsanza, C. Tipple. Published in Clinical medicine (London) 1 April 2016. Medicine. TLDR. In this review, an update of modern syphilis epidemiology, clinical presentations, and testing and treatment strategies is provided. Expand.
Introduction. Syphilis is caused by the bacterium Treponema pallidum subspecies pallidum. 1 This motile, gram-negative spirochete can be transmitted both sexually and from mother to child, and can invade virtually any organ or structure in the human body. The disease, which should be considered systemic throughout, is characterised by overlapping clinical stages and a relapsing and remitting ...
A PGD medication was provided in 21% of consultations, including 79 patients for nitrofurantoin, 37 patients for fusidic acid and ten patients for phenoxymethylpenicillin.. Of patients accessing the service, 24% were under 13 and 12% were over 65 years of age. Reception staff referred 96% of patients.
Abstract. Ear, nose and throat (ENT) conditions present in about 10% of all GP consultations. The most common presentations include otalgia, cough, rhinorrhoea and deafness. These presentations are caused typically by self-limiting infections, but a small proportion is caused by rare or serious conditions needing referral to secondary care for ...
The Tamil Nadu Dr. MGR Medical University Chennai - 600 032. 2: Dr.Shravanthi G: Post Graduate student won the gold medal for paper presentation in Tapicon in 2020: 3: Dr. Athul Paul: Postgraduate has won the 2nd prize silver medal in Tapicon 2021 paper presentation: 4: Prof Dr. K.Subramaniyan
Peripheral artery disease, or PAD, continues to increase in prevalence worldwide due to risk factors such as advanced age, diabetes mellitus, and obesity. Critical limb ischemia (CLTI) is the advanced form of PAD that can result in lack of healing and limb loss as the most devastating consequence. Patients with PAD, especially CLTI, benefit from multidisciplinary care to optimize outcomes by ...
A total of 3260 patients were assigned to receive empagliflozin and 3262 to receive placebo. During a median follow-up of 17.9 months, a first hospitalization for heart failure or death from any ...
This paper is in the following e-collection/theme issue: Demographics of Users, Social & Digital Divide (651) E-Health Policy and Health Systems Innovation (192) Equity and Digital Divide (155) Use and User Demographics of mHealth (299) Health Care Quality and Health Services Research (209) Digital Health, Telehealth and e-Innovation in Clinical Settings (313)
This paper speaks about our experience in adding support for post-quantum cryptography to a number of software components underlying and supporting the e-Governance processes of Estonia. In the paper, we briefly introduce our approach with state of the art of post-quantum engineering and our methodology. Then, we describe several Estonia's e-Government-related projects and provide an ...